Staphylococcus lugdunensis Endophthalmitis: Case Series and Literature Review
Abstract
:1. Introduction
2. Methods and Materials
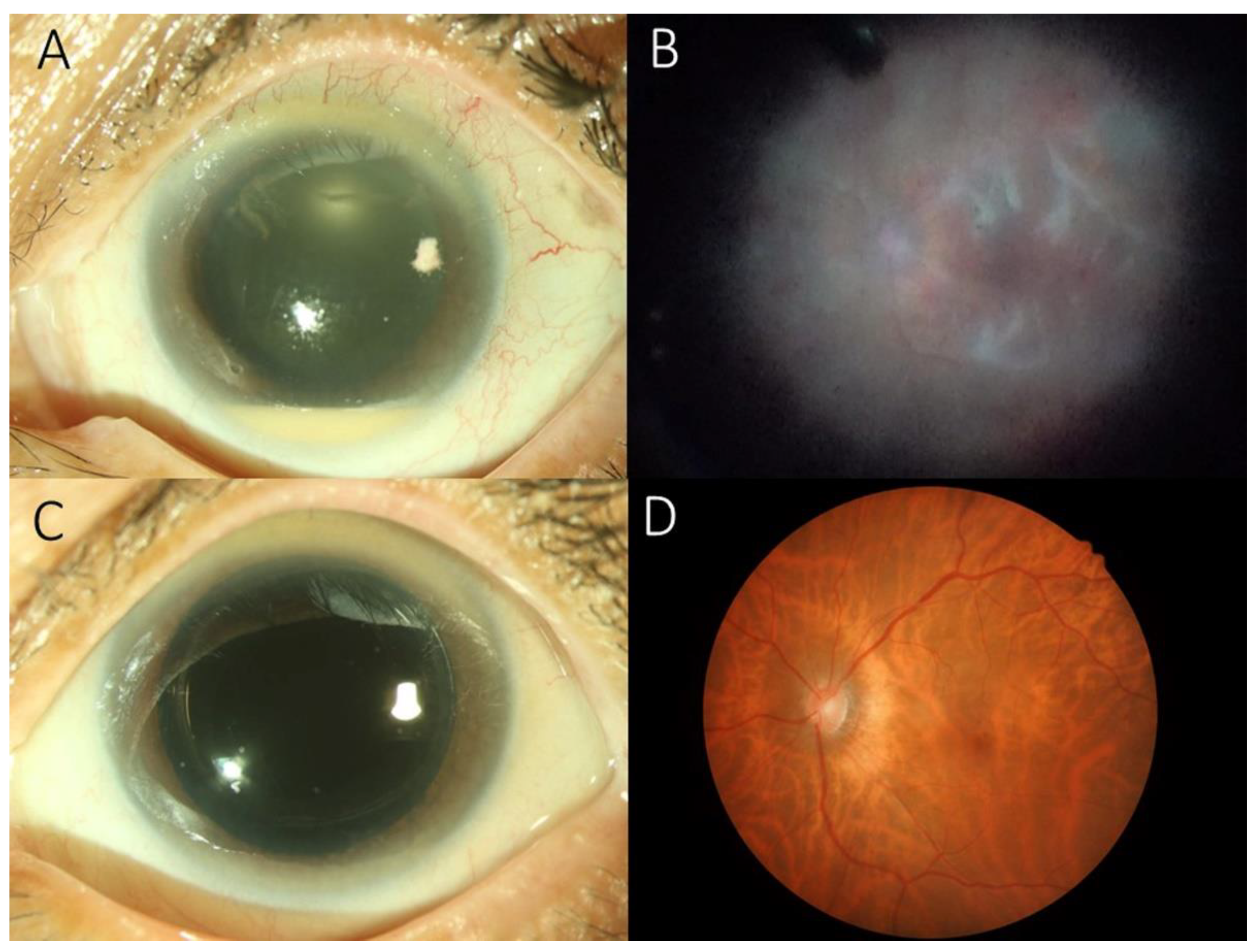
3. Results
Antibiotic Susceptibility Testing
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Clarke, B.; Williamson, T.H.; Gini, G.; Gupta, B. Management of bacterial postoperative endophthalmitis and the role of vitrectomy. Surv. Ophthalmol. 2018, 63, 677–693. [Google Scholar] [CrossRef] [PubMed]
- Singh, R.; Davoudi, S.; Ness, S. Preventive factors, diagnosis, and management of injection-related endophthalmitis: A literature review. Graefe′s Arch. Clin. Exp. Ophthalmol. 2022, 260, 2399–2416. [Google Scholar] [CrossRef] [PubMed]
- Han, D.P.; Wisniewski, S.R.; Wilson, L.A.; Barza, M.; Vine, A.K.; Doft, B.H.; Kelsey, S.F. Spectrum and susceptibilities of microbiologic isolates in the Endophthalmitis Vitrectomy Study. Am. J. Ophthalmol. 1996, 122, 1–17. [Google Scholar] [CrossRef]
- Bannerman, T.L.; Rhoden, D.L.; McAllister, S.K.; Miller, J.M.; Wilson, L.A. The source of coagulase-negative staphylococci in the Endophthalmitis Vitrectomy Study. A comparison of eyelid and intraocular isolates using pulsed-field gel electrophoresis. Arch. Ophthalmol. 1997, 115, 357–361. [Google Scholar] [CrossRef] [PubMed]
- Sampathkumar, P.; Osmon, D.R.; Cockerill, F.R., 3rd. Prosthetic joint infection due to Staphylococcus lugdunensis. Mayo Clin. Proc. 2000, 75, 511–512. [Google Scholar] [CrossRef] [Green Version]
- Frank, K.L.; Del Pozo, J.L.; Patel, R. From clinical microbiology to infection pathogenesis: How daring to be different works for Staphylococcus lugdunensis. Clin. Microbiol. Rev. 2008, 21, 111–133. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yeh, C.F.; Chang, S.C.; Cheng, C.W.; Lin, J.F.; Liu, T.P.; Lu, J.J. Clinical Features, Outcomes, and Molecular Characteristics of Community- and Health Care-Associated Staphylococcus lugdunensis Infections. J. Clin. Microbiol. 2016, 54, 2051–2057. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chiquet, C.; Pechinot, A.; Creuzot-Garcher, C.; Benito, Y.; Croize, J.; Boisset, S.; Romanet, J.P.; Lina, G.; Vandenesch, F. Acute postoperative endophthalmitis caused by Staphylococcus lugdunensis. J. Clin. Microbiol. 2007, 45, 1673–1678. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Murad-Kejbou, S.; Kashani, A.H.; Capone, A., Jr.; Ruby, A. Staphylococcus lugdunensis endophthalmitis after intravitreal injection: A case series. Retin. Cases Brief Rep. 2014, 8, 41–44. [Google Scholar] [CrossRef] [PubMed]
- Salceanu, S.O.; Hamada, D.; Ursu, R.G.; Saad, A.A. Staphylococcus lugdunensis endophthalmitis following dexamethasone intravitreal implant. Indian J. Ophthalmol. 2019, 67, 424–426. [Google Scholar] [CrossRef] [PubMed]
- Veliev, A.; Nakipoglu, Y. Investigation of Staphylococcus lugdunensis and Selected Coagulase Negative Staphylococci Isolated from Blood Culture bottles and Determination of their Sensitivities to Antibiotics. Pak. J. Med. Sci. 2022, 38, 657–662. [Google Scholar] [CrossRef] [PubMed]
- Wani, V.B.; Al-Kandari, J.; Sabti, K.; Aljassar, F.; Qali, H.; Kumar, N.; Uboweja, A.; Al-Sabah, K.; Diab, F.A.; Al-Rashidi, S. Incidence of Endophthalmitis after Intravitreal Bevacizumab using Aliquots Prepared On-site in 2 Operating Rooms in Kuwait. Middle East Afr. J. Ophthalmol. 2016, 23, 64–70. [Google Scholar] [CrossRef] [PubMed]
- Garoon, R.B.; Miller, D.; Flynn, H.W., Jr. Acute-onset endophthalmitis caused by Staphylococcus lugdunensis. Am. J. Ophthalmol. Case Rep. 2018, 9, 28–30. [Google Scholar] [CrossRef] [PubMed]
- Xu, S.; Zhang, H. Bacteriological profile of conjunctiva bacterial Flora in Northeast China: A hospital-based study. BMC Ophthalmol. 2022, 22, 223. [Google Scholar] [CrossRef] [PubMed]
- Bieber, L.; Kahlmeter, G. Staphylococcus lugdunensis in several niches of the normal skin flora. Clin. Microbiol. Infect. 2010, 16, 385–388. [Google Scholar] [CrossRef] [Green Version]
- Heilbronner, S.; Foster, T.J. Staphylococcus lugdunensis: A Skin Commensal with Invasive Pathogenic Potential. Clin. Microbiol. Rev. 2021, 34, e00205-20. [Google Scholar] [CrossRef] [PubMed]
- Chen, K.J.; Chen, Y.P.; Wang, N.K.; Sun, M.H.; Sun, C.C.; Wu, W.C.; Lai, C.C. Retinal Vasculitis and Posterior Pole Preretinal Exudates in Exogenous Bacterial Endophthalmitis: Management and Visual Outcomes. Ocul. Immunol. Inflamm. 2022, 30, 491–496. [Google Scholar] [CrossRef] [PubMed]
- Relhan, N.; Albini, T.A.; Pathengay, A.; Kuriyan, A.E.; Miller, D.; Flynn, H.W. Endophthalmitis caused by Gram-positive organisms with reduced vancomycin susceptibility: Literature review and options for treatment. Br. J. Ophthalmol. 2016, 100, 446–452. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, K.-J.; Sun, M.-H.; Hou, C.-H.; Chen, H.-C.; Chen, Y.-P.; Wang, N.-K.; Liu, L.; Wu, W.-C.; Chou, H.-D.; Kang, E.Y.-C.; et al. Susceptibility of bacterial endophthalmitis isolates to vancomycin, ceftazidime, and amikacin. Sci. Rep. 2021, 11, 15878. [Google Scholar] [CrossRef] [PubMed]
| No. | Sex/Age /Eye | Interval (Days) | Symptom (Days) | Etiology | IOP (mmHg) | Culture Sites | Systemic Diseases | Initial VA | Treatment | Final VA | Other Eye Condition | Follow-Up (Months) | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Primary | Secondary | ||||||||||||
| 1 | F/67/OS | 7 | 2 | CE + IOL | 10 | AC, V | CHF, HT, DM, CVA | HM 10 cm | PPV + IVAB | IVAB(1M) | 20/50 | M-NPDR | 36 |
| 2 | F/75/OD | 41 | 1 | PPV + CE + IOL | 12 | AC, V | HM 30 cm | PPV + IVAB | 4/200 | MM | 16 | ||
| 3 | F/74/OD | 83 | 3 | CE + IOL | 30 | AC, V | Goiter | LP 10 cm | PPV + IVAB | IVAB(3D) | NLP | RD | 3 |
| 4 | F/68/OS | 3 | 1 | CE + IOL | 7 | V | Miller-Fisher syndrome | HM 40 cm | PPV + IVAB | 20/50 | 54 | ||
| Antibiotics | Patient | |||
|---|---|---|---|---|
| 1 | 2 | 3 | 4 | |
| Penicillin | R | R | S | R |
| Oxacillin | S | S | S | |
| Teicoplanin | S | S | S | S |
| Vancomycin | S | S | S | S |
| Tigecycline | S | S | S | S |
| SMX/TMP | S | S | S | S |
| Linezolid | S | |||
| Clindamycin | S | S | R | S |
| Erythromycin | S | S | R | S |
| No. | Author | Nation | Year (Published) | No. of Eyes | Interval (Days) | Etiology | Initial VA | VAN | Treatment | Final VA | Cause of Poor VA |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Chiquet et al. [8] | France | 2004–2005 (2007) | 5 | 7 | CE | HM | S | IVAB, PPV | 20/40 | |
| 6 | CE | LP | S | IVAB, PPV | HM | RD | |||||
| 5 | CE + IOL | LP | S | IVAB, PPV | NLP | RD | |||||
| 12 | CE + IOL | 20/100 | S | IVAB | 20/20 | ||||||
| 7 | CE + IOL | HM | S | IVAB, PPV | CF | RD | |||||
| 2 | Garoon et al. [13] | US | 1990–2017 (2018) | 6 | 10 | CE + IOL | CF | S | IVAB | 20/30 | |
| 8 | CE + IOL | HM | S | IVAB | 20/40 | ||||||
| 21 | IVI | CF | S | IVAB | 20/40 | ||||||
| 6 | CE + IOL | HM | S | IVAB, PPV | 20/40 | ||||||
| 2 | Trauma | HM | S | PPV + IVAB | 20/400 | ||||||
| 3 | Trauma | LP | S | PPV + IVAB | 20/100 | ||||||
| 3 | Salceanu et al. [10] | UK | 2019 | 1 | 4 | IVI (Ozurdex) | CF | NA | PPV + IVAB | 20/120 | |
| 4 | Wani et al. [12] | Kuwait | NA (2016) | 1 | 3 | IVI (Avastin) | 20/150 | NA | IVAB | 20/30 | |
| 5 | Veliev et al. [11] | Turkey | NA (2022) | 1 | NA | postoperative | NA | NA | NA | NA | |
| 6 | Murad-Kejbou et al. [9] | US | 2011–2012 (2014) | 3 | 2 | IVI (Lucentis) | LP | S | PPV + IVAB | HM | |
| 3 | IVI (Lucentis) | 20/200 | S | IVAB | 20/200 | ||||||
| 2 | IVI (Avastin) | 20/200 | S | IVAB, PPV | 20/100 | ||||||
| 7 | Bannerman et al. [4] | US | 1990–1996 (1997) | 4 | NA | postoperative | NA | NA | NA | NA | |
| 8 | Current study Chen et al. | Taiwan | 2010–2019 | 4 | 7 | CE + IOL | HM | S | PPV + IVAB | 20/50 | |
| 41 | PPV + CE + IOL | HM | S | PPV + IVAB | 4/200 | MM | |||||
| 83 | CE + IOL | LP | S | PPV + IVAB | NLP | RD | |||||
| 3 | CE + IOL | HM | S | PPV + IVAB | 20/50 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, K.-J.; Sun, M.-H.; Tsai, A.S.H.; Sun, C.-C.; Wu, W.-C.; Lai, C.-C. Staphylococcus lugdunensis Endophthalmitis: Case Series and Literature Review. Antibiotics 2022, 11, 1485. https://doi.org/10.3390/antibiotics11111485
Chen K-J, Sun M-H, Tsai ASH, Sun C-C, Wu W-C, Lai C-C. Staphylococcus lugdunensis Endophthalmitis: Case Series and Literature Review. Antibiotics. 2022; 11(11):1485. https://doi.org/10.3390/antibiotics11111485
Chicago/Turabian StyleChen, Kuan-Jen, Ming-Hui Sun, Andrew S. H. Tsai, Chi-Chin Sun, Wei-Chi Wu, and Chi-Chun Lai. 2022. "Staphylococcus lugdunensis Endophthalmitis: Case Series and Literature Review" Antibiotics 11, no. 11: 1485. https://doi.org/10.3390/antibiotics11111485
APA StyleChen, K.-J., Sun, M.-H., Tsai, A. S. H., Sun, C.-C., Wu, W.-C., & Lai, C.-C. (2022). Staphylococcus lugdunensis Endophthalmitis: Case Series and Literature Review. Antibiotics, 11(11), 1485. https://doi.org/10.3390/antibiotics11111485







