Antibiotic Usage and Resistance in Food Animal Production: What Have We Learned from Bangladesh?
Abstract
1. Introduction
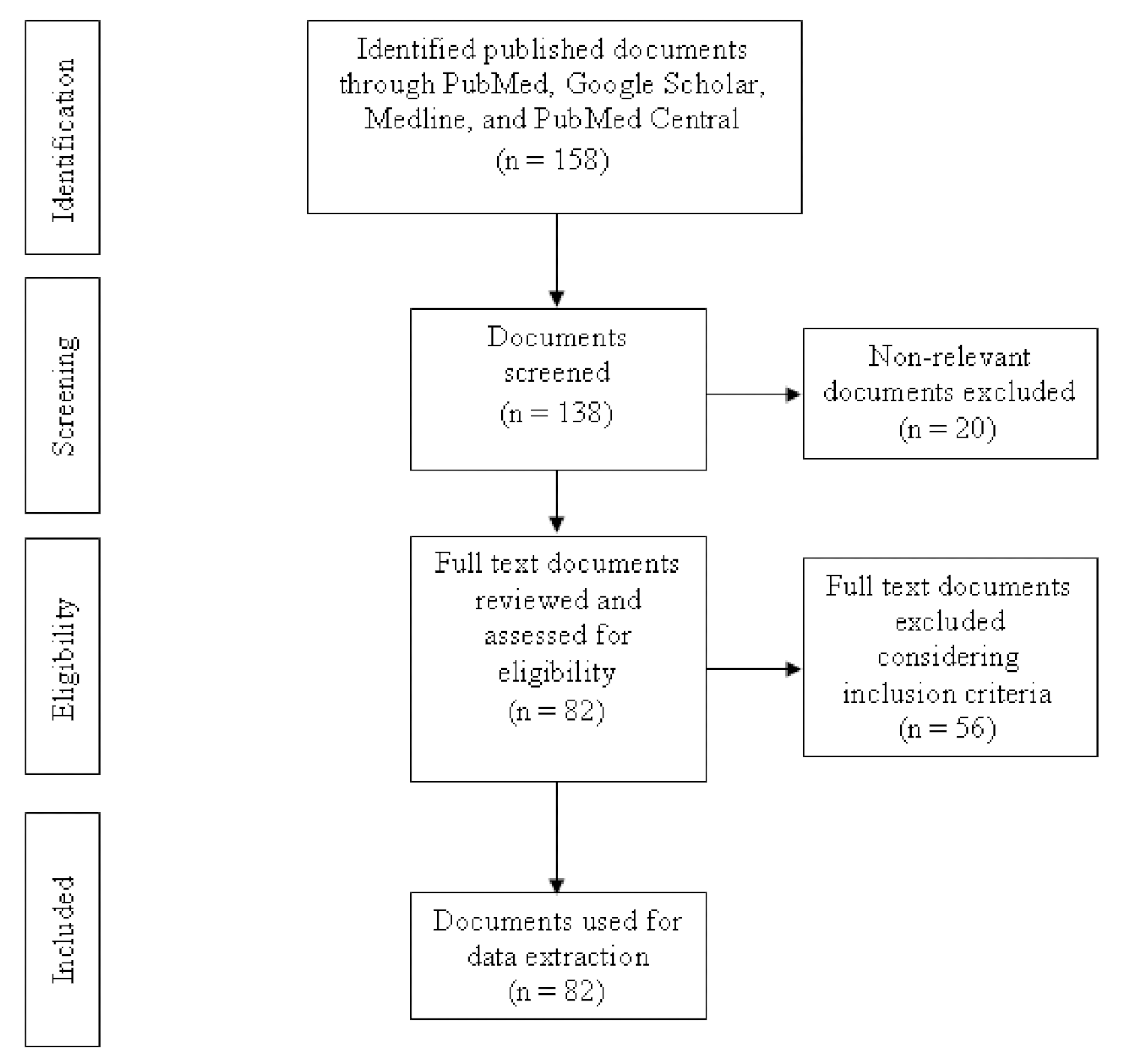
2. Materials and Methods
3. Results
3.1. Antibiotic Usage and Resistance in Commercial Layer Chicken
3.2. Antibiotic Usage and Resistance in Commercial Broiler Chicken
3.3. Antibiotic Usage and Resistance in Aquaculture
3.4. Antibiotic Usage and Resistance in Duck, Pigeon, Quail, and Sonali Chicken
3.5. Antibiotic Usage and Resistance in Livestock
3.6. Antibiotic Residues and Resistance in Animal-Origin Foods
4. Discussion
5. Conclusions and Recommendations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Smolinski, M.; Hamburg, M.; Lederberg, J. Emerging Microbial Threats to Health in the 21st Century; National Academy of Sciences: Washington DC, USA, 2003. [Google Scholar]
- Jansen, W.; Van der Bruggen, J.; Verhoef, J.; Fluit, A. Bacterial resistance: A sensitive issue: Complexity of the challenge and containment strategy in Europe. Drug. Resist. Updates 2006, 9, 123–133. [Google Scholar] [CrossRef]
- Wongsuvan, G.; Wuthiekanun, V.; Hinjoy, S.; Day, N.P.; Limmathurotsakul, D. Antibiotic use in poultry: A survey of eight farms in Thailand. Bull. World Health Organ. 2018, 96, 94. [Google Scholar] [CrossRef] [PubMed]
- Carrique-Mas, J.J.; Trung, N.V.; Hoa, N.T.; Mai, H.H.; Thanh, T.H.; Campbell, J.I.; Wagenaar, J.A.; Hardon, A.; Hieu, T.Q.; Schultsz, C. Antimicrobial usage in chicken production in the Mekong Delta of Vietnam. Zoonoses Public Health 2015, 62, 70–78. [Google Scholar] [CrossRef] [PubMed]
- Tasmim, S.T.; Hasan, M.M.; Talukder, S.; Mandal, A.K.; Parvin, M.S.; Ali, M.Y.; Ehsan, M.A.; Islam, M.T. Socio-demographic determinants of use and misuse of antibiotics in commercial poultry farms in Bangladesh. Int. J. Infect. Dis. 2020, 101, 90. [Google Scholar] [CrossRef]
- Van Boeckel, T.P.; Brower, C.; Gilbert, M.; Grenfell, B.T.; Levin, S.A.; Robinson, T.P.; Teillant, A.; Laxminarayan, R. Global trends in antimicrobial use in food animals. Proc. Natl. Acad. Sci. USA 2015, 112, 5649–5654. [Google Scholar] [CrossRef] [PubMed]
- OIE. OIE Standards, Guidelines and Resolutionon Antimicrobial Resistanceand the Use of Antimicrobial Agents. World Organisation for Animal Health. Available online: https://web.oie.int/delegateweb/eng/ebook/AF-book-AMR-ANG_FULL.pdf?WAHISPHPSESSID=03152ead00d06990fa9066b7b71fcabc (accessed on 30 June 2021).
- EMA. Categorisation of Antibiotics in the European Union. Answer to the Request from the European Commission for Updating the Scientific Advice on the Impact on Public Health and Animal Health of the Use of Antibiotics in Animals. European Medicines Agency. Available online: https://www.ema.europa.eu/en/documents/report/categorisation-antibiotics-european-union-answer-request-european-commission-updating-scientific_en.pdf (accessed on 4 April 2021).
- Pokharel, S.; Raut, S.; Adhikari, B. Tackling Antimicrobial Resistance in Low-Income and Middle-Income Countries. BMJ Glob. Health 2019, 4, e002104. [Google Scholar] [CrossRef]
- Rabinowitz, P.M.; Kock, R.; Kachani, M.; Kunkel, R.; Thomas, J.; Gilbert, J.; Wallace, R.; Blackmore, C.; Wong, D.; Karesh, W. Toward proof of concept of a one health approach to disease prediction and control. Emerg. Infect. Dis. 2013, 19, e130265. [Google Scholar] [CrossRef]
- Kahn, L.H. The need for one health degree programs. Infect. Ecol. Epidemiol. 2011, 1, 7919. [Google Scholar] [CrossRef]
- WHO. Global Antimicrobial Resistance and Use Surveillance System (GLASS) Report: 2021. World Health Organization. Available online: https://www.who.int/publications/i/item/9789240027336 (accessed on 3 March 2021).
- Dolberg, F. Poultry Sector Country Review, Bangladesh. Available online: http://www.fao.org/3/ai319e/ai319e.pdf (accessed on 25 February 2021).
- Hennessey, M.; Fournié, G.; Hoque, M.A.; Biswas, P.K.; Alarcon, P.; Ebata, A.; Mahmud, R.; Hasan, M.; Barnett, T. Intensification of fragility: Poultry production and distribution in Bangladesh and its implications for disease risk. Prev. Vet. Med. 2021, 191, 105367. [Google Scholar] [CrossRef]
- Hossain, A.; Nakamichi, S.; Habibullah-Al-Mamun, M.; Tani, K.; Masunaga, S.; Matsuda, H. Occurrence, distribution, ecological and resistance risks of antibiotics in surface water of finfish and shellfish aquaculture in Bangladesh. Chemosphere 2017, 188, 329–336. [Google Scholar] [CrossRef]
- Belton, B.; Azad, A. The characteristics and status of pond aquaculture in Bangladesh. Aquaculture 2012, 358, 196–204. [Google Scholar] [CrossRef]
- Islam, K.S.; Shiraj-Um-Mahmuda, S.; Hazzaz-Bin-Kabir, M. Antibiotic usage patterns in selected broiler farms of Bangladesh and their public health implications. J. Public Health Dev. Ctries. 2016, 2, 276–284. [Google Scholar]
- Ali, H.; Rico, A.; Murshed-e-Jahan, K.; Belton, B. An assessment of chemical and biological product use in aquaculture in Bangladesh. Aquaculture 2016, 454, 199–209. [Google Scholar]
- Al Masud, A.; Rousham, E.K.; Islam, M.A.; Alam, M.-U.; Rahman, M.; Al Mamun, A.; Sarker, S.; Asaduzzaman, M.; Unicomb, L. Drivers of antibiotic use in poultry production in Bangladesh: Dependencies and dynamics of a patron-client relationship. Front. Vet. Sci. 2020, 7, 78. [Google Scholar] [CrossRef]
- Rousham, E.K.; Asaduzzaman, M.; Mozmader, T.A.U.; Amin, M.B.; Rahman, M.; Hossain, M.I.; Islam, M.R.; Mahmud, Z.H.; Unicomb, L.; Islam, M.A. Human Colonization with Extended-Spectrum Beta-Lactamase-Producing, E. coli in Relation to Animal and Environmental Exposures in Bangladesh: An Observational One Health Study. Environ. Health Perspect. 2021, 129, 037001. [Google Scholar] [CrossRef]
- Al Amin, M.; Hoque, M.N.; Siddiki, A.Z.; Saha, S.; Kamal, M.M. Antimicrobial resistance situation in animal health of Bangladesh. Vet. World 2020, 13, 2713. [Google Scholar] [CrossRef]
- Landers, T.F.; Cohen, B.; Wittum, T.E.; Larson, E.L. A review of antibiotic use in food animals: Perspective, policy, and potential. Public Health Rep. 2012, 127, 4–22. [Google Scholar] [CrossRef] [PubMed]
- MOHFW. National Action Plan Antimicrobial Resistance Containment in Bangladesh 2017–2022. Ministry of Health & Family Welfare, Bangladesh. Available online: https://www.flemingfund.org/wp-content/uploads/d3379eafad36f597500cb07c21771ae3.pdf (accessed on 15 March 2021).
- DGDA. National Drug Policy 2016. Directorate General of Drug Administration. Ministry of Health & Family Welfare, Government of the People’s Republic of Bangladesh. 2016. Available online: https://www.dgda.gov.bd/index.php/laws-and-policies/261-national-drug-policy-2016-english-version/file (accessed on 23 April 2021).
- Bangladesh Gazette. Fish Feed and Animal Feed Act 2010. Available online: http://extwprlegs1.fao.org/docs/pdf/bgd165024.pdf (accessed on 20 April 2021).
- The Fleming Fund. Terms of Reference for Request for Proposals for The Fleming Fund Country Grant to Bangladesh. Available online: https://www.flemingfund.org/wp-content/uploads/1eb5e64133eb067da9f28acb86cd39cd.pdf (accessed on 30 May 2021).
- Imam, T.; Gibson, J.S.; Foysal, M.; Das, S.B.; Gupta, S.D.; Fournié, G.; Hoque, M.A.; Henning, J. A cross-sectional study of antimicrobial usage on commercial broiler and layer chicken farms in Bangladesh. Front. Vet. Sci. 2020, 7, 576113. [Google Scholar] [CrossRef] [PubMed]
- Ferdous, J.; Sachi, S.; Zakaria Al Noman, S.; Hussani, Y.A.S.; Sikder, M.H. Assessing farmers’ perspective on antibiotic usage and management practices in small-scale layer farms of Mymensingh district, Bangladesh. Vet. World 2019, 12, 1441. [Google Scholar] [CrossRef] [PubMed]
- Roess, A.A.; Winch, P.J.; Ali, N.A.; Akhter, A.; Afroz, D.; El Arifeen, S.; Darmstadt, G.L.; Baqui, A.H.; Group, B.P.S. Animal husbandry practices in rural Bangladesh: Potential risk factors for antimicrobial drug resistance and emerging diseases. Am. J. Trop. Med. Hyg. 2013, 89, 965–970. [Google Scholar] [PubMed]
- Islam, S.; Urmi, U.L.; Rana, M.; Sultana, F.; Jahan, N.; Hossain, B.; Iqbal, S.; Hossain, M.M.; Mosaddek, A.S.M.; Nahar, S. High abundance of the colistin resistance gene mcr-1 in chicken gut-bacteria in Bangladesh. Sci. Rep. 2020, 10, 1–11. [Google Scholar] [CrossRef]
- Ahmed, S.; Das, T.; Islam, M.Z.; Herrero-Fresno, A.; Biswas, P.K.; Olsen, J.E. High prevalence of mcr-1-encoded colistin resistance in commensal Escherichia coli from broiler chicken in Bangladesh. Sci. Rep. 2020, 10, 1–13. [Google Scholar] [CrossRef]
- Jakobsen, L.; Spangholm, D.J.; Pedersen, K.; Jensen, L.B.; Emborg, H.-D.; Agersø, Y.; Aarestrup, F.M.; Hammerum, A.M.; Frimodt-Møller, N. Broiler chickens, broiler chicken meat, pigs and pork as sources of ExPEC related virulence genes and resistance in Escherichia coli isolates from community-dwelling humans and UTI patients. Int. J. Food Microbiol. 2010, 142, 264–272. [Google Scholar] [CrossRef]
- Ievy, S.; Islam, M.; Sobur, M.; Talukder, M.; Rahman, M.; Khan, M.F.R. Molecular detection of avian pathogenic Escherichia coli (APEC) for the first time in layer farms in Bangladesh and their antibiotic resistance patterns. Microorganisms 2020, 8, 1021. [Google Scholar] [CrossRef] [PubMed]
- Hasan, B.; Faruque, R.; Drobni, M.; Waldenström, J.; Sadique, A.; Ahmed, K.U.; Islam, Z.; Parvez, M.H.; Olsen, B.; Alam, M. High prevalence of antibiotic resistance in pathogenic Escherichia coli from large-and small-scale poultry farms in Bangladesh. Avian Dis. 2011, 55, 689–692. [Google Scholar] [CrossRef] [PubMed]
- Humphrey, T. Public-health aspects of Salmonella infection. Salmonella Domest. Anim. 2000, 1, 245–263. [Google Scholar]
- Sarker, B.R.; Ghosh, S.; Chowdhury, S.; Dutta, A.; Chandra Deb, L.; Krishna Sarker, B.; Sultana, T.; Mozaffor Hossain, K.M. Prevalence and antimicrobial susceptibility profiles of non-typhoidal Salmonella isolated from chickens in Rajshahi, Bangladesh. Vet. Med. Sci. 2021, 7, 820–830. [Google Scholar] [CrossRef] [PubMed]
- Catry, B.; Cavaleri, M.; Baptiste, K.; Grave, K.; Grein, K.; Holm, A.; Jukes, H.; Liebana, E.; Navas, A.L.; Mackay, D. Use of colistin-containing products within the European Union and European Economic Area (EU/EEA): Development of resistance in animals and possible impact on human and animal health. Int. J. Antimicrob. Agents 2015, 46, 297–306. [Google Scholar] [CrossRef]
- Das, A.; Dhar, P.K.; Dutta, A.; Jalal, M.S.; Ghosh, P.; Das, T.; Barua, H.; Biswas, P.K. Circulation of oxytetracycline-and ciprofloxacin-resistant commensal Escherichia coli strains in broiler chickens and farm environments, Bangladesh. Vet. World 2020, 13, 2395. [Google Scholar] [CrossRef]
- Sarker, M.S.; Mannan, M.S.; Ali, M.Y.; Bayzid, M.; Ahad, A.; Bupasha, Z.B. Antibiotic resistance of Escherichia coli isolated from broilers sold at live bird markets in Chattogram, Bangladesh. J. Adv. Vet. Anim. Res. 2019, 6, 272. [Google Scholar] [CrossRef]
- Alam, B.; Uddin, M.; Mridha, D.; Akhter, A.; Islam, S.; Haque, A.; Kabir, S. Occurrence of Campylobacter spp. in Selected Small Scale Commercial Broiler Farms of Bangladesh Related to Good Farm Practices. Microorganisms 2020, 8, 1778. [Google Scholar] [CrossRef] [PubMed]
- Neogi, S.B.; Islam, M.M.; Islam, S.S.; Akhter, A.T.; Sikder, M.M.H.; Yamasaki, S.; Kabir, S.L. Risk of multi-drug resistant Campylobacter spp. and residual antimicrobials at poultry farms and live bird markets in Bangladesh. BMC Infect. Dis. 2020, 20, 1–14. [Google Scholar] [CrossRef]
- Al Azad, M.; Rahman, A.; Rahman, M.; Amin, R.; Begum, M.; Ara, I.; Fries, R.; Husna, A.; Khairalla, A.S.; Badruzzaman, A. Susceptibility and multidrug resistance patterns of Escherichia coli isolated from cloacal swabs of live broiler chickens in Bangladesh. Pathogens 2019, 8, 118. [Google Scholar] [CrossRef] [PubMed]
- Alam, S.B.; Mahmud, M.; Akter, R.; Hasan, M.; Sobur, A.; Nazir, K.; Noreddin, A.; Rahman, T.; El Zowalaty, M.E.; Rahman, M. Molecular detection of multidrug resistant Salmonella species isolated from broiler farm in Bangladesh. Pathogens 2020, 9, 201. [Google Scholar] [CrossRef]
- Antunes, P.; Mourão, J.; Campos, J.; Peixe, L. Salmonellosis: The role of poultry meat. Clin. Microbiol. Infect. 2016, 22, 110–121. [Google Scholar] [CrossRef] [PubMed]
- Authority, E.F.S. Analysis of the baseline survey on the prevalence of Campylobacter in broiler batches and of Campylobacter and Salmonella on broiler carcasses, in the EU, 2008-Part B: Analysis of factors associated with Campylobacter colonisation of broiler batches and with Campylobacter contamination of broiler carcasses; and investigation of the culture method diagnostic characteristics used to analyse broiler carcass samples. EFSA J. 2010, 8, 1522. [Google Scholar]
- Kawsar, M.A.; Alam, M.T.; Ahamed, S.; Mou, M.H. Aqua drugs and antibiotics used in freshwater aquaculture of North Chittagong, Bangladesh. Int. J. Fish. Aquat. Stud. 2019, 7, 28–34. [Google Scholar]
- Rahman, M.Z. Aquaculture drugs used for fish and shellfish health management in the Southwestern Bangladesh. Asian J. Biol. Sci. 2014, 7, 225–232. [Google Scholar]
- Chowdhury, A.J.; Saha, D.; Hossain, M.B.; Shamsuddin, M.; Minar, M.H. Chemicals used in freshwater aquaculture with special emphasis to fish health management of Noakhali, Bangladesh. Afr. J. Basic Appl. Sci. 2012, 4, 110–114. [Google Scholar]
- Uddin, S.A.; Kader, M.A. The use of antibiotics in shrimp hatcheries in Bangladesh. J. Fish. Aquat. Sci. 2006, 1, 64–67. [Google Scholar]
- Hossain, F.E.; Chakraborty, S.; Bhowmick, N.C.; Rahman, M.A.; Ahmed, F. Comparative analysis of antibiotic resistance pattern of bacteria isolated from fish of cultured and natural ponds: A study based on noakhali region of Bangladesh. Biores. Commun.-BRC 2018, 4, 586–591. [Google Scholar]
- Foysal, M.; Rahman, M.; Alam, M. Antibiotic sensitivity and in vitro antimicrobial activity of plant extracts to pseudomonas fluorescens isolates collected from diseased fish. Int. J. Nat. Sci. 2011, 1, 82–88. [Google Scholar] [CrossRef]
- Ahmed, T.; Baidya, S.; Sharma, B.C.; Malek, M.; Das, K.K.; Acharjee, M.; Munshi, S.K.; Noor, R. Identification of drug-resistant bacteria among export quality shrimp samples in Bangladesh. AsianJ. Microbiol. Biotechnol.Environ. Sci. 2013, 15, 31–36. [Google Scholar]
- Siddique, A.B.; Moniruzzaman, M.; Ali, S.; Dewan, M.; Islam, M.R.; Islam, M.; Amin, M.B.; Mondal, D.; Parvez, A.K.; Mahmud, Z.H. Characterization of Pathogenic Vibrio parahaemolyticus Isolated From Fish Aquaculture of the Southwest Coastal Area of Bangladesh. Front. Microbiol. 2021, 12, 266. [Google Scholar] [CrossRef] [PubMed]
- Rahman, M.M.; Rahman, M.M.; Meher, M.M.; Khan, M.S.I.; Anower, A.M. Isolation and antibiogram of Salmonella spp. from duck and pigeon in Dinajpur, Bangladesh. J. Adv. Vet. Anim. Res. 2016, 3, 386–391. [Google Scholar] [CrossRef]
- Kamruzzaman, M.; Islam, M.; Hossain, M.; Hassan, M.; Kabir, M.; Sabrin, M.; Khan, M. Isolation, Characterization and Antibiogram Study of Pasteurella multocida Isolated from Ducks of Kishoreganj District, Bangladesh. Int. J. Anim. Res. 2016, 1, 69–76. [Google Scholar]
- Sultana, S.; Islam, M.A.; Khatun, M.M.; Nasrin, S. Multidrug Resistant Bacteria in the Respiratory Tract of Apparently Healthy Quails. Microbes Health 2012, 1, 46–49. [Google Scholar] [CrossRef]
- Jahan, S.; Zihadi, M.A.H.; Nazir, K.N.H.; Islam, M.S.; Rahman, M.B.; Rahman, M. Molecular detection and antibiogram of Salmonella spp. from apparently healthy Japanese quails of three different quail farms in Mymensingh. J. Adv. Vet. Anim. Res. 2018, 5, 60–66. [Google Scholar] [CrossRef]
- Bhowmik, P.; Ahaduzzaman, M.; Hasan, R. A cross sectional anthropo-clinical study on antimicrobials prescription pattern in goat patients at Chittagong, Bangladesh. Bangladesh J. Vet. Med. 2017, 15, 119–126. [Google Scholar] [CrossRef][Green Version]
- Samad, M.; Haldar, P.; Dash, A.; Sultana, S.; Arfin, S.; Bari, M.; Sayeed, M. Cross-sectional survey on food animal diseases and pharmaceuticals prescribing pattern in Jhenaidah, Bangladesh. Res. J. Vet. Pract. 2020, 8, 4–10. [Google Scholar] [CrossRef]
- Johura, F.-T.; Parveen, R.; Islam, A.; Sadique, A.; Rahim, M.N.; Monira, S.; Khan, A.R.; Ahsan, S.; Ohnishi, M.; Watanabe, H. Occurrence of hybrid Escherichia coli strains carrying Shiga toxin and heat-stable toxin in livestock of Bangladesh. Front. Public Health 2017, 4, 287. [Google Scholar] [CrossRef][Green Version]
- Sohidullah, M.; Khan, M.S.R.; Islam, M.S.; Islam, M.M.; Rahman, S.; Begum, F. Isolation, molecular identification and antibiogram profiles of Escherichia coli and Salmonella spp. from diarrhoeic cattle reared in selected areas of Bangladesh. Asian J. Med. Biol. Res. 2016, 2, 587–595. [Google Scholar] [CrossRef][Green Version]
- Hoque, M.; Das, Z.; Rahman, A.; Haider, M.; Islam, M. Molecular characterization of Staphylococcus aureus strains in bovine mastitis milk in Bangladesh. Int. J. Vet. Sci. Med. 2018, 6, 53–60. [Google Scholar] [CrossRef]
- Sarker, H.; Samad, M. Udder-halve-wise comparative prevalence of clinical and sub-clinical mastitis in lactating goats with their bacterial pathogens and antibiotic sensitivity patterns in Bangladesh. Bangladesh J. Vet. Med. 2011, 9, 137–143. [Google Scholar] [CrossRef]
- Shourav, A.H.; Hasan, M.; Ahmed, S. Antibiotic susceptibility pattern of Listeria spp. isolated from cattle farm environment in Bangladesh. J. Agric. Food Res. 2020, 2, 100082. [Google Scholar] [CrossRef]
- Ferdous, J.; Bradshaw, A.; Islam, S.A.; Zamil, S.; Islam, A.; Ahad, A.; Fournie, G.; Anwer, M.S.; Hoque, M.A. Antimicrobial residues in chicken and fish, Chittagong, Bangladesh. EcoHealth 2019, 16, 429–440. [Google Scholar] [CrossRef]
- Bari, M.; Kober, A.; Hoque, M.; Debnath, G.; Chanda, G. Prevalence of antibiotic residues and associated risk factors in milk in Chittagong, Bangladesh. Adv. Anim. Vet. Sci. 2020, 8, 701–708. [Google Scholar] [CrossRef]
- Rahman, M.A.; Rahman, A.A.; Islam, M.A.; Alam, M.M. Multi–drug resistant Staphylococcus aureus isolated from milk, chicken meat, beef and egg in Bangladesh. Res. Agric. Livest. Fish. 2018, 5, 175–183. [Google Scholar] [CrossRef]
- Pondit, A.; Haque, Z.F.; Sabuj, A.A.M.; Khan, M.S.R.; Saha, S. Characterization of Staphylococcus aureus isolated from chicken and quail eggshell. J. Adv. Vet. Anim. Res. 2018, 5, 466. [Google Scholar] [CrossRef]
- Parvin, M.; Talukder, S.; Ali, M.; Chowdhury, E.H.; Rahman, M.; Islam, M. Antimicrobial resistance pattern of Escherichia coli isolated from frozen chicken meat in Bangladesh. Pathogens 2020, 9, 420. [Google Scholar] [CrossRef]
- Rahman, M.M.; Husna, A.; Elshabrawy, H.A.; Alam, J.; Runa, N.Y.; Badruzzaman, A.; Banu, N.A.; Al Mamun, M.; Paul, B.; Das, S. Isolation and molecular characterization of multidrug-resistant Escherichia coli from chicken meat. Sci. Rep. 2020, 10, 1–11. [Google Scholar] [CrossRef]
- Parvin, M.; Ali, M.; Talukder, S.; Nahar, A.; Chowdhury, E.H.; Rahman, M.; Islam, M. Prevalence and Multidrug Resistance Pattern of Methicillin Resistant S. aureus Isolated from Frozen Chicken Meat in Bangladesh. Microorganisms 2021, 9, 636. [Google Scholar] [CrossRef]
- Hossain, M.S.; Hossain, K.M.; Sarker, M.M.A.; Hamid, S.A. Prevalence and antibiotic susceptibility of Salmonella from chicken eggs in Naogaon district of Bangladesh. J. Adv. Microbiol. 2019, 2, 1–6. [Google Scholar] [CrossRef]
- Sultana, F.; Afroz, H.; Jahan, A.; Fakruddin, M.; Datta, S. Multi–antibiotic resistant bacteria in frozen food (ready to cook food) of animal origin sold in Dhaka, Bangladesh. Asian Pac. J. Trop. Biomed. 2014, 4, S268–S271. [Google Scholar] [CrossRef] [PubMed]
- Tanzin, T.; Nazir, K.N.H.; Zahan, M.N.; Parvej, M.S.; Zesmin, K.; Rahman, M.T. Antibiotic resistance profile of bacteria isolated from raw milk samples of cattle and buffaloes. J. Adv. Vet. Anim. Res. 2016, 3, 62–67. [Google Scholar] [CrossRef]
- Xu, J.; Sangthong, R.; McNeil, E.; Tang, R.; Chongsuvivatwong, V. Antibiotic use in chicken farms in northwestern China. Antimicrob. Resist. Infect. Control 2020, 9, 1–9. [Google Scholar] [CrossRef]
- Aidara-Kane, A.; Angulo, F.J.; Conly, J.M.; Minato, Y.; Silbergeld, E.K.; McEwen, S.A.; Collignon, P.J. World Health Organization (WHO) guidelines on use of medically important antimicrobials in food-producing animals. Antimicrob. Resist. Infect. Control 2018, 7, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Laxminarayan, R.; Duse, A.; Wattal, C.; Zaidi, A.K.; Wertheim, H.F.; Sumpradit, N.; Vlieghe, E.; Hara, G.L.; Gould, I.M.; Goossens, H. Antibiotic resistance—The need for global solutions. Lancet Infect. Dis. 2013, 13, 1057–1098. [Google Scholar] [CrossRef]
- WHO. Report of a Joint FAO/OIE/WHO Expert Consultation on Antimicrobial Use in Aquaculture and Antimicrobial Resistance. World Health Organization. Available online: http://www.fao.org/3/a-bq501e.pdf (accessed on 20 February 2021).
- Tiong, J.J.; Loo, J.S.; Mai, C.-W. Global antimicrobial stewardship: A closer look at the formidable implementation challenges. Front. Microbiol. 2016, 7, 1860. [Google Scholar] [CrossRef]
- Depaola, A.; Peeler, J.T.; Rodrick, G.E. Effect of oxytetracycline-medicated feed on antibiotic resistance of gram-negative bacteria in catfish ponds. Appl. Environ. Microbiol. 1995, 61, 2335–2340. [Google Scholar] [CrossRef]
- Nisha, A. Antibiotic residues—A global health hazard. Vet. World 2008, 1, 375. [Google Scholar] [CrossRef]
- Haider, N.; Khan, S.; Islam, A.; Osmani, M.; Rahman, M.; Epstein, J.; Daszak, P.; Zeidner, N. Efficiency of the clinical veterinary diagnostic practices and drug choices for infectious diseases in livestock in Bangladesh. Transbound. Emerg. Dis. 2017, 64, 1329–1333. [Google Scholar] [CrossRef]
| Study Author, Year | Study Description | Key Findings |
|---|---|---|
| Tasneem Imam et al., 2020 [27] | A cross-sectional study to collect information on antimicrobial usage in commercial broiler and layer farms. | One hundred percent of broiler and layer farms used antibiotics in the current production cycle. Moreover, 13% of the layer farmers used antibiotics for prophylactic purposes. Ciprofloxacin (37%) was mostly used, followed by amoxicillin (33%), tiamulin (32%), colistin (28%), doxycycline (26%), tylosin (17%), and oxytetracycline (15%); 18% of the broiler farmers used antibiotics for prophylactic purposes. Colistin, ciprofloxacin, tylosin, neomycin, amoxicillin, trimethoprim, sulfonamides, doxycycline, and tiamulin were used more frequently. |
| K. B. M. Saiful Islam et al., 2016 [17] | Surveyed 73 poultry farms from different regions of Bangladesh to explore the pattern of antibiotic usage. | One hundred percent of farms used at least one antibiotic in the last 12 months. |
| Emily K.Rousham et al., 2021 [20] | A cross-sectional survey to detect ESBL-EC carriage in adults from three communities with close human–poultry interactions; backyard poultry in rural households; small commercial broiler poultry farms; and urban food markets that sell live poultry with on-site slaughtering and processing. | Ninety-five percent of broiler farms used antibiotics, and 80% of them administered multiple antibiotics. Tetracycline (63%) mainly was administered, followed by ciprofloxacin (55%) and enrofloxacin (55%), erythromycin (38%), tylosin (38%), and colistin sulfate (15%). |
| Jannatul Ferdous et al., 2019 [28] | Surveyed 120 small–scale layer farms to collect data on antibiotic usage. | All farms administered antibiotics in the chicken production cycle. The most common antibiotics were ciprofloxacin (23%), followed by enrofloxacin (18%), amoxicillin (17%), oxytetracycline (11%), sulfa drugs (3%), and norfloxacin (2%); 73% of antibiotics are critically important for humans. |
| S.T. Tasmim et al., 2021 [5] | A qualitative survey of 70 farmers was conducted to assess poultry farmer’s knowledge and practices regarding antibiotics, antibiotic use, and antimicrobial resistance and to identify the factors. | Fifty-four percent of commercial poultry farmers used antibiotics from the first day of a chicken production cycle, 43% of farmers used antibiotics for preventive purposes, and 4% used antibiotics as a growth promoter. |
| Amira A. Roess et al., 2013 [29] | Semi-structured in-depth interviews with key informants (female household members, village doctors, pharmaceutical representatives, veterinarians, and government officials) and performed observations at animal health clinics. | Most of the farmers used antimicrobial drugs to treat their backyard animals. |
| Salequl Islam et al., 2020 [30] | A cross-sectional study to examine the colistin resistance mcr-1 to mcr-5 genes prevalence in bacterial isolates from chicken droppings. | Sixty-seven percent of the broiler farms and 38% of the layer farms used colistin in the chicken production cycle. |
| Shahana Ahmed et al., 2020 [31] | A study to examine the colistin resistance mcr-1 to mcr-5 genes prevalence in bacterial isolates from broiler chicken. | Sixty-five percent of broiler farms administered colistin in the chicken production cycle. |
| Study Author, Year | Study Description | Key Findings |
|---|---|---|
| Badrul Hasan et al., 2011 [34] | A total of 279 dead or sick broiler and layer chickens of different ages were tested for pathogenic E. coli strains and to determine the phenotypic expression of antimicrobial resistance against antibiotics. | More than 55% of E. coli isolates were resistant to at least one antibiotic, and 36.6% of the isolates showed resistance against multiple antibiotics. |
| Samina Ievy et al., 2020 [33] | A total of 99 samples from commercial layer farms were tested to determine the prevalence of avian pathogenic E. coli (APEC), the associated virulence genes and their antibiotic resistance profiles. | APEC-associated virulence genes showed 100% resistance against ampicillin and tetracycline, followed by chloramphenicol (97%), erythromycin (97%), enrofloxacin (56%), norfloxacin (50%), ciprofloxacin (50%), streptomycin (19%), colistin (11%), and gentamicin (8%). |
| Avijit Das et al., 2020 [38] | E. coli strains isolated from 30 broiler farms were examined to detect resistance against oxytetracycline and ciprofloxacin. | E. coli showed resistance against oxytetracycline (100%) and ciprofloxacin (78%). |
| Badrul Hasan et al., 2011 [34] | A total of 279 dead or sick broiler and layer chicken of different ages were tested for pathogenic E. coli strains, and to determine the phenotypic expression of antimicrobial resistance against antibiotics. | More than 55% of E. coli isolates were resistant to at least one antibiotic, and 36.6% of the isolates showed resistance against multiple antibiotics. |
| Emily K.Rousham et al., 2021 [20] | A cross-sectional survey to detect ESBL-EC carriage in adults from three communities with close human–poultry interactions; backyard poultry in rural households; small commercial broiler poultry farms; and urban food markets that sell live poultry with on-site slaughtering and processing. | A total of 71% of the ESBL-producing E. coli isolates showed resistance against fluoroquinolones and cefepime, followed by sulfonamides (65%) and aminoglycosides (31%). |
| Md. Samun Sarker et al., 2019 [39] | A study to detect E. coli in apparently healthy broiler chicken and detect antibiotic-resistant genes. | E. coli was detected in 62% of broiler chicken. E. coli isolates were 100% resistant to ampicillin and tetracycline followed by sulfamethoxazole-trimethoprim (95%) and nalidixic acid (92%). |
| Badrul Alam et al., 2020 [40] | A total of 128 cloacal swabs from broiler chicken, 64 poultry feed, 64 drinking water, 64 attendants’ hand rinsed water, and 32 whole broiler carcasses were tested to detect Campylobacter spp. All Campylobacter spp. strains were tested against eight antimicrobial agents. | Twenty-six percent of samples tested positive for Campylobacter spp. A total of 93 isolates of Campylobacter were detected. Among them, 22 isolates of Campylobacter jejuni showed resistance against amoxicillin, streptomycin, tetracycline, ciprofloxacin, amoxicillin, norfloxacin, and azithromycin. |
| Sucharit Basu Neogi et al., 2020 [41] | A total of 224 samples from 7 hatcheries, 9 broiler farms and 4 live bird markets were tested to examine the occurrence and MDR patterns of Campylobacter spp. | Thirty-two percent of samples were tested positive for Campylobacter spp.; 49% of strains of C. jejuni showed resistance to three or more antimicrobials, including tetracycline, amoxicillin, streptomycin, fluoroquinolones, and macrolides. |
| Muha. Ajijur Rahman Al Azad et al., 2019 [42] | A study to detect E. coli strains from live broiler chickens and to determine their susceptibility and resistant patterns to selected antimicrobial agents. | Detected 100% prevalence of E. coli in cloacal swabs. All E. coli isolates were found resistant against ampicillin, tetracycline, streptomycin, ciprofloxacin, erythromycin, and trimethoprim–sulfamethoxazole. Colistin sulfate and gentamicin showed the highest susceptibility to antibiotics. |
| Shanzida Binte Alam et al., 2019 [43] | A total of 100 samples from broiler chickens were tested to detect multi drug resistant Salmonella along with the resistance pattern. | Salmonella isolates showed the highest resistance to tetracycline (97%), followed by chloramphenicol (94%), ampicillin (83%), and streptomycin (77%). |
| Salequl Islam et al., 2020 [30] | A cross-sectional study to examine the colistin resistance mcr-1 to mcr-5 genes prevalence in bacterial isolates from chicken droppings. | A total of 64 isolates from commercial chicken (broiler and layer) and 28 isolates from native chicken showed colistin-resistance. |
| Shahana Ahmed et al., 2020 [31] | A study to examine the colistin resistance mcr-1 to mcr-5 genes prevalence in bacterial isolates from broiler chicken. | Twenty-five percent of E. coli isolates carried colistin-resistant mcr-1 genes. E. coli isolates also showed resistance against Tetracycline, and Beta-Lactam antibiotics. |
| Study Author, Year | Study Description | Key Findings |
|---|---|---|
| Sheikh Aftab Uddin et al., 2006 [49] | A cross-sectional study to know the pattern of antibiotics and other chemical use in shrimp hatcheries. | Eighty percent of shrimp hatcheries used antibiotics. Chloramphenicol, erythromycin, oxytetracycline, and prefuran were commonly used antibiotics. |
| Md. Abu Kawsar et al., 2019 [46] | A study to assess the aqua drugs and antibiotics used in aquaculture. | Fifty-two percent of farmers used erythromycin, 18% used ciprofloxacin and 10% used oxytetracycline. |
| A.K. Jilani Chowdhury et al., 2012 [48] | A cross-sectional study to find out different chemicals used in fish hatcheries, nurseries, and culture farms. | Fourty-seven percent of fish farmers used oxytetracycline to treat diseases. |
| Study Author, Year | Study Description | Key Findings |
|---|---|---|
| Farzana Ehetasum Hossain et al., 2018 [50] | A study to investigate the presence of bacteria in fish samples and to analyze multidrug resistance pattern of the bacteria. | Most of the bacterial isolates in drug used ponds were 100% resistant against tetracyclines, penicillins, cephalosporins, aminoglycosides, and macrolides; 80% resistance against sulfanilamide and fluoroquinolones. |
| Foysal MJ et al., 2011 [51] | A study to isolate and identify Pseudomonas fluorescens from bacterial hemorrhagic septicemia infected carp and catfish to find out their antibiotic sensitivity pattern. | Most of the Pseudomonas fluorescens isolates (80%) were found resistant to chloramphenicol, followed by sulfamethoxazole (70%), erythromycin (60%), and cephradine (30%). |
| Tasnia Ahmed et al., 2013 [52] | Tested export quality shrimp samples to detect Listeria spp., Staphylococcus aureus, and E. coli and to determine the antibiotic resistance. | Listeria spp. was resistant against penicillin G and ampicillin, whereas S. aureus showed resistance against trimethoprim, erythromycin, sulfamethoxazole, and E. coli showed resistance against erythromycin and polymyxin B. |
| Abu Baker Siddique et al., 2021 [53] | A total of 216 samples from water, sediment, Oreochromis niloticus (tilapia fish), Labeo rohita (rui fish), and Penaeus monodon (shrimp) were tested to detect Vibrio parahaemolyticus and to analyze multidrug resistance pattern of the bacteria. | Sixty percent of samples from the aquaculture system tested positive for V. parahaemolyticus. Most of the V. parahaemolyticus isolates were found resistant to ampicillin and amoxicillin (94%), followed by cefotaxime (29%), and ceftriaxone (18%). |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chowdhury, S.; Ghosh, S.; Aleem, M.A.; Parveen, S.; Islam, M.A.; Rashid, M.M.; Akhtar, Z.; Chowdhury, F. Antibiotic Usage and Resistance in Food Animal Production: What Have We Learned from Bangladesh? Antibiotics 2021, 10, 1032. https://doi.org/10.3390/antibiotics10091032
Chowdhury S, Ghosh S, Aleem MA, Parveen S, Islam MA, Rashid MM, Akhtar Z, Chowdhury F. Antibiotic Usage and Resistance in Food Animal Production: What Have We Learned from Bangladesh? Antibiotics. 2021; 10(9):1032. https://doi.org/10.3390/antibiotics10091032
Chicago/Turabian StyleChowdhury, Sukanta, Sumon Ghosh, Mohammad Abdul Aleem, Shahana Parveen, Md. Ariful Islam, Md. Mahbubur Rashid, Zubair Akhtar, and Fahmida Chowdhury. 2021. "Antibiotic Usage and Resistance in Food Animal Production: What Have We Learned from Bangladesh?" Antibiotics 10, no. 9: 1032. https://doi.org/10.3390/antibiotics10091032
APA StyleChowdhury, S., Ghosh, S., Aleem, M. A., Parveen, S., Islam, M. A., Rashid, M. M., Akhtar, Z., & Chowdhury, F. (2021). Antibiotic Usage and Resistance in Food Animal Production: What Have We Learned from Bangladesh? Antibiotics, 10(9), 1032. https://doi.org/10.3390/antibiotics10091032







