Blood Cultures and Appropriate Antimicrobial Administration after Achieving Sustained Return of Spontaneous Circulation in Adults with Nontraumatic Out-of-Hospital Cardiac Arrest
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
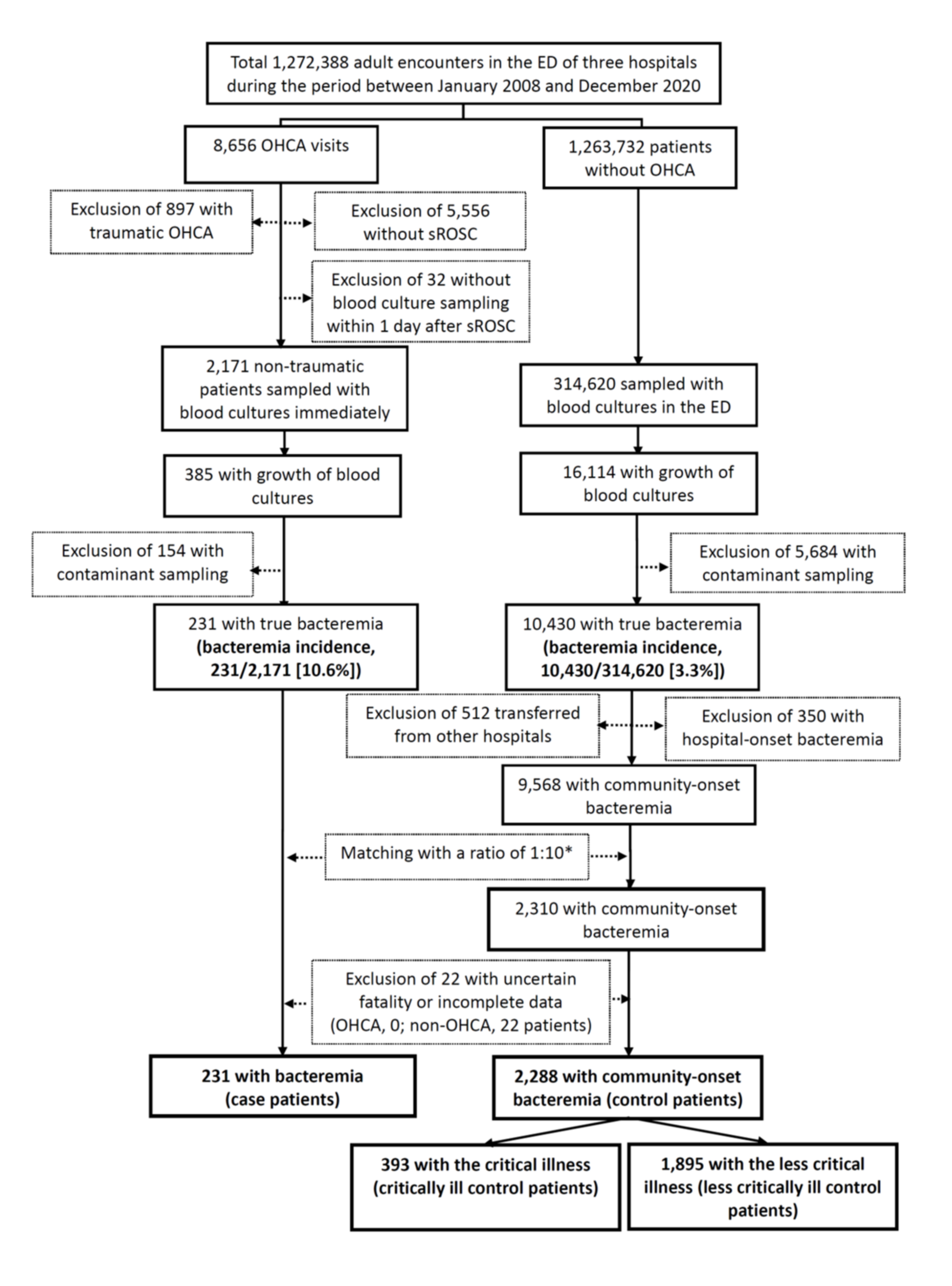
2.2. Selection of Participants
2.3. Measurements and Outcomes
2.4. Sampling of Blood Cultures and Microbiological Methods
2.5. Definitions
2.6. Statistical Analyses
3. Results
3.1. Characteristics of Study Subjects
3.2. Clinical Characteristics and Outcomes of Case and Control Patients
3.3. Microorganisms and Susceptibilities in Case and Control Patients
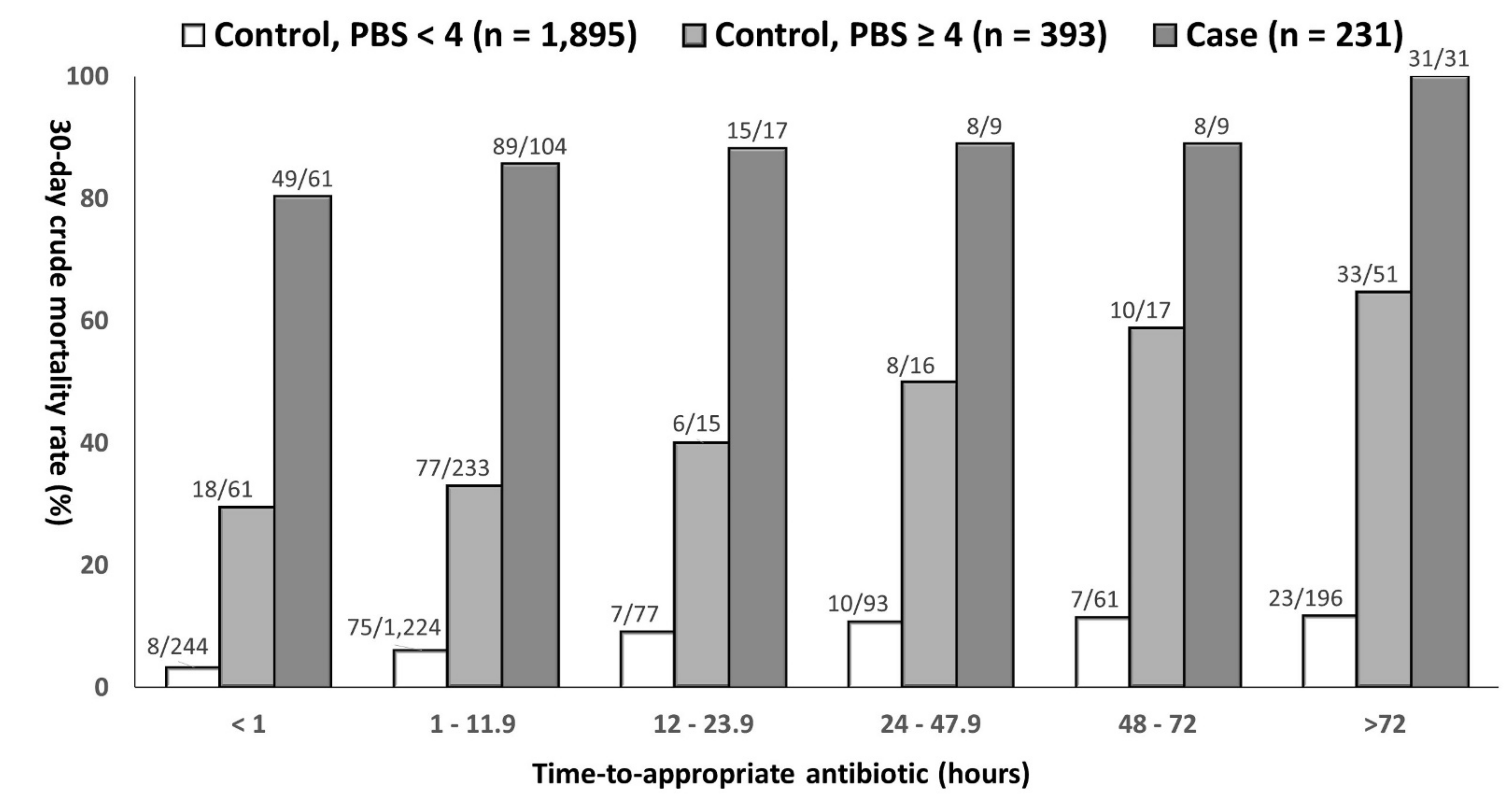
3.4. Impacts of Delayed AAT on Mortality of Patients with Varied Bacteremia Severity
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bates, D.W.; Pruess, K.E.; Lee, T.H. How bad are bacteremia and sepsis? Outcomes in a cohort with suspected bacteremia. Arch. Intern. Med. 1995, 155, 593–598. [Google Scholar] [CrossRef]
- Laupland, K.B.; Gregson, D.B.; Flemons, W.W.; Hawkins, D.; Ross, T.; Church, D.L. Burden of community-onset bloodstream infection: A population-based assessment. Epidemiol. Infect. 2006, 135, 1037–1042. [Google Scholar] [CrossRef] [PubMed]
- Laupland, K.B.; Pasquill, K.; Dagasso, G.; Parfitt, E.C.; Steele, L.; Schonheyder, H.C. Population-based risk factors for community-onset bloodstream infections. Eur. J. Clin. Microbiol. Infect. Dis. 2019, 39, 753–758. [Google Scholar] [CrossRef]
- Valles, J.; Rello, J.; Ochagavia, A.; Garnacho, J.; Alcala, M.A. Community-acquired bloodstream infection in critically ill adult patients: Impact of shock and inappropriate antibiotic therapy on survival. Chest 2003, 123, 1615–1624. [Google Scholar] [CrossRef]
- Lee, C.-C.; Lee, C.-H.; Hong, M.-Y.; Tang, H.-J.; Ko, W.-C. Timing of appropriate empirical antimicrobial administration and outcome of adults with community-onset bacteremia. Crit. Care 2017, 21, 119. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Corona, A.; Bertolini, G.; Lipman, J.; Wilson, A.P.R.; Singer, M. Antibiotic use and impact on outcome from bacteraemic critical illness: The BActeraemia Study in Intensive Care (BASIC). J. Antimicrob. Chemother. 2010, 65, 1276–1285. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, C.-C.; Lee, C.-H.; Yang, C.-Y.; Hsieh, C.-C.; Tang, H.-J.; Ko, W.-C. Beneficial effects of early empirical administration of appropriate antimicrobials on survival and defervescence in adults with community-onset bacteremia. Crit. Care 2019, 23, 363. [Google Scholar] [CrossRef] [Green Version]
- Berdowski, J.; Berg, R.A.; Tijssen, J.G.; Koster, R.W. Global incidences of out-of-hospital cardiac arrest and survival rates: Systematic review of 67 prospective studies. Resuscitation 2010, 81, 1479–1487. [Google Scholar] [CrossRef]
- Tsai, M.-S.; Chiang, W.-C.; Lee, C.-C.; Hsieh, C.-C.; Ko, P.C.-I.; Hsu, C.-Y.; Su, C.-P.; Chen, S.-Y.; Chang, W.-T.; Yuan, A.; et al. Infections in the survivors of out-of-hospital cardiac arrest in the first 7 days. Intensiv. Care Med. 2005, 31, 621–626. [Google Scholar] [CrossRef]
- Mongardon, N.; Perbet, S.; Lemiale, V.; Dumas, F.; Poupet, H.; Charpentier, J.; Pene, F.; Chiche, J.-D.; Mira, J.-P.; Cariou, A. Infectious complications in out-of-hospital cardiac arrest patients in the therapeutic hypothermia era. Crit. Care Med. 2011, 39, 1359–1364. [Google Scholar] [CrossRef] [PubMed]
- Dankiewicz, J.; Nielsen, N.; Linder, A.; Kuiper, M.; Wise, M.P.; Cronberg, T.; Erlinge, D.; Gasche, Y.; Harmon, M.B.; Hassager, C. Infectious complications after out-of-hospital cardiac arrest—A comparison between two target temperatures. Resuscitation 2017, 113, 70–76. [Google Scholar] [CrossRef]
- Coba, V.; Jaehne, A.K.; Suarez, A.; Dagher, G.A.; Brown, S.C.; Yang, J.J.; Manteuffel, J.; Rivers, E.P. The incidence and significance of bacteremia in out of hospital cardiac arrest. Resuscitation 2014, 85, 196–202. [Google Scholar] [CrossRef] [PubMed]
- Merchant, R.M.; Topjian, A.A.; Panchal, A.R.; Cheng, A.; Aziz, K.; Berg, K.M.; Lavonas, E.J.; Magid, D.J. Part 1: Executive summary: 2020 American heart association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 2020, 142, S337–S357. [Google Scholar] [CrossRef]
- Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Susceptibility Testing; Approved Standard. 31th Informational Supplement; CLSI Document M100-S31; CLSI: Wayne, PA, USA, 2021. [Google Scholar]
- Lee, C.C.; Lin, W.J.; Shih, H.I.; Wu, C.J.; Chen, P.L.; Lee, H.C.; Lee, N.Y.; Chang, C.M.; Wang, L.R.; Ko, W.C. Clinical significance of potential contaminants in blood cultures among patients in a medical center. J. Microbiol. Immunol. Infect. 2007, 40, 438–444. [Google Scholar] [PubMed]
- Gilbert, D.N.; Chambers, H.F.; Saag, M.S. Antimicrobial Drug Dosage/Side Effects. In The Sanford Guide to Antimicrobial Therapy 2021; Antimicrobial Therapy, Incorpo: Sperryville, VA, USA, 2021; pp. 117–135. [Google Scholar]
- Schellevis, F.; Van der Velden, J.; Van de Lisdonk, E.; Van Eijk, J.; Van Weel, C. Comorbidity of chronic diseases in general practice. J. Clin. Epidemiol. 1993, 46, 469–473. [Google Scholar] [CrossRef] [Green Version]
- McCabe, W.R. Gram-negative bacteremia. Adv. Intern. Med. 1974, 19, 135–158. [Google Scholar] [CrossRef] [PubMed]
- Garner, J.S.; Jarvis, W.R.; Emori, T.G.; Horan, T.C.; Hughes, J.M. CDC definitions for nosocomial infections, 1988. Am. J. Infect. Control. 1988, 16, 128–140. [Google Scholar] [CrossRef]
- Rhodes, A.A.; Evans, L.E.; Alhazzani, W.; Levy, M.M.; Antonelli, M.; Ferrer, R.; Kumar, A.; Sevransky, J.E.; Sprung, C.L.; Nunnally, M.E.; et al. Surviving sepsis campaign: International guidelines for management of sepsis and septic shock: 2016. Crit. Care Med. 2017, 45, 486–552. [Google Scholar] [CrossRef]
- VanderWeele, T.J.; Ding, P. Sensitivity analysis in observational research: Introducing the E-value. Ann. Intern. Med. 2017, 167, 268–274. [Google Scholar] [CrossRef] [PubMed]
- Chalkias, A.; Scheetz, M.; Gulati, A.; Xanthos, T. Periarrest intestinal bacterial translocation and resuscitation outcome. J. Crit. Care 2016, 31, 217–220. [Google Scholar] [CrossRef]
- McCabe, R.E.; Remington, J.S. C-reactive protein in patients with bacteremia. J. Clin. Microbiol. 1984, 20, 317–319. [Google Scholar] [CrossRef] [Green Version]
- Iwami, T.; Nichol, G.; Hiraide, A.; Hayashi, Y.; Nishiuchi, T.; Kajino, K.; Morita, H.; Yukioka, H.; Ikeuchi, H.; Sugimoto, H.; et al. Continuous improvements in “Chain of Survival” increased survival after out-of-hospital cardiac arrests. Circulation 2009, 119, 728–734. [Google Scholar] [CrossRef] [Green Version]
- Christensen, D.; Rajan, S.; Kragholm, K.; Søndergaard, K.; Hansen, O.M.; Gerds, T.; Torp-Pedersen, C.; Gislason, G.; Lippert, F.K.; Barcella, C. Bystander cardiopulmonary resuscitation and survival in patients with out-of-hospital cardiac arrest of non-cardiac origin. Resuscitation 2019, 140, 98–105. [Google Scholar] [CrossRef]
- Hall, K.K.; Lyman, J.A. Updated review of blood culture contamination. Clin. Microbiol. Rev. 2006, 19, 788–802. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, C.-C.; Lee, N.-Y.; Chuang, M.-C.; Chen, P.-L.; Chang, C.-M.; Ko, W.-C. The impact of overcrowding on the bacterial contamination of blood cultures in the ED. Am. J. Emerg. Med. 2012, 30, 839–845. [Google Scholar] [CrossRef] [PubMed]
- Peltan, I.D.; Bledsoe, J.R.; Oniki, T.A.; Sorensen, J.; Jephson, A.R.; Allen, T.L.; Samore, M.H.; Hough, C.L.; Brown, S. Emergency department crowding is associated with delayed antibiotics for sepsis. Ann. Emerg. Med. 2019, 73, 345–355. [Google Scholar] [CrossRef] [PubMed]
- Gaieski, D.F.; Agarwal, A.K.; Mikkelsen, M.E.; Drumheller, B.; Sante, S.C.; Shofer, F.S.; Goyal, M.; Pines, J.M. The impact of ED crowding on early interventions and mortality in patients with severe sepsis. Am. J. Emerg. Med. 2017, 35, 953–960. [Google Scholar] [CrossRef] [PubMed]
- Diekema, D.; Beekmann, S.E.; Chapin, K.C.; Morel, K.A.; Munson, E.; Doern, G.V. Epidemiology and outcome of nosocomial and community-onset bloodstream infection. J. Clin. Microbiol. 2003, 41, 3655–3660. [Google Scholar] [CrossRef] [Green Version]
- Paterson, D.L.; Bonomo, R.A. Extended-spectrum β-lactamases: A clinical update. Clin. Microbiol. Rev. 2005, 18, 657–686. [Google Scholar] [CrossRef] [Green Version]
- Lee, C.-H.; Chu, F.-Y.; Hsieh, C.-C.; Hong, M.-Y.; Chi, C.-H.; Ko, W.-C.; Lee, C.-C. A simple scoring algorithm predicting extended-spectrum β-lactamase producers in adults with community-onset monomicrobial Enterobacteriaceae bacteremia. Medicine 2017, 96, e6648. [Google Scholar] [CrossRef]
- Hunt, K.A.; Weber, E.J.; Showstack, J.; Colby, D.C.; Callaham, M. Characteristics of frequent users of emergency departments. Ann. Emerg. Med. 2006, 48, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Bernstein, S.L. Frequent emergency department visitors: The end of inappropriateness. Ann. Emerg. Med. 2006, 48, 18–20. [Google Scholar] [CrossRef] [PubMed]
- Gilbert, E.H.; Lowenstein, S.R.; Koziol-McLain, J.; Barta, D.C.; Steiner, J. Chart reviews in emergency medicine research: Where are the methods? Ann. Emerg. Med. 1996, 27, 305–308. [Google Scholar] [CrossRef]

| Variables | Patient Numbers (%) | p Value | |
|---|---|---|---|
| Case n = 231 | Control n = 2288 | ||
| Patient demographics | |||
| Gender, male | 121 (52.4) | 1162 (50.8) | 0.64 |
| The elderly, ≥65 years | 153 (66.2) | 1399 (61.1) | 0.13 |
| Nursing-home residents | 34 (14.7) | 127 (5.6) | <0.001 |
| Bed-ridden status | 82 (35.5) | 289 (12.6) | <0.001 |
| ED visits within prior 6 months, median (IQR) | 2 (1–3) | 0 (0–1) | <0.001 |
| Polymicrobial bacteremia | 43 (18.6) | 219 (9.6) | <0.001 |
| Pitt bacteremia score ≥4 at ED arrival | 231 (100) | 393 (17.2) | <0.001 |
| Major sources of bacteremia | |||
| Low respiratory tract infections | 136 (58.9) | 302 (13.2) | <0.001 |
| Urinary tract infections | 17 (7.4) | 765 (33.4) | <0.001 |
| Skin and soft-tissue infections | 14 (6.1) | 233 (10.2) | 0.045 |
| Intra-abdominal infections | 10 (4.3) | 293 (12.8) | <0.001 |
| Biliary tract infections | 4 (1.7) | 207 (9.0) | <0.001 |
| Ultimately or rapidly fatal comorbidities (McCabe–Johnson classification) | 59 (25.5) | 545 (23.8) | 0.56 |
| Major comorbidities | |||
| Cardiovascular diseases | 125 (54.1) | 1211 (52.9) | 0.73 |
| Neurological diseases | 96 (41.6) | 545 (23.8) | <0.001 |
| Diabetes mellitus | 95 (41.1) | 849 (37.1) | 0.23 |
| Malignancies | 70 (30.3) | 647 (28.3) | 0.52 |
| Chronic kidney diseases | 45 (19.5) | 417 (18.2) | 0.64 |
| Urological diseases | 19 (8.2) | 154 (6.7) | 0.39 |
| Chronic obstructive pulmonary diseases | 18 (7.8) | 113 (4.9) | 0.06 |
| Liver cirrhosis | 17 (7.4) | 293 (12.8) | 0.02 |
| Psychological diseases | 14 (5.1) | 33 (1.4) | <0.001 |
| Time-to-appropriate antibiotic, hours, median (IQR) | 10 (0.9–20.0) | 2.0 (1.1–8.0) | <0.001 |
| Laboratory data at EDs, median (IQR) | |||
| Leukocyte (1000/mm3) | 13.5 (7.1–20.6) | 11.5 (7.5–16.3) | <0.001 |
| C-reactive protein (mg/L), n = 2734 | 121.3 (41.7–214.3) | 69.9 (28.3–186.3) | <0.001 |
| Crude mortality rates | |||
| 3-day | 142 (61.5) | 99 (4.3) | <0.001 |
| 15-day | 177 (76.6) | 195 (8.5) | <0.001 |
| 30-day | 200 (86.6) | 282 (12.3) | <0.001 |
| Clinical Variables | Patient Number (%) | Univariate Analysis | Multivariate Analysis | |||
|---|---|---|---|---|---|---|
| Death | Survival | OR (95% CI) | p-Value | AOR (95% CI) | p Value | |
| Case patients (n = 231) | n = 200 | n = 31 | ||||
| Time-to-appropriate antibiotic (hour) * | – | – | – | – | 1.106 (1.031–1.187) | 0.005 |
| Time-to-sROSC ** > 11 min | 114 (57.0) | 3 (9.7) | 12.4 (3.6–42.0) | <0.001 | 19.00 (5.32–67.83) | <0.001 |
| Ultimately or rapidly fatal comorbidities (McCabe–Johnson classification) | 58 (29.0) | 1 (3.2) | 12.25 (1.63–91.97) | 0.002 | 8.82 (1.09–72.28) | 0.04 |
| Comorbidities | ||||||
| Cardiovascular diseases | 103 (51.5) | 22 (71.0) | 0.43 (0.19–0.99) | 0.04 | NS | NS |
| Malignancies | 65 (32.5) | 5 (16.1) | 2.50 (0.92–6.82) | 0.07 | NS | NS |
| Psychological diseases | 9 (4.5) | 5 (16.1) | 0.25 (0.08–0.79) | 0.01 | NS | NS |
| Critically ill control patients (n = 393) | n = 152 | n = 241 | ||||
| Time-to-appropriate antibiotic (hour) * | – | – | – | – | 1.007 (1.004–1.010) | <0.001 |
| Gender, male | 99 (65.1) | 130 (53.9) | 1.60 (1.05–2.43) | 0.03 | NS | NS |
| Inadequate source control | 8 (5.3) | 6 (2.5) | 2.18 (0.74–6.40) | 0.15 | 2.72 (0.83–8.87) | 0.10 |
| Bacteremia sources | ||||||
| Urinary tract infections | 17 (11.2) | 79 (32.8) | 0.26 (0.15–0.46) | <0.001 | 0.44 (0.23–0.83) | 0.01 |
| Low respiratory tract infections | 62 (40.8) | 62 (25.7) | 1.99 (1.29–3.06) | 0.002 | 1.74 (1.05–2.89) | 0.03 |
| Ultimately or rapidly fatal comorbidities (McCabe–Johnson classification) | 70 (46.1) | 58 (24.1) | 2.69 (1.74–4.18) | <0.001 | 2.42 (1.51–3.89) | <0.001 |
| Comorbidities | ||||||
| Malignancies | 70 (46.1) | 66 (27.4) | 2.26 (1.48–3.47) | <0.001 | NS | NS |
| Diabetes mellitus | 52 (34.2) | 105 (43.6) | 0.67 (0.441–1.03) | 0.06 | 0.63 (0.39–1.006) | 0.05 |
| Neurological diseases | 48 (31.6) | 98 (40.7) | 0.67 (0.44–1.03) | 0.07 | NS | NS |
| Liver cirrhosis | 28 (17.1) | 19 (7.9) | 2.41 (1.26–4.53) | 0.005 | NS | NS |
| Urological diseases | 8 (5.3) | 32 (13.3) | 0.36 (0.16–0.81) | 0.01 | NS | NS |
| COPD | 7 (4.6) | 25 (10.4) | 0.42 (0.18–0.99) | 0.04 | 0.40 (0.15–1.06) | 0.07 |
| Less critically ill control patients (n = 1895) | n = 130 | n = 1765 | ||||
| Time-to-appropriate antibiotic (hour) * | – | – | – | – | 1.003 (1.001 −1.005) | 0.004 |
| Inadequate source control | 6 (4.6) | 45 (2.5) | 1.85 (0.77–4.42) | 0.16 | 2.35 (0.92 − 6.05) | 0.08 |
| Gender, male | 75 (57.7) | 858 (48.6) | 1.44 (1.01–2.07) | 0.046 | NS | NS |
| Nursing-home residents | 14 (10.8) | 58 (3.3) | 3.55 (1.92–6.56) | <0.001 | 4.27 (2.14–8.54) | <0.001 |
| Polymicrobial bacteremia | 20 (15.4) | 136 (7.7) | 2.18 (1.31–3.62) | 0.002 | 2.04 (1.17–3.54) | 0.01 |
| Bacteremia sources | ||||||
| Low respiratory tract infections | 31 (23.8) | 147 (8.3) | 3.45 (2.23–5.34) | <0.001 | 2.07 (1.26–3.43) | 0.04 |
| Intraabdominal infections | 26 (20.0) | 227 (12.9) | 1.69 (1.08–2.66) | 0.02 | NS | NS |
| Urinary tract infections | 21 (16.2) | 648 (36.7) | 0.33 (0.21–0.54) | <0.001 | 0.50 (0.29–0.85) | 0.01 |
| Ultimately or rapidly fatal comorbidities (McCabe–Johnson classification) | 76 (58.5) | 341 (19.3) | 5.88 (4.07–8.49) | <0.001 | 3.65 (2.33–5.72) | <0.001 |
| Comorbidities | ||||||
| Malignancies | 74 (56.9) | 437 (24.8) | 4.02 (2.79–5.78) | <0.001 | 1.98 (1.26–3.13) | 0.003 |
| Liver cirrhosis | 35 (26.9) | 213 (12.1) | 2.68 (1.78–4.06) | <0.001 | NS | NS |
| COPD | 13 (10.0) | 68 (3.9) | 2.77 (1.49–5.17) | 0.001 | 2.44 (1.20–4.94) | 0.01 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lin, C.-H.; Chen, P.-L.; Huang, Y.-T.; Ho, C.-Y.; Hsieh, C.-C.; Wang, W.Y.C.; Lee, C.-C.; Ko, W.-C. Blood Cultures and Appropriate Antimicrobial Administration after Achieving Sustained Return of Spontaneous Circulation in Adults with Nontraumatic Out-of-Hospital Cardiac Arrest. Antibiotics 2021, 10, 876. https://doi.org/10.3390/antibiotics10070876
Lin C-H, Chen P-L, Huang Y-T, Ho C-Y, Hsieh C-C, Wang WYC, Lee C-C, Ko W-C. Blood Cultures and Appropriate Antimicrobial Administration after Achieving Sustained Return of Spontaneous Circulation in Adults with Nontraumatic Out-of-Hospital Cardiac Arrest. Antibiotics. 2021; 10(7):876. https://doi.org/10.3390/antibiotics10070876
Chicago/Turabian StyleLin, Chih-Hao, Po-Lin Chen, Yi-Tzu Huang, Ching-Yu Ho, Chih-Chia Hsieh, William Yu Chung Wang, Ching-Chi Lee, and Wen-Chien Ko. 2021. "Blood Cultures and Appropriate Antimicrobial Administration after Achieving Sustained Return of Spontaneous Circulation in Adults with Nontraumatic Out-of-Hospital Cardiac Arrest" Antibiotics 10, no. 7: 876. https://doi.org/10.3390/antibiotics10070876
APA StyleLin, C.-H., Chen, P.-L., Huang, Y.-T., Ho, C.-Y., Hsieh, C.-C., Wang, W. Y. C., Lee, C.-C., & Ko, W.-C. (2021). Blood Cultures and Appropriate Antimicrobial Administration after Achieving Sustained Return of Spontaneous Circulation in Adults with Nontraumatic Out-of-Hospital Cardiac Arrest. Antibiotics, 10(7), 876. https://doi.org/10.3390/antibiotics10070876









