A Wearable and Real-Time Pulse Wave Monitoring System Based on a Flexible Compound Sensor
Abstract
:1. Introduction
2. Materials and Methods
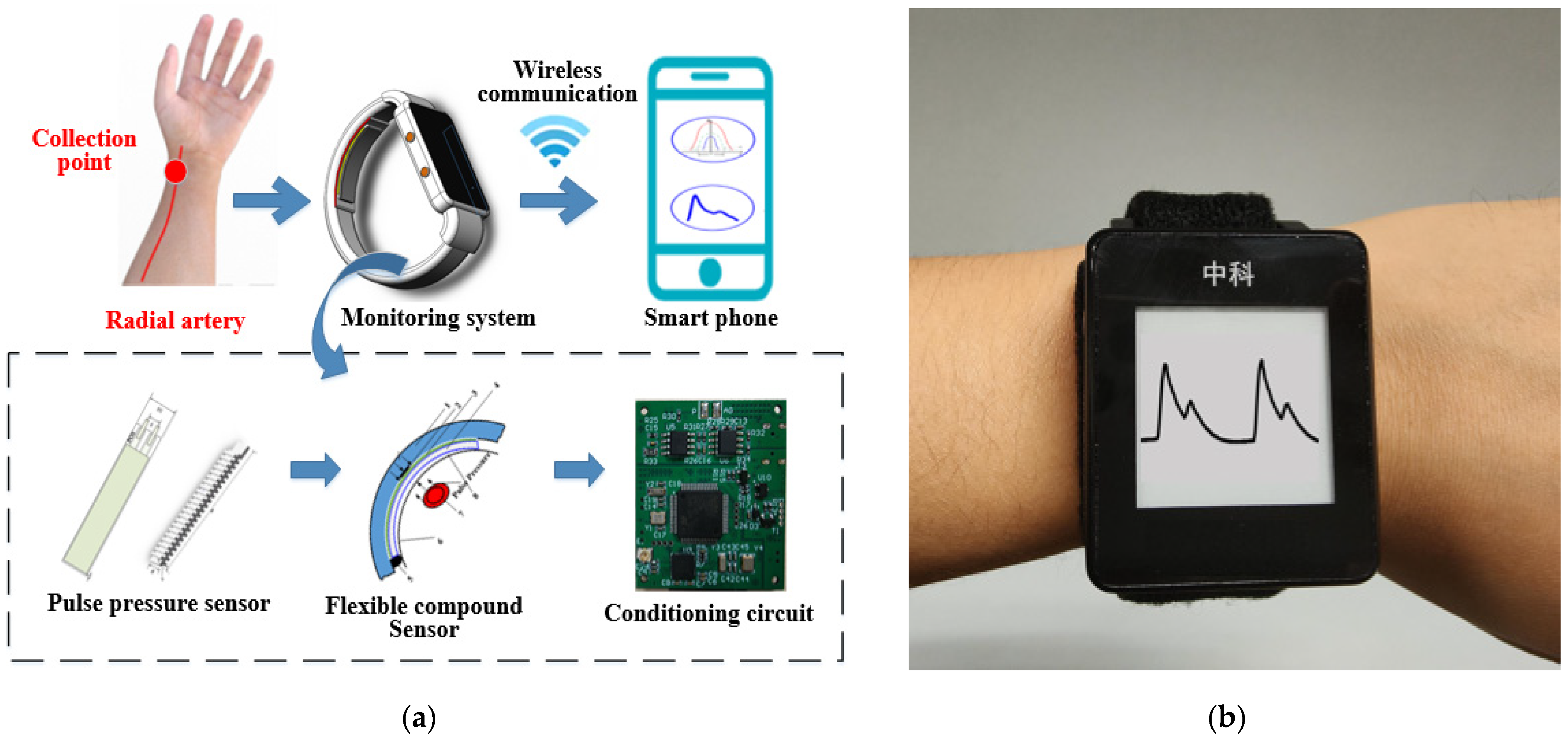
2.1. System Overview
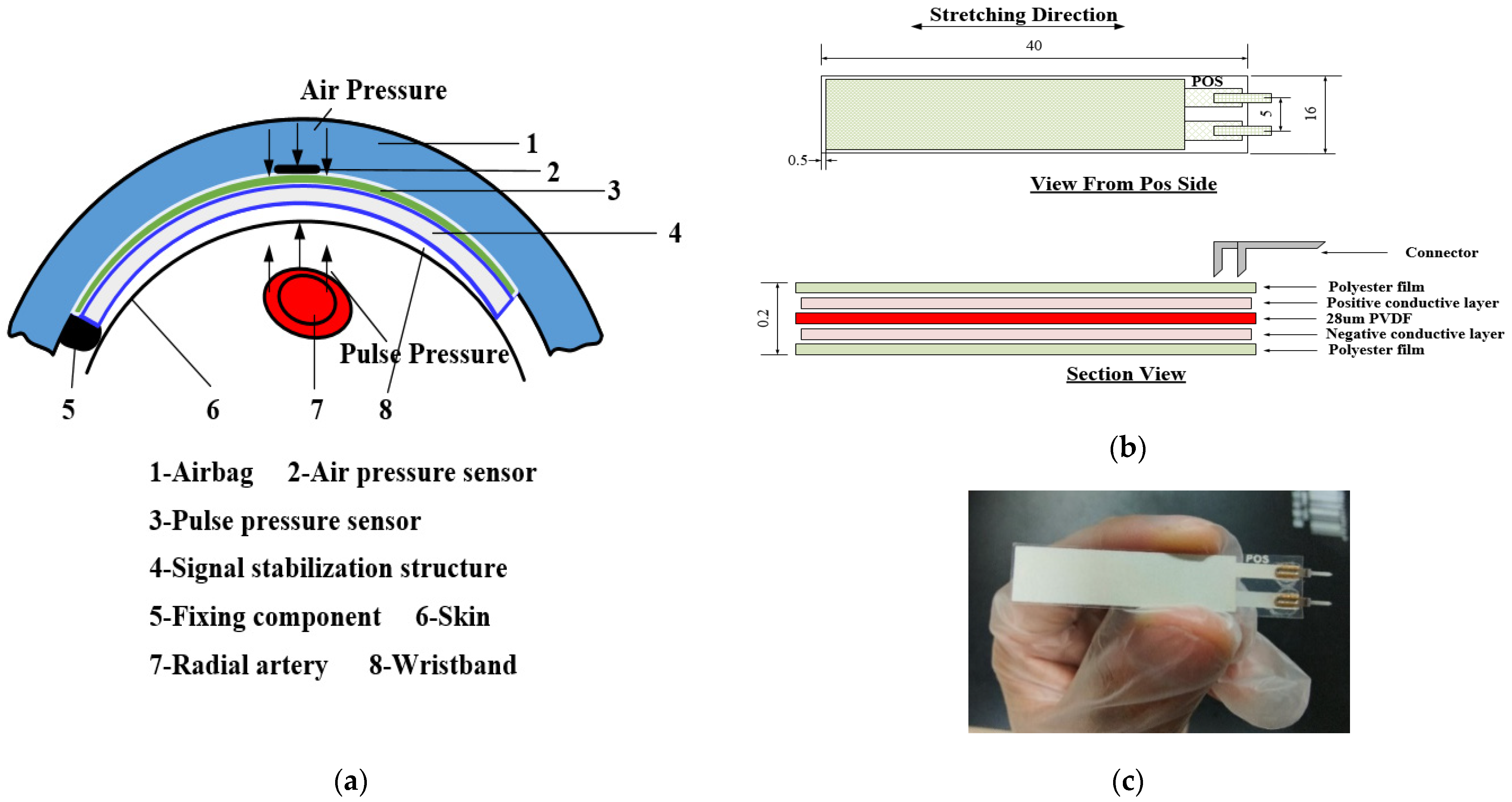
2.2. Flexible Compound Sensor
2.2.1. Pulse Pressure Sensor
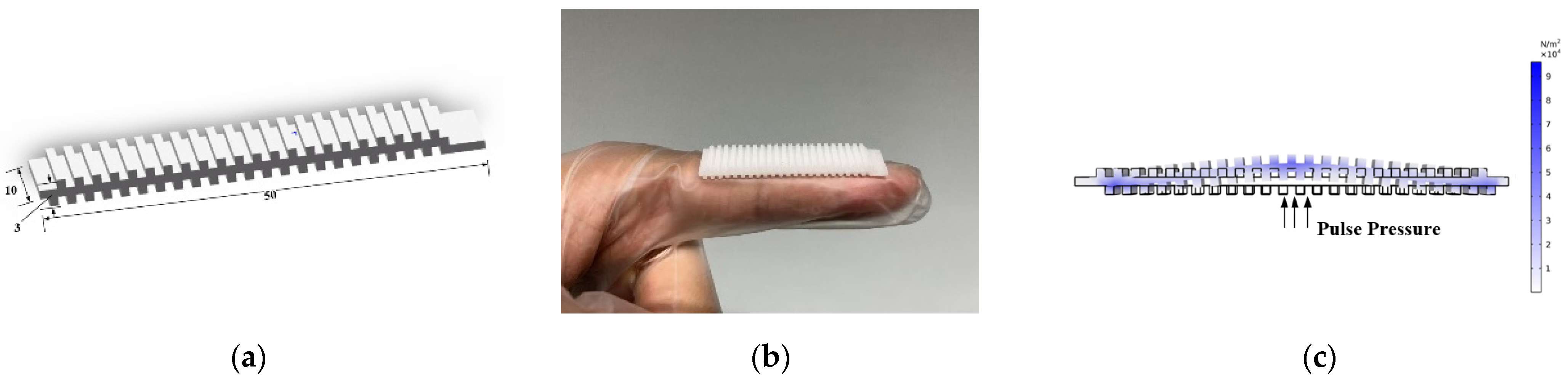
2.2.2. Pulse Signal Stabilization Structure
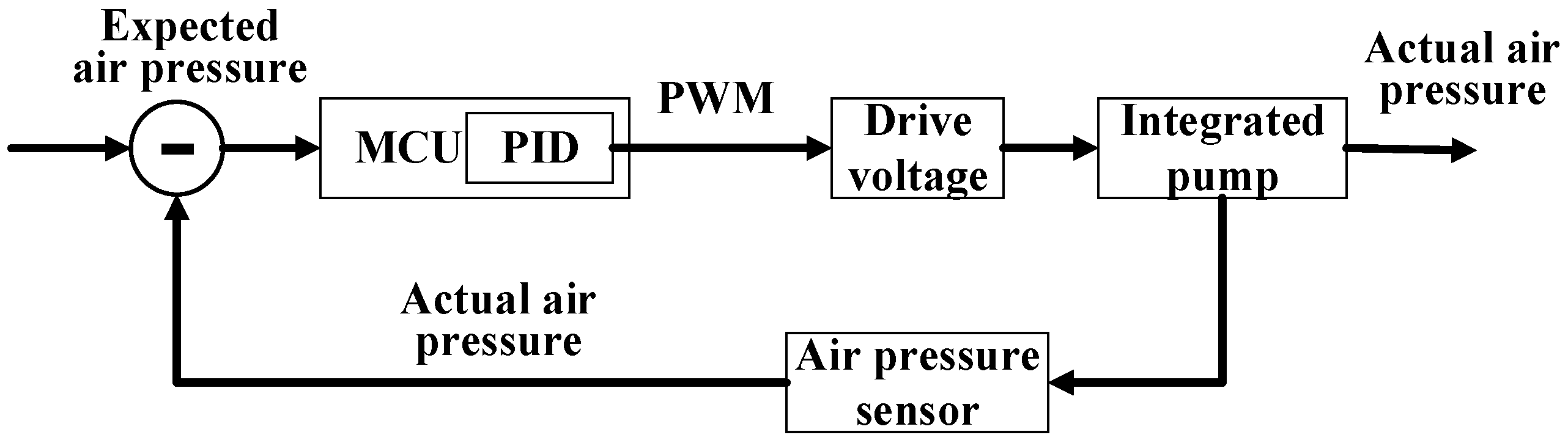
2.2.3. Micro Pressurization System
2.3. Signal Processing
2.3.1. Circuit Architecture
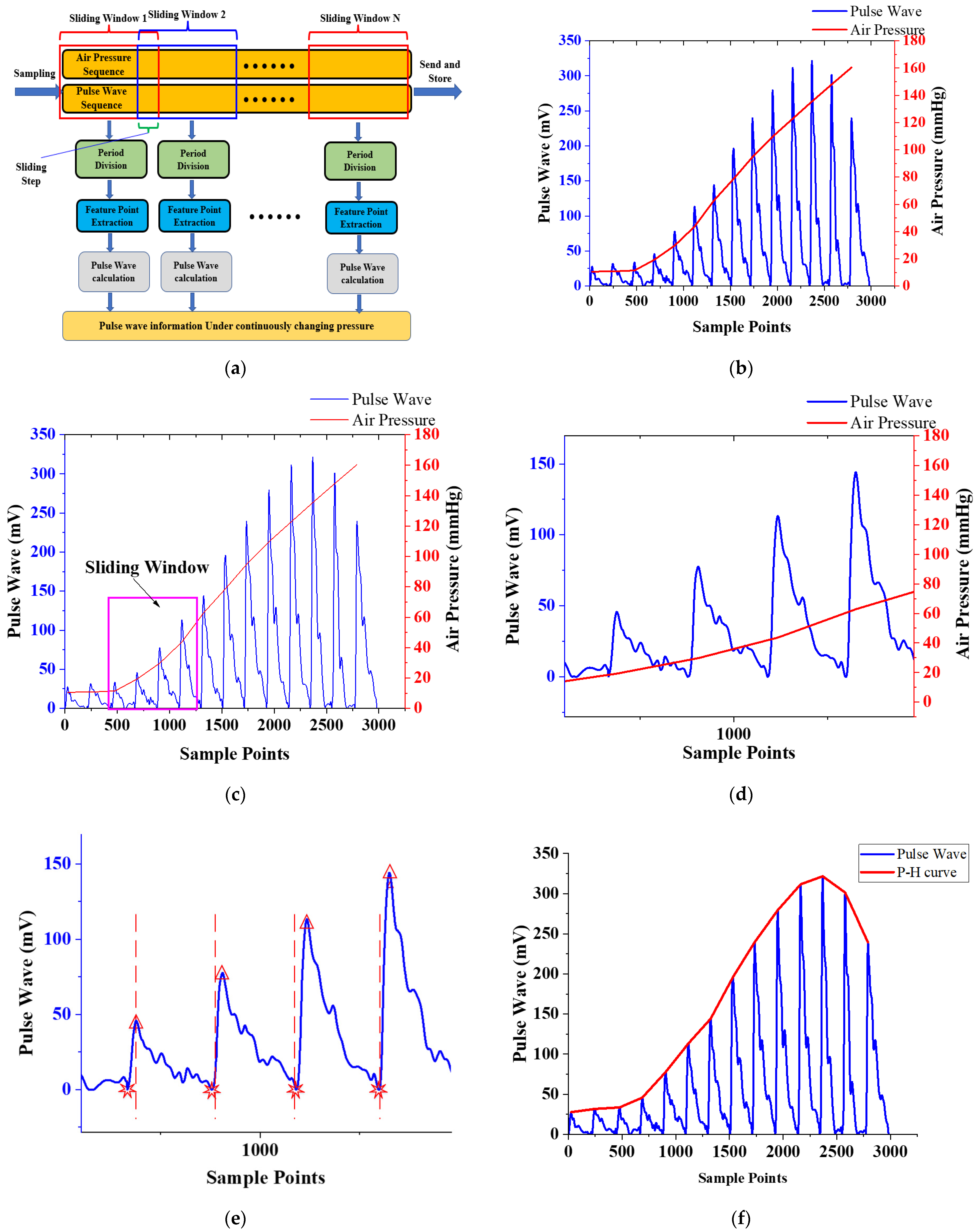
2.3.2. Real-Time Calculation Algorithm
3. Experimental Results and Discussion
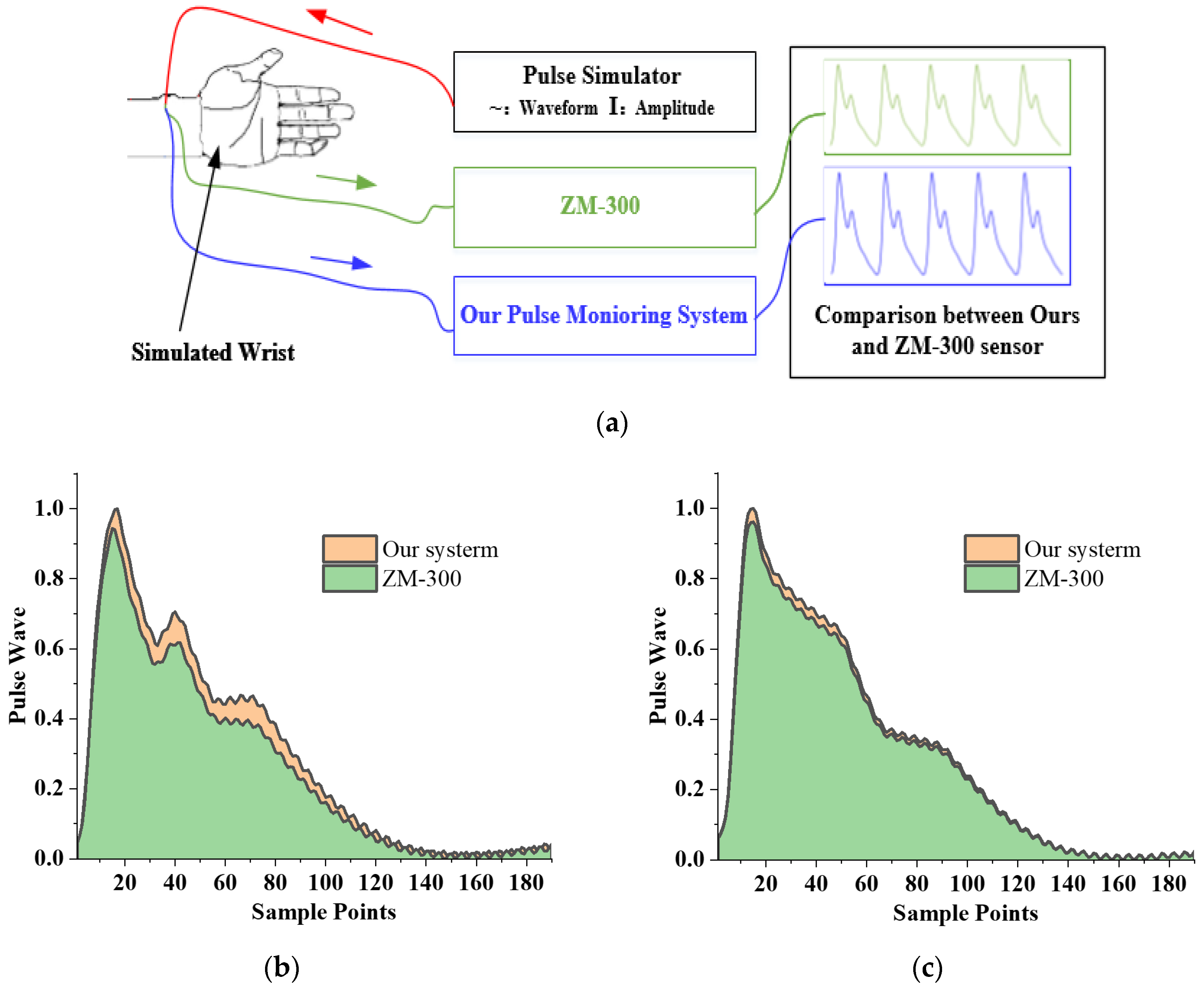
3.1. Test Device for Performance Test of the Flexible Compound Sensor
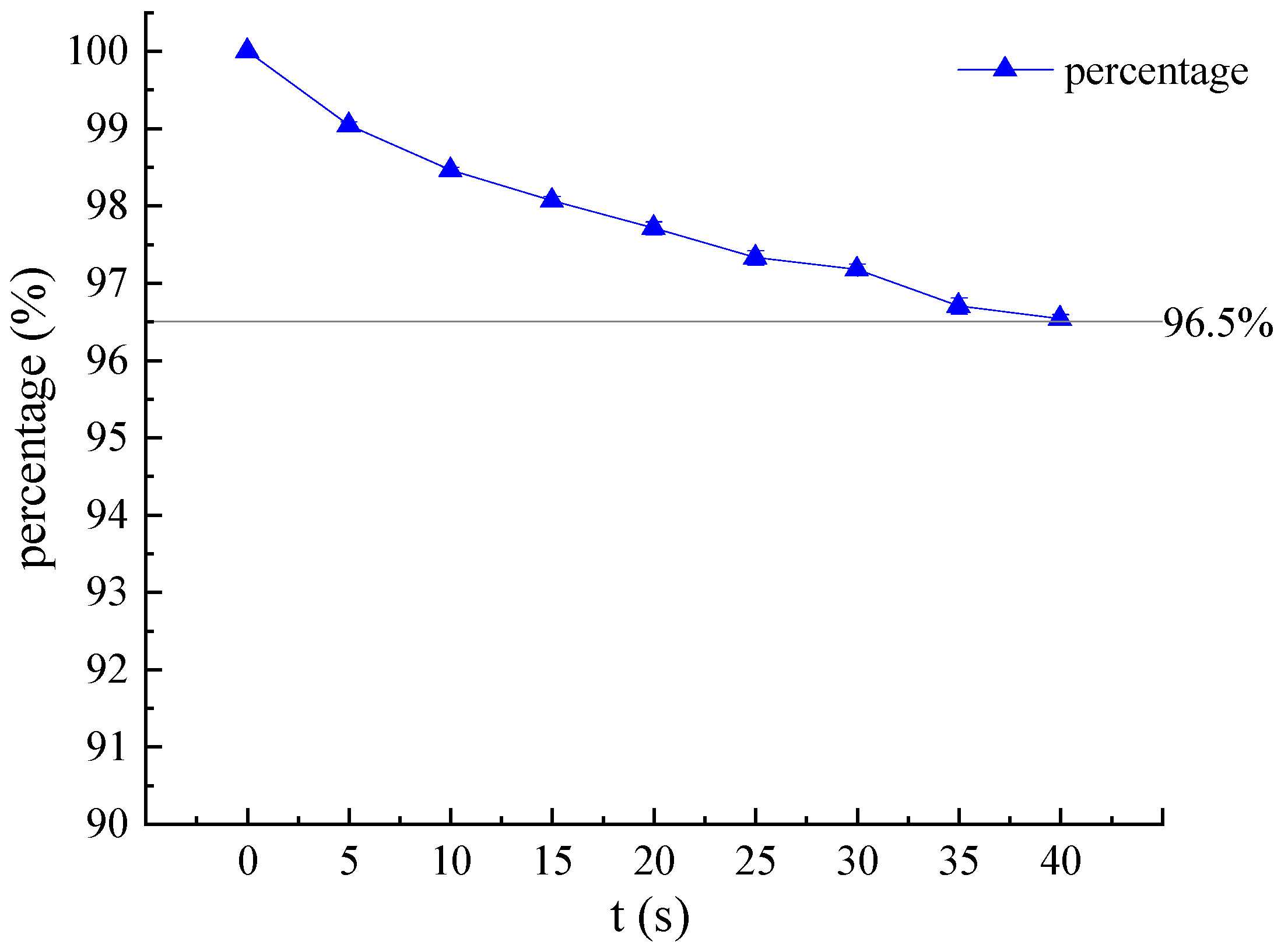
3.2. Verification of Airtightness
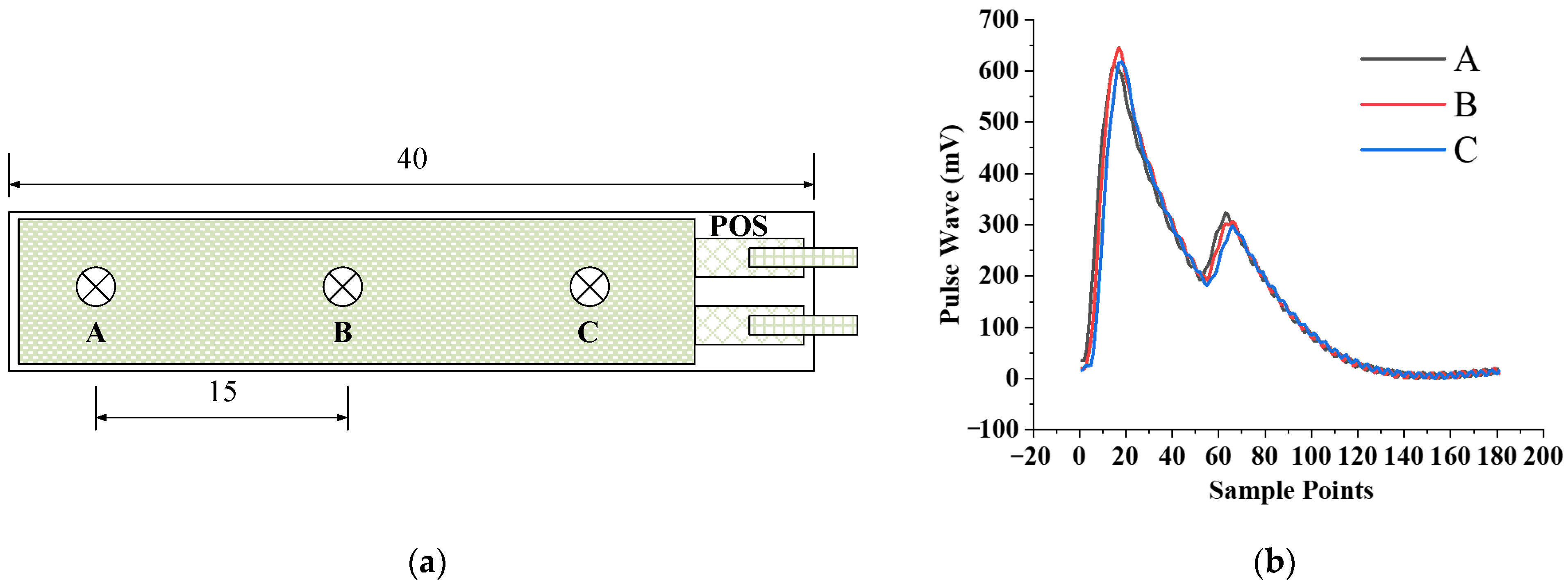
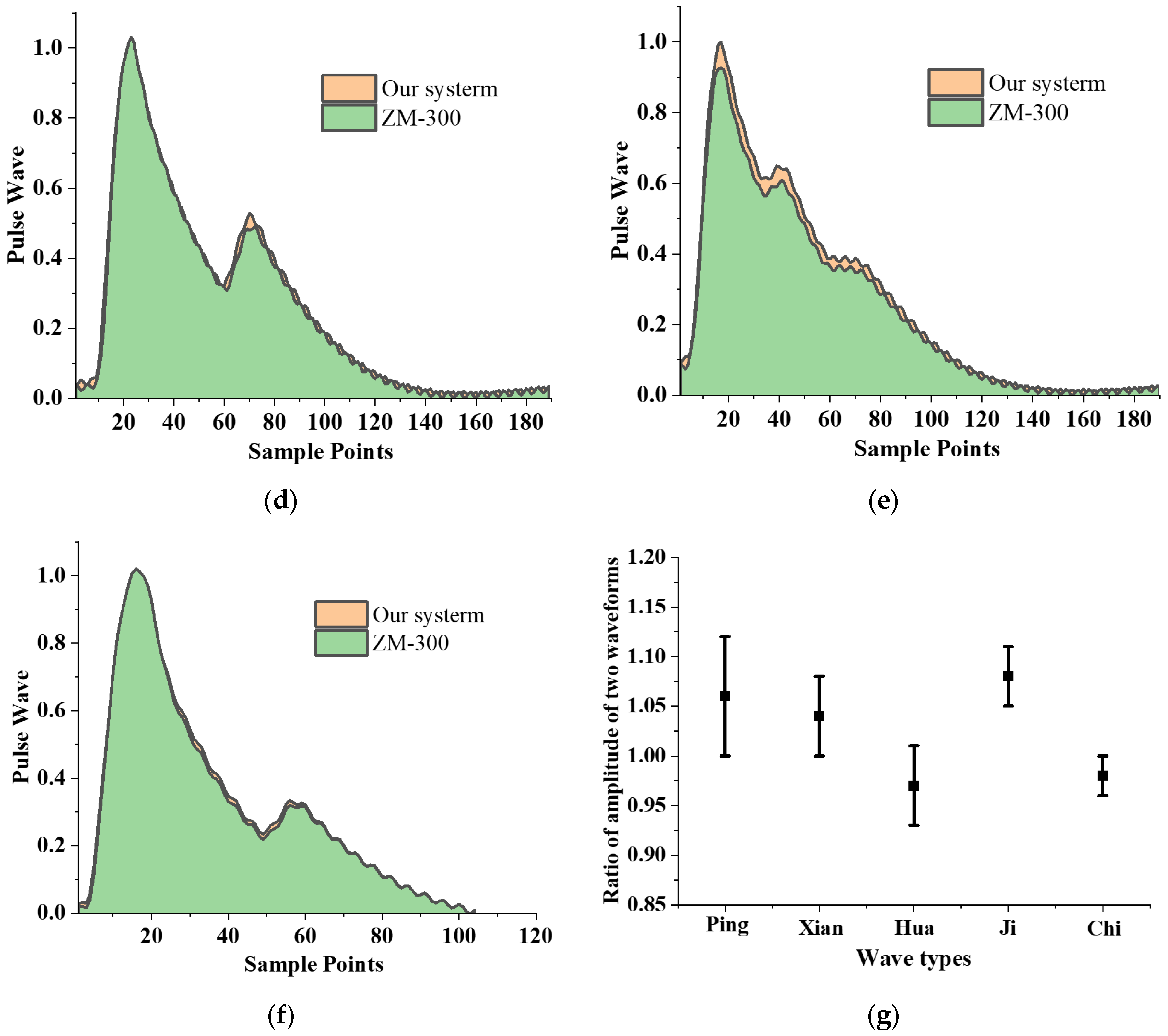
3.3. Consistency of Different Positioning of the Sensor
3.4. Repeatability of Flexible Compound Sensor
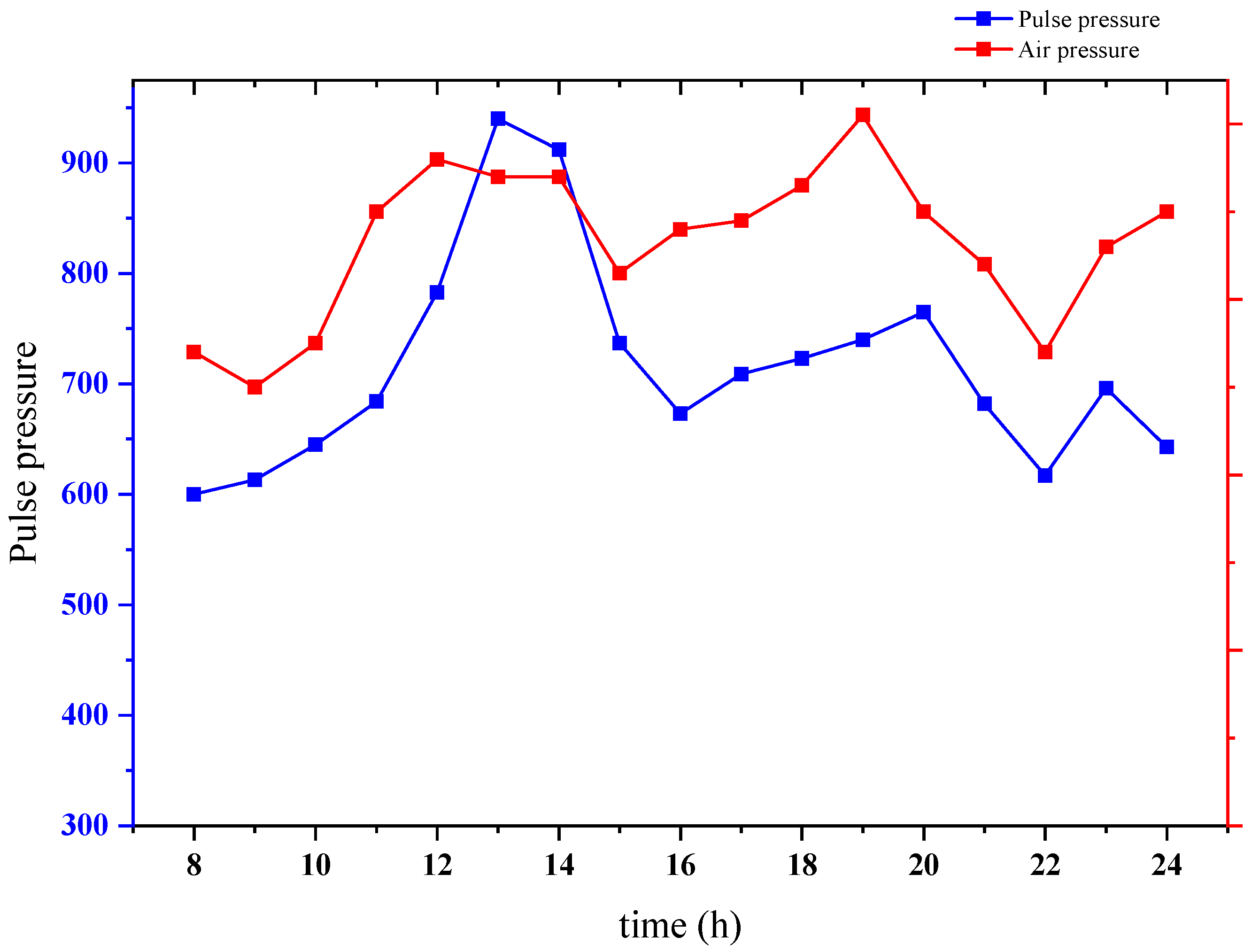
3.5. Verification of Pulse Pressure and Air Pressure Collection
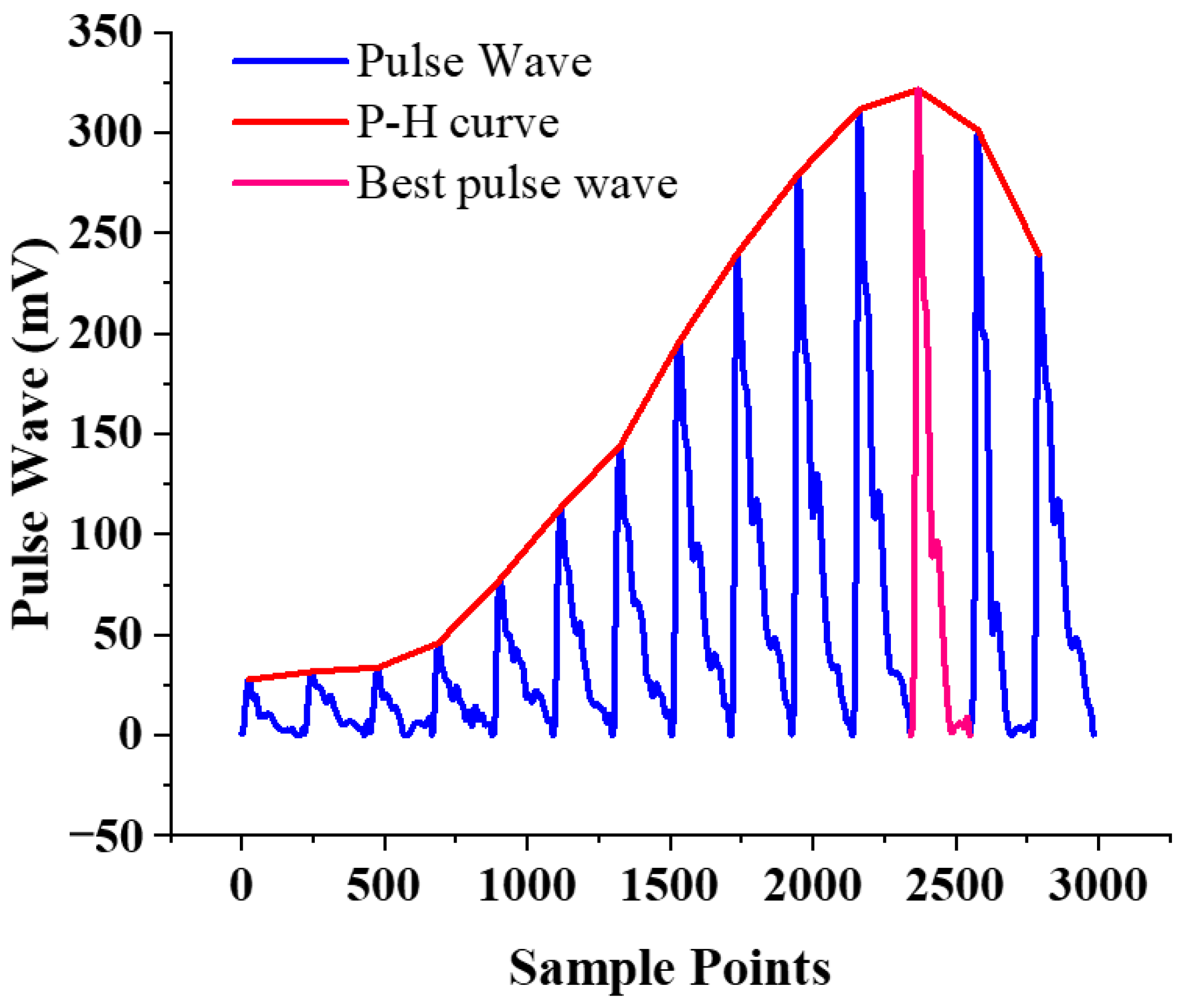
3.6. Verification of Best Pulse Wave Positioning
3.7. Pulse Wave Continuous Monitoring
4. Conclusions
5. Patents
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Chen, C.; Li, Z.; Zhang, Y.; Zhang, S.; Hou, J.; Zhang, H. A 3D Wrist Pulse Signal Acquisition System for Width Information of Pulse Wave. Sensors 2020, 20, 11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, S.; Zhang, S.; Zhang, Y.; Geng, X.; Zhang, J.; Zhang, H. A novel flexible pressure sensor array for depth information of radial artery. Sens. Actuators A Phys. 2018, 272, 92–101. [Google Scholar] [CrossRef]
- Zhang, Z.; Zhang, Y.; Yao, L.; Song, H.; Kos, A. A Sensor-Based Wrist Pulse Signal Processing and Lung Cancer Recognition. J. Biomed. Inform. 2018, 79, 107–116. [Google Scholar] [CrossRef] [PubMed]
- He, D.; Wang, L.; Fan, X.; Yao, Y.; Geng, N.; Sun, Y.; Xu, L.; Qian, W. A New Mathematical Model of Wrist Pulse Waveforms Characterizes Patients with Cardiovascular Disease—A Pilot Study. Med. Eng. Phys. 2017, 48, 142–149. [Google Scholar] [CrossRef] [PubMed]
- Moura, N.; Ferreira, A. Pulse Waveform Analysis of Chinese Pulse Images and Its Association with Disability in Hypertension. J. Acupunct. Meridian Stud. 2016, 9, 93–98. [Google Scholar] [CrossRef] [PubMed]
- Lee, Q.Y.; Chan, G.S.H.; Redmond, S.J.; Middleton, P.M.; Steel, E.; Malouf, P.; Critoph, C.; Flynn, G.; O’Lone, E.; Lovell, N.H. Classification of low systemic vascular resistance using photoplethysmogram and routine cardiovascular measurements. In Proceedings of the 2010 Annual International Conference of the IEEE Engineering in Medicine and Biology, Buenos Aires, Argentina, 31 August–4 September 2010; Volume 2010, pp. 1930–1933. [Google Scholar]
- Wang, D.; Zhang, D.; Lu, G. A Novel Multichannel Wrist Pulse System with Different Sensor Arrays. IEEE Trans. Instrum. Meas. 2015, 64, 2020–2034. [Google Scholar] [CrossRef]
- Malinauskas, K.; Palevicius, P.; Ragulskis, M.; Ostaševičius, V.; Dauksevicius, R. Validation of Noninvasive MOEMS-Assisted Measurement System Based on CCD Sensor for Radial Pulse Analysis. Sensors 2013, 13, 5368–5380. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Convertino, V.A.; Schauer, S.G.; Weitzel, E.K.; Cardin, S.; Stackle, M.E.; Talley, M.J.; Sawka, M.N.; Inan, O.T. Wearable Sensors Incorporating Compensatory Reserve Measurement for Advancing Physiological Monitoring in Critically Injured Trauma Patients. Sensors 2020, 20, 6413. [Google Scholar] [CrossRef] [PubMed]
- Chung, C.Y.; Cheng, Y.W.; Luo, C.H. Neural network study for standardizing pulse-taking depth by the width of artery. Comput. Biol. Med. 2015, 57, 26–31. [Google Scholar] [CrossRef]
- Convertino, V.A.; Sawka, M.N. Wearable compensatory reserve measurement for hypovolemia sensing. Appl. Physiol. 2018, 124, 442–451. [Google Scholar] [CrossRef] [PubMed]
- Yoo, S.K.; Shin, K.Y.; Lee, T.B.; Jin, S.O. New pulse wave measurement method using different hold-down wrist pressures according to individual patient characteristics. SpringerPlus 2013, 2, 1–8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, Y.-Y.; Chang, R.-S.; Jwo, K.-W.; Hsu, C.-C.; Tsao, C.-P. A Non-Contact Pulse Automatic Positioning Measurement System for Traditional Chinese Medicine. Sensors 2015, 15, 9899–9914. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chan, M.; Ganti, V.G.; Heller, J.A.; Abdallah, C.A.; Etemadi, M.; Inan, O.T. Enabling Continuous Wearable Reflectance Pulse Oximetry at the Sternum. Biosensors 2021, 11, 521. [Google Scholar] [CrossRef]
- Martín-Escudero, P.; Cabanas, A.M.; Fuentes-Ferrer, M.; Galindo-Canales, M. Oxygen Saturation Behavior by Pulse Oximetry in Female Athletes: Breaking Myths. Biosensors 2021, 11, 391. [Google Scholar] [CrossRef]
- Nam, D.-H.; Lee, W.-B.; Hong, Y.-S.; Lee, S.-S. Measurement of Spatial Pulse Wave Velocity by Using a Clip-Type Pulsimeter Equipped with a Hall Sensor and Photoplethysmography. Sensors 2013, 13, 4714–4723. [Google Scholar] [CrossRef]
- Warren, K.M.; Harvey, J.R.; Chon, K.H.; Mendelson, Y. Improving pulse rate measurements during random motion using a wearable multichannel reflectance photoplethysmograph. Sensors 2016, 16, 342. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, Y.; Lu, B.; Chen, Y.; Feng, X. Biocompatible and Ultra-Flexible Inorganic Strain Sensors Attached to Skin for Long-Term Vital Signs Monitoring. IEEE Electron Device Lett. 2016, 37, 496–499. [Google Scholar] [CrossRef]
- Wang, Z.; Wang, S.; Zeng, J.; Ren, X.; Chee, A.J.Y.; Yiu, B.Y.S.; Chung, W.C.; Yang, Y.; Yu, A.C.H.; Roberts, R.C.; et al. High Sensitivity, Wearable, Piezoresistive Pressure Sensors Based on Irregular Microhump Structures and its Applications in Body Motion Sensing. Small 2016, 12, 3827–3836. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.; Ren, T.-L.; Luo, J. Effects of parameters on the accuracy and precision of ultrasound-based local pulse wave velocity measurement: A simulation study. IEEE Trans. Ultrason. Ferroelectr. Freq. Control 2014, 61, 2001–2018. [Google Scholar] [CrossRef] [PubMed]
- Murphy, J.C.; Morrison, K.; Mclaughlin, J.; Manoharan, G.; Adgey, A.J. An innovative piezoelectric-based method for measuring pulse wave velocity in patients with hypertension. J. Clin. Hypertens. 2011, 13, 497–505. [Google Scholar] [CrossRef] [PubMed]
- Kan-heng, Z.; Peng, Q.; Chun-ming, X.; Yi-qin, W. Research on a Novel Three-Channel Self-Pressurized Wrist Pulse Acquisition System. In Biomedical Engineering Systems and Technologies; Springer: Berlin/Heidelberg, Germany, 2015; pp. 49–59. [Google Scholar]
- Fu, Y.; Zhao, S.; Zhu, R. A Wearable Multifunctional Pulse Monitor Using Thermosensation-Based Flexible Sensors. IEEE Trans. Biomed. Eng. 2018, 66, 1412–1421. [Google Scholar] [CrossRef] [PubMed]
- Jin, C.; Xia, C.; Zhang, S.; Wang, L.; Wang, Y.; Yan, H. A Wearable Combined Wrist Pulse Measurement System Using Airbags for Pressurization. Sensors 2019, 19, 386. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kabigting, J.E.T.; Chen, A.D.; Chang, E.J.; Lee, W.; Roberts, R.C. Mems pressure sensor array wearable for traditional Chinese medicine pulse-taking. In Proceedings of the IEEE 14th International Conference on Wearable and Implantable Body Sensor Networks (BSN), Eindhoven, The Netherlands, 9–12 May 2017. [Google Scholar]
- Hsieh, T.-C.; Wu, C.-M.; Tsai, C.-C.; Lo, W.-C.; Wang, Y.-M.; Smith, S. Portable Interactive Pulse Tactile Recorder and Player System. Sensors 2021, 21, 4339. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Zhang, J.; Hu, J.; Luo, N.; Sun, F.; Venkatesan, H.; Zhao, N.; Zhang, Y. Ultrafast-Response/Recovery Flexible Piezoresistive Sensors with DNA-Like Double Helix Yarns for Epidermal Pulse Monitoring. Adv. Mater. 2022, 34, 2104313. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Sun, K.; Zheng, R.; Sun, Y.; Yang, H.; Zhong, Y.; Li, X. Three-Dimensional Arterial Pulse Signal Acquisition in Time Domain Using Flexible Pressure-Sensor Dense Arrays. Micromachines 2021, 12, 569. [Google Scholar] [CrossRef] [PubMed]




| Variables | Parameters |
|---|---|
| Density | 1.78 × 103 kg/m3 |
| Active area | 40 mm × 10 mm |
| Thickness | 28 μm |
| Capacitance | 1.6 nF |
| Young’s Modulus | 2 × 109 N/m2 |
| Mylar | 5 mil |
| Sensitivity | 14.4 V/N |
| Time (s) | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| RSD of Pulse Pressure | 8.7% | 9.0% | 10.7% | 16.7% | 5.4% | 5.9% | 6.4% | 3.4% | 4.5% | 5.0% | 5.0% | 3.6% | 3.5% | 3.4% | 4.0% | 4.2% | 5.3% | 5.9% |
| RSD of Air Pressure | 33.2% | 13.2% | 7.8% | 5.6% | 4.5% | 4.1% | 3.8% | 3.5% | 3.5% | 2.4% | 2.1% | 1.9% | 1.7% | 1.5% | 1.1% | 0.8% | 0.7% | 0.8% |
| Pulse Type | Ping | Xian | Hua | Chi | Ji |
|---|---|---|---|---|---|
| Pearson correlation | 0.99 | 0.97 | 0.97 | 0.98 | 0.99 |
| Variables | Parameters | Experimental Result | ||
|---|---|---|---|---|
| YES | NO | Accuracy | ||
| Gender | 19 | 1 | 95% | |
| Male | 10 | |||
| Female | 10 | |||
| Age (year) | 29 ± 5.0 (22–46) | |||
| Height (cm) | 174.6 ± 7.4 (153–190) | |||
| Weight (Kg) | 72.5 ± 18.3 (41–115) | |||
| BMI | 22.04 ± 3.4 (16.1–38.9) | |||
| System | Jessica et al. [25] | Liu et al. [2] | J.C. et al. [24] | Chen C. et al. [1] | Hsieh et al. [26] | Chen J. et al. [27] | Li et al. [28] | Proposed |
|---|---|---|---|---|---|---|---|---|
| Wearable | YES | NO | YES | NO | YES | YES | YES | YES |
| Real-time | NO | NO | NO | NO | NO | NO | NO | YES |
| Weight | Not mentioned | 1164.4 g | ~800 g | Not mentioned | 10 g | Not mentioned | Not mentioned | 52.8 g |
| Portable | NO | NO | NO | NO | YES | YES | NO | YES |
| Flexible | NO | YES | NO | YES | NO | YES | YES | YES |
| Pulse-taking pressure acquiring | NO | YES | YES | YES | NO | NO | YES | YES |
| Measure under continuously changing pressure | NO | NO | YES | NO | NO | NO | NO | YES |
| Pressurization method | Manually | Pump and air bag | Pump and air bag | Pump and air bag | Manually | Manually | Manually | Integrated air pump (weight: 2.48 g) and air bag |
| Year of publication | 2017 | 2018 | 2019 | 2020 | 2021 | 2021 | 2021 | 2022 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kang, X.; Zhang, J.; Shao, Z.; Wang, G.; Geng, X.; Zhang, Y.; Zhang, H. A Wearable and Real-Time Pulse Wave Monitoring System Based on a Flexible Compound Sensor. Biosensors 2022, 12, 133. https://doi.org/10.3390/bios12020133
Kang X, Zhang J, Shao Z, Wang G, Geng X, Zhang Y, Zhang H. A Wearable and Real-Time Pulse Wave Monitoring System Based on a Flexible Compound Sensor. Biosensors. 2022; 12(2):133. https://doi.org/10.3390/bios12020133
Chicago/Turabian StyleKang, Xiaoxiao, Jun Zhang, Zheming Shao, Guotai Wang, Xingguang Geng, Yitao Zhang, and Haiying Zhang. 2022. "A Wearable and Real-Time Pulse Wave Monitoring System Based on a Flexible Compound Sensor" Biosensors 12, no. 2: 133. https://doi.org/10.3390/bios12020133
APA StyleKang, X., Zhang, J., Shao, Z., Wang, G., Geng, X., Zhang, Y., & Zhang, H. (2022). A Wearable and Real-Time Pulse Wave Monitoring System Based on a Flexible Compound Sensor. Biosensors, 12(2), 133. https://doi.org/10.3390/bios12020133





