Occurrence of Rare Pathogens at the Site of Periprosthetic Hip and Knee Joint Infections: A Retrospective, Single-Center Study
Abstract
:1. Introduction
2. Results
3. Discussion
4. Materials and Methods
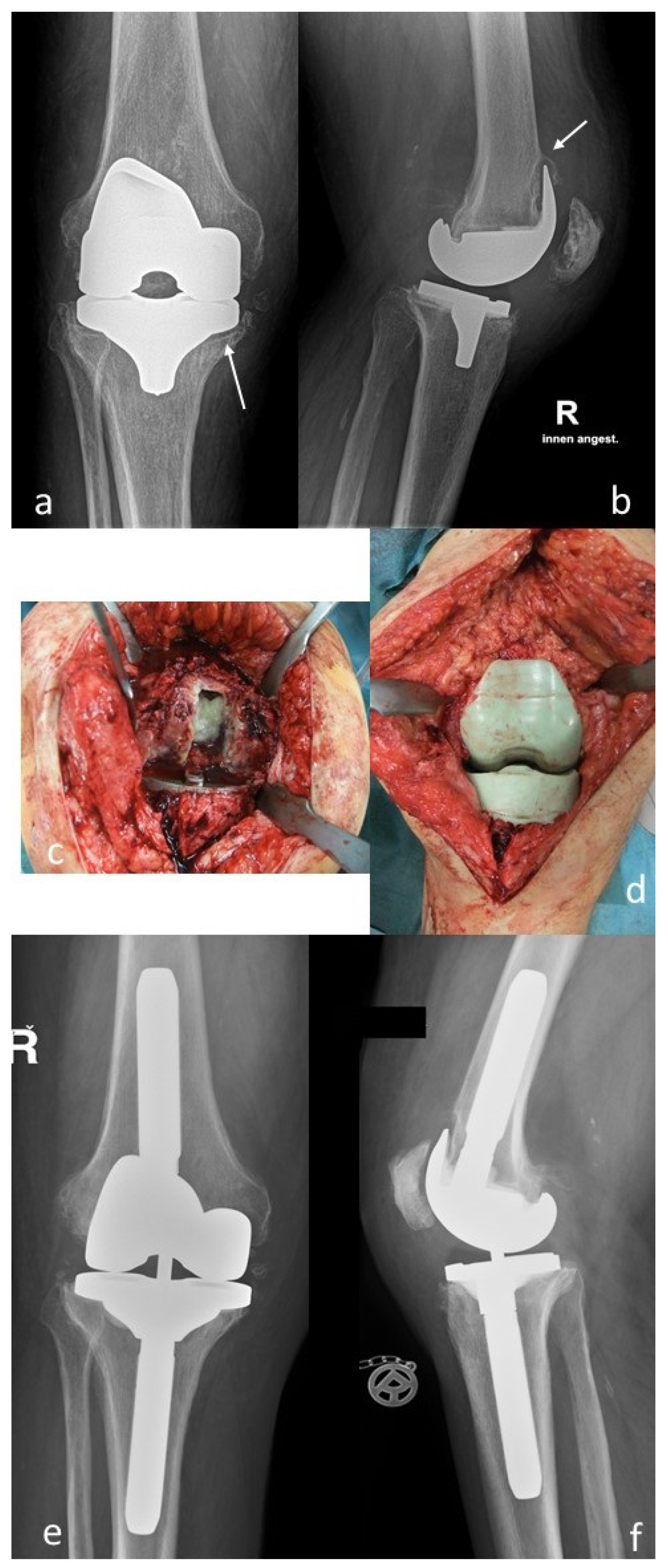
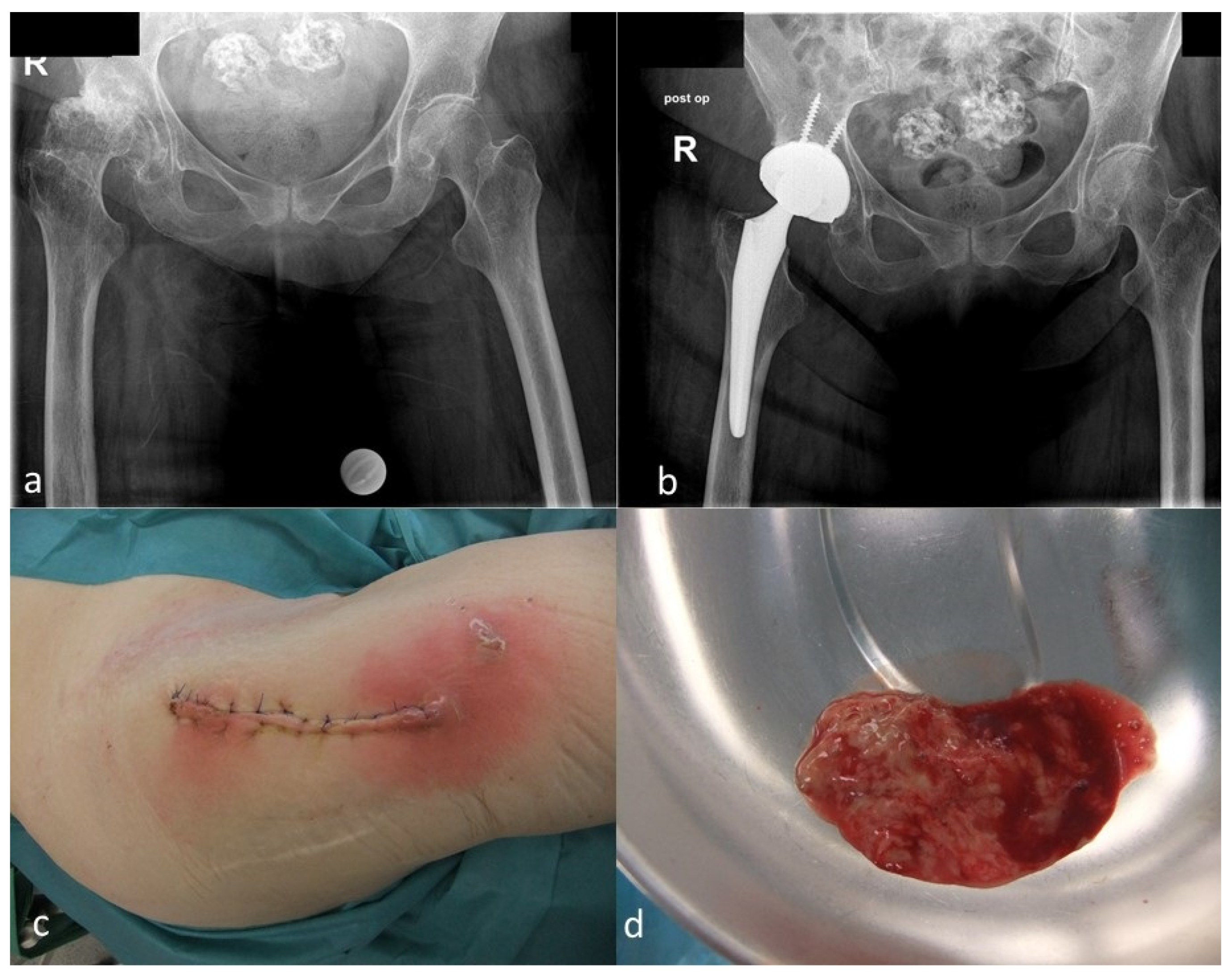
4.1. Surgical Management
4.2. Microbiological and Histopathological Diagnostic Techniques
4.3. Definition of Rare Organisms
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tsai, Y.; Chang, C.-H.; Lin, Y.-C.; Lee, S.-H.; Hsieh, P.-H.; Chang, Y. Different microbiological profiles between hip and knee prosthetic joint infections. J. Orthop. Surg. 2019, 27, 1–8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Parvizi, J. Orthopaedic infections: No one is denying anymore that we have a problem! Knee Surg. Relat. Res. 2019, 31, 17. [Google Scholar] [CrossRef] [PubMed]
- Salgado, C.D.; Dash, S.; Cantey, J.R.; Marculescu, C.E. Higher risk of failure of methicillin-resistant Staphylococcus aureus prosthetic joint infections. Clin. Orthop. Relat. Res. 2007, 461, 48–53. [Google Scholar] [CrossRef] [PubMed]
- Mortazavi, S.M.; Vegari, D.; Ho, A.; Zmistowski, B.; Parvizi, J. Two-stage exchange arthroplasty for infected total knee arthroplasty: Predictors of failure. Clin. Orthop. Relat. Res. 2011, 469, 3049–3054. [Google Scholar] [CrossRef] [Green Version]
- Drago, L.; De Vecchi, E.; Bortolin, M.; Zagra, L.; Romano, C.L.; Cappelletti, L. Epidemiology and antibiotic resistance of late prosthetic knee and hip infections. J. Arthroplast. 2017, 32, 2496–2500. [Google Scholar] [CrossRef]
- Nickinson, R.S.J.; Board, T.N.; Gambhir, A.K.; Porter, M.L.; Kay, P.R. The microbiology of the infected knee arthroplasty. Int. Orthop. 2010, 34, 505–510. [Google Scholar] [CrossRef] [Green Version]
- Rafiq, I.; Gambhir, A.K.; Wroblewski, B.M.; Kay, P.R. The microbiology of the infected hip arthroplasty. Int. Orthop. 2006, 30, 532–535. [Google Scholar] [CrossRef] [Green Version]
- Bjerke-Kroll, B.T.; Christ, A.B.; McLawhorn, A.S.; Sculco, P.K.; Jules-Elysee, K.M.; Sculco, T.P. Periprosthetic joint infections treated with two-stage revision over 14 years: An evolving microbiologic profile. J. Arthroplast. 2014, 29, 877–882. [Google Scholar] [CrossRef]
- Holleyman, R.J.; Deehan, D.J.; Walker, L.; Charlett, A.; Samuel, J.; Shirley, M.D.F.; Baker, P.N. Staphylococcal resistance profiles in deep infection following primary hip and knee arthroplasty: A study using the NJR dataset. Arch. Orthop. Trauma Surg. 2019, 139, 1209–1215. [Google Scholar] [CrossRef] [Green Version]
- Holleyman, R.J.; Baker, P.; Charlett, A.; Gould, K.; Deehan, D.J. Microorganisms responsible for periprosthetic knee infections in England and Wales. Knee Surg. Sports Traumatol. Arthosc. 2016, 24, 3080–3087. [Google Scholar] [CrossRef] [PubMed]
- Holleyman, R.J.; Baker, P.N.; Charlett, A.; Gould, K.; Deehan, D.J. Analysis of causative microorganisms in 248 primary hip arthroplasties revised for infection: A study using the NJR dataset. Hip. Int. 2016, 26, 82–89. [Google Scholar] [CrossRef]
- McLawhorn, A.S.; Nawabi, D.H.; Ranawat, A.S. Management of resistant, atypical and culture-negative periprosthetic joint infections after hip and knee arthroplasty. Open Orthop. J. 2016, 10, 615–632. [Google Scholar] [CrossRef]
- Szymczak, S.; Michalski, P.; Dudek, J.; Plusa, T.; Baranowski, P.; Burczy, M.; Burczy, J. Finegoldia magna the cause of hip revision surgery—a two case report. Pol. Merkur. Lekarski 2019, 47, 99–102. [Google Scholar] [PubMed]
- Zaninetti-Schaerer, A.; Van Delden, C.; Genevay, S.; Gabay, C. Total hip prosthetic joint infection due to Veilonella species. Joint Bone Spine 2004, 71, 161–163. [Google Scholar] [CrossRef] [PubMed]
- Honnorat, E.; Seng, P.; Savini, H.; Pinelli, P.-O.; Simon, F.; Stein, A. Prosthetic joint infection caused by Pasteurella multocida: A case series and review of the literature. BMC Infect. Dis. 2016, 16, 435. [Google Scholar] [CrossRef]
- Libertin, C.R.; Peterson, J.H.; Brodersen, M.P.; Huff, T. A case of penicillin-resistant Veilonella prosthetic joint infection of the knee. Case Rep. Orthop. 2016, 2016, 7171947. [Google Scholar] [PubMed] [Green Version]
- Curtis, L.; Lipp, M.J. Clostridium difficile infection of a prosthetic knee joint requiring amputation. Surg. Infect. 2013, 14, 163–164. [Google Scholar] [CrossRef]
- Randall, D.; Jee, Y.; Vanood, A.; Mayo, D. Atypical presentation of periprosthetic joint infection after total knee arthroplasty due to Parvimonas micra. Arthroplast. Today 2020, 6, 901–905. [Google Scholar] [CrossRef] [PubMed]
- Hischebeth, G.T.; Kohlhof, H.; Wimmer, M.D.; Randau, T.M.; Bekeredjian-Ding, I.; Gravius, S. Detection of Pantoea agglomerans in hip prosthetic infection by sonication of the removed prosthesis: The first reported case. Technol. Health Care 2013, 21, 613–618. [Google Scholar] [CrossRef]
- Shi, T.B.; Fang, X.Y.; Wang, C.X.; Cai, Y.Q.; Li, W.B.; Zhang, W.M. Rare occurrence of acute hematogenous periprosthetic joint infection due to Fusobacterium nucleatum in the background of a dental procedure: A case report. Orthop. Surg. 2020, 12, 2026–2030. [Google Scholar] [CrossRef] [PubMed]
- Rieber, H.; Frontzek, A.; Fischer, M. Periprosthetic joint infection associated with Mycoplasma hominis after transurethral instrumentation in an immunocompetent patient. Unusual or underestimated? A case report and review of the literature. Int. J. Infect. Dis. 2019, 82, 86–88. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aggarwal, V.K.; Bakhshi, H.; Ecker, N.U.; Parvizi, J.; Gehrke, T.; Kendoff, D. Organism profile in periprosthetic joint infection: Pathogens differ at two arthroplasty infection referral centers in Europe and in the United States. J. Knee Surg. 2014, 27, 399–406. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lindsay, J.A. Staphylococci: Evolving genomes. Microbiol. Spectr. 2019, 7. [Google Scholar] [CrossRef] [PubMed]
- Trampuz, A.; Piper, K.E.; Jacobson, M.J.; Hanssen, A.D.; Unni, K.K.; Osmon, D.R.; Mandrekar, J.N.; Cockerill, F.R.; Steckelberg, J.M.; Greenleaf, J.F.; et al. Sonication of removed hip and knee prostheses for diagnosis of infection. N. Engl. J. Med. 2007, 357, 654–663. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Holinka, J.; Bauer, L.; Hirschl, A.M.; Graninger, W.; Windhager, R.; Presterl, E. Sonication cultures of explanted components as an add-on test to routinely conducted microbiological diagnostics improve pathogen detection. J. Orthop. Res. 2011, 29, 617–622. [Google Scholar] [CrossRef] [PubMed]
- Moojen, D.J.; van Hellemondt, G.; Vogely, H.C.; Burger, B.J.; Walenkamp, G.H.; Tulp, N.J.; Schreurs, B.W.; de Meulemeester, F.R.; Schot, C.S.; van de Pol, I.; et al. Incidence of low-grade infection in aseptic loosening of total hip arthroplasty. Acta Orthop. 2010, 81, 667–673. [Google Scholar] [CrossRef]
- Clarke, M.T.; Roberts, C.P.; Lee, P.T.; Gray, J.; Keene, G.S.; Rushton, N. Polymerase chain reaction can detect bacterial DNA in aseptically loose total hip arthroplasties. Clin. Orthop. Relat. Res. 2004, 427, 132–137. [Google Scholar] [CrossRef]
- Mariani, B.D.; Martin, D.S.; Levine, M.J.; Booth, R.E., Jr.; Tuan, R.S. The Coventry Award. Polymerase chain reaction detection of bacterial infection in total knee arthroplasty. Clin. Orthop. Relat. Res. 1996, 331, 11–22. [Google Scholar] [CrossRef] [PubMed]
- Schäfer, P.; Fink, B.; Sandow, D.; Margull, A.; Berger, I.; Frommelt, L. Prolonged Bacterial Culture to Identify Late Periprosthetic Joint Infection: A Promising Strategy. Clin. Infect. Dis. 2008, 47, 1403–1409. [Google Scholar] [CrossRef] [Green Version]
- Klement, M.R.; Cunningham, D.J.; Wooster, B.M.; Wellman, S.S.; Bolognesi, M.P.; Green, C.L.; Garrigues, G.E. Comparing standard versus extended culture duration in acute hip and knee periprosthetic joint infection. J. Am. Acad. Orthop. Surg. 2019, 27, e437–e443. [Google Scholar] [CrossRef]
- Osmon, D.R.; Berbari, E.F.; Berendt, A.R.; Lew, D.; Zimmerli, W.; Steckelberg, J.M.; Rao, N.; Hanssen, A.; Wilson, W.R.; Infectious Diseases Society of America. Diagnosis and management of prosthetic joint infection: Clinical practise guidelines by the Infectious Diseases Society of America. Clin. Infect. Dis. 2013, 56, e1–e25. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thiery, A.; Anagnostakos, K. Periprosthetic hip-TEP infections after dental procedures: Maybe an indication for antibiotic treatment at all? Orthopäde 2018, 47, 590–593. [Google Scholar] [CrossRef]
- Watters, W.; Rethman, M.P.; Hanson, N.B.; Abt, E.; Anderson, P.A.; Carroll, K.C.; Futrell, H.C.; Garvin, K.; Glenn, S.O.; Hellstein, J.; et al. Prevention of orthopaedic implant infection in patients undergoing dental procedures. J. Am. Acad. Orthop. Surg. 2013, 21, 180–189. [Google Scholar] [CrossRef] [PubMed]
- Flurin, L.; Greenwood-Quaintance, K.E.; Patel, R. Microbiology of polymicrobial joint infection. Diagn. Microbiol. Infect. Dis. 2019, 94, 255–259. [Google Scholar] [CrossRef]
- Marchandin, H.; Jean-Pierre, H.; Carriere, C.; Canovas, F.; Darbas, H.; Jumas-Bilak, E. Prosthetic joint infection due to Veilonella dispar. Eur. J. Clin. Microbiol. Infect. Dis. 2001, 20, 340–342. [Google Scholar] [CrossRef] [PubMed]
- Smith, C.D.; Sridhar, M.S. Life-threatening, bleeding pseudoaneurysm of the external iliac artery in the setting of an infected total hip arthroplasty from Pasteurella multocida. Arthroplast. Today 2020, 6, 560–565. [Google Scholar] [CrossRef]
- Schweon, S.J. Pasteurella infection: An unexpected complication after hip arthroplasty. Nursing 2015, 45, 66–67. [Google Scholar] [CrossRef]
- Heydemann, J.; Heydemann, J.S.; Antony, S. Acute infection of a total knee arthroplasty caused by Pasteurella multocida: A case report and a comprehensive review of the literature in the last 10 years. Int. J. Infect. Dis. 2010, 14, e242–e245. [Google Scholar] [CrossRef] [Green Version]
- Chikwe, J.; Bowditch, M.; Villar, R.N.; Bedford, A.F. Sleeping with the enemy: Pasteurella multocida infection of a total hip replacement. J. R. Soc. Med. 2000, 93, 478–479. [Google Scholar] [CrossRef] [Green Version]
- Takwale, V.J.; Wright, E.D.; Bates, J.; Edge, A.J. Pasteurella multocida infection of a total hip arthroplasty following act scratch. J. Infect. 1997, 34, 263–264. [Google Scholar] [CrossRef]
- Braithwaite, B.D.; Giddins, G. Pasteurella multocida infection of a total hip arthroplasty. A case report. J. Arthroplast. 1992, 7, 309–310. [Google Scholar] [CrossRef]
- Kim, J.H.; Chun, S.K.; Yoon, Y.C.; Lakhotia, D.; Shon, W.Y. Efficacy of debridement for early periprosthetic joint infection after hip arthroplasty. Hip. Pelvis. 2014, 26, 227–234. [Google Scholar] [CrossRef]
- Kaufmann, A.M.; Watters, T.S.; Henderson, R.A.; Wellmann, S.S.; Bolognesi, M.P. Citrobacter koseri as a cause of early periprosthetic infection after primary total hip arthroplasty. J. Arthroplast. 2011, 26, e13–e16. [Google Scholar] [CrossRef]
- Zmistowski, B.; Fedorka, C.J.; Sheehan, E.; Deirmengian, C.; Austin, M.S.; Parvizi, J. Prosthetic joint infection caused by gram-negative organisms. J. Arthroplast. 2011, 26, 104–108. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, P.H.; Lee, M.S.; Hsu, K.Y.; Chang, Y.H.; Shih, H.N.; Ueng, S.W. Gram-negative prosthetic joint infections: Risk factors and outcome of treatment. Clin. Infect. Dis. 2009, 49, 1036–1043. [Google Scholar] [CrossRef]
- Azzam, K.; Parvizi, J.; Jungkind, D.; Hanssen, A.; Fehring, T.; Springer, B.; Bozic, K.; Della Valle, C.; Pullido, L.; Barrack, R. Microbiological, clinical, and surgical features of fungal prosthetic joint infections: A multi-institutional experience. J. Bone Joint Surg. Am. 2009, 91, 142–149. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fusini, F.; Aprato, A.; Massé, A.; Bistolfi, A.; Girardo, M.; Artiaco, S. Candida periprosthetic infection of the hip: A systematic review of surgical treatment and clinical outcomes. Int. Orthop. 2020, 44, 15–22. [Google Scholar] [CrossRef] [PubMed]
- Kuiper, J.W.; van den Bekerom, M.P.; van der Stappen, J.; Nolte, P.A.; Colen, S. 2-stage revision recommended for treatment of fungal hip and knee prosthetic joint infections. Acta Orthop. 2013, 84, 517–523. [Google Scholar] [CrossRef]
- Tan, T.L.; Gomez, M.M.; Kheir, M.M.; Maltenofrt, M.G.; Chen, A.F. Should preoperative antibiotics be tailored according to patient’s comorbidities and susceptibility to organisms? J. Arthroplast. 2017, 32, 1089–1094. [Google Scholar] [CrossRef]
- Wimmer, M.D.; Hischebeth, G.T.R.; Randau, T.M.; Gathen, M.; Schildberg, F.A.; Fröschen, F.S.; Kohlhof, H.; Gravius, S. Difficult-to-treat pathogens significantly reduce infection resolution in periprosthetic joint infections. Diagn. Microbiol. Infect. Dis. 2020, 98, 115114. [Google Scholar] [CrossRef] [PubMed]
- Akgün, D.; Perka, C.; Trampuz, A.; Renz, N. Outcome of hip and knee periprosthetic joint infections caused by pathogens resistant to biofilm-active antibiotics: Results from a prospective cohort study. Arch. Orthop. Trauma Surg. 2018, 138, 635–642. [Google Scholar] [CrossRef]
- Rodriguez-Pardo, D.; Pigrau, C.; Lora-Tamayo, J.; Soriano, A.; del Toro, M.D.; Cobo, J.; Palomino, J.; Euba, G.; Riera, M.; Sanchez-Somolinos, M.; et al. Gram-negative prosthetic joint infection: Outcome of debridement, antibiotics and implant retention approach. A large multicentre study. Clin. Microbiol. Infect. 2014, 20, O911–O919. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thoendel, M.J.; Jeraldo, P.R.; Greenwood-Quaintance, K.E.; Yao, J.Z.; Chia, N.; Hanssen, A.D.; Abdel, M.P.; Patel, R. Identification of Prosthetic Joint Infection Pathogens Using a Shotgun Metagenomics Approach. Clin. Infect. Dis. 2018, 67, 1333–1338. [Google Scholar] [CrossRef] [Green Version]
- Parvizi, J.; Zmistowski, B.; Berbari, E.F.; Bauer, T.W.; Springer, B.D.; Della Valle, C.J.; Garvin, K.L.; Mont, M.A.; Wongworawat, M.D.; Zalavras, C.G. New Definition for Periprosthetic Joint Infection: From the Workgroup of the Musculoskeletal Infection Society. Clin. Orthop. Relat. Res. 2011, 469, 2992–2994. [Google Scholar] [CrossRef] [Green Version]
- Argenson, J.N.; Arndt, M.; Babis, G.; Battenberg, A.; Budhiparama, N.; Catani, F.; Chen, F.; de Beaubien, B.; Ebied, A.; Esposito, S.; et al. Hip and knee section, treatment, debridement, and retention of implant: Proceedings of international consensus on orthopedic infections. J. Arthroplast. 2019, 34, S399–S419. [Google Scholar] [CrossRef]
- Anagnostakos, K.; Jung, J.; Schmid, N.V.; Schmitt, E.; Kelm, J. Mechanical complications and reconstruction strategies at the site of hip spacer implantation. Int. J. Med. Sci. 2009, 6, 274–279. [Google Scholar] [CrossRef] [PubMed]
- Engh, G.A.; Ammeen, D.J. Bone loss with revision total knee arthroplasty: Defect classification and alternatives for reconstruction. Instr. Course Lect. 1999, 48, 167–175. [Google Scholar]
- Preininger, B.; Janz, V.; Von Roth, P.; Trampuz, A.; Pfitzner, T.; Perka, C.F. Inadequacy of Joint Aspiration for Detection of Persistent Periprosthetic Infection During Two-Stage Septic Revision Knee Surgery. Orthopedics 2017, 40, 231–234. [Google Scholar] [CrossRef] [Green Version]
- Boelch, S.P.; Roth, M.; Arnholdt, J.; Rudert, M.; Luedemann, M. Synovial Fluid Aspiration Should Not Be Routinely Performed during the Two-Stage Exchange of the Knee. BioMed Res. Int. 2018, 2018, 6720712. [Google Scholar] [CrossRef] [PubMed]
- Krenn, V.T.; Morawietz, L.; Baumhoer, D.; Krukemeyer, M.; Natu, S.; Boettner, F.; Zustin, J.; Kölbel, B.; Rüther, W.; Kretzer, J.; et al. Revised histopathological consensus classification of joint implant related pathology. Pathol. Res. Pract. 2014, 210, 779–786. [Google Scholar] [CrossRef]
| Treatment Category | n = | Gender | Mean Age (y.) (Min–Max) |
|---|---|---|---|
| Total cohort | 165 | 76 f/89 m | 70.8 (35–89) |
| Hip—total | 100 | 52 f/48 m | 72 (35–89) |
| hip—DAIR | 49 | 22 f/29 m | 71.9 (35–89) |
| hip—2-stage * | 51 | 30 f/19 m | 72.1 (35–89) |
| knee—total | 65 | 24 f/41 m | 69.1 (51–87) |
| knee—DAIR | 12 | 5 f/7 m | 69.9 (57–80) |
| knee—2-stage | 53 | 19 f/34 m | 68.9 (51–87) |
| Microorganism | n (Percentage) |
|---|---|
| Staphylococcus epidermidis | 43 (29.1%) |
| Methicillin-resistant S. epidermidis (MRSE) | 33 (22.3%) |
| Methicillin-susceptible S. epidermidis (MSSE) | 10 (6.8%) |
| Staphylococcus aureus | 26 (17.6%) |
| Methicillin-resistant S. aureus (MRSA) | 2 (1.4%) |
| Methicillin-susceptible S. aureus (MSSA) | 24 (16.2%) |
| Enterococcus faecalis | 13 (8.8%) |
| Beta-hemolytic streptococci | 9 (6.0%) |
| Escherichia coli | 6 (4.0%) |
| Serratia marcescens | 4 (2.7%) |
| Pseudomonas aeruginosa | 4 (2.7%) |
| Enterococcus faecium | 4 (2.7%) |
| Staphylococcus caprae | 3 (2.0%) |
| Staphylococcus haemolyticus | 3 (2.0%) |
| Enterobacter cloacae | 3 (2.0%) |
| Staphylococcus hominis | 3 (2.0%) |
| Cutibacterium acnes | 3 (2.0%) |
| Staphylococcus warneri | 2 (1.3%) |
| Streptococcus gallolyticus | 2 (1.3%) |
| Parvimonas micra | 2 (1.3%) |
| Candida albicans | 2 (1.3%) |
| Citrobacter koseri/diversus | 1 (0.6%) |
| Pasteurella sp. | 1 (0.6%) |
| Proteus mirabilis | 1 (0.6%) |
| Alpha-hemolytic streptococci (not further specified) | 1 (0.6%) |
| Klebsiella pneumoniae | 1 (0.6%) |
| Staphylococcus capitis | 1 (0.6%) |
| Pantoea sp. | 1 (0.6%) |
| Clostridium difficile | 1 (0.6%) |
| Finegoldia magna | 1 (0.6%) |
| Streptococcus oralis | 1 (0.6%) |
| Enterobacterales (not further specified) | 1 (0.6%) |
| Streptococci–(not further specified) | 1 (0.6%) |
| Veilonella parvula/ tobetsuensis | 1 (0.6%) |
| Candida guilliermondii | 1 (0.6%) |
| Morganella morganii | 1 (0.6%) |
| Patient | Gender | Age | Comorbidities |
|---|---|---|---|
| 1 | f | 52 | NIDDM, chronic venous insufficiency, hypothyreosis, hepatitis C, drugs abuse |
| 2 | m | 51 | depression |
| 3 | f | 64 | arterial hypertension, obesity |
| 4 | f | 79 | renal insufficiency, heart insufficiency, peripheral arterial obstructive disease, cerebral hemorrhage, atrial fibrillation |
| 5 | m | 71 | arterial hypertension, obstructive sleep apnea syndrome, NIDDM, coronary heart disease with stents implantation, gout, colon cancer |
| 6 | m | 77 | none |
| 7 | m | 56 | splenectomy due to hereditary spherocytosis |
| 8 | m | 56 | NIDDM, coronary heart disease with bypass surgery, anxiety disorder |
| 9 | f | 82 | arterial hypertension, Alzheimer’s disease |
| 10 | m | 71 | arterial hypertension, atrial fibrillation, anxiety disorder |
| 11 | m | 68 | none |
| 12 | m | 69 | none |
| 13 | m | 85 | arterial hypertension, coronary heart disease, atrial fibrillation |
| 14 | f | 67 | renal insufficiency, atrial fibrillation, Ogilvie syndrome |
| 15 | m | 79 | pulmonary hypertension, heart insufficiency, |
| 16 | f | 63 | arterial hypertension, osteoporosis, obesity, stomach stapling operation |
| Causative Bacterium | M. morganii | V. parvula/tobetsuensis * | F. magna | Cl. difficile | Pantoea sp. | Pasteurella sp. | P. micra (1) | P. micra (2) * | C. koseri/diversus | S. marcescens (1) | S. marcescens (2) | S. marcescens (3) | S. marcescens (4) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ampicillin | r | n.t. | n.t. | n.t. | s | s | s | n.t | r | i | r | r | i |
| Ampicillin/sulbactam | i | n.t. | n.t. | n.t. | s | s | s | n.t | s | s | i | i | s |
| Piperacillin | s | n.t. | n.t. | n.t. | s | s | s | n.t | i | s | s | s | s |
| Piperacillin/tazobactam | s | n.t. | n.t. | n.t. | s | s | s | n.t. | s | s | s | s | s |
| Cefuroxime | s | n.t. | n.t. | n.t. | s | s | s | n.t. | s | r | r | r | r |
| Cefpodoxime | s | n.t. | n.t. | n.t. | s | s | s | n.t. | s | s | s | s | s |
| Cefotaxime | s | n.t. | n.t. | n.t. | s | s | s | n.t. | s | s | s | s | s |
| Ceftazidime | s | n.t. | n.t. | n.t. | s | i | s | n.t. | s | s | s | s | s |
| Imipenem | s | n.t. | n.t. | n.t. | s | s | s | n.t. | s | s | s | s | s |
| Meropenem | s | n.t. | n.t. | n.t. | s | s | s | n.t. | s | s | s | s | s |
| Ertapenem | s | n.t. | n.t. | n.t. | s | n.t. | s | n.t. | s | s | s | s | s |
| Ciprofloxacin | s | n.t. | n.t. | n.t. | s | s | s | n.t. | s | s | s | s | s |
| Moxifloxacin | s | n.t. | n.t. | n.t. | s | s | s | n.t. | s | s | s | s | s |
| Gentamicin | s | n.t. | n.t. | n.t. | s | s | s | n.t. | s | s | s | s | s |
| Tigecycline | r | n.t. | n.t. | n.t. | s | n.t. | s | n.t. | s | i | s | s | s |
| Co-trimoxazole | s | n.t. | n.t. | n.t. | s | s | s | n.t. | s | s | s | s | s |
| Organism | Joint | Primary Surgical Indication | Treatment Procedure | Systemic Antibiotic Therapy | Follow-Up (Months) | Infection Eradication |
|---|---|---|---|---|---|---|
| Morganella morganii * (+ MSSA, E. faecalis) | hip | primary THA | two-stage | rifampicin + vancomycin | lost | unclear |
| Veilonella parvula/tobetsuensis | knee | primary TKA | two-stage | levofloxacine | 12 | yes |
| Finegoldia magna | hip | primary THA | DAIR | ciprofloxacine | 7 | no |
| Clostridium difficile | hip | primary THA | DAIR | rifampicin + ceftriaxone | 10 | yes |
| Pantoea sp. | knee | primary TKA | DAIR | rifampicin + ciprofloxacin | 13 | yes |
| Pasteurella sp. | knee | primary TKA | DAIR | rifampicin + cefuroxime/ciprofloxacine | 54 | yes |
| Parvimonas micra | hip | primary THA | two-stage | moxifloxacine | 42 | yes |
| Parvimonas micra | hip | primary THA | two-stage | ciprofloxacine | 8 | yes |
| Citrobacter koseri/diversus | hip | primary THA | two-stage | meropenem + ciprofloxacine | lost | unclear |
| Serratia marcescens | knee | primary TKA | two-stage | ciprofloxacine | 58 | yes |
| Serratia marcescens | hip | primary THA | DAIR | rifampicin + meropenem/ ciprofloxacine | 34 | yes |
| Serratia marcescens | hip | acetabular cup revision | DAIR | rifampicin + meropenem/ ciprofloxacine | 36 | yes |
| Serratia marcescens | knee | primary TKA | two-stage | ciprofloxacine | 6 | no |
| Candida albicans * (+ E. coli, E. faecium) | knee | primary TKA | two-stage | meropenem + teicoplanin + fluconazole | lost | unclear |
| Candida albicans | hip | primary THA | DAIR | fluconazole | exitus | n.r. |
| Candida guilliermondii | knee | primary TKA | two-stage | voriconazole | 19 | no |
| Bacterium | Gram Stain | Aerobic/ Anaerobic | Family | Microscopic Morphology | Physiologic Environment |
|---|---|---|---|---|---|
| Morganella morganii | negative | facultatively anaerobic | Morganellaceae | rods | normal flora in intestinal tracts of humans, mammals, and reptiles |
| Veilonella sp. | negative | anaerobic | Veilonellaceae | cocci | normal flora in intestinal tracts and oral mucosa from mammals |
| Finegoldia magna | positive | anaerobic | Clostridia | cocci | normal flora on human skin, mucous membranes |
| Clostridium difficile | positive | anaerobic | Clostridioides | rods | normal flora in intestinal tracts of humans |
| Pantoea sp. | negative | facultatively anaerobic | Erwiniaceae | rods | plant surfaces, seeds, fruit, animal/human feces |
| Pasteurella sp. | negative | facultatively anaerobic | Pasteurellaceae | rods | oral flora from cats and dogs |
| Parvimonas micra | positive | anaerobic | Peptoniphilaceae | cocci | oral flora in humans |
| Citrobacter koseri/diversus | negative | facultatively anaerobic | Enterobacteriaeae | rods | normal flora from human and animal digestive tracts |
| Serratia marcescens | negative | facultatively anaerobic | Yersiniaceae | rods | human and animal digestive tracts, dust, soil, surface waters |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Anagnostakos, K.; Grzega, C.; Sahan, I.; Geipel, U.; Becker, S.L. Occurrence of Rare Pathogens at the Site of Periprosthetic Hip and Knee Joint Infections: A Retrospective, Single-Center Study. Antibiotics 2021, 10, 882. https://doi.org/10.3390/antibiotics10070882
Anagnostakos K, Grzega C, Sahan I, Geipel U, Becker SL. Occurrence of Rare Pathogens at the Site of Periprosthetic Hip and Knee Joint Infections: A Retrospective, Single-Center Study. Antibiotics. 2021; 10(7):882. https://doi.org/10.3390/antibiotics10070882
Chicago/Turabian StyleAnagnostakos, Konstantinos, Christoph Grzega, Ismail Sahan, Udo Geipel, and Sören L. Becker. 2021. "Occurrence of Rare Pathogens at the Site of Periprosthetic Hip and Knee Joint Infections: A Retrospective, Single-Center Study" Antibiotics 10, no. 7: 882. https://doi.org/10.3390/antibiotics10070882
APA StyleAnagnostakos, K., Grzega, C., Sahan, I., Geipel, U., & Becker, S. L. (2021). Occurrence of Rare Pathogens at the Site of Periprosthetic Hip and Knee Joint Infections: A Retrospective, Single-Center Study. Antibiotics, 10(7), 882. https://doi.org/10.3390/antibiotics10070882








