Antibiotics Used in Empiric Treatment of Ocular Infections Trigger the Bacterial Rcs Stress Response System Independent of Antibiotic Susceptibility
Abstract
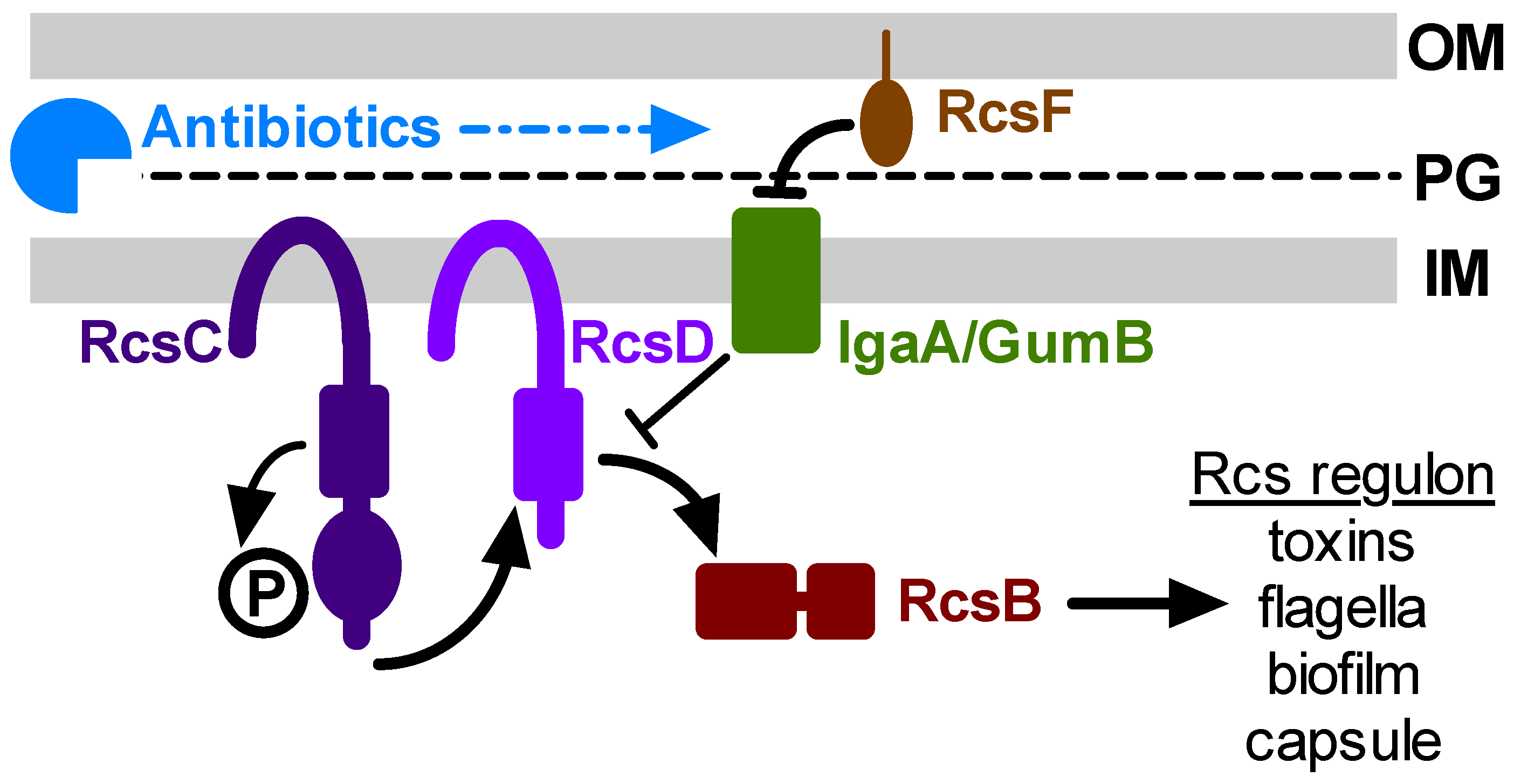
1. Introduction
2. Results
2.1. Generation of Luminescent Reporter Plasmids for Rcs System Activity
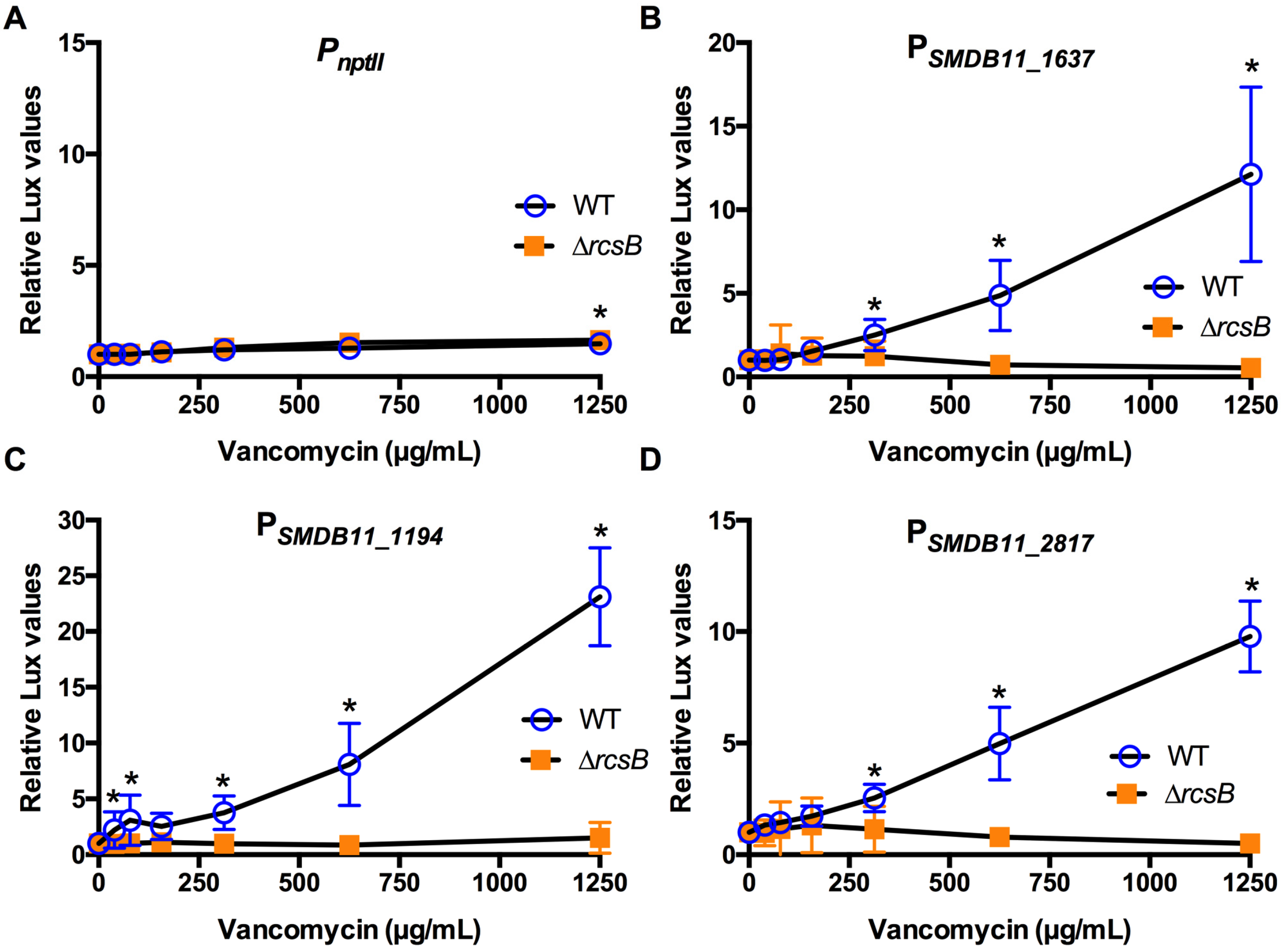
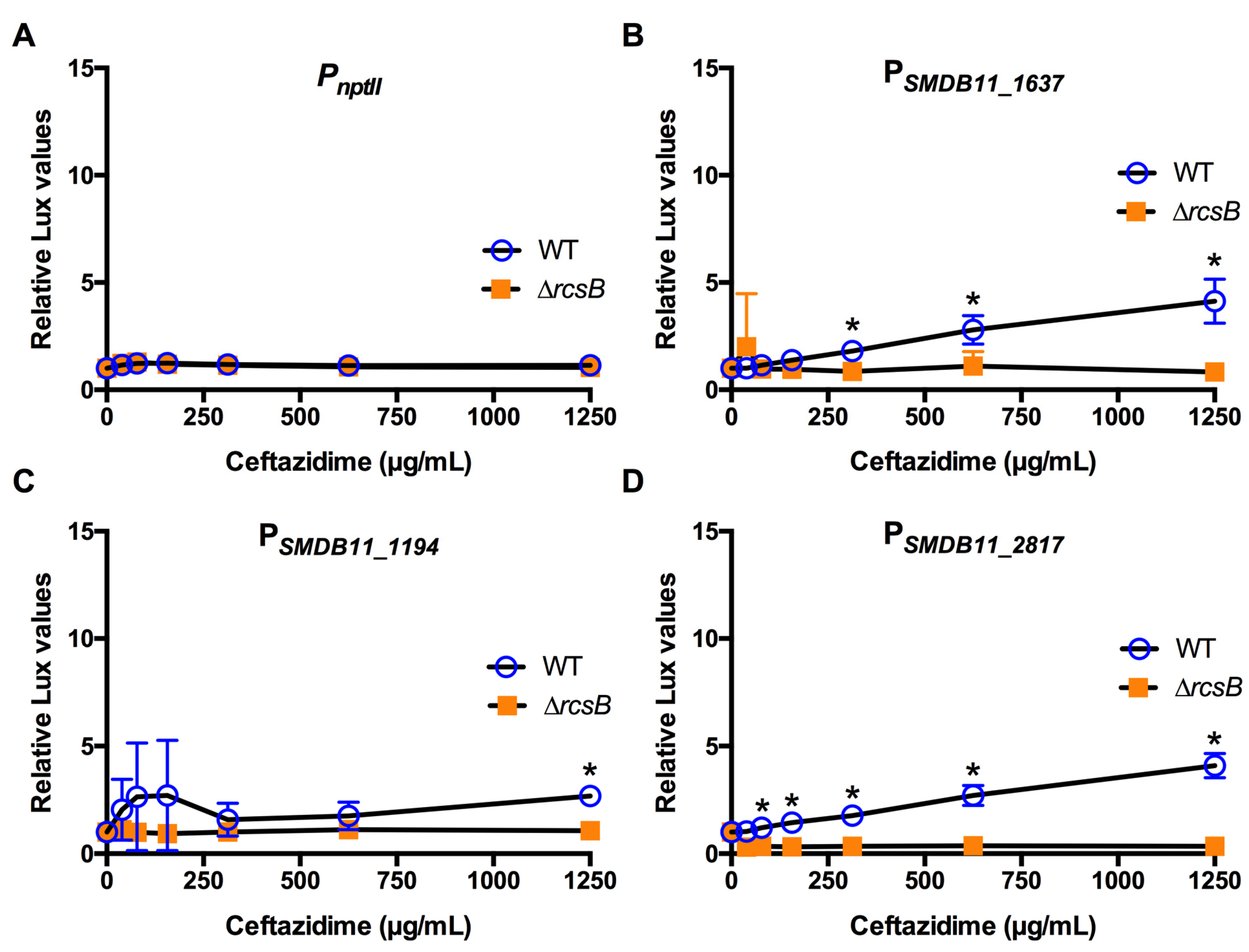
2.2. Antibiotics Targeting the Cell Envelope Activate the S. marcescens Rcs System Regardless of the Antibiotic Susceptibility Status of the Bacterium
2.3. Non-Cell Envelope-Targeting Antibiotics Activated the Test Promoters in an Rcs-Independent Manner
3. Discussion
4. Materials and Methods
4.1. Bacterial Growth and Media
4.2. Generation of Luminescence Reporters
4.3. Luminescent Reporter Assays
4.4. Minimum Inhibitory Concentration Analysis
4.5. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Conflicts of Interest
References
- Alexandrakis, G.; Alfonso, E.C.; Miller, D. Shifting trends in bacterial keratitis in south Florida and emerging resistance to fluoroquinolones. Ophthalmology 2000, 107, 1497–1502. [Google Scholar] [CrossRef]
- Hume, E.B.; Willcox, M.D. Emergence of Serratia marcescens as an ocular surface pathogen. Arch. Soc. Esp. Oftalmol. 2004, 79, 475–477. [Google Scholar]
- Mah-Sadorra, J.H.; Najjar, D.M.; Rapuano, C.J.; Laibson, P.R.; Cohen, E.J. Serratia corneal ulcers: A retrospective clinical study. Cornea 2005, 24, 793–800. [Google Scholar] [CrossRef] [PubMed]
- Mahlen, S.D. Serratia infections: From military experiments to current practice. Clin. Microbiol. Rev. 2011, 24, 755–791. [Google Scholar] [CrossRef] [PubMed]
- Richards, M.J.; Edwards, J.R.; Culver, D.H.; Gaynes, R.P. Nosocomial infections in combined medical-surgical intensive care units in the United States. Infect. Control Hosp. Epidemiol. 2000, 21, 510–515. [Google Scholar] [CrossRef] [PubMed]
- Stock, I.; Grueger, T.; Wiedemann, B. Natural antibiotic susceptibility of strains of Serratia marcescens and the S. liquefaciens complex: S. liquefaciens sensu stricto, S. proteamaculans and S. grimesii. Int. J. Antimicrob. Agents 2003, 22, 35–47. [Google Scholar] [CrossRef]
- Kowalski, R.P.; Kowalski, T.A.; Shanks, R.M.; Romanowski, E.G.; Karenchak, L.M.; Mah, F.S. In vitro comparison of combination and monotherapy for the empiric and optimal coverage of bacterial keratitis based on incidence of infection. Cornea 2013, 32, 830–834. [Google Scholar] [CrossRef]
- Wall, E.; Majdalani, N.; Gottesman, S. The Complex Rcs Regulatory Cascade. Annu. Rev. Microbiol. 2018, 72, 111–139. [Google Scholar] [CrossRef]
- Steenhuis, M.; Ten Hagen-Jongman, C.M.; van Ulsen, P.; Luirink, J. Stress-based high-througput screen assays to identify inhibitors of cell envelope biogenesis. Antibiotics 2020, 9, 808. [Google Scholar] [CrossRef] [PubMed]
- Erickson, K.D.; Detweiler, C.S. The Rcs phosphorelay system is specific to enteric pathogens/commensals and activates ydeI, a gene important for persistent Salmonella infection of mice. Mol. Microbiol. 2006, 62, 883–894. [Google Scholar] [CrossRef] [PubMed]
- Farris, C.; Sanowar, S.; Bader, M.W.; Pfuetzner, R.; Miller, S.I. Antimicrobial peptides activate the Rcs regulon through the outer membrane lipoprotein RcsF. J. Bacteriol. 2010, 192, 4894–4903. [Google Scholar] [CrossRef]
- Laubacher, M.E.; Ades, S.E. The Rcs phosphorelay is a cell envelope stress response activated by peptidoglycan stress and contributes to intrinsic antibiotic resistance. J. Bacteriol. 2008, 190, 2065–2074. [Google Scholar] [CrossRef] [PubMed]
- Konovalova, A.; Mitchell, A.M.; Silhavy, T.J. A lipoprotein/b-barrel complex monitors lipopolysaccharide integrity transducing information across the outer membrane. Elife 2016, 5, e15276. [Google Scholar] [CrossRef] [PubMed]
- Hirakawa, H.; Nishino, K.; Yamada, J.; Hirata, T.; Yamaguchi, A. Beta-lactam resistance modulated by the overexpression of response regulators of two-component signal transduction systems in Escherichia coli. J. Antimicrob. Chemother. 2003, 52, 576–582. [Google Scholar] [CrossRef] [PubMed]
- Lewis, K. Multidrug tolerance of biofilms and persister cells. Curr. Top. Microbiol. Immunol. 2008, 322, 107–131. [Google Scholar] [CrossRef]
- Stella, N.A.; Brothers, K.M.; Callaghan, J.D.; Passerini, A.M.; Sigindere, C.; Hill, P.J.; Liu, X.; Wozniak, D.J.; Shanks, R.M.Q. An IgaA/UmoB-family protein from Serratia marcescens regulates motility, capsular polysaccharide, and secondary metabolite production. Appl. Environ. Microbiol. 2018, 84, e02517–e02575. [Google Scholar] [CrossRef] [PubMed]
- Clarke, D.J. The Rcs phosphorelay: More than just a two-component pathway. Future Microbiol. 2010, 5, 1173–1184. [Google Scholar] [CrossRef]
- Smith, L.M.; Jackson, S.A.; Malone, L.M.; Ussher, J.E.; Gardner, P.P.; Fineran, P.F. The Rcs stress response inversely controls surface and CRISPR-Cas adaptive immunity to discriminate plasmids and phages. Nat. Microbiol. 2021, 6, 162–172. [Google Scholar] [CrossRef]
- Brothers, K.M.; Callaghan, J.D.; Stella, N.A.; Bachinsky, J.M.; AlHigaylan, M.; Lehner, K.L.; Franks, J.M.; Lathrop, K.L.; Collins, E.; Schmitt, D.M.; et al. Blowing epithelial cell bubbles with GumB: ShlA-family pore-forming toxins induce blebbing and rapid cellular death in corneal epithelial cells. PLoS Pathog. 2019, 15, e1007825. [Google Scholar] [CrossRef] [PubMed]
- Di Venanzio, G.; Stepanenko, T.M.; Garcia Vescovi, E. Serratia marcescens ShlA pore-forming toxin is responsible for early induction of autophagy in host cells and is transcriptionally regulated by RcsB. Infect. Immun. 2014, 82, 3542–3554. [Google Scholar] [CrossRef]
- Pan, X.; Tang, M.; You, J.; Liu, F.; Sun, C.; Osire, T.; Fu, W.; Yi, G.; Yang, T.; Yang, S.T.; et al. Regualtor RcsB controls prodigiosin synthesis and various cellular processes in Serratia marcescens JNB5-1. Appl. Environ. Microbiol. 2020, in press. [Google Scholar] [CrossRef]
- Romanowski, E.G.; Stella, N.A.; Romanowski, J.E.; Yates, K.A.; Dhaliwal, D.K.; St Leger, A.J.; Shanks, R.M.Q. The Rcs stress response system regulator GumB modulates Serratia marcescens induced inflammation and bacterial proliferation in a rabbit keratitis model and cytotoxicity in vitro. Infect. Immun. 2021, 89, e00111–e00121. [Google Scholar] [CrossRef]
- Lin, A.; Rhee, M.K.; Akpek, E.K.; Amescua, G.; Farid, M.; Garcia-Ferrer, F.J.; Varu, D.M.; Musch, D.C.; Dunn, S.P.; Mah, F.S.; et al. Bacterial Keratitis Preferred Practice Pattern(R). Ophthalmology 2019, 126, P1–P55. [Google Scholar] [CrossRef]
- Wang, D.; Qi, M.; Calla, B.; Korban, S.S.; Clough, S.J.; Cock, P.J.; Sundin, G.W.; Toth, I.; Zhao, Y. Genome-wide identification of genes regulated by the Rcs phosphorelay system in Erwinia amylovora. Mol. Plant-Microbe Interact. 2012, 25, 6–17. [Google Scholar] [CrossRef]
- Bury-Moné, S.; Nomane, Y.; Reymond, N.; Barbet, R.; Jacquet, E.; Imbeaud, S.; Jacq, A.; Bouloc, P. Global analysis of extracytoplasmic stress signaling in Escherichia coli. PLoS Genet. 2009, 5, e1000651. [Google Scholar] [CrossRef] [PubMed]
- Boulanger, A.; Frances-Charlot, A.; Conter, A.; Castanié-Cornet, M.-P.; Cam, K.; Gutierrez, C. Multistress regulation in Escherichia coli: Expression of osmB involves two independent promoters responding either to sigmaS or to the RcsCDB His-Asp phosphorelay. J. Bacteriol. 2005, 187, 3282–3286. [Google Scholar] [CrossRef] [PubMed]
- Howery, K.E.; Clemmer, K.M.; Rather, P.N. The Rcs regulon in Proteus mirabilis: Implications for motility, biofilm formation, and virulence. Curr. Genet. 2016, 62, 775–789. [Google Scholar] [CrossRef]
- Huesa, J.; Giner-Lamia, J.; Pucciarelli, M.G.; Paredes-Martínez, F.; García del Portillo, F.; Marina, A.; Casino, P. Structure-based analysis of Salmonella RcsB variants unravel new features of the Rcs regulon. Nucleic Acids Res. 2021, 49, 2357–2374. [Google Scholar] [CrossRef]
- Hinchliffe, S.J.; Howard, S.L.; Huang, Y.H.; Clarke, D.J.; Wren, B.W. The importance of the Rcs phosphorelay in the survival and pathogenesis of the enteropathogenic yersiniae. Microbiology 2008, 154, 1117–1131. [Google Scholar] [CrossRef]
- Lehner, K.M.; Stella, N.A.; Calvario, R.C.; Shanks, R.M.Q. mCloverBlaster: A tool to make markerless deletions and fusion using lambda red and I-SceI in Gram-negative bacterial genomes. J. Microbiol. Methods 2020, 178. [Google Scholar] [CrossRef]
- Cunha, B.A. Antibiotic Essentials; Physicians Press: Royal Oak, MI, USA, 2002. [Google Scholar]
- Healy, D.P.; Holland, E.J.; Nordlund, M.L.; Dunn, S.; Chow, C.; Lindstrom, R.L.; Hardten, D.; Davis, E. Concentrations of levofloxacin, ofloxacin, and ciprofloxacin in human corneal stromal tissue and aqueous humor after topical administration. Cornea 2004, 23, 255–263. [Google Scholar] [CrossRef]
- Tajima, K.; Miyake, T.; Koike, N.; Hattori, T.; Kumakura, S.; Yamaguchi, T.; Matsumoto, T.; Fujita, K.; Kuroda, M.; Ito, N.; et al. In vivo challenging of polymyxins and levofloxacin eye drops against multidrug-resistant Pseudomonas aeruginosa keratits. J. Infect. Chemother. 2014, 20, 343–349. [Google Scholar] [CrossRef]
- Protzko, E.; Bowman, L.; Abelson, M.; Shapiro, A. Phase 3 safety comparisons for 1.0% azithromycin in polymeric mucoadhesive eye drops versus 0.3% tobramycin eye drops for bacterial conjuntivitis. Investig. Ophthalmol. Vis. Sci. 2007, 48, 3425–3429. [Google Scholar] [CrossRef]
- Romanowski, E.G.; Romanowski, J.E.; Shanks, R.M.Q.; Yates, K.A.; Mammen, A.; Dhaliwal, D.K.; Jhanji, V.; Kowalski, R.P. Topical vancomycin 5% is more efficacious than 2.5% and 1.25% for reducing viable methicillin-resistant Staphylococcus aureus in infectious keratitis. Cornea 2020, 39, 250–253. [Google Scholar] [CrossRef]
- Cahane, M.; Ben Simon, G.J.; Barequet, I.S.; Grinbaum, A.; Diamanstein-Weiss, L.; Goller, O.; Rubinstein, E.; Avni, I. Human corneal stromal tissue concentration after consecutive doses of topically applied 3.3% vancomycin. Br. J. Ophthalmol. 2004, 88, 22–24. [Google Scholar] [CrossRef] [PubMed][Green Version]
- CLSI. Performance Standards for Antimicrobial Susceptibility Testing 24th Informational Supplement; CLSI Document M100-S24; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2014; pp. 51–57. [Google Scholar]
- Lin, Q.Y.; Tsai, Y.L.; Liu, M.C.; Lin, W.C.; Hsueh, P.R.; Liaw, S.J. Serratia marcescens arn, a PhoP-regulated locus necessary for polymyxin B resistance. Antimicrob. Agents Chemother. 2014, 58, 5180–5190. [Google Scholar] [CrossRef]
- Romanowski, E.G.; Mah, F.S.; Yates, K.A.; Kowalski, R.P.; Gordon, Y.J. The successful treatment of gatifloxacin-resistant Staphylococcus aureus keratitis with Zymar (gatifloxacin 0.3%) in a NZW rabbit model. Am. J. Ophthalmol. 2005, 139, 867–877. [Google Scholar] [CrossRef]
- Kowalski, R.P.; Romanowski, E.G.; Mah, F.S.; Shanks, R.M.; Gordon, Y.J. Topical levofloxacin 1.5% overcomes in vitro resistance in rabbit keratitis models. Acta Ophthalmol. 2010, 88, e120–e125. [Google Scholar] [CrossRef] [PubMed]
- Kowalski, R.P.; Romanowski, E.G.; Yates, K.A.; Romanowski, J.E.; Grewal, A.; Bilonick, R.A. Is there a role for topical penicillin treatment of Staphylococcus aureus keratitis based on elevated corneal concentrations? J. Clin. Ophthalmol. Optom. 2018, 2, 103. [Google Scholar]
- McDermott, A.M. Antimicrobial compounds in tears. Exp. Eye Res. 2013, 117, 53–61. [Google Scholar] [CrossRef] [PubMed]
- Pearlman, E.; Sun, Y.; Roy, S.; Karmakar, M.; Hise, A.G.; Szczotka-Flynn, L.; Ghannoum, M.; Chinnery, H.R.; McMenamin, P.G.; Rietsch, A. Host defense at the ocular surface. Int. Rev. Immunol. 2013, 32, 4–18. [Google Scholar] [CrossRef]
- Vasilchenko, A.S.; Rogozhin, E.A. Sub-inhibitory effects of antimicrobial peptides. Front. Microbiol. 2019, 10, 1160. [Google Scholar] [CrossRef] [PubMed]
- Poole, K. Bacterial stress responses as determinants of antimicrobial resistance. J. Antimicrob. Chemother. 2012, 67, 2069–2089. [Google Scholar] [CrossRef]
- Flores-Kim, J.; Darwin, A.J. Regulation of bacterial virulence gene expression by cell envelope stress responses. Virulence 2014, 5, 835–851. [Google Scholar] [CrossRef]
- Laloux, G.; Collet, J.F. Major Tom to ground control: How lipoproteins communicate extracytoplasmic stress to the decision center of the cell. J. Bact. 2017, 199, 00216–00217. [Google Scholar] [CrossRef] [PubMed]
- Macritchie, D.M.; Raivio, T.L. Envelope Stress Responses. EcoSal Plus 2009, 3. [Google Scholar] [CrossRef] [PubMed]
- Bruna, R.E.; Molino, M.V.; Lazzaro, M.; Mariscotti, J.F.; Garcia Véscovi, E. CpxR-dependent thermoregulation of Serratia marcescens PrtA metalloprotease expression and its contribution to bacterial biofilm formation. J. Bacteriol. 2018, 200, e00006–e00018. [Google Scholar] [CrossRef] [PubMed]
- Qin, H.; Liu, Y.; Cao, X.; Jiang, J.; Lian, W.; Qiao, D.; Xu, H.; Cao, Y. RpoS is a peiotropic regulator of motility, biofilm formation, exoenzymes, siderophore and prodigiosin production, and trade-off during prolonged stationary phase in Serratia marcescens. PLoS ONE 2020, 15, e0232549. [Google Scholar] [CrossRef]
- Sun, Y.; Wang, L.; Pan, X.; Osire, T.; Fang, H.; Zhang, H.; Yang, S.T.; Yang, T.; Rao, Z. Improved prodigiosin production by relieving CpxR temperature-sensitive inhibition. Front. Bioeng. Biotechnol. 2020, 8, 344. [Google Scholar] [CrossRef]
- Wilf, N.M.; Salmond, G.P. The stationary phase sigma factor, RpoS, regulates the production of a carbapenem antibiotic, a bioactive prodigiosin and virulence in the enterobacterial pathogen Serratia sp. ATCC 39006. Microbiology 2012, 158, 648–658. [Google Scholar] [CrossRef]
- Steenhuis, M.; Corona, F.; Ten Hagen-Jongman, C.M.; Vollmer, W.; Lambin, D.; Selhorst, P.; Klaassen, H.; Versele, M.; Chatltin, P.; Luirink, J. Combining cell envelope stress reporter assays in a screening approach to identify BAM complex inhibitors. ACS Infect. Dis. 2021, in press. [Google Scholar] [CrossRef] [PubMed]
- Bertani, G. Studies on lysogenesis. I. The mode of phage liberation by lysogenic Escherichia coli. J. Bacteriol. 1951, 62, 293–300. [Google Scholar] [CrossRef] [PubMed]
- Shanks, R.M.; Stella, N.A.; Kalivoda, E.J.; Doe, M.R.; O’Dee, D.M.; Lathrop, K.L.; Guo, F.L.; Nau, G.J. A Serratia marcescens OxyR homolog mediates surface attachment and biofilm formation. J. Bacteriol. 2007, 189, 7262–7272. [Google Scholar] [CrossRef] [PubMed]
- Romanowski, E.G.; Lehner, K.M.; Martin, N.C.; Patel, K.R.; Callaghan, J.D.; Stella, N.A.; Shanks, R.M.Q. Thermoregulation of prodigiosin biosynthesis by Serratia marcescens is controlled at the transcriptional level and requires HexS. Pol. J. Microbiol. 2019, 68, 43–50. [Google Scholar] [CrossRef]
- Shanks, R.M.; Caiazza, N.C.; Hinsa, S.M.; Toutain, C.M.; O’Toole, G.A. Saccharomyces cerevisiae-based molecular tool kit for manipulation of genes from gram-negative bacteria. Appl. Environ. Microbiol. 2006, 72, 5027–5036. [Google Scholar] [CrossRef]
- Shanks, R.M.; Kadouri, D.E.; MacEachran, D.P.; O’Toole, G.A. New yeast recombineering tools for bacteria. Plasmid 2009, 62, 88–97. [Google Scholar] [CrossRef]
- Callaghan, J.D.; Stella, N.A.; Lehner, K.M.; Treat, B.R.; Brothers, K.M.; St Leger, A.J.; Shanks, R.M.Q. Generation of Xylose-inducible promoter tools for Pseudomonas species and their use in implicating a role for the Type II secretion system protein XcpQ in inhibition of corneal epithelial wound closure. Appl. Environ. Microbiol. 2020, 86, e00250-20. [Google Scholar] [CrossRef] [PubMed]





| Antibiotic | Typical Topical Drug Concentration [23] | Corneal Tissue Concentration | Typical Systemic Dose | Peak Serum Concentration (µg/mL) | Antibiotic Concentration Used in This Study (µg/mL) |
|---|---|---|---|---|---|
| Cefazolin | 50 mg/mL Fortified [23] | NA | 1 g (IV) q8h [31] | 200 µg/mL [31] | 39–1250 |
| Ceftazidime | 50 mg/mL Fortified [23] | NA | 2 g (IV) q8h [31] | 120 µg/mL [31] | 39–1250 |
| Ciprofloxacin | 3 mg/mL Commercial [23] | 9.92 ± 10.99 μg/g [32] | 400 mg (IV) q12h [31] 500–750 mg (PO) q12h [31] | 4.6 µg/mL [31] (IV) 2.8 µg/mL [31] (PO) | 2.5–75 |
| Polymyxin B | 0.75–1 mg/mL (7500–10,000 units/mL) Commercial [33] | NA | 1.25 mg/kg (IV) q12h (1 mg = 10,000 units) [31] | 8 µg/mL [31] | 30–10,000 |
| Tobramycin | 3 mg/mL Commercial [34] 9–14 mg/mL Fortified [23] | NA | 5 mg/kg (IV) q24h [31] or 240 mg (IV) q24h [31] (preferred over q8h dosing) | 16–24 µg/mL q24h dosing [31] | 8–250 |
| Vancomycin | 10–50 mg/mL [23,35] | 46.7 µg/g [36] | 1 g (IV) q12h [31] | 40 µg/mL [31] | 39–1250 |
| Antibiotic | Class | Target | MIC a—WT (µg/mL) | MIC—∆rcsB (µg/mL) | Susceptibility b | Rcs-Specific Induction c |
|---|---|---|---|---|---|---|
| Cefazolin | Cephalosporin | Cell wall | >256, >256 | >256, >256 | No | Yes |
| Ceftazidime | Cephalosporin | Cell wall | 0.25, 0.19 | 0.19, 0.19 | Yes | Yes |
| Ciprofloxacin | Fluoroquinolone | DNA gyrase and topoisomerase IV | 0.064, 0.064 | 0.094, 0.470 | Yes | No |
| Polymyxin B | Polymyxin | Cell membrane | >1024, >1024 | >1024, >1024 | No | Yes |
| Tobramycin | Aminoglycoside | Ribosome | 2, 2 | 1.5, 1.5 | Yes | No |
| Vancomycin | Glycopeptide | Cell wall | >256, >256 | >256, >256 | No | Yes |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Harshaw, N.S.; Stella, N.A.; Lehner, K.M.; Romanowski, E.G.; Kowalski, R.P.; Shanks, R.M.Q. Antibiotics Used in Empiric Treatment of Ocular Infections Trigger the Bacterial Rcs Stress Response System Independent of Antibiotic Susceptibility. Antibiotics 2021, 10, 1033. https://doi.org/10.3390/antibiotics10091033
Harshaw NS, Stella NA, Lehner KM, Romanowski EG, Kowalski RP, Shanks RMQ. Antibiotics Used in Empiric Treatment of Ocular Infections Trigger the Bacterial Rcs Stress Response System Independent of Antibiotic Susceptibility. Antibiotics. 2021; 10(9):1033. https://doi.org/10.3390/antibiotics10091033
Chicago/Turabian StyleHarshaw, Nathaniel S., Nicholas A. Stella, Kara M. Lehner, Eric G. Romanowski, Regis P. Kowalski, and Robert M. Q. Shanks. 2021. "Antibiotics Used in Empiric Treatment of Ocular Infections Trigger the Bacterial Rcs Stress Response System Independent of Antibiotic Susceptibility" Antibiotics 10, no. 9: 1033. https://doi.org/10.3390/antibiotics10091033
APA StyleHarshaw, N. S., Stella, N. A., Lehner, K. M., Romanowski, E. G., Kowalski, R. P., & Shanks, R. M. Q. (2021). Antibiotics Used in Empiric Treatment of Ocular Infections Trigger the Bacterial Rcs Stress Response System Independent of Antibiotic Susceptibility. Antibiotics, 10(9), 1033. https://doi.org/10.3390/antibiotics10091033







