Strong Antimicrobial and Healing Effects of Beta-Acids from Hops in Methicillin-Resistant Staphylococcus aureus-Infected External Wounds In Vivo
Abstract
1. Introduction
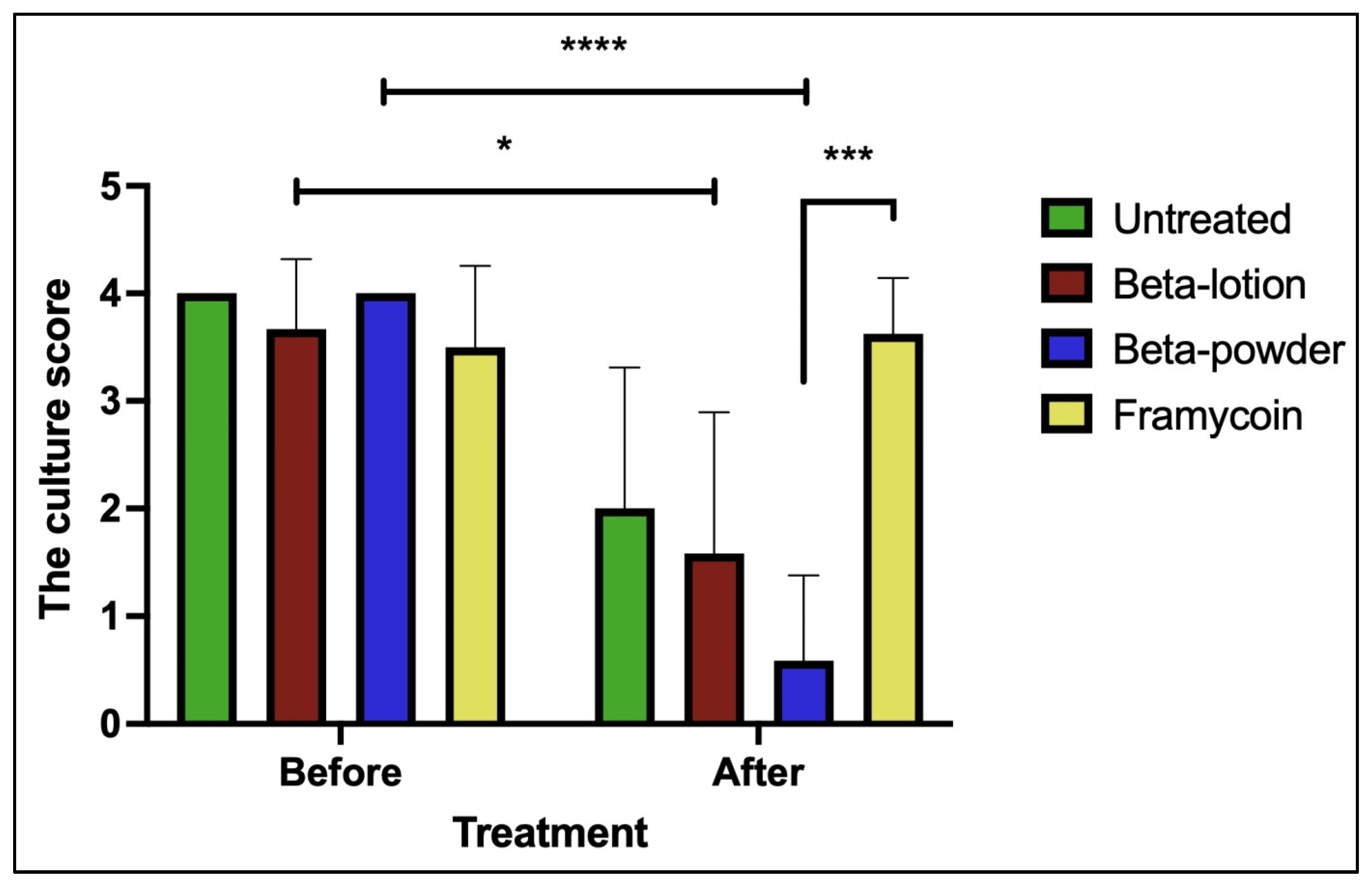
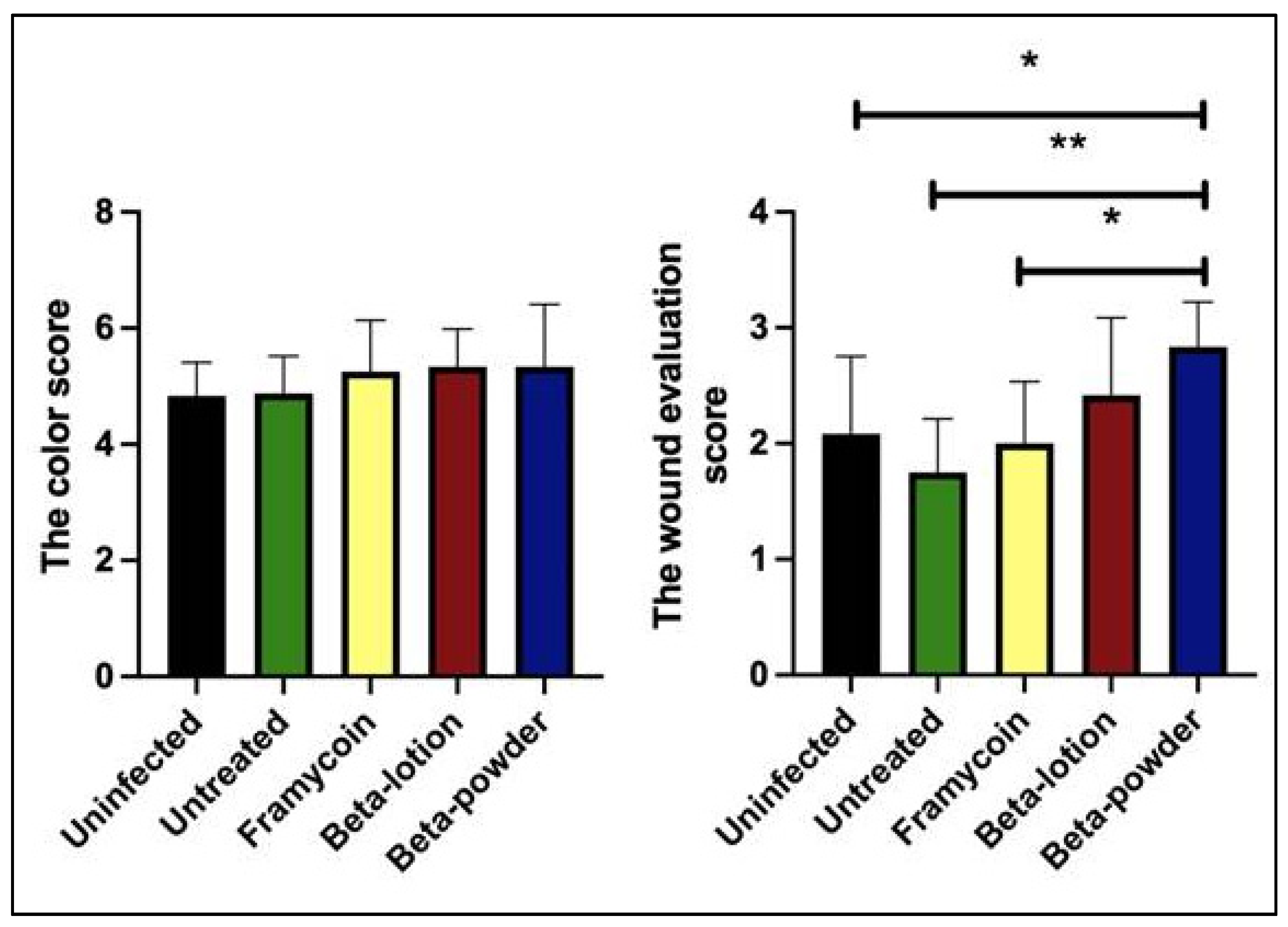
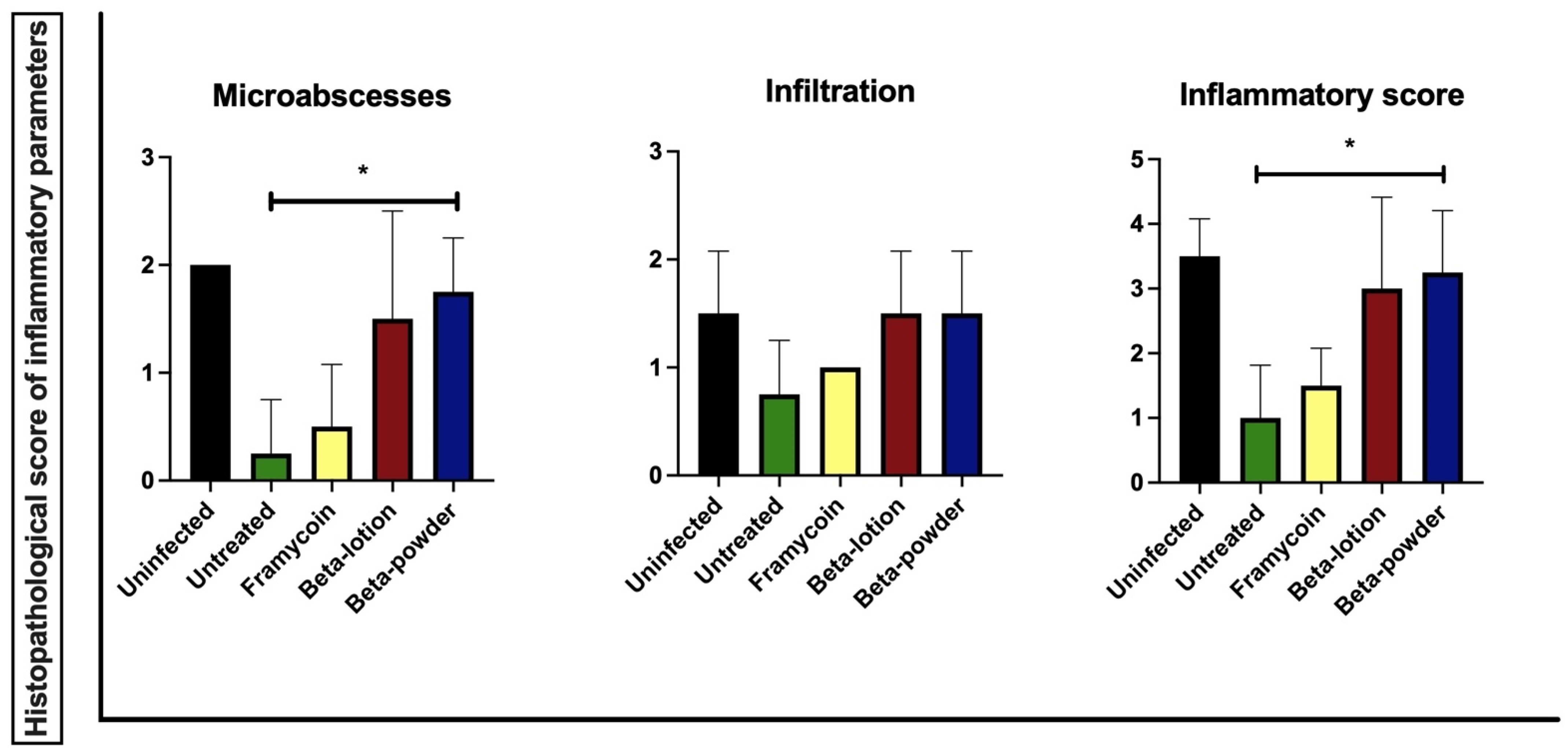
2. Results
3. Discussion
4. Materials and Methods
4.1. Hop Compounds
4.2. Bacterial Strain and Culture Conditions
4.3. In Vitro Antimicrobial Testing of Hops Compounds
4.4. Animals and Housing
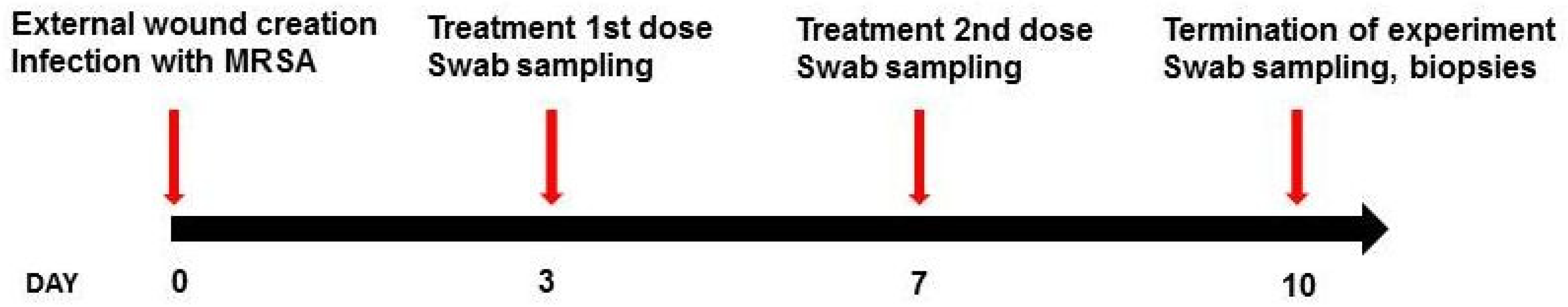
4.5. Experimental Model
4.6. Wound Treatments and Macroscopic Assessment
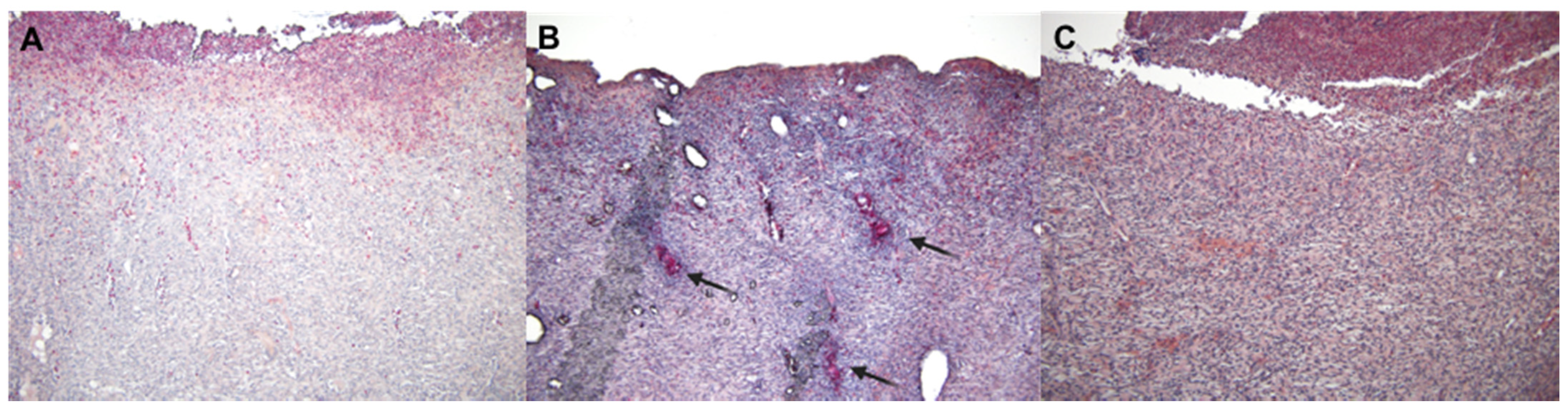
4.7. Histopathology Examination
4.8. Data Analysis
5. Conclusions
6. Patents
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sakr, A.; Bregeon, F.; Mege, J.L.; Rolain, J.M.; Blin, O. Staphylococcus aureus Nasal Colonization: An Update on Mechanisms, Epidemiology, Risk Factors, and Subsequent Infections. Front. Microbiol. 2018, 9, 2419. [Google Scholar] [CrossRef] [PubMed]
- Lone, A.G.; Atci, E.; Renslow, R.; Beyenal, H.; Noh, S.; Fransson, B.; Abu-Lail, N.; Park, J.J.; Gang, D.R.; Call, D.R. Staphylococcus aureus induces hypoxia and cellular damage in porcine dermal explants. Infect. Immun. 2015, 83, 2531–2541. [Google Scholar] [CrossRef] [PubMed]
- McCaig, L.F.; McDonald, L.C.; Mandal, S.; Jernigan, D.B. Staphylococcus aureus-associated skin and soft tissue infections in ambulatory care. Emerg. Infect. Dis. 2006, 12, 1715–1723. [Google Scholar] [CrossRef] [PubMed]
- Turner, N.A.; Sharma-Kuinkel, B.K.; Maskarinec, S.A.; Eichenberger, E.M.; Shah, P.P.; Carugati, M.; Holland, T.L.; Fowler, V.G., Jr. Methicillin-resistant Staphylococcus aureus: An overview of basic and clinical research. Nat. Rev. Microbiol. 2019, 17, 203–218. [Google Scholar] [CrossRef]
- Bogdanova, K.; Roderova, M.; Kolar, M.; Langova, K.; Dusek, M.; Jost, P.; Kubelkova, K.; Bostik, P.; Olsovska, J. Antibiofilm activity of bioactive hop compounds humulone, lupulone and xanthohumol toward susceptible and resistant staphylococci. Res. Microbiol. 2018, 169, 127–134. [Google Scholar] [CrossRef] [PubMed]
- Cermak, P.; Olsovska, J.; Mikyska, A.; Dusek, M.; Kadleckova, Z.; Vanicek, J.; Nyc, O.; Sigler, K.; Bostikova, V.; Bostik, P. Strong antimicrobial activity of xanthohumol and other derivatives from hops (Humulus lupulus L.) on gut anaerobic bacteria. APMIS 2017, 125, 1033–1038. [Google Scholar] [CrossRef]
- Roehrer, S.; Behr, J.; Stork, V.; Ramires, M.; Medard, G.; Frank, O.; Kleigrewe, K.; Hofmann, T.; Minceva, M. Xanthohumol C. A minor bioactive hop compound: Production, purification strategies and antimicrobial test. J. Chromatogr. B Analyt. Technol. Biomed. Life Sci. 2018, 1095, 39–49. [Google Scholar] [CrossRef]
- Barington, K.; Dich-Jorgensen, K.; Jensen, H.E. A porcine model for pathomorphological age assessment of surgically excised skin wounds. Acta Vet. Scand. 2018, 60, 33. [Google Scholar] [CrossRef]
- Dai, T.; Kharkwal, G.B.; Tanaka, M.; Huang, Y.Y.; Bil de Arce, V.J.; Hamblin, M.R. Animal models of external traumatic wound infections. Virulence 2011, 2, 296–315. [Google Scholar] [CrossRef]
- Jensen, L.K.; Johansen, A.S.B.; Jensen, H.E. Porcine Models of Biofilm Infections with Focus on Pathomorphology. Front. Microbiol. 2017, 8, 1961. [Google Scholar] [CrossRef]
- Meyer, W.; Schwarz, R.; Neurand, K. The skin of domestic mammals as a model for the human skin, with special reference to the domestic pig. Curr. Probl. Dermatol. 1978, 7, 39–52. [Google Scholar] [CrossRef]
- Zurawski, D.V.; Black, C.C.; Alamneh, Y.A.; Biggemann, L.; Banerjee, J.; Thompson, M.G.; Wise, M.C.; Honnold, C.L.; Kim, R.K.; Paranavitana, C.; et al. A Porcine Wound Model of Acinetobacter baumannii Infection. Adv. Wound Care (New Rochelle) 2019, 8, 14–27. [Google Scholar] [CrossRef] [PubMed]
- Bogdanova, K.; Kolar, M.; Langova, K.; Dusek, M.; Mikyska, A.; Bostikova, V.; Bostik, P.; Olsovska, J. Inhibitory effect of hop fractions against Gram-positive multi-resistant bacteria. A pilot study. Biomed. Pap. Med. Fac. Univ. Palacky. Olomouc Czech Repub 2018. [Google Scholar] [CrossRef] [PubMed]
- Bacitracin—Natural Peptide with Minimal Resistance Issues. Available online: https://www.thepigsite.com/articles/bacitracin-natural-peptide-with-minimal-resistance-issues (accessed on 15 May 2018).
- Gray, D.; White, R.; Cooper, P.; Kingsley, A. Applied Wound Management and Using the Wound Healing Continuum in Practice. Wound Essent. 2010, 5, 131–139. [Google Scholar]
- Kolar, M.; Cermak, P.; Hobzova, L.; Bogdanova, K.; Neradova, K.; Mlynarcik, P.; Bostik, P. Antibiotic Resistance in Nosocomial Bacteria Isolated from Infected Wounds of Hospitalized Patients in Czech Republic. Antibiotics (Basel) 2020, 9, 342. [Google Scholar] [CrossRef]
- Dou, J.L.; Jiang, Y.W.; Xie, J.Q.; Zhang, X.G. New is old, and old is new: Recent advances in antibiotic-based, antibiotic-free and ethnomedical treatments against methicillin-resistant Staphylococcus aureus wound infections. Int. J. Mol. Sci 2016, 17, 617. [Google Scholar] [CrossRef]
- Nusbaum, A.G.; Gil, J.; Rippy, M.K.; Warne, B.; Valdes, J.; Claro, A.; Davis, S.C. Effective method to remove wound bacteria: Comparison of various debridement modalities in an in vivo porcine model. J. Surg. Res. 2012, 176, 701–707. [Google Scholar] [CrossRef]
- Lio, P.A.; Kaye, E.T. Topical antibacterial agents. Infect. Dis. Clin. N. Am. 2009, 23, 945–963. [Google Scholar] [CrossRef]
- Arias, C.A.; Murray, B.E. Antibiotic-resistant bugs in the 21st century—A clinical super-challenge. N. Engl. J. Med. 2009, 360, 439–443. [Google Scholar] [CrossRef]
- Boucher, H.W.; Talbot, G.H.; Bradley, J.S.; Edwards, J.E.; Gilbert, D.; Rice, L.B.; Scheld, M.; Spellberg, B.; Bartlett, J. Bad bugs, no drugs: No ESKAPE! An update from the Infectious Diseases Society of America. Clin. Infect. Dis. 2009, 48, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Spellberg, B.; Powers, J.H.; Brass, E.P.; Miller, L.G.; Edwards, J.E., Jr. Trends in antimicrobial drug development: Implications for the future. Clin. Infect. Dis. 2004, 38, 1279–1286. [Google Scholar] [CrossRef]
- Edmondson, M.; Newall, N.; Carville, K.; Smith, J.; Riley, T.V.; Carson, C.F. Uncontrolled, open-label, pilot study of tea tree (Melaleuca alternifolia) oil solution in the decolonisation of methicillin-resistant Staphylococcus aureus positive wounds and its influence on wound healing. Int. Wound J. 2011, 8, 375–384. [Google Scholar] [CrossRef]
- Jenkins, R.; Cooper, R. Improving antibiotic activity against wound pathogens with manuka honey in vitro. PLoS ONE 2012, 7, e45600. [Google Scholar] [CrossRef]
- Davis, S.C.; Li, J.; Gil, J.; Head, C.; Valdes, J.; Glinos, G.D.; Solis, M.; Higa, A.; Pastar, I. Preclinical evaluation of a novel silver gelling fiber dressing on Pseudomonas aeruginosa in a porcine wound infection model. Wound Repair Regen. 2019, 27, 360–365. [Google Scholar] [CrossRef] [PubMed]
- Hadad, I.; Johnstone, B.H.; Brabham, J.G.; Blanton, M.W.; Rogers, P.I.; Fellers, C.; Solomon, J.L.; Merfeld-Clauss, S.; DesRosiers, C.M.; Dynlacht, J.R.; et al. Development of a porcine delayed wound-healing model and its use in testing a novel cell-based therapy. Int J. Radiat. Oncol. Biol. Phys. 2010, 78, 888–896. [Google Scholar] [CrossRef]
- Malmsjo, M.; Ingemansson, R.; Martin, R.; Huddleston, E. Negative-pressure wound therapy using gauze or open-cell polyurethane foam: Similar early effects on pressure transduction and tissue contraction in an experimental porcine wound model. Wound Repair Regen. 2009, 17, 200–205. [Google Scholar] [CrossRef]
- Mokhtari, A.; Gustafsson, R.; Sjogren, J.; Nilsson, J.; Lindstedt, S.; Malmsjo, M.; Ingemansson, R. Haemodynamic effects of -75 mmHg negative pressure therapy in a porcine sternotomy wound model. Int. Wound J. 2009, 6, 48–54. [Google Scholar] [CrossRef] [PubMed]
- Dos Santos, M.R.; Alcaraz-Espinoza, J.J.; da Costa, M.M.; de Oliveira, H.P. Usnic acid-loaded polyaniline/polyurethane foam wound dressing: Preparation and bactericidal activity. Mater. Sci. Eng. C Mater. Biol. Appl. 2018, 89, 33–40. [Google Scholar] [CrossRef]
- Lee, J.W.; Song, K.Y. Evaluation of a polyurethane foam dressing impregnated with 3% povidone-iodine (Betafoam) in a rat wound model. Ann. Surg. Treat. Res. 2018, 94, 1–7. [Google Scholar] [CrossRef]
- Lipsky, B.A.; Hoey, C. Topical antimicrobial therapy for treating chronic wounds. Clin. Infect. Dis. 2009, 49, 1541–1549. [Google Scholar] [CrossRef] [PubMed]
- Krofta, K.; Liskova, H.; Vrabcova, S. Process for Preparing Pure Beta Acids of Hop. CZ303017B6, 29 February 2012. [Google Scholar]
- Elmarsafi, T.; Garwood, C.S.; Steinberg, J.S.; Evans, K.K.; Attinger, C.E.; Kim, P.J. Effect of semiquantitative culture results from complex host surgical wounds on dehiscence rates. Wound Repair Regen. 2017, 25, 210–216. [Google Scholar] [CrossRef]
- Hashimoto, S.; Shime, N. Evaluation of semi-quantitative scoring of Gram staining or semi-quantitative culture for the diagnosis of ventilator-associated pneumonia: A retrospective comparison with quantitative culture. J. Intensive Care 2013, 1, 2. [Google Scholar] [CrossRef] [PubMed]
- Jault, P.; Leclerc, T.; Jennes, S.; Pirnay, J.P.; Que, Y.A.; Resch, G.; Rousseau, A.F.; Ravat, F.; Carsin, H.; Le Floch, R.; et al. Efficacy and tolerability of a cocktail of bacteriophages to treat burn wounds infected by Pseudomonas aeruginosa (PhagoBurn): A randomised, controlled, double-blind phase 1/2 trial. Lancet Infect. Dis. 2019, 19, 35–45. [Google Scholar] [CrossRef]
- Kallstrom, G. Are quantitative bacterial wound cultures useful? J. Clin. Microbiol. 2014, 52, 2753–2756. [Google Scholar] [CrossRef] [PubMed]
- Kilkenny, C.; Browne, W.J.; Cuthi, I.; Emerson, M.; Altman, D.G. Improving bioscience research reporting: The ARRIVE guidelines for reporting animal research. Vet. Clin. Pathol. 2012, 41, 27–31. [Google Scholar] [CrossRef] [PubMed]
- Pejchal, J.; Novotny, J.; Marak, V.; Osterreicher, J.; Tichy, A.; Vavrova, J.; Sinkorova, Z.; Zarybnicka, L.; Novotna, E.; Chladek, J.; et al. Activation of p38 MAPK and expression of TGF-beta1 in rat colon enterocytes after whole body gamma-irradiation. Int. J. Radiat. Biol. 2012, 88, 348–358. [Google Scholar] [CrossRef]
- Pavlik, V.; Sobotka, L.; Pejchal, J.; Cepa, M.; Nesporova, K.; Arenbergerova, M.; Mrozkova, A.; Velebny, V. Silver distribution in chronic wounds and the healing dynamics of chronic wounds treated with dressings containing silver and octenidine. FASEB J. 2021, 35, e21580. [Google Scholar] [CrossRef]
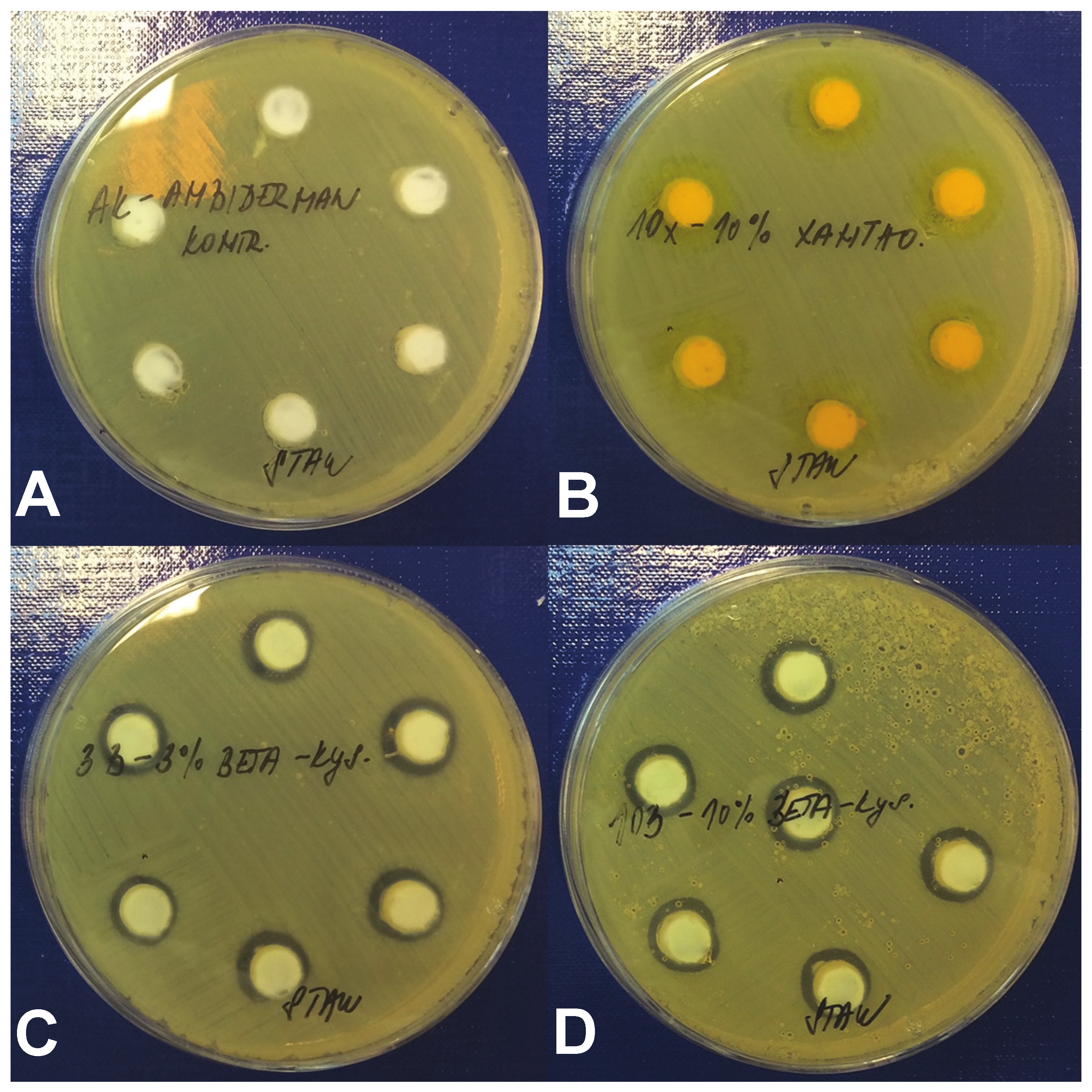


| Tested Compound | Diameter of Inhibition Zone (mm) 1 | ||
|---|---|---|---|
| 3% | 5% | 10% | |
| Beta-acids | 11.2 ± 1.1 | 11.6 ± 1.3 | 12.8 ± 0.8 |
| Xanthohumol | 0 | 0 | 0 |
| Ambiderman | 0 | 0 | 0 |
| Score | 0 | 1 | 2 | 3 |
|---|---|---|---|---|
| Healing of Epithelial Layer | ||||
| Extent of the newly formed layer | Does not Reach the Cutting Edge | On the Cutting Edge | ≤50% of the Wound a | ≥50% of the Wound a |
| Differentiation | none | spinous | granular | |
| Healing of Connective Tissue | ||||
| Amount of Granulation Tissue | profound | moderate | scanty | absent |
| Collagen Fiber Orientation | vertical | mixed | horizontal | |
| Collagen Fiber Pattern | reticular | mixed | fascicle | |
| Amount of Early Collagen | profound | moderate | minimal | absent |
| Amount of Mature Collagen | absent | minimal | moderate | profound |
| Inflammatory Response | ||||
| Inflammatory Infiltrate | Plenty | Moderate | Mild | A few |
| Presence of MicroAbscesses | ≥2 | 1 | none | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sleha, R.; Radochova, V.; Malis, J.; Mikyska, A.; Houska, M.; Krofta, K.; Bogdanova, K.; Janovska, S.; Pejchal, J.; Kolar, M.; et al. Strong Antimicrobial and Healing Effects of Beta-Acids from Hops in Methicillin-Resistant Staphylococcus aureus-Infected External Wounds In Vivo. Antibiotics 2021, 10, 708. https://doi.org/10.3390/antibiotics10060708
Sleha R, Radochova V, Malis J, Mikyska A, Houska M, Krofta K, Bogdanova K, Janovska S, Pejchal J, Kolar M, et al. Strong Antimicrobial and Healing Effects of Beta-Acids from Hops in Methicillin-Resistant Staphylococcus aureus-Infected External Wounds In Vivo. Antibiotics. 2021; 10(6):708. https://doi.org/10.3390/antibiotics10060708
Chicago/Turabian StyleSleha, Radek, Vera Radochova, Jiri Malis, Alexander Mikyska, Milan Houska, Karel Krofta, Katerina Bogdanova, Sylva Janovska, Jaroslav Pejchal, Milan Kolar, and et al. 2021. "Strong Antimicrobial and Healing Effects of Beta-Acids from Hops in Methicillin-Resistant Staphylococcus aureus-Infected External Wounds In Vivo" Antibiotics 10, no. 6: 708. https://doi.org/10.3390/antibiotics10060708
APA StyleSleha, R., Radochova, V., Malis, J., Mikyska, A., Houska, M., Krofta, K., Bogdanova, K., Janovska, S., Pejchal, J., Kolar, M., Cermak, P., & Bostik, P. (2021). Strong Antimicrobial and Healing Effects of Beta-Acids from Hops in Methicillin-Resistant Staphylococcus aureus-Infected External Wounds In Vivo. Antibiotics, 10(6), 708. https://doi.org/10.3390/antibiotics10060708








