Salivary Diagnostics in Pediatrics and the Status of Saliva-Based Biosensors
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Participants
2.3. Data Collection
3. Salivary Biomarkers as Diagnostic Tools in Autoimmune Disorders
3.1. Metabolomics
3.2. Proteomics
4. Salivary Biomarkers as Diagnostic Tools in Developmental Conditions
4.1. Metabolomics
4.2. Proteomics
4.3. Genomics
4.4. Transcriptomics
4.5. Microbiomics
5. Salivary Biomarkers as Diagnostic Tools in Neuropsychiatry
5.1. Metabolomics
5.2. Proteomics
5.3. Genomics
5.4. Transcriptomics
5.5. Microbiomics
6. Salivary Biomarkers as Diagnostic Tools in Metabolic, Gastrointestinal, and Pulmonary Diseases
6.1. Metabolomics
6.2. Proteomics
6.3. Microbiomics
7. Salivary Biomarkers as Diagnostic Tools in Oral Diseases
7.1. Metabolomics
7.2. Proteomics
7.3. Microbiomics
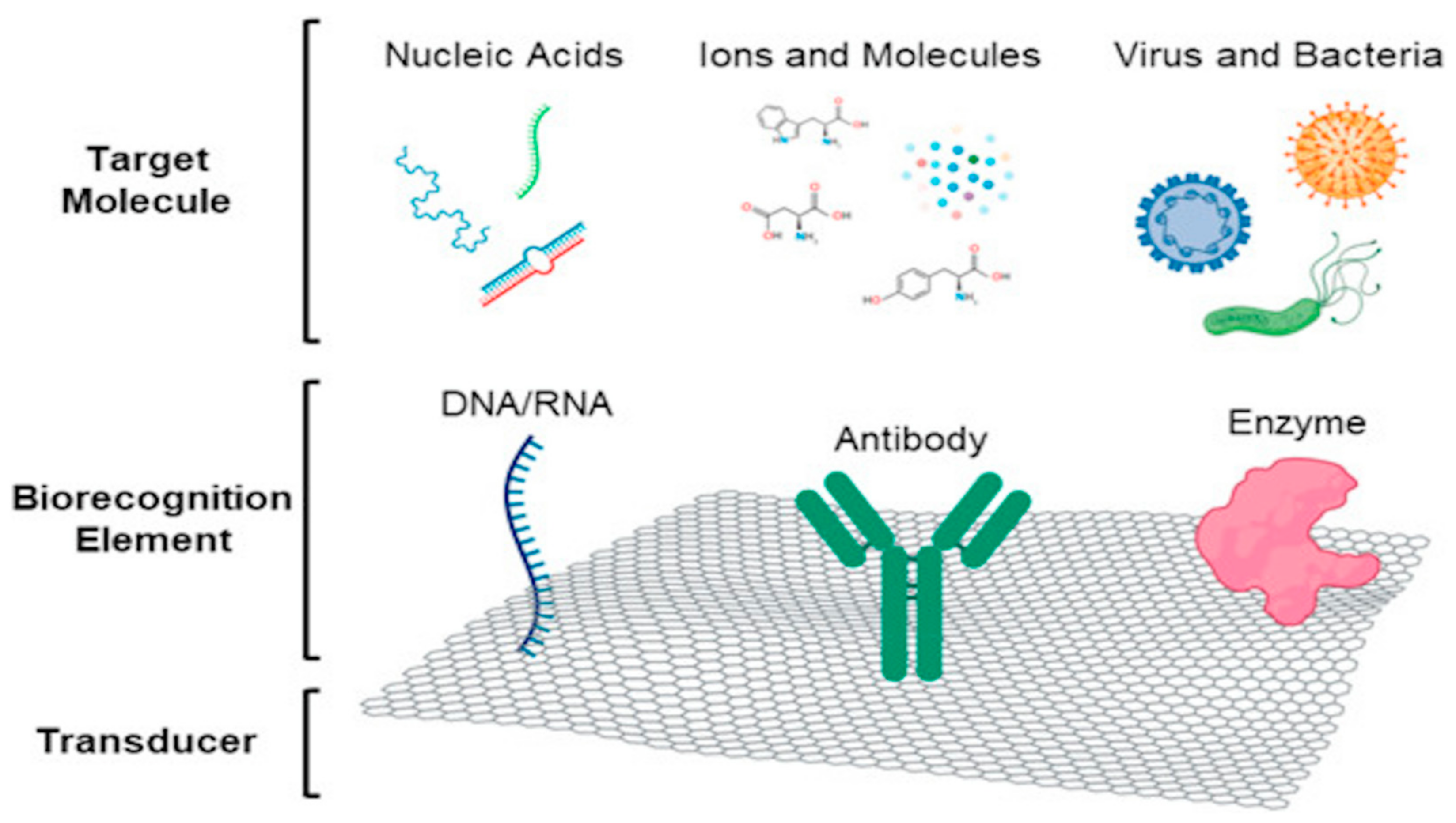
8. Current Status and Advances in Saliva-Based Biosensors
9. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Aral, C.A.; Nalbantoglu, O.; Nur, B.G.; Altunsoy, M.; Aral, K. Metabolic control and periodontal treatment decreases elevated oxidative stress in the early phases of type 1 diabetes onset. Arch. Oral Biol. 2017, 82, 115–120. [Google Scholar] [CrossRef] [PubMed]
- Collin, M.; Ernberg, M.; Christidis, N.; Hedenberg-Magnusson, B. Salivary biomarkers in children with juvenile idiopathic arthritis and healthy age-matched controls: A prospective observational study. Sci. Rep. 2022, 12, 3240. [Google Scholar] [CrossRef] [PubMed]
- Ganelin-Cohen, E.; Tartakovsky, E.; Klepfish, E.; Golderman, S.; Rozenberg, A.; Kaplan, B. Personalized Disease Monitoring in Pediatric Onset Multiple Sclerosis Using the Saliva Free Light Chain Test. Front. Immunol. 2022, 13, 821499. [Google Scholar] [CrossRef] [PubMed]
- Gomez Hernandez, M.P.; Starman, E.E.; Davis, A.B.; Withanage, M.H.H.; Zeng, E.; Lieberman, S.M.; Brogden, K.A.; Lanzel, E.A. A distinguishing profile of chemokines, cytokines and biomarkers in the saliva of children with Sjogren’s syndrome. Rheumatology 2021, 60, 4765–4777. [Google Scholar] [CrossRef]
- Al-Khatieeb, M.M.; Rafeeq, R.A.; Saleem, A.I. Relationship between Orthodontic Force Applied by Monoblock and Salivary Levels of Alkaline Phosphatase and Lactate Dehydrogenase Enzymes. J. Contemp. Dent. Pract. 2018, 19, 1346–1351. [Google Scholar] [CrossRef]
- Alhazmi, N.; Trotman, C.A.; Finkelman, M.; Hawley, D.; Zoukhri, D.; Papathanasiou, E. Salivary alkaline phosphatase activity and chronological age as indicators for skeletal maturity. Angle Orthod. 2019, 89, 637–642. [Google Scholar] [CrossRef]
- Hegde, S.S.; Revankar, A.V.; Patil, A.K. Identification of bone-specific alkaline phosphatase in saliva and its correlation with skeletal age. Indian J. Dent. Res. Off. Publ. Indian Soc. Dent. Res. 2018, 29, 721–725. [Google Scholar] [CrossRef]
- Deshpande, R.R.; Dungarwal, P.P.; Bagde, K.K.; Thakur, P.S.; Gajjar, P.M.; Kamath, A.P. Comparative evaluation of salivary zinc concentration in autistic and healthy children in mixed dentition age group-pilot study. Indian J. Dent. Res. Off. Publ. Indian Soc. Dent. Res. 2019, 30, 43–46. [Google Scholar] [CrossRef]
- Symons, F.J.; ElGhazi, I.; Reilly, B.G.; Barney, C.C.; Hanson, L.; Panoskaltsis-Mortari, A.; Armitage, I.M.; Wilcox, G.L. Can biomarkers differentiate pain and no pain subgroups of nonverbal children with cerebral palsy? A preliminary investigation based on noninvasive saliva sampling. Pain Med. 2015, 16, 249–256. [Google Scholar] [CrossRef]
- Almalki, A. Association of Salivary IGF and IGF/IGFBP-3 Molar Ratio with Cervical Vertebral Maturation Stages from Pre-Adolescent to Post-Adolescent Transition Period-A Cross-Sectional Exploratory Study. Int. J. Environ. Res. Public Health 2022, 19, 5172. [Google Scholar] [CrossRef]
- Almalki, A.; Thomas, J.T.; Khan, A.R.A.; Almulhim, B.; Alassaf, A.; Alghamdi, S.A.; Joseph, B.; Alqerban, A.; Alotaibi, S. Correlation between Salivary Levels of IGF-1, IGFBP-3, IGF-1/IGFBP3 Ratio with Skeletal Maturity Using Hand-Wrist Radiographs. Int. J. Environ. Res. Public Health 2022, 19, 3723. [Google Scholar] [CrossRef]
- Hori, H.; Izawa, S.; Yoshida, F.; Kunugi, H.; Kim, Y.; Mizukami, S.; Inoue, Y.; Tagaya, H.; Hakamata, Y. Association of childhood maltreatment history with salivary interleukin-6 diurnal patterns and C-reactive protein in healthy adults. Brain Behav. Immun. 2022, 101, 377–382. [Google Scholar] [CrossRef]
- Marques-Feixa, L.; Castro-Quintas, A.; Palma-Gudiel, H.; Romero, S.; Morer, A.; Rapado-Castro, M.; Martin, M.; Zorrilla, I.; Blasco-Fontecilla, H.; Ramirez, M.; et al. Secretory immunoglobulin A (s-IgA) reactivity to acute psychosocial stress in children and adolescents: The influence of pubertal development and history of maltreatment. Brain Behav. Immun. 2022, 103, 122–129. [Google Scholar] [CrossRef]
- Schmeer, K.K.; Ford, J.L.; Browning, C.R. Early childhood family instability and immune system dysregulation in adolescence. Psychoneuroendocrinology 2019, 102, 189–195. [Google Scholar] [CrossRef]
- Ngounou Wetie, A.G.; Wormwood, K.L.; Russell, S.; Ryan, J.P.; Darie, C.C.; Woods, A.G. A Pilot Proteomic Analysis of Salivary Biomarkers in Autism Spectrum Disorder. Autism Res. 2015, 8, 338–350. [Google Scholar] [CrossRef]
- Ngounou Wetie, A.G.; Wormwood, K.L.; Charette, L.; Ryan, J.P.; Woods, A.G.; Darie, C.C. Comparative two-dimensional polyacrylamide gel electrophoresis of the salivary proteome of children with autism spectrum disorder. J. Cell. Mol. Med. 2015, 19, 2664–2678. [Google Scholar] [CrossRef]
- Mota, F.S.B.; Nascimento, K.S.; Oliveira, M.V.; Osterne, V.J.S.; Clemente, J.C.M.; Correia-Neto, C.; Lima-Neto, A.B.; van Tilburg, M.F.; Leal-Cardoso, J.H.; Guedes, M.I.F.; et al. Potential protein markers in children with Autistic Spectrum Disorder (ASD) revealed by salivary proteomics. Int. J. Biol. Macromol. 2022, 199, 243–251. [Google Scholar] [CrossRef]
- Lavor, J.R.; Lacerda, R.H.W.; Modesto, A.; Vieira, A.R. Maxillary incisor enamel defects in individuals born with cleft lip/palate. PLoS ONE 2020, 15, e0244506. [Google Scholar] [CrossRef]
- Talaat, D.M.; Hachim, I.Y.; Afifi, M.M.; Talaat, I.M.; ElKateb, M.A. Assessment of risk factors and molecular biomarkers in children with supernumerary teeth: A single-center study. BMC Oral Health 2022, 22, 117. [Google Scholar] [CrossRef]
- Nelson, C.A.; Varcin, K.J.; Coman, N.K.; De Vivo, I.; Tager-Flusberg, H. Shortened Telomeres in Families with a Propensity to Autism. J. Am. Acad. Child Adolesc. Psychiatry 2015, 54, 588–594. [Google Scholar] [CrossRef]
- Sharma, R.; Frasch, M.G.; Zelgert, C.; Zimmermann, P.; Fabre, B.; Wilson, R.; Waldenberger, M.; MacDonald, J.W.; Bammler, T.K.; Lobmaier, S.M.; et al. Maternal-fetal stress and DNA methylation signatures in neonatal saliva: An epigenome-wide association study. Clin. Epigenet. 2022, 14, 87. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.-J.; Chan, W.-C.; Chou, M.-C.; Chou, W.-J.; Lee, M.-J.; Lee, S.-Y.; Lin, P.-Y.; Yang, Y.-H.; Yen, C.-F. Polymorphisms of STS gene and SULT2A1 gene and neurosteroid levels in Han Chinese boys with attention-deficit/hyperactivity disorder: An exploratory investigation. Sci. Rep. 2017, 7, 45595. [Google Scholar] [CrossRef] [PubMed]
- Kong, X.; Liu, J.; Cetinbas, M.; Sadreyev, R.; Koh, M.; Huang, H.; Adeseye, A.; He, P.; Zhu, J.; Russell, H.; et al. New and Preliminary Evidence on Altered Oral and Gut Microbiota in Individuals with Autism Spectrum Disorder (ASD): Implications for ASD Diagnosis and Subtyping Based on Microbial Biomarkers. Nutrients 2019, 11, 2128. [Google Scholar] [CrossRef] [PubMed]
- Sehovic, E.; Spahic, L.; Smajlovic-Skenderagic, L.; Pistoljevic, N.; Dzanko, E.; Hajdarpasic, A. Identification of developmental disorders including autism spectrum disorder using salivary miRNAs in children from Bosnia and Herzegovina. PLoS ONE 2020, 15, e0232351. [Google Scholar] [CrossRef]
- Hicks, S.D.; Johnson, J.; Carney, M.C.; Bramley, H.; Olympia, R.P.; Loeffert, A.C.; Thomas, N.J. Overlapping MicroRNA Expression in Saliva and Cerebrospinal Fluid Accurately Identifies Pediatric Traumatic Brain Injury. J. Neurotrauma 2018, 35, 64–72. [Google Scholar] [CrossRef]
- Angeli, E.; Korpa, T.; Johnson, E.O.; Apostolakou, F.; Papassotiriou, I.; Chrousos, G.P.; Pervanidou, P. Salivary cortisol and alpha-amylase diurnal profiles and stress reactivity in children with Attention Deficit Hyperactivity Disorder. Psychoneuroendocrinology 2018, 90, 174–181. [Google Scholar] [CrossRef]
- Yirmiya, K.; Djalovski, A.; Motsan, S.; Zagoory-Sharon, O.; Feldman, R. Stress and immune biomarkers interact with parenting behavior to shape anxiety symptoms in trauma-exposed youth. Psychoneuroendocrinology 2018, 98, 153–160. [Google Scholar] [CrossRef]
- Ferreira, A.C.F.M.; Eveloff, R.J.; Freire, M.; Santos, M.T.B.R. The Impact of Oral-Gut Inflammation in Cerebral Palsy. Front. Immunol. 2021, 12, 619262. [Google Scholar] [CrossRef]
- AlMaummar, M.; AlThabit, H.O.; Pani, S. The impact of dental treatment and age on salivary cortisol and alpha-amylase levels of patients with varying degrees of dental anxiety. BMC Oral Health 2019, 19, 211. [Google Scholar] [CrossRef]
- Llorens, M.; Barba, M.; Torralbas, J.; Nadal, R.; Armario, A.; Gagliano, H.; Betriu, M.; Urraca, L.; Pujol, S.; Montalvo, I.; et al. Stress-related biomarkers and cognitive functioning in adolescents with ADHD: Effect of childhood maltreatment. J. Psychiatr. Res. 2022, 149, 217–225. [Google Scholar] [CrossRef]
- Ntihabose, R.; Surette, C.; Foucher, D.; Clarisse, O.; Bouchard, M.F. Assessment of saliva, hair and toenails as biomarkers of low level exposure to manganese from drinking water in children. Neurotoxicology 2018, 64, 126–133. [Google Scholar] [CrossRef]
- Cullen, A.E.; Tappin, B.M.; Zunszain, P.A.; Dickson, H.; Roberts, R.E.; Nikkheslat, N.; Khondoker, M.; Pariante, C.M.; Fisher, H.L.; Laurens, K.R. The relationship between salivary C-reactive protein and cognitive function in children aged 11–14years: Does psychopathology have a moderating effect? Brain Behav. Immun. 2017, 66, 221–229. [Google Scholar] [CrossRef]
- Santos, M.T.B.R.; Diniz, M.B.; Guare, R.O.; Ferreira, M.C.D.; Gutierrez, G.M.; Gorjao, R. Inflammatory markers in saliva as indicators of gingival inflammation in cerebral palsy children with and without cervical motor control. Int. J. Paediatr. Dent. 2017, 27, 364–371. [Google Scholar] [CrossRef]
- Ghaziuddin, N.; Shamseddeen, W.; Bertram, H.; McInnis, M.; Wilcox, H.C.; Mitchell, P.B.; Fullerton, J.M.; Roberts, G.M.P.; Glowinski, A.L.; Kamali, M.; et al. Salivary melatonin onset in youth at familial risk for bipolar disorder. Psychiatry Res. 2019, 274, 49–57. [Google Scholar] [CrossRef]
- Mandrell, B.N.; Avent, Y.; Walker, B.; Loew, M.; Tynes, B.L.; Crabtree, V.M. In-home salivary melatonin collection: Methodology for children and adolescents. Dev. Psychobiol. 2018, 60, 118–122. [Google Scholar] [CrossRef]
- Cheng, Y.; Pereira, M.; Raukar, N.; Reagan, J.L.; Queseneberry, M.; Goldberg, L.; Borgovan, T.; LaFrance, W.C., Jr.; Dooner, M.; Deregibus, M.; et al. Potential biomarkers to detect traumatic brain injury by the profiling of salivary extracellular vesicles. J. Cell. Physiol. 2019, 234, 14377–14388. [Google Scholar] [CrossRef]
- Cicchetti, D.; Hetzel, S.; Rogosch, F.A.; Handley, E.D.; Toth, S.L. An investigation of child maltreatment and epigenetic mechanisms of mental and physical health risk. Dev. Psychopathol. 2016, 28, 1305–1317. [Google Scholar] [CrossRef]
- Johnson, J.J.; Loeffert, A.C.; Stokes, J.; Olympia, R.P.; Bramley, H.; Hicks, S.D. Association of Salivary MicroRNA Changes with Prolonged Concussion Symptoms. JAMA Pediatr. 2018, 172, 65–73. [Google Scholar] [CrossRef]
- Miller, K.E.; MacDonald, J.P.; Sullivan, L.; Venkata, L.P.R.; Shi, J.; Yeates, K.O.; Chen, S.; Alshaikh, E.; Taylor, H.G.; Hautmann, A.; et al. Salivary miRNA Expression in Children with Persistent Post-concussive Symptoms. Front. Public Health 2022, 10, 890420. [Google Scholar] [CrossRef]
- Ford, J.L.; Stowe, R.P. Depressive symptoms are associated with salivary shedding of Epstein-Barr virus in female adolescents: The role of sex differences. Psychoneuroendocrinology 2017, 86, 128–133. [Google Scholar] [CrossRef]
- Troisi, J.; Belmonte, F.; Bisogno, A.; Lausi, O.; Marciano, F.; Cavallo, P.; Guercio Nuzio, S.; Landolfi, A.; Pierri, L.; Vajro, P. Salivary markers of hepato-metabolic comorbidities in pediatric obesity. Dig. Liver Dis. 2019, 51, 516–523. [Google Scholar] [CrossRef] [PubMed]
- Alqaderi, H.; Hegazi, F.; Al-Mulla, F.; Chiu, C.-J.; Kantarci, A.; Al-Ozairi, E.; Abu-Farha, M.; Bin-Hasan, S.; Alsumait, A.; Abubaker, J.; et al. Salivary Biomarkers as Predictors of Obesity and Intermediate Hyperglycemia in Adolescents. Front. Public Health 2022, 10, 800373. [Google Scholar] [CrossRef] [PubMed]
- Shi, P.; Goodson, J.M.; Hartman, M.-L.; Hasturk, H.; Yaskell, T.; Vargas, J.; Cugini, M.; Barake, R.; Alsmadi, O.; Al-Mutawa, S.; et al. Continuous Metabolic Syndrome Scores for Children Using Salivary Biomarkers. PLoS ONE 2015, 10, e0138979. [Google Scholar] [CrossRef] [PubMed]
- Gofin, Y.; Fanous, E.; Pasternak, Y.; Prokocimer, Z.; Zagoory-Sharon, O.; Feldman, R.; Codick, G.; Waisbourd-Zinman, O.; Fried, S.; Livni, G. Salivary C-reactive protein-a possible predictor of serum levels in pediatric acute respiratory illness. Eur. J. Pediatr. 2021, 180, 2465–2472. [Google Scholar] [CrossRef]
- Zamora-Mendoza, B.N.; Espinosa-Tanguma, R.; Ramirez-Elias, M.G.; Cabrera-Alonso, R.; Montero-Moran, G.; Portales-Perez, D.; Rosales-Romo, J.A.; Gonzalez, J.F.; Gonzalez, C. Surface-enhanced raman spectroscopy: A non invasive alternative procedure for early detection in childhood asthma biomarkers in saliva. Photodiagn. Photodyn. Ther. 2019, 27, 85–91. [Google Scholar] [CrossRef]
- Okazaki, S.; Murai, H.; Kidoguchi, S.; Nomura, E.; Itoh, N.; Hashimoto, N.; Hamada, T.; Kawakita, A.; Yasutomi, M.; Ohshima, Y. The Biomarker Salivary SP-D May Indicate Small Airway Inflammation and Asthma Exacerbation. J. Investig. Allergol. Clin. Immunol. 2017, 27, 305–312. [Google Scholar] [CrossRef]
- Davidovich, E.; Mozer, Y.; Polak, D. Salivary inflammatory cytokines echo the low inflammatory burden in liver-transplanted children. Clin. Oral Investig. 2021, 25, 2993–2998. [Google Scholar] [CrossRef]
- Iwasawa, K.; Suda, W.; Tsunoda, T.; Oikawa-Kawamoto, M.; Umetsu, S.; Takayasu, L.; Inui, A.; Fujisawa, T.; Morita, H.; Sogo, T.; et al. Dysbiosis of the salivary microbiota in pediatric-onset primary sclerosing cholangitis and its potential as a biomarker. Sci. Rep. 2018, 8, 5480. [Google Scholar] [CrossRef]
- Kordy, K.; Li, F.; Lee, D.J.; Kinchen, J.M.; Jew, M.H.; La Rocque, M.E.; Zabih, S.; Saavedra, M.; Woodward, C.; Cunningham, N.J.; et al. Metabolomic Predictors of Non-alcoholic Steatohepatitis and Advanced Fibrosis in Children. Front. Microbiol. 2021, 12, 713234. [Google Scholar] [CrossRef]
- Alqaderi, H.; Tavares, M.; Al-Mulla, F.; Al-Ozairi, E.; Goodson, J.M. Late bedtime and dental caries incidence in Kuwaiti children: A longitudinal multilevel analysis. Community Dent. Oral Epidemiol. 2020, 48, 181–187. [Google Scholar] [CrossRef]
- Syed, M.; Sachdev, V.; Chopra, R. Intercomparison of salivary nitric oxide as a biomarker of dental caries risk between caries-active and caries-free children. Eur. Arch. Paediatr. Dent. 2016, 17, 239–243. [Google Scholar] [CrossRef]
- De-Sousa, E.T.; Lima-Holanda, A.T.; Nobre-Dos-Santos, M. Carbonic anhydrase VI activity in saliva and biofilm can predict early childhood caries: A preliminary study. Int. J. Paediatr. Dent. 2021, 31, 361–371. [Google Scholar] [CrossRef]
- Jurczak, A.; Koscielniak, D.; Papiez, M.; Vyhouskaya, P.; Krzysciak, W. A study on beta-defensin-2 and histatin-5 as a diagnostic marker of early childhood caries progression. Biol. Res. 2015, 48, 61. [Google Scholar] [CrossRef]
- Rinderknecht, C.; Filippi, C.; Ritz, N.; Fritschi, N.; Simmen, U.; Filippi, A.; Diesch-Furlanetto, T. Associations between salivary cytokines and oral health, age, and sex in healthy children. Sci. Rep. 2022, 12, 15991. [Google Scholar] [CrossRef]
- Sharma, V.; Gupta, N.; Srivastava, N.; Rana, V.; Chandna, P.; Yadav, S.; Sharma, A. Diagnostic potential of inflammatory biomarkers in early childhood caries—A case control study. Clin. Chim. Acta Int. J. Clin. Chem. 2017, 471, 158–163. [Google Scholar] [CrossRef]
- Hemadi, A.S.; Huang, R.; Zhou, Y.; Zou, J. Salivary proteins and microbiota as biomarkers for early childhood caries risk assessment. Int. J. Oral Sci. 2017, 9, e1. [Google Scholar] [CrossRef]
- Manzoor, M.; Lommi, S.; Furuholm, J.; Sarkkola, C.; Engberg, E.; Raju, S.; Viljakainen, H. High abundance of sugar metabolisers in saliva of children with caries. Sci. Rep. 2021, 11, 4424. [Google Scholar] [CrossRef]
- Goodson, J.M.; Shi, P.; Razzaque, M.S. Dietary phosphorus enhances inflammatory response: A study of human gingivitis. J. Steroid Biochem. Mol. Biol. 2019, 188, 166–171. [Google Scholar] [CrossRef]
- Sridharan, S.; Sravani, P.; Satyanarayan, A.; Kiran, K.; Shetty, V. Salivary Alkaline Phosphatase as a Noninvasive Marker for Periodontal Disease in Children with Uncontrolled Type 1 Diabetes Mellitus. J. Clin. Pediatr. Dent. 2017, 41, 70–74. [Google Scholar] [CrossRef]
- Hertel, S.; Hannig, M.; Hannig, C.; Sterzenbach, T. Mucins 5b and 7 and secretory IgA in the oral acquired pellicle of children with caries and caries-free children. Arch. Oral Biol. 2022, 134, 105314. [Google Scholar] [CrossRef]
- Kim, B.-S.; Han, D.-H.; Lee, H.; Oh, B. Association of Salivary Microbiota with Dental Caries Incidence with Dentine Involvement after 4 Years. J. Microbiol. Biotechnol. 2018, 28, 454–464. [Google Scholar] [CrossRef] [PubMed]
- Taylor, J.J.; Jaedicke, K.M.; van de Merwe, R.C.; Bissett, S.M.; Landsdowne, N.; Whall, K.M.; Pickering, K.; Thornton, V.; Lawson, V.; Yatsuda, H.; et al. A Prototype Antibody-based Biosensor for Measurement of Salivary MMP-8 in Periodontitis using Surface Acoustic Wave Technology. Sci. Rep. 2019, 9, 11034. [Google Scholar] [CrossRef] [PubMed]
- Goldoni, R.; Farronato, M.; Connelly, S.T.; Tartaglia, G.M.; Yeo, W.-H. Recent advances in graphene-based nanobiosensors for salivary biomarker detection. Biosens. Bioelectron. 2021, 171, 112723. [Google Scholar] [CrossRef] [PubMed]
- Van Staden, R.I.S.; Gugoasa, L.A.; Calenic, B.; Legler, J. Pattern recognition of estradiol, testosterone and dihydrotestosterone in children’s saliva samples using stochastic microsensors. Sci. Rep. 2014, 4, 5. [Google Scholar] [CrossRef]
- Lukose, J.; Barik, A.K.; Pai, K.M.; Unnikrishnan, V.K.; George, S.D.; Kartha, V.B.; Chidangil, S. Photonics of human saliva: Potential optical methods for the screening of abnormal health conditions and infections. Biophys. Rev. 2021, 13, 359–385. [Google Scholar] [CrossRef]

| Disease | Observed Biomarker | Methodology | Ref. | |
|---|---|---|---|---|
| 1. | Type I Diabetes Mellitus | Oxidative Stress Index (OSI), assessed by examining:
| Commercially available assay kits (Rel Assay, Mega Tıp, Gaziantep, Turkey) | [1] |
| 2. | Juvenile Idiopathic Arthritis | TNF-alpha, TNFRSF1B, MMP-1, MMP-2, MMP-3, MMP-13, IL-1alpha, IL-1beta, IL-1 RII, IL-2, IL-6, IL-6Ralpha, IL-8, IL-10, IL-12, CCL2, CCL3, CCL11, CCL22, CXCL9, S100A8 | Customized R&D-bead based immunoassay (R&D SYSTEMS/Bio-Techne; Minneapolis, MN, USA) | [2] |
| 3. | Pediatric-Onset Multiple Sclerosis | FLC as Monomers & Dimers (kapapaM, lambdaM, kappaD, lambdaD) | Gel Analysis & Blotting using rabbit antibodies to human Ig kappa and lambda light chains | [3] |
| 4. | Sjogren’s Syndrome | IL27, MIA, CCL4, TNFRSF18 and TNF-alpha (Among others) | Multiplex fluorescent microparticle-based immunoassays | [4] |
| Disease | Observed Biomarker | Methodology | Ref. | |
|---|---|---|---|---|
| 1. | Autism Spectrum Disorder | Salivary zinc | Plasma emission spectroscopy | [8] |
| 16s rRNA | 16s RNA gene amplicon sequencing | [23,24] | ||
| Calmodulin-3 Plastin-2 S100-a7 | Bio-Rad protein assay | [17] | ||
| 2. | Skeletal Maturity | LDH | Spectrophotometry | [5] |
| ALP | ALP and protein assay | [6] | ||
| Salivary B-ALP | ELISA | [7] | ||
| IGF-1 IGFBP-3 | Spectrophotometry | [10,11] | ||
| 3. | Attention Deficit Hyperactivity Disorder | DHEA CpG methylation | TaqMan assay | [22] |
| Condition | Observed Biomarker | Methodology | Ref. | |
|---|---|---|---|---|
| 1. | Stress | s-IgA | s-IgA ELISA kit (EUROIMMUN AG; Luebeck, Germany) | [27] |
| Cortisol | Commercial ELISA kit (Salimetrics, USA) | [27] | ||
| Alpha-amylase | Commercially available chemoimmunoluminiscence assay kits (Cobas integra400 plus, Roche Diagnostics, Risch-Rotkreuz, Switzerland) and analyzer (Cobas e411, Roche Diagnostics, Risch-Rotkreuz, Switzerland) | [29] | ||
| 2. | Cerebral Palsy | IL-1β IL-6 IL-8 IL-10 TNF-α | CBA Cytokine Inflammatory Kit (Becton Dickinson, CA, USA) | [28] |
| 3. | Systemic Inflammation | C-reactive proteins | Commercially available enzyme-linked immunoassay kit from Salimetrics, Suffolk, UK | [32] |
| Cytokine concentrations (IL-1β, IL-6, IL-8, and TNF-α) | MILLIPLEX MAP HCYTOMAG-60K-04 kit (Millipore, Billerica, MA, USA) | [31] | ||
| s-IgA | Colorimetric immunoenzymatic assay (ELISA) using an s-IgA saliva kit (DiaMetra, Milano, Italy) | [31] | ||
| 4. | Mild TBI | CDC2, CSNK1A1 and CTSD | NanoSight NS500 instrument (Nanosight, Malvern, UK), transmission electron microscopy, Western blot analysis, Taqman | [36] |
| miR-182-5p, miR-221-3p, mir-26b-5p, miR-320c, miR-29c-3p, miR-30e-5p | Oragene RE-100 saliva collection kit (DNA Genotek; Ottawa, Canada) | [25] | ||
| 5. | Child Maltreatment | ALDH2, ANKK1 and NR3C1 | Oragene DNA Self-Collection kits | [37] |
| 6. | Prolonged Concussion Syndrome | miR-320c-1, miR-133a-5p, miR-769-5p, let-7a-3p, and miR-1307-3p | Plasma/Serum Circulating and Exosomal RNA Purification Kits (Norgen Biotek) | [38,40] |
| hsa-miR-95-3p, hsa-miR-301a-5p, hsa-miR-626, hsa-miR-548y, hsa-miR-203a-5p, hsa-miR-548e-5p, hsa-miR-585-3p, hsa-miR-378h, hsa-miR-1323, hsa-miR-183-5p, hsa-miR-200a-3p, hsa-miR-888-5p, hsa-miR-199a-3p + hsa-miR-199b-3p | nCounter® human V3 miRNA assay kit (NanoString Technologies Inc., Seattle, WA, USA) | [39] | ||
| 7. | Depression | EBV | QiaAmp blood kit (Qiagen, Valencia, CA, USA) | [40] |
| Condition | Observed Biomarker | Methodology | Ref. | |
|---|---|---|---|---|
| 1. | Non-Alcoholic Fatty Liver Disease | Uric acid | Gas chromatography-mass spectrometry | [41] |
| Veillonella colonies Prevotella colonies | Bacterial 16S rRNA gene sequencing | [49] | ||
| 2. | Liver Graft versus Host Rejection | IL-6 IL-10 IL-1b | ELISA | [47] |
| 3. | Primary Sclerosing Cholangitis | Haemophilus colonies Oribacterium colonies | Bacterial 16S rRNA gene sequencing | [48] |
| 4. | Obesity | Insulin | Multiplex magnetic bead assays | [42] |
| CRP | [43] | |||
| Leptin | ||||
| Adiponectin | ||||
| 5. | Pediatric Pneumonia | CRP | ELISA | [44] |
| CP-D | ELISA | [46] | ||
| 6. | Asthma | IL-8 IL-10 sCD163 | Immunoassay and surface-enhanced Raman spectroscopy | [45] |
| Disease | Observed Biomarker | Methodology | Ref. | |
|---|---|---|---|---|
| 1. | Dental Caries | Leptin and Ghrelin | Multiplex Magnetic Bead Panels on a Luminex 200 Platform | [50] |
| NO (measured as total nitrates and nitrites) | Griess reaction method | [51] | ||
| Carbonic Anhydrase-VI | Zymography method | [52] | ||
| Beta-defensin-2 Histatin-5 | ELISA | [53] | ||
| IL6 IL8 TNF-alpha | ELISA | [54,55] | ||
| Streptococcus mutans spp. C. albicans Paludibacter Neisseria (Among others) | 16S rRNA | [56,57] | ||
| 2. | Periodontal Disease | Phosphate | Multiplex Magnetic Bead Panels | [58] |
| Alkaline Phosphatase (In T1DM patients only) | DEA-AMP Method | [59] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Min, H.; Zhu, S.; Safi, L.; Alkourdi, M.; Nguyen, B.H.; Upadhyay, A.; Tran, S.D. Salivary Diagnostics in Pediatrics and the Status of Saliva-Based Biosensors. Biosensors 2023, 13, 206. https://doi.org/10.3390/bios13020206
Min H, Zhu S, Safi L, Alkourdi M, Nguyen BH, Upadhyay A, Tran SD. Salivary Diagnostics in Pediatrics and the Status of Saliva-Based Biosensors. Biosensors. 2023; 13(2):206. https://doi.org/10.3390/bios13020206
Chicago/Turabian StyleMin, Hayeon, Sophie Zhu, Lydia Safi, Munzer Alkourdi, Bich Hong Nguyen, Akshaya Upadhyay, and Simon D. Tran. 2023. "Salivary Diagnostics in Pediatrics and the Status of Saliva-Based Biosensors" Biosensors 13, no. 2: 206. https://doi.org/10.3390/bios13020206
APA StyleMin, H., Zhu, S., Safi, L., Alkourdi, M., Nguyen, B. H., Upadhyay, A., & Tran, S. D. (2023). Salivary Diagnostics in Pediatrics and the Status of Saliva-Based Biosensors. Biosensors, 13(2), 206. https://doi.org/10.3390/bios13020206





