Optical Fiber Distributed Sensing Network for Thermal Mapping in Radiofrequency Ablation Neighboring a Blood Vessel
Abstract
1. Introduction
2. Experimental Setup
2.1. Radiofrequency Ablation Setup
2.2. Distributed Sensing Network
2.3. Thermal Ablation Experiments
2.4. Thermal Maps Evaluation
3. Experimental Results
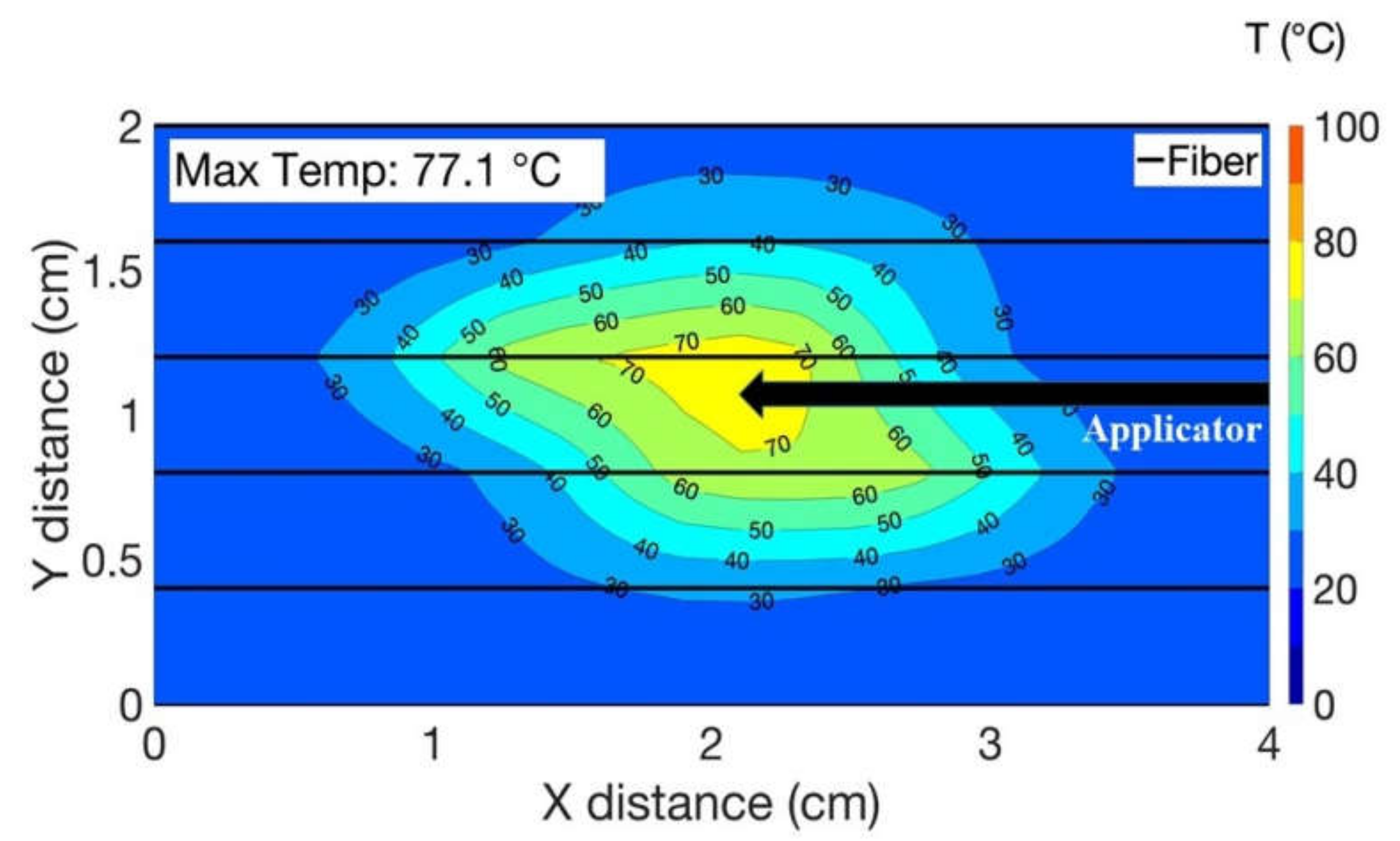
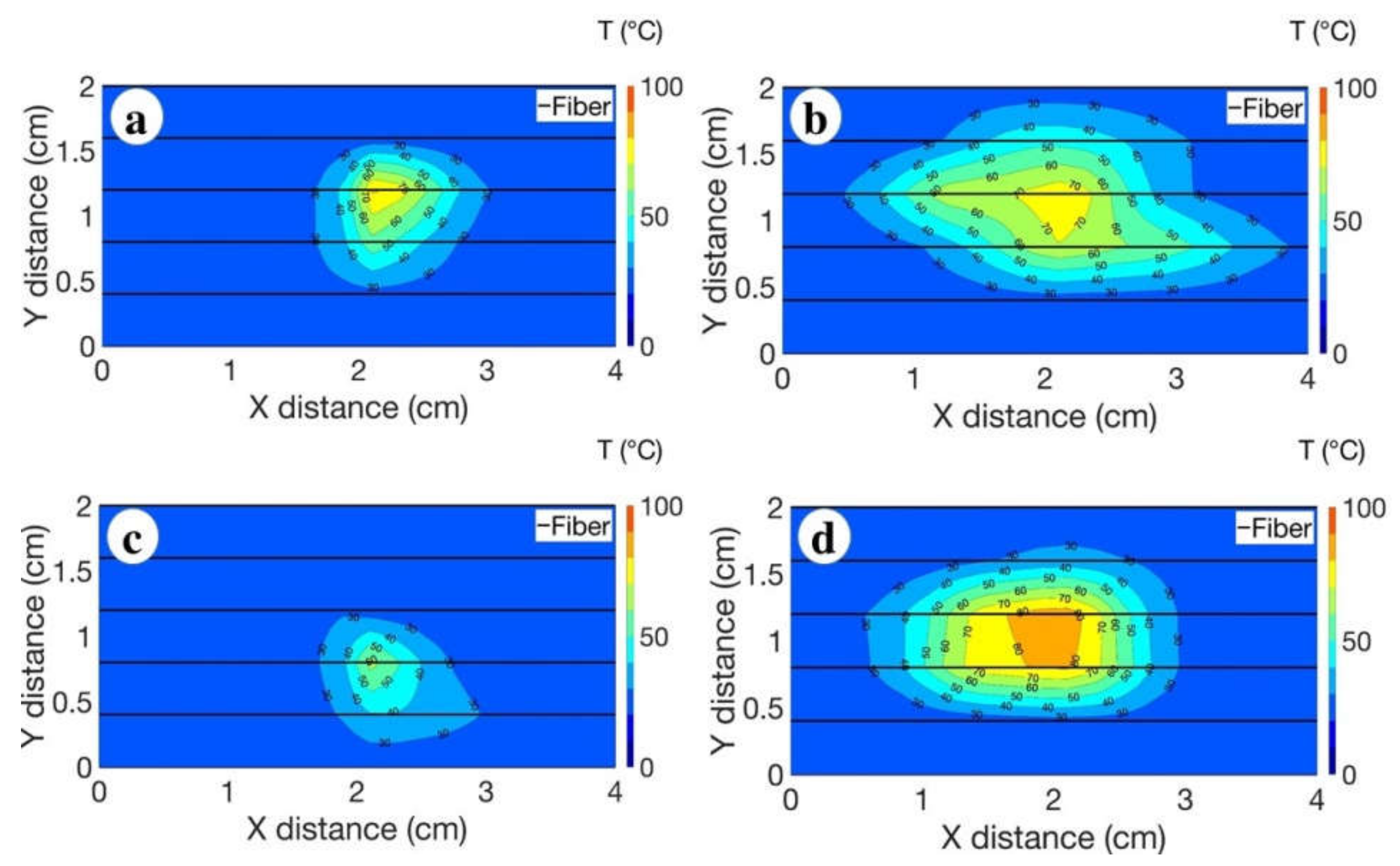
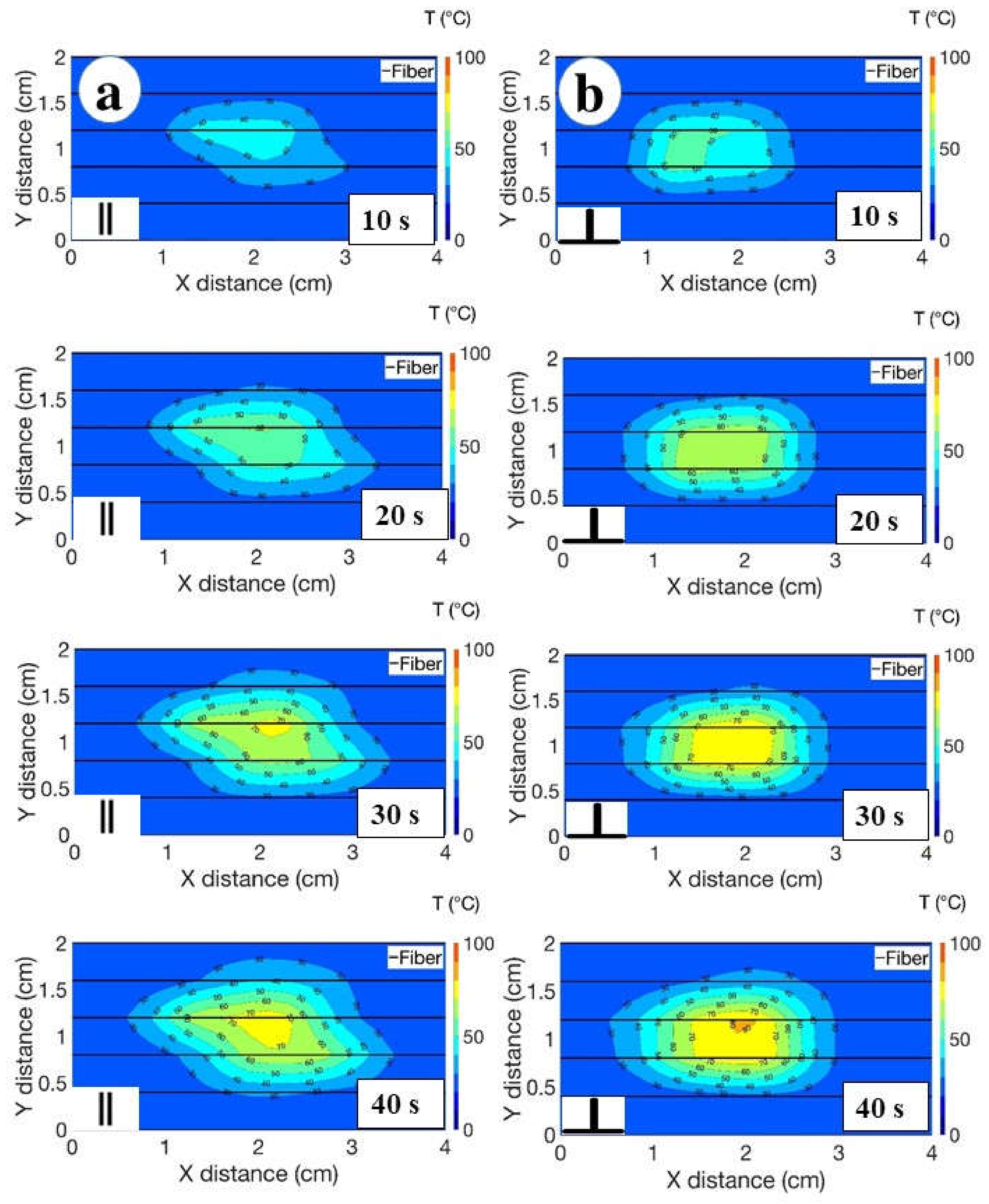
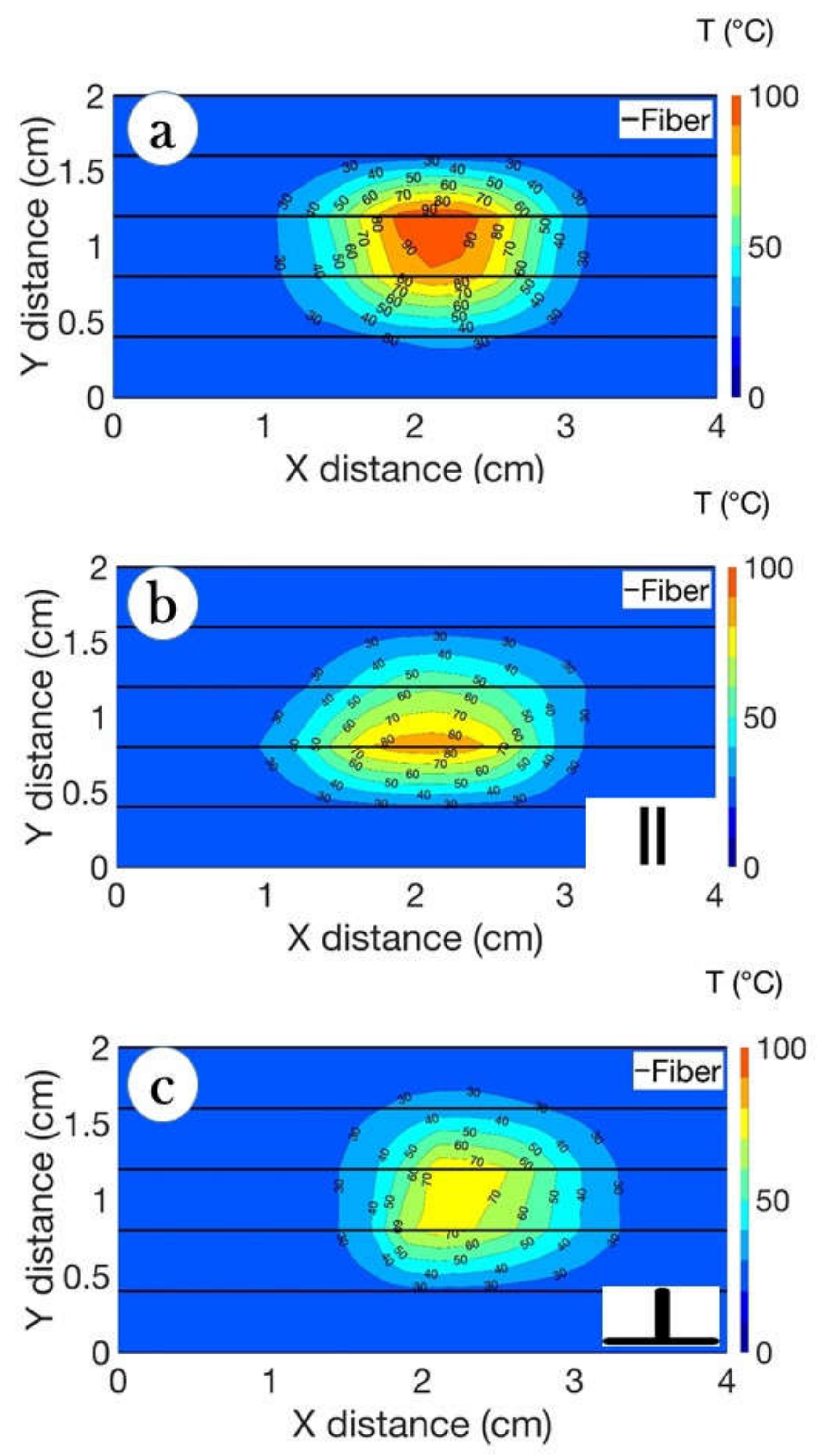
3.1. Thermal Maps
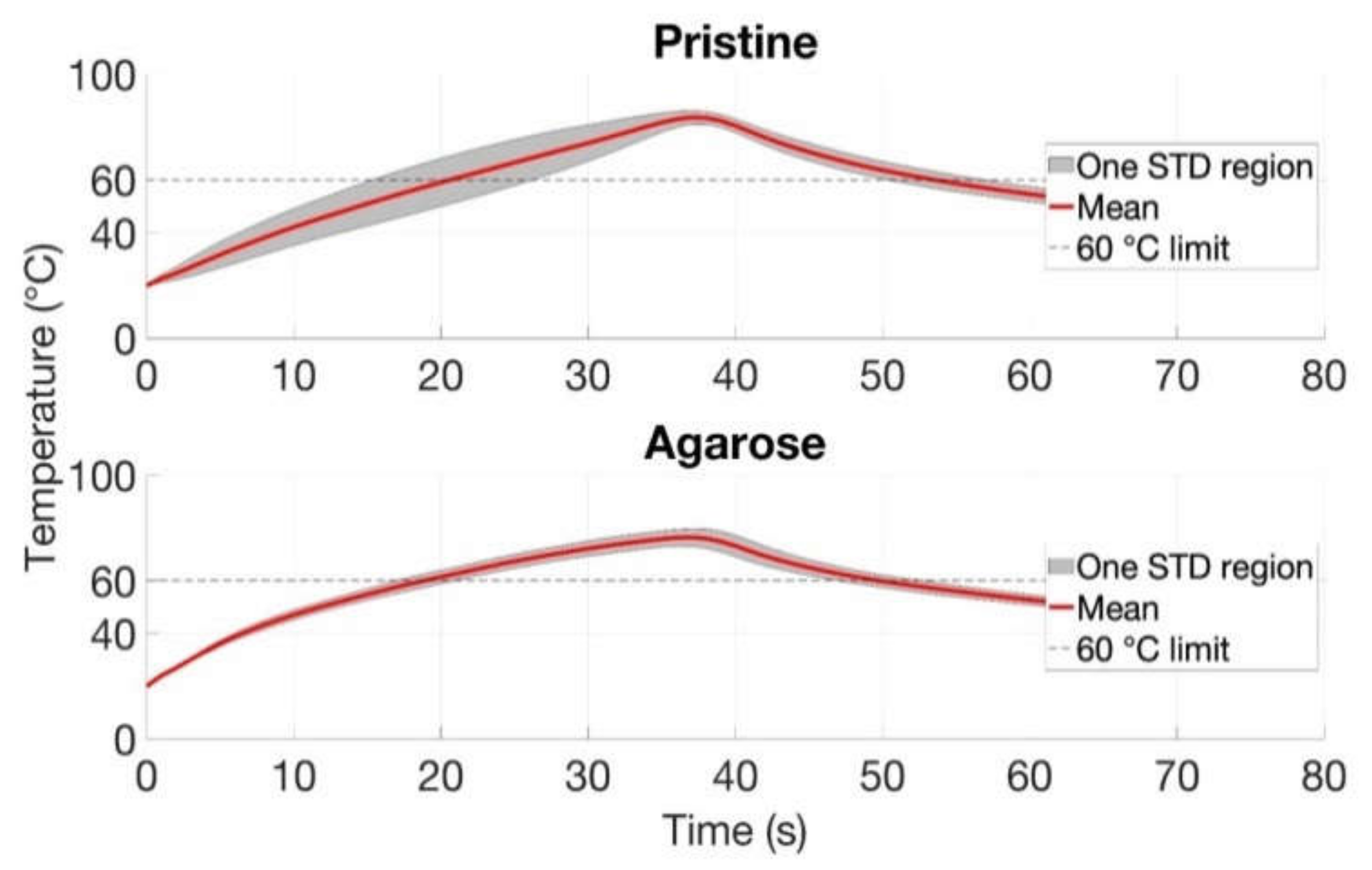
3.2. Maximum Temperature
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Livraghi, T.; Meloni, M.F.; Di Stasi, M.; Rolle, E.; Solbiati, L.; Tinelli, C.; Rossi, S. Sustained complete response and complications rates after radiofrequency ablation of very early hepatocellular carcinoma in cirrhosis: Is resection still the treatment of choice? Hepatology 2007, 47, 82–89. [Google Scholar] [CrossRef]
- Friedman, M.; Mikityansky, I.; Kam, A.; Libutti, S.K.; Walther, M.C.M.; Neeman, Z.; Locklin, J.K.; Wood, B.J. Radiofrequency ablation of cancer. Cardiovasc. Interv. Radiol. 2004, 27, 427–434. [Google Scholar] [CrossRef]
- Lencioni, R.; Crocetti, L. Radiofrequency Ablation of Liver Cancer. Technol. Vasc. Interv. Radiol. 2007, 10, 38–46. [Google Scholar] [CrossRef]
- Morady, F. Radio-Frequency Ablation as Treatment for Cardiac Arrhythmias. N. Engl. J. Med. 1999, 340, 534–544. [Google Scholar] [CrossRef]
- Kapural, L.; Mekhail, N. Radiofrequency ablation for chronic pain control. Curr. Pain Headache Rep. 2001, 5, 517–525. [Google Scholar] [CrossRef] [PubMed]
- Rossi, S.; Garbagnati, F.; Lencioni, R.; Allgaier, H.-P.; Marchianò, A.; Fornari, F.; Quaretti, P.; Di Tolla, G.; Ambrosi, C.; Mazzaferro, V.M.; et al. Percutaneous Radio-frequency Thermal Ablation of Nonresectable Hepatocellular Carcinoma after Occlusion of Tumor Blood Supply. Radiology 2000, 217, 119–126. [Google Scholar] [CrossRef]
- Liang, P.; Wang, Y. Microwave Ablation of Hepatocellular Carcinoma. Oncology 2007, 72, 124–131. [Google Scholar] [CrossRef]
- Natarajan, S.; Raman, S.; Priester, A.M.; Garritano, J.; Margolis, D.J.; Lieu, P.; Macairan, M.L.; Huang, J.; Grundfest, W.; Marks, L.S. Focal Laser Ablation of Prostate Cancer: Phase I Clinical Trial. J. Urol. 2016, 196, 68–75. [Google Scholar] [CrossRef] [PubMed]
- Mohammadi, A.; Bianchi, L.; Korganbayev, S.; De Landro, M.; Saccomandi, P. Thermomechanical Modeling of Laser Ablation Therapy of Tumors: Sensitivity Analysis and Optimization of Influential Variables. IEEE Trans. Biomed. Eng. 2022, 69, 302–313. [Google Scholar] [CrossRef] [PubMed]
- Cavagnaro, M.; Amabile, C.; Bernardi, P.; Pisa, S.; Tosoratti, N. A Minimally Invasive Antenna for Microwave Ablation Therapies: Design, Performances, and Experimental Assessment. IEEE Trans. Biomed. Eng. 2011, 58, 949–959. [Google Scholar] [CrossRef]
- Haemmerich, D.; Tungjitkusolmun, S.; Staelin, S.; Lee, F.; Mahvi, D.; Webster, J. Finite-element analysis of hepatic multiple probe radio-frequency ablation. IEEE Trans. Biomed. Eng. 2002, 49, 836–842. [Google Scholar] [CrossRef]
- Sametova, A.; Kurmashev, S.; Ashikbayeva, Z.; Amantayeva, A.; Blanc, W.; Atabaev, T.S.; Tosi, D. Fiber-optic distributed sensing network for thermal mapping of gold nanoparticles-mediated radiofrequency ablation. Biosensors 2022, 12, 352. [Google Scholar] [CrossRef] [PubMed]
- Ashikbayeva, Z.; Aitkulov, A.; Atabaev, T.S.; Blanc, W.; Inglezakis, V.J.; Tosi, D. Green-Synthesized Silver Nanoparticle–Assisted Radiofrequency Ablation for Improved Thermal Treatment Distribution. Nanomaterials 2022, 12, 426. [Google Scholar] [CrossRef] [PubMed]
- Sapareto, S.A.; Dewey, W.C. Thermal dose determination in cancer therapy. Int. J. Radiat. Oncol. Biol. Phys. 1984, 10, 787–800. [Google Scholar] [CrossRef]
- Huang, H.-W. Influence of blood vessel on the thermal lesion formation during radiofrequency ablation for liver tumors. Med. Phys. 2013, 40, 073303. [Google Scholar] [CrossRef]
- Zorbas, G.; Samaras, T. A study of the sink effect by blood vessels in radiofrequency ablation. Comput. Biol. Med. 2015, 57, 182–186. [Google Scholar] [CrossRef]
- De Vita, E.; De Tommasi, F.; Massaroni, C.; Iadicicco, A.; Faiella, E.; Carassiti, M.; Grasso, R.F.; Schena, E.; Campopiano, S. Investigation of the Heat Sink Effect During Microwave Ablation in Hepatic Tissue: Experimental and Numerical Analysis. IEEE Sens. J. 2021, 21, 22743–22751. [Google Scholar] [CrossRef]
- De Vita, E.; De Landro, M.; Massaroni, C.; Iadicicco, A.; Saccomandi, P.; Schena, E.; Campopiano, S. Fiber Optic Sensors-Based Thermal Analysis of Perfusion-Mediated Tissue Cooling in Liver Undergoing Laser Ablation. IEEE Trans. Biomed. Eng. 2021, 68, 1066–1073. [Google Scholar] [CrossRef] [PubMed]
- Tungjitkusolmun, S.; Staelin, S.; Haemmerich, D.; Tsai, J.-Z.; Cao, H.; Webster, J.; Lee, F.; Mahvi, D.; Vorperian, V. Three-dimensional finite-element analyses for radio-frequency hepatic tumor ablation. IEEE Trans. Biomed. Eng. 2002, 49, 3–9. [Google Scholar] [CrossRef]
- Vaidya, N.; Baragona, M.; Lavezzo, V.; Maessen, R.; Veroy, K. Simulation study of the cooling effect of blood vessels and blood coagulation in hepatic radio-frequency ablation. Int. J. Hyperth. 2021, 38, 95–104. [Google Scholar] [CrossRef]
- Hong, K.; Georgiades, C. Radiofrequency Ablation: Mechanism of Action and Devices. J. Vasc. Interv. Radiol. 2010, 21, S179–S186. [Google Scholar] [CrossRef]
- Nakamuta, M.; Kohjima, M.; Morizono, S.; Yoshimoto, T.; Miyagi, Y.; Sakai, H.; Enjoji, M.; Kotoh, K. Comparison of tissue pressure and ablation time between the LeVeen and cool-tip needle methods. Comp. Hepatol. 2006, 5, 10. [Google Scholar] [CrossRef]
- Ashikbayeva, Z.; Tosi, D.; Balmassov, D.; Schena, E.; Saccomandi, P.; Inglezakis, V. Application of Nanoparticles and Nanomaterials in Thermal Ablation Therapy of Cancer. Nanomaterials 2019, 9, 1195. [Google Scholar] [CrossRef] [PubMed]
- Puza, C.J.; Wang, Q.; Kim, C.Y. Evaluation of the Heat Sink Effect After Transarterial Embolization When Performed in Combination with Thermal Ablation of the Liver in a Rabbit Model. Cardiovasc. Interv. Radiol. 2018, 41, 1773–1778. [Google Scholar] [CrossRef] [PubMed]
- Pillai, K.; Akhter, J.; Chua, T.C.; Shehata, M.; Alzahrani, N.; Al-Alem, I.; Morris, D.L. Heat Sink Effect on Tumor Ablation Characteristics as Observed in Monopolar Radiofrequency, Bipolar Radiofrequency, and Microwave, Using Ex Vivo Calf Liver Model. Medicine 2015, 94, e580. [Google Scholar] [CrossRef] [PubMed]
- Saccomandi, P.; Schena, E.; Silvestri, S. Techniques for temperature monitoring during laser-induced thermotherapy: An overview. Int. J. Hyperth. 2013, 29, 609–619. [Google Scholar] [CrossRef]
- Beisenova, A.; Issatayeva, A.; Sovetov, S.; Korganbayev, S.; Jelbuldina, M.; Ashikbayeva, Z.; Blanc, W.; Schena, E.; Sales, S.; Molardi, C.; et al. Multi-fiber distributed thermal profiling of minimally invasive thermal ablation with scattering-level multiplexing in MgO-doped fibers. Biomed. Opt. Express 2019, 10, 1282. [Google Scholar] [CrossRef]
- Froggatt, M.; Moore, J. High-spatial-resolution distributed strain measurement in optical fiber with Rayleigh scatter. Appl. Opt. 1998, 37, 1735. [Google Scholar] [CrossRef] [PubMed]
- Macchi, E.G.; Tosi, D.; Braschi, G.; Gallati, M.; Cigada, A.; Busca, G.; Lewis, E. Optical fiber sensors-based temperature distribution measurement in ex vivo radiofrequency ablation with submillimeter resolution. J. Biomed. Opt. 2014, 19, 117004. [Google Scholar] [CrossRef]
- Blanc, W.; Martin, I.; Francois-Saint-Cyr, H.; Bidault, X.; Chaussedent, S.; Hombourger, C.; Lacomme, S.; Le Coustumer, P.; Neuville, D.R.; Larson, D.J.; et al. Compositional Changes at the Early Stages of Nanoparticles Growth in Glasses. J. Phys. Chem. C 2019, 123, 29008–29014. [Google Scholar] [CrossRef]
- Beisenova, A.; Issatayeva, A.; Ashikbayeva, Z.; Jelbuldina, M.; Aitkulov, A.; Inglezakis, V.; Blanc, W.; Saccomandi, P.; Molardi, C.; Tosi, D. Distributed Sensing Network Enabled by High-Scattering MgO-Doped Optical Fibers for 3D Temperature Monitoring of Thermal Ablation in Liver Phantom. Sensors 2021, 21, 828. [Google Scholar] [CrossRef]
- Chen, R.; Lu, F.; Wu, F.; Jiang, T.; Xie, L.; Kong, D. An analytical solution for temperature distributions in hepatic radiofrequency ablation incorporating the heat-sink effect of large vessels. Phys. Med. Biol. 2018, 63, 235026. [Google Scholar] [CrossRef] [PubMed]
- Blanc, W.; Dussardier, B. Formation and applications of nanoparticles in silica optical fibers. J. Opt. 2015, 45, 247–254. [Google Scholar] [CrossRef]
- Blanc, W.; Lu, Z.; Robine, T.; Pigeonneau, F.; Molardi, C.; Tosi, D. Nanoparticles in optical fiber, issue and opportunity of light scattering [Invited]. Opt. Mater. Express 2022, 12, 2635. [Google Scholar] [CrossRef]
- Beisenova, A.; Issatayeva, A.; Korganbayev, S.; Molardi, C.; Blanc, W.; Tosi, D. Simultaneous Distributed Sensing on Multiple MgO-Doped High Scattering Fibers by Means of Scattering-Level Multiplexing. J. Light. Technol. 2019, 37, 3413–3421. [Google Scholar] [CrossRef]
- Veber, A.; Lu, Z.; Vermillac, M.; Pigeonneau, F.; Blanc, W.; Petit, L. Nano-Structured Optical Fibers Made of Glass-Ceramics, and Phase Separated and Metallic Particle-Containing Glasses. Fibers 2019, 7, 105. [Google Scholar] [CrossRef]
- Schena, E.; Saccomandi, P.; Fong, Y. Laser ablation for cancer: Past, present and future. J. Funct. Biomater. 2017, 8, 19. [Google Scholar] [CrossRef]






Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sametova, A.; Kurmashev, S.; Ashikbayeva, Z.; Blanc, W.; Tosi, D. Optical Fiber Distributed Sensing Network for Thermal Mapping in Radiofrequency Ablation Neighboring a Blood Vessel. Biosensors 2022, 12, 1150. https://doi.org/10.3390/bios12121150
Sametova A, Kurmashev S, Ashikbayeva Z, Blanc W, Tosi D. Optical Fiber Distributed Sensing Network for Thermal Mapping in Radiofrequency Ablation Neighboring a Blood Vessel. Biosensors. 2022; 12(12):1150. https://doi.org/10.3390/bios12121150
Chicago/Turabian StyleSametova, Akbota, Sabit Kurmashev, Zhannat Ashikbayeva, Wilfried Blanc, and Daniele Tosi. 2022. "Optical Fiber Distributed Sensing Network for Thermal Mapping in Radiofrequency Ablation Neighboring a Blood Vessel" Biosensors 12, no. 12: 1150. https://doi.org/10.3390/bios12121150
APA StyleSametova, A., Kurmashev, S., Ashikbayeva, Z., Blanc, W., & Tosi, D. (2022). Optical Fiber Distributed Sensing Network for Thermal Mapping in Radiofrequency Ablation Neighboring a Blood Vessel. Biosensors, 12(12), 1150. https://doi.org/10.3390/bios12121150







