Efficacy of Thai Plant Extracts for Antibacterial and Anti-Biofilm Activities against Pathogenic Bacteria
Abstract
:1. Introduction
2. Results
2.1. Antibacterial Activity of Plant Extracts
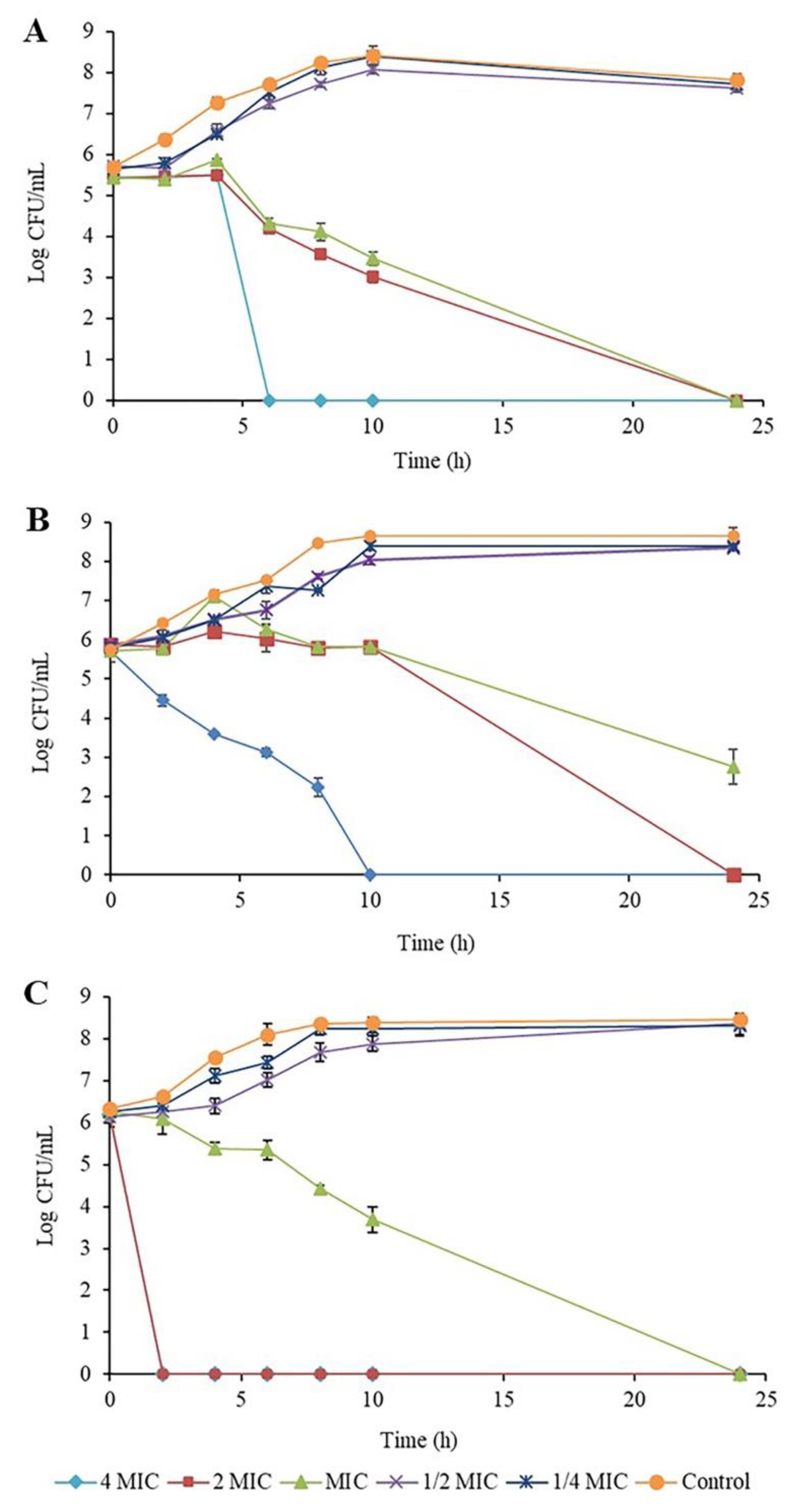
2.2. Time-Kill Kinetic Assay of Piper betle Extract against the Bacteria
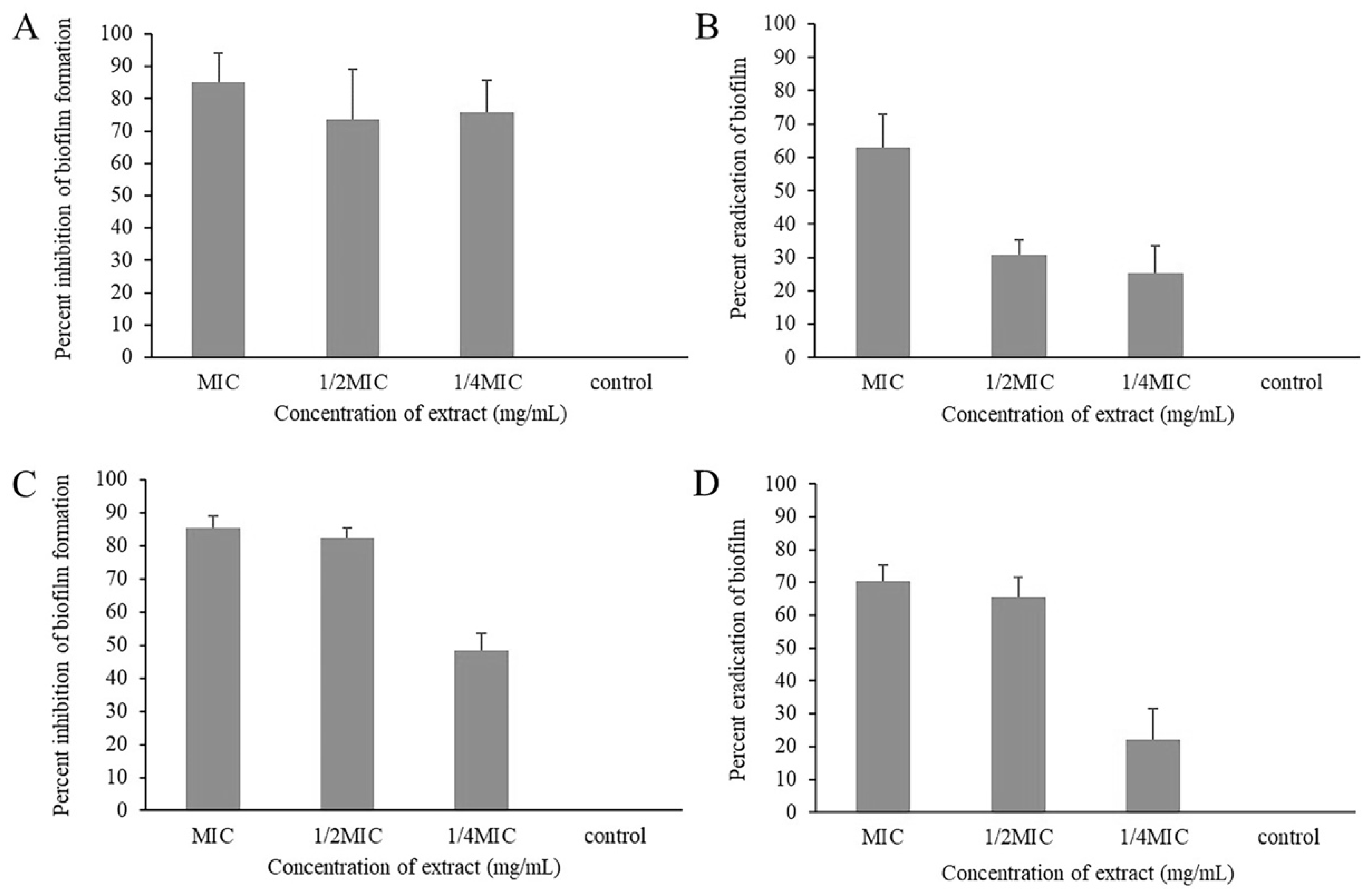
2.3. Biofilm Inhibitory and Eradicating Activity of Piper betle Extract
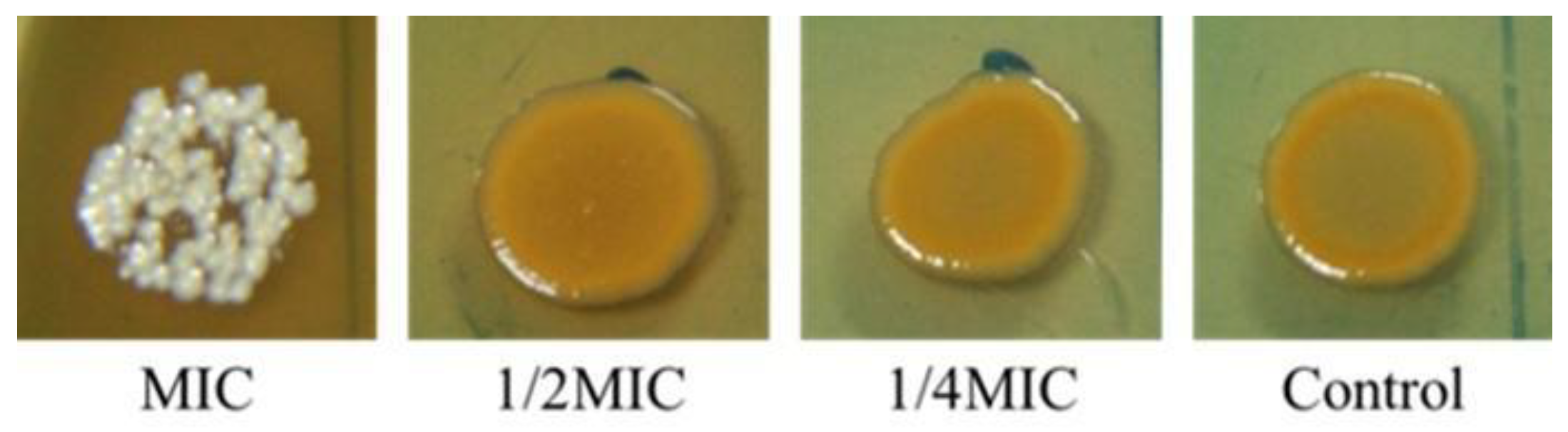
2.4. Inhibition of Staphyloxanthin Biosynthesis in Staphylococcus aureus by Piper betle
2.5. Phytochemical Analysis of Piper betle Leaf Extract
3. Discussion
4. Materials and Methods
4.1. Plant Materials and Extract Preparation
4.2. Bacterial Strains and Growth Conditions
4.3. Evaluation of Antibacterial Activity
4.3.1. Determination of Minimum Inhibitory Concentrations (MICs)
4.3.2. Determination of Minimum Bactericidal Concentrations (MBCs)
4.3.3. Time-Kill Assay
4.4. Evaluation of Anti-Biofilm Activity
4.4.1. Biofilm Formation
4.4.2. Biofilm Eradication
4.4.3. Production of Staphyloxanthin
4.5. Bioactive Compound Assay
4.6. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Abebe, G.M. The Role of Bacterial Biofilm in Antibiotic Resistance and Food Contamination. Int. J. Microbiol. 2020, 2020, 1705814. [Google Scholar] [CrossRef]
- Reuben, R.; Roy, P.; Sarkar, S.; Ha, S.-D.; Jahid, I.K. Multispecies interactions in biofilms and implications to safety of drinking water distribution system. Microbiol. Biotechnol. Lett. 2019, 47, 473–486. [Google Scholar] [CrossRef]
- Olsen, I. Biofilm-specific antibiotic tolerance and resistance. Eur. J. Clin. Microbiol. Infect. Dis. 2015, 34, 877–886. [Google Scholar] [CrossRef]
- Kim, N.-H.; Kang, Y.M.; Han, W.D.; Park, K.U.; Park, K.-H.; Yoo, J.I.; Lee, D.-G.; Park, C.; Song, K.-H.; Kim, E.S.; et al. Small-colony variants in persistent and recurrent Staphylococcus aureus bacteremia. Microb. Drug Resist. 2016, 22, 538–544. [Google Scholar] [CrossRef]
- Barbieri, R.; Coppo, E.; Marchese, A.; Daglia, M.; Sobarzo-Sánchez, E.; Nabavi, S.F.; Nabavi, S.M. Phytochemicals for human disease: An update on plant-derived compounds antibacterial activity. Microbiol. Res. 2017, 196, 44–68. [Google Scholar] [CrossRef] [PubMed]
- Jarriyawattanachaikul, W.; Chaveerach, P.; Chokesajjawatee, N. Antimicrobial activity of Thai-herbal plants against food-borne pathogens E. coli, S. aureus and C. jejuni. Agric. Agric. Sci. Procedia 2016, 11, 20–24. [Google Scholar] [CrossRef]
- Siriwatanametanon, N.; Dodgson, W.; Dodgson, J. Investigation of antimicrobial activity of 13 Thai medicinal plants against bacteria and fungi. J. Pure Appl. Microbiol. 2017, 11, 1351–1356. [Google Scholar] [CrossRef]
- Parichat, P.; Kanit, V.; Jaehong, H.; Sukanda, V. High antioxidant and phenolic contents related to antibacterial activity against gastrointestinal pathogenic bacteria of some Thai medicinal plants. Pharmacogn. J. 2018, 10, 341–348. [Google Scholar]
- Teanpaisan, R.; Kawsud, P.; Pahumunto, N.; Puripattanavong, J. Screening for antibacterial and antibiofilm activity in Thai medicinal plant extracts against oral microorganisms. J. Tradit. Complement. Med. 2017, 7, 172–177. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Beloborodova, N.V.; Bairamov, I.T.; Olenin, A.Y. Microbial biofilms produce higher concentrations of sepsis-associated exometabolites compared with the planktonic phenotype. Glob. J. Pathol. Microbiol. 2017, 5, 15–25. [Google Scholar]
- Woo, C.S.J.; Lau, J.S.H.; El-Nezami, H. Chapter 10-herbal medicine: Toxicity and recent trends in assessing their potential toxic effects. Adv. Bot. Res. 2012, 62, 365–384. [Google Scholar]
- Huie, C.W. A review of modern sample-preparation techniques for the extraction and analysis of medicinal plants. Anal. Bioanal. Chem. 2002, 373, 23–30. [Google Scholar] [CrossRef] [PubMed]
- Ríos, J.L.; Recio, M.C. Medicinal plants and antimicrobial activity. J. Ethnopharmacol. 2005, 100, 80–84. [Google Scholar] [CrossRef]
- Radhakrishnan, N.; Gnanamani, A.; Mandal, A.B. A potential antibacterial agent Embelin, a natural benzoquinone extracted from Embelia ribes. Biol. Med. 2011, 3, 1–7. [Google Scholar]
- Resch, A.; Rosenstein, R.; Nerz, C.; Götz, F. Differential gene expression profiling of Staphylococcus aureus cultivated under biofilm and planktonic conditions. Appl. Environ. Microbiol. 2005, 71, 2663–2676. [Google Scholar] [CrossRef] [Green Version]
- Altemimi, A.; Lakhssassi, N.; Baharlouei, A.; Watson, D.G.; Lightfoot, D.A. Phytochemicals: Extraction, isolation, and identifica-tion of bioactive compounds from plant extracts. Plants 2017, 6, 42. [Google Scholar] [CrossRef] [PubMed]
- Siddique, S.; Parveen, Z.; Firdaus, E.B.; Mazhar, S. Chemical composition, antibacterial and antioxidant activities of essential oils from leaves of three Melaleuca species of Pakistani flora. Arab. J. Chem. 2020, 13, 67–74. [Google Scholar] [CrossRef]
- Siddique, S.; Parveen, Z.; Firdaus, E.B.; Chaudhary, M.N.; Mazhar, S.; Nawaz, S. The essential oil of Melaleuca armillaris (Sol. ex Gaertn.) Sm. leaves from Pakistan: A potential source of eugenol methyl ether. Ind. Crop. Prod. 2017, 109, 912–917. [Google Scholar] [CrossRef]
- Mahdavi, B.; Yaacob, W.A.; Din, L.B. Chemical composition, antioxidant, and antibacterial activity of essential oils from Etlingera sayapensis A.D. Poulsen & Ibrahim. Asian Pac. J. Trop. Med. 2017, 10, 819–826. [Google Scholar] [CrossRef]
- Xu, J.-G.; Liu, T.; Hu, Q.-P.; Cao, X.-M. Chemical composition, antibacterial properties and mechanism of action of essential oil from clove buds against Staphylococcus aureus. Molecules 2016, 21, 1194. [Google Scholar] [CrossRef]
- Božik, M.; Nový, P.; Klouček, P. Susceptibility of postharvest pathogens to esential oils. Sci. Agric. Bohem. 2017, 48, 103–111. [Google Scholar] [CrossRef] [Green Version]
- Olszewska, M.A.; Gędas, A.; Simões, M. The effects of eugenol, trans-cinnamaldehyde, citronellol, and terpineol on Escherichia coli biofilm control as assessed by culture-dependent and -independent methods. Molecules 2020, 25, 2641. [Google Scholar] [CrossRef]
- CLSI. M100 Performance Standards for Susceptibility Testing; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2018. [Google Scholar]
- Jantorn, P.; Heemmamad, H.; Soimala, T.; Indoung, S.; Saising, J.; Chokpaisarn, J.; Wanna, W.; Tipmanee, V.; Saeloh, D. Antibiotic resistance profile and biofilm production of Staphylococcus pseudintermedius isolated from dogs in Thailand. Pharmaceuticals 2021, 14, 592. [Google Scholar] [CrossRef] [PubMed]
- Saising, J.; Ongsakul, M.; Voravuthikunchai, S.P. Rhodomyrtus tomentosa (Aiton) Hassk. ethanol extract and rhodomyrtone: A potential strategy for the treatment of biofilm-forming staphylococci. J. Med. Microbiol. 2011, 60, 1793–1800. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Medicinal Plant | Common Name | Local Name | Plant Part | Susceptibility Testing (mg/mL) | ||
|---|---|---|---|---|---|---|
| S. aureus ATCC29213 | MRSA NPRC001R | E. coli ATCC25922 | ||||
| Artocarpus lakoocha Roxb. | Green Tampang | Ka noon pa | Leaf | 10/10 | 10/10 | 10/>10 |
| Boesenbergia rotunda (Roxb.) Schltr. | Fingerroot | Krachai | Rhizome | 0.15/0.15 | 0.15/0.15 | >10/>10 |
| Casearia grewiifolia Vent. | - | Kruai Pa | Fruit | 0.62/0.62 | 1.25/2.5 | >10/>10 |
| Chromolaena odorata (L.) R.M.King & H. Rob. | Christmas bush | Sap suea | leaf | 5/>10 | 10/>10 | >10/>10 |
| Limnophila aromatica (Lam.) Merr | Rice paddy herb | Phak kha Yeang | Whole plant | 2.5/5 | 2.5/5 | >10/>10 |
| Millingtonia hortensis Linn. | Cork tree | Hian | Leaf | 2.5/>2.5 | 2.5/2.5 | 5/>10 |
| Oroxylum indicum (L.) Kurz. | Broken bones plant | Pheka | Leaf | 2.5/>2.5 | 2.5/>2.5 | >10/>10 |
| Piper betle Linn. | Betel | Plue | Leaf | 0.62/0.62 | 0.62/0.62 | 2.5/2.5 |
| Rhodomyrtus tomentosa (Aiton) Hassk. | Rose myrtle | Phruat | Leaf | 0.31/0.62 | 0.62/0.62 | >10/>10 |
| Syzygium cumini Linn. | Black plum | Waa | Leaf | 2.5/5 | 2.5/5 | 10/>10 |
| Xanthostemon chrysanthus (F.Muell.) Benth. | Golden myrtle | Rak raek pop | Leaf | 1.25/2.50 | 1.25/2.50 | >10/>10 |
| Zingiber officinale Roscoe. | Ginger | Khing daeng | Rhizome | 1.25/>10 | >10/>10 | 10/>10 |
| Ziziphus mauritiana Lam. | Jujube | Phutsa | Leaf | 2.5/10 | 5/>10 | >10/>10 |
| Number of Isolates | Antibacterial Activities of Piper betle Ethanol Extract | |
|---|---|---|
| MIC Range (mg/mL) | MBC Range (mg/mL) | |
| MRSA (n = 48) | 0.31–2.5 | 0.31–5.0 |
| E. coli (n = 43) | 1.25–2.5 | 1.25–5.0 |
| No. | RT (min) | CAS RN | Extract Constituent | %Area | %Prob |
|---|---|---|---|---|---|
| 1 | 10.841 | 501-92-8 | 4-Allylphenol | 0.33 | 71.0 |
| 2 | 15.358 | 97-53-0 | Eugenol | 18.80 | 27.4 |
| 3 | 16.891 | 87-44-5 | Caryophyllene | 0.90 | 31.7 |
| 4 | 18.162 | 6753-98-6 | Alpha-caryophyllene | 0.25 | 49.1 |
| 5 | 19.086 | 1460-97-5 | Gamma-cadinene | 1.21 | 29.1 |
| 6 | 20.371 | 13620-82-1 | 4-Allyl-1,2-diacetoxybenzene | 70.32 | 42.2 |
| 7 | 20.938 | 483-76-1 | Delta-cadinene | 0.78 | 33.6 |
| 8 | 23.129 | 6750-60-3 | (-)-Spathulenol | 0.06 | 29.7 |
| 9 | 23.302 | 1139-30-6 | Caryophyllene oxide | 0.07 | 27.4 |
| 10 | 36.594 | 628-97-7 | Hexadecanoic acid, ethyl ester | 0.15 | 45.1 |
| 11 | 39.109 | 150-86-7 | Phytol | 0.76 | 83.5 |
| 12 | 39.992 | 544-35-4 | Linoleic acid ethyl ester | 0.15 | 20.8 |
| 13 | 40.114 | 112-63-0 | Linoleic acid methyl ester | 0.23 | 13.9 |
| 14 | 41.012 | 10236-16-5 | Phytol acetate | 0.76 | 51.4 |
| 15 | 42.057 | 3033-62-3 | Bis(2-(dimethylamino)ethyl) ether | 0.16 | 39.2 |
| 16 | 43.470 | 122-79-2 | Acetic acid, 3-(adamant-2-ylidene-methoxymethyl)-,phenyl ester | 0.10 | 57.8 |
| 17 | 44.000 | 1778-02-5 | 6,16-Dimethyl-20-oxo pregn-5-en-3-yl acetate | 0.13 | 23.2 |
| 18 | 44.403 | 604-09-1 | 14-Hydroxypregn-4-ene-3,20-dione | 0.17 | 22.0 |
| 19 | 45.428 | 23470-00-0 | Glycerol beta-palmitate | 0.69 | 65.0 |
| 20 | 45.575 | 542-44-9 | Glycerol alpha-palmitate | 0.07 | 41.0 |
| 21 | 46.785 | 55268-70-7 | Hexadecanoic acid, 2,3-bis(acetyloxy)propyl ester | 0.24 | 59.8 |
| 22 | 47.785 | 3443-82-1 | Beta-monolinolein | 0.42 | 27.7 |
| 23 | 47.870 | 56797-43-4 | Cis,cis,cis-7,10,13-hexadecatrienal | 0.31 | 29.4 |
| 24 | 48.976 | 55401-63-3 | 9-Octadecenoic acid (Z)-, 2-(acetyloxy)-1-[(acetyloxy)methyl] ethyl ester | 0.22 | 43.5 |
| 25 | 53.759 | 7695-91-2 | DL-alpha-tocopherol | 0.21 | 53.7 |
| 26 | 55.666 | 474-62-4 | Campesterol | 0.30 | 30.2 |
| 27 | 56.364 | 83-48-7 | Stigmasterol | 0.35 | 43.4 |
| 28 | 57.809 | 83-47-6 | Gamma-sitosterol | 1.15 | 75.0 |
| 29 | 59.655 | 1259-10-5 | Cycloartenol acetate | 0.20 | 7.3 |
| 30 | 61.465 | 79897-80-6 | Stigmastan-3,5-diene | 0.51 | 66.0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Saeloh, D.; Visutthi, M. Efficacy of Thai Plant Extracts for Antibacterial and Anti-Biofilm Activities against Pathogenic Bacteria. Antibiotics 2021, 10, 1470. https://doi.org/10.3390/antibiotics10121470
Saeloh D, Visutthi M. Efficacy of Thai Plant Extracts for Antibacterial and Anti-Biofilm Activities against Pathogenic Bacteria. Antibiotics. 2021; 10(12):1470. https://doi.org/10.3390/antibiotics10121470
Chicago/Turabian StyleSaeloh, Dennapa, and Monton Visutthi. 2021. "Efficacy of Thai Plant Extracts for Antibacterial and Anti-Biofilm Activities against Pathogenic Bacteria" Antibiotics 10, no. 12: 1470. https://doi.org/10.3390/antibiotics10121470
APA StyleSaeloh, D., & Visutthi, M. (2021). Efficacy of Thai Plant Extracts for Antibacterial and Anti-Biofilm Activities against Pathogenic Bacteria. Antibiotics, 10(12), 1470. https://doi.org/10.3390/antibiotics10121470







