Appropriateness of Outpatient Antibiotic Use in Seniors across Two Canadian Provinces
Abstract
:1. Introduction
2. Results
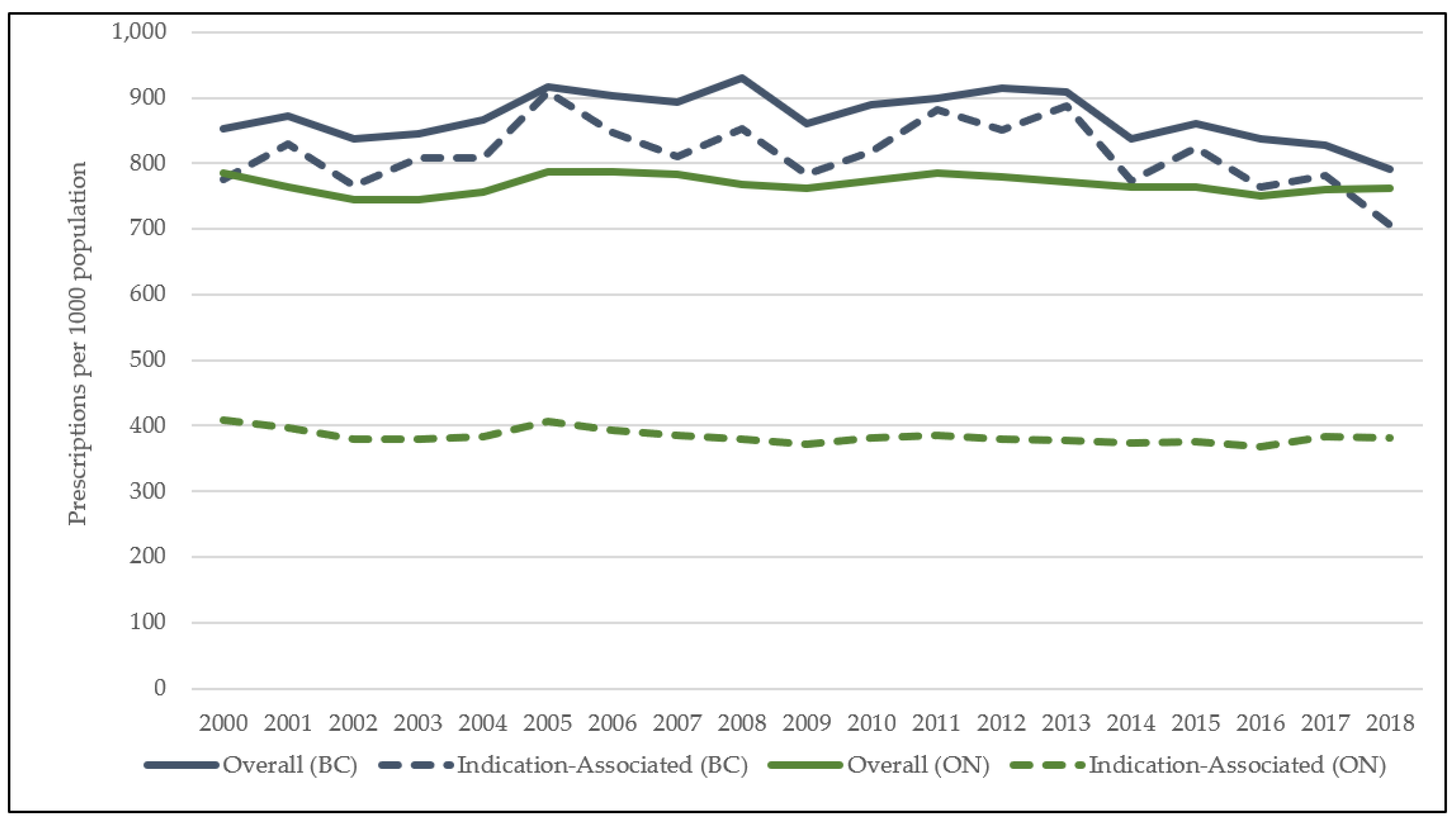
Primary Outcome: Indication-Associated Antibiotic Use & Inappropriate Prescribing
3. Discussion
4. Materials and Methods
4.1. Data Sources
4.2. Study Population
4.3. Outcomes & Statistical Analyses
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Global Action Plan on Antimicrobial Resistance. 2015. Available online: https://apps.who.int/iris/handle/10665/193736 (accessed on 14 September 2020).
- Atlanta: Division of Healthcare Quality Promotion, National Center for Emerging and Zoonotic Infectious Disease, Centers for Disease Control and Prevention. National Action Plan for Combating Antibiotic-Resistant Bacteria. 2015. Available online: www.cdc.gov/drugresistance/pdf/national_action_plan_for_combating_antibotic-resistant_bacteria.pdf (accessed on 20 October 2021).
- Contained and Controlled: The UK’s 20-Year Vision for Antimicrobial Resistance. London (UK): HM Government. 2019. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/773065/uk-20-year-vision-for-antimicrobial-resistance.pdf (accessed on 20 October 2021).
- Tackling Antimicrobial Resistance 2019–2024: The UK’s Five-Year National Action Plan. London (UK): HM Government. 2019. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/784894/UK_AMR_5_year_national_action_plan.pdf (accessed on 19 October 2021).
- Australia’s National Antimicrobial Resistance Strategy–2020 and beyond. Antimicrobial Resistance. Published 10 March 2020. Available online: https://www.amr.gov.au/resources/australias-national-antimicrobial-resistance-strategy-2020-and-beyond (accessed on 22 October 2021).
- Van Katwyk, S.R.; Grimshaw, J.M.; Hoffman, S.J. Ten Years of Inaction on Antimicrobial Resistance: An Environmental Scan of Policies in Canada from 2008 to 2018. Healthc. Policy 2020, 15, 48–62. [Google Scholar] [CrossRef]
- Public Health Agency of Canada. Handling Antibiotics with Care: Preserving Antibiotics Now and in the Future: Spotlight Report 2019. Published 20 September 2019. Available online: https://www.canada.ca/en/public-health/corporate/publications/chief-public-health-officer-reports-state-public-health-canada/preserving-antibiotics/handling-antibiotics.html (accessed on 4 June 2020).
- Public Health Agency of Canada. Canadian Antimicrobial Resistance Surveillance System-Update 2020. aem. Published 9 July 2020. Available online: https://www.canada.ca/en/public-health/services/publications/drugs-health-products/canadian-antimicrobial-resistance-surveillance-system-2020-report.html (accessed on 5 August 2021).
- Public Health Agency of Canada. Canadian Antimicrobial Resistance Surveillance System 2017 Report-Executive Summary. aem. Published 10 November 2017. Available online: https://www.canada.ca/en/public-health/services/publications/drugs-health-products/canadian-antimicrobial-resistance-surveillance-system-2017-report-executive-summary.html (accessed on 17 January 2021).
- Silverman, M.; Povitz, M.; Sontrop, J.M.; Li, L.; Richard, L.; Cejic, S.; Shariff, S. Antibiotic Prescribing for Nonbacterial Acute Upper Respiratory Infections in Elderly Persons. Ann. Intern. Med. 2017, 166, 765–774. [Google Scholar] [CrossRef] [PubMed]
- Tan, C.; Graves, E.; Lu, H.; Chen, A.; Li, S.; Schwartz, K.L.; Daneman, N. A decade of outpatient antimicrobial use in older adults in Ontario: A descriptive study. CMAJ Open 2017, 5, E878–E885. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jain, S.; Self, W.H.; Wunderink, R.G.; Fakhran, S.; Balk, R.; Bramley, A.M.; Reed, C.; Grijalva, C.G.; Anderson, E.J.; Courtney, D.M.; et al. Community-Acquired Pneumonia Requiring Hospitalization among US Adults. N. Engl. J. Med. 2015, 373, 415–427. [Google Scholar] [CrossRef] [Green Version]
- Chen, H.; Hara, Y.; Horita, N.; Saigusa, Y.; Hirai, Y.; Kaneko, T. Declined Functional Status Prolonged Hospital Stay for Community-Acquired Pneumonia in Seniors. Clin. Interv. Aging 2020, 15, 1513–1519. [Google Scholar] [CrossRef]
- Schwartz, K.L.; Langford, B.J.; Daneman, N.; Chen, B.; Brown, K.A.; McIsaac, W.; Tu, K.; Candido, E.; Johnstone, J.; Leung, V.; et al. Unnecessary antibiotic prescribing in a Canadian primary care setting: A descriptive analysis using routinely collected electronic medical record data. CMAJ Open 2020, 8, E360–E369. [Google Scholar] [CrossRef]
- Gulliford, M.C.; Prevost, T.; Charlton, J.; Juszczyk, D.; Soames, J.; McDermott, L.; Sultana, K.; Wright, M.; Fox, R.; Hay, A.; et al. Effectiveness and safety of electronically delivered prescribing feedback and decision support on antibiotic use for respiratory illness in primary care: REDUCE cluster randomised trial. BMJ 2019, 364, l236. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brown, K.A.; Langford, B.; Schwartz, K.L.; Diong, C.; Garber, G.; Daneman, N. Antibiotic Prescribing Choices and Their Comparative C. Difficile Infection Risks: A Longitudinal Case-Cohort Study. Clin. Infect. Dis. 2021, 72, 836–844. [Google Scholar] [CrossRef] [Green Version]
- Saha, S.; Kapoor, S.; Tariq, R.; Schuetz, A.N.; Tosh, P.K.; Pardi, D.S.; Khanna, S. Increasing antibiotic resistance in Clostridioides difficile: A systematic review and meta-analysis. Anaerobe 2019, 58, 35–46. [Google Scholar] [CrossRef]
- So, A.D.; Shah, T.A.; Roach, S.; Chee, Y.L.; Nachman, K.E. An Integrated Systems Approach is Needed to Ensure the Sustainability of Antibiotic Effectiveness for Both Humans and Animals. J. Law Med. Ethics 2015, 43, 38–45. [Google Scholar] [CrossRef]
- Laxminarayan, R.; Duse, A.; Wattal, C.; Zaidi, A.K.M.; Wertheim, H.F.L.; Sumpradit, N.; Vlieghe, E.; Hara, G.L.; Gould, I.M.; Goossens, H.; et al. Antibiotic resistance—the need for global solutions. Lancet Infect. Dis. 2013, 13, 1057–1098. [Google Scholar] [CrossRef] [Green Version]
- Aarestrup, F.M.; Wegener, H.C.; Collignon, P. Resistance in bacteria of the food chain: Epidemiology and control strategies. Expert Rev. Anti-Infect. Ther. 2008, 6, 733–750. [Google Scholar] [CrossRef] [PubMed]
- O’Neill, J. Tackling Drug-Resistant Infections Globally: Final Report and Recommendations. Government of the United King-dom. 2016. Available online: https://apo.org.au/node/63983 (accessed on 27 October 2021).
- Spivak, E.S.; Cosgrove, S.E.; Srinivasan, A. Measuring Appropriate Antimicrobial Use: Attempts at Opening the Black Box. Clin. Infect. Dis. 2016, 63, 1–6. [Google Scholar] [CrossRef] [Green Version]
- McKay, R.M.; Vrbova, L.; Fuertes, E.; Chong, M.; David, S.; Dreher, K.; Purych, D.; Blondel-Hill, E.; Henry, B.; Marra, F.; et al. Evaluation of the Do Bugs Need Drugs? Program in British Columbia: Can we curb antibiotic prescribing? Can. J. Infect. Dis. Med. Microbiol. 2011, 22, 19–24. [Google Scholar] [CrossRef]
- Fleming-Dutra, K.E.; Hersh, A.L.; Shapiro, D.J.; Bartoces, M.; Enns, E.A.; File, T.M., Jr.; Finkelstein, J.A.; Gerber, J.S.; Hyun, D.Y.; Linder, J.A.; et al. Prevalence of Inappropriate Antibiotic Prescriptions Among US Ambulatory Care Visits, 2010–2011. JAMA 2016, 315, 1864–1873. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hersh, A.L.; King, L.M.; Shapiro, D.J.; Hicks, L.A.; Fleming-Dutra, K.E. Unnecessary Antibiotic Prescribing in US Ambulatory Care Settings, 2010–2015. Clin. Infect. Dis. 2021, 72, 133–137. [Google Scholar] [CrossRef]
- Chua, K.-P.; Fischer, M.A.; Linder, J.A. Appropriateness of outpatient antibiotic prescribing among privately insured US patients: ICD-10-CM based cross sectional study. BMJ 2019, 364, k5092. [Google Scholar] [CrossRef] [Green Version]
- Dolk, F.C.K.; Pouwels, K.B.; Smith, D.R.M.; Robotham, J.V.; Smieszek, T. Antibiotics in primary care in England: Which antibiotics are prescribed and for which conditions? J. Antimicrob. Chemother. 2018, 73 (Suppl. 2), ii2–ii10. [Google Scholar] [CrossRef]
- Smieszek, T.; Pouwels, K.B.; Dolk, F.C.K.; Smith, D.; Hopkins, S.; Sharland, M.; Hay, A.; Moore, M.; Robotham, J.V. Potential for reducing inappropriate antibiotic prescribing in English primary care. J. Antimicrob. Chemother. 2018, 73 (Suppl. 2), ii36–ii43. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pouwels, K.B.; Dolk, F.C.K.; Smith, D.R.M.; Robotham, J.V.; Smieszek, T. Actual versus ‘ideal’ antibiotic prescribing for common conditions in English primary care. J. Antimicrob. Chemother. 2018, 73 (Suppl. 2), 19–26. [Google Scholar] [CrossRef]
- Ontario, C.A. Get Coverage for Prescription Drugs. Available online: http://www.ontario.ca/page/get-coverage-prescription-drugs (accessed on 1 December 2021).
- PharmaCare Drug Review Results. Available online: https://fmdb.hlth.gov.bc.ca/ (accessed on 28 September 2021).
- Government of Canada Statistics Canada. Population Estimates, Quarterly. Published 18 March 2021. Available online: https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1710000901 (accessed on 17 May 2021).
- Blondel-Hill, E.; Fryters, S. Bugs & Drugs: An Antimicrobial/Infectious Diseases Reference; Alberta Health Services: Edmonton, AB, Canada, 2012. [Google Scholar]
- Healthcare Professionals. Do Bugs Need Drugs? Available online: http://www.dobugsneeddrugs.org/health-care-professionals/ (accessed on 1 December 2021).
- Antimicrobial Awareness Week Canada. Available online: https://antibioticawareness.ca/ (accessed on 2 October 2021).
- Born, K.B.; Leis, J.A.; Gold, W.L.; Levinson, W. “Choosing Wisely Canada” and antimicrobial stewardship: A shared focus on reducing unnecessary care. Can. Commun. Dis. Rep. 2015, 41 (Suppl. 4), 9–13. [Google Scholar] [CrossRef] [PubMed]
- Levy, A.R.; O’Brien, B.J.; Sellors, C.; Grootendorst, P.; Willison, N. Coding accuracy of administrative drug claims in the Ontario Drug Benefit database. Can. J. Clin. Pharmacol. J. Can. Pharmacol. Clin. 2003, 10, 67–71. [Google Scholar]
- Cadieux, G.; Tamblyn, R. Accuracy of Physician Billing Claims for Identifying Acute Respiratory Infections in Primary Care. Health Serv. Res. 2008, 43, 2223–2238. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- BC Ministry of Health [Creator]. PharmaNet. V2. BC Ministry of Health [Publisher]. Data Extract. Data Stewardship Committee. 2011. Available online: http://www.popdata.bc.ca/data (accessed on 1 December 2021).
- British Columbia Ministry of Health [creator]. Medical Services Plan (MSP) Payment Information File. V2. Population Data BC [publisher]. Data Extract. MOH. 2011. Available online: http://www.popdata.bc.ca/data (accessed on 1 December 2021).
- British Columbia Ministry of Health. Diagnostic Code Descriptions (ICD-9)-Province of British Columbia. Available online: https://www2.gov.bc.ca/gov/content/health/practitioner-professional-resources/msp/physicians/diagnostic-code-descriptions-icd-9 (accessed on 1 December 2021).
- ICD-9 International Classification of Diseases, Ninth Revision. Published 1 March 2019. Available online: https://www.cdc.gov/nchs/icd/icd9.htm (accessed on 3 November 2020).
- Saatchi, A.; Morris, A.M.; Patrick, D.M.; Mccormack, J.; Reyes, R.C.; Morehouse, P.; Reid, J.; Shariff, S.; Povitz, M.; Silverman, M.; et al. Outpatient antibiotic use in British Columbia, Canada: Reviewing major trends since 2000. JAC-Antimicrobial. Resist. 2021, 3, dlab116. [Google Scholar] [CrossRef] [PubMed]
- WHO Collaborating Centre for Drug Statistics Methodology, Folkehelseinstituttet (Noruega). Guidelines for ATC Classification and DDD Assignment 2011. WHO Collaborating Centre for Drug Statistics Methodology: Norwegian Institute of Public Health. 2010. Available online: http://www.whocc.no/filearchive/publications/2011guidelines.pdf (accessed on 15 April 2020).
- IntelliHealth Ontario. Available online: https://intellihealth.moh.gov.on.ca (accessed on 28 September 2021).
- British Columbia Ministry of Health [creator]. Consolidation File (MSP Registration & Premium Billing). V2. Population Data BC [publisher]. Data Extract. MOH. 2011. Available online: http://www.popdata.bc.ca/data (accessed on 1 December 2021).
| Cohort Characteristics (N) | British Columbia | Ontario | ||||||
|---|---|---|---|---|---|---|---|---|
| Overall | 2000 | 2009 | 2018 | Overall | 2000 | 2009 | 2018 | |
| Total Unique Patients | 4,858,511 | 201,610 | 244,228 | 319,057 | 13,998,138 | 601,759 | 703,900 | 946,499 |
| Number of patients by age (%) | ||||||||
| 65–79 | 3,389,791 (69.8%) | 146,173 (72.5%) | 167,001 (68.4%) | 227,559 (71.3%) | 9,980,422 (71.3%) | 456,569 (75.9%) | 494,359 (70.2%) | 674,699 (71.3%) |
| 80+ | 1,468,720 (30.2%) | 55,437 (27.5%) | 77,227 (31.6%) | 91,498 (28.7%) | 4,017,836 (28.7%) | 145,190 (24.1%) | 209,541 (29.8%) | 271,800 (28.7%) |
| Number of patients by sex (%) | ||||||||
| Female | 2,752,378 (56.7%) | 114,265 (56.7%) | 138,883 (56.9%) | 178,936 (56.1%) | 8,189,152 (58.5%) | 355,282 (59.0%) | 413,658 (58.8%) | 545,627 (57.6%) |
| Male | 2,103,436 (43.3%) | 86,900 (43.1%) | 105,257 (43.1%) | 140,115 (43.9%) | 5,809,106 (41.5%) | 246,477 (41.0%) | 290,242 (41.2%) | 400,872 (42.4%) |
| Number of patients by income quintile 1 (%) | ||||||||
| Quintile 2 1 (Lowest) | 1,031,509 (21.2%) | 47,707 (23.7%) | 52,032 (21.3%) | 64,684 (20.3%) | 2,813,645 (20.1%) | 128,790 (21.4%) | 135,953 (19.3%) | 192,716 (20.4%) |
| Quintile 2 | 979,783 (20.2%) | 39,759 (19.7%) | 50,011 (20.5%) | 63,912 (20.0%) | 2,938,637 (21.0%) | 133,887 (22.2%) | 144,402 (20.5%) | 198,441 (21.0%) |
| Quintile 3 | 920,488 (19.0%) | 36,471 (18.1%) | 46,374 (19%) | 61,574 (19.3%) | 2,772,633 (19.8%) | 120,285 (20.0%) | 138,695 (19.7%) | 188,395 (19.9%) |
| Quintile 4 | 888,518 (18.3%) | 33,419 (16.6%) | 44,544 (18.2%) | 61,254 (19.2%) | 2,670,403 (19.1%) | 105,682 (17.6%) | 140,380 (19.9%) | 177,228 (18.7%) |
| Quintile 5 (Highest) | 949,983 (19.6%) | 36,246 (18.0%) | 47,952 (19.6%) | 63,341 (19.9%) | 2,761,308 (19.7%) | 111,744 (18.6%) | 141,974 (20.2%) | 187,176 (19.8%) |
| Missing 3 | 71,014 (14.6%) | 7475 (3.7%) | 2458 (1.0%) | 2764 (0.9%) | 40,261 (0.003%) | 1371 (0.2%) | 2496 (0.4%) | 2543 (0.3%) |
| Number of patients by rural/urban status 4 (%) | ||||||||
| Rural | 803,136 (16.5%) | 32,303 (16.0%) | 40,565 (16.6%) | 54,185 (17.0%) | 1,806,438 (12.9%) | 87,610 (14.6%) | 91,868 (13.1%) | 110,068 (11.6%) |
| Urban | 3,882,869 (80.0%) | 162,064 (80.4%) | 194,937 (79.8%) | 254,485 (79.8%) | 1,2178,924 (87.0%) | 513,854 (85.4%) | 612,025 (86.9%) | 834,225 (88.1%) |
| Missing | 172,506 (35.5%) | 7243 (3.6%) | 8726 (35.7%) | 10,387 (3.3%) | 12,896 (0.01%) | 295 (0.0%) | 7 (0.0%) | 2206 (0.2%) |
| Total antibiotic prescriptions (N) | 11,166,401 | 450,517 | 557,931 | 721,191 | 27,656,014 | 1,197,646 | 1,393,583 | 1,865,267 |
| Total indication-associated prescriptions (N) | 10,444,129 | 409,280 | 508,372 | 645,183 | 13,793,763 | 622,917 | 682,192 | 934,958 |
| Total unlinked 5 prescriptions (N) | 722,272 | 41,237 | 49,559 | 76,008 | 13,862,251 | 574,729 | 711,391 | 930,309 |
| Diagnosis Category | British Columbia | Ontario | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 2000 1 | 2018 | Percent Change 2 | Spearman Coefficient | p Value 3 | 2000 | 2018 | Percent Change | Spearman Coefficient | p Value | |
| Tier 1 | 123 | 177 | 44 | 0.96 | <0.0001 | 95 | 121 | 27 | 1.00 | <0.0001 |
| Miscellaneous bacterial | 2 | 18 | 800 | 1.00 | <0.0001 | 1 | 3 | 200 | 1.00 | <0.0001 |
| Pneumonia | 27 | 30 | 11 | 0.93 | <0.0001 | 27 | 29 | 7 | 0.9 | 0.053 |
| Urinary tract infection | 94 | 129 | 37 | 0.23 | <0.0001 | 67 | 89 | 33 | 0.29 | <0.0001 |
| Tier 2 | 93 | 95 | 2 | 0.97 | 0.058 | 64 | 74 | 16 | 1.00 | <0.0001 |
| Pharyngitis | 2 | 1 | −50 | −0.51 | <0.0001 | 4 | 3 | −25 | 0.95 | 0.76 |
| Sinusitis | 22 | 25 | 14 | 0.96 | <0.0001 | 19 | 23 | 21 | 0.99 | <0.0001 |
| Otitis media | 6 | 3 | −50 | −0.37 | <0.0001 | 3 | 2 | −33 | 0.60 | <0.0001 |
| Skin and soft tissue infection | 58 | 62 | 7 | 0.97 | <0.0001 | 37 | 44 | 19 | 0.99 | <0.0001 |
| Acne | 1 | 1 | 0 | 0.26 | <0.0001 | 1 | 1 | 0 | 0.97 | <0.0001 |
| Gastrointestinal infections | 4 | 4 | 0 | 0.69 | <0.0001 | 3 | 3 | 0 | 0.98 | <0.0001 |
| Tier 3 | 396 | 306 | −23 | 0.89 | <0.0001 | 249 | 187 | −25 | 0.88 | <0.0001 |
| Asthma/allergy | 17 | 9 | −47 | 0.29 | <0.0001 | 12 | 6 | −50 | −0.31 | <0.0001 |
| Bronchitis | 79 | 81 | 3 | 0.95 | <0.0001 | 95 | 64 | −33 | 0.52 | <0.0001 |
| Influenza | 5 | 3 | −40 | 0.33 | <0.0001 | 4 | 2 | −50 | −0.35 | <0.0001 |
| Non-suppurative OM | 2 | 1 | −50 | −0.14 | <0.0001 | 4 | 3 | −25 | 0.72 | <0.0001 |
| Viral URTI | 77 | 34 | −56 | −0.80 | <0.0001 | 59 | 37 | −37 | 0.36 | <0.0001 |
| Other respiratory tract | 69 | 34 | −51 | −0.67 | <0.0001 | 15 | 18 | 20 | 0.98 | <0.0001 |
| Other genitourinary conditions | 87 | 90 | 3 | 0.92 | <0.0001 | 25 | 23 | −8 | 0.99 | <0.0001 |
| Other skin, cutaneous and mucosal conditions | 60 | 53 | −12 | 0.94 | <0.0001 | 35 | 33 | −6 | 0.96 | <0.0001 |
| Miscellaneous non-bacterial | 1 | 2 | 100 | 0.92 | <0.0001 | 1 | 1 | 0 | 0.99 | <0.0001 |
| Unlinked Antibiotics 4 | 78 | 83 | 6 | 0.38 | <0.0001 | 377 | 380 | 1 | 1.00 | <0.0001 |
| Antibiotic (ATC Class) | British Columbia | Ontario | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 2000 1 | 2018 | Percent Change 2 | Spearman Coefficient | p Value 3 | 2000 | 2018 | Percent Change | Spearman Coefficient | p Value | |
| Overall (J01) | 775 | 707 | −9 | 0.95 | <0.0001 | 408 | 382 | −6 | 0.97 | <0.0001 |
| Tetracyclines (J01A) | 33 | 67 | 103 | 0.91 | <0.0001 | 5 | 7 | 40 | −0.48 | <0.0001 |
| Beta-Lactam Penicillins (J01C) | 129 | 138 | 7 | 0.75 | <0.0001 | 82 | 93 | 13 | 0.61 | <0.0001 |
| Other Beta-Lactams (J01D) | 153 | 134 | −13 | 0.94 | <0.0001 | 69 | 70 | 1 | 0.94 | <0.0001 |
| Sulfonamides & Trimethoprim (J01E) | 71 | 45 | −37 | 0.97 | <0.0001 | 32 | 17 | −47 | −0.28 | <0.0001 |
| Macrolides, Lincosamides and Streptogramins (J01F) | 148 | 82 | −44 | −0.28 | <0.0001 | 105 | 74 | −30 | 0.48 | <0.0001 |
| Quinolones (J01M) | 192 | 136 | −29 | 0.36 | <0.0001 | 101 | 69 | −32 | 0.59 | <0.0001 |
| Other Antibacterials (J01X) | 50 | 105 | 109 | 0.97 | <0.0001 | 15 | 52 | 247 | 1.00 | <0.0001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Saatchi, A.; Reid, J.N.; Povitz, M.; Shariff, S.Z.; Silverman, M.; Morris, A.M.; Reyes, R.C.; Patrick, D.M.; Marra, F. Appropriateness of Outpatient Antibiotic Use in Seniors across Two Canadian Provinces. Antibiotics 2021, 10, 1484. https://doi.org/10.3390/antibiotics10121484
Saatchi A, Reid JN, Povitz M, Shariff SZ, Silverman M, Morris AM, Reyes RC, Patrick DM, Marra F. Appropriateness of Outpatient Antibiotic Use in Seniors across Two Canadian Provinces. Antibiotics. 2021; 10(12):1484. https://doi.org/10.3390/antibiotics10121484
Chicago/Turabian StyleSaatchi, Ariana, Jennifer N. Reid, Marcus Povitz, Salimah Z. Shariff, Michael Silverman, Andrew M. Morris, Romina C. Reyes, David M. Patrick, and Fawziah Marra. 2021. "Appropriateness of Outpatient Antibiotic Use in Seniors across Two Canadian Provinces" Antibiotics 10, no. 12: 1484. https://doi.org/10.3390/antibiotics10121484
APA StyleSaatchi, A., Reid, J. N., Povitz, M., Shariff, S. Z., Silverman, M., Morris, A. M., Reyes, R. C., Patrick, D. M., & Marra, F. (2021). Appropriateness of Outpatient Antibiotic Use in Seniors across Two Canadian Provinces. Antibiotics, 10(12), 1484. https://doi.org/10.3390/antibiotics10121484





