Consumption of Antibiotics in Primary Care Setting before and during COVID-19 Pandemic in Republic of Srpska, Bosnia and Herzegovina
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design and Data Collection
2.2. Outcome Assessment
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
6. Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. Director-General’s Opening Remarks at the Media Briefing on COVID-19. 2020. Available online: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19 (accessed on 11 March 2020).
- CDC. Assessing Risk Factors for Severe COVID-19 Illness. 2020. Available online: https://www.cdc.gov/coronavirus/2019-ncov/covid-data/investigations-discovery/assessing-risk-factors.html (accessed on 20 August 2022).
- Bharati, S.; Podder, P.; Mondal, M.R.H.; Podder, P.; Kose, U. A review on epidemiology, genomic characteristics, spread, and treatments of COVID-19. In Data Science for COVID-19; Academic Press: Cambridge, MA, USA, 2022; pp. 487–505. [Google Scholar]
- Centers for Disease Control and Prevention. Symptoms of Coronavirus. Available online: https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html (accessed on 21 September 2022).
- World Health Organization. Clinical Care for Severe Acute Respiratory Infection: Toolkit: COVID-19 Adaptation. 2022. Available online: https://apps.who.int/iris/handle/10665/331736 (accessed on 25 August 2022).
- Aćimović, J.; Jandrić, L.; Dević, J.Đ.; Subotić, B.; Radojčić, T.; Bojanić, J.; Vukmir, N.R.; Zeljković, B. Epidemiologic characteristics of COVID-19 infection in the Republic of Srpska: A hundred days survey. Scr. Med. 2020, 51, 74–80. [Google Scholar]
- Zhong, B.-L.; Luo, W.; Li, H.-M.; Zhang, Q.-Q.; Liu, X.-G.; Li, W.-T.; Li, Y. Knowledge, attitudes, and practices towards COVID-19 among Chinese residents during the rapid rise period of the COVID-19 outbreak: A quick online cross-sectional survey. Int. J. Biol. Sci. 2020, 16, 1745–1752. [Google Scholar] [CrossRef] [PubMed]
- Worldometer. COVID-19 Coronavirus Pandemic. 2022. Available online: https://www.worldometers.info/coronavirus/ (accessed on 7 January 2022).
- Regional Office for Europe and the European Observatory on Health Systems and Policies. Health Systems in Action: Bosnia and Herzegovina. 2022. Available online: https://eurohealthobservatory.who.int/publications/i/health-systems-in-action-bosnia-and-herzegovina-2022 (accessed on 10 September 2022).
- Dicker, B.; Swain, A.; Todd, V.F.; Tunnage, B.; McConachy, E.; Drake, H.; Brett, M.; Spearing, D.; Howie, G.J. Changes in demand for emergency ambulances during a nationwide lockdown that resulted in elimination of COVID-19: An observational study from New Zealand. BMJ Open 2020, 10, e044726. [Google Scholar] [CrossRef] [PubMed]
- Andrew, E.; Nehme, Z.; Stephenson, M.; Walker, T.; Smith, K. The impact of the COVID-19 pandemic on demand for emergency ambulances in Victoria, Australia. Prehospital Emerg. Care 2022, 26, 23–29. [Google Scholar] [CrossRef] [PubMed]
- Högberg, L.D.; Vlahović-Palčevski, V.; Pereira, C.; Weist, K.; Monnet, D.L. ESAC-Net study group Decrease in community antibiotic consumption during the COVID-19 pandemic, EU/EEA, 2020. Eurosurveillance 2021, 26, 2101020. [Google Scholar] [CrossRef] [PubMed]
- Llor, C.; Ouchi, D.; Giner-Soriano, M.; García-Sangenís, A.; Bjerrum, L.; Morros, R. Correlation between Previous Antibiotic Exposure and COVID-19 Severity. A Population-Based Cohort Study. Antibiotics 2021, 10, 1364. [Google Scholar] [CrossRef]
- Chedid, M.; Waked, R.; Haddad, E.; Chetata, N.; Saliba, G.; Choucair, J. Antibiotics in treatment of COVID-19 complications: A review of frequency, indications, and efficacy. J. Infect. Public Health 2021, 14, 570–576. [Google Scholar] [CrossRef]
- Grau, S.; Echeverria-Esnal, D.; Gómez-Zorrilla, S.; Navarrete-Rouco, M.E.; Masclans, J.R.; Espona, M.; Gracia-Arnillas, M.P.; Duran, X.; Comas, M.; Horcajada, J.P.; et al. Evolution of Antimicrobial Consumption During the First Wave of COVID-19 Pandemic. Antibiotics 2021, 10, 132. [Google Scholar] [CrossRef]
- Russell, C.D.; Fairfield, C.J.; Drake, T.M.; Turtle, L.; Seaton, R.A.; Wootton, D.G.; Sigfrid, L.; Harrison, E.M.; Docherty, A.B.; de Silva, T.I.; et al. Co-infections, secondary infections, and antimicrobial use in patients hospitalised with COVID-19 during the first pandemic wave from the ISARIC WHO CCP-UK study: A multicentre, prospective cohort study. Lancet Microbe 2021, 2, e354–e365. [Google Scholar] [CrossRef]
- World Health Organisation. WHO Releases the 2019 AWaRe Classification Antibiotics. 2019. Available online: https://www.who.int/news/item/01-10-2019-who-releases-the-2019-aware-classification-antibiotics (accessed on 10 September 2022).
- Bojanić, L.; Marković-Peković, V.; Skrbić, R.; Stojaković, N.; Ðermanović, M.; Bojanić, J.; Fürst, J.; Kurdi, A.B.; Godman, B. Recent Initiatives in the Republic of Srpska to Enhance Appropriate Use of Antibiotics in Ambulatory Care; Their Influence and Implications. Front. Pharmacol. 2018, 9, 442. [Google Scholar] [CrossRef]
- Public Health Institute of the Republic of Srpska. Available online: https://www.phi.rs.ba/index.php?lang=EN (accessed on 20 August 2022).
- WHO Expert Committee. The selection and use of essential medicines. World Health Organ. Tech. Rep. Ser. 2009, 958, 1–242. [Google Scholar]
- Republic of Srpska—Institute of Statistics.Cities an Municipalities of Republika Srpska 2021. 2021. Available online: https://www.rzs.rs.ba/static/uploads/bilteni/gradovi_i_opstine_republike_srpske/2021/Gradovi_I_Opstine_Republike_Srpske_2021_WEB_II.pdf (accessed on 27 August 2022).
- Republic of Srpska—Institute of Statistics. Cities an Municipalities of Republika Srpska 2021. 2020. Available online: https://www.rzs.rs.ba/static/uploads/bilteni/gradovi_i_opstine_republike_srpske/2020/Gradovi_I_Opstine_Republike_Srpske_2020_WEB.pdf (accessed on 22 August 2022).
- ESAC-Net. European Centre for Disease Prevention and Control. Antimicrobial Consumption Database (ESAC-Net). 2022. Available online: https://www.ecdc.europa.eu/en/antimicrobial-consumption/surveillance-and-disease-data/database (accessed on 9 September 2022).
- Del Fiol, F.S.; Bergamaschi, C.C.; De Andrade, I.P., Jr.; Lopes, L.C.; Silva, M.T.; Barberato-Filho, S. Consumption Trends of Antibiotics in Brazil during the COVID-19 Pandemic. Front. Pharmacol. 2022, 13, 844818. [Google Scholar] [CrossRef] [PubMed]
- Bogdanić, N.; Močibob, L.; Vidović, T.; Soldo, A.; Begovać, J. Azithromycin consumption during the COVID-19 pandemic in Croatia, 2020. PLoS ONE 2022, 17, e0263437. [Google Scholar]
- Sultana, J.; Cutroneo, P.M.; Crisafulli, S.; Puglisi, G.; Caramori, G.; Trifirò, G. Azithromycin in COVID-19 Patients: Pharmacological Mechanism, Clinical Evidence and Prescribing Guidelines. Drug Saf. 2020, 43, 691–698. [Google Scholar] [CrossRef] [PubMed]
- Gautret, P.; Lagier, J.C.; Parola, P.; Hoang, V.T.; Meddeb, L.; Mailhe, M.; Doudier, B.; Courjon, J.; Giordanengo, V.; Vieira, V.E.; et al. Hydroxychloroquine and azithromycin as a treatment of COVID-19: Results of an open-label non-randomized clinical trial. Int. J. Antimicrob. Agents 2020, 56, 105949. [Google Scholar] [CrossRef]
- Siemieniuk, R.A.; Bartoszko, J.J.; Ge, L.; Zeraatkar, D.; Izcovich, A.; Kum, E.; Pardo-Hernandez, H.; Qasim, A.; Martinez, J.P.D.; Rochwerg, B.; et al. Drug treatments for COVID-19: Living systematic review and network meta-analysis. BMJ 2020, 370, m2980. [Google Scholar] [CrossRef]
- Roche, N.; Crichton, M.L.; Goeminne, P.C.; Cao, B.; Humbert, M.; Shteinberg, M.; Antoniou, K.M.; Ulrik, C.S.; Parks, H.; Wang, C.; et al. Update June 2022: Management of hospitalised adults with coronavirus disease 2019 (COVID-19): A European Respiratory Society living guideline. Eur. Respir. J. 2022, 60, 2200803. [Google Scholar] [CrossRef]
- Mijović, B.; Mašić, S.; Petković, M.; Knežević, D.; Aćimović, J.; Djaković-Dević, J.; Puhalo-Sladoje, D.; Zeljković, B.; Spaić, D.; Bokonjić, D.; et al. Seroprevalence of SARS-CoV-2 antibodies and knowledge, attitude and practice toward COVID-19 in the Republic of Srpska-Bosnia & Herzegovina: A population-based study. PLoS ONE 2022, 17, e0262738. [Google Scholar]
- Auta, A.; Hadi, M.A.; Oga, E.; Adewuyi, E.O.; Abdu-Aguye, S.N.; Adeloye, D.; Strickland-Hodge, B.; Morgan, D.J. Global access to antibiotics without prescription in community pharmacies: A systematic review and meta-analysis. J. Infect. 2019, 78, 8–18. [Google Scholar] [CrossRef]
- Bara, W.; Brun-Buisson, C.; Coignard, B.; Watier, L. Outpatient Antibiotic Prescriptions in France: Patients and Providers Characteristics and Impact of the COVID-19 Pandemic. Antibiotics 2022, 11, 643. [Google Scholar] [CrossRef]
- Huttner, B.D.; Catho, G.; Pano-Pardo, J.R.; Pulcini, C.; Schouten, J. COVID-19: Don’t neglect antimicrobial stewardship principles! Clin. Microbiol. Infect. 2020, 26, 808–810. [Google Scholar] [CrossRef] [PubMed]
- Santoso, P.; Sung, M.; Hartantri, Y.; Andriyoko, B.; Sugianli, A.K.; Alisjahbana, B.; Tjiam, J.S.L.; Debora, J.; Kusumawati, D.; Soeroto, A.Y. MDR Pathogens Organisms as Risk Factor of Mortality in Secondary Pulmonary Bacterial Infections Among COVID-19 Patients: Observational Studies in Two Referral Hospitals in West Java, Indonesia. Int. J. Gen. Med. 2022, 15, 4741–4751. [Google Scholar] [CrossRef] [PubMed]
| Penicillins J01C | Cephalosporins J01D | Macrolides J01F | Quinolones J01M | Tetracyclines J01A | Other |
|---|---|---|---|---|---|
| Phenoxymeth * J01CE02 | cephalexin J01DB01 | Erythromycin J01FA01 | ciprofloxacin J01MA02 | doxycycline J01AA02 | TMS *** J01EE01 |
| ampicillin J01CA01 | cefuroxime J01DC02 | Roxithromycin J01FA06 | nofloxacin J01MA06 | clindamycin J01FF01 | |
| Amoxicillin J01CA04 | cefaclor J01DC04 | clarithromycin J01FA09 | levofloxacin J01MA12 | linkomycin J01FF02 | |
| amox/clav ** J01CR02 | ceftriaxone J01DD04 | Azithromycin J01FA10 | moxifloxacin J01MA14 | gentamicin J01GB03 | |
| cefixim J01DD08 | metronidazole J01XD01 | ||||
| cefpodoxim J01DD13 | Nitrofurantoin J01XE01 |
| Groups of Antibiotics | INN | ATC | DDD/TID | Ratio | p | |||
|---|---|---|---|---|---|---|---|---|
| 2019 | 2020 | |||||||
| Mean | SD | Mean | SD | |||||
| Penicillins | Phenoxymet | J01CEO2 | 0.84 | 0.33 | 0.55 | 0.22 | 0.66 | 0.211 ** |
| Amoxicillin | J01CA04 | 6.60 | 6.71 | 13.21 | 3.78 | 2.00 | <0.001 ** | |
| Ampicillin po | J01CA01 | 0.14 | 0.35 | 0.09 | 0.14 | 0.61 | 0.881 ** | |
| Ampicillin pe | 0.01 | 0.20 | 0.01 | 0.11 | 0.90 | 0.921 * | ||
| Amox/clav po | J01CR02 | 2.95 | 4.13 | 2.85 | 0.71 | 0.97 | 0.532 ** | |
| Amox/clav pe | 0.04 | 0.04 | 0.39 | 0.20 | 9.28 | 0.198 ** | ||
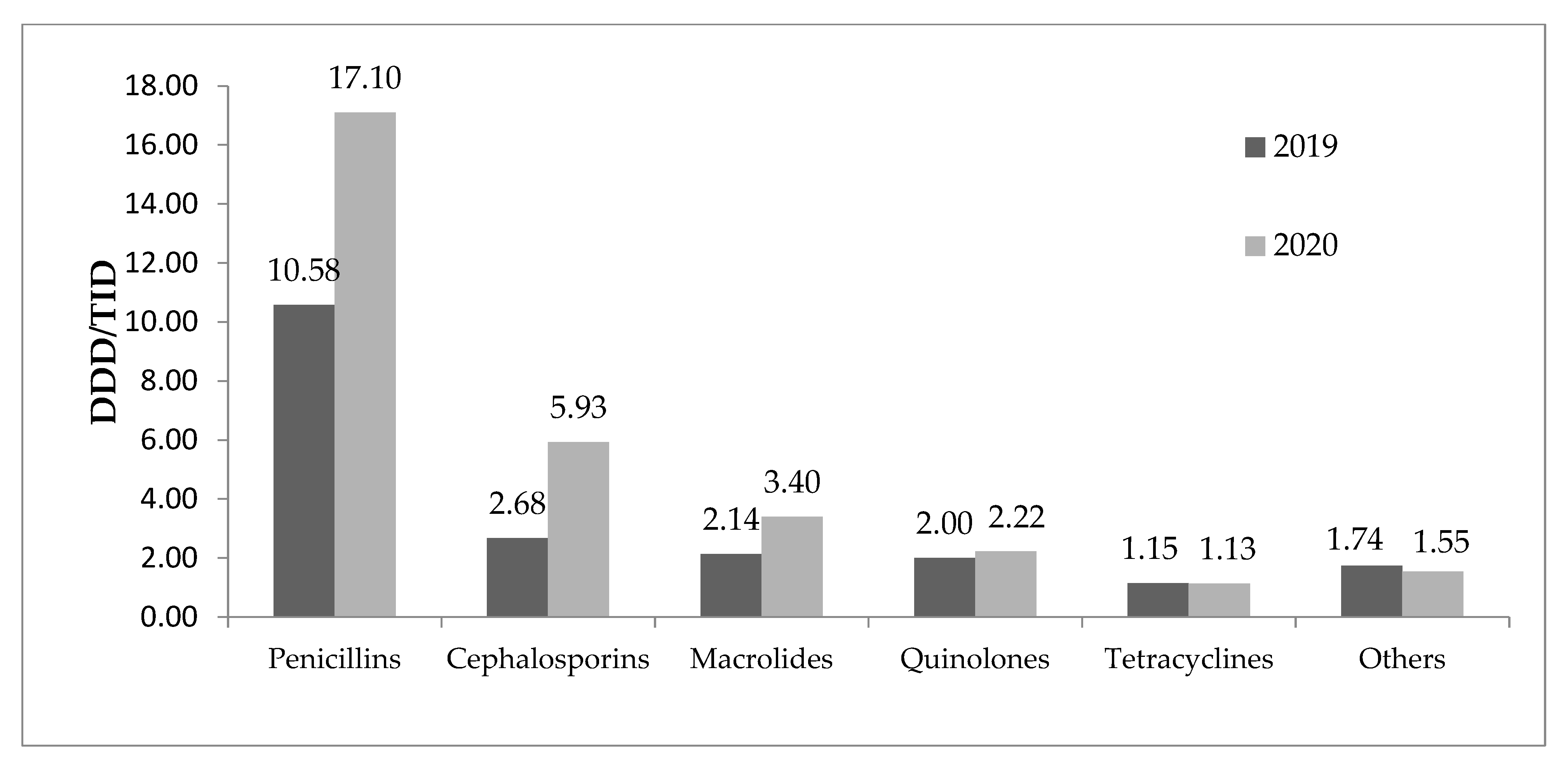
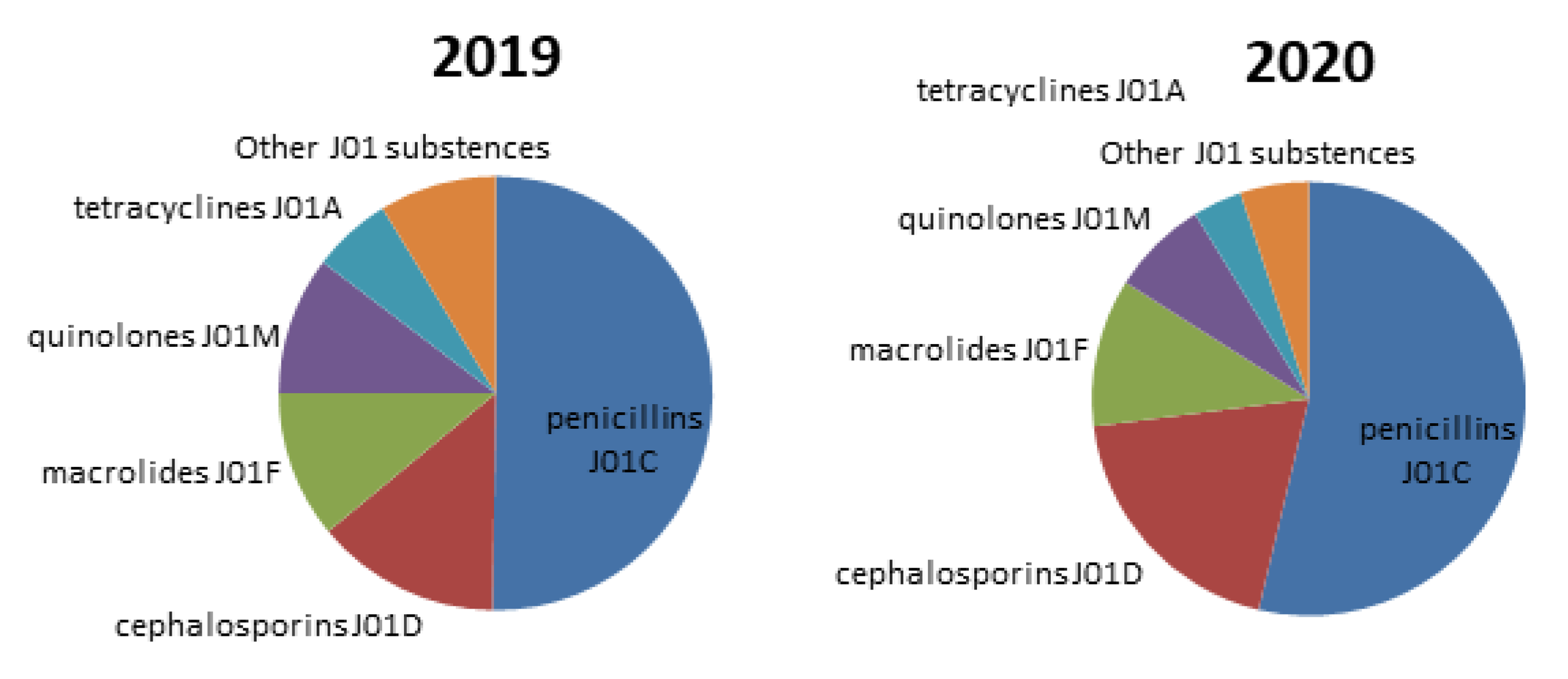
| TOTAL | 10.58 | 11.01 | 17.10 | 13.63 | 1.61 | <0.001 ** | ||
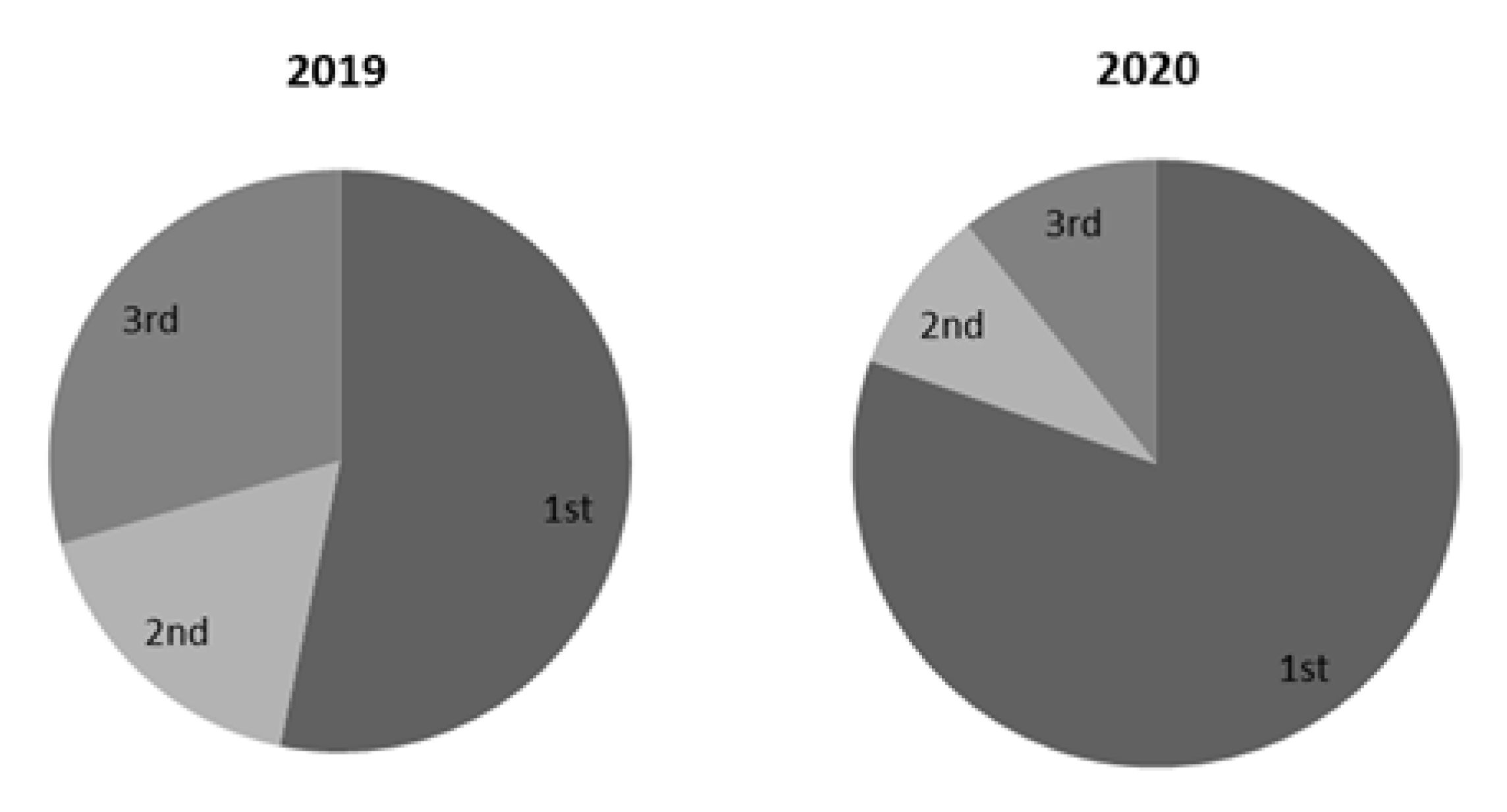
| Cephalosporins | Cefalexin | JO1DB01 | 1.60 | 1.18 | 4.77 | 2.71 | 2.98 | 0.009 * |
| SUM 1st generation | 1.60 | 1.18 | 4.77 | 2.71 | 2.98 | 0.009 * | ||
| Cefuroxim po | J01DC02 | 0.57 | 0.22 | 0.50 | 0.20 | 0.87 | 0.257 * | |
| Cefuroxim pe | 0.01 | 0.02 | 0.01 | 0.01 | 0.76 | 0.890 ** | ||
| Cefaclor | J01DC04 | 0.03 | 0.01 | 0.02 | 0.01 | 0.51 | 0.711 ** | |
| SUM 2nd generation | 0.61 | 0.25 | 0.52 | 0.21 | 0.85 | 0.562 * | ||
| Cefixim po | J01DD08 | 0.24 | 0.16 | 0.38 | 0.25 | 1.60 | 0.032 * | |
| Cefpodoxim | J01DD13 | 0.04 | 0.05 | 0.05 | 0.08 | 1.21 | 0.921 ** | |
| Ceftriaxon | J01DD04 | 0.18 | 1.10 | 0.20 | 1.45 | 1.09 | 0.111 ** | |
| SUM 3rd generation | 0.46 | 1.15 | 0.63 | 1.48 | 1.37 | 0.211 ** | ||
| TOTAL | 2.68 | 1.90 | 5.93 | 2.77 | 2.22 | <0.001 ** | ||
| Macrolides | Azythromycin po | J01FA10 | 1.27 | 1.18 | 2.73 | 2.81 | 2.15 | 0.007 ** |
| Azithromycin pe | 0.01 | 0.02 | 0.06 | 0.11 | 5.27 | 0.332 ** | ||
| Eryithromycin | J01FA01 | 0.34 | 0.40 | 0.19 | 0.13 | 0.57 | 0.042 ** | |
| Clarithromycin po | J01FA09 | 0.49 | 0.64 | 0.40 | 0.41 | 0.82 | 0.092 ** | |
| Clarithromycinepo | 0.00 | 0.01 | 0.01 | 0.01 | 4.71 | 0.821 ** | ||
| Roxithromycine | J01FA06 | 0.02 | 0.04 | 0.01 | 0.01 | 0.44 | 0.623 ** | |
| TOTAL | 2.14 | 2.22 | 3.40 | 3.44 | 1.59 | 0.001 ** | ||
| Quinolones | Ciprofloxacin po | J01MA02 | 1.43 | 0.89 | 1.29 | 0.74 | 0.90 | 0.192 ** |
| Ciprofloxacin pe | 0.02 | 0.02 | 0.03 | 0.01 | 1.58 | 0.581 ** | ||
| Levofloxacin | J01MA12 | 0.32 | 0.22 | 0.65 | 0.29 | 2.02 | 0.098 ** | |
| Moxifloxacin | J01MA14 | 0.03 | 0.04 | 0.06 | 0.09 | 2.07 | 0.299 ** | |
| Moxifloxacin pe | 0.01 | 0.01 | 0.02 | 0.03 | 3.07 | 0.760 * | ||
| Norfloxacin | J01MA06 | 0.19 | 1.41 | 0.17 | 1.33 | 0.88 | 0.812 ** | |
| TOTAL | 2.00 | 2.55 | 2.22 | 2.46 | 1.11 | 0.449 ** | ||
| Tetracyclines | Doxycycline | J01AA02 | 1.15 | 0.58 | 1.13 | 1.04 | 0.98 | 0.771 ** |
| TMS | J01EE01 | 1.04 | 0.96 | 0.86 | 0.49 | 0.83 | 0.192 ** | |
| Lincomycin po | J01FF02 | 0.05 | 0.18 | 0.03 | 0.06 | 0.53 | 0.792 ** | |
| Lincomycin pe | 0.00 | 0.01 | 0.00 | 0.00 | 0.58 | 0.891 ** | ||
| Clindamycin po | J01FF01 | 0.04 | 0.11 | 0.04 | 0.17 | 1.08 | 0.992 ** | |
| Clindamycin pe | 0.00 | 0.03 | 0.01 | 0.03 | 1.45 | 0.875 ** | ||
| Gentamicin | J01GB03 | 0.04 | 1.13 | 0.03 | 1.15 | 0.79 | 0.569 ** | |
| Nitrufurantoin | J01XE01 | 0.15 | 1.23 | 0.23 | 2.00 | 1.50 | 0.772 ** | |
| Metronidazol po | J01XD01 | 0.01 | 1.15 | 0.03 | 1.45 | 3.84 | 0.780 ** | |
| Metronidazol pe | 0.40 | 3.18 | 0.32 | 0.19 | 0.78 | 0.298 ** | ||
| TOTAL | 1.74 | 0.34 | 1.55 | 0.28 | 0.89 | 0.662 ** | ||
| Region of the Republic of Srpska | Groups of Antibiotics | DDD/TID | p | |||
|---|---|---|---|---|---|---|
| 2019 | 2020 | |||||
| Mean | SD | Mean | SD | |||
| Prijedor | Penicillins | 33.65 | 13.78 | 37.99 | 9.93 | 0.291 * |
| Cephalosporins | 5.97 | 1.72 | 7.06 | 1.87 | 0.039 * | |
| Macrolides | 6.78 | 1.44 | 10.80 | 3.45 | 0.002 * | |
| Quinolones | 6.95 | 1.58 | 7.28 | 1.49 | 0.078 ** | |
| Tetracyclines | 2.01 | 0.92 | 3.05 | 1.45 | 0.219 ** | |
| Others | 7.69 | 0.98 | 4.36 | 0.49 | 0.001 ** | |
| Banja Luka | Penicillins | 8.64 | 2.15 | 30.84 | 10.13 | <0.001 * |
| Cephalosporins | 2.02 | 0.43 | 9.21 | 4.08 | 0.003 * | |
| Macrolides | 1.95 | 0.48 | 2.86 | 0.91 | 0.023 * | |
| Quinolones | 1.75 | 0.39 | 1.97 | 0.36 | 0.562 ** | |
| Tetracyclines | 1.19 | 1.01 | 0.93 | 0.62 | 0.491 ** | |
| Others | 4.80 | 0.64 | 4.06 | 0.55 | 0.319 ** | |
| Doboj | Penicillins | 7.19 | 1.70 | 6.38 | 1.54 | 0.078 * |
| Cephalosporins | 1.38 | 0.27 | 1.63 | 0.30 | 0.639 * | |
| Macrolides | 1.07 | 0.26 | 1.41 | 0.46 | 0.048 * | |
| Quinolones | 1.07 | 0.22 | 1.04 | 0.19 | 0.344 ** | |
| Tetracyclines | 0.64 | 0.21 | 0.40 | 0.33 | 0.827 ** | |
| Others | 2.40 | 0.34 | 2.67 | 0.40 | 0.182 ** | |
| Bijeljina | Penicillins | 6.76 | 1.66 | 10.73 | 2.75 | 0.056 * |
| Cephalosporins | 0.17 | 0.42 | 1.82 | 2.22 | 0.872 * | |
| Macrolides | 1.44 | 0.28 | 2.32 | 0.73 | 0.009 * | |
| Quinolones | 1.41 | 0.33 | 1.73 | 0.38 | 0.412 ** | |
| Tetracyclines | 1.42 | 0.90 | 1.22 | 0,88 | 0.806 ** | |
| Others | 5.73 | 1.30 | 6.32 | 1.48 | 0.002 ** | |
| East Sarajevo | Penicillins | 5.79 | 1.05 | 8.64 | 2.32 | 0.276 * |
| Cephalosporins | 5.22 | 1.46 | 3.74 | 0.67 | 0.491 * | |
| Macrolides | 1.25 | 0.23 | 2.80 | 0.78 | 0.045 * | |
| Quinolones | 0.94 | 0.19 | 1.13 | 0.20 | 0.464 ** | |
| Tetracyclines | 0.52 | 0.14 | 0.69 | 0.51 | 0.374 ** | |
| Others | 7.50 | 1.22 | 5.62 | 1.14 | 0.091 ** | |
| Trebinje | Penicillins | 5.61 | 0.99 | 8.29 | 2.22 | 0.322 * |
| Cephalosporins | 3.21 | 0.64 | 6.79 | 2.22 | 0.079 * | |
| Macrolides | 1.29 | 0.29 | 3.09 | 1.09 | 0.005 * | |
| Quinolones | 0.64 | 0.17 | 0.88 | 0.20 | 0.093 ** | |
| Tetracyclines | 0.68 | 0.48 | 0.89 | 0.52 | 0.081 ** | |
| Others | 12.03 | 2.61 | 3.55 | 0.54 | 0.004 ** | |
| Region of the Republic of Srpska | Incidence Rate | Mortality Rate |
|---|---|---|
| Prijedor | 1467.80 | 145.39 |
| Banja Luka | 4248.47 | 183.45 |
| Doboj | 1947.16 | 159.90 |
| Bijeljina | 3019.22 | 109.39 |
| Istočno Sarajevo | 3763.21 | 160.90 |
| Trebinje | 4318.14 | 171.51 |
| Consumption of Antibiotics in Regions in the Republic of Srpska | Incidence Rate r (p) | Mortality Rate r (p) |
|---|---|---|
| Consumption of antibiotics (DDD/TID) in 2020 | 0.992 (<0.001) | −0.998 (<0.001) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sokolović, D.; Drakul, D.; Joksimović, B.; Lalović, N.; Avram, N.; Milić, M.; Nogo-Živanović, D.; Mijović, B. Consumption of Antibiotics in Primary Care Setting before and during COVID-19 Pandemic in Republic of Srpska, Bosnia and Herzegovina. Antibiotics 2022, 11, 1319. https://doi.org/10.3390/antibiotics11101319
Sokolović D, Drakul D, Joksimović B, Lalović N, Avram N, Milić M, Nogo-Živanović D, Mijović B. Consumption of Antibiotics in Primary Care Setting before and during COVID-19 Pandemic in Republic of Srpska, Bosnia and Herzegovina. Antibiotics. 2022; 11(10):1319. https://doi.org/10.3390/antibiotics11101319
Chicago/Turabian StyleSokolović, Dragana, Dragana Drakul, Bojan Joksimović, Nenad Lalović, Nada Avram, Marija Milić, Dajana Nogo-Živanović, and Biljana Mijović. 2022. "Consumption of Antibiotics in Primary Care Setting before and during COVID-19 Pandemic in Republic of Srpska, Bosnia and Herzegovina" Antibiotics 11, no. 10: 1319. https://doi.org/10.3390/antibiotics11101319
APA StyleSokolović, D., Drakul, D., Joksimović, B., Lalović, N., Avram, N., Milić, M., Nogo-Živanović, D., & Mijović, B. (2022). Consumption of Antibiotics in Primary Care Setting before and during COVID-19 Pandemic in Republic of Srpska, Bosnia and Herzegovina. Antibiotics, 11(10), 1319. https://doi.org/10.3390/antibiotics11101319








