Common Infections and Antibiotic Prescribing during the First Year of the COVID-19 Pandemic: A Primary Care-Based Observational Cohort Study
Abstract
:1. Introduction
2. Results
2.1. Study Population
2.2. Number of Infectious Disease Episodes for the Four Common Infection Types
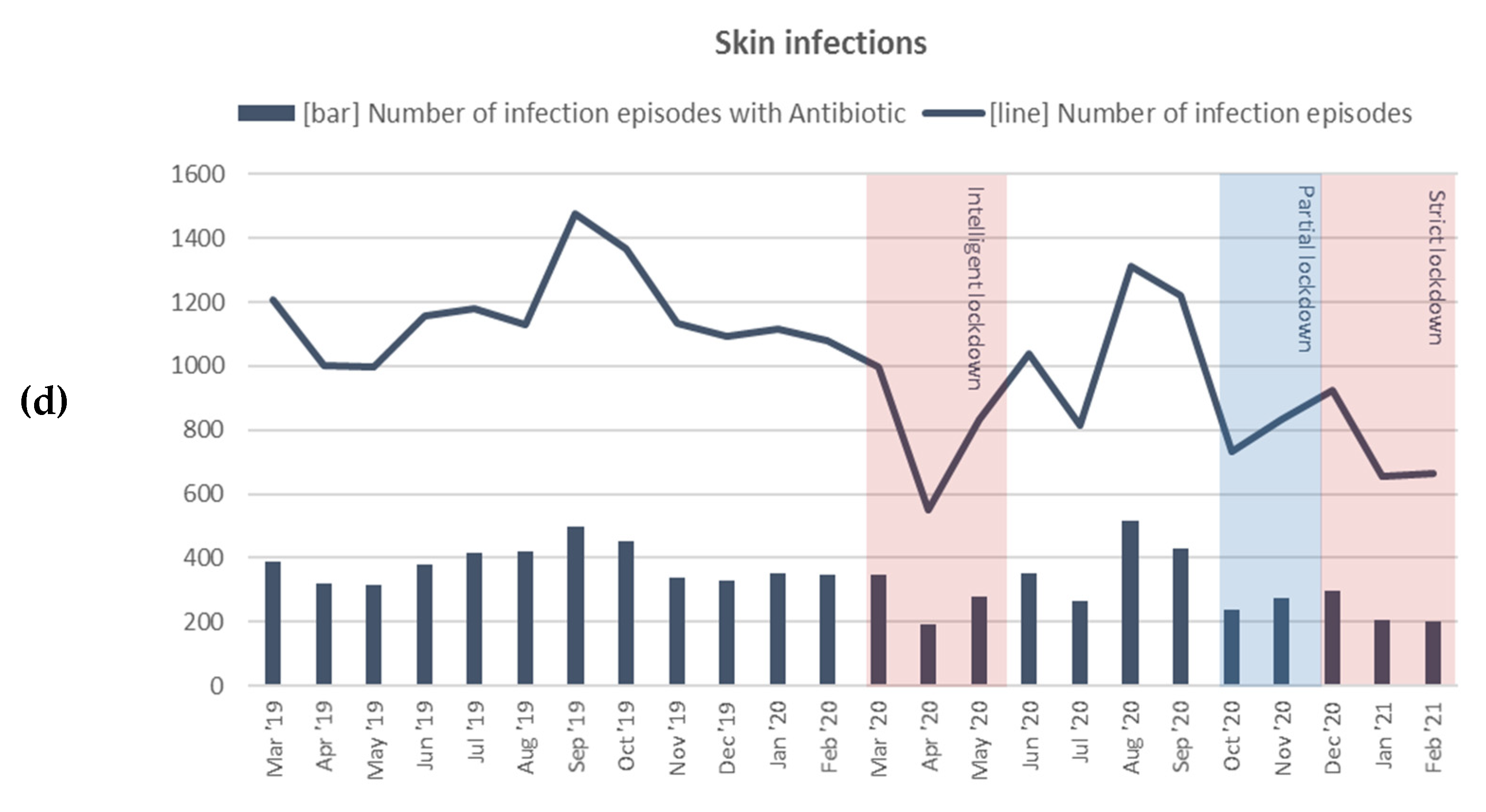
2.3. Number of Infectious Disease Episodes with Antibiotics
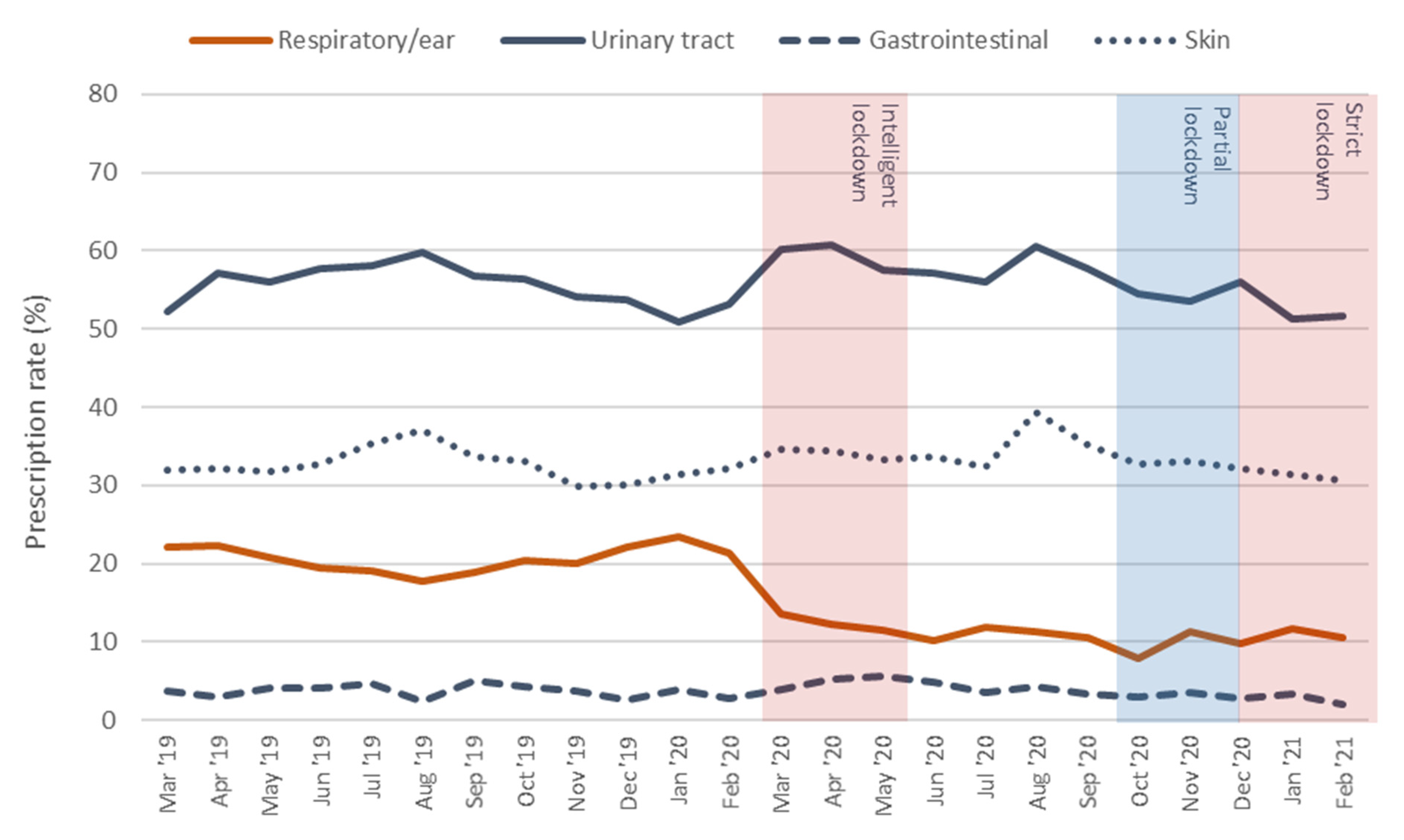
2.4. Antibiotic Prescription Rate
2.5. Respiratory Tract/Ear Infection Episodes and Antibiotic Prescribing per Age Group
2.6. Complications
2.7. Remote Consultations
3. Discussion
3.1. Main Findings
3.2. Comparison with Other Literature
3.3. Strengths and Limitations
3.4. Implications for Further Research
4. Materials and Methods
4.1. Design and Study Population
4.2. Data Extraction
4.3. Analyses
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| ICPC Chapter | |
|---|---|
| H—Ear R—Respiratory tract | H71 acute otitis media H99 ear/mastoid disease H01 earache H04 ear discharge H70 otitis externa H72 serous otitis media H74 chronic otitis media/other otitis H74.01 chronic otitis media H74.02 mastoiditis R21 throat symptoms R22 tonsil symptoms R72 strep throat R74 acute upper RTI R76 tonsillitis/tonsillar abscess R76.01 tonsillitis R76.02 tonsillar abscess R77 laryngitisR80 influenza R83 other RTI (including COVID-19) R05 cough R09 sinus symptoms R75 sinusitis R78 bronchitis R81 pneumonia R82 pleurisy R71 whooping cough R70 tuberculosis |
| U—Urinary tract | U01 dysuria U02 urgency U71 cystitis U70 pyelonephritis Y73 prostatitis |
| D—Gastrointestinal | D11 diarrhoea D70 gastrointestinal infection D73 gastroenteritis D22 parasites D92 diverticular disease |
| S—Skin | S09 infected finger/toe S10 boil/carbuncle S11 skin infection post-traumatic S76 other skin infection S84 impetigo |
References
- World Health Organization. WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19–11 March 2020. Available online: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (accessed on 25 October 2021).
- Rijksoverheid. Corona Dashboard. Available online: https://coronadashboard.rijksoverheid.nl/ (accessed on 30 October 2021).
- Rijksoverheid. Coronavirus tijdlijn. Available online: https://www.rijksoverheid.nl/onderwerpen/coronavirus-tijdlijn (accessed on 25 October 2021).
- Pouwels, B.D.C.; Simons, S.O.; Theunissen, M.; Peters, M.L.; Schoenmaekers, J.J.; Bekkers, S.C.; van den Beuken-van Everdingen, M.H.J. Healthcare use during COVID-19 and the effect on psychological distress in patients with chronic cardiopulmonary disorders in the Netherlands: A cross-sectional study. B. M. J. Open 2021, 11, e046883. [Google Scholar] [CrossRef]
- Schäfer, I.; Hansen, H.; Menzel, A.; Eisele, M.; Tajdar, D.; Lühmann, D.; Scherer, M. The effect of COVID-19 pandemic and lockdown on consultation numbers, consultation reasons and performed services in primary care: Results of a longitudinal observational study. B. M. C. Fam Pract 2021, 22, 125. [Google Scholar] [CrossRef]
- Uyl-de Groot, C.A.; Schuurman, M.S.; Huijgens, P.C.; Praagman, J. Onderdiagnostiek bij kanker door de COVID-19-crisis naar diagnose, leeftijd en provincie [Fewer cancer diagnoses during the COVID-19 epidemic according to diagnosis, age and region]. TSG 2020, 99, 1–8. [Google Scholar]
- Williams, R.; Jenkins, D.A.; Ashcroft, D.M.; Brown, B.; Campbell, S.; Carr, M.J.; Cheraghi-Sohi, S.; Kapur, N.; Thomas, O.; Webb, R.T.; et al. Diagnosis of physical and mental health conditions in primary care during the COVID-19 pandemic: A retrospective cohort study. Lancet Public Health 2020, 5, e543–e550. [Google Scholar] [CrossRef]
- van de Pol, A.C.; Boeijen, J.A.; Venekamp, R.P.; Platteel, T.; Damoiseaux, R.A.M.J.; Kortekaas, M.F.; van der Velden, A.W. Impact of the COVID-19 Pandemic on Antibiotic Prescribing for Common Infections in The Netherlands: A Primary Care-Based Observational Cohort Study. Antibiotics 2021, 10, 196. [Google Scholar] [CrossRef] [PubMed]
- Gautret, P.; Lagier, J.C.; Parola, P.; Hoang, V.T.; Meddeb, L.; Mailhe, M.; Doudier, B.; Courjon, J.; Giordanengo, V.; Vieira, V.E.; et al. Hydroxychloroquine and azithromycin as a treatment of COVID-19: Results of an open-label non-randomized clinical trial. Int. J. Antimicrob. Agents 2020, 56, 105949. [Google Scholar] [CrossRef] [PubMed]
- Rosendaal, F.R. Review of: “Hydroxychloroquine and azithromycin as a treatment of COVID-19: Results of an open-label non-randomized clinical trial Gautret et al. 2010, DOI:10.1016/j.ijantimicag.2020.105949. Int. J. Antimicrob. Agents 2020, 56, 106063. [Google Scholar] [CrossRef] [PubMed]
- Stichting Werkgroep Antibioticabeleid (SWAB). Medicamenteuze Behandeling Vvoor Patiënten Met COVID-19 (Infectie Met SARS-CoV-2). Available online: https://swab.nl/nl/covid-19#to_20 (accessed on 30 October 2021).
- Arnold, S.R.; Straus, S.E. Interventions to improve antibiotic prescribing practices in ambulatory care. Cochrane Database Syst Rev 2005, 2005, CD003539. [Google Scholar] [CrossRef] [PubMed]
- van der Velden, A.W.; Pijpers, E.J.; Kuyvenhoven, M.M.; Tonkin-Crine, S.K.; Little, P.; Verheij, T.J. Effectiveness of physician-targeted interventions to improve antibiotic use for respiratory tract infections. Br. J. Gen. Pract. 2012, 62, e801–e807. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- European Center for Disease Prevention and Control (ECDC). Antimicrobial Consumption in the EU/EEA, Annual Epidemiological Report for 2018; ECDC: Stockholm, Sweden, 2019.
- van der Velden, A.W.; Bax, E.A.; Bongard, E.; Munck Aabenhus, R.; Anastasaki, M.; Anthierens, S.; Balan, A.; Bohmer, F.; Bruno, P.; Chlabicz, S.; et al. Primary care for patients with respiratory tract infection before and early on in the COVID-19 pandemic: An observational study in 16 European countries. BMJ Open 2021, 11, e049257. [Google Scholar] [CrossRef] [PubMed]
- Rezel-Potts, E.; L’Esperance, V.; Gulliford, M.C. Antimicrobial stewardship in the UK during the COVID-19 pandemic: A population-based cohort study and interrupted time-series analysis. Br. J. Gen. Pract. 2021, 71, e331–e338. [Google Scholar] [CrossRef] [PubMed]
- Wasag, D.R.; Cannings-John, R.; Hughes, K.; Ahmed, H. Antibiotic dispensing during the COVID-19 pandemic: Analysis of Welsh primary care dispensing data. Fam. Pract. 2021, cmab141. [Google Scholar] [CrossRef] [PubMed]
- Zhu, N.; Aylin, P.; Rawson, T.; Gilchrist, M.; Majeed, A.; Holmes, A. Investigating the impact of COVID-19 on primary care antibiotic prescribing in North West London across two epidemic waves. Clin. Microbiol. Infect. 2021, 27, 762–768. [Google Scholar] [CrossRef] [PubMed]
- Hullegie, S.; Schilder, A.G.M.; Marchisio, P.; de Sévaux, J.L.H.; van der Velden, A.W.; van de Pol, A.C.; Boeijen, J.A.; Platteel, T.N.; Torretta, S.; Damoiseaux, R.A.M.J.; et al. A Strong Decline in the Incidence of Childhood Otitis Media During the COVID-19 Pandemic in the Netherlands. Front. Cell. Infect. Microbiol. 2021, 1, 768377. [Google Scholar] [CrossRef]
- Little, P.; Stuart, B.; Hobbs, F.D.R.; Moore, M.; Barnett, J.; Popoola, D.; Middleton, K.; Kelly, J.; Mullee, M.; Raftery, J.; et al. An internet-delivered handwashing intervention to modify influenza-like illness and respiratory infection transmission (PRIMIT): A primary care randomised trial. The Lancet 2015, 386, 1631–1639. [Google Scholar] [CrossRef]
- Smeets, H.M.; Kortekaas, M.F.; Rutten, F.H.; Bots, M.L.; van der Kraan, W.; Daggelders, G.; Smits-Pelser, H.; Helsper, C.W.; Hoes, A.W.; de Wit, N.J. Routine primary care data for scientific research, quality of care programs and educational purposes: The Julius General Practitioners’ Network (JGPN). B. M. C. Health Serv. Res. 2018, 18, 735. [Google Scholar] [CrossRef]

| Episodes | Episodes with Antibiotics | |||||
|---|---|---|---|---|---|---|
| Pre- Pandemic | Pandemic | Pre- Pandemic | Pandemic | |||
| n | n | RR (CI) | n | n | RR (CI) | |
| Respiratory tract/ear | 73,089 | 56,875 | 0.77 (CI 0.76 to 0.77) * | 15,335 | 6358 | 0.41 (CI 0.40 to 0.42) * |
| Urinary tract | 25,703 | 22,690 | 0.87 (CI 0.85 to 0.88) * | 14,216 | 12,815 | 0.89 (CI 0.87 to 0.91) * |
| Gastrointestinal | 9990 | 5870 | 0.58 (CI 0.56 to 0.60) * | 374 | 223 | 0.59 (CI 0.50 to 0.69) * |
| Skin | 13,943 | 10,580 | 0.75 (CI 0.73 to 0.77) * | 4558 | 3592 | 0.78 (CI 0.74 to 0.81) * |
| Total | 122,725 | 96,015 | 0.77 (CI 0.76 to 0.78) * | 34,483 | 22,988 | 0.66 (CI 0.65 to 0.67) * |
| Pre-Pandemic | Pandemic | Difference (CI) | |
|---|---|---|---|
| % | % | ||
| Respiratory tract/ear | 21% | 11% | −10% (CI −10.4 to −9.6%) * |
| Urinary tract | 55% | 56% | +1% (CI 0.1% to 1.9%) * |
| Gastrointestinal | 4% | 4% | +0% (CI −0.6% to 0.6%) |
| Skin | 33% | 34% | +1% (CI −0.2% to 2.2%) |
| Total | 28% | 24% | −4% (CI −4.4 to −3.6%) * |
| Age Group | Episodes | Episodes with Antibiotic | Prescription Rate | |
|---|---|---|---|---|
| Pre-Pandemic | Pandemic | |||
| RR (CI) | RR (CI) | % | % | |
| 0–12 | 0.50 (CI 0.49 to 0.51) | 0.33 (CI 0.31 to 0.35) | 22% | 14% |
| 13–40 | 0.87 (CI 0.85 to 0.88) | 0.42 (CI 0.40 to 0.44) | 18% | 9% |
| 41–65 | 0.96 (CI 0.95 to 0.98) | 0.49 (CI 0.46 to 0.52) | 20% | 10% |
| >65 | 0.72 (CI 0.70 to 0.74) | 0.42 (CI 0.39 to 0.44) | 26% | 15% |
| Total | 0.77 (CI 0.76 to 0.77) | 0.41 (CI 0.40 to 0.42) | 21% | 11% |
| Pre-Pandemic | Pandemic | ||
|---|---|---|---|
| n | n | RR (CI) | |
| Pyelonephritis | 460 | 467 | 1.00 (CI 0.88 to 1.14) |
| Pneumonia | 3934 | 1423 | 0.36 (CI 0.34 to 0.38) * |
| Mastoiditis | 28 | 16 | 0.56 (CI 0.30 to 1.04) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Boeijen, J.A.; van der Velden, A.W.; Hullegie, S.; Platteel, T.N.; Zwart, D.L.M.; Damoiseaux, R.A.M.J.; Venekamp, R.P.; van de Pol, A.C. Common Infections and Antibiotic Prescribing during the First Year of the COVID-19 Pandemic: A Primary Care-Based Observational Cohort Study. Antibiotics 2021, 10, 1521. https://doi.org/10.3390/antibiotics10121521
Boeijen JA, van der Velden AW, Hullegie S, Platteel TN, Zwart DLM, Damoiseaux RAMJ, Venekamp RP, van de Pol AC. Common Infections and Antibiotic Prescribing during the First Year of the COVID-19 Pandemic: A Primary Care-Based Observational Cohort Study. Antibiotics. 2021; 10(12):1521. https://doi.org/10.3390/antibiotics10121521
Chicago/Turabian StyleBoeijen, Josi A., Alike W. van der Velden, Saskia Hullegie, Tamara N. Platteel, Dorien L. M. Zwart, Roger A. M. J. Damoiseaux, Roderick P. Venekamp, and Alma C. van de Pol. 2021. "Common Infections and Antibiotic Prescribing during the First Year of the COVID-19 Pandemic: A Primary Care-Based Observational Cohort Study" Antibiotics 10, no. 12: 1521. https://doi.org/10.3390/antibiotics10121521
APA StyleBoeijen, J. A., van der Velden, A. W., Hullegie, S., Platteel, T. N., Zwart, D. L. M., Damoiseaux, R. A. M. J., Venekamp, R. P., & van de Pol, A. C. (2021). Common Infections and Antibiotic Prescribing during the First Year of the COVID-19 Pandemic: A Primary Care-Based Observational Cohort Study. Antibiotics, 10(12), 1521. https://doi.org/10.3390/antibiotics10121521





