Abstract
Antimicrobial resistance (AMR) fundamentally weakens societal foundations economically and in health care. The development of well-considered policies against AMR is important. However, in many places, AMR policy implementation remains elusive. This study aims to identify enablers and deterrents as well as processes and conditions in AMR policy advocacy. It also aims to identify AMR implementation conditions where AMR national policies are adopted and, to a certain extent, formulated and implemented. This study adopts qualitative research methodology and applies the Grounded Theory Framework to identify thematic findings from interviews conducted in China, Japan, Norway, the United Kingdom (UK), and the United States of America (US). It was identified that AMR policy protagonists are critical to filtering AMR issues and identifying policies “fit to prioritize” and “fit to implement”. They have helped move policy prioritization needles in the UK and the US and engaged in diplomatic efforts in the UK. In these cases, no clientelism was considered. In the US, protagonists who talked to the right decision-makers in the right office at the right time both moved AMR issues from individuals to institutional agenda and from social norms to policy agenda. To conclude, there are three thematic policy conditions that are significant to AMR policy advocacy and implementation: committed personal championship, institutionalization of policies, and social norms facilitate AMR policy advocacy and implementation.
1. Introduction
COVID-19 has compellingly made the case that certain threats of infectious diseases can not only harm individuals directly but undermine the functioning of countries. Similar to severe pandemics, antimicrobial resistance (AMR) has the potential to fundamentally weaken societal foundations [1,2]. Due to AMR, infections that once were reliably treatable are becoming more complicated or lethal. The pattern is global and is threatening the ability of countries to deliver modern health care and food security [3,4]. The development of well-considered policies against AMR is necessary to focus and guide resources, attention, and support. In 2015, WHO adopted a Global Action Plan on antimicrobial resistance [5,6]. More than 120 countries have elaborated a national action plan. However, in many locations, the implementation of AMR policies remains elusive [7,8,9].
In past years, countries have strived to formulate AMR policies based on evidence, data, and scientific consensus on AMR transmission pathways, contributing practices, and conditions [10,11,12]. However, the advocacy also heavily relies on the economic, political, and social relationships among health care systems, food production, trade, and domestic productivity costs [13,14]. By the same token, solutions to reduce AMR often require deeper investigations into infrastructure and governance problems with equitable access to universal health care, essential medicines, the use of antibiotic-free commodities, reduced antimicrobial prescriptions, and consumption [15,16]. For some policy administrations, AMR policy development has magnified the merit and weakness of governance, infrastructure, and policy instruments both nationally and sub-nationally [17,18]. What conditions and factors do protagonists and decision-makers consider that facilitate AMR policy advocacy?
To address the question, we conducted a qualitative study to identify some of the enablers and deterrents and the processes and conditions. These variables affect AMR policy agenda-setting and advocacy among selected countries where AMR national policies are adopted and, to a certain extent, administrated. The narrative is identified so other countries might use some of the lessons and advance their own policies. Informants are purposefully recruited based on their roles centering on antimicrobial resistance and their policy representation in public services, public health, human health care, food–animal agriculture, pharmaceuticals, and the environmental sectors. A total of 34 open-ended, semi-structured, in-depth interviews were conducted. Interview coding and thematic development were conducted according to grounded theory [19,20,21,22].
For clarity and comprehensiveness of the study, interviews were conducted based on a 30-item checklist that was established from the AMR-Intervene and AMR-PACT policy variables (Table 1) [23,24]. Interview analysis identified three main themes that characterized common and contrasting AMR policymaking. The findings facilitated a better understanding of how policies for AMR have been developed in China, Japan, Norway, the United Kingdom (UK), and the United States of America (US). Some of the themes helped identify strategies to address the challenges and to examine pathways and conditions that enable or deter AMR policy implementation in different contexts. In summary, it was identified that AMR policy protagonists are critical to filtering AMR issues and identifying policies “fit to prioritize” and “fit to implement”. They have helped move policy prioritization needles in the UK and the US, and engaged in diplomatic efforts in the UK. In these cases, no clientelism was considered. In the US, protagonists who talked to the right decision-makers in the right office at the right time moved AMR issues from individuals to institutional agenda and from social norm to policy agenda. Comparatively, the protagonists’ effects were invisible in political agenda-setting in China and Japan. It was opined that AMR experts in China and Japan tend to look to international peers for policy prioritization and political symbolic support. In all cases, unless AMR policies were institutionalized as exemplified in Norway, interviewees opined both public and private entities need to find ways to fund programs, institutionalize policies, and build social norms to sustain AMR policy in the long run.

Table 1.
Core interview variables and sample questions categorized as micro-, meso- and macro-determinants.
2. Results
A total of 34 interviews were conducted from 2019 to 2020 (Table 2). Overall, we identified 97 codes that can be summarized as six themes (Supplementary Tables S1 and S2). We organized themes into three main areas. First, individual championship is pivotal but insufficient in AMR policymaking. Observation centers on the importance of championships and where they are sub-optimal. Second, the institutionalization of AMR policymaking is key to sustaining and implementing AMR policies. Third, free markets play an ambivalent role in AMR policymaking while social norms can be an enabler in policy implementation.

Table 2.
Summary of interviewee profiles.
Of all informants, 12 interviewees are policy advisors to national action plans or personally champion the AMR agenda at ministerial or diplomatic levels. Fifteen interviewees are policy advisors to sub-national policy implementation. Sixteen interviewees are technocrats on AMR steering committees, policy representatives in agriculture, and human health care professional bodies. Six interviewees are bureaucrats in AMR leadership roles who formulate or adopt AMR policies. A summary of grounded theory theme-based and country-based key findings is listed in Table 3.

Table 3.
Grounded Theory thematic and country-based key findings.
2.1. Individual Championship Is Pivotal but Insufficient in the AMR Policymaking Arena
Individual champions were pivotal to advocate, initiate, and implement AMR policies. These AMR policy protagonists generated awareness, used bureaucratic ties, and lobbied decision-makers to raise the profile of AMR on the agenda based on personal, professional, public health, and social responsibilities. The success of these individual champions in shaping policy depended on access to key decision-makers in Norway, the US, and the UK. Policy advocacy on AMR was most successful when coupled with institutional and bureaucratic buy-in, bottom-up social norm support, and multistakeholder partnerships. By contrast, the lack of unified social norms on seeing antimicrobials as a common good gave a weaker voice to changing or prioritizing AMR on agendas in Japan and China. Some of these personal efforts had gone as far as directly changing national policy prioritization, overcoming diplomatic gridlock, and in some cases sustaining AMR policies in the long term. In Japan and China, AMR policy protagonists agreed that AMR policymaking would benefit from international support on technical and policy capacity building. In China, AMR policy personal champions were mostly technical advisors who have tried but were not able to directly influence key political decision making at national or sub-national levels. Alternatively, the absence might simply be due to the marked separation between the political and public health spheres
All interviewees who were AMR policy protagonists found implementation of AMR policies challenging. Public health, medical, and policy experts who were able to influence policymakers indicated their frustration of failing to foresee or bridge the gap between prioritizing AMR policy at national levels and the implementation of policies at sub-national and sectoral levels. Interviewees from the UK, the US, Norway, China, and Japan recalled their actions during policy advocacy and that there was “little consideration” to see beyond the initial stage of the initiation of the policy process. Other UK policy experts emphasized anticipating conditions for policy implementation was just as important as policy initiation. The interviewees opined that the consequences of such gaps lead to failure to provide the needed infrastructure, resources, and governance for AMR policy implementation. Interview quotes are included as 2.1.1 to 2.1.4 in Supplementary Table S3.
AMR policy protagonists who were allowed to advise policy at stages of policy initiation and formulation helped converge public, professional, and policy perspectives. They introduced or recombined relevant information, especially in the case of policy initiation impasse [25]. Different societies, however, permitted protagonists to become involved in AMR policies at different stages of the policy process and with varying levels of influence. Compared to Norway, the UK, and the US where interviewees were involved in the early stages of the policy process, interviewees in China and Japan were recruited at a later stage, some for technical advice after the government agenda was set and decisions about priorities were made. Additionally, interviewees who worked to influence AMR policies in China and Japan opined there was lower accessibility to political decision making. This was opined partly due to accessibility problems to key decision-makers in a classical hierarchical governance approach. In addition, the data collected highlighted intrinsic differences among different policy situations. In the UK, the US, and Norway, interviewed policy protagonists were involved in discussion during policy prioritization and spoke directly to political decision-makers. The US interviewees also used leverage from society and the media when advocating AMR policies. Interviewees from China emphasized a more top-down approach to AMR policymaking Interview quotes are included as 2.1.5 to 2.1.9 in Supplementary Table S3.
Comparatively, there were specific policymaking considerations within China and Japan. We found two distinct patterns in policy advocacy and implementation. First, interviewees from China and Japan—though some were considered by their countries as experts—described fewer links between technocrats and those that were politically powerful to influence policies. It was even less common for these individuals to have experience or access to political nexuses or to negotiate for diplomatic support. Overall, personal championship indicated a more important role in the UK and the US than in Japan or China. It appeared that it was uncommon culturally and socially in China or Japan to confer an important advisory role to an individual outside of established political structures. Most individuals interviewed in China and Japan had tried to reach or influence AMR policy decision making. Most interviewees from these countries also described a lack of political interest and political commitment as one of the major obstacles to the implementation of AMR policies. Interviewees from China and Japan opined that international peers were an important source of leadership to advocate and implement AMR policies.
2.2. Policy Institutionalization Facilitates AMR Policy Prioritization and Implementation
Personal championship was an essential enabler in AMR policy advocacy and also for maintaining long-term policy commitment. In some cases, reduced involvement from an individual champion was associated with a loss of AMR policy continuity. In cases when personal champions played a key role in the adoption of AMR policies by bureaucracies without institutionalization, lack of institutional memory was prominent in some countries. This lack of institutional memory continued to revert AMR policies to their earlier stages. For instance, during the discussion of AMR policy implementation in China, interviewees observed that individuals who led the AMR work often engage in endogenous effort and resources to influence guidelines and stewardship programs at the implementation phase and settings. However, the implementation and policy fidelity were individual-dependent and therefore more likely to be inconsistent. In the US, a change of political leadership led to AMR policy deprioritization. This emphasized the issue of long-term commitment to addressing AMR. Interview quotes are included as 2.2.1 to 2.2.3 in Supplementary Table S3.
Interviewees suggested that prioritization and resource commitment on AMR need to transition from personal advocacy to institutionalization. Personal advocacy was much more prominent in the UK and the US than in Japan and China. Among these four countries, a commonality underpinned the ultimate implementation of policies—an individual or individuals from hospitals, farming, community pharmacies, public service systems, medical systems, and government offices stepped up endogenously, or in other cases followed through with their jobs. Interviewees opined AMR governance around organizational collaboration, orchestration, establishment, and enforcement of policies, guidelines, and regulations was built on personal investment and motivation rather than well-defined institutional processes. These findings stood in contrast with findings from Norway, which were indicated to be incorporated and institutionalized AMR policies based on their existing governance and administration capacity rather than by relying on individual champions.
The example of Norway illustrated some of the factors that were important in supporting countries’ effective capacity to address AMR. Interviewees described sustained cross-sectoral collaboration to address AMR, which was based on a mutual understanding of its significance for local and global health and could use well-established infrastructure and political instruments. In Norway, AMR control, according to experts from both the public health sector and the veterinary sector, was seen as a core part of infectious disease control, food safety, and zoonotic disease prevention. Well-established cooperation among human, animal, and food sectors at government and non-government offices also helped AMR policy development. As a result, the governance, infrastructure, and cross-sectoral relationships provided the backbone for AMR policies. By comparison, interviews in the US, the UK, Japan, and China indicated a lower level of support for collaborative governance and policy prioritization to institutionalize which usually takes time and resources.
2.3. Free Markets Play an Ambivalent Role While Social Norms Are a Driver in AMR Policymaking
Protagonists opined that economic and financial incentivization to increase antimicrobial innovation and reduce antimicrobial use was still very much in the hands of private industries. For antibiotic innovations, there were non-profit mechanisms such as Combating Antibiotic Resistant Bacteria Biopharmaceutical Accelerator (CARB-X) and Global Antibiotic Research & Development Partnership (GARDP) which brought new antibiotics to market [26]. However, interviewees in the UK and China who worked closely with pharmaceutical development and medical insurance policies emphasized the need for a “business case” to sustain AMR innovation policies. Interviewees also opined that there were not sufficient public–private partnerships, especially in the face of hurdles in drug legislation, cost of drug development, and low potential for financial profit. For reducing antimicrobial use, the US interviewees stated contemporary public and private medical insurance reimbursement mechanisms that encouraged patients to use medical facilities and services with infectious disease prevention and control programs had also facilitated antimicrobial use stewardship programs. Additionally, in China, financial disincentives changed antimicrobial prescription and consumption behavior in hospitals [27].
Without social norms, interviewees opined that financial direction among antimicrobial users ultimately overrode the protagonists’ influences—be that antimicrobial stewardship, antimicrobial production quality control, or pharmaceutical innovation. Interviewees emphasized that local social norms such as patient antibiotics use compliance, food-producing animal farming industrial practices, and consumers’ willingness to pay for antibiotics-free food influenced antimicrobial use. For instance, interviews from Norway confirmed strong social values and norms to protect public health as a key determinant behind AMR policy advocacy. Additionally, the younger generation was perceived to be the next social norm to facilitate prudent antimicrobial use in China. On the contrary, an interview in Japan provided insight that perceived hurt to national economics has driven social norm and policymakers to side with softer or different policies. Interview quotes are included as 2.3.1 to 2.3.7 in Supplementary Table S3.
2.4. Summary of AMR Policy Advocacy and Implementation Variables
Variables that influence policy protagonists and AMR policy advocacy and implementation can be categorized as three levels of micro-, meso-, and macro-determinants (Figure 1). Personal championship represented by personal belief, professional obligation in medicine and public health are represented as micro-determinants. The political, social, cultural, and economic variables influencing policy protagonists and their actions in advocacy and implementation are represented as macro-determinants. The organizational dynamics and conditions such as an organization’s memory of policies, institutional management coherence, governance, and infrastructure capacity are represented as meso-determinants. These three determinants and their relationships either enabled or inhibited policy protagonists in exercising their advocacy roles and capacities, institutionalization of policies for policy sustainability, and policy climate for advocacy or implementation of AMR policies.
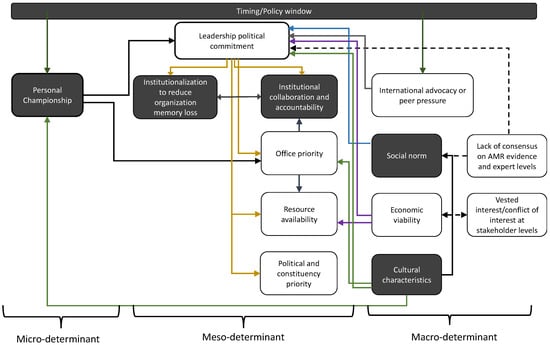
Figure 1.
AMR policy protagonists consider multiple variables in their policy advocacy and implementation process. The main themes identified are indicated in black boxes. Solid arrows depict how variables are opined to have facilitated advocacy and/implementation. Dashed arrows depict deterrents in policy development. Yellow arrows depict political, green depict cultural, purple depict economic, and blue depict social characteristics. Micro-, meso-, and macro-determinants are bracketed.
3. Discussion
We identified commonalities and variations in policymaking that are pertinent to the design and implementation of effective and sustainable AMR policies. First, AMR policy requires resources and planning, especially for implementation, which has proved to be a challenge in many countries. Though initiation and advocacy of policies were described, most countries either did not factor in or found out that they underestimated the amount of resources needed to successfully implement the policies in their action plans. Second, personal championship works well to advocate AMR policies in the respective cultures and societies of the US and the UK. However, individual champions from China and Japan do not appear to have equal success in advocating for policy change. Rather, Japan and China’s AMR policy advocacy benefits from strong international leadership and symbolic policy advocacy. Third, AMR policymaking is challenging in a public health network and social norm which are not ready to pull together politically and economically sustainable AMR efforts. Rather than relying solely on the private market for antibiotics innovation or stewardship, public–private partnerships and social norms are needed to overcome economic systems that are less developed in considering AMR as a public health entity.
Policies for AMR are still at an early level of development in some countries for several reasons—in countries where individual championship is viewed with skepticism, policy development and implementation have often stalled and are not yet incorporated into bureaucratic structures and processes. For policy advocacy that relies on international and national peer influences, policies drafted and programmed were not given sufficient in situ consideration to tailor to sub-national and sector contexts. For policies that landed without infrastructure and governance, AMR advocacy was perceived to be a waste of political credit or time.
Our article had several limitations. The first was the difficulty to recruit policy protagonists and decision-makers, especially in China and Japan. The narrative from decision makers in AMR policy development remained limited in these two countries. The second limitation was to recruit sufficient representation in face of the separation of technical protagonists and political decision-makers. The third limitation was interview variation that could occur with different interviewers’ office positions in different countries. Despite these limitations, three key points can be considered in some countries around AMR policy advocacy. First, public health offices should involve leaders in the field to ensure existing policies are being effectively implemented. Policymakers should engage these technical and policy protagonists to answer AMR policy questions because protagonists can help share the burden of policy decisions, fine-tune policy drafting, and help campaign for AMR policy implementation. Second, public offices can focus on policymaking at governance and infrastructure building, transitioning protagonists’ recommendations to sub-national levels, and focusing on institutionalizing AMR policymaking. Third, social norms are an important variable for policy advocacy and resource commitment in policy implementation.
4. Methods and Material
4.1. Sampling Technique, Enrolment, and Interview Methodology
Countries were included for their diverse contexts, different policy advocacy processes, and policy processes around AMR national policies. Interviewers were key collaborators (technical working group, TWG) who were invited to participate in this study because of their experiences and work in antimicrobial resistance policies. Training and interview guidance was provided to all interviewers. Interviews were piloted in Norway and China. Interviews were conducted in China (Mainland, Macau, and Hong Kong) (September 2018 to November 2019), Norway (March to May, 2019), Japan (June to August, 2019), the United Kingdom (September, 2019), and the United States (October, 2019 to February, 2020).
Interviewees were individuals with track records of influencing AMR policies in China, Japan, Norway, the UK, and the US. Interviewees were primarily selected by knowledge of individuals’ expertise and their influences on AMR policies (Table 2). Further recruitment of interviewees was carried out through interviewees’ recommendations on local policy protagonists.
For interview planning and clarity, the core questions list and policy variables were developed from the AMR-IMPACT and AMR-Intervene frameworks (Table 1). Face-to-face, semi-structured, open-ended interviews were conducted. All in-person interviews were audio-recorded and online interviews were audio- and video-recorded. For interviews conducted in a language other than English, transcripts were translated to English by OC, LP, and the TWG and validated by reverse translation and local collaborators. Interviews were continued until the themes of the interview content were saturated and when the content of interviews covered the different sectors that are relevant to AMR including food/animal production, food production, and human medical sectors in each country.
4.2. Data Analysis
All audio files were transcribed verbatim to Word documents. Familiarization with data was conducted by researchers listening to audio recordings (O.S.K.C. and P.L.) and reading interview transcripts (O.S.K.C. and P.L.). Transcribed interviews were imported into qualitative analysis software ATLAS-ti 8.4.25 (ATLAS ti Scientific Software Development GmbH. version 8) for analysis and codebook development. All identities of informants were delinked from the transcripts from the coding stage onwards.
Researchers read recursively and iteratively among data, codes, and themes for constant comparison. All codes were sets of pre-designated English letters and Roman numerals simplified from variables designated in AMR-PACT and AMR-Intervene [23,24]. All open codes were first assigned to endogenous and exogenous determinants that affected these policy protagonists [28,29,30]. Further open-, axial-, and selective coding was performed according to the Grounded Theory (GT) framework. Thematic and construct analyses were derived inductively according to selective codes [31,32,33,34,35]. The thematic reporting framework followed the Consolidated Criteria for Reporting Qualitative Research (COREQ) [36].
5. Conclusions
Though individual championships, or “principal coalition actors” according to the Advocacy Coalition Framework [37,38], are pivotal to establishing AMR policies, they alone are insufficient to sustain policy implementation. Additional policy processes, political will, and economic resources are needed to institutionalize AMR policymaking so that stakeholders and agencies can sustain and implement AMR policies. It is also observed that free markets play an ambivalent role in AMR policymaking while social norms are important to enable AMR policy implementation. Ethnographically, the protagonists’ effects were felt to be invisible in political agenda-setting in China and Japan. To that, informants opined that AMR experts in China and Japan tend to look to international peers for policy prioritization and political symbolic support. In all cases, unless AMR policies were institutionalized as exemplified in Norway, interviewees opined that both public and private entities need to find ways to fund programs, institutionalize policies, and build social norms to sustain AMR policy in the long run.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/antibiotics11101434/s1, Table S1: Coding categorized as micro-determinants of AMR policymaking; Table S2: Coding categorized as macro-determinants of AMR policymaking; Table S3. Interview themes, sub-themes, quote identifier, and quotes.
Author Contributions
Conceptualization, O.S.K.C. and K.F.; methodology, K.F., W.W.T.L., O.S.K.C. and D.W.; software, O.S.K.C. and P.L.; validation, K.F., J.L, N.O., X.D.Z. and Y.X.; formal analysis, O.S.K.C., K.F. and P.L.; investigation, K.F., O.S.K.C., J.L., N.O., X.D.Z. and P.L.; resources, K.F. and H.M.T.; data curation, O.S.K.C., K.F. and P.L.; writing—original draft preparation, O.S.K.C. and K.F.; writing—review and editing, K.F., W.W.T.L., D.W., N.O., J.L., X.D.Z., H.M.T., P.L. and Y.X.; visualization, O.S.K.C. and K.F.; supervision, W.W.T.L., H.M.T. and K.F.; project administration, P.L.; funding acquisition, K.F. All authors have read and agreed to the published version of the manuscript.
Funding
The study was supported by the Research Impact Fund, University Grants Committee (project no. R7033-18F) and Strategic Public Policy Research Fund, Policy Innovation and Co-ordination Office (project no. S2017.A8.005.17S) of the Government of Hong Kong Special Administrative Region, National Natural Science Foundation of China (NSFC)-Research Grant Council (RGC) Joint Research Scheme (project no. N_HKU740/19), and Wellcome Trust Grant Funding (project no. 219622/Z/19/Z).
Institutional Review Board Statement
The study obtained Ethics Approval by the Institutional Review Board of The University of Hong Kong/Hospital Authority Hong Kong West Cluster Reference Number UW18-206 approved on 5 March 2018.
Acknowledgments
We wish to thank all informants and interviewees for their generosity with their time and for sharing their experiences.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Paul, R.J.; Varghese, D. AMR in Animal Health: Issues and One Health Solutions for LMICs. In Antimicrobial Resistance; Springer: Berlin/Heidelberg, Germany, 2020; pp. 135–149. [Google Scholar]
- Tacconelli, E.; Pezzani, M.D. Public health burden of antimicrobial resistance in Europe. Lancet Infect. Dis. 2019, 19, 4–6. [Google Scholar] [CrossRef]
- George, A. Antimicrobial resistance, trade, food safety and security. One Health 2018, 5, 6. [Google Scholar] [CrossRef] [PubMed]
- Florez-Cuadrado, D.; Moreno, M.A.; Ugarte-Ruíz, M.; Domínguez, L. Antimicrobial resistance in the food chain in the European Union. Adv. Food Nutr. Res. 2018, 86, 115–136. [Google Scholar] [PubMed]
- Team, E.E. WHO member states adopt global action plan on antimicrobial resistance. Eurosurveillance 2015, 20, 21137. [Google Scholar]
- Mendelson, M.; Matsoso, M.P. The World Health Organization global action plan for antimicrobial resistance. SAMJ S. Afr. Med. J. 2015, 105, 325. [Google Scholar] [CrossRef]
- Hayes, L.; Smith, R.; Duggan, J.; Georgescu, C.; Cole, K. Implementation of an Antimicrobial Restriction Policy: Is the “Paper” More Persuasive? Open Forum Infect. Dis. 2017, 4, S261. [Google Scholar] [CrossRef][Green Version]
- Sommanustweechai, A.; Tangcharoensathien, V.; Malathum, K.; Sumpradit, N.; Kiatying-Angsulee, N.; Janejai, N.; Jaroenpoj, S. Implementing national strategies on antimicrobial resistance in Thailand: Potential challenges and solutions. Public Health 2018, 157, 142–146. [Google Scholar] [CrossRef]
- Ahmed, S.M.; Naher, N.; Tune, S.N.B.K.; Islam, B.Z. The Implementation of National Action Plan (NAP) on Antimicrobial Resistance (AMR) in Bangladesh: Challenges and Lessons Learned from a Cross-Sectional Qualitative Study. Antibiotics 2022, 11, 690. [Google Scholar] [CrossRef]
- Kaier, K.; Meyer, E.; Dettenkofer, M.; Frank, U. Epidemiology meets econometrics: Using time-series analysis to observe the impact of bed occupancy rates on the spread of multidrug-resistant bacteria. J. Hosp. Infect. 2010, 76, 108–113. [Google Scholar] [CrossRef]
- Wielinga, P.R.; Jensen, V.F.; Aarestrup, F.M.; Schlundt, J. Evidence-based policy for controlling antimicrobial resistance in the food chain in Denmark. Food Control 2014, 40, 185–192. [Google Scholar] [CrossRef]
- Shen, L.; Wei, X.; Yin, J.; Haley, D.R.; Sun, Q.; Lundborg, C.S. Interventions to optimize the use of antibiotics in China: A scoping review of evidence from humans, animals, and the environment from a One Health perspective. One Health 2022, 14, 100388. [Google Scholar] [CrossRef]
- Coast, J.; Smith, R.D.; Millar, M.R. An economic perspective on policy to reduce antimicrobial resistance. Soc. Sci. Med. 1998, 46, 29–38. [Google Scholar] [CrossRef]
- Jit, M.; Ng, D.H.L.; Luangasanatip, N.; Sandmann, F.; Atkins, K.E.; Robotham, J.V.; Pouwels, K.B. Quantifying the economic cost of antibiotic resistance and the impact of related interventions: Rapid methodological review, conceptual framework and recommendations for future studies. BMC Med. 2020, 18, 38. [Google Scholar] [CrossRef]
- Haenssgen, M.J.; Charoenboon, N.; Khine Zaw, Y. It is time to give social research a voice to tackle antimicrobial resistance? J. Antimicrob. Chemother. 2018, 73, 1112–1113. [Google Scholar] [CrossRef]
- Heyman, G.; Cars, O.; Bejarano, M.-T.; Peterson, S. Access, excess, and ethics—Towards a sustainable distribution model for antibiotics. Upsala J. Med. Sci. 2014, 119, 134–141. [Google Scholar] [CrossRef]
- Chandler, C.I. Current accounts of antimicrobial resistance: Stabilisation, individualisation and antibiotics as infrastructure. Palgrave Commun. 2019, 5, 53. [Google Scholar] [CrossRef]
- Charoenboon, N.; Haenssgen, M.J.; Warapikuptanun, P.; Xayavong, T.; Zaw, Y.K. Translating antimicrobial resistance: A case study of context and consequences of antibiotic-related communication in three northern Thai villages. Palgrave Commun. 2019, 5, 23. [Google Scholar] [CrossRef]
- Thornberg, R.; Charmaz, K. Grounded theory and theoretical coding. In The SAGE Handbook of Qualitative Data Analysis; Sage: New York, NY, USA, 2014; Volume 5, pp. 153–169. [Google Scholar]
- Foley, G.; Timonen, V. Using grounded theory method to capture and analyze health care experiences. Health Serv. Res. 2015, 50, 1195–1210. [Google Scholar] [CrossRef]
- Belgrave, L.; Seide, K. Coding for grounded theory. In The SAGE Handbook of Current Developments in Grounded Theory; Sage: London, UK, 2019; pp. 167–185. [Google Scholar]
- Bryant, A.; Charmaz, K. The SAGE Handbook of Current Developments in Grounded Theory; SAGE Publications: London, UK, 2019. [Google Scholar]
- Ogyu, A.; Chan, O.; Littmann, J.; Pang, H.H.; Lining, X.; Liu, P.; Matsunaga, N.; Ohmagari, N.; Fukuda, K.; Wernli, D. National action to combat AMR: A One-Health approach to assess policy priorities in action plans. BMJ Glob. Health 2020, 5, e002427. [Google Scholar] [CrossRef]
- Léger, A.; Lambraki, I.; Graells, T.; Cousins, M.; Henriksson, P.J.; Harbarth, S.; Carson, C.; Majowicz, S.; Troell, M.; Parmley, E.J. AMR-Intervene: A social–ecological framework to capture the diversity of actions to tackle antimicrobial resistance from a One Health perspective. J. Antimicrob. Chemother. 2021, 76, 1–21. [Google Scholar] [CrossRef]
- Arnold, G. Does entrepreneurship work? Understanding what policy entrepreneurs do and whether it matters. Policy Stud. J. 2021, 49, 968–991. [Google Scholar] [CrossRef]
- Blaskovich, M.A. Antibiotics Special Issue: Challenges and Opportunities in Antibiotic Discovery and Development. ACS Infect. Dis. 2020, 6, 1286–1288. [Google Scholar] [CrossRef]
- Chan, O.S.K.; Wernli, D.; Liu, P.; Tun, H.M.; Fukuda, K.; Lam, W.; Xiao, Y.H.; Zhou, X.; Grépin, K.A. Unpacking Multi-Level Governance of Antimicrobial Resistance Policies: The Case of Guangdong, China. Health Policy Plan. 2022, 37, 1148–1157. [Google Scholar] [CrossRef]
- Schmid, N.; Sewerin, S.; Schmidt, T.S. Explaining Advocacy Coalition Change with Policy Feedback. Policy Stud. J. 2020, 48, 1109–1134. [Google Scholar] [CrossRef]
- Ancillotti, M.; Eriksson, S.; Veldwijk, J.; Fahlquist, J.N.; Andersson, D.I.; Godskesen, T. Public awareness and individual responsibility needed for judicious use of antibiotics: A qualitative study of public beliefs and perceptions. BMC Public Health 2018, 18, 1153. [Google Scholar] [CrossRef]
- Weible, C.M.; Sabatier, P.A. Theories of the Policy Process, 4th ed.; Routledge: London, UK, 2018; Volume 1. [Google Scholar]
- Axelrod, R. Structure of Decision: The Cognitive Maps of Political Elites; Princeton University Press: Princeton, NJ, USA, 2015. [Google Scholar]
- Pope, C.; Ziebland, S.; Mays, N. Analysing qualitative data. BMJ 2000, 320, 114–116. [Google Scholar] [CrossRef]
- Bradley, E.H.; Curry, L.A.; Devers, K.J. Qualitative data analysis for health services research: Developing taxonomy, themes, and theory. Health Serv. Res. 2007, 42, 1758–1772. [Google Scholar] [CrossRef]
- Gilson, L. Qualitative research synthesis for health policy analysis: What does it entail and what does it offer? Health Policy Plan. 2014, 29, iii1–iii5. [Google Scholar] [CrossRef]
- Barnett-Page, E.; Thomas, J. Methods for the synthesis of qualitative research: A critical review. BMC Med. Res. Methodol. 2009, 9, 59. [Google Scholar] [CrossRef]
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int. J. Qual. Health Care 2007, 19, 349–357. [Google Scholar] [CrossRef]
- Jenkins-Smith, H.C.; Nohrstedt, D.; Weible, C.M.; Ingold, K. The advocacy coalition framework: An overview of the research program. In Theories of the Policy Process; Routledge: London, UK, 2018; pp. 135–171. [Google Scholar]
- Weible, C.M.; Sabatier, P.A. A guide to the advocacy coalition framework. In Handbook of Public Policy Analysis; CRC Press: Boca Raton, FL, USA, 2006; pp. 123–136. [Google Scholar]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).