Source Localization and Classification of Pulmonary Valve-Originated Electrocardiograms Using Volume Conductor Modeling with Anatomical Models
Abstract
1. Introduction
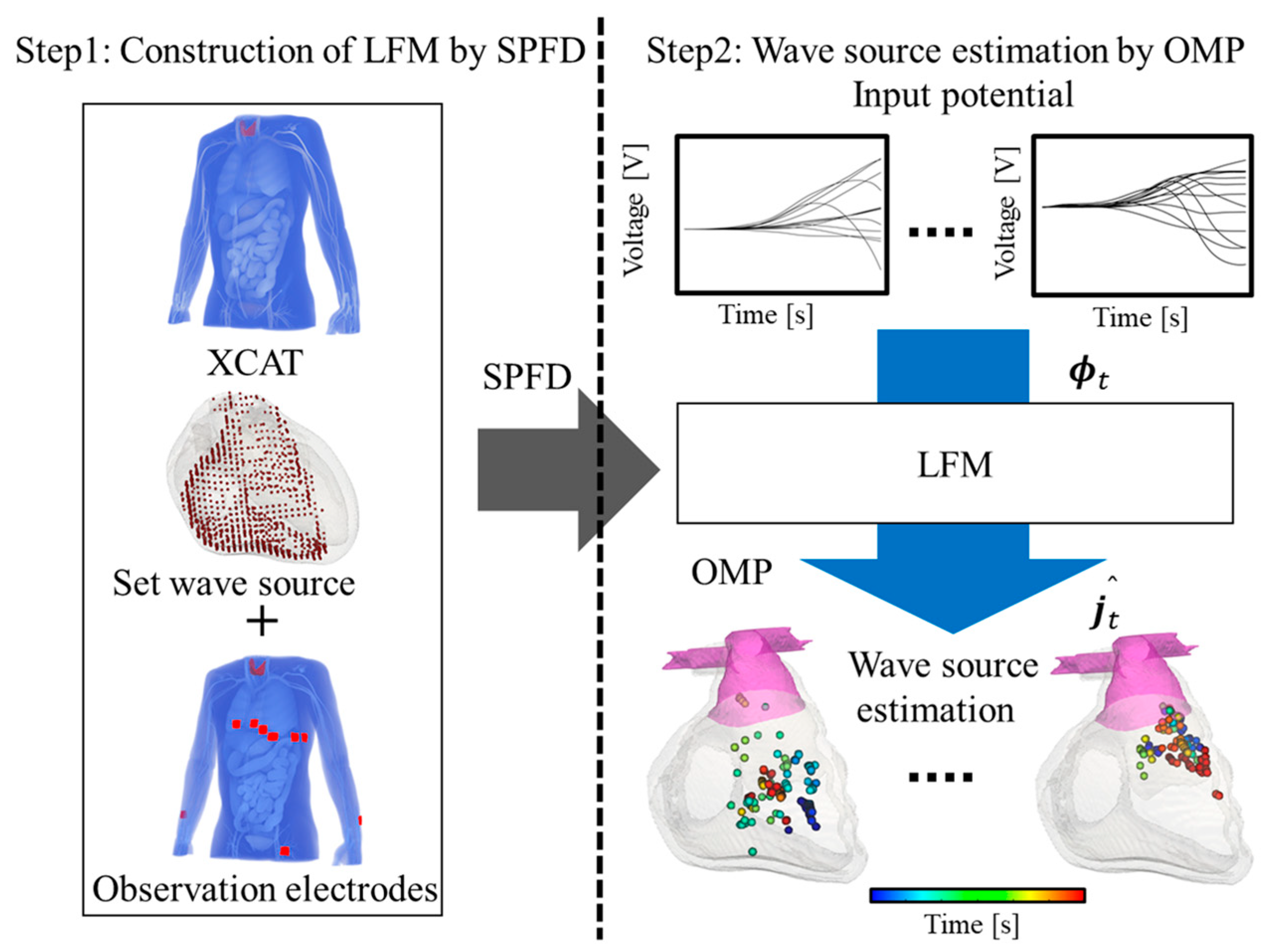
2. Method
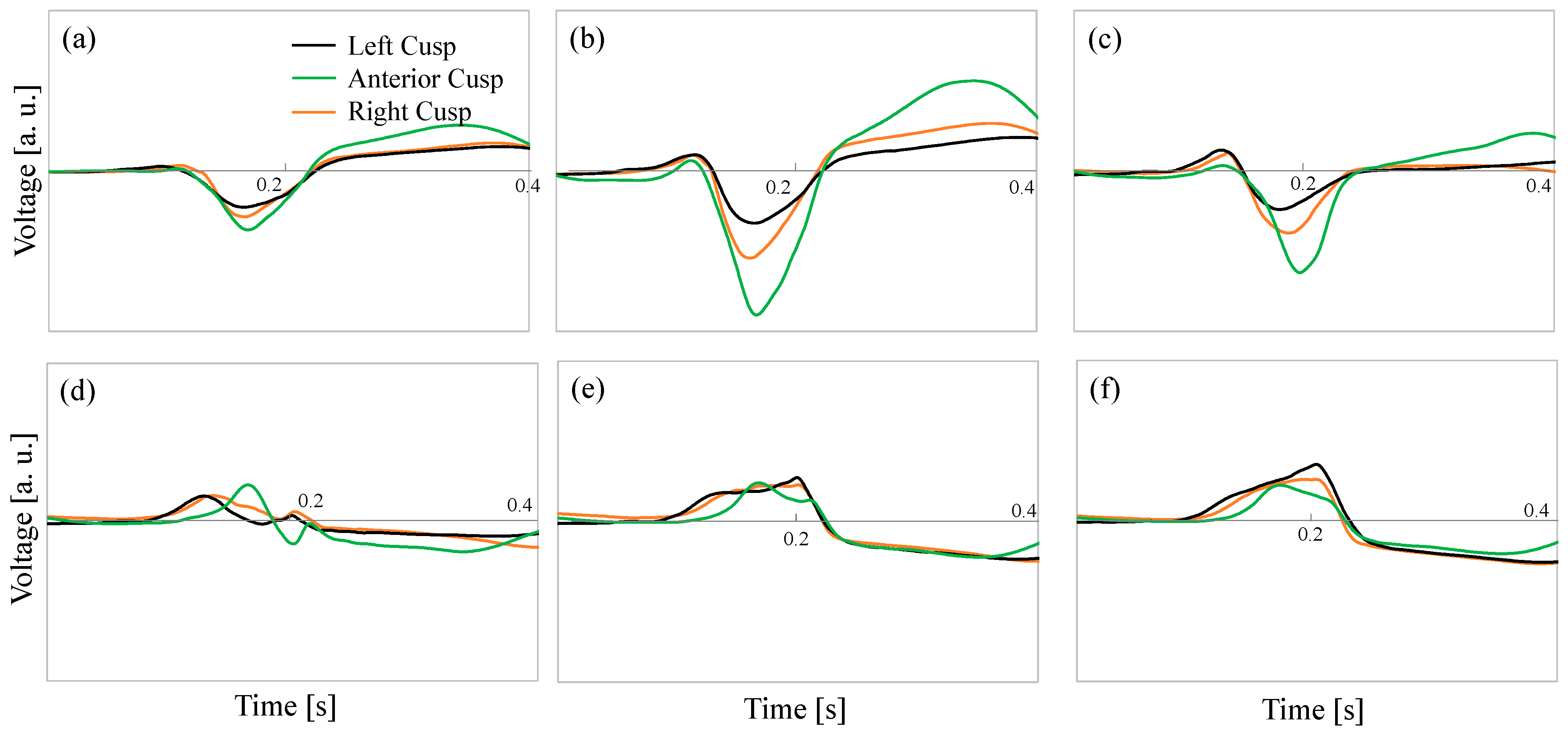
2.1. Data Source and Its Acquisition Scenario
2.2. Human Body Model
2.3. Volume Conductor Model
2.4. Lead Field Matrix
2.5. Scenarios
| Algorithm 1 Pseudocode of the proposed algorithm using orthogonal matching pursuit |
| Initialize current density vector: |
| Initialize support vector: = 0 |
| for |
| end for |
| Estimated source location: |
| Support vector: |
| Reconstruction of current density: |
| Update the residual: |
2.6. Analysis Procedure
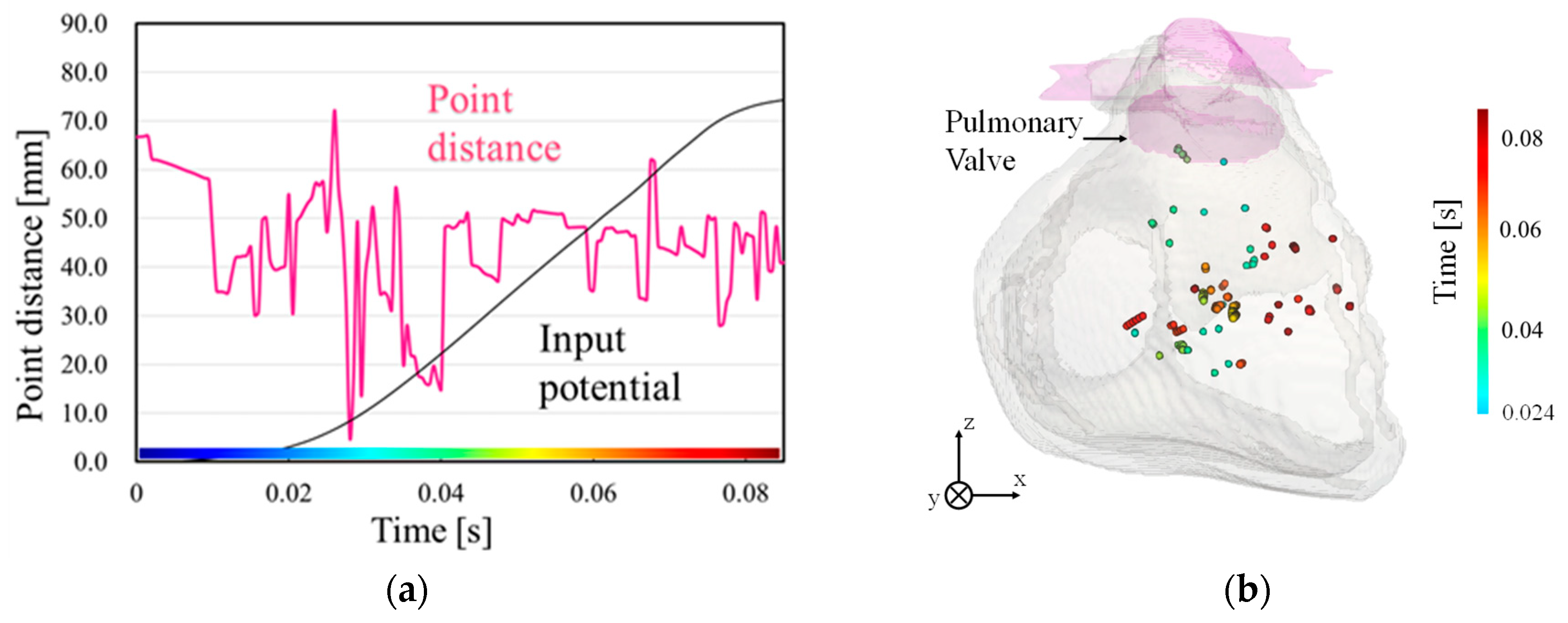
3. Results
4. Discussion and Concluding Remarks
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Amini, M.; Zayeri, F.; Salehi, M. Trend analysis of cardiovascular disease mortality, incidence, and mortality-to-incidence ratio: Results from global burden of disease study 2017. BMC Public Health 2021, 21, 401. [Google Scholar] [CrossRef]
- Kumagai, K. Idiopathic ventricular arrhythmias arising from the left ventricular outflow tract: Tips and tricks. J. Arrhythmia 2014, 30, 211–221. [Google Scholar] [CrossRef]
- Malmivuo, J.; Plonsey, R. Bioelectromagnetism: Principles and Applications of Bioelectric and Biomagnetic Fields; Oxford University Press: New York, NY, USA, 1995. [Google Scholar]
- Huang, S.K.S.; Miller, J.M. Catheter Ablation of Cardiac Arrhythmias: Catheter Ablation of Cardiac Arrhythmias E-Book; Elsevier Health Sciences: Amsterdam, The Netherlands, 2019; Available online: https://www.sciencedirect.com/book/9780323529921/catheter-ablation-of-cardiac-arrhythmias (accessed on 5 September 2024).
- Bhandari, A.; Morady, F.; Shen, E.N.; Schwartz, A.B.; Botvinick, E.; Scheinman, M.M. Catheter-induced His bundle ablation in a patient with reentrant tachycardia associated with a nodoventricular tract. J. Am. Coll. Cardiol. 1984, 4, 611–616. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Di Biase, L.; Wang, Y.; Horton, R.; Gallinghouse, G.J.; Mohanty, P.; Sanchez, J.; Patel, D.; Dare, M.; Canby, R.; Price, L.D. Ablation of atrial fibrillation utilizing robotic catheter navigation in comparison to manual navigation and ablation: Single-center experience. J. Cardiovasc. Electrophysiol. 2009, 20, 1328–1335. [Google Scholar] [CrossRef] [PubMed]
- Cheng, Z.; Deng, H.; Chen, T.; Gao, P.; Zhu, K.; Fang, Q. The R-wave deflection interval in lead V3 combining with R-wave amplitude index in lead V1: A new surface ECG algorithm for distinguishing left from right ventricular outflow tract tachycardia origin in patients with transitional lead at V3. Int. J. Cardiol. 2013, 168, 1342–1348. [Google Scholar] [CrossRef] [PubMed]
- Qin, F.; Zhao, Y.; Bai, F.; Ma, Y.; Sun, C.; Liu, N.; Li, B.; Li, Y.; Liu, C.; Liu, Q. Coupling interval variability: A new diagnostic method for distinguishing left from right ventricular outflow tract origin in idiopathic outflow tract premature ventricular contractions patients with precordial R/S transition at lead V3. Int. J. Cardiol. 2018, 269, 126–132. [Google Scholar] [CrossRef] [PubMed]
- Zheng, J.; Fu, G.; Abudayyeh, I.; Yacoub, M.; Chang, A.; Feaster, W.W.; Ehwerhemuepha, L.; El-Askary, H.; Du, X.; He, B. A high-precision machine learning algorithm to classify left and right outflow tract ventricular tachycardia. Front. Physiol. 2021, 12, 641066. [Google Scholar] [CrossRef]
- Nakasone, K.; Nishimori, M.; Kiuchi, K.; Shinohara, M.; Fukuzawa, K.; Takami, M.; El Hamriti, M.; Sommer, P.; Sakai, J.; Nakamura, T. Development of a visualization deep learning model for classifying origins of ventricular arrhythmias. Circ. J. 2022, 86, 1273–1280. [Google Scholar] [CrossRef]
- Bajaj, S.; Bennett, M.T.; Rabkin, S.W. Identifying Premature Ventricular Complexes from Outflow Tracts Based on PVC Configuration: A Machine Learning Approach. J. Clin. Med. 2023, 12, 5558. [Google Scholar] [CrossRef]
- Liang, W.; Zhang, Y.; Tan, J.; Li, Y. A novel approach to ECG classification based upon two-layered HMMs in body sensor networks. Sensors 2014, 14, 5994–6011. [Google Scholar] [CrossRef]
- Hammad, M.; Meshoul, S.; Dziwiński, P.; Pławiak, P.; Elgendy, I.A. Efficient lightweight multimodel deep fusion based on ECG for arrhythmia classification. Sensors 2022, 22, 9347. [Google Scholar] [CrossRef] [PubMed]
- Xiao, Q.; Lee, K.; Mokhtar, S.A.; Ismail, I.; Pauzi, A.L.b.M.; Zhang, Q.; Lim, P.Y. Deep learning-based ECG arrhythmia classification: A systematic review. Appl. Sci. 2023, 13, 4964. [Google Scholar] [CrossRef]
- Hassaballah, M.; Wazery, Y.M.; Ibrahim, I.E.; Farag, A. Ecg heartbeat classification using machine learning and metaheuristic optimization for smart healthcare systems. Bioengineering 2023, 10, 429. [Google Scholar] [CrossRef] [PubMed]
- Shin, S.-Y.; Joo, H.-J.; Kim, J.-H.; Jang, J.-K.; Park, J.-S.; Kim, Y.-H.; Lee, H.-S.; Choi, J.-I.; Lim, H.-E.; Kim, Y.-H. Epicardial conduction properties and electrocardiographic characteristics of premature ventricular complexes or ventricular tachycardias that originate at the aortic cusp. Korean Circ. J. 2007, 37, 616–622. [Google Scholar] [CrossRef]
- Yamada, T.; Yoshida, N.; Murakami, Y.; Okada, T.; Muto, M.; Murohara, T.; McElderry, H.T.; Kay, G.N. Electrocardiographic characteristics of ventricular arrhythmias originating from the junction of the left and right coronary sinuses of Valsalva in the aorta: The activation pattern as a rationale for the electrocardiographic characteristics. Heart Rhythm 2008, 5, 184–192. [Google Scholar] [CrossRef]
- Im, S.I.; Park, K.-M.; Park, S.-J.; Kim, J.S.; On, Y.K. New electrocardiographic criteria for predicting successful ablation of premature ventricular contractions from the right coronary cusp. Int. J. Cardiol. 2016, 224, 199–205. [Google Scholar] [CrossRef]
- Crozier, A.; Augustin, C.; Neic, A.; Prassl, A.; Holler, M.; Fastl, T.; Hennemuth, A.; Bredies, K.; Kuehne, T.; Bishop, M. Image-based personalization of cardiac anatomy for coupled electromechanical modeling. Ann. Biomed. Eng. 2016, 44, 58–70. [Google Scholar] [CrossRef]
- Corrado, C.; Whitaker, J.; Chubb, H.; Williams, S.; Wright, M.; Gill, J.; O’Neill, M.D.; Niederer, S.A. Personalized models of human atrial electrophysiology derived from endocardial electrograms. IEEE Trans. Biomed. Eng. 2016, 64, 735–742. [Google Scholar] [CrossRef]
- Monaci, S.; Gillette, K.; Puyol-Antón, E.; Rajani, R.; Plank, G.; King, A.; Bishop, M. Automated localization of focal ventricular tachycardia from simulated implanted device electrograms: A combined physics–AI approach. Front. Physiol. 2021, 12, 682446. [Google Scholar] [CrossRef]
- Wisneski, A.D.; Wang, Y.; Cutugno, S.; Pasta, S.; Stroh, A.; Yao, J.; Nguyen, T.C.; Mahadevan, V.S.; Guccione, J.M. Left ventricle biomechanics of low-flow, low-gradient aortic stenosis: A patient-specific computational model. Front. Physiol. 2022, 13, 848011. [Google Scholar] [CrossRef]
- Gao, Y.; Soman, V.V.; Lombardi, J.P.; Rajbhandari, P.P.; Dhakal, T.P.; Wilson, D.G.; Poliks, M.D.; Ghose, K.; Turner, J.N.; Jin, Z. Heart monitor using flexible capacitive ECG electrodes. IEEE Trans. Instrum. Meas. 2019, 69, 4314–4323. [Google Scholar] [CrossRef]
- Tan, R.L.S.; Tey, J.N.; Kerk, W.T.; Lok, B.K. Roll-to-roll manufacturing of printed biosensor electrodes for ECG monitoring. In Proceedings of the 2020 IEEE 22nd Electronics Packaging Technology Conference (EPTC), Singapore, 2–4 December 2020; pp. 213–215. [Google Scholar]
- Huang, Y.; Song, Y.; Gou, L.; Zou, Y. A novel wearable flexible dry electrode based on cowhide for ECG measurement. Biosensors 2021, 11, 101. [Google Scholar] [CrossRef] [PubMed]
- Zheng, J.; Fu, G.; Anderson, K.; Chu, H.; Rakovski, C. A 12-Lead ECG database to identify origins of idiopathic ventricular arrhythmia containing 334 patients. Sci. Data 2020, 7, 98. [Google Scholar] [CrossRef] [PubMed]
- Segars, W.P.; Mahesh, M.; Beck, T.J.; Frey, E.C.; Tsui, B.M. Realistic CT simulation using the 4D XCAT phantom. Med. Phys. 2008, 35, 3800–3808. [Google Scholar] [CrossRef] [PubMed]
- Gabriel, S.; Lau, R.W.; Gabriel, C. The dielectric properties of biological tissues: III. Parametric models for the dielectric spectrum of tissues. Phys. Med. Biol. 1996, 41, 2271–2293. [Google Scholar] [CrossRef]
- Dimbylow, P. Induced current densities from low-frequency magnetic fields in a 2 mm resolution, anatomically realistic model of the body. Phys. Med. Biol. 1998, 43, 221–230. [Google Scholar] [CrossRef]
- Sanjo, K.; Hebiguchi, K.; Tang, C.; Rashed, E.A.; Kodera, S.; Togo, H.; Hirata, A. Sensitivity of Electrocardiogram on Electrode-Pair Locations for Wearable Devices: Computational Analysis of Amplitude and Waveform Distortion. Biosensors 2024, 14, 153. [Google Scholar] [CrossRef]
- Dawson, T.W.; Stuchly, M.A. Analytic validation of a three-dimensional scalar-potential finite-difference code for low-frequency magnetic induction. Appl. Comput. Electromagnet. J. 1996, 11, 72–81. [Google Scholar]
- Laakso, I.; Hirata, A. Fast multigrid-based computation of the induced electric field for transcranial magnetic stimulation. Phys. Med. Biol. 2012, 57, 7753–7765. [Google Scholar] [CrossRef]
- Nakane, T.; Ito, T.; Matsuura, N.; Togo, H.; Hirata, A. Forward electrocardiogram modeling by small dipoles based on whole-body electric field analysis. IEEE Access 2019, 7, 123463–123472. [Google Scholar] [CrossRef]
- Nakano, Y.; Rashed, E.A.; Nakane, T.; Laakso, I.; Hirata, A. ECG localization method based on volume conductor model and Kalman filtering. Sensors 2021, 21, 4275. [Google Scholar] [CrossRef] [PubMed]
- Svehlikova, J.; Teplan, M.; Tysler, M. Geometrical constraint of sources in noninvasive localization of premature ventricular contractions. J. Electrocardiol. 2018, 51, 370–377. [Google Scholar] [CrossRef] [PubMed]
- Svehlikova, J.; Pribilova, A.; Zelinka, J.; Ondrusova, B.; Kromkova, K.; Hlivak, P.; Hatala, R.; Tysler, M. The importance of ECG offset correction for premature ventricular contraction origin localization from clinical data. Meas. Sci. Rev. 2022, 22, 246–252. [Google Scholar] [CrossRef]

| Subjects | Minimum Point Distance (Mean ± SD [mm]) |
|---|---|
| LC (n = 15) | 4.59 ± 8.54 |
| AC (n = 6) | 10.42 ± 12.45 |
| RC (n = 6) | 9.06 ± 6.00 |
| Subject | Origin in the Pulmonary Valve | ||
|---|---|---|---|
| LC | AC | RC | |
| LC (n = 15) | 73.3% (n = 11) | 20.0% (n = 3) | 6.7% (n = 1) |
| AC (n = 6) | 16.7% (n = 1) | 83.3% (n = 5) | 0% |
| RC (n = 6) | 33.3% (n = 2) | 0% | 66.7% (n = 4) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ogawa, K.; Hirata, A. Source Localization and Classification of Pulmonary Valve-Originated Electrocardiograms Using Volume Conductor Modeling with Anatomical Models. Biosensors 2024, 14, 513. https://doi.org/10.3390/bios14100513
Ogawa K, Hirata A. Source Localization and Classification of Pulmonary Valve-Originated Electrocardiograms Using Volume Conductor Modeling with Anatomical Models. Biosensors. 2024; 14(10):513. https://doi.org/10.3390/bios14100513
Chicago/Turabian StyleOgawa, Kota, and Akimasa Hirata. 2024. "Source Localization and Classification of Pulmonary Valve-Originated Electrocardiograms Using Volume Conductor Modeling with Anatomical Models" Biosensors 14, no. 10: 513. https://doi.org/10.3390/bios14100513
APA StyleOgawa, K., & Hirata, A. (2024). Source Localization and Classification of Pulmonary Valve-Originated Electrocardiograms Using Volume Conductor Modeling with Anatomical Models. Biosensors, 14(10), 513. https://doi.org/10.3390/bios14100513





