An in vitro Study of Betadine’s Ability to Eliminate Live Bacteria on the Eye: Should It Be Used for Protection against Endophthalmitis?
Abstract
:1. Introduction
2. Materials and Methods:
2.1. Povidone-Iodide Solution Preparation
2.2. Bacterial Strains, Media, and Growth Conditions
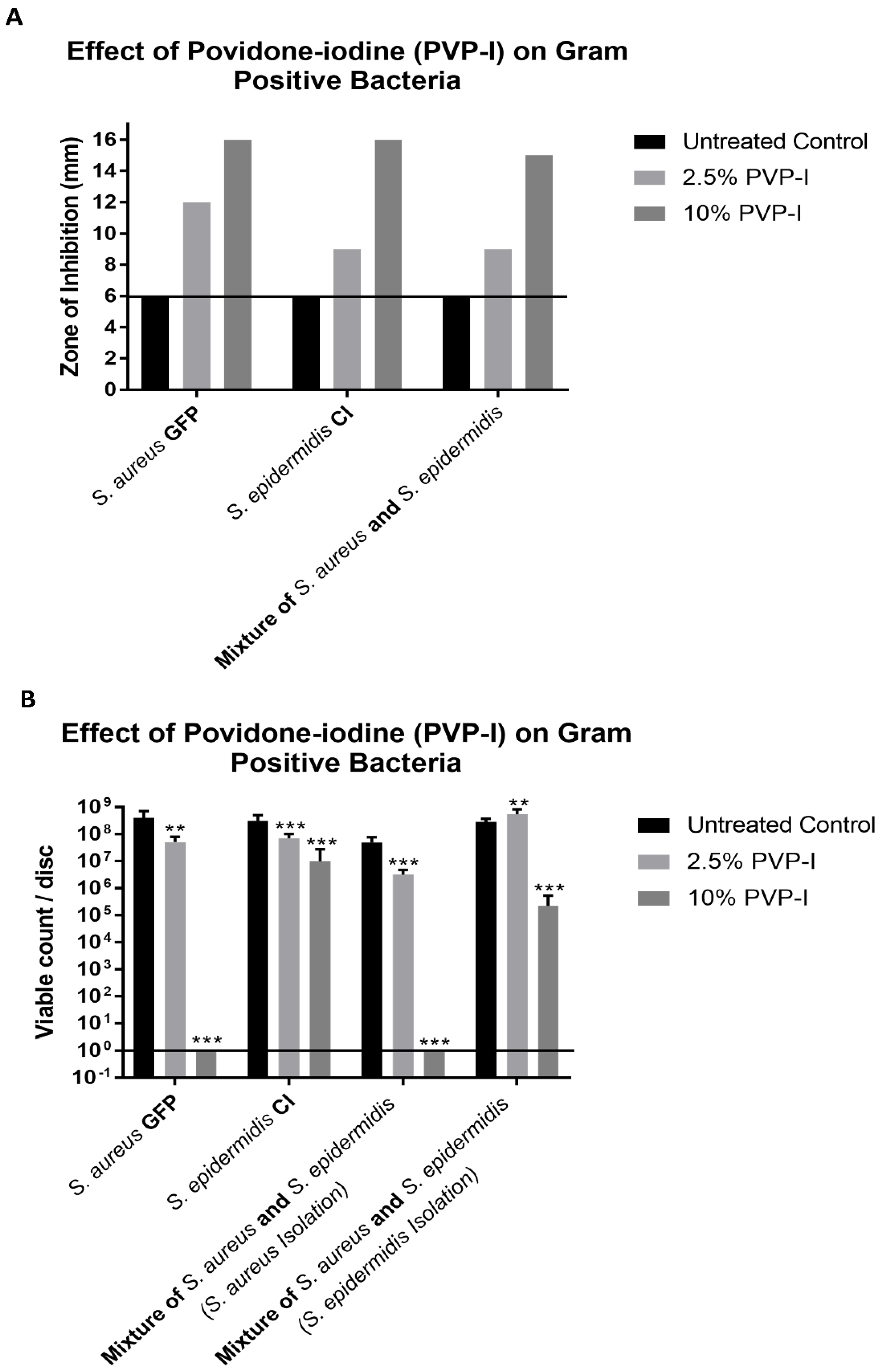
2.3. Zone of Inhibition (ZOI) Assay
2.4. Colony Forming Unit (CFU) Assay on the Betadine Treated Disc
2.5. Confocal Laser Scanning Microscopy (CLSM)
2.6. Bacterial Combination Assay
2.7. Zero-Hour Biofilm Assay
2.8. 24-Hour Biofilm Assay
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Grzybowski, A.; Kanclerz, P.; Myers, W.G. The use of povidone-iodine in ophthalmology. Curr. Opin. Ophthalmol. 2018, 29, 19–32. [Google Scholar] [CrossRef] [PubMed]
- Junka, A.; Bartoszewicz, M.; Smutnicka, D.; Secewicz, A.; Szymczyk, P. Efficacy of antiseptics containing povidone-iodine, octenidine dihydrochloride and ethacridine lactate against biofilm formed by Pseudomonas aeruginosa and Staphylococcus aureus measured with the novel biofilm-oriented antiseptics test. Int. Wound J. 2014, 11, 730–734. [Google Scholar] [CrossRef] [PubMed]
- Lepelletier, D.; Maillard, J.Y.; Pozzetto, B.; Simon, A. Povidone Iodine: Properties, Mechanisms of Action, and Role in Infection Control and Staphylococcus aureus Decolonization. Antimicrob. Agents Chemother. 2020, 64, e00682-20. [Google Scholar] [CrossRef] [PubMed]
- Bigliardi, P.L.; Alsagoff, S.A.L.; El-Kafrawi, H.Y.; Pyon, J.K.; Wa, C.T.C.; Villa, M.A. Povidone iodine in wound healing: A review of current concepts and practices. Int. J. Surg. 2017, 44, 260–268. [Google Scholar] [CrossRef] [PubMed]
- Duan, F.; Wu, K.; Liao, J.; Zheng, Y.; Yuan, Z.; Tan, J.; Lin, X. Causative Microorganisms of Infectious Endophthalmitis: A 5-Year Retrospective Study. J. Ophthalmol. 2016, 2016, 6764192. [Google Scholar] [CrossRef] [Green Version]
- Goswami, K.; Austin, M.S. Intraoperative povidone-iodine irrigation for infection prevention. Arthroplast. Today 2019, 5, 306–308. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Isenberg, S.J.; Apt, L.; Campeas, D. Ocular Applications of Povidone-Iodine. Dermatology 2002, 204, 92–95. [Google Scholar] [CrossRef]
- Darouiche, R.O.; Wall, M.J., Jr.; Itani, K.M.F.; Otterson, M.F.; Webb, A.L.; Carrick, M.M.; Miller, H.J.; Awad, S.S.; Crosby, C.T.; Mosier, M.C.; et al. Chlorhexidine-Alcohol versus Povidone-Iodine for Surgical-Site Antisepsis. N. Engl. J. Med. 2010, 362, 18–26. [Google Scholar] [CrossRef] [Green Version]
- Stranz, C.V.; Fraenkel, G.E.; Butcher, A.R.; Esterman, A.J.; Goggin, M.J. Survival of bacteria on the ocular surface following double application of povidone-iodine before cataract surgery. Eye 2011, 25, 1423–1428. [Google Scholar] [CrossRef] [Green Version]
- Reibaldi, M.; Avitabile, T.; Bandello, F.; Longo, A.; Bonfiglio, V.; Russo, A.; Castellino, N.; Rejdak, R.; Nowomiejska, K.; Toro, M.; et al. The Effectiveness of 0.6% Povidone Iodine Eye Drops in Reducing the Conjunctival Bacterial Load and Needle Contamination in Patients Undergoing Anti-VEGF Intravitreal Injection: A Prospective, Randomized Study. J. Clin. Med. 2019, 8, 1031. [Google Scholar] [CrossRef]
- Wass, S.; Albrektsen, G.; Ødegård, M.T.; Sand, M.; Austeng, D. Antiseptic effect of low-concentration povidone-iodine applied with a depot device in the conjunctiva before cataract surgery. Eye 2018, 32, 1900–1907. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ferguson, A.W.; Scott, J.A.; McGavigan, J.; Elton, R.A.; McLean, J.; Schmidt, U.; Kelkar, R.; Dhillon, B. Comparison of 5% povidone-iodine solution against 1% povidone-iodine solution in preoperative cataract surgery antisepsis: A prospective randomised double blind study. Br. J. Ophthalmol. 2003, 87, 163–167. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hosseini, H.; Ashraf, M.J.; Saleh, M.; Nowroozzadeh, M.H.; Nowroozizadeh, B.; Abtahi, M.B.; Nowroozizadeh, S. Effect of povidone–iodine concentration and exposure time on bacteria isolated from endophthalmitis cases. J. Cataract. Refract. Surg. 2012, 38, 92–96. [Google Scholar] [CrossRef] [PubMed]
- Ta, C.N.; Singh, K.; Egbert, P.R.; de Kaspar, H.M. Prospective comparative evaluation of povidone–iodine (10% for 5 minutes versus 5% for 1 minute) as prophylaxis for ophthalmic surgery. J. Cataract. Refract. Surg. 2008, 34, 171–172. [Google Scholar] [CrossRef]
- Centers for Disease Control (CDC). Contaminated Povidone-Iodine Solution—Texas. Arch. Dermatol. 1989, 125, 607. [Google Scholar] [CrossRef]
- Costerton, J.W.; Stewart, P.S. Battling Biofilms. Sci. Am. 2001, 285, 74–81. [Google Scholar] [CrossRef]
- Tran, P.; Kopel, J.; Luth, K.; Dong, H.; Dev, A.; Mehta, D.; Mitchell, K.; Moeller, K.W.; Moeller, C.D.; Reid, T. The in vitro efficacy of betadine antiseptic solution and colloidal silver gel combination in inhibiting the growth of bacterial biofilms. Am. J. Infect. Control 2022. [Google Scholar] [CrossRef]
- Malone, C.L.; Boles, B.R.; Lauderdale, K.J.; Thoendel, M.; Kavanaugh, J.S.; Horswill, A.R. Fluorescent reporters for Staphylococcus aureus. J. Microbiol. Methods 2009, 77, 251–260. [Google Scholar] [CrossRef] [Green Version]
- Holloway, B.W.; Krishnapillai, V.; Morgan, A.F. Chromosomal genetics of Pseudomonas. Microbiol. Rev. 1979, 43, 73–102. [Google Scholar] [CrossRef]
- Miller, K.G.; Tran, P.L.; Haley, C.L.; Kruzek, C.; Colmer-Hamood, J.A.; Myntti, M.; Hamood, A.N. Next science wound gel technology, a novel agent that inhibits biofilm development by gram-positive and gram-negative wound pathogens. Antimicrob. Agents Chemother. 2014, 58, 3060–3072. [Google Scholar] [CrossRef]
- Barreto, R.; Barrois, B.; Lambert, J.; Malhotra-Kumar, S.; Santos-Fernandes, V.; Monstrey, S. Addressing the challenges in antisepsis: Focus on povidone iodine. Int. J. Antimicrob. Agents 2020, 56, 106064. [Google Scholar] [CrossRef] [PubMed]
- Castelnuovo, S. Povidone Iodine 0.66% to Fight Pseudomonas aeruginosa in Contact Lens Wearer: A Case Report. Case Rep. Ophthalmol. 2022, 13, 398–407. [Google Scholar] [CrossRef]
- Parvin, F.; Vickery, K.; Deva, A.K.; Hu, H. Efficacy of Surgical/Wound Washes against Bacteria: Effect of Different In Vitro Models. Materials 2022, 15, 3630. [Google Scholar] [CrossRef] [PubMed]
- Oliverio, G.W.; Spinella, R.; Postorino, E.I.; Inferrera, L.; Aragona, E.; Aragona, P. Safety and Tolerability of an Eye Drop Based on 0.6% Povidone-Iodine Nanoemulsion in Dry Eye Patients. J. Ocul. Pharmacol. Ther. 2021, 37, 90–96. [Google Scholar] [CrossRef]
- Papanikolaou, T.; Islam, T.; Hashim, A. Tolerability and Safety Profile of Povidone Iodine in Pre-Operative kin and Eye Disinfection Prior to Intraocular Surgery. J. Clin. Amp. Exp. Ophthalmol. 2011, 2, 2. [Google Scholar] [CrossRef]
- Ridder, W.H.; Oquindo, C.; Dhamdhere, K.; Burke, J. Effect of Povidone Iodine 5% on the Cornea, Vision, and Subjective Comfort. Optom. Vis. Sci. 2017, 94, 732–741. [Google Scholar] [CrossRef]
- Peden, M.C.; Hammer, M.E.; Suñer, I.J. Dilute Povidone-Iodine Prophylaxis Maintains Safety While Improving Patient Comfort After Intravitreal Injections. Retina 2019, 39, 2219–2224. [Google Scholar] [CrossRef]




Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nagle, A.; Kopel, J.; Reed, J.; Jacobo, U.; Tran, P.; Mitchell, K.; Reid, T.W. An in vitro Study of Betadine’s Ability to Eliminate Live Bacteria on the Eye: Should It Be Used for Protection against Endophthalmitis? Antibiotics 2022, 11, 1549. https://doi.org/10.3390/antibiotics11111549
Nagle A, Kopel J, Reed J, Jacobo U, Tran P, Mitchell K, Reid TW. An in vitro Study of Betadine’s Ability to Eliminate Live Bacteria on the Eye: Should It Be Used for Protection against Endophthalmitis? Antibiotics. 2022; 11(11):1549. https://doi.org/10.3390/antibiotics11111549
Chicago/Turabian StyleNagle, Alyssa, Jonathan Kopel, John Reed, Unique Jacobo, Phat Tran, Kelly Mitchell, and Ted W. Reid. 2022. "An in vitro Study of Betadine’s Ability to Eliminate Live Bacteria on the Eye: Should It Be Used for Protection against Endophthalmitis?" Antibiotics 11, no. 11: 1549. https://doi.org/10.3390/antibiotics11111549
APA StyleNagle, A., Kopel, J., Reed, J., Jacobo, U., Tran, P., Mitchell, K., & Reid, T. W. (2022). An in vitro Study of Betadine’s Ability to Eliminate Live Bacteria on the Eye: Should It Be Used for Protection against Endophthalmitis? Antibiotics, 11(11), 1549. https://doi.org/10.3390/antibiotics11111549





