Determination of Susceptibility Breakpoint for Cefquinome against Streptococcus suis in Pigs
Abstract
1. Introduction
2. Results
2.1. MIC Distribution of CEF against S. suis
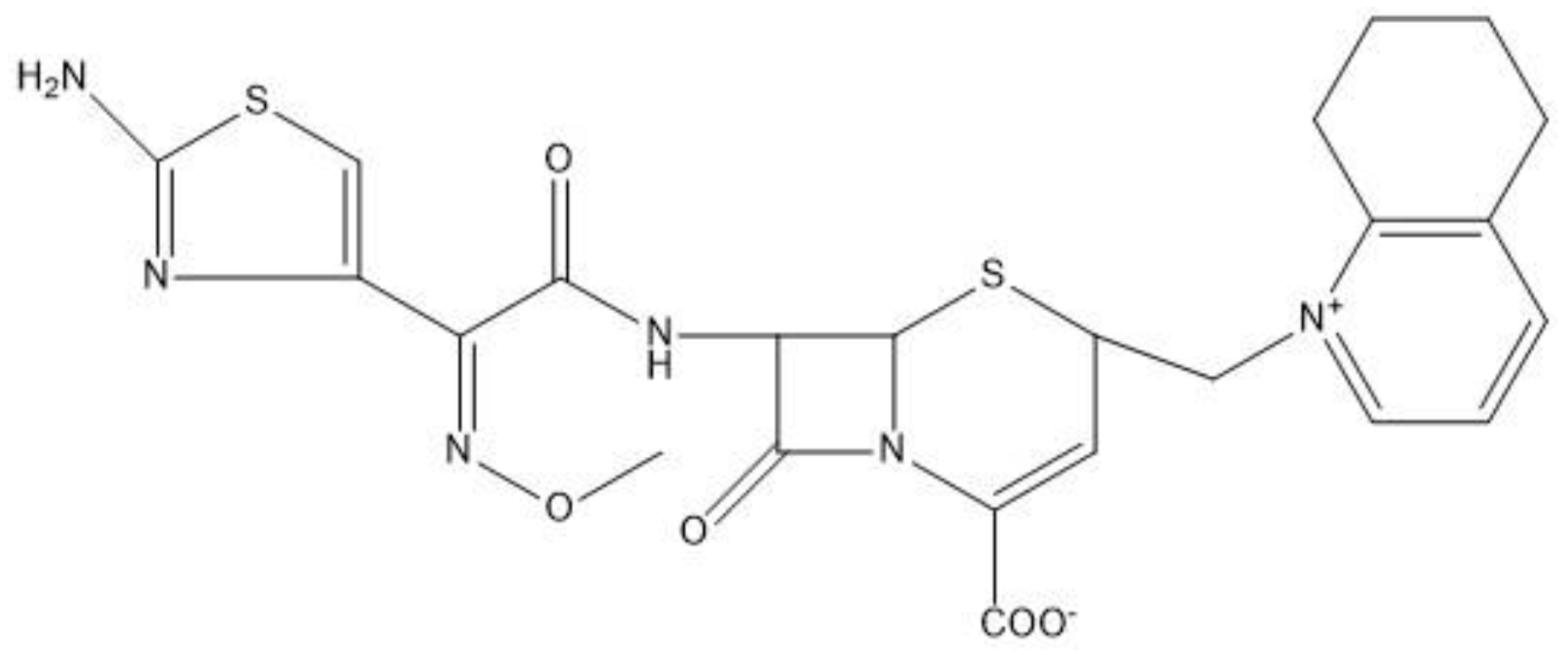
2.2. MIC, MBC, MPC and PAE of Cefquinome against SS0061
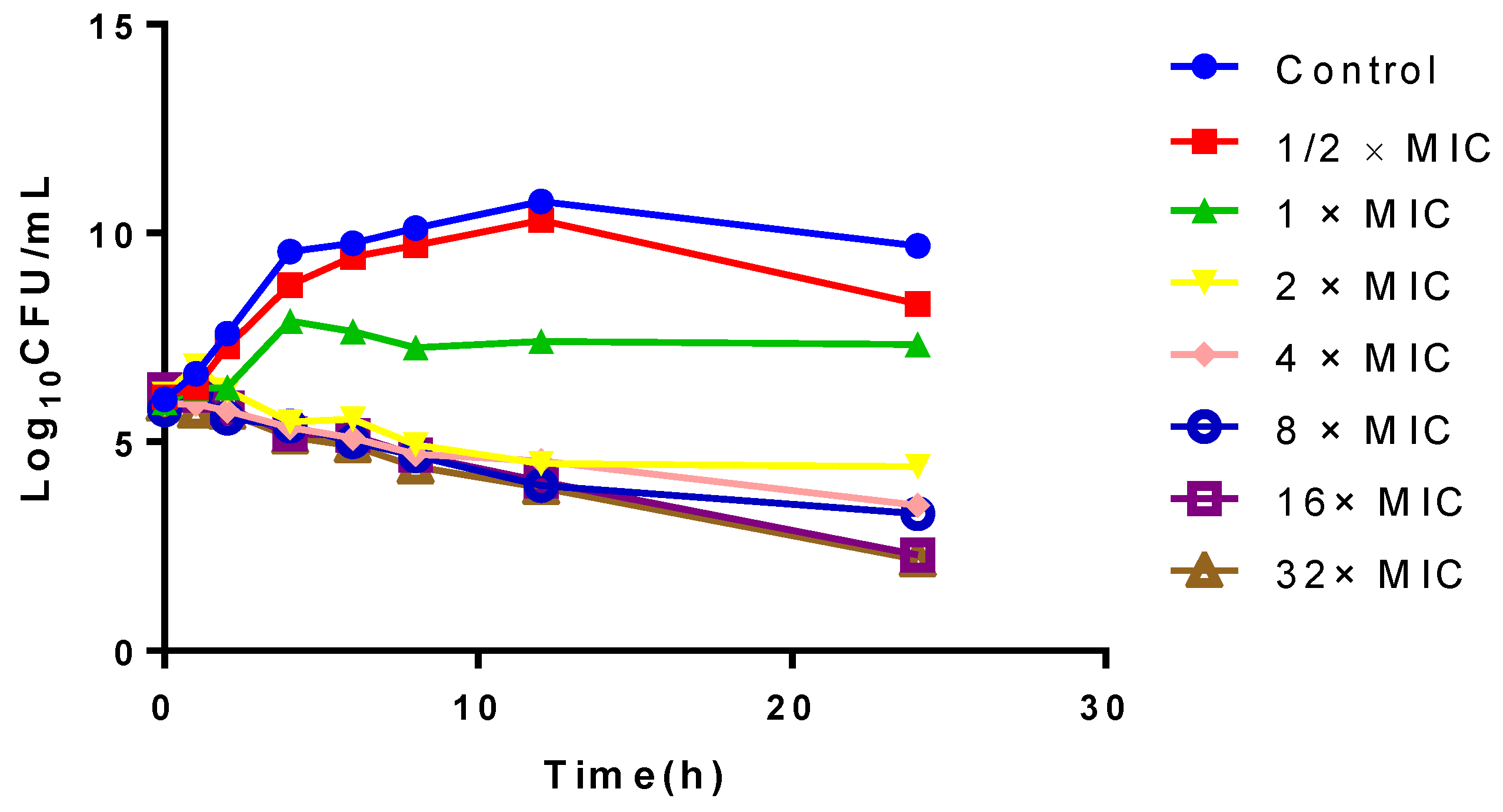
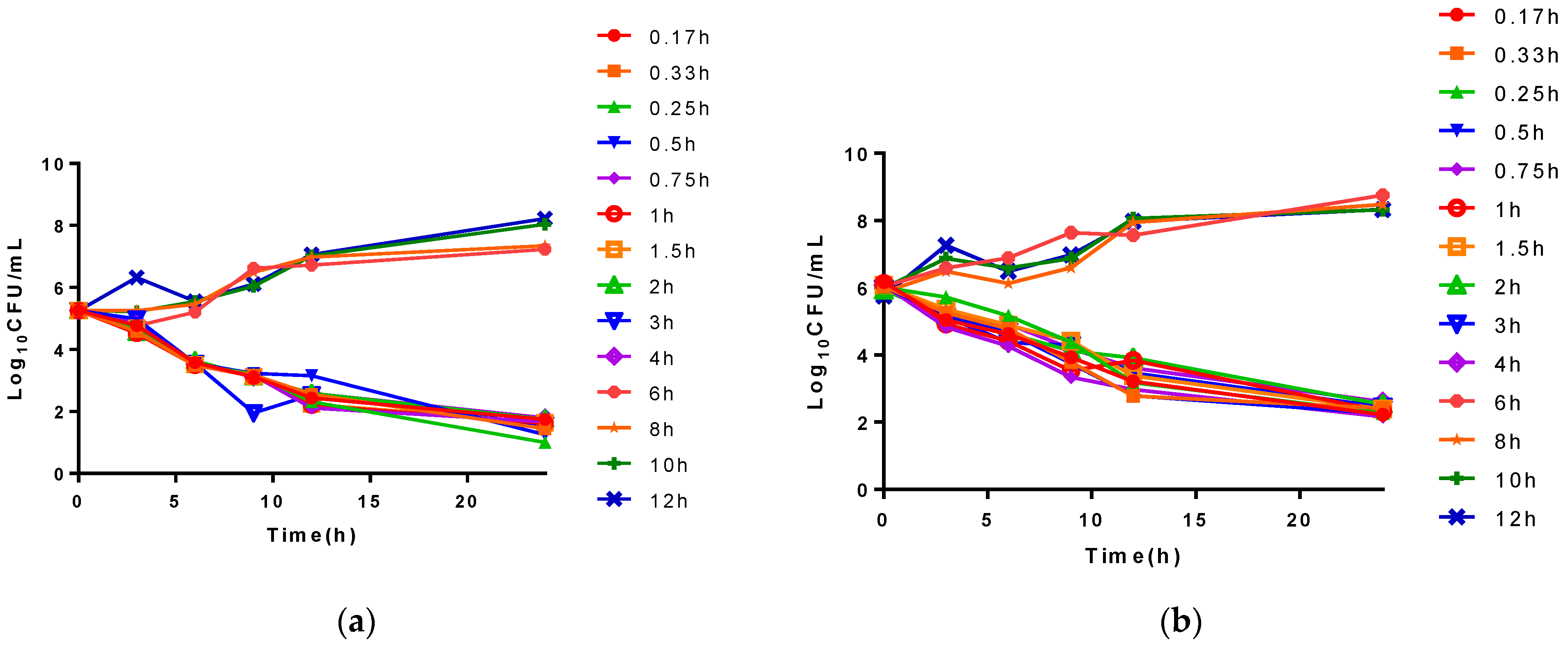
2.3. In Vitro and Ex Vivo Time-Killing Curves
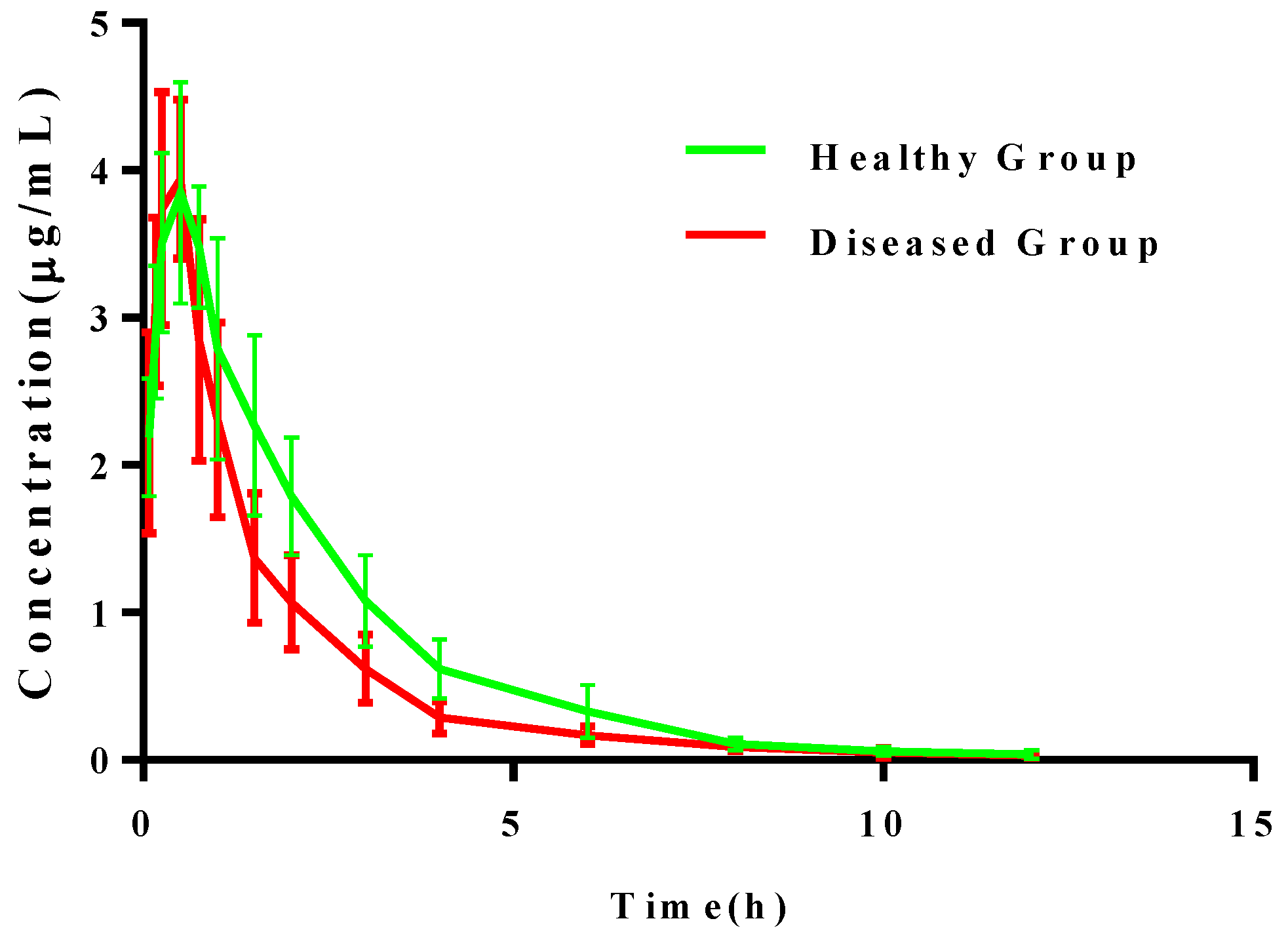
2.4. Pharmacokinetic Analysis of Cefquinome in Plasma
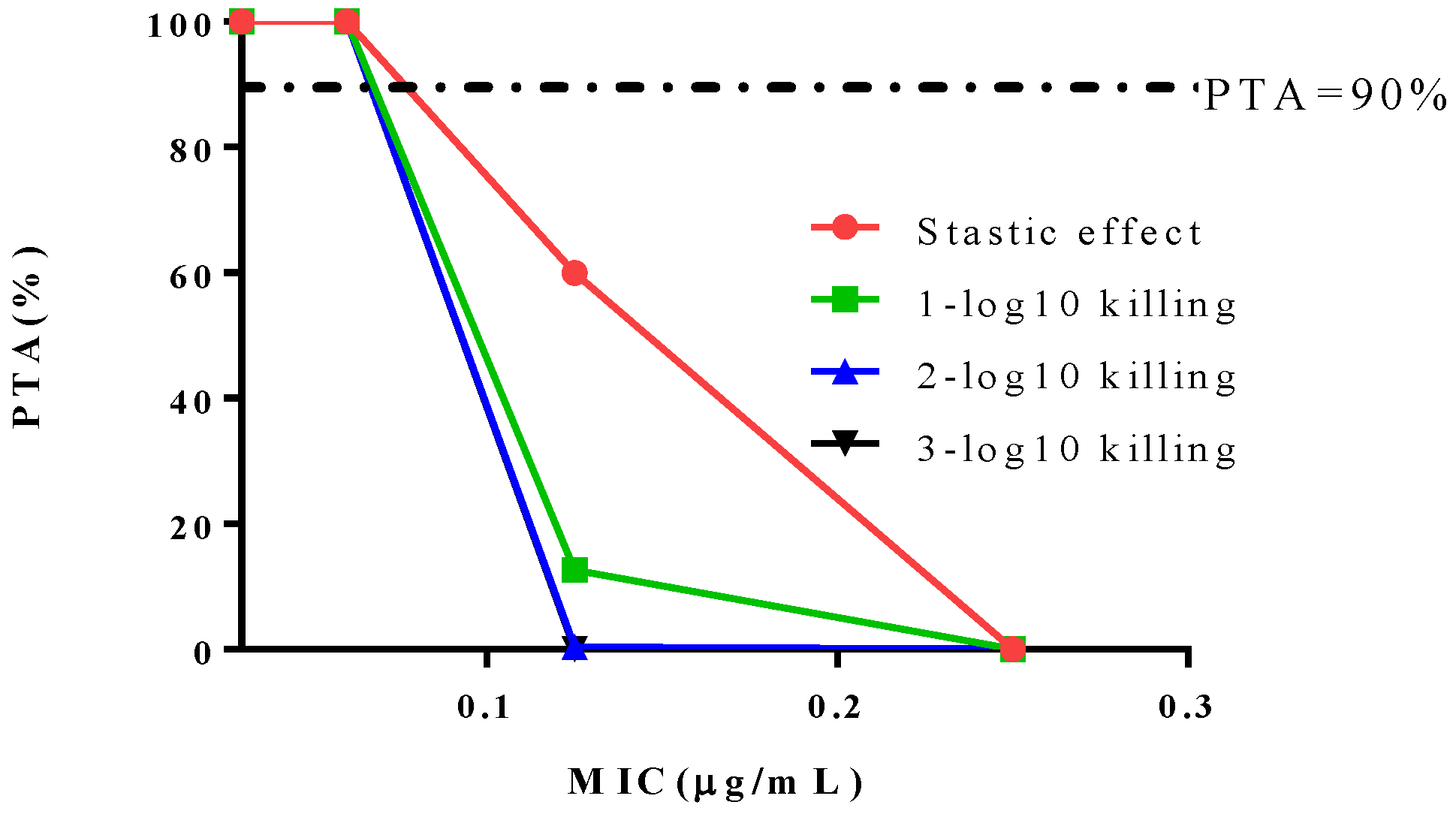
2.5. PK/PD Integration Modeling and Dose Estimation
2.6. Determination of COPD
2.7. Clinical Outcomes and Determination of COCL
2.8. Development of Susceptibility Breakpoints
3. Discussion
4. Materials and Methods
4.1. Determination of the Epidemiologic Cutoff
4.2. Pharmacodynamics of Cefquinome against SS0061
4.2.1. MIC and MBC Determination of SS0061 In Vitro and Ex Vivo
4.2.2. In Vitro and Ex Vivo Time-Killing Curve of SS0061
4.2.3. Determination of the MPC of Cefquinome against SS0061
4.2.4. In Vitro PAE
4.3. Pharmacokinetics of Cefquinome in the Plasma of Pigs
4.3.1. Animals and Dosing
4.3.2. Sample Collection
4.3.3. Sample Analysis
4.4. Pharmacokinetic/Pharmacodynamic Integration Model
4.5. Determination of COPD by Monte Carlo Simulation
4.6. Dose Estimations
4.7. Clinical Effectiveness of Cefquinome on Pigs Infected with Different S. suis Isolates
4.7.1. Animal Groups and Establishment of Infected Model
4.7.2. Statistical Analysis of Clinical Outcome and Clinical Cutoff
4.8. Development of Susceptibility Breakpoints
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Chengappa, M.M.; Pace, L.W.; Williams, J.A.; Herren, C.H.; Ascher, S.E. Efficacy of tiamulin against experimentally induced Streptococcus suis type-2 infection in swine. J. Am. Veter. Med. Assoc. 1990, 197, 1467–1470. [Google Scholar]
- Staats, J.; Feder, I.; Okwumabua, O.; Chengappa, M. Streptococcus Suis: Past and Present. Veter. Res. Commun. 1997, 21, 381–407. [Google Scholar] [CrossRef] [PubMed]
- Chin, N.-X.; Gu, J.-W.; Fang, W.; Neu, H.C. In vitro activity of cefquinome, a new cephalosporin, compared with other cephalosporin antibiotics. Diagn. Microbiol. Infect. Dis. 1992, 15, 331–337. [Google Scholar] [CrossRef]
- Limbert, M.; Isert, D.; Klesel, N.; Markus, A.; Seeger, K.; Seibert, G.; Schrinner, E. Antibacterial activities in vitro and in vivo and pharmacokinetics of cefquinome (HR 111V), a new broad-spectrum cephalosporin. Antimicrob. Agents Chemother. 1991, 35, 14–19. [Google Scholar] [CrossRef]
- CVMP. Cefquinome Summary Report. Emea/Mrl/005/95; European Agency for the Evaluation of Medicinal Products: London, UK, 1995.
- Turnidge, J.; Paterson, D.L. Setting and Revising Antibacterial Susceptibility Breakpoints. Clin. Microbiol. Rev. 2007, 20, 391–408. [Google Scholar] [CrossRef] [PubMed]
- Kahlmeter, G.; Brown, D.; Goldstein, F.; MacGowan, A.; Mouton, J.; Odenholt, I.; Rodloff, A.; Soussy, C.-J.; Steinbakk, M.; Soriano, F.; et al. European Committee on Antimicrobial Susceptibility Testing (EUCAST) Technical Notes on antimicrobial susceptibility testing. Clin. Microbiol. Infect. 2006, 12, 501–503. [Google Scholar] [CrossRef] [PubMed]
- Drusano, G.L.; D’Argenio, D.Z.; Preston, S.L.; Barone, C.; Symonds, W.; LaFon, S.; Rogers, M.; Prince, W.; Bye, A.; Bilello, J.A. Use of Drug Effect Interaction Modeling with Monte Carlo Simulation to Examine the Impact of Dosing Interval on the Projected Antiviral Activity of the Combination of Abacavir and Amprenavir. Antimicrob. Agents Chemother. 2000, 44, 1655–1659. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, E.I.; Friberg, L.E. Pharmacokinetic-Pharmacodynamic Modeling of Antibacterial Drugs. Pharmacol. Rev. 2013, 65, 1053–1090. [Google Scholar] [CrossRef] [PubMed]
- Toutain, P.-L.; Bousquet-Melou, A.; Damborg, P.; Ferran, A.A.; Mevius, D.; Pelligand, L.; Veldman, K.T.; Lees, P. En Route towards European Clinical Breakpoints for Veterinary Antimicrobial Susceptibility Testing: A Position Paper Explaining the VetCAST Approach. Front. Microbiol. 2017, 8, 2344. [Google Scholar] [CrossRef]
- Mi, K.; Sun, D.; Li, M.; Hao, H.; Zhou, K.; Liu, Z.; Yuan, Z.; Huang, L. Evidence for Establishing the Clinical Breakpoint of Cefquinome against Haemophilus Parasuis in China. Pathogens 2021, 10, 105. [Google Scholar] [CrossRef] [PubMed]
- Hughes, J.M.; Wilson, M.E.; Wertheim, H.F.; Nghia, H.D.T.; Taylor, W.; Schultsz, C. Streptococcus suis:An Emerging Human Pathogen. Clin. Infect. Dis. 2009, 48, 617–625. [Google Scholar] [CrossRef]
- Pfaller, M.A.; Espinel-Ingroff, A.; Canton, E.; Castanheira, M.; Cuenca-Estrella, M.; Diekema, D.; Fothergill, A.; Fuller, J.; Ghannoum, M.; Jones, R.N.; et al. Wild-Type MIC Distributions and Epidemiological Cutoff Values for Amphotericin B, Flucytosine, and Itraconazole and Candida spp. as Determined by CLSI Broth Microdilution. J. Clin. Microbiol. 2012, 50, 2040–2046. [Google Scholar] [CrossRef]
- Turnidge, J.; Kahlmeter, G.; Kronvall, G. Statistical characterisation of bacterial wild-type MIC value distributions and the determination of epidemiological cut-off values. Clin. Microbiol. Infect. 2006, 12, 418–425. [Google Scholar] [CrossRef]
- Ambrose, P.G.; Grasela, D.M. The Use of Monte Carlo Simulation to Examine Pharmacodynamic Variance of Drugs: Fluoroquinolone Pharmacodynamics against Streptococcus Pneumoniae. Diagn. Microbiol. Infect. Dis. 2000, 38, 151–157. [Google Scholar] [CrossRef]
- Lei, Z.; Liu, Q.; Qi, Y.; Yang, B.; Khaliq, H.; Xiong, J.; Moku, G.K.; Ahmed, S.; Li, K.; Zhang, H.; et al. Optimal Regimens and Cutoff Evaluation of Tildipirosin Against Pasteurella multocida. Front. Pharmacol. 2018, 9, 765. [Google Scholar] [CrossRef]
- Xiao, X.; Sun, J.; Chen, Y.; Huang, R.-J.; Huang, T.; Qiao, G.G.; Zhou, Y.-F.; Liu, Y.-H. In vitro dynamic pharmacokinetic/pharmacodynamic (PK/PD) modeling and PK/PD cutoff of cefquinome against Haemophilus parasuis. BMC Veter. Res. 2015, 11, 33. [Google Scholar] [CrossRef] [PubMed]
- Velkov, T.; Bergen, P.J.; Lora-Tamayo, J.; Landersdorfer, C.; Li, J. PK/PD models in antibacterial development. Curr. Opin. Microbiol. 2013, 16, 573–579. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.-H.; Birhanu, B.T.; Lee, E.-B.; Lee, S.-J.; Boby, N.; Park, Y.-S.; Park, S.-C. Pharmacokinetic and pharmacodynamic integration for optimal dosage of cefquinome against Streptococcus equi subsp. equi in foals. Vet. Res. 2020, 51, 131. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Wu, X.; Huang, Z.; Zhang, N.; Wu, Y.; Cai, Q.; Shen, X.; Ding, H. Pharmacokinetic/pharmacodynamic assessment of cefquinome against Actinobacillus Pleuropneumoniae in a piglet tissue cage infection model. Veter. Microbiol. 2018, 219, 100–106. [Google Scholar] [CrossRef]
- Ahmad, I.; Hao, H.; Huang, L.; Sanders, P.; Wang, X.; Chen, D.; Tao, Y.; Xie, S.; Xiuhua, K.; Li, J.; et al. Integration of PK/PD for dose optimization of Cefquinome against Staphylococcus aureus causing septicemia in cattle. Front. Microbiol. 2015, 6, 588. [Google Scholar] [CrossRef]
- Zhou, Y.-F.; Bu, M.-X.; Liu, P.; Sun, J.; Liu, Y.-H.; Liao, X.-P. Epidemiological and PK/PD cutoff values determination and PK/PD-based dose assessment of gamithromycin against Haemophilus parasuis in piglets. BMC Veter. Res. 2020, 16, 81. [Google Scholar] [CrossRef] [PubMed]
- Bottner, A.; de Jong, A.; Schmid, P.; Schuller, S.; Traeder, W.; Weiskopf, S. Determination of Breakpoints for Veterinary Antimicrobial Substances for Resistance Assessment of Veterinary Pathogens; Berliner und Munchener Tierarztliche Wochenschrift: Berlin, Germany, 2000; Volume 113, pp. 344–347. [Google Scholar]
- Moore, C.L.; Lu, M.; Cheema, F.; Osaki-Kiyan, P.; Perri, M.B.; Donabedian, S.; Haque, N.Z.; Zervos, M.J. Prediction of Failure in Vancomycin-Treated Methicillin-Resistant Staphylococcus aureus Bloodstream Infection: A Clinically Useful Risk Stratification Tool. Antimicrob. Agents Chemother. 2011, 55, 4581–4588. [Google Scholar] [CrossRef]
- CLSI. Development of in Vitro Susceptibility. In Testing Criteria and Quality Control Parameters for Veterinary Antimicrobial Agents; Approved Guideline, 3rd ed.; CLSI: Wayne, PA, USA, 2009. [Google Scholar]
- Zhang, P.; Hao, H.; Li, J.; Ahmad, I.; Cheng, G.; Chen, D.; Tao, Y.; Huang, L.; Wang, Y.; Dai, M.; et al. The Epidemiologic and Pharmacodynamic Cutoff Values of Tilmicosin against Haemophilus parasuis. Front. Microbiol. 2016, 7, 385. [Google Scholar] [CrossRef] [PubMed]
- Rottbøll, L.A.H.; Friis, C. Penetration of antimicrobials to pulmonary epithelial lining fluid and muscle and impact of drug physicochemical properties determined by microdialysis. J. Pharmacol. Toxicol. Methods 2016, 78, 58–65. [Google Scholar] [CrossRef] [PubMed]
- Turnidge, J.D.; Martinez, M.N. Proposed method for estimating clinical cut-off (CO CL) values: An attempt to address challenges encountered when setting clinical breakpoints for veterinary antimicrobial agents. Veter. J. 2017, 228, 33–37. [Google Scholar] [CrossRef]
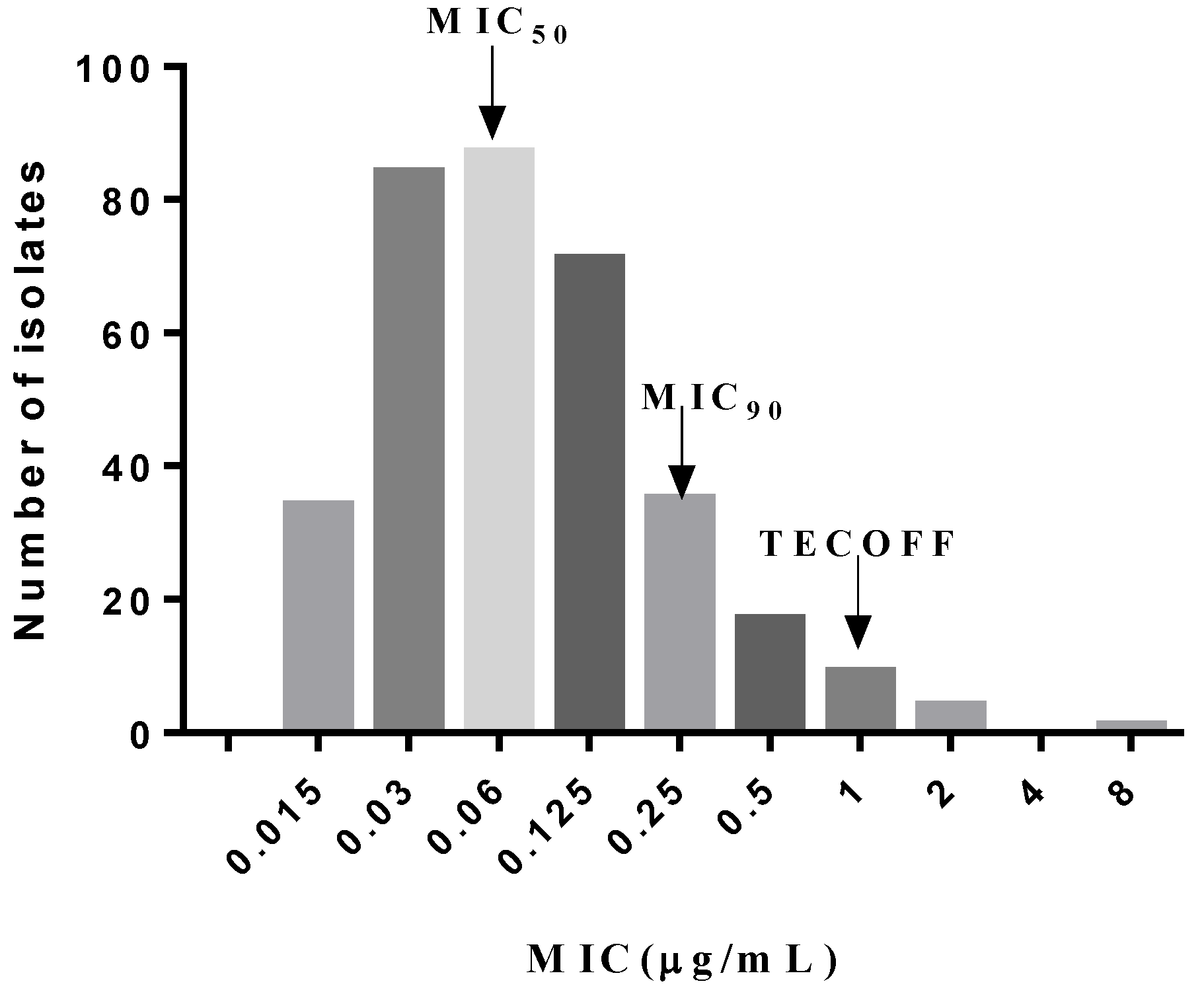

| Subset Fitted | MIC (μg/mL) | True | Estimate | Diff. | Probabilities |
|---|---|---|---|---|---|
| 97.5% Subset ECOFF | 0.25 | 311 | 332 | 21 | 90.9% |
| 99% Subset ECOFF | 0.5 | 328 | 340 | 12 | 95.9% |
| 99.9% Subset ECOFF | 1 | 337 | 340 | 3 | 98.5% |
| Concentrations | PAE (h) | |
|---|---|---|
| Expose 1 h | Expose 2 h | |
| 1 × MIC | 0.12 | 0.68 |
| 2 × MIC | 0.62 | 0.74 |
| 4 × MIC | 1.04 | 1.24 |
| Parameters | Units | Plasma | |
|---|---|---|---|
| Healthy (n = 8) | Infected (n = 8) | ||
| α | 1/h | 4.73 ± 0.79 | 4.54 ± 0.94 |
| β | 1/h | 0.31 ± 0.17 | 0.34 ± 0.16 |
| T1/2α | h | 0.15 ± 0.03 | 0.16 ± 0.03 |
| T1/2β | h | 2.24 ± 0.23 | 2.33 ± 0. 21 |
| Tmax | h | 0.45 ± 0.02 | 0.42 ± 0.03 |
| AUC | h·μg/mL | 9.77 ± 0.63 | 9.86 ± 0.78 |
| Cmax | μg/mL | 3.93 ± 0.11 | 3.92 ± 0.13 |
| CL/F | mL/kg/h | 204.51 ± 19.50 | 202.77 ± 17.03 |
| Vd/F | L/kg | 0.11 ± 0.06 | 0.10 ± 0.02 |
| Parameters | Units | Healthy | Infected |
|---|---|---|---|
| Imax | Log CFU/mL | 6.53 ± 0.13 | 6.00 ± 0.25 |
| E0 | Log CFU/mL | 2.89 ± 0.19 | 2.92 ± 0.47 |
| EC50 | h | 79.14 ± 2.44 | 46.38 ± 4.48 |
| N | - | 7.54 ± 0.61 | 24.81 ± 10.12 |
| Static effect | h | 76.73 ± 1.84 | 46.00 ± 4.53 |
| 1-log10 killing | h | 83.32 ± 1.84 | 47.59 ± 3.95 |
| 2-log10 killing | h | 91.54 ± 1.96 | 49.66 ± 3.34 |
| 3-log10 killing | h | 106.44 ± 3.28 | - |
| Groups | MIC (μg/mL) | Mortality Rate (%) | Cure Rate (%) | AUCsucc | AUCtotal | CAR | %Success ≤ MIC | MaxDiff |
|---|---|---|---|---|---|---|---|---|
| SSZD01 | 0.015 | 0 | 100 | 0.05 | 0.05 | 1.00 | 100.00 | 25.00 |
| SS1496 | 0.06 | 0 | 100 | 0.32 | 0.32 | 1.00 | 100.00 | 33.30 |
| SS0061 | 0.25 | 17 | 83 | 1.36 | 1.46 | 0.93 | 83.33 | 25.03 |
| SS14130 | 1 | 33 | 67 | 4.74 | 5.96 | 0.80 | 66.67 | 16.67 |
| SS2481 | 2 | 50 | 50 | 8.24 | 11.96 | 0.69 | 50.00 | 0.00 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mi, K.; Li, M.; Sun, L.; Hou, Y.; Zhou, K.; Hao, H.; Pan, Y.; Liu, Z.; Xie, C.; Huang, L. Determination of Susceptibility Breakpoint for Cefquinome against Streptococcus suis in Pigs. Antibiotics 2021, 10, 958. https://doi.org/10.3390/antibiotics10080958
Mi K, Li M, Sun L, Hou Y, Zhou K, Hao H, Pan Y, Liu Z, Xie C, Huang L. Determination of Susceptibility Breakpoint for Cefquinome against Streptococcus suis in Pigs. Antibiotics. 2021; 10(8):958. https://doi.org/10.3390/antibiotics10080958
Chicago/Turabian StyleMi, Kun, Mei Li, Lei Sun, Yixuan Hou, Kaixiang Zhou, Haihong Hao, Yuanhu Pan, Zhenli Liu, Changqing Xie, and Lingli Huang. 2021. "Determination of Susceptibility Breakpoint for Cefquinome against Streptococcus suis in Pigs" Antibiotics 10, no. 8: 958. https://doi.org/10.3390/antibiotics10080958
APA StyleMi, K., Li, M., Sun, L., Hou, Y., Zhou, K., Hao, H., Pan, Y., Liu, Z., Xie, C., & Huang, L. (2021). Determination of Susceptibility Breakpoint for Cefquinome against Streptococcus suis in Pigs. Antibiotics, 10(8), 958. https://doi.org/10.3390/antibiotics10080958







