Educational Activities for Students and Citizens Supporting the One-Health Approach on Antimicrobial Resistance
Abstract
:1. Introduction
- Antimicrobial is a wide term used to identify a compound able to selectively kill microorganisms. Bacteria, fungi or parasites are all microorganisms.
- The term antibiotics is widely accepted for antimicrobials that specifically target bacteria.
- Antimicrobial resistance and antibiotic resistance are terms that refer to the development of resistance to specific antibiotics or antimicrobials. Microorganisms find ways to survive. This can occur by restricting the access of the antimicrobial into the cell, degradation, and the complexation of the antibiotic. DNA mutations affecting the antibiotic target site is another way to acquire resistance.
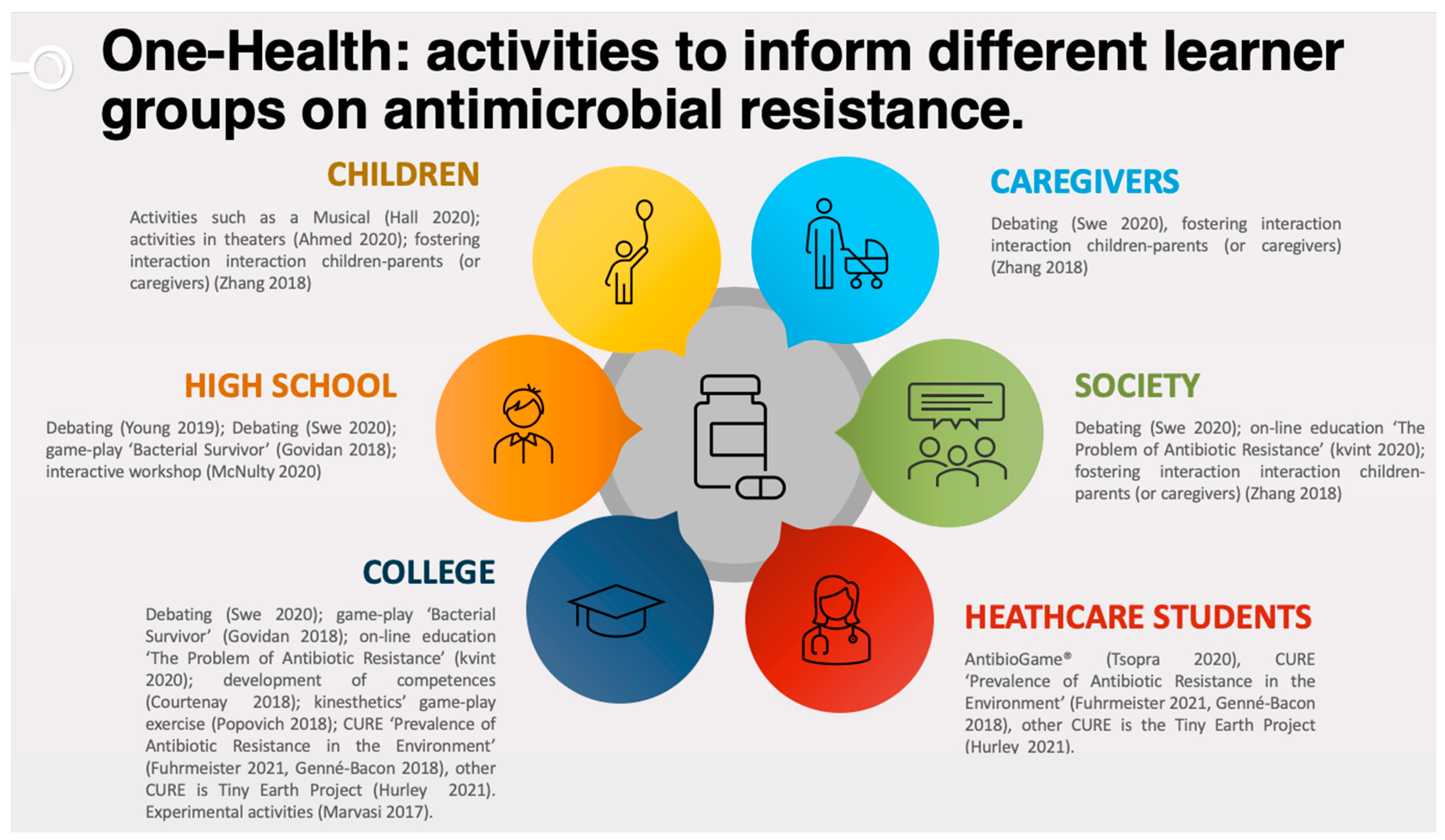
- The One-Health approach is a comprehensive process, which includes multiple disciplines (medicine, biology, social science, education, citizen science) that communicate and work together to achieve better public health outcomes [10,11]. In other words, the One-Heath approach is a collaborative, multisectoral and transdisciplinary strategy in which no single organization or sector can address the issue of antimicrobial resistance at the human–environment interface alone.
- Antimicrobial stewardship involves interdisciplinary professionals in an effort to effect prudent antimicrobial use for patients [12]. For example, medical students should be better informed on the mechanisms of microbial evolution to foster an appreciation and awareness of antibiotic resistant development as a result of unnecessary antibiotic prescriptions [13]. Every medical student, during their professional practice, should aim to resolve the patient’s infection while minimizing the development of antimicrobial resistance [14].
2. Fewer Antibiotics for Youth and Adults (Non-Medical Students)
2.1. Informal Education: Theater Presentations
2.2. Formal Education: Presential or Virtual Workshops
2.3. Combining Informal and Formal Education: Role Playing and Others
2.4. Course-Based Research Experiences for Diverse and International AR Programs
2.5. Online Activities
3. Activities for Medical Students
4. Conclusions and Perspectives
Author Contributions
Funding
Conflicts of Interest
References
- Cassini, A.; Högberg, L.D.; Plachouras, D.; Quattrocchi, A.; Hoxha, A.; Simonsen, G.S.; Colomb-Cotinat, M.; Kretzschmar, M.E.; Devleesschauwer, B.; Cecchini, M.; et al. Attributable deaths and disability-adjusted life-years caused by infections with antibiotic-resistant bacteria in the EU and the European Economic Area in 2015: A population-level modelling analysis. Lancet Infect. Dis. 2019, 19, 56–66. [Google Scholar] [CrossRef] [Green Version]
- Da Silva, R.M.R.; de Mendonça, S.C.B.; Leão, I.N.; dos Santos, Q.N.; Batista, A.M.; Melo, M.S.; da Xavier, M.M.; Quintans Júnior, L.J.; da Silva, W.B.; Lobo, I.M.F. Use of monitoring indicators in hospital management of antimicrobials. BMC Infect. Dis. 2021, 21, 827. [Google Scholar] [CrossRef]
- Wu, Q.; Sabokroo, N.; Wang, Y.; Hashemian, M.; Karamollahi, S.; Kouhsari, E. Systematic review and meta-analysis of the epidemiology of vancomycin-resistance Staphylococcus aureus isolates. Antimicrob. Resist. Infect. Control 2021, 10, 101. [Google Scholar] [CrossRef]
- National Health Serve. Tackling Antimicrobial Resistance: Educational Priorities Full Report; National Health Serve: London, UK, 2018.
- Courtenay, M.; Lim, R.; Castro-Sanchez, E.; Deslandes, R.; Hodson, K.; Morris, G.; Reeves, S.; Weiss, M.; Ashiru-Oredope, D.; Bain, H.; et al. Development of consensus-based national antimicrobial stewardship competencies for UK undergraduate healthcare professional education. J. Hosp. Infect. 2018, 100, 245–256. [Google Scholar] [CrossRef] [PubMed]
- McMaster, D.; Courtenay, M.; Santucci, C.; Davies, A.P.; Kirby, A.; Seddon, O.; Price, D.A.; Barlow, G.; Lim, F.H.; Davies, B.S.; et al. Consensus-based antimicrobial resistance and stewardship competencies for UK undergraduate medical students. JAC-Antimicrob. Resist. 2020, 2, dlaa096. [Google Scholar] [CrossRef]
- Klein, E.Y.; Milkowska-Shibata, M.; Tseng, K.K.; Sharland, M.; Gandra, S.; Pulcini, C.; Laxminarayan, R. Assessment of WHO antibiotic consumption and access targets in 76 countries, 2000–15: An analysis of pharmaceutical sales data. Lancet Infect. Dis. 2021, 21, 107–115. [Google Scholar] [CrossRef]
- Collignon, P.; Beggs, J.J.; Walsh, T.R.; Gandra, S.; Laxminarayan, R. Anthropological and socioeconomic factors contributing to global antimicrobial resistance: A univariate and multivariable analysis. Lancet Planet. Health 2018, 2, e398–e405. [Google Scholar] [CrossRef]
- Vikesland, P.; Garner, E.; Gupta, S.; Kang, S.; Maile-Moskowitz, A.; Zhu, N. Differential Drivers of Antimicrobial Resistance across the World. Acc. Chem. Res. 2019, 52, 916–924. [Google Scholar] [CrossRef] [PubMed]
- Bordier, M.; Uea-Anuwong, T.; Binot, A.; Hendrikx, P.; Goutard, F.L. Characteristics of One Health surveillance systems: A systematic literature review. Prev. Vet. Med. 2020, 181, 104560. [Google Scholar] [CrossRef] [PubMed]
- WHO. Available online: https://www.who.int/news-room/q-a-detail/one-health (accessed on 8 September 2021).
- McIsaac, W.; Kukan, S.; Huszti, E.; Szadkowski, L.; O’Neill, B.; Virani, S.; Ivers, N.; Lall, R.; Toor, N.; Shah, M.; et al. A pragmatic randomized trial of a primary care antimicrobial stewardship intervention in Ontario, Canada. BMC Fam. Pract. 2021, 22, 185. [Google Scholar] [CrossRef]
- Vassallo, A.; Kett, S.; Purchase, D.; Marvasi, M. Antibiotic-Resistant Genes and Bacteria as Evolving Contaminants of Emerging Concerns (e-CEC): Is It Time to Include Evolution in Risk Assessment? Antibiotics 2021, 10, 1066. [Google Scholar] [CrossRef]
- Mayi, B.S.; Mainville, M.; Altaf, R.; Lanspa, M.; Vaniawala, S.; Ollerhead, T.A.; Raja, A. A Crucial Role for Antimicrobial Stewardship in the Midst of COVID-19. J. Microbiol. Biol. Educ. 2021, 22. [Google Scholar] [CrossRef]
- Rosenbaum, L. No Cure without Care—Soothing Science Skepticism. N. Engl. J. Med. 2021, 384, 1462–1465. [Google Scholar] [CrossRef]
- Hall, J.; Jones, L.; Robertson, G.; Hiley, R.; Nathwani, D.; Perry, M.R. ‘The Mould that Changed the World’: Quantitative and qualitative evaluation of children’s knowledge and motivation for behavioural change following participation in an antimicrobial resistance musical. PLoS ONE 2020, 15, e0240471. [Google Scholar] [CrossRef]
- Ahmed, R.; Bashir, A.; Brown, J.E.P.; Cox, J.A.G.; Hilton, A.C.; Hilton, C.E.; Lambert, P.A.; Theodosiou, E.; Tritter, J.Q.; Watkin, S.J.; et al. The drugs don’t work: Evaluation of educational theatre to gauge and influence public opinion on antimicrobial resistance. J. Hosp. Infect. 2020, 104, 193–197. [Google Scholar] [CrossRef] [Green Version]
- Swe, M.M.M.; Hlaing, P.H.; Phyo, A.P.; Aung, H.H.; Smithuis, F.; Ashley, E.A.; Cheah, P.Y. Evaluation of the forum theatre approach for public engagement around antibiotic use in Myanmar. PLoS ONE 2020, 15, e0235625. [Google Scholar] [CrossRef]
- Zhang, Y.; Kabba, J.; Chang, J.; Ji, W.; Zhu, S.; Yu, J.; Xu, S.; Fang, Y. A School-Based Educational Intervention for School-Aged Children and Caregivers about Rational Use of Antibiotics in Urban Areas of Shaanxi Province: A Study Protocol for a Randomized Controlled Research. Int. J. Environ. Res. Public Health 2018, 15, 1912. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marvasi, M.; Choudhury, M.; Vala, N.B.; Teplitski, M. Fitness of Antibiotic-Resistant Bacteria in the Environment: A Laboratory Activity. J. Microbiol. Biol. Educ. 2017. [Google Scholar] [CrossRef] [Green Version]
- Popovich, J.; Stephens, M.; Celaya, H.; Suwarno, S.; Barclay, S.; Yee, E.; Dean, D.A.; Farris, M.; Haydel, S.E. Building and Breaking the Cell Wall in Four Acts: A Kinesthetic and Tactile Role-Playing Exercise for Teaching Beta-Lactam Antibiotic Mechanism of Action and Resistance. J. Microbiol. Biol. Educ. 2018, 19. [Google Scholar] [CrossRef] [Green Version]
- Govindan, B. Bacterial Survivor: An Interactive Game that Combats Misconceptions about Antibiotic Resistance. J. Microbiol. Biol. Educ. 2018, 19, 2. [Google Scholar] [CrossRef] [Green Version]
- Young, V.L.; Berry, M.; Verlander, N.Q.; Ridgway, A.; McNulty, C.A. Using debate to educate young people in schools about antibiotic use and resistance: A before and after evaluation using a questionnaire survey. J. Infect. Prev. 2019, 20, 281–288. [Google Scholar] [CrossRef] [PubMed]
- McNulty, C.A.M.; Brown, C.L.; Syeda, R.B.; Bennett, C.V.; Schofield, B.; Allison, D.G.; Francis, N. Teacher and Student Views on the Feasibility of Peer to Peer Education as a Model to Educate 16–18 Year Olds on Prudent Antibiotic Use—A Qualitative Study. Antibiotics 2020, 9, 194. [Google Scholar] [CrossRef]
- Fuhrmeister, E.R.; Larson, J.R.; Kleinschmit, A.J.; Kirby, J.E.; Pickering, A.J.; Bascom-Slack, C.A. Combating Antimicrobial Resistance Through Student-Driven Research and Environmental Surveillance. Front. Microbiol. 2021, 12. [Google Scholar] [CrossRef]
- Broadening the Talent Pool: Creating More Inclusive Course-Based Undergrad Research Experiences (CUREs). Available online: https://asm.org/Articles/2020/June/Broadening-the-Talent-Pool-Creating-More-Inclusive (accessed on 2 November 2021).
- Estrada, M.; Woodcock, A.; Hernandez, P.R.; Schultz, P.W. Toward a Model of Social Influence that Explains Minority StudentIntegration into the Scientific Community. J. Educ. Psychol. 2011, 103, 206. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Adkins-Jablonsky, S.J.; Akscyn, R.; Bennett, B.C.; Roberts, Q.; Morris, J.J. Is Community Relevance Enough? Civic and Science Identity Impact of Microbiology CUREs Focused on Community Environmental Justice. Front. Microbiol. 2020, 11, 3282. [Google Scholar] [CrossRef] [PubMed]
- Genné-Bacon, E.A.; Bascom-Slack, C.A. The PARE Project: A Short Course-Based Research Project for National Surveillance of Antibiotic-Resistant Microbes in Environmental Samples. J. Microbiol. Biol. Educ. 2018, 19. [Google Scholar] [CrossRef] [Green Version]
- Hurley, A.; Chevrette, M.G.; Acharya, D.D.; Lozano, G.L.; Garavito, M.; Heinritz, J.; Balderrama, L.; Beebe, M.; Denhartog, M.L.; Corinaldi, K.; et al. Tiny earth: A big idea for stem education and antibiotic discovery. MBio 2021, 12, e03432-20. [Google Scholar] [CrossRef] [PubMed]
- Kvint, K.; Palm, M.; Farewell, A. Teaching about antibiotic resistance to a broad audience: A multidisciplinary approach. FEMS Microbiol. Lett. 2020, 367, fnaa111. [Google Scholar] [CrossRef] [PubMed]
- Justo, J.A.; Gauthier, T.P.; Scheetz, M.H.; Chahine, E.B.; Bookstaver, P.B.; Gallagher, J.C.; Hermsen, E.D.; DePestel, D.D.; Ernst, E.J.; Jacobs, D.M.; et al. Knowledge and Attitudes of Doctor of Pharmacy Students Regarding the Appropriate Use of Antimicrobials. Clin. Infect. Dis. 2014, 59, S162–S169. [Google Scholar] [CrossRef] [Green Version]
- Higuita-Gutiérrez, L.F.; Roncancio Villamil, G.E.; Jiménez Quiceno, J.N. Knowledge, attitude, and practice regarding antibiotic use and resistance among medical students in Colombia: A cross-sectional descriptive study. BMC Public Health 2020, 20, 1861. [Google Scholar] [CrossRef]
- Tsopra, R.; Courtine, M.; Sedki, K.; Eap, D.; Cabal, M.; Cohen, S.; Bouchaud, O.; Mechaï, F.; Lamy, J.-B. AntibioGame®: A serious game for teaching medical students about antibiotic use. Int. J. Med. Inform. 2020, 136, 104074. [Google Scholar] [CrossRef]
- Chapot, L.; Sarker, M.S.; Begum, R.; Hossain, D.; Akter, R.; Hasan, M.M.; Bupasha, Z.B.; Bayzid, M.; Salauddin, M.; Parvej, M.S.; et al. Knowledge, Attitudes and Practices Regarding Antibiotic Use and Resistance among Veterinary Students in Bangladesh. Antibiotics 2021, 10, 332. [Google Scholar] [CrossRef]
- Bangera, G.; Brownell, S.E. Course-Based Undergraduate Research Experiences Can Make Scientific Research More Inclusive. CBE—Life Sci. Educ. 2014, 13, 602–606. [Google Scholar] [CrossRef] [Green Version]
- Asai, D.J. Race Matters. Cell 2020, 181, 754–757. [Google Scholar] [CrossRef]
- NSF. Women, Minorities, and Persons with Disabilities in Science and Engineering:National Science Foundation; NSF: Alexandria, VA, USA, 2021.
- Siddiky, N.A.; Khan, M.S.R.; Sarker, M.S.; Bhuiyan, M.K.J.; Mahmud, A.; Rahman, M.T.; Ahmed, M.M.; Samad, M.A. Knowledge, attitude and practice of chicken vendors on food safety and foodborne pathogens at wet markets in Dhaka, Bangladesh. Food Control 2022, 131, 108456. [Google Scholar] [CrossRef]
- Singh, S.; Charani, E.; Devi, S.; Sharma, A.; Edathadathil, F.; Kumar, A.; Warrier, A.; Shareek, P.S.; Jaykrishnan, A.V.; Ellangovan, K. A road-map for addressing antimicrobial resistance in low- and middle-income countries: Lessons learnt from the public private participation and co-designed antimicrobial stewardship programme in the State of Kerala, India. Antimicrob. Resist. Infect. Control 2021, 10, 32. [Google Scholar] [CrossRef]
- Eley, C.V.; Young, V.L.; Hayes, C.V.; McNulty, C.A.M. Evaluation of an e-Learning platform for educators to improve education around infection prevention and antibiotics. Technol. Pedagog. Educ. 2019, 28, 485–501. [Google Scholar] [CrossRef]
- Sakr, S.; Ghaddar, A.; Hamam, B.; Sheet, I. Antibiotic use and resistance: An unprecedented assessment of university students’ knowledge, attitude and practices (KAP) in Lebanon. BMC Public Health 2020, 20, 535. [Google Scholar] [CrossRef] [Green Version]
| Type of Activity | Merits | Demerits |
|---|---|---|
| Informal education: Theater presentations | These activities are driven by learners’ interest and have been developed for a wide range of audiences and children. | As the target audiences are the general public and children, the activities tend to be at a superficial level of understanding. |
| Formal education: Presential or virtual workshops | These activities reach deeper explanation and concepts. | Level of participation is dependent on students’ interest and motivation. It may require studying some concepts in advance. |
| Combining informal and formal education | Useful to stimulate less interested students. | Students with prior knowledge may become disinterested and less engaged. |
| Course-based research experiences | The best in terms of understanding, motivation and interest. | Highly resources-intensive in terms of instructors’ involvement and consumables. It needs to be carefully organized. |
| Online activities | Activities always available. After preparation, they require relatively low maintenance from the instructor. | It attracts only motivated students and interested audiences. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marvasi, M.; Casillas, L.; Vassallo, A.; Purchase, D. Educational Activities for Students and Citizens Supporting the One-Health Approach on Antimicrobial Resistance. Antibiotics 2021, 10, 1519. https://doi.org/10.3390/antibiotics10121519
Marvasi M, Casillas L, Vassallo A, Purchase D. Educational Activities for Students and Citizens Supporting the One-Health Approach on Antimicrobial Resistance. Antibiotics. 2021; 10(12):1519. https://doi.org/10.3390/antibiotics10121519
Chicago/Turabian StyleMarvasi, Massimiliano, Lilliam Casillas, Alberto Vassallo, and Diane Purchase. 2021. "Educational Activities for Students and Citizens Supporting the One-Health Approach on Antimicrobial Resistance" Antibiotics 10, no. 12: 1519. https://doi.org/10.3390/antibiotics10121519
APA StyleMarvasi, M., Casillas, L., Vassallo, A., & Purchase, D. (2021). Educational Activities for Students and Citizens Supporting the One-Health Approach on Antimicrobial Resistance. Antibiotics, 10(12), 1519. https://doi.org/10.3390/antibiotics10121519






