Antibiotics Self Medication among Children: A Systematic Review
Abstract
1. Introduction
2. Results
2.1. Study Characteristics
2.2. Antibiotics Self-Medication (ASM)
2.3. Parents’ Characteristics and Association with Antibiotic Self-Medication
2.3.1. Parents Relationship with Children
2.3.2. Age of Parents
2.3.3. Socioeconomic Status
2.3.4. Educational Level
2.3.5. Working in a Medical Field
2.3.6. Accessibility to Health Services
2.4. Parents’ Knowledge Associated with Antibiotics Self-Medication
2.4.1. Antimicrobial Resistance
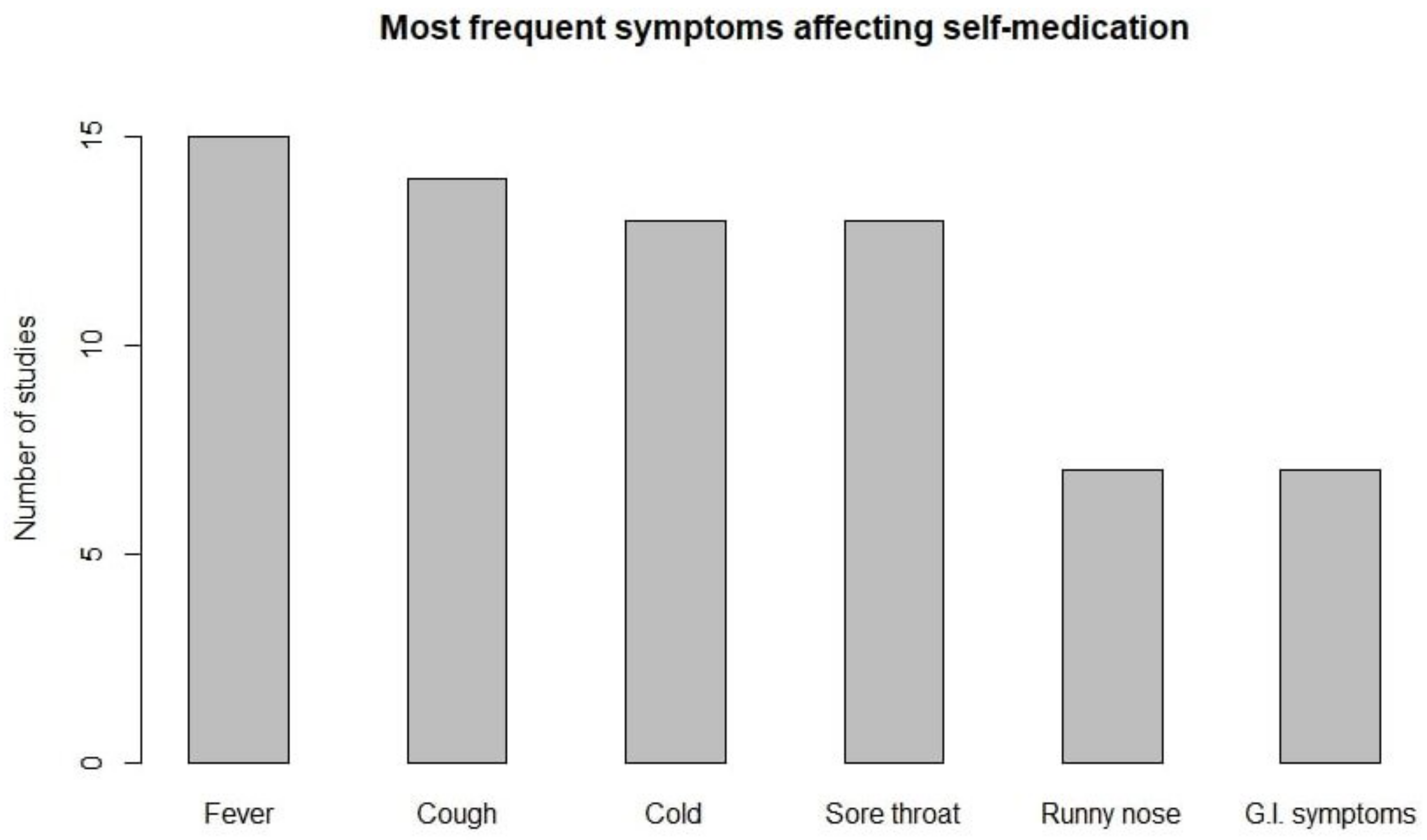
2.4.2. Symptoms Affecting ASM in Children
2.4.3. Antibiotics to Treat Viruses
2.4.4. Ability to Recognize Antibiotics
2.5. Parents’ Attitude Associated with Antibiotics Self-Medication
2.5.1. Management of Leftover Antibiotics
2.5.2. Experience with Antibiotics
2.5.3. Relationship with Physician
2.6. Children Features Associated with Antibiotic Self-Medication
2.6.1. Age of Children
2.6.2. Number of Children
2.6.3. Children Symptoms
2.6.4. Children Health Status Perception
2.7. Source of Information
2.7.1. Physicians
2.7.2. Pharmacists
2.7.3. Other Source of Information
2.8. Source of Antibiotics
2.8.1. Purchasing Antibiotics without Prescription
2.8.2. Leftover Antibiotics from Previous Prescribed Treatment
3. Materials and Methods
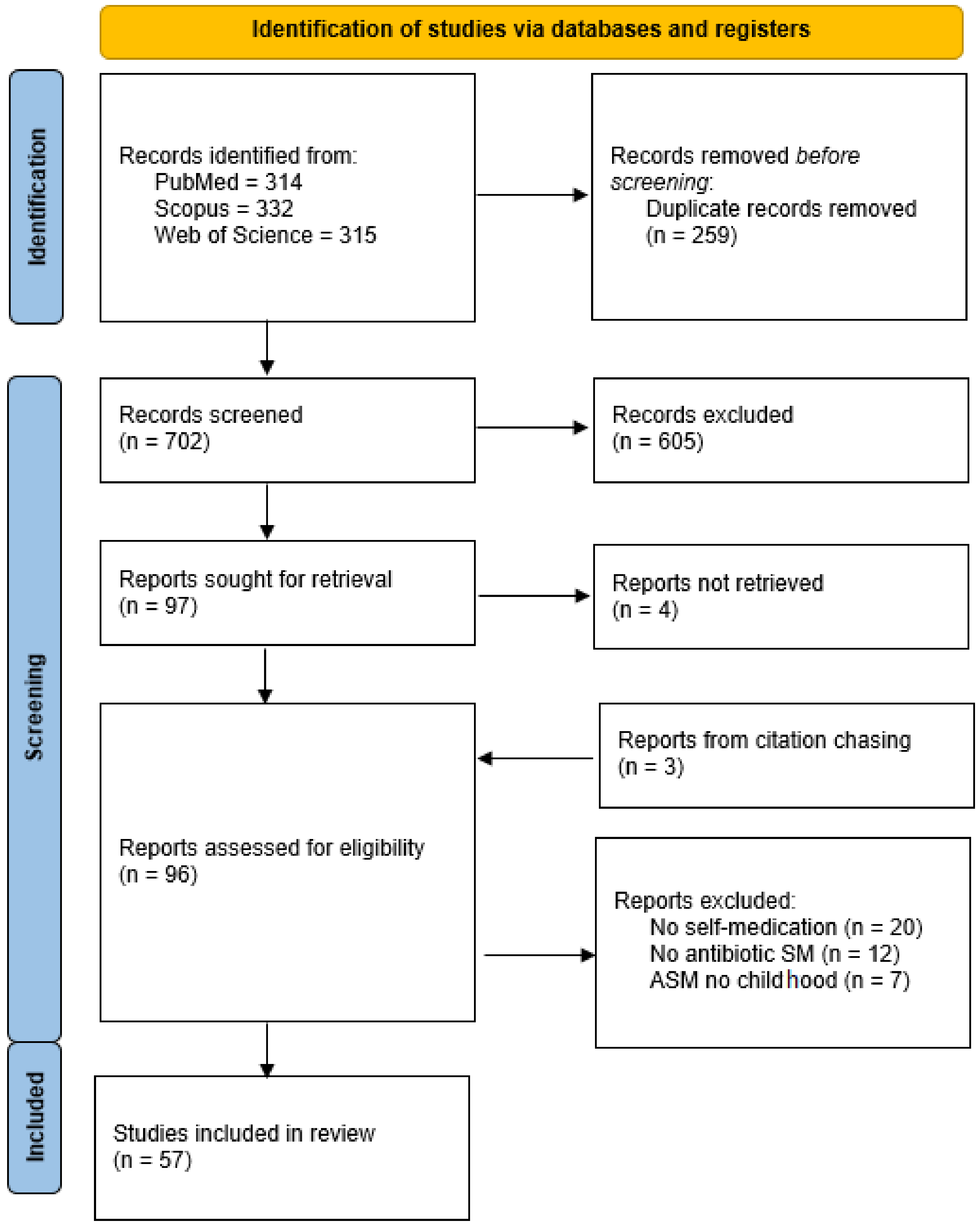
3.1. Search Strategy and Selection Criteria
3.2. Eligibility Criteria
- Study was available in English language.
- Study contained information about parental attitude to antibiotics self-medication.
- Study focused on infant, pre-school, or scholar-age children.
3.3. Definitions
- Self-medication consists in the self administration of medication not prescribed by a physician or in a manner not directed by a physician.
- Antibiotics or anti-bacterial agents are defined as substances that inhibit the growth or reproduction of bacteria.
- Children are divided by age in: infant (less than 2), pre-school (between 2 and 5), and school-age (between 6 and 12).
3.4. Data Extraction and Management
4. Discussion
Supplementary Materials
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AMR | Anti Microbial Resistance |
| ASM | Antibiotic Self-Medication |
| CI | Confidence Interval |
| OR | Odds Ratio |
References
- Murray, C.J.; Ikuta, K.S.; Sharara, F.; Swetschinski, L.; Aguilar, G.R.; Gray, A.; Han, C.; Bisignano, C.; Rao, P.; Wool, E.; et al. Global burden of bacterial antimicrobial resistance in 2019: A systematic analysis. Lancet 2022, 399, 629–655. [Google Scholar] [CrossRef]
- Shrivastava, S.R.; Shrivastava, P.S.; Ramasamy, J. World health organization releases global priority list of antibiotic-resistant bacteria to guide research, discovery, and development of new antibiotics. J. Med. Soc. 2018, 32, 76. [Google Scholar] [CrossRef]
- Thangaraju, P.; Venkatesan, S. WHO Ten threats to global health in 2019: Antimicrobial resistance. Cukurova Med. J. 2019, 44, 1150–1151. [Google Scholar]
- World Health Organization. Antimicrobial Resistance Surveillance in Europe 2022–2020 Data; World Health Organization: Geneva, Switzerland, 2022. [Google Scholar]
- World Health Organization. Monitoring and Evaluation of the Global Action Plan on Antimicrobial Resistance: Framework and Recommended Indicators; World Health Organization: Geneva, Switzerland, 2019. [Google Scholar]
- Kardas, P.; Devine, S.; Golembesky, A.; Roberts, C. A systematic review and meta-analysis of misuse of antibiotic therapies in the community. Int. J. Antimicrob. Agents 2005, 26, 106–113. [Google Scholar] [CrossRef]
- Wise, R. Antimicrobial resistance: Priorities for action. J. Antimicrob. Chemother. 2002, 49, 585–586. [Google Scholar] [CrossRef] [PubMed]
- Knopf, H.; Wolf, I.K.; Sarganas, G.; Zhuang, W.; Rascher, W.; Neubert, A. Off-label medicine use in children and adolescents: Results of a population-based study in Germany. BMC Public Health 2013, 13, 631. [Google Scholar] [CrossRef] [PubMed]
- Schillie, S.F.; Shehab, N.; Thomas, K.E.; Budnitz, D.S. Medication overdoses leading to emergency department visits among children. Am. J. Prev. Med. 2009, 37, 181–187. [Google Scholar] [CrossRef] [PubMed]
- Currie, J.; Lin, W.; Zhang, W. Patient knowledge and antibiotic abuse: Evidence from an audit study in China. J. Health Econ. 2011, 30, 933–949. [Google Scholar] [CrossRef]
- Eckel, N.; Sarganas, G.; Wolf, I.K.; Knopf, H. Pharmacoepidemiology of common colds and upper respiratory tract infections in children and adolescents in Germany. BMC Pharmacol. Toxicol. 2014, 15, 44. [Google Scholar] [CrossRef]
- Nyquist, A.C.; Gonzales, R.; Steiner, J.F.; Sande, M.A. Antibiotic prescribing for children with colds, upper respiratory tract infections, and bronchitis. JAMA 1998, 279, 875–877. [Google Scholar] [CrossRef]
- Goossens, H. Antibiotic consumption and link to resistance. Clin. Microbiol. Infect. 2009, 15, 12–15. [Google Scholar] [CrossRef]
- Shehnaz, S.I.; Agarwal, A.K.; Khan, N. A systematic review of self-medication practices among adolescents. J. Adolesc. Health 2014, 55, 467–483. [Google Scholar] [CrossRef]
- Gualano, M.R.; Bert, F.; Passi, S.; Stillo, M.; Galis, V.; Manzoli, L.; Siliquini, R. Use of self-medication among adolescents: A systematic review and meta-analysis. Eur. J. Public Health 2015, 25, 444–450. [Google Scholar] [CrossRef]
- Torres, N.F.; Chibi, B.; Kuupiel, D.; Solomon, V.P.; Mashamba-Thompson, T.P.; Middleton, L.E. The use of non-prescribed antibiotics; prevalence estimates in low-and-middle-income countries. A systematic review and meta-analysis. Arch. Public Health 2021, 79, 2. [Google Scholar] [CrossRef]
- Lescure, D.; Paget, J.; Schellevis, F.; Van Dijk, L. Determinants of self-medication with antibiotics in European and Anglo-Saxon countries: A systematic review of the literature. Front. Public Health 2018, 6, 370. [Google Scholar] [CrossRef]
- Jasim, A. Parental self medication of antibiotics for children in Baghdad city. Int. J. Pharm. Pharm. Sci. 2014, 6, 485–489. [Google Scholar]
- Maltezou, H.C.; Dedoukou, X.; Asimaki, H.; Kontou, I.; Ioannidou, L.; Mitromara, K.; Theodoridou, K.; Katerelos, P.; Theodoridou, M. Consumption of antibiotics by children in Greece: A cross-sectional study. Int. J. Pediatr. Adolesc. Med. 2017, 4, 108–111. [Google Scholar] [CrossRef]
- Al-Ayed, M.S.Z. Parents’ knowledge, attitudes and practices on antibiotic use by children. Saudi J. Med. Med. Sci. 2019, 7, 93. [Google Scholar] [CrossRef]
- Abdulaziz, H.A.; Haytham, A.S.; Faiza, N.A.; Abdulaziz, U.J.; Rowayda, M.M.; Amna, R.S.; Abdulaziz, B.S. Socio-demographic determinants of antibiotic misuse in children. A survey from the central region of Saudi Arabia. Saudi Med. J. 2013, 34, 832–840. [Google Scholar]
- Ochoa, T.J.; Balmaceda, M.P.; Elias, R.; Navarro, R.; Watanabe, T.; Moran, F.; Paredes, J.L.; Reategui, A.; Bardellini, M. Knowledge, attitudes and practices of parents towards antibiotic use in rural communities in Peru: A cross-sectional multicentre study. BMC Public Health 2022, 22, 459. [Google Scholar]
- Afolabi, B.; Brieger, W.; Salako, L. Management of childhood febrile illness prior to clinic attendance in urban Nigeria. J. Health Popul. Nutr. 2004, 2, 46–51. [Google Scholar]
- Afolabi, O.A.; Ehalaiye, B.F.; Fadare, J.O.; Abdur-Rahman, A.B.; Ehalaiye, D.N. Survey of ototopical self medication among patients attending ENT and family medicine departments in a Nigerian hospital. Eur. J. Gen. Pract. 2011, 17, 167–170. [Google Scholar] [CrossRef] [PubMed]
- Al-Shawi, M.M.; Darwish, M.A.; Wahab, M.M.A.; Al-Shamlan, N.A. Misconceptions of parents about antibiotic use in upper respiratory tract infections: A survey in primary schools of the Eastern province, KSA. J. Fam. Community Med. 2018, 25, 5. [Google Scholar]
- Solangi, M.A.; Ali, M.; Mushtaq, D.; Zaid, M.; Riaz, M.; Nasir, A. Parent-based self-medication in Pakistani children: A qualitative cross-sectional survey. Bangladesh J. Med. Sci. 2016, 15, 33–38. [Google Scholar] [CrossRef]
- Bi, P.; Tong, S.; Parton, K.A. Family self-medication and antibiotics abuse for children and juveniles in a Chinese city. Soc. Sci. Med. 2000, 50, 1445–1450. [Google Scholar] [CrossRef]
- Cantarero-Arévalo, L.; Hallas, M.P.; Kaae, S. Parental knowledge of antibiotic use in children with respiratory infections: A systematic review. Int. J. Pharm. Pract. 2017, 25, 31–49. [Google Scholar] [CrossRef]
- Chang, J.; Lv, B.; Zhu, S.; Yu, J.; Zhang, Y.; Ye, D.; Aziz, M.M.; Yang, C.; Fang, Y. Non-prescription use of antibiotics among children in urban China: A cross-sectional survey of knowledge, attitudes, and practices. Expert Rev. Anti-Infect. Ther. 2018, 16, 163–172. [Google Scholar] [CrossRef]
- Cruz, M.J.; Dourado, L.F.; Bodevan, E.C.; Andrade, R.A.; Santos, D.F. Medication use among children 0–14 years old: Population baseline study. J. Pediatr. 2014, 90, 608–615. [Google Scholar] [CrossRef][Green Version]
- Santos, D.B.d.; Barreto, M.L.; Coelho, H.L.L. Use of prescribed and non-prescribed medications among children living in poor areas in the city of Salvador, Bahia State, Brazil. Cad. Saúde Pública 2011, 90, 2032–2040. [Google Scholar] [CrossRef][Green Version]
- Ecker, L.; Ochoa, T.J.; Ruiz, J.; Vargas, M.; Del Valle, L.J. Caretakers knowledge, attitude and practices about antibiotics use in childrens in a setting where antibiotics are available without medical prescription. Am. J. Trop. Med. Hyg. 2010, 83, 278. [Google Scholar]
- Ecker, L.; Ochoa, T.J.; Vargas, M.; Del Valle, L.J.; Ruiz, J. Factors affecting caregivers’ use of antibiotics available without a prescription in Peru. Pediatrics 2013, 131, e1771–e1779. [Google Scholar] [CrossRef]
- Edwards, D.J.; Richman, P.B.; Bradley, K.; Eskin, B.; Mandell, M. Parental use and misuse of antibiotics: Are there differences in urban vs. suburban settings? Acad. Emerg. Med. Off. J. Soc. Acad. Emerg. Med. 2002, 9, 22–26. [Google Scholar] [CrossRef][Green Version]
- Elong Ekambi, G.A.; Okalla Ebongue, C.; Penda, I.C.; Nnanga Nga, E.; Mpondo Mpondo, E.; Eboumbou Moukoko, C.E. Knowledge, practices and attitudes on antibiotics use in Cameroon: Self-medication and prescription survey among children, adolescents and adults in private pharmacies. PLoS ONE 2019, 14, e0212875. [Google Scholar] [CrossRef]
- El-Hawy, R.M.; Ashmawy, M.I.; Kamal, M.M.; Khamis, H.A.; El-Hamed, N.M.A.; Eladely, G.I.; Abdo, M.H.; Hashem, Y.; Ramadan, M.; Hamdy, D.A. Studying the knowledge, attitude and practice of antibiotic misuse among Alexandria population. Eur. J. Hosp. Pharm. 2017, 24, 349–354. [Google Scholar] [CrossRef]
- Gungor, A.; Cakir, B.; Yalcin, H.; Cakir, H.; Karauzun, A. Evaluation of parents’ attitudes and behaviors related to the use of antibiotics in children. Turk. J. Pediatr. Dis. 2019, 13, 203–207. [Google Scholar]
- Ivanovska, V.; Angelovska, B.; Van Dijk, L.; Zdravkovska, M.; Leufkens, H.G.; Mantel-Teeuwisse, A.K. Change in parental knowledge, attitudes and practice of antibiotic use after a national intervention programme. Eur. J. Public Health 2018, 28, 724–729. [Google Scholar] [CrossRef]
- Ivanovska, V.; Zdravkovska, M.; Bosevska, G.; Angelovska, B. Antibiotics for upper respiratory infections: Public knowledge, beliefs and self-medication in the Republic of Macedonia. Contrib. Sec. Biol. Med. Sci. 2013, 34, 60–70. [Google Scholar]
- Kadam, Y.R.; Pimple, A.N.; Dhumale, G.B.; Gore, A.D.; Patil, S.A. Parental Use of Antibiotics as Self Medication to Their School Going Children: A Cross Sectional Study. J. Krishna Inst. Med Sci. (JKIMSU) 2018, 7, 16–24. [Google Scholar]
- Lin, L.; Harbarth, S.; Hargreaves, J.R.; Zhou, X.; Li, L. Large-scale survey of parental antibiotic use for paediatric upper respiratory tract infections in China: Implications for stewardship programmes and national policy. Int. J. Antimicrob. Agents 2021, 57, 106302. [Google Scholar] [CrossRef]
- Lin, L.; Harbarth, S.; Wang, X.; Zhou, X. Survey of parental use of antimicrobial drugs for common childhood infections, China. Emerg. Infect. Dis. 2020, 26, 1517. [Google Scholar] [CrossRef]
- Metlo, M.; Ubed-Ur-Rehman, M.A.; Dayo, A.; Ahmed, Z.; Arain, M.I.; Parveen, R.; Memon, A. Evaluation of Sources of Information and Reasons for Self-Medication by Educated Parents Among Their Children in District Khairpur, Pakistan. Lat. Am. J. Pharm. 2019, 38, 110–115. [Google Scholar]
- Mohanna, M. Self-medication with antibiotic in children in Sana’a City, Yemen. Oman Med. J. 2010, 25, 41. [Google Scholar] [CrossRef] [PubMed]
- Mukattash, T.L.; Alkhatatbeh, M.J.; Andrawos, S.; Jarab, A.S.; AbuFarha, R.K.; Nusair, M.B. Parental self-medication of antibiotics for children in Jordan. J. Pharm. Health Serv. Res. 2020, 11, 75–80. [Google Scholar] [CrossRef]
- Nazir, S.; Goel, K.; Mittal, A.; Singh, J.; Goel, R.; Rashid, A. Parent induced self-medication among under five children: An observational cross sectional study. TAF Prev. Med. Bull. 2015, 14, 81–86. [Google Scholar] [CrossRef]
- Nyeko, R.; Otim, F.; Obiya, E.M.; Abala, C. Pre-hospital exposures to antibiotics among children presenting with fever in northern Uganda: A facility-based cross-sectional study. BMC Pediatr. 2022, 22, 322. [Google Scholar] [CrossRef] [PubMed]
- Okide, C.; Grey-Ekejiuba, O.; Ubaka, C.; Schellack, N.; Okonta, M. Parents’ Knowledge, Attitudes and Use of Antibiotics in Upper Respiratory Infections in Nigerian Children. Afr. J. Biomed. Res. 2020, 23, 213–220. [Google Scholar]
- Oshikoya, K.; Njokanma, O.; Bello, J.; Ayorinde, E. Family self-medication for children in an urban area of Nigeria. Paediatr. Perinat. Drug Ther. 2007, 8, 124. [Google Scholar] [CrossRef]
- Oshikoya, K. The Use of Prescribed and Non-Prescribed Drugs in Infants in Lagos, Nigeria “KA Oshikoya,“OF. Njokanma,” JA Bello and” EO Ayorinde. J. Med. Sci 2008, 8, 111–117. [Google Scholar]
- Parimi, N.; Pereira, L.M.P.; Prabhakar, P. Caregivers’ practices, knowledge and beliefs of antibiotics in paediatric upper respiratorytract infections in Trinidad and Tobago: A cross-sectional study. BMC Fam. Pract. 2004, 5, 28. [Google Scholar] [CrossRef]
- Peker, E.; Sahin, E.M.; Topaloğlu, N.; Uludağ, A.; Ağaoğlu, H.; Güngör, S. Knowledge, attitude and behavior of mothers related to acute respiratory infections. Minerva Pediatr. 2014, 68, 114–120. [Google Scholar]
- Revathi, B.; Pandurangan, K.K. A Cross Sectional Survey of Knowledge, Attitude and Practice of Antibiotic Use for Children in Chennai among Mothers. J. Pharm. Res. Int. 2020, 32, 103–112. [Google Scholar] [CrossRef]
- Salama, R.A.; Bader, K.N.; Rahmen, A.S.; Hashmi, F. Parents Knowledge, attitude and practice of antibiotic use for upper respiratory tract infections in children: A cross-sectional study in Ras Al khaimah, United Arab Emirates. Epidemiol. Biostat. Public Health 2018, 15. [Google Scholar] [CrossRef]
- Sharif, S.I.; Masalmeh, B.E.; Awad, H.; Osama, A.; Abdulmqasood, Y.A.; Bugaighis, L.M. Parents’ knowledge and attitude to self-medication of children with antibiotics. Arch. Pharm. Pract. 2015, 6, 71. [Google Scholar] [CrossRef]
- Simon, B.; Kazaura, M. Prevalence and factors associated with parents self-medicating under-fives with antibiotics in Bagamoyo District Council, Tanzania: A cross-sectional study. Patient Prefer. Adherence 2020, 14, 1445. [Google Scholar] [CrossRef]
- Sun, C.; Hu, Y.J.; Wang, X.; Lu, J.; Lin, L.; Zhou, X. Influence of leftover antibiotics on self-medication with antibiotics for children: A cross-sectional study from three Chinese provinces. BMJ Open 2019, 9, e033679. [Google Scholar] [CrossRef]
- Szenborn, L.; Maciaga, P.; Dul, A.; Bortnowska, K.; Jasonek, J. Antibiotic therapy in children–Knowledge and behavior of parents. Pediatr. Pol. 2017, 92, 699–704. [Google Scholar] [CrossRef]
- Togoobaatar, G.; Ikeda, N.; Ali, M.; Sonomjamts, M.; Dashdemberel, S.; Mori, R.; Shibuya, K. Survey of non-prescribed use of antibiotics for children in an urban community in Mongolia. Bull. World Health Organ. 2010, 88, 930–936. [Google Scholar] [CrossRef]
- Xu, J.; Wang, X.; Sun, K.S.; Lin, L.; Zhou, X. Parental self-medication with antibiotics for children promotes antibiotic over-prescribing in clinical settings in China. Antimicrob. Resist. Infect. Control 2020, 9, 150. [Google Scholar] [CrossRef]
- Xu, Y.; Lu, J.; Sun, C.; Wang, X.; Hu, Y.J.; Zhou, X. A cross-sectional study of antibiotic misuse among Chinese children in developed and less developed provinces. J. Infect. Dev. Ctries 2020, 14, 129–137. [Google Scholar] [CrossRef]
- Yu, M.; Zhao, G.; Stålsby Lundborg, C.; Zhu, Y.; Zhao, Q.; Xu, B. Knowledge, attitudes, and practices of parents in rural China on the use of antibiotics in children: A cross-sectional study. BMC Infect. Dis. 2014, 14, 112. [Google Scholar] [CrossRef]
- Yuan, J.; Du, W.; Li, Z.; Deng, Q.; Ma, G. Prevalence and Risk Factors of Self-Medication Among the Pediatric Population in China: A National Survey. Front. Public Health 2021, 9, 770709. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Mendoza, R.; Costa, M.M.; Ottoni, E.J.; Bertaco, A.S.; Santos, J.C.; D’avila, N.E.; Faria, C.S.; Zenobini, E.C.; Gomesa, A. Antibiotic use in community-based pediatric outpatients in southern region of Brazil. J. Trop. Pediatr. 2005, 51, 304–309. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Z.; Zhao, D.; Zhang, H.; Shen, C.; Cao, D.; Liu, G.; Zhu, L.; Fang, Y. Understanding parental self-medication with antibiotics among parents of different nationalities: A cross-sectional study. Glob. Health Res. Policy 2021, 6, 42. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Y.; Tang, X.; Yan, R.; Shao, Z.; Zhou, Y.; Deng, X.; Luo, S.; He, H. Non-prescription antibiotic use for cough among Chinese children under 5 years of age: A community-based cross-sectional study. BMJ Open 2021, 11, e051372. [Google Scholar] [CrossRef] [PubMed]
- Zyoud, S.H.; Abu Taha, A.; Araj, K.F.; Abahri, I.A.; Sawalha, A.F.; Sweileh, W.M.; Awang, R.; Al-Jabi, S.W. Parental knowledge, attitudes and practices regarding antibiotic use for acute upper respiratory tract infections in children: A cross-sectional study in Palestine. BMC Pediatr. 2015, 15, 176. [Google Scholar] [CrossRef]
- Chakraborty, K.; Chakraborty, A.; Devi, S.; Devi, J. Family self medication in children attending a tertiary care hospital in Northeast India. Int. J. Pharm. Sci. Res. 2012, 3, 4899. [Google Scholar]
- Pfaffenbach, G.; Tourinho, F.S.; Bucaretchi, F. Self-medication among children and adolescents. Curr. Drug Saf. 2010, 5, 324–328. [Google Scholar] [CrossRef]
- Palmer, D.A.; Bauchner, H. Parents’ and physicians’ views on antibiotics. Pediatrics 1997, 99, e6. [Google Scholar] [CrossRef]
- Rousounidis, A.; Papaevangelou, V.; Hadjipanayis, A.; Panagakou, S.; Theodoridou, M.; Syrogiannopoulos, G.; Hadjichristodoulou, C. Descriptive study on parents’ knowledge, attitudes and practices on antibiotic use and misuse in children with upper respiratory tract infections in Cyprus. Int. J. Environ. Res. Public Health 2011, 8, 3246–3262. [Google Scholar] [CrossRef]
- Panagakou, S.G.; Spyridis, N.; Papaevangelou, V.; Theodoridou, K.M.; Goutziana, G.P.; Theodoridou, M.N.; Syrogiannopoulos, G.A.; Hadjichristodoulou, C.S. Antibiotic use for upper respiratory tract infections in children: A cross-sectional survey of knowledge, attitudes, and practices (KAP) of parents in Greece. BMC Pediatr. 2011, 11, 60. [Google Scholar] [CrossRef]
- Cristescu, C.; Negreș, S.; Suciu, M.; Voicu, A.; Buda, V.; Suciu, L.; Proks, M.; Voicu, M. Study regarding the parents’ use of self–medication among children under 12 years old. Farmacia 2018, 66, 811–819. [Google Scholar] [CrossRef]
- Penda, C.I.; Moukoko, E.C.E.; Youmba, J.F.N.; Mpondo, E.M. Characterization of pharmaceutical medication without a medical prescription in children before hospitalization in a resource-limited setting, Cameroon. Pan Afr. Med. J. 2018, 30, 302. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Syst. Rev. 2021, 10, 1–11. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2018. [Google Scholar]
- Batista, A.D.; Rodrigues, D.A.; Figueiras, A.; Zapata-Cachafeiro, M.; Roque, F.; Herdeiro, M.T. Antibiotic dispensation without a prescription worldwide: A systematic review. Antibiotics 2020, 9, 786. [Google Scholar] [CrossRef]
- Belachew, S.A.; Hall, L.; Selvey, L.A. Non-prescription dispensing of antibiotic agents among community drug retail outlets in Sub-Saharan African countries: A systematic review and meta-analysis. Antimicrob. Resist. Infect. Control 2021, 10, 13. [Google Scholar] [CrossRef]
- Chang, J.; Ye, D.; Lv, B.; Jiang, M.; Zhu, S.; Yan, K.; Tian, Y.; Fang, Y. Sale of antibiotics without a prescription at community pharmacies in urban China: A multicentre cross-sectional survey. J. Antimicrob. Chemother. 2017, 72, 1235–1242. [Google Scholar] [CrossRef]
- Auta, A.; Hadi, M.A.; Oga, E.; Adewuyi, E.O.; Abdu-Aguye, S.N.; Adeloye, D.; Strickland-Hodge, B.; Morgan, D.J. Global access to antibiotics without prescription in community pharmacies: A systematic review and meta-analysis. J. Infect. 2019, 78, 8–18. [Google Scholar] [CrossRef]


| Features Associated with ASM | Risk of ASM 1 | Citation |
|---|---|---|
| Child relationship: Mother | OR 0.30 (0.09–0.96) | Nyeko et al. [47] |
| OR 0.83 (0.74-0.94) | Sun et al. [57] | |
| Child relationship: Father | OR 0.74 (0.4–1.3) | Abdulaziz H et al. [21] |
| OR 0.53 (0.3–0.96) | Zhu et al. [66] | |
| OR 1.27 (1.1–1.5) | Yuan et al. [63] | |
| High distance from hospital/Rural Area | OR 3.70 (1.9–7.2) | Nyeko et al. [47] |
| OR 1.20 (1.1–1.3) | Simon and Kazaura [56] | |
| OR 1.60 (1.1–2.4) | Yu et al. [62] | |
| Low/middle Economic Status | OR 4.44 (1.5–19.0) | Zhu et al. [66] |
| OR 3.60 (1.3–9.7) | Zhou et al. [65] | |
| OR 2.00 (1.1–3.8) | Abdulaziz H et al. [21] | |
| High Economic Status | OR 0.66 (0.5–1) | Sun et al. [57] |
| Having medical insurance | OR 0.36 (0.1–1) | Zhou et al. [65] |
| OR 2.31 (1.4–4.0) | Bi et al. [27] | |
| OR 1.30 (1.1–1.6) | Chang et al. [29] | |
| High level of instruction | OR 0.71 (0.5–1) | Sun et al. [57] |
| OR 0.34 (0.2–0.5) | Zhang et al. [64] | |
| Working in medical field | OR 1.38 (1.1–1.7) | Chang et al. [29] |
| OR 2.74 (1.1–7.1) | Zhou et al. [65] | |
| Medium ability to recognize antibiotics | OR 1.55 (1.1–2.1) | Lin et al. [41] |
| High ability to recognize antibiotics | OR 1.73 (1.3–2.3) | Lin et al. [41] |
| Tendency toward self-medication | OR 6.30 (3.8–10.5) | Togoobaatar et al. [59] |
| Requesting antibiotics to physician | OR 3.22 (1.2-8.6) | Xu et al. [60] |
| Knowing antibiotics should be prescribed | OR 0.77 (0.7–0.9) | Chang et al. [29] |
| Features Associated with ASM | Risk of ASM 1 | Citation |
|---|---|---|
| Age of children | OR 1.30 (1.1–1.4) | Ecker et al. [33] |
| OR 1.15 (1.1–1.3) | Yu et al. [62] | |
| Having more than one child | OR 2.17 (1.5–3.2) | Yu et al. [62] |
| OR 1.68 (1.0–2.9) | Abdulaziz H et al. [21] | |
| Children poor health status | OR 2.10 (1.75–2.5) 2 | Chang et al. [29] |
| OR 1.76 (1.40–2.23) | Lin et al. [41] | |
| Fever | OR 1.89 (1.6–2.3) | Lin et al. [41] |
| Cough | OR 3.54 (1.6–8.1) | Nyeko et al. [47] |
| Diarrhea | OR 8.00 (3.3–19.3) | Nyeko et al. [47] |
| Runny Nose | OR 1.86 (1.13–3.19) | Zhu et al. [66] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bert, F.; Previti, C.; Calabrese, F.; Scaioli, G.; Siliquini, R. Antibiotics Self Medication among Children: A Systematic Review. Antibiotics 2022, 11, 1583. https://doi.org/10.3390/antibiotics11111583
Bert F, Previti C, Calabrese F, Scaioli G, Siliquini R. Antibiotics Self Medication among Children: A Systematic Review. Antibiotics. 2022; 11(11):1583. https://doi.org/10.3390/antibiotics11111583
Chicago/Turabian StyleBert, Fabrizio, Christian Previti, Francesco Calabrese, Giacomo Scaioli, and Roberta Siliquini. 2022. "Antibiotics Self Medication among Children: A Systematic Review" Antibiotics 11, no. 11: 1583. https://doi.org/10.3390/antibiotics11111583
APA StyleBert, F., Previti, C., Calabrese, F., Scaioli, G., & Siliquini, R. (2022). Antibiotics Self Medication among Children: A Systematic Review. Antibiotics, 11(11), 1583. https://doi.org/10.3390/antibiotics11111583







