Prevalence of Vancomycin-Resistant Enterococcus (VRE) in Companion Animals: The First Meta-Analysis and Systematic Review
Abstract
1. Introduction
2. Results
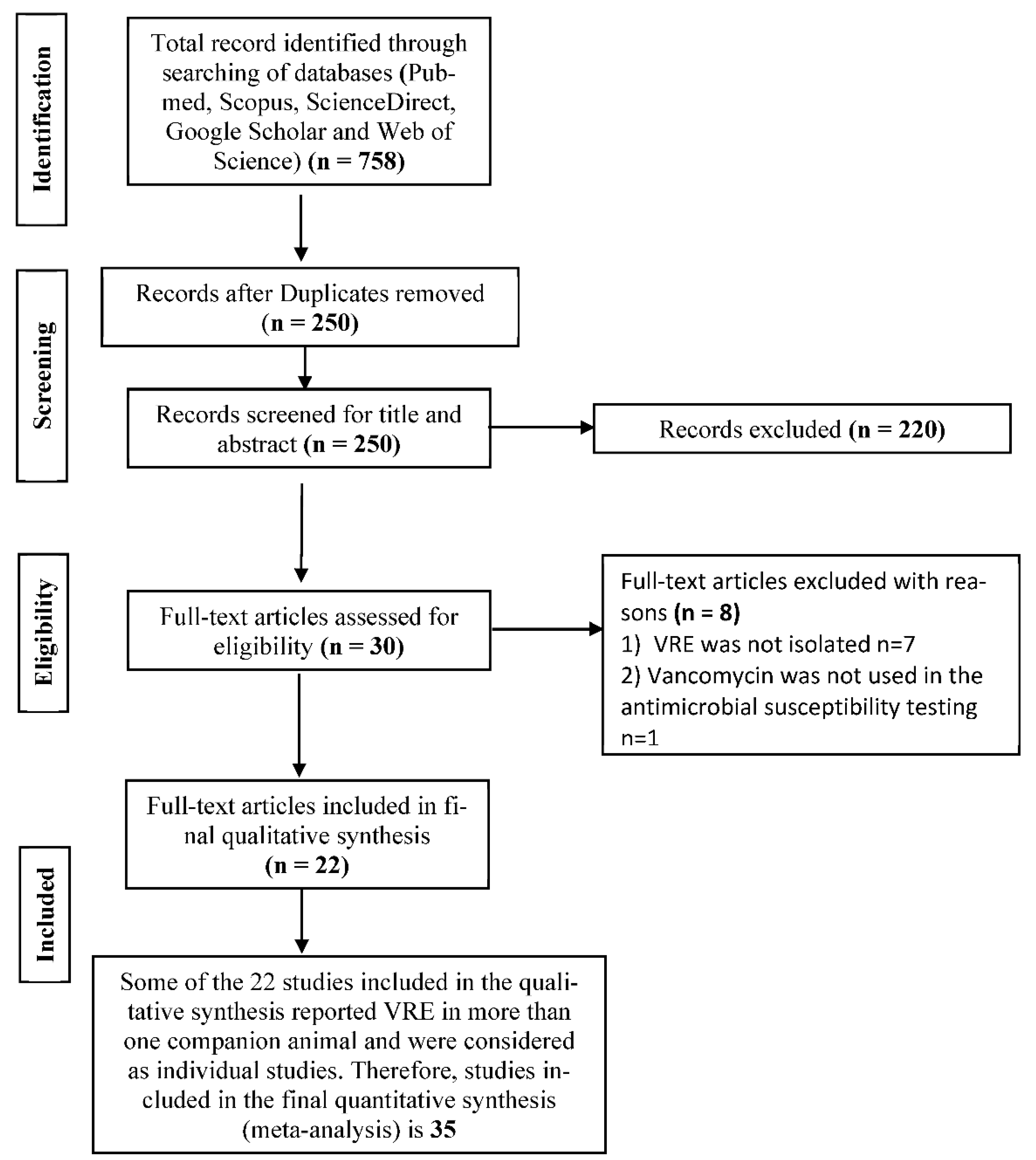
2.1. Search Results and Eligible Studies
2.2. The Pooled Prevalence of VRE in Companion Animals
2.3. Subgroup Meta-Analysis
2.4. Meta-Regression
3. Discussion
4. Materials and Methods
4.1. Study Design and Protocol
4.2. Literature Review
4.3. Inclusion and Exclusion Criteria for Studies
4.4. Data Extraction
4.5. Study Quality Assessment
4.6. Data Analysis
4.7. Bias and Heterogeneity Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wada, Y.; Harun, A.B.; Yean, C.Y.; Zaidah, A.R. Vancomycin-resistant Enterococcus: Issues in human health, animal health, resistant mechanisms and the Malaysian paradox. Adv. Anim. Vet. Sci. 2019, 7, 1021–1034. [Google Scholar] [CrossRef]
- García-Solache, M.; Rice, L.B. The enterococcus: A model of adaptability to its environment. Clin. Microbiol. Rev. 2019, 32. [Google Scholar] [CrossRef] [PubMed]
- Delpech, G.; Allende, L.G.; Sparo, M. Mobile Genetic Elements in Vancomycin-Resistant Enterococcus faecium Population; IntechOpen: London, UK, 2019. [Google Scholar] [CrossRef][Green Version]
- Fiore, E.; Van Tyne, D.; Gilmore, M.S. Pathogenicity of Enterococci. Microbiol. Spectr. 2019, 7. [Google Scholar] [CrossRef] [PubMed]
- Buetti, N.; Wassilew, N.; Rion, V.; Senn, L.; Gardiol, C.; Widmer, A.; Marschall, J. Emergence of vancomycin-resistant enterococci in Switzerland: A nation-wide survey. Antimicrob. Resist. Infect. Control 2019, 8, 16. [Google Scholar] [CrossRef]
- Bager, F.; Madsen, M.; Christensen, J.; Aarestrup, F.M. Avoparcin used as a growth promoter is associated with the occurrence of vancomycin-resistant Enterococcus Faecium on Danish poultry and pig farms. Prev. Vet. Med. 1997, 31, 95–112. [Google Scholar] [CrossRef]
- Werner, G.; Neumann, B.; Weber, R.E.; Kresken, M.; Wendt, C.; Bender, J.K.; Becker, K.; Borgmann, S.; Diefenbach, A.; Hamprecht, A.; et al. Thirty years of VRE in Germany—“Expect the unexpected”: The view from the national reference centre for staphylococci and enterococci. Drug Resist. Updates 2020, 100732. [Google Scholar] [CrossRef]
- Ünal, N.; Bal, E.; Karagöz, A.; Altun, B.; Koçak, N. Detection of vancomycin-resistant enterococci in samples from broiler flocks and houses in Turkey. Acta Vet. Hung. 2020, 68, 117–122. [Google Scholar] [CrossRef]
- Ahmed, M.O.; Baptiste, K.E. Vancomycin-resistant enterococci: A review of antimicrobial resistance mechanisms and perspectives of human and animal health. Microb. Drug Resist. 2018, 24, 590–606. [Google Scholar] [CrossRef]
- Pomba, C.; Rantala, M.; Greko, C.; Baptiste, K.E.; Catry, B.; van Duijkeren, E.; Mateus, A.; Moreno, M.A.; Pyörälä, S.; Ružauskas, M.; et al. Public health risk of antimicrobial resistance transfer from companion animals. J. Antimicrob. Chemother. 2017, 72, 957–968. [Google Scholar] [CrossRef]
- Muloi, D.; Ward, M.J.; Pedersen, A.B.; Fèvre, E.M.; Woolhouse, M.E.J.; Van Bunnik, B.A.D. Are food animals responsible for transfer of antimicrobial-resistant Escherichia Coli or their resistance determinants to human populations? A systematic review. Foodborne Pathog. Dis. 2018, 15, 467–474. [Google Scholar] [CrossRef]
- Carvalho, I.; Alonso, C.A.; Silva, V.; Pimenta, P.; Cunha, R.; Martins, C.; Igrejas, G.; Torres, C.; Poeta, P. Extended-spectrum beta-lactamase-producing Klebsiella Pneumoniae isolated from healthy and sick dogs in Portugal. Microb. Drug Resist. 2020, 26, 709–715. [Google Scholar] [CrossRef] [PubMed]
- Belas, A.; Menezes, J.; Gama, L.T.; Pomba, C. Sharing of clinically important antimicrobial resistance genes by companion animals and their human household members. Microb. Drug Resist. 2020, 26, 1174–1185. [Google Scholar] [CrossRef] [PubMed]
- Joosten, P.; Ceccarelli, D.; Odent, E.; Sarrazin, S.; Graveland, H.; Van Gompel, L.; Battisti, A.; Caprioli, A.; Franco, A.; Wagenaar, J.A.; et al. Antimicrobial usage and resistance in companion animals: A cross-sectional study in three European countries. Antibiotics 2020, 9, 87. [Google Scholar] [CrossRef]
- Thépault, A.; Rose, V.; Queguiner, M.; Chemaly, M.; Rivoal, K. Dogs and cats: Reservoirs for highly diverse Campylobacter Jejuni and a potential source of human exposure. Animals 2020, 10, 838. [Google Scholar] [CrossRef] [PubMed]
- Sfaciotte, R.A.P.; Parussolo, L.; Melo, F.D.; Wildemann, P.; Bordignon, G.; Israel, N.D.; Leitzke, M.; Wosiacki, S.R.; Salbego, F.Z.; da Costa, U.M.; et al. Identification and characterization of multidrug-resistant extended-spectrum beta-lactamase-producing bacteria from healthy and diseased dogs and cats admitted to a veterinary hospital in Brazil. Microb. Drug Resist. 2020. [Google Scholar] [CrossRef] [PubMed]
- Devriese, L.A.; Ieven, M.; Goossens, H.; Vandamme, P.; Pot, B.; Hommez, J.; Haesebrouck, F. Presence of vancomycin-resistant enterococci in farm and pet animals. Antimicrob. Agents Chemother. 1996, 40, 2285–2287. [Google Scholar] [CrossRef]
- van Belkun, A.; van den Braak, N.; Thomassen, R.; Verbrugh, H.; Endtz, H. Vancomycin-resistant enterococci in cats and dogs. Lancet 1996, 348, 1038–1039. [Google Scholar] [CrossRef]
- Simjee, S.; White, D.G.; McDermott, P.F.; Wagner, D.D.; Zervos, M.J.; Donabedian, S.M.; English, L.L.; Hayes, J.R.; Walker, R.D. Characterization of Tn1546 in vancomycin-resistant Enterococcus Faecium isolated from canine urinary tract infections: Evidence of gene exchange between human and animal enterococci. J. Clin. Microbiol. 2002, 40, 4659–4665. [Google Scholar] [CrossRef]
- Herrero, I.A.; Fernández-Garayzábal, J.F.; Moreno, M.A.; Domínguez, L. Dogs should be included in surveillance programs for vancomycin-resistant enterococci. J. Clin. Microbiol. 2004, 42, 1384–1385. [Google Scholar] [CrossRef]
- Thongchai Chalermchaikit (Chulalongkorn University, Bangkok (Thailand)). Prevalence of Vancomycin-Resistant Enterococci in Dogs and Cats in Khon Kaen Province. Available online: https://agris.fao.org/agris-search/search.do?recordID=TH2005001433 (accessed on 20 December 2020).
- de Niederhäusern, S.; Sabia, C.; Messi, P.; Guerrieri, E.; Manicardi, G.; Bondi, M. VanA-type vancomycin-resistant enterococci in equine and swine rectal swabs and human clinical samples. Curr. Microbiol. 2007, 55, 240–246. [Google Scholar] [CrossRef]
- Singh, B.R. Prevalence of vancomycin resistance and multiple drug resistance in enterococci in equids in North India. J. Infect. Dev. Ctries. 2009, 3, 498–503. [Google Scholar] [CrossRef] [PubMed]
- Siriwattanachai, K.; Chalermchaikit, T.; Lertworapreecha, N.; Angkititrakul, S.; Suriyasathaporn, W. Prevalence of Vancomycin-resistant Enterococci (VRE) in companion dogs and cats in Thailand. In Proceedings of the 8th Chulalongkorn University Veterinary Annual Conference, Bangkok, Thailand, 3 April 2009; p. 82. [Google Scholar]
- Ahmed, M.O.; Clegg, P.D.; Williams, N.J.; Baptiste, K.E.; Bennett, M. Vancomycin-Resistant Enterococci (VRE) in Equine-Faecal Samples. In Science and Technology Against Microbial Pathogens: Research, Development and Evaluation, Proceedings of the International Conference on Antimicrobial Research (ICAR2010), Valladolid, Spain, 3–5 November 2010; World Scientific Publishing Co Pte Ltd.: Singapore, 2011; pp. 357–362. [Google Scholar]
- Gonçalves, A.; Poeta, P.; Silva, N.; Araújo, C.; López, M.; Ruiz, E.; Uliyakina, I.; Direitinho, J.; Igrejas, G.; Torres, C. Characterization of vancomycin-resistant enterococci isolated from fecal samples of ostriches by molecular methods. Foodborne Pathog. Dis. 2010, 7, 1133–1136. [Google Scholar] [CrossRef] [PubMed]
- Ghosh, A.; KuKanich, K.; Brown, C.E.; Zurek, L. Resident cats in small animal veterinary hospitals carry multi-drug resistant enterococci and are likely involved in cross-contamination of the hospital environment. Front. Microbiol. 2012, 3, 62. [Google Scholar] [CrossRef] [PubMed]
- Kataoka, Y.; Umino, Y.; Ochi, H.; Harada, K.; Sawada, T. Antimicrobial susceptibility of enterococcal species isolated from antibiotic-treated dogs and cats. J. Vet. Med. Sci. 2014, 76, 1399–1402. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Bağcığil, A.; Ikiz, S.; Ak, S.; Özgür, N. Isolation of vancomycin-resistant enterococci from animal faeces, detection of antimicrobial resistance profiles and vancomycin-resistant genes. Kafkas Üniversitesi Vet. Fakültesi Derg. 2015, 21, 87–94. [Google Scholar]
- Gulhan, T.; Boynukara, B.; Ciftci, A.; Sogut, M.U.; Findik, A. Characterization of enterococcus faecalis isolates originating from different sources for their virulence factors and genes, antibiotic resistance patterns, genotypes and biofilm production. Iran. J. Vet. Res. 2015, 16, 261–266. [Google Scholar] [CrossRef]
- Bağcigil, A.F.; Koenhemsi, L.; Çelik, B.; Metiner, K.; Or, M.E.; Ak, S. Kedi ve köpek rektal svablarindan izole edilen Vankomisin Dirençli Enterokokların (VRE) araştirilmasi. İstanbul Univ. Vet. Fakültesi Derg. 2016, 42. [Google Scholar] [CrossRef]
- Pasotto, D.; Dotto, G.; Menandro, M.L.; Mondin, A.; Martini, M. Prevalence and antimicrobial-resistance characterization of Vancomycin-Resistant Enterococci (VRE) strain in healthy household dogs in Italy. Int. J. Infect. Dis. 2016, 53, 50. [Google Scholar] [CrossRef][Green Version]
- Aslantaş, Ö.; Tek, E. Isolation of ampicillin and vancomycin-resistant Enterococcus Faecium from dogs and cats. Kafkas Univ. Vet. Fak. Derg. 2019, 25, 263–269. [Google Scholar] [CrossRef]
- van den Bunt, G.; Top, J.; Hordijk, J.; de Greeff, S.C.; Mughini-Gras, L.; Corander, J.; van Pelt, W.; Bonten, M.J.M.; Fluit, A.C.; Willems, R.J.L. Intestinal carriage of ampicillin- and vancomycin-resistant Enterococcus Faecium in humans, dogs and cats in The Netherlands. J. Antimicrob. Chemother. 2018, 73, 607–614. [Google Scholar] [CrossRef]
- Anyanwu, M.U.; Okorie-Kanu, O.J.; Ogugua, A.J.; Ezenduka, E.V.; Anidebe, C.O. Occurrence, antibiogram and vancomycin resistance of generic enterococci in horses in Nigeria. Revue Méd. Vét 2019, 170, 46–52. [Google Scholar]
- Cabral, B.G.; Davies, Y.M.; Menão, M.C.; Saidenberg, A.B.S.; Gomes, V.T.M.; Moreno, L.Z.; Sato, M.I.Z.; Moreno, A.M.; Knöbl, T. Companion psittacine birds as reservoir of gentamicin and vancomycin-resistant Enterococcus Spp. Pesqui. Vet. Bras. 2020, 40, 129–133. [Google Scholar] [CrossRef]
- Iseppi, R.; Di Cerbo, A.; Messi, P.; Sabia, C. Antibiotic resistance and virulence traits in Vancomycin-Resistant Enterococci (VRE) and extended-spectrum β-Lactamase/AmpC-Producing (ESBL/AmpC) Enterobacteriaceae from humans and pets. Antibiotics 2020, 9, 152. [Google Scholar] [CrossRef] [PubMed]
- Wagenvoort, J.H.T. Absence of Vancomycin-Resistant Enterococci (VRE) in companion dogs in the conurbation of Parkstad Limburg, The Netherlands. J. Antimicrob. Chemother. 2003, 52, 532. [Google Scholar] [CrossRef] [PubMed]
- Manson, J.M.; Keis, S.; Smith, J.M.B.; Cook, G.M. Characterization of a Vancomycin-Resistant Enterococcus Faecalis (VREF) isolate from a dog with mastitis: Further evidence of a clonal lineage of VREF in New Zealand. J. Clin. Microbiol. 2003, 41, 3331–3333. [Google Scholar] [CrossRef][Green Version]
- Wada, Y.; Harun, A.B.; Yean, C.Y.; Zaidah, A.R. Vancomycin-Resistant Enterococci (VRE) in Nigeria: The first systematic review and meta-analysis. Antibiotics 2020, 9, 565. [Google Scholar] [CrossRef] [PubMed]
- Piezzi, V.; Gasser, M.; Atkinson, A.; Kronenberg, A.; Vuichard-Gysin, D.; Harbarth, S.; Marschall, J.; Buetti, N. Increasing proportion of vancomycin resistance among enterococcal bacteraemias in Switzerland: A 6-year nation-wide surveillance, 2013 to 2018. Eurosurveillance 2020, 25, 1900575. [Google Scholar] [CrossRef]
- Nobrega, D.B.; Tang, K.L.; Caffrey, N.P.; De Buck, J.; Cork, S.C.; Ronksley, P.E.; Polachek, A.J.; Ganshorn, H.; Sharma, N.; Kastelic, J.P.; et al. Prevalence of antimicrobial resistance genes and its association with restricted antimicrobial use in food-producing animals: A systematic review and meta-analysis. J. Antimicrob. Chemother. 2020. [Google Scholar] [CrossRef]
- European Food Safety Authority (EFSA). ECDC, EFSA and EMA joint scientific opinion on a list of outcome indicators as regards surveillance of antimicrobial resistance and antimicrobial consumption in humans and food-producing animals. EFSA J. 2017, 15, 5017. [Google Scholar] [CrossRef]
- Sabença, C.; de Sousa, T.; Oliveira, S.; Viala, D.; Théron, L.; Chambon, C.; Hébraud, M.; Beyrouthy, R.; Bonnet, R.; Caniça, M.; et al. Next-generation sequencing and MALDI Mass spectrometry in the study of multiresistant processed meat Vancomycin-Resistant Enterococci (VRE). Biology 2020, 9, 89. [Google Scholar] [CrossRef]
- Klees, S.; Effelsberg, N.; Stührenberg, B.; Mellmann, A.; Schwarz, S.; Köck, R. Prevalence and epidemiology of multidrug-resistant pathogens in the food chain and the urban environment in Northwestern Germany. Antibiotics 2020, 9, 708. [Google Scholar] [CrossRef] [PubMed]
- Bennani, H.; Mateus, A.; Mays, N.; Eastmure, E.; Stärk, K.D.C.; Häsler, B. Overview of evidence of antimicrobial use and antimicrobial resistance in the food chain. Antibiotics 2020, 9, 49. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Chu, L.; Wojnárovits, L.; Takács, E. Occurrence and fate of antibiotics, Antibiotic-Resistant Genes (ARGs) and Antibiotic-Resistant Bacteria (ARB) in municipal wastewater treatment plant: An overview. Sci. Total Environ. 2020, 744, 140997. [Google Scholar] [CrossRef] [PubMed]
- ElFeky, D.S.; Awad, A.R.; Elshobaky, M.A.; Elawady, B.A. Effect of ceftaroline, vancomycin, gentamicin, macrolides, and ciprofloxacin against methicillin-resistant Staphylococcus Aureus isolates: An in vitro study. Surg. Infect. (Larchmt.) 2020, 21, 150–157. [Google Scholar] [CrossRef] [PubMed]
- Hubbard, L.E.; Givens, C.E.; Griffin, D.W.; Iwanowicz, L.R.; Meyer, M.T.; Kolpin, D.W. Poultry litter as potential source of pathogens and other contaminants in groundwater and surface water proximal to large-scale confined poultry feeding operations. Sci. Total Environ. 2020, 735, 139459. [Google Scholar] [CrossRef]
- Zainab, S.M.; Junaid, M.; Xu, N.; Malik, R.N. Antibiotics and Antibiotic-Resistant Genes (ARGs) in groundwater: A global review on dissemination, sources, interactions, environmental and human health risks. Water Res. 2020, 187, 116455. [Google Scholar] [CrossRef]
- Vendrik, K.E.W.; Terveer, E.M.; Kuijper, E.J.; Nooij, S.; Boeije-Koppenol, E.; Sanders, I.M.J.G.; van Lingen, E.; Verspaget, H.W.; Berssenbrugge, E.K.L.; Keller, J.J.; et al. Periodic screening of donor faeces with a quarantine period to prevent transmission of multidrug-resistant organisms during faecal microbiota transplantation: A retrospective cohort study. Lancet Infect. Dis. 2020. [Google Scholar] [CrossRef]
- Bassis, C.M.; Moore, N.M.; Lolans, K.; Seekatz, A.M.; Weinstein, R.A.; Young, V.B.; Hayden, M.K. Comparison of stool versus rectal swab samples and storage conditions on bacterial community profiles. BMC Microbiol. 2017, 17, 78. [Google Scholar] [CrossRef]
- Biehl, L.M.; Garzetti, D.; Farowski, F.; Ring, D.; Koeppel, M.B.; Rohde, H.; Schafhausen, P.; Stecher, B.; Vehreschild, M.J.G.T. Usability of rectal swabs for microbiome sampling in a cohort study of hematological and oncological patients. PLoS ONE 2019, 14, e0215428. [Google Scholar] [CrossRef]
- Carroll, I.M.; Ringel-Kulka, T.; Siddle, J.P.; Klaenhammer, T.R.; Ringel, Y. Characterization of the fecal microbiota using high-throughput sequencing reveals a stable microbial community during storage. PLoS ONE 2012, 7, e46953. [Google Scholar] [CrossRef]
- Fouhy, F.; Deane, J.; Rea, M.C.; O’Sullivan, Ó.; Ross, R.P.; O’Callaghan, G.; Plant, B.J.; Stanton, C. The effects of freezing on faecal microbiota as determined using MiSeq sequencing and culture-based investigations. PLoS ONE 2015, 10, e0119355. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.; Hofstaedter, C.E.; Zhao, C.; Mattei, L.; Tanes, C.; Clarke, E.; Lauder, A.; Sherrill-Mix, S.; Chehoud, C.; Kelsen, J.; et al. Optimizing methods and dodging pitfalls in microbiome research. Microbiome 2017, 5, 52. [Google Scholar] [CrossRef] [PubMed]
- Artim, S.C.; Sheh, A.; Burns, M.A.; Fox, J.G. Evaluating rectal swab collection method for gut microbiome analysis in the common marmoset (Callithrix Jacchus). PLoS ONE 2019, 14, e0224950. [Google Scholar] [CrossRef] [PubMed]
- McKenna, P.; Hoffmann, C.; Minkah, N.; Aye, P.P.; Lackner, A.; Liu, Z.; Lozupone, C.A.; Hamady, M.; Knight, R.; Bushman, F.D. The macaque gut microbiome in health, lentiviral infection, and chronic enterocolitis. PLoS Pathog. 2008, 4, e20. [Google Scholar] [CrossRef] [PubMed]
- Yasuda, K.; Oh, K.; Ren, B.; Tickle, T.L.; Franzosa, E.A.; Wachtman, L.M.; Miller, A.D.; Westmoreland, S.V.; Mansfield, K.G.; Vallender, E.J.; et al. Biogeography of the intestinal mucosal and lumenal microbiome in the rhesus macaque. Cell Host Microbe 2015, 17, 385–391. [Google Scholar] [CrossRef]
- Jensen, B.J. Screening specimens for vancomycin-resistant enterococcus. Lab. Med. 1996, 27, 53–55. [Google Scholar] [CrossRef][Green Version]
- van Horn, K.G.; Gedris, C.A.; Rodney, K.M. Selective isolation of vancomycin-resistant enterococci. J. Clin. Microbiol. 1996, 34, 924–927. [Google Scholar] [CrossRef]
- Tenover, F.C.; Tokars, J.; Swenson, J.; Paul, S.; Spitalny, K.; Jarvis, W. Ability of clinical laboratories to detect antimicrobial agent-resistant enterococci. J. Clin. Microbiol. 1993, 31, 1695–1699. [Google Scholar] [CrossRef]
- Jett, B.; Free, L.; Sahm, D.F. Factors influencing the vitek gram-positive susceptibility system’s detection of vanb-encoded vancomycin resistance among enterococci. J. Clin. Microbiol. 1996, 34, 701–706. [Google Scholar] [CrossRef]
- Shamseer, L.; Moher, D.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A.; Altman, D.G.; Booth, A.; et al. Preferred reporting items for systematic review and meta-analysis protocols (Prisma-p) 2015: Elaboration and explanation. BMJ 2015, 350, g7647. [Google Scholar] [CrossRef]
- Joanna Briggs Institute (JBI). Checklist for Prevalence Studies; Joanna Briggs Institute: Adelaide, Australia, 2017. [Google Scholar]
- George, B.J.; Aban, I.B. An application of meta-analysis based on DerSimonian and laird method. J. Nucl. Cardiol. 2016, 23, 690–692. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.T.; Thompson, S.G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002, 21, 1539–1558. [Google Scholar] [CrossRef] [PubMed]
- Wallace, B.C.; Dahabreh, I.J.; Trikalinos, T.A.; Lau, J.; Trow, P.; Schmid, C.H. Closing the gap between methodologists and end-users: R as a computational back-end. J. Stat. Softw. 2012, 49, 1–15. [Google Scholar] [CrossRef]
- Comprehensive Meta-Analysis Software (CMA). Available online: https://www.meta-analysis.com/ (accessed on 21 December 2020).


| S/No | Author, Publication Year | Sampling Period | Country | Companion Animal | Sample Size | Number Positive | Prevalence (%) | Detection Method | Sample Type | Study Design |
|---|---|---|---|---|---|---|---|---|---|---|
| 1a | Devriese et al., 1996 [17] | 1995 | Belgium | Dog | 49 | 4 | 8.16 | Enrichment culture | Fecal | Cross-sectional |
| 1b | Devriese et al., 1996 [17] | 1995 | Belgium | Cat | 21 | 1 | 4.76 | Enrichment culture | Fecal | Cross-sectional |
| 1c | Devriese et al., 1996 [17] | 1995 | Belgium | Horse | 83 | 8 | 9.64 | Enrichment culture | Fecal | Cross-sectional |
| 1d | Devriese et al., 1996 [17] | 1995 | Belgium | Rabbit | 33 | 1 | 3.03 | Enrichment culture | Fecal | Cross-sectional |
| 1e | Devriese et al., 1996 [17] | 1995 | Belgium | Pheasants | 14 | 2 | 14.29 | Enrichment culture | Fecal | Cross-sectional |
| 2a | van Belkum et al., 1996 [18] | 1996 | Netherlands | Dog | 23 | 11 | 48 | Selective culture | Rectal swab | Cross-sectional |
| 2b | van Belkum et al., 1996 [18] | 1996 | Netherlands | Cat | 24 | 4 | 16 | Selective culture | Rectal swab | Cross-sectional |
| 3 | Simjee et al., 2002 [19] | 1996–1998 | United States of America | Dog | 35 | 16 | 45.71 | Broth microdilution | Urine | Cross-sectional |
| 4 | Herrero et al., 2004 [20] | 1998–2003 | Spain | Dog | 87 | 15 | 17.24 | Sensititre system | Fecal | Cross-sectional |
| 5a | Chalermchaikit et al., 2005 [21] | - | Thailand | Dog | 210 | 41 | 19.5 | Agar dilution | Fecal | Cross-sectional |
| 5b | Chalermchaikit et al., 2005 [21] | - | Thailand | Cat | 114 | 26 | 22.8 | Agar dilution | Fecal | Cross-sectional |
| 6a | Chalermchaikit et al., 2005 [21] | - | Thailand | Dog | 209 | 13 | 6.22 | Agar dilution | Fecal | Cross-sectional |
| 6b | Chalermchaikit et al., 2005 [21] | - | Thailand | Cat | 121 | 9 | 7.44 | Agar dilution | Fecal | Cross-sectional |
| 7 | de Niederhausern et al., 2007 [22] | 2005 | Italy | Horse | 104 | 7 | 6.73 | Agar dilution | Fecal | Cross-sectional |
| 8 | Singh, 2009 [23] | 2008 | India | Horse | 267 | 214 | 80.2 | Disc diffusion | Fecal | Cross-sectional |
| 9a | Siriwattanachai et al., 2009 [24] | 2003–2004 | Thailand | Dog | 324 | 299 | 92.28 | Agar dilution | Fecal | Cross-sectional |
| 9b | Siriwattanachai et al., 2009 [24] | 2003–2004 | Thailand | Cat | 330 | 292 | 88.48 | Agar dilution | Fecal | Cross-sectional |
| 10 | Ahmed et al., 2011 [25] | 2010 | United Kingdom | Horse | 264 | 9 | 3.41 | Enrichment agar | Fecal | Cross-sectional |
| 11 | Goncalves et al., 2010 [26] | - | Portugal | Ostrich | 54 | 7 | 13.0 | Disc diffusion | Fecal | Cross-sectional |
| 12 | Ghosh et al., 2012 [27] | - | United States of America | Cat | 180 | 7 | 3.89 | Disc diffusion | Fecal | Cross-sectional |
| 13 | Kataoka et al., 2014 [28] | 2011–2012 | Japan | Dog | 77 | 4 | 5.19 | Broth microdilution | Fecal | Cross-sectional |
| 14a | Bagcigil et al., 2015 [29] | - | Turkey | Dog | 100 | 20 | 20.0 | Broth microdilution | Fecal | Cross-sectional |
| 14b | Bagcigil et al., 2015 [29] | - | Turkey | Cat | 100 | 17 | 17.0 | Broth microdilution | Fecal | Cross-sectional |
| 15 | Gulhan et al., 2015 [30] | - | Turkey | Dog | 26 | 1 | 3.85 | Disc diffusion | Fecal | Cross-sectional |
| 16a | Bagcigil et al., 2016 [31] | 2015 | Turkey | Dog | 86 | 12 | 13.95 | Disc diffusion | Fecal | Cross-sectional |
| 16b | Bagcigil et al., 2016 [31] | 2015 | Turkey | Cat | 71 | 8 | 11.27 | Disc diffusion | Fecal | Cross-sectional |
| 17 | Pasotto et al., 2016 [32] | - | Italy | Dog | 170 | 84 | 49.41 | Disc diffusion | Fecal | Cross-sectional |
| 18a | Aslantas and Tek, 2019 [33] | 2018 | Turkey | Dog | 276 | 1 | 0.13 | Disc diffusion | Rectal swab | Cross-sectional |
| 18b | Aslantas and Tek, 2019 [33] | 2018 | Turkey | Cat | 255 | 2 | 0.8 | Disc diffusion | Rectal swab | Cross-sectional |
| 19a | van den Bunt et al., 2018 [34] | 2014–2015 | Netherlands | Dog | 277 | 71 | 25.63 | Enrichment culture | Fecal | Cross-sectional |
| 19b | van den Bunt et al., 2018 [34] | 2014–2015 | Netherlands | Cat | 118 | 6 | 5.08 | Enrichment culture | Fecal | Cross-sectional |
| 20 | Anyanwu et al., 2019 [35] | 2018 | Nigeria | Horse | 30 | 7 | 23.3 | Disc diffusion | Rectal swab | Cross-sectional |
| 21 | Cabral et al., 2020 [36] | - | Brazil | Parrots | 36 | 2 | 5.5 | Disc diffusion | Cloacal swab | Cross-sectional |
| 22a | Issepi et al., 2020 [37] | 2017 | Italy | Dog | 48 | 3 | 6.25 | Broth microdilution | Fecal | Cross-sectional |
| 22b | Issepi et al., 2020 [37] | 2017 | Italy | Cat | 72 | 17 | 23.6 | Broth microdilution | Fecal | Cross-sectional |
| Sampling Period | Number of Studies | Prevalence (%) | 95% CI | I2 (%) | Q | Heterogeneity Test | |
|---|---|---|---|---|---|---|---|
| DF | p | ||||||
| 1995 | 5 | 8.6 | 5.3–13.6 | 0.00 | 2.245 | 4 | 0.691 |
| 1996 | 2 | 30.9 | 9.1–66.4 | 79.539 | 4.887 | 1 | 0.027 |
| 1996–1998 | 1 | 45.7 | 30.2–62.1 | 0.00 | 0.00 | 0 | 1.00 |
| 1998–2003 | 1 | 17.2 | 10.7–26.7 | 0.00 | 0.00 | 0 | 1.00 |
| 2003–2004 | 2 | 90.4 | 86.0–93.6 | 62.658 | 2.678 | 1 | 0.102 |
| 2005 | 1 | 6.7 | 3.2–13.5 | 0.00 | 0.00 | 0 | 1.00 |
| 2008 | 1 | 80.1 | 74.9–84.5 | 0.00 | 0.00 | 0 | 1.00 |
| 2010 | 1 | 3.4 | 1.8–6.4 | 0.00 | 0.00 | 0 | 1.00 |
| 2011-2012 | 1 | 5.2 | 2.0–13.0 | 0.00 | 0.00 | 0 | 1.00 |
| 2014-2015 | 2 | 12.4 | 2.2–46.7 | 94.386 | 17.814 | 1 | 0.00 |
| 2015 | 2 | 12.8 | 8.4–19.0 | 0.00 | 0.252 | 1 | 0.616 |
| 2017 | 2 | 13.6 | 3.4–41.2 | 81.616 | 5.440 | 1 | 0.020 |
| 2018 | 3 | 2.2 | 0.1–30.8 | 93.266 | 29.701 | 2 | 0.00 |
| Companion Animal | Number of Studies | Prevalence (%) | 95% CI | I2 (%) | Q | Heterogeneity Test | |
|---|---|---|---|---|---|---|---|
| DF | p | ||||||
| Cat | 11 | 12.3 | 3.8–33.1 | 97.654 | 424.639 | 10 | 0.00 |
| Dog | 15 | 18.2 | 9.4–32.5 | 96.745 | 430.158 | 14 | 0.00 |
| Horse | 5 | 16.9 | 2.2–65.3 | 98.505 | 267.595 | 4 | 0.00 |
| Ostrich | 1 | 13.0 | 6.3–24.8 | 0.00 | 0.00 | 0 | 1.00 |
| Parrot | 1 | 5.6 | 1.4–19.7 | 0.00 | 0.00 | 0 | 1.00 |
| Pheasant | 1 | 14.3 | 3.6–42.7 | 0.00 | 0.00 | 0 | 1.00 |
| Rabbit | 1 | 3.0 | 0.4–18.6 | 0.00 | 0.00 | 0 | 1.00 |
| Country | Number of Studies | Prevalence (%) | 95% CI | I2 (%) | Q | Heterogeneity Test | |
|---|---|---|---|---|---|---|---|
| DF | p | ||||||
| Belgium | 5 | 8.6 | 5.3–13.6 | 0.00 | 2.245 | 4 | 0.691 |
| Brazil | 1 | 5.6 | 1.4–19.7 | 0.00 | 0.00 | 0 | 1.00 |
| India | 1 | 80.1 | 74.9–84.5 | 0.00 | 0.00 | 0 | 1.00 |
| Italy | 4 | 17.2 | 5.3–43.4 | 94.801 | 57.703 | 3 | 0.00 |
| Japan | 1 | 5.2 | 2.0–13.0 | 0.00 | 0.00 | 0 | 1.00 |
| Netherlands | 4 | 19.8 | 8.3–40.2 | 88.249 | 25.529 | 3 | 0.00 |
| Nigeria | 1 | 23.3 | 11.6–41.5 | 0.00 | 0.00 | 0 | 1.00 |
| Portugal | 1 | 13.0 | 6.3–24.8 | 0.00 | 0.00 | 0 | 1.00 |
| Spain | 1 | 17.2 | 10.7–26.7 | 0.00 | 0.00 | 0 | 1.00 |
| Thailand | 6 | 36.6 | 8.8–77.5 | 99.040 | 520.613 | 5 | 0.00 |
| Turkey | 7 | 7.2 | 3.4–14.5 | 84.383 | 38.421 | 6 | 0.00 |
| United Kingdom | 1 | 3.4 | 1.8–6.4 | 0.00 | 0.00 | 0 | 1.00 |
| United States of America | 2 | 15.7 | 0.9–78.4 | 97.137 | 34.934 | 1 | 0.00 |
| Sample Types | Number of Studies | Prevalence (%) | 95% CI | I2 (%) | Q | Heterogeneity Test | |
|---|---|---|---|---|---|---|---|
| DF | p | ||||||
| Cloacal swab | 1 | 5.5 | 1.4–19.7 | 0.00 | 0.00 | 0 | 1.00 |
| Fecal | 28 | 15.9 | 9.0–26.6 | 97.540 | 1097.423 | 27 | 0.00 |
| Rectal swab | 5 | 7.4 | 1.4–31.7 | 92.148 | 50.941 | 4 | 0.00 |
| Urine | 1 | 45.7 | 30.2–62.1 | 0.00 | 0.00 | 0 | 1.00 |
| Detection Method | Number of Studies | Prevalence (%) | 95% CI | I2 (%) | Q | Heterogeneity Test | |
|---|---|---|---|---|---|---|---|
| DF | p | ||||||
| Agar dilution | 7 | 30.1 | 7.5–69.5 | 98.936 | 563.712 | 6 | 0.00 |
| Broth microdilution | 6 | 17.5 | 10.1–28.6 | 81.876 | 27.588 | 5 | 0.00 |
| Disc diffusion | 11 | 10.2 | 3.5–26.2 | 97.037 | 337.479 | 10 | 0.00 |
| Enrichment culture | 1 | 3.4 | 1.8–6.4 | 0.00 | 0.00 | 0 | 1.00 |
| Enrichment culture | 7 | 9.3 | 4.3–18.8 | 82.647 | 34.576 | 6 | 0.00 |
| Selective culture | 2 | 30.9 | 9.1–66.4 | 79.539 | 4.887 | 1 | 0.027 |
| Sensititre system | 1 | 17.2 | 10.7–26.7 | 0.00 | 0.00 | 0 | 1.00 |
| Variable | Coefficient | 95% CI | p-Value |
|---|---|---|---|
| Country | |||
| Belgium | Reference | ||
| Brazil | −0.538 | −0.747–−0.329 | <0.001 |
| India | 0.705 | 0.587–0.823 | <0.001 |
| Italy | −0.099 | −0.257–0.059 | 0.218 |
| Japan | −0.188 | −0.352–−0.024 | 0.025 |
| Netherlands | 0.081 | −0.010–0.172 | 0.083 |
| Nigeria | −0.359 | −0.664–−0.053 | 0.021 |
| Portugal | −0.464 | −0.679–−0.249 | <0.001 |
| Spain | 0.093 | −0.032–0.218 | 0.145 |
| Thailand | −0.527 | −0.879–−0.175 | 0.003 |
| Turkey | −0.555 | −0.804–−0.306 | <0.001 |
| United Kingdom | −0.062 | −0.172–0.047 | 0.266 |
| United States of America | −0.526 | −0.723–−0.329 | <0.001 |
| Companion Animal | |||
| Dog | Reference | ||
| Cat | −0.029 | −0.067–0.009 | 0.141 |
| Horse | 0.017 | −0.099–0.133 | 0.772 |
| Ostrich | 0.064 | −0.144–0.271 | 0.548 |
| Parrot | −0.049 | −0.162–0.064 | 0.397 |
| Pheasant | 0.496 | 0.253–0.738 | <0.001 |
| Rabbit | 0.743 | 0.513–0.973 | <0.001 |
| Sample Type | |||
| Fecal | References | ||
| Cloacal swab | 0.070 | −0.127–0.267 | 0.485 |
| Rectal swab | 0.161 | 0.041–0.281 | 0.009 |
| Urine | −0.357 | −0.637–−0.078 | 0.012 |
| Detection Method | |||
| Enrichment culture | |||
| Agar dilution | 0.514 | 0.345–0.683 | <0.001 |
| Broth microdilution | 1.296 | 1.115–1.476 | <0.001 |
| Disc diffusion | 0.616 | 0.368–0.864 | <0.001 |
| Constant | 0.079 | 0.004–0.154 | 0.039 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wada, Y.; Irekeola, A.A.; E.A.R., E.N.S.; Yusof, W.; Lih Huey, L.; Ladan Muhammad, S.; Harun, A.; Yean, C.Y.; Zaidah, A.R. Prevalence of Vancomycin-Resistant Enterococcus (VRE) in Companion Animals: The First Meta-Analysis and Systematic Review. Antibiotics 2021, 10, 138. https://doi.org/10.3390/antibiotics10020138
Wada Y, Irekeola AA, E.A.R. ENS, Yusof W, Lih Huey L, Ladan Muhammad S, Harun A, Yean CY, Zaidah AR. Prevalence of Vancomycin-Resistant Enterococcus (VRE) in Companion Animals: The First Meta-Analysis and Systematic Review. Antibiotics. 2021; 10(2):138. https://doi.org/10.3390/antibiotics10020138
Chicago/Turabian StyleWada, Yusuf, Ahmad Adebayo Irekeola, Engku Nur Syafirah E.A.R., Wardah Yusof, Lee Lih Huey, Suwaiba Ladan Muhammad, Azian Harun, Chan Yean Yean, and Abdul Rahman Zaidah. 2021. "Prevalence of Vancomycin-Resistant Enterococcus (VRE) in Companion Animals: The First Meta-Analysis and Systematic Review" Antibiotics 10, no. 2: 138. https://doi.org/10.3390/antibiotics10020138
APA StyleWada, Y., Irekeola, A. A., E.A.R., E. N. S., Yusof, W., Lih Huey, L., Ladan Muhammad, S., Harun, A., Yean, C. Y., & Zaidah, A. R. (2021). Prevalence of Vancomycin-Resistant Enterococcus (VRE) in Companion Animals: The First Meta-Analysis and Systematic Review. Antibiotics, 10(2), 138. https://doi.org/10.3390/antibiotics10020138








