Bioprinting on Organ-on-Chip: Development and Applications
Abstract
:1. Introduction
2. 3D Bioprinting Techniques
2.1. Nozzle-Based Methods for Bioprinting
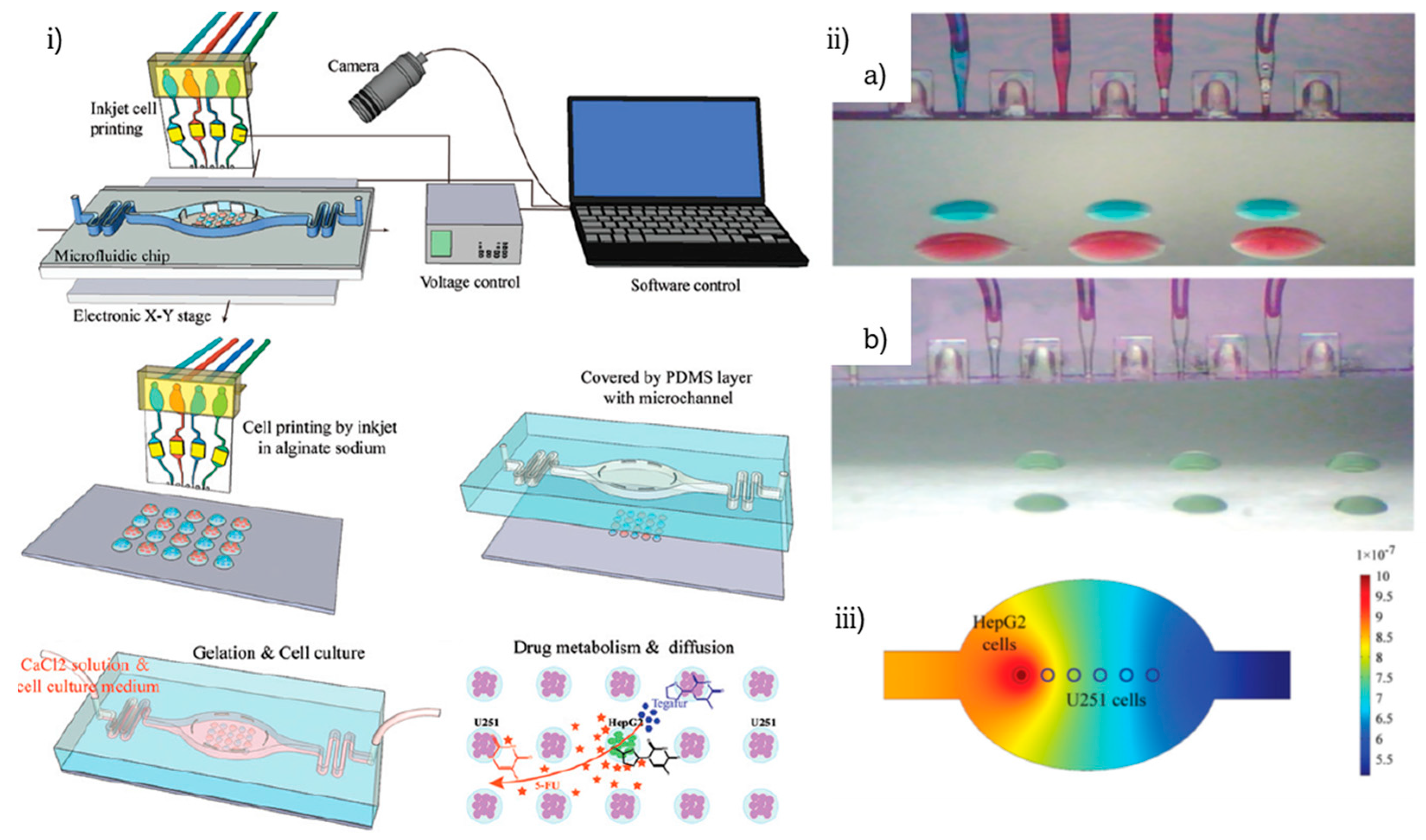
2.1.1. Inkjet Bioprinting
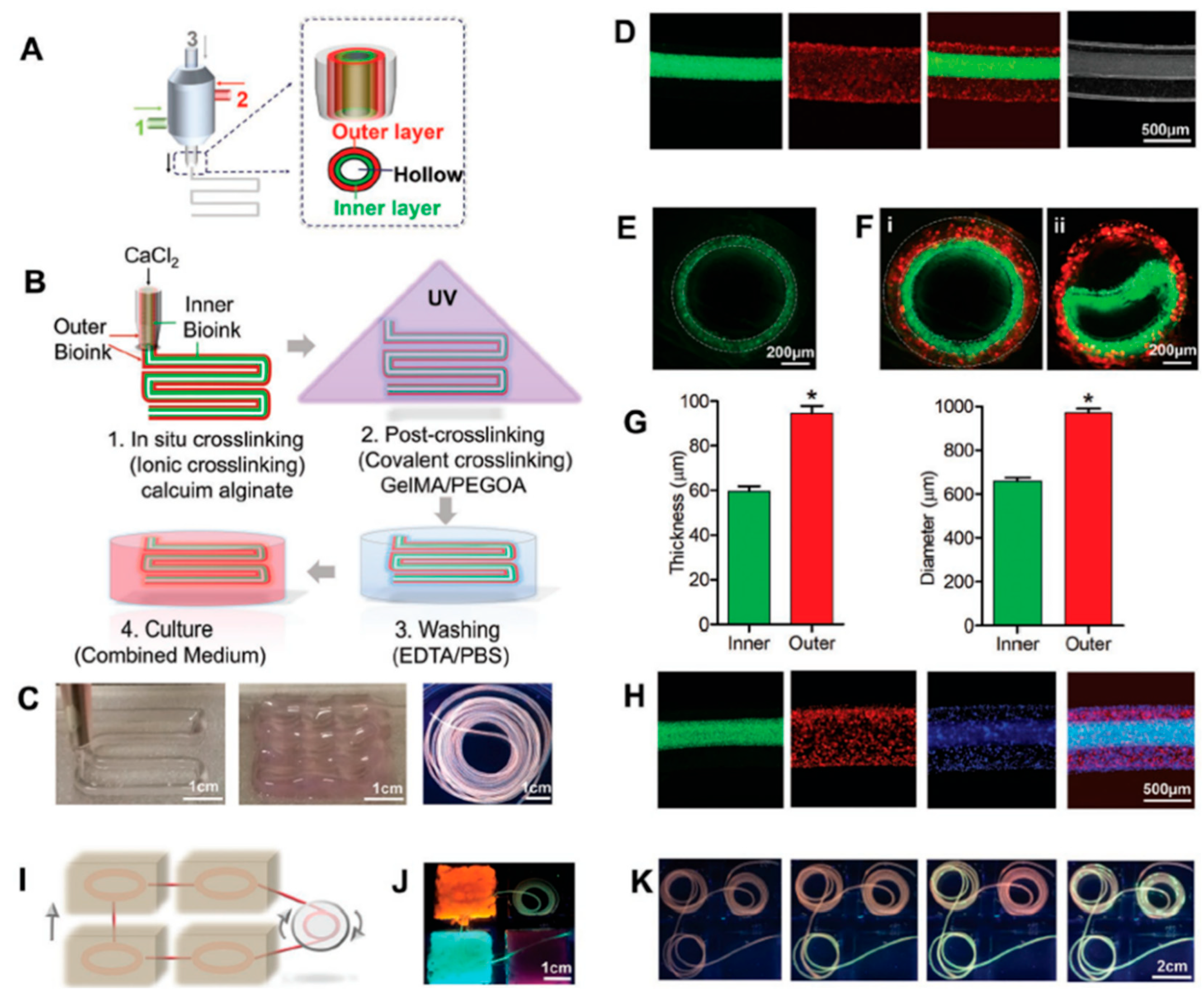
2.1.2. Micro-Extrusion Bioprinting
2.1.3. Freeform Reversible Embedding of Suspended Hydrogels (FRESH)
2.2. Light-Assisted Methods for Bioprinting
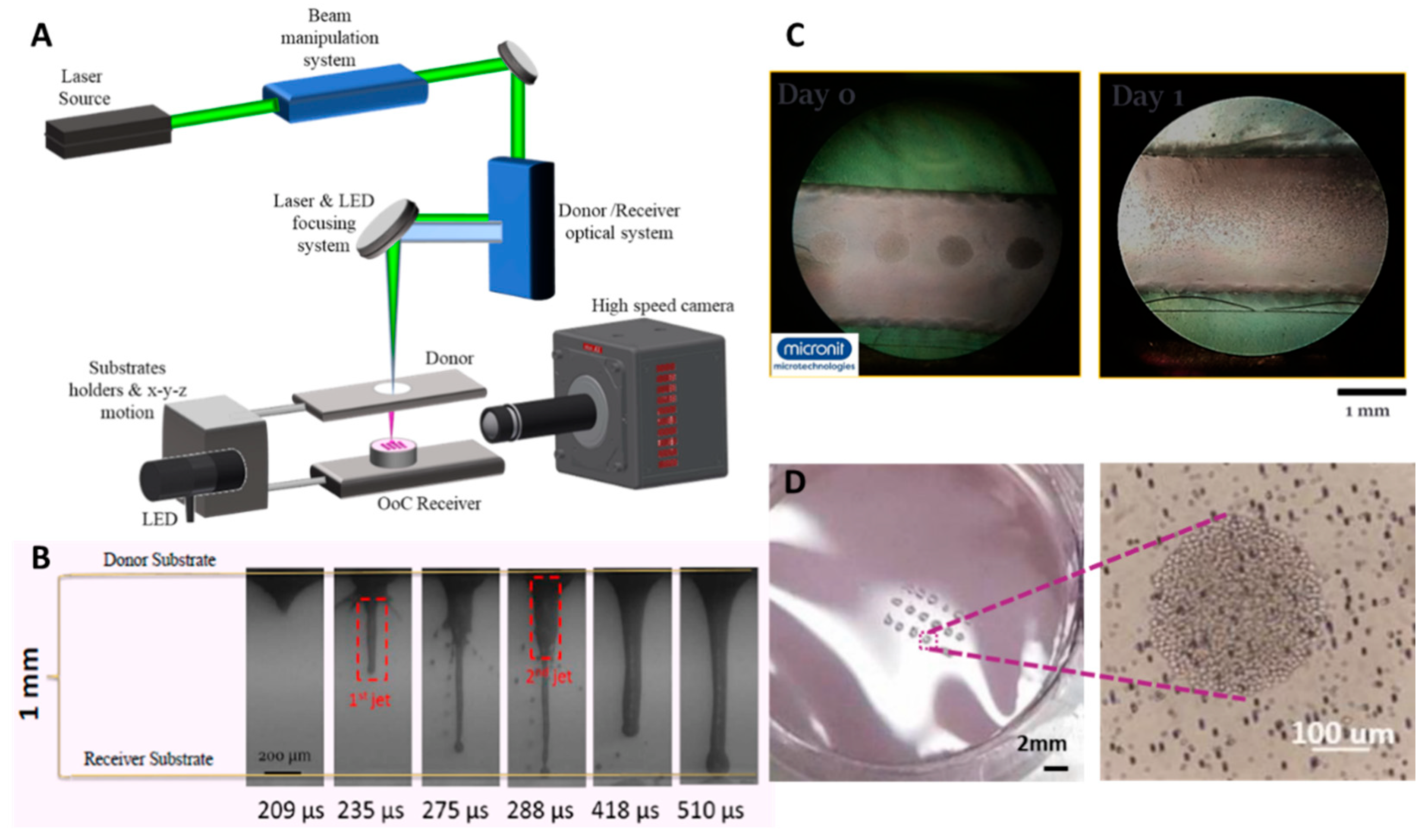
2.2.1. Laser-Induced Forward Transfer
2.2.2. Stereolithography and Digital Light Processing
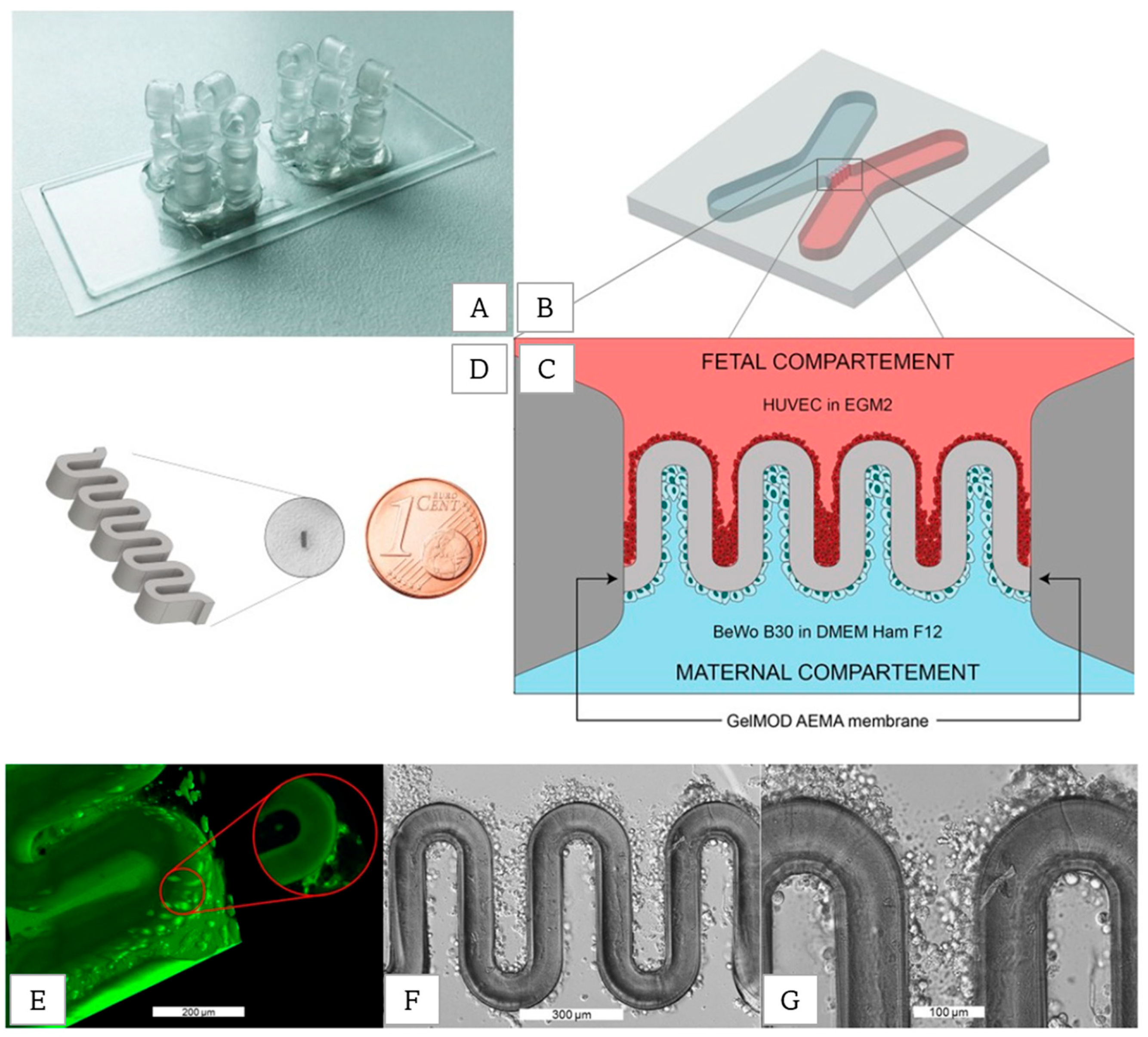
2.2.3. Micro-Molding Bioprinting
2.2.4. Two-Photon Polymerization
2.2.5. Tomographic Volumetric Bioprinting (TVB)
2.2.6. Filamented Light (FLight) Bioprinting
2.3. Micro-Valve Bioprinting
2.4. Acousting Bioprinting
3. Advantages of Bioprinting in OoC Devices
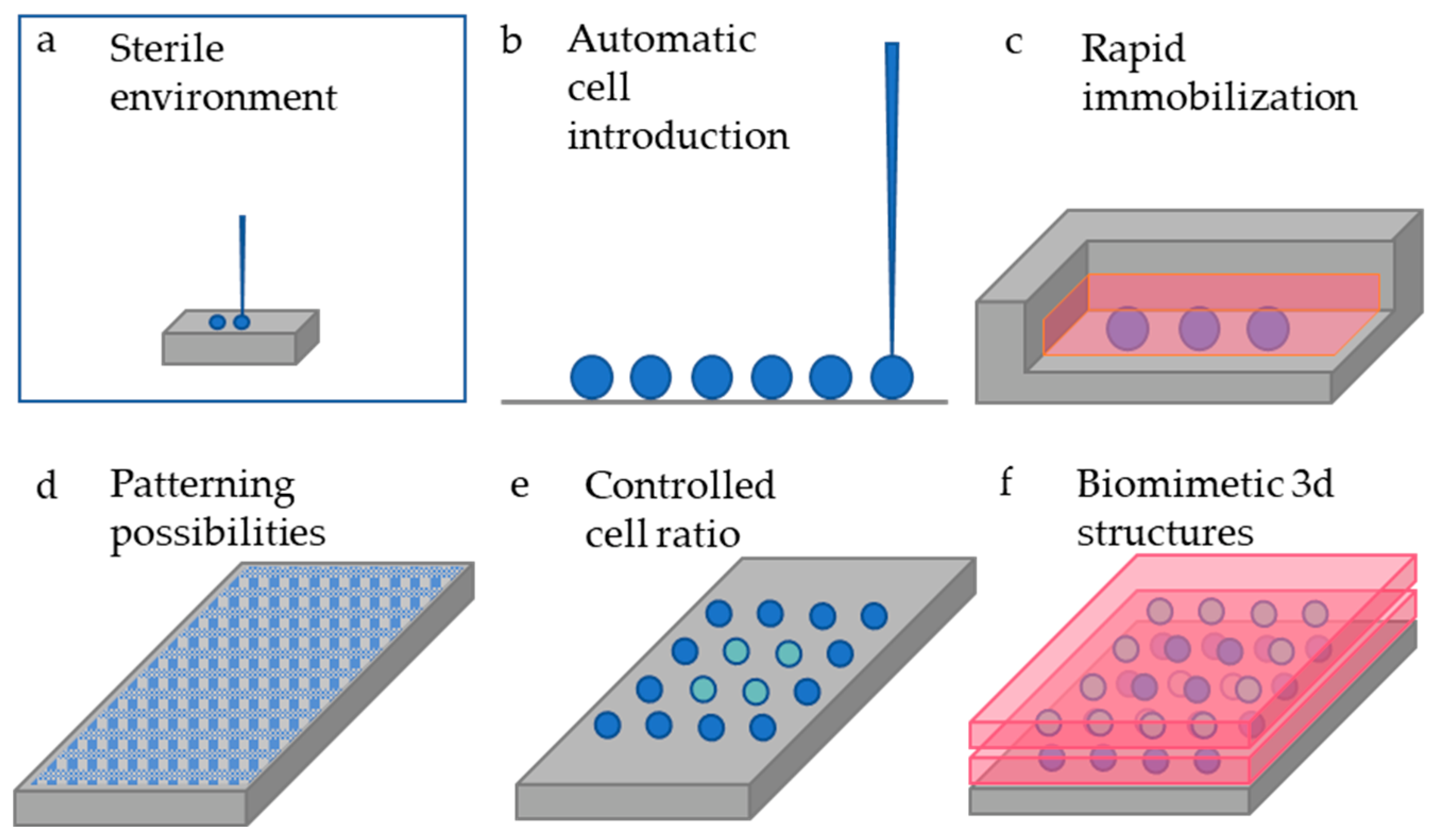
- In most cases, the introduction of cells in microfluidic devices is preformed manually via pipette. Knowing that laboratory personnel is one of the greatest sources of contamination [48], by installing bioprinters inside sterile environments, human interference would be minimized which will lead to less exposure to contaminating agents.
- Bioprinting techniques will enhance the automatic introduction of cells in microfluidic devices for developing less time-consuming experiments with higher reproducibility [49] than those where the cells are introduced via pipette.
- Rapid immobilization of cells, achieved through bioprinting, supports direct introduction of liquid flow. Normal cells, when seeded with a pipette, take 6–8 h to develop attachment proteins, hence when seeded in microfluidic devices, they are usually left overnight to reach adherence, resulting in serious time delays before adding culture media flow.
- To replicate physiological cell functions in vitro, it is necessary to simulate cell communications [56] by introducing the desired cell to cell ratios with great precision. Bioprinted techniques can be utilized to deposit a range of cells per droplet, depending on the printing conditions, even with resolutions down to one cell per droplet [19,57], which offers consequential ratio control.
- High levels of biomimicry can be achieved. The greatest benefit of 3D bioprinting is the ability to digitally fabricate the tissue of interest and reproduce the 3D physical structure through automated techniques and at resolutions not possible with traditional photolithography techniques [19,58,59,60].
- Traditional introduction of cells in OoCs or in cell culture plates, with the use of pipettes or pumps, stands as a less expensive cell introduction method; however, it is not suitable for cell patterning, instant immobilization or for achieving high levels of biomimicry.
4. Applications of Bioprinting in OoC
4.1. Blood Vessels and Vascular Microenvironments
4.2. Brain
4.3. Gut
4.4. Heart
4.5. Kidney
4.6. Liver
4.7. Lung
4.8. Ovaries
4.9. Placenta
4.10. Urothelium
4.11. Tumor in General
| Reference | Organ/Tissue | Bioprinting Technique | Bioink | Aim | Outcome |
|---|---|---|---|---|---|
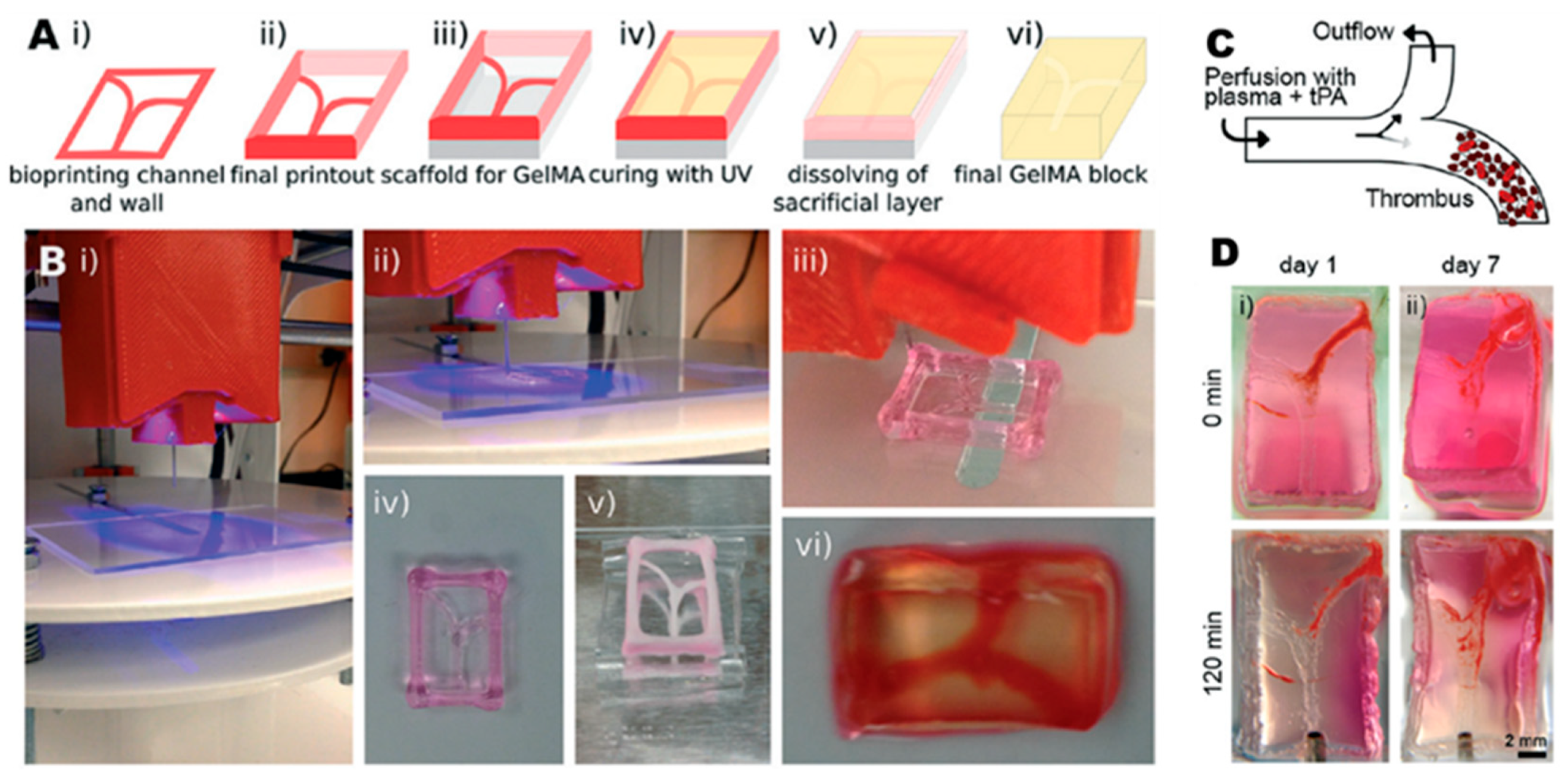
| Y.S. Zhang et al. [65] | Vascular thrombosis | Micro-molding | Fibroblast mixed with GelMA, HUVECs | Fabrication of an in vitro platform for potential therapeutics to treat thrombosis | Encapsulation of fibroblasts in GelMA demonstrated potential cell migration to clot |
| M. Abudupataer et al. [66] | Vessel | Micro-extrusion | GelMA, HAECs, HASMC, NIH/3 T3 | Stimulate different types of vessels and blood flows | Cellular coculture system based vessel-on-a-chip model with a continuous flow |
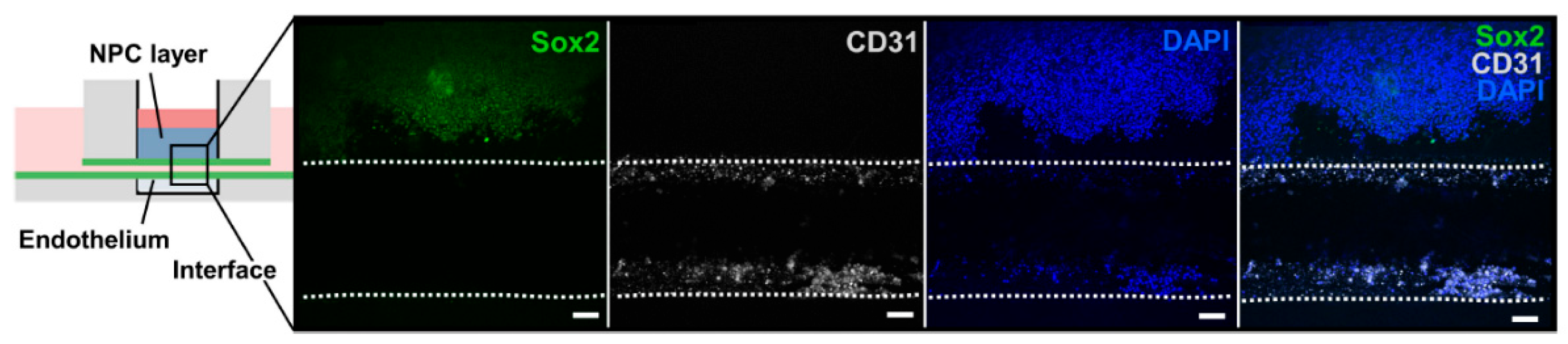
| D. F. D. Campos et al. [67] | Vascular tissue | DoD and Micro-extrusion | ELP, engineered hydrogels, hiPSC-NPCs | Tissue models, di-rectly dispensed onto endothelialized on-chip platform | Compatible bioprinting techniques with single cell suspension and spheroid aggregates of breast cells |
| H.G. Yi et al. [72] | Glioblastoma | Inkjet | BdECM, patient derived cells | Treatment testing | Establishment of a glioblastoma-on-a-chip platform |
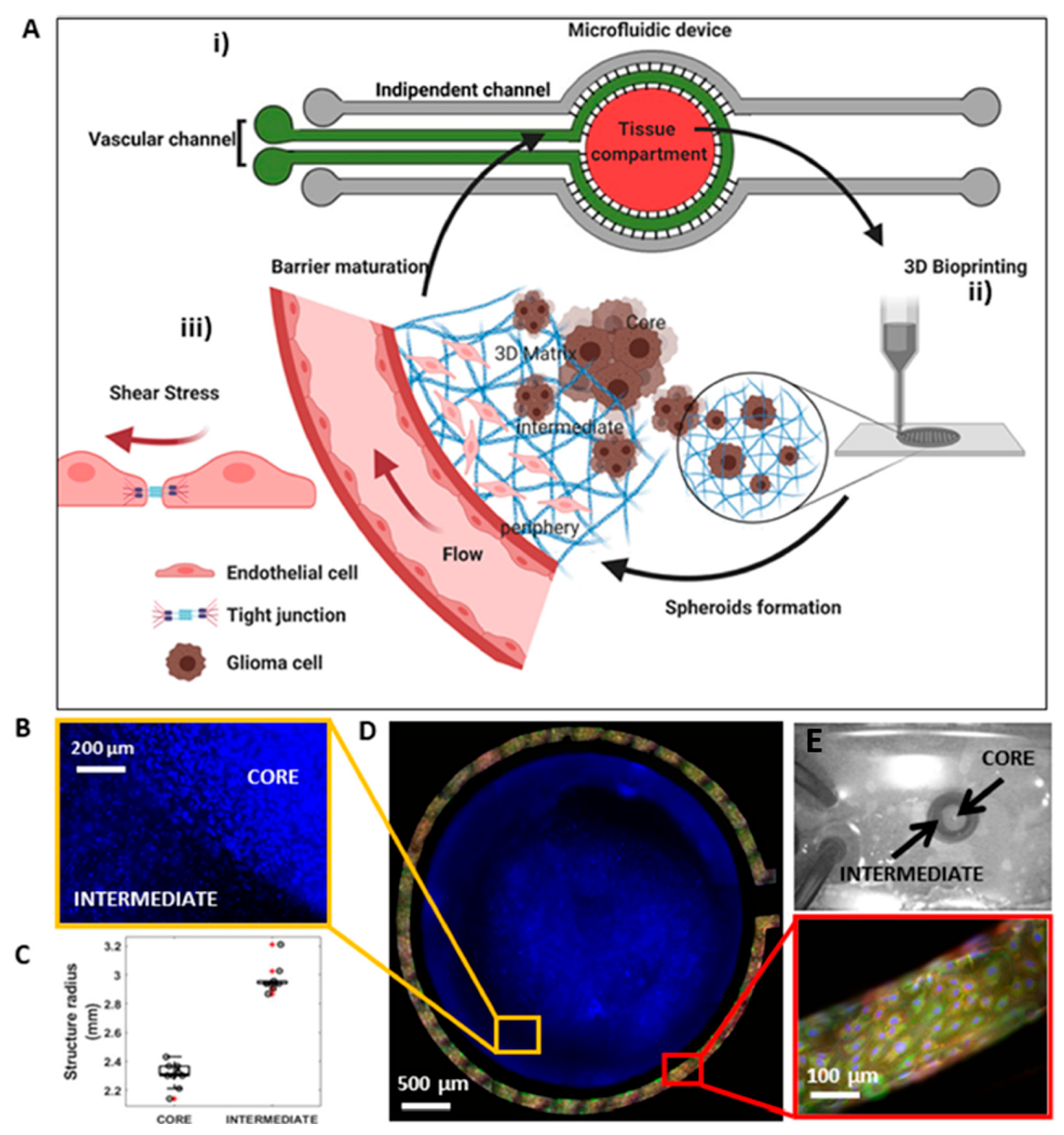
| G. Silvani et al. [74] | Glioblastoma | Micro-extrusion | GelMA, GBM cells, Endothelial cells | Test of brain tumor responses to microgravity | Absence of micro-gravitational fields, inhibited invasion, and aggregation of glioblastoma cells |
| E.B. García et al. [76] | Gut | SLA | GelMA, PEGDA, cell-laden | Replicate gut epithelial barrier and lamina propria | No migration observed in gut-on-a-chip |
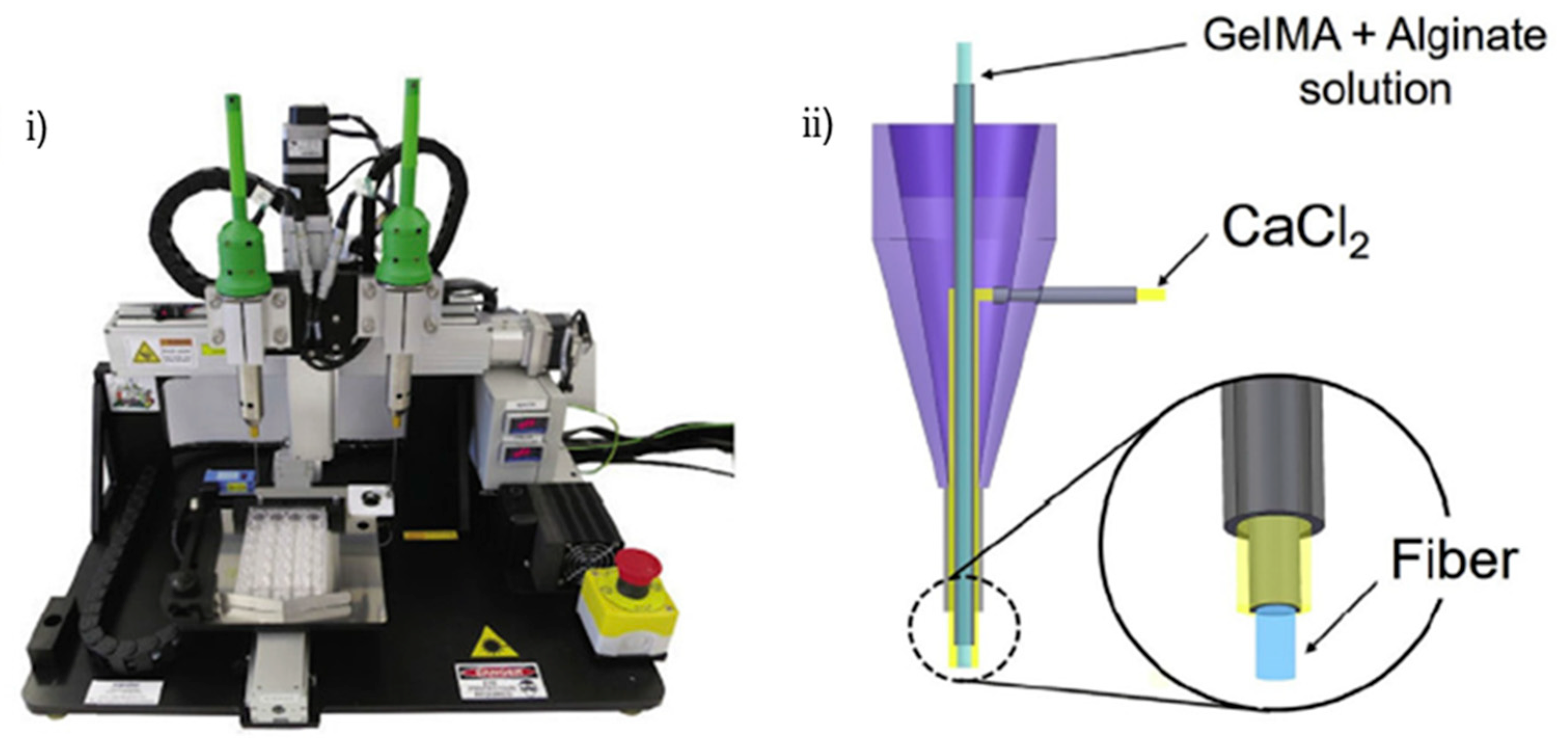
| Y.S. Zhang et al. [77] | Myocardium | Micro-extrusion | GelMA, HUVECs | Fabrication of en-dothelialized my-ocardium | Endothelial cells bioprinted within microfibrous hydrogel scaffolds, migration towards peripheries, layer of confluent endotheliumobserved |
| K.A. Homan et al. [39] | Proximal tubule | Micro-molding | Gelatin fibrinogen | Create 3D human renal proximal tubules in vitro | 2-month maintenance in perfusable culture |
| R. Chang et al. [80] | Hepatocyte tissue | Nozzle-based | Alginate-encapsulated hepatocytes | Development of in vitro pharmacokinetic model | Nonfluorescent prodrug, metabolized by the liver chamber which produced an effluent fluorescent metabolite |
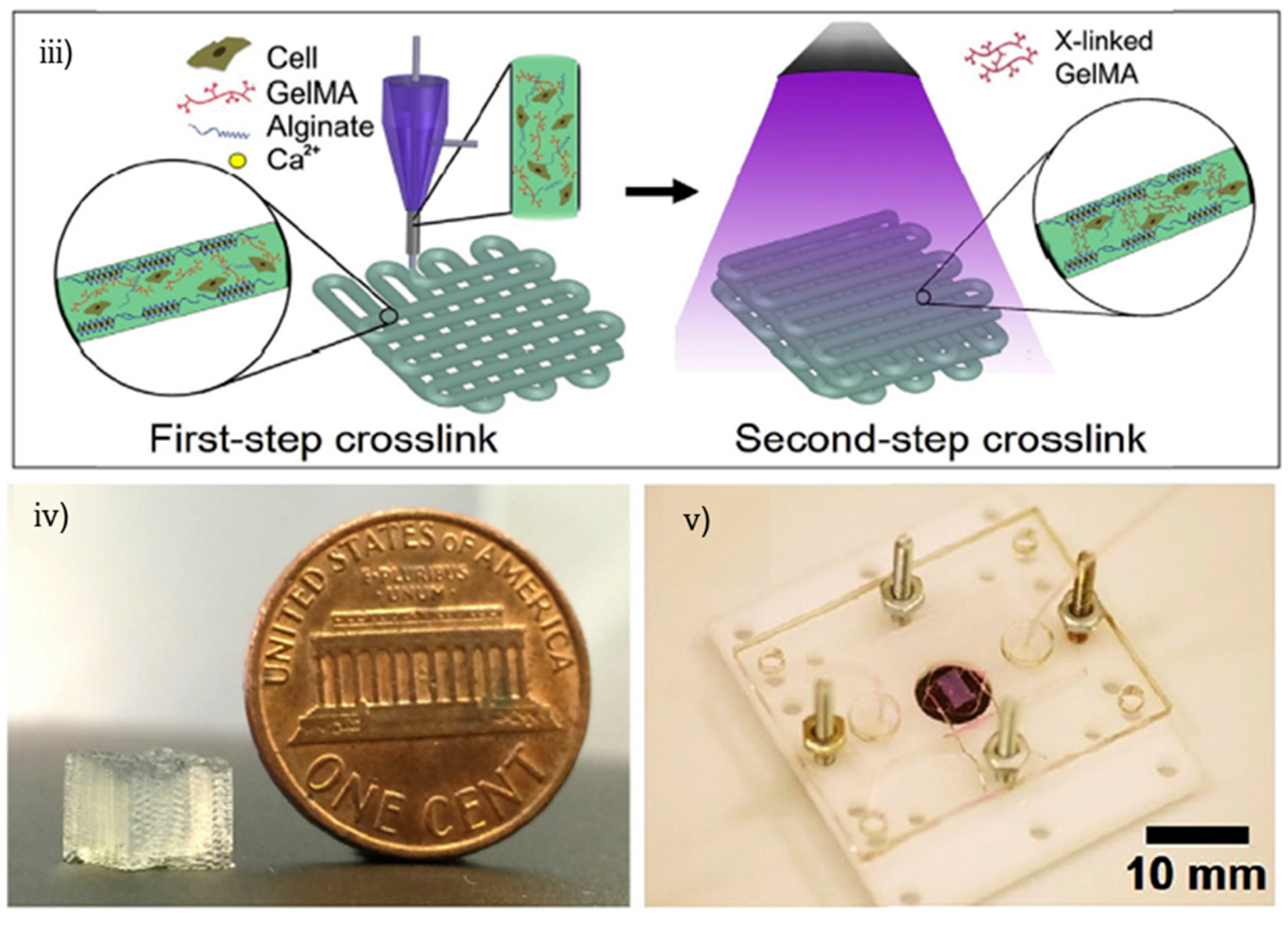
| J.E. Snyder et al. [81] | Liver | Micro-extrusion | HepG2, M10, Matrigel | Drug conversion and radiation protection of living liver tissue analogs | Observed radiation shielding in the dual-tissue microfluidic system caused by the 2-cell type interaction |
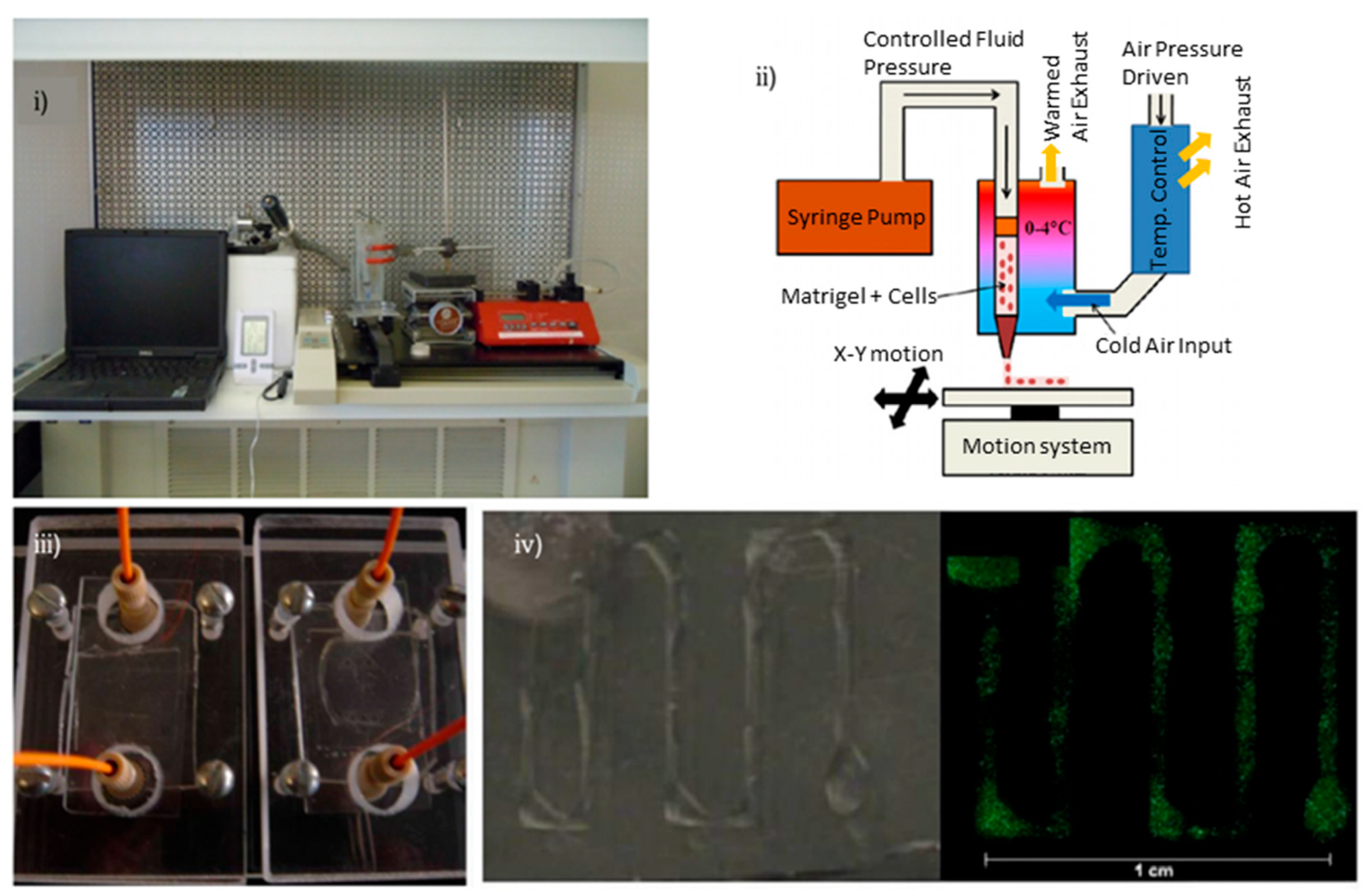
| N.S. Bhise et al. [82] | Liver | Piston micro-extrusion | GelMA, Hepatic spheroids (HepG2,C3A) | Assembly of a biomimetic liver-on-a-chip platform | In situ monitoring of culture environment, viability after 30 days, responsive to treatment |
| J. Zhang et al. [83] | Liver | Inkjet | HepG2, U251, alginate hydrogel | Detection of drug metabolism and diffusion | Viability gradient observed during drug metabolism and diffusion |
| H. Lee and D.W. Cho [84] | Liver | Pneumatic micro-extrusion | HepG2, HUVECs, Gelatin, Collagen | One step liver-on-chip fabrication | Established new micro-engineering method for organ-on-chip to overcome drawbacks |
| H. Lee et al. [85] | Liver | Nozzle-based | dECM, HUVECs | Fabrication of biomimetic liver-on-chip with biliary system | Function of chip superior to 2D or 3D cultures, sensitive drug response |
| S. Elezoglou et al. [34] | Lung | LIFT | LLC cell line | Using LIFT Bioprinting technique to deposit high concentration cells in organ-on-chip platform | Preliminary studies of bioprinting lung cancer cells, optimization studies about LIFT bioprinting inside OoC. |
| Y.S. Choi et al. [86] | Ovary | Not mentioned | Mouse ovarian aggregates, GelMA | Ovary-on-a-chip platform development for ovarian endocrine function in vitro | Physiologically relevant hormonal production |
| D. Mandt et al. [55] | Placenta | Two-photon polymerization | GelMOD- AEM, | Pattern placental barrier | Versatile biomimetic on chip barrier structure establishment |
| Q. Pi [87] | Urothelial tissue | Micro-extrusion | hSMCs, HUVECs, HBdSMCs, GelMA | Single step cannular tissues circumferentially multilayered | Sustained viability, similar to human characteristics, 2-week continuous perfusion |
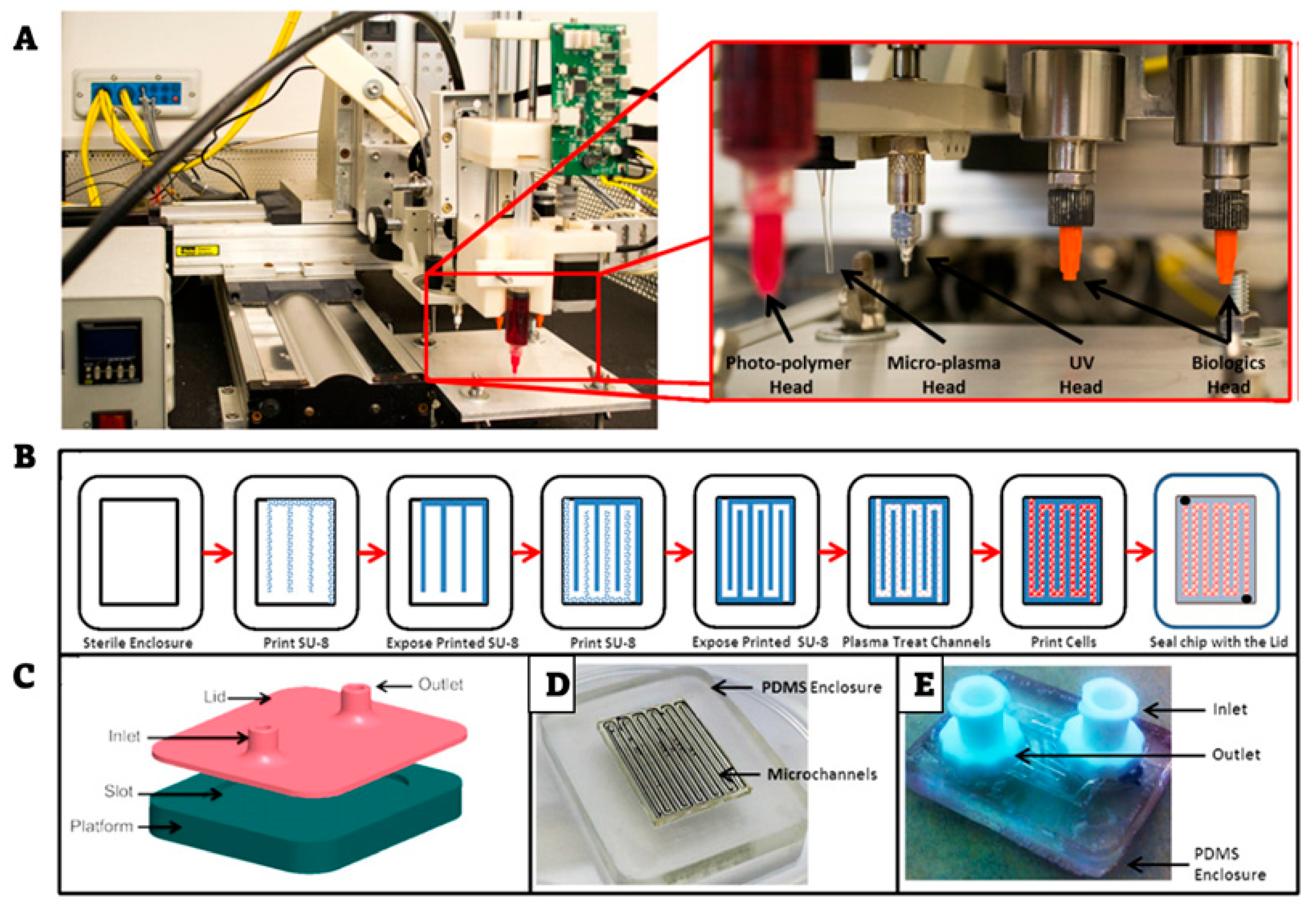
| Q. Hamid et al. [92] | Tumor | Piston microxtrusion | HepG2, MDA-MB-231 | Maskless fabrication techniques for cell-laden microfluidics development | Fabrication system eliminates the limitations of conventional photolithography |
| X. Cao et al. [93] | Tumor | Nozzle-based | GelMA, PEGDA/PEGOA | Bioprinting of blood and lymphatic vessels | Permeability parameters of bioprinted blood and lymphatic vessels could be controlled by precisely tuning the bioink’s composition |
| M. Xie et al. [94] | Tumor | Inkjet | GelMA, MDA-MB-231 | 3D tumor array chip (TAC) fabrication for drug testing | 3D-TAC has potential to become a widely applied standard 3D drug screening system |
5. Summary/Conclusions
6. Future Directions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sun, D.; Gao, W.; Hu, H.; Zhou, S. Why 90% of clinical drug development fails and how to improve it? Acta Pharm. Sin. B 2022, 12, 3049–3062. [Google Scholar] [CrossRef] [PubMed]
- Takebe, T.; Imai, R.; Ono, S. The Current Status of Drug Discovery and Development as Originated in United States Academia: The Influence of Industrial and Academic Collaboration on Drug Discovery and Development. Clin. Transl. Sci. 2018, 11, 597–606. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Koyilot, M.C.; Natarajan, P.; Hunt, C.R.; Sivarajkumar, S.; Roy, R.; Joglekar, S.; Pandita, S.; Tong, C.W.; Marakkar, S.; Subramanian, L.; et al. Breakthroughs and Applications of Organ-on-a-Chip Technology. Cells 2022, 11, 1828. [Google Scholar] [CrossRef] [PubMed]
- Huh, D.; Hamilton, G.A.; Ingber, D.E. From 3D cell culture to organs-on-chips. Trends Cell Biol. 2011, 21, 745–754. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Akhtar, A. The Flaws and Human Harms of Animal Experimentation. Camb. Q. Health Ethic 2015, 24, 407–419. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grimm, D.U.S. EPA to Eliminate all Mammal Testing by 2035. Available online: https://www.science.org/content/article/us-epa-eliminate-all-mammal-testing-2035 (accessed on 10 September 2019).
- Administrator Wheeler Signs Memo to Reduce Animal Testing, Awards $4.25 Million to Advance Research on Alternative Methods to Animal Testing. Available online: https://www.epa.gov/newsreleases/administrator-wheeler-signs-memo-reduce-animal-testing-awards-425-million-advance (accessed on 10 September 2019).
- Yan, J.; Li, Z.; Guo, J.; Liu, S.; Guo, J. Organ-on-a-chip: A new tool for in vitro research. Biosens. Bioelectron. 2022, 216, 114626. [Google Scholar] [CrossRef]
- Sontheimer-Phelps, A.; Hassell, B.A.; Ingber, D.E. Modelling cancer in microfluidic human organs-on-chips. Nat. Rev. Cancer 2019, 19, 65–81. [Google Scholar] [CrossRef]
- Lantada, A.D.; Pfleging, W.; Besser, H.; Guttmann, M.; Wissmann, M.; Plewa, K.; Smyrek, P.; Piotter, V.; García-Ruíz, J.P. Research on the Methods for the Mass Production of Multi-Scale Organs-On-Chips. Polymers 2018, 10, 1238. [Google Scholar] [CrossRef] [Green Version]
- Probst, C.; Schneider, S.; Loskill, P. High-throughput organ-on-a-chip systems: Current status and remaining challenges. Curr. Opin. Biomed. Eng. 2018, 6, 33–41. [Google Scholar] [CrossRef]
- Low, A.L.; Tagle, A.D. Organs-on-chips: Progress, challenges, and future directions. Exp. Biol. Med. 2017, 242, 1573–1578. [Google Scholar] [CrossRef]
- Murphy, S.V.; Atala, A. 3D bioprinting of tissues and organs. Nat. Biotechnol. 2014, 32, 773–785. [Google Scholar] [CrossRef] [PubMed]
- Karzyński, K.; Kosowska, K.; Ambrożkiewicz, F.; Berman, A.; Cichoń, J.; Klak, M.; Serwańska-Świętek, M.; Wszoła, M. Use of 3D bioprinting in biomedical engineering for clinical application. Med. Stud. 2018, 34, 93–97. [Google Scholar] [CrossRef] [Green Version]
- Sun, W.; Starly, B.; Daly, A.C.; Burdick, A.J.; Groll, J.; Skeldon, G.; Shu, W.; Sakai, Y.; Shinohara, M.; Nishikawa, M.; et al. The bioprinting roadmap. Biofabrication 2020, 12, 022002. [Google Scholar] [CrossRef] [PubMed]
- Muskan; Gupta, D.; Negi, N.P. 3D bioprinting: Printing the future and recent advances. Bioprinting 2022, 27, e00211. [Google Scholar] [CrossRef]
- Jain, P.; Kathuria, H.; Dubey, N. Advances in 3D bioprinting of tissues/organs for regenerative medicine and in-vitro models. Biomaterials 2022, 287, 121639. [Google Scholar] [CrossRef] [PubMed]
- Miri, A.K.; Mostafavi, E.; Khorsandi, D.; Hu, S.-K.; Malpica, M.; Khademhosseini, A. Bioprinters for organs-on-chips. Biofabrication 2019, 11, 042002. [Google Scholar] [CrossRef]
- Zhang, L.G.; Leong, K.; Fisher, J.P. 3D Bioprinting and Nanotechnology in Tissue Engineering and Regenerative Medicine; Academic Press: Cambridge, MA, USA, 2022. [Google Scholar]
- Gudapati, H.; Dey, M.; Ozbolat, I. A comprehensive review on droplet-based bioprinting: Past, present and future. Biomaterials 2016, 102, 20–42. [Google Scholar] [CrossRef] [Green Version]
- Xu, T.; Jin, J.; Gregory, C.; Hickman, J.J.; Boland, T. Inkjet printing of viable mammalian cells. Biomaterials 2005, 26, 93–99. [Google Scholar] [CrossRef]
- Saunders, R.E.; Gough, J.E.; Derby, B. Delivery of human fibroblast cells by piezoelectric drop-on-demand inkjet printing. Biomaterials 2008, 29, 193–203. [Google Scholar] [CrossRef]
- Kumar, P.; Ebbens, S.; Zhao, X. Inkjet printing of mammalian cells—Theory and applications. Bioprinting 2021, 23, e00157. [Google Scholar] [CrossRef]
- Horváth, L.; Umehara, Y.; Jud, C.; Blank, F.; Fink, A.; Rothen-Rutishauser, B. Engineering an in vitro air-blood barrier by 3D bioprinting. Sci. Rep. 2015, 5, srep07974. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nair, K.; Gandhi, M.; Khalil, S.; Yan, K.C.; Marcolongo, M.; Barbee, K.; Sun, W. Characterization of cell viability during bioprinting processes. Biotechnol. J. 2009, 4, 1168–1177. [Google Scholar] [CrossRef] [PubMed]
- Shim, J.-H.; Lee, J.-S.; Kim, J.Y.; Cho, D.-W. Bioprinting of a mechanically enhanced three-dimensional dual cell-laden construct for osteochondral tissue engineering using a multi-head tissue/organ building system. J. Micromech. Microeng. 2012, 22, 085014. [Google Scholar] [CrossRef]
- Ozbolat, I.T.; Hospodiuk, M. Current advances and future perspectives in extrusion-based bioprinting. Biomaterials 2016, 76, 321–343. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tan, N.; Yang, Y.Y. Building blocks to the future of regenerative medicine: Organoid bioprinting. Matter 2021, 4, 2659–2661. [Google Scholar] [CrossRef]
- Tejo-Otero, A.; Colly, A.; Courtial, E.; Fenollosa-Artés, F.; Buj-Corral, I.; Marquette, C.A. Freeform Reversible Embedding of Suspended Hydrogels for the Manufacturing of Biomedical Applications Design of State of the Art Mechanical Infinite Continuously Variable Transmission View Project 3D Printing of Soft PDMS View Project Edwin-Joffrey Courtial Freeform Reversible Embedding of Suspended Hydrogels for the Manufacturing of Biomedical Applications. Available online: https://www.researchgate.net/publication/346314447 (accessed on 7 April 2022).
- Karakaidos, P.; Kryou, C.; Simigdala, N.; Klinakis, A.; Zergioti, I. Laser Bioprinting of Cells Using UV and Visible Wavelengths: A Comparative DNA Damage Study. Bioengineering 2022, 9, 378. [Google Scholar] [CrossRef]
- Kryou, C.; Leva, V.; Chatzipetrou, M.; Zergioti, I. Bioprinting for Liver Transplantation. Bioengineering 2019, 6, 95. [Google Scholar] [CrossRef] [Green Version]
- Koch, L.; Deiwick, A.; Franke, A.; Schwanke, K.; Haverich, A.; Zweigerdt, R.; Chichkov, B.N. Laser bioprinting of human induced pluripotent stem cells—The effect of printing and biomaterials on cell survival, pluripotency, and differentiation. Biofabrication 2018, 10, 035005. [Google Scholar] [CrossRef]
- Zergioti, I.; Karaiskou, A.; Papazoglou, D.; Fotakis, C.; Kapsetaki, M.; Kafetzopoulos, D. Femtosecond laser microprinting of biomaterials. Appl. Phys. Lett. 2005, 86, 163902. [Google Scholar] [CrossRef] [Green Version]
- Stavroula, E. Laser Bioprinting of Cells and Tumor Organoids for Organ-on-Chip Applications. Available online: https://spie.org/photonics-west/presentation/Laser-bioprinting-of-cells-and-tumor-organoids-for-organ-on/12411-12 (accessed on 7 April 2022).
- Zheng, Z.; Eglin, D.; Alini, M.; Richards, G.R.; Qin, L.; Lai, Y. Visible Light-Induced 3D Bioprinting Technologies and Corresponding Bioink Materials for Tissue Engineering: A Review. Engineering 2020, 7, 966–978. [Google Scholar] [CrossRef]
- Wang, Z.; Abdulla, R.; Parker, B.; Samanipour, R.; Ghosh, S.; Kim, K. A simple and high-resolution stereolithography-based 3D bioprinting system using visible light crosslinkable bioinks. Biofabrication 2015, 7, 045009. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lim, K.S.; Levato, R.; Costa, P.F.; Castilho, M.D.; Alcala-Orozco, C.R.; van Dorenmalen, A.K.M.; Melchels, F.P.W.; Gawlitta, D.; Hooper, G.J.; Malda, J.; et al. Bio-resin for high resolution lithography-based biofabrication of complex cell-laden constructs. Biofabrication 2018, 10, 034101. [Google Scholar] [CrossRef] [PubMed]
- Yeh, J.; Ling, Y.; Karp, J.M.; Gantz, J.; Chandawarkar, A.; Eng, G.; Iii, J.B.; Langer, R.; Khademhosseini, A. Micromolding of shape-controlled, harvestable cell-laden hydrogels. Biomaterials 2006, 27, 5391–5398. [Google Scholar] [CrossRef] [PubMed]
- Homan, K.A.; Kolesky, D.B.; Skylar-Scott, M.A.; Herrmann, J.; Obuobi, H.; Moisan, A.; Lewis, J.A. Bioprinting of 3D Convoluted Renal Proximal Tubules on Perfusable Chips. Sci. Rep. 2016, 6, 34845. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhou, X.; Hou, Y.; Lin, J. A review on the processing accuracy of two-photon polymerization. AIP Adv. 2015, 5, 030701. [Google Scholar] [CrossRef]
- Huang, X.; Zhang, Y.; Shi, M.; Zhang, L.-P.; Zhang, Y.; Zhao, Y. A highly biocompatible bio-ink for 3D hydrogel scaffolds fabrication in the presence of living cells by two-photon polymerization. Eur. Polym. J. 2021, 153, 110505. [Google Scholar] [CrossRef]
- Gehlen, J.; Qiu, W.; Schädli, G.N.; Müller, R.; Qin, X.-H. Tomographic volumetric bioprinting of heterocellular bone-like tissues in seconds. Acta Biomater. 2022, in press. [CrossRef]
- Madrid-Wolff, J.; Boniface, A.; Loterie, D.; Delrot, P.; Moser, C. Controlling Light in Scattering Materials for Volumetric Additive Manufacturing. Adv. Sci. 2022, 9, 2105144. [Google Scholar] [CrossRef]
- Bernal, P.N.; Bouwmeester, M.; Madrid-Wolff, J.; Falandt, M.; Florczak, S.; Rodriguez, N.G.; Li, Y.; Größbacher, G.; Samsom, R.; van Wolferen, M.; et al. Volumetric Bioprinting of Organoids and Optically Tuned Hydrogels to Build Liver-Like Metabolic Biofactories. Adv. Mater. 2022, 34, 2110054. [Google Scholar] [CrossRef]
- Kollep, M.; Konstantinou, G.; Madrid-Wolff, J.; Boniface, A.; Hagelüken, L.; Sasikumar, P.V.W.; Blugan, G.; Delrot, P.; Loterie, D.; Brugger, J.; et al. Tomographic Volumetric Additive Manufacturing of Silicon Oxycarbide Ceramics. Adv. Eng. Mater. 2022, 24, 2101345. [Google Scholar] [CrossRef]
- Liu, H.; Chansoria, P.; Delrot, P.; Angelidakis, E.; Rizzo, R.; Rütsche, D.; Applegate, L.A.; Loterie, D.; Zenobi-Wong, M. Filamented Light (FLight) Biofabrication of Highly Aligned Tissue-Engineered Constructs. Adv. Mater. 2022, 34, 2204301. [Google Scholar] [CrossRef] [PubMed]
- Ng, W.L.; Lee, J.M.; Yeong, W.Y.; Naing, M.W. Microvalve-based bioprinting—Process, bio-inks and applications. Biomater. Sci. 2017, 5, 632–647. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Drexler, H.G.; Uphoff, C.C. Mycoplasma Contamination of Cell Cultures: Incidence, Sources, Effects, Detection, Elimination, Prevention. Cytotechnology 2002, 39, 75–90. [Google Scholar] [CrossRef] [PubMed]
- Matsusaki, M.; Sakaue, K.; Kadowaki, K.; Akashi, M. Three-Dimensional Human Tissue Chips Fabricated by Rapid and Automatic Inkjet Cell Printing. Adv. Health Mater. 2012, 2, 534–539. [Google Scholar] [CrossRef] [PubMed]
- Roth, E.A.; Xu, T.; Das, M.; Gregory, C.; Hickman, J.J.; Boland, T. Inkjet printing for high-throughput cell patterning. Biomaterials 2004, 25, 3707–3715. [Google Scholar] [CrossRef]
- Bourget, J.-M.; Kérourédan, O.; Medina, M.; Rémy, M.; Thébaud, N.B.; Bareille, R.; Chassande, O.; Amédée, J.; Catros, S.; Devillard, R. Patterning of Endothelial Cells and Mesenchymal Stem Cells by Laser-Assisted Bioprinting to Study Cell Migration. BioMed. Res. Int. 2016, 2016, 3569843. [Google Scholar] [CrossRef] [Green Version]
- Ma, X.; Qu, X.; Zhu, W.; Li, Y.; Yuan, S.; Zhang, H.; Liu, J.; Wang, P.; Lai, C.S.E.; Zanella, F.; et al. Deterministically patterned biomimetic human iPSC-derived hepatic model via rapid 3D bioprinting. Proc. Natl. Acad. Sci. USA 2016, 113, 2206–2211. [Google Scholar] [CrossRef] [Green Version]
- Snyder, J.; Son, A.R.; Hamid, Q.; Sun, W. Fabrication of Microfluidic Manifold by Precision Extrusion Deposition and Replica Molding for Cell-Laden Device. J. Manuf. Sci. Eng. 2015, 138, 041007. [Google Scholar] [CrossRef]
- Yu, F.; Choudhury, D. Microfluidic bioprinting for organ-on-a-chip models. Drug Discov. Today 2019, 24, 1248–1257. [Google Scholar] [CrossRef]
- Mandt, D.; Gruber, P.; Markovic, M.; Tromayer, M.; Rothbauer, M.; Kratz, S.R.A.; Ali, F.; Van Hoorick, J.; Holnthoner, W.; Mühleder, S.; et al. Fabrication of placental barrier structures within a microfluidic device utilizing two-photon polymerization. Int. J. Bioprinting 2018, 4, 144. [Google Scholar] [CrossRef]
- Armingol, E.; Officer, A.; Harismendy, O.; Lewis, N.E. Deciphering cell–cell interactions and communication from gene expression. Nat. Rev. Genet. 2020, 22, 71–88. [Google Scholar] [CrossRef] [PubMed]
- Yamaguchi, S.; Ueno, A.; Akiyama, Y.; Morishima, K. Cell patterning through inkjet printing of one cell per droplet. Biofabrication 2012, 4, 045005. [Google Scholar] [CrossRef] [PubMed]
- Chansoria, P.; Shirwaiker, R. 3D bioprinting of anisotropic engineered tissue constructs with ultrasonically induced cell patterning. Addit. Manuf. 2020, 32, 101042. [Google Scholar] [CrossRef]
- Saunders, R.; Derby, B. Inkjet printing biomaterials for tissue engineering: Bioprinting. Int. Mater. Rev. 2014, 59, 430–448. [Google Scholar] [CrossRef]
- Campbell, P.G.; Weiss, E.L. Tissue engineering with the aid of inkjet printers. Expert Opin. Biol. Ther. 2007, 7, 1123–1127. [Google Scholar] [CrossRef] [PubMed]
- Fetah, K.; Tebon, P.; Goudie, M.J.; Eichenbaum, J.; Ren, L.; Barros, N.; Nasiri, R.; Ahadian, S.; Ashammakhi, N.; Dokmeci, M.R.; et al. The emergence of 3D bioprinting in organ-on-chip systems. Prog. Biomed. Eng. 2019, 1, 012001. [Google Scholar] [CrossRef]
- Ma, J.; Wang, Y.; Liu, J. Bioprinting of 3D tissues/organs combined with microfluidics. RSC Adv. 2018, 8, 21712–21727. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Park, J.Y.; Jang, J.; Kang, H.-W. 3D Bioprinting and its application to organ-on-a-chip. Microelectron. Eng. 2018, 200, 1–11. [Google Scholar] [CrossRef]
- Gold, K.; Gaharwar, A.K.; Jain, A. Emerging trends in multiscale modeling of vascular pathophysiology: Organ-on-a-chip and 3D printing. Biomaterials 2019, 196, 2–17. [Google Scholar] [CrossRef]
- Zhang, Y.S.; Davoudi, F.; Walch, P.; Manbachi, A.; Luo, X.; Dell’Erba, V.; Miri, A.K.; Albadawi, H.; Arneri, A.; Li, X.; et al. Bioprinted thrombosis-on-a-chip. Lab Chip 2016, 16, 4097–4105. [Google Scholar] [CrossRef]
- Abudupataer, M.; Chen, N.; Yan, S.; Alam, F.; Shi, Y.; Wang, L.; Lai, H.; Li, J.; Zhu, K.; Wang, C. Bioprinting a 3D vascular construct for engineering a vessel-on-a-chip. Biomed. Microdevices 2019, 22, 10. [Google Scholar] [CrossRef] [PubMed]
- Campos, D.F.D.; Lindsay, C.D.; Roth, J.; LeSavage, B.L.; Seymour, A.J.; Krajina, B.A.; Ribeiro, R.; Costa, P.F.; Blaeser, A.; Heilshorn, S.C. Bioprinting Cell- and Spheroid-Laden Protein-Engineered Hydrogels as Tissue-on-Chip Platforms. Front. Bioeng. Biotechnol. 2020, 8, 374. [Google Scholar] [CrossRef] [PubMed]
- Griep, L.M.; Wolbers, F.; De Wagenaar, B.; Ter Braak, P.M.; Weksler, B.B.; Romero, I.; Couraud, P.O.; Vermes, I.; van der Meer, A.; Berg, A.V.D. BBB ON CHIP: Microfluidic platform to mechanically and biochemically modulate blood-brain barrier function. Biomed. Microdevices 2012, 15, 145–150. [Google Scholar] [CrossRef] [PubMed]
- Van Der Helm, M.W.; van der Meer, A.; Eijkel, J.C.; van den Berg, A.; Segerink, L.I. Microfluidic organ-on-chip technology for blood-brain barrier research. Tissue Barriers 2016, 4, e1142493. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Deosarkar, S.P.; Prabhakarpandian, B.; Wang, B.; Sheffield, J.B.; Krynska, B.; Kiani, M.F. A Novel Dynamic Neonatal Blood-Brain Barrier on a Chip. PLoS ONE 2015, 10, e0142725. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tang, M.; Rich, J.N.; Chen, S. Biomaterials and 3D Bioprinting Strategies to Model Glioblastoma and the Blood–Brain Barrier. Adv. Mater. 2020, 33, e2004776. [Google Scholar] [CrossRef]
- Yi, H.-G.; Jeong, Y.H.; Kim, Y.; Choi, Y.-J.; Moon, H.E.; Park, S.H.; Kang, K.S.; Bae, M.; Jang, J.; Youn, H.; et al. A bioprinted human-glioblastoma-on-a-chip for the identification of patient-specific responses to chemoradiotherapy. Nat. Biomed. Eng. 2019, 3, 509–519. [Google Scholar] [CrossRef]
- Jung, J.W.; Lee, J.-S.; Cho, D.-W. Computer-aided multiple-head 3D printing system for printing of heterogeneous organ/tissue constructs. Sci. Rep. 2016, 6, 21685. [Google Scholar] [CrossRef] [Green Version]
- Silvani, G.; Basirun, C.; Wu, H.; Mehner, C.; Poole, K.; Bradbury, P.; Chou, J. A 3D-Bioprinted Vascularized Glioblastoma-on-a-Chip for Studying the Impact of Simulated Microgravity as a Novel Pre-Clinical Approach in Brain Tumor Therapy. Adv. Ther. 2021, 4, 2100106. [Google Scholar] [CrossRef]
- Ashammakhi, N.; Nasiri, R.; de Barros, N.R.; Tebon, P.; Thakor, J.; Goudie, M.; Shamloo, A.; Martin, M.G.; Khademhosseini, A. Gut-on-a-chip: Current progress and future opportunities. Biomaterials 2020, 255, 120196. [Google Scholar] [CrossRef]
- van Breukelen, G.E.; García Díaz, M.; Torras Andrés Tutor, N.; Martínez, E.F. Bioprinted Gut-on-a-Chip to Mimic the Small Intestinal Mucosa. Bachelor’s Thesis, Project Biomedical Engineernig Degree. University Barcelona, Barcelona, Spain, 14 June 2021. [Google Scholar]
- Zhang, Y.S.; Arneri, A.; Bersini, S.; Shin, S.-R.; Zhu, K.; Goli-Malekabadi, Z.; Aleman, J.; Colosi, C.; Busignani, F.; Dell’Erba, V.; et al. Bioprinting 3D microfibrous scaffolds for engineering endothelialized myocardium and heart-on-a-chip. Biomaterials 2016, 110, 45–59. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Heydari, Z.; Pooyan, P.; Bikmulina, P.; Pozdnyakov, A.; Fomin, V.; Seydi, H.; Shpichka, A.; Timashev, P.; Vosough, M. Mimicking the liver function in micro-patterned units: Challenges and perspectives in 3D bioprinting. Bioprinting 2022, 27, e00208. [Google Scholar] [CrossRef]
- Dabbagh, S.R.; Ozdalgic, B.; Mustafaoglu, N.; Tasoglu, S. Three-Dimensional-Bioprinted Liver Chips and Challenges. Appl. Sci. 2022, 12, 5029. [Google Scholar] [CrossRef]
- Chang, R.; Nam, J.; Sun, W. Direct Cell Writing of 3D Microorgan for In Vitro Pharmacokinetic Model. Tissue Eng. Part C Methods 2008, 14, 157–166. [Google Scholar] [CrossRef] [PubMed]
- Snyder, E.J.; Hamid, Q.; Wang, C.; Chang, R.; Emami, K.; Wu, H.; Sun, W. Bioprinting cell-laden matrigel for radioprotection study of liver by pro-drug conversion in a dual-tissue microfluidic chip. Biofabrication 2011, 3, 034112. [Google Scholar] [CrossRef] [Green Version]
- Bhise, N.S.; Manoharan, V.; Massa, S.; Tamayol, A.; Ghaderi, M.; Miscuglio, M.; Lang, Q.; Zhang, Y.S.; Shin, S.R.; Calzone, G.; et al. A liver-on-a-chip platform with bioprinted hepatic spheroids. Biofabrication 2016, 8, 014101. [Google Scholar] [CrossRef] [Green Version]
- Zhang, J.; Chen, F.; He, Z.; Ma, Y.; Uchiyama, K.; Lin, J.-M. A novel approach for precisely controlled multiple cell patterning in microfluidic chips by inkjet printing and the detection of drug metabolism and diffusion. Analyst 2016, 141, 2940–2947. [Google Scholar] [CrossRef]
- Lee, H.; Cho, D.-W. One-step fabrication of an organ-on-a-chip with spatial heterogeneity using a 3D bioprinting technology. Lab Chip 2016, 16, 2618–2625. [Google Scholar] [CrossRef] [Green Version]
- Lee, H.; Chae, S.; Kim, J.Y.; Han, W.; Kim, J.; Choi, Y.-J.; Cho, D.-W. Cell-printed 3D liver-on-a-chip possessing a liver microenvironment and biliary system. Biofabrication 2018, 11, 025001. [Google Scholar] [CrossRef]
- Amin, M.; Scott, C.; Brunckhorst, O.; Ahmed, K. MP38-03 Effects Of Haematological Malignancy Treatment To Fertility In Young Males: A Systematic Review Mp38-04 Bioprinted Ovary-on-a-Chip Platform as a Model of Ovarian Physiology And Disease. J. Urol. 2020, 203 (Suppl. S4), e570. [Google Scholar]
- Pi, Q.; Maharjan, S.; Yan, X.; Liu, X.; Singh, B.; Van Genderen, A.M.; Robledo-Padilla, F.; Parra, R.; Hu, N.; Jia, W.; et al. Digitally Tunable Microfluidic Bioprinting of Multilayered Cannular Tissues. Adv. Mater. 2018, 30, e1706913. [Google Scholar] [CrossRef] [PubMed]
- Knowlton, S.; Joshi, A.; Yenilmez, B.; Ozbolat, I.T.; Chua, C.K.; Khademhosseini, A.; Tasoglu, S. Advancing cancer research using bioprinting for tumor-on-a-chip platforms. Int. J. Bioprinting 2016, 2, 77. [Google Scholar] [CrossRef] [Green Version]
- Radhakrishnan, J.; Varadaraj, S.; Dash, S.K.; Sharma, A.; Verma, R.S. Organotypic cancer tissue models for drug screening: 3D constructs, bioprinting and microfluidic chips. Drug Discov. Today 2020, 25, 879–890. [Google Scholar] [CrossRef] [PubMed]
- Samadian, H.; Jafari, S.; Sepand, M.; Alaei, L.; Malvajerd, S.S.; Jaymand, M.; Ghobadinezhad, F.; Jahanshahi, F.; Hamblin, M.; Derakhshankhah, H.; et al. 3D bioprinting technology to mimic the tumor microenvironment: Tumor-on-a-chip concept. Mater. Today Adv. 2021, 12, 100160. [Google Scholar] [CrossRef]
- Fang, L.; Liu, Y.; Qiu, J.; Wan, W. Bioprinting and its Use in Tumor-On-A-Chip Technology for Cancer Drug Screening: A Review. Int. J. Bioprinting 2022, 8, 603. [Google Scholar] [CrossRef] [PubMed]
- Hamid, Q.; Wang, C.; Snyder, J.; Williams, S.; Liu, Y.; Sun, W. Maskless fabrication of cell-laden microfluidic chips with localized surface functionalization for the co-culture of cancer cells. Biofabrication 2015, 7, 015012. [Google Scholar] [CrossRef] [PubMed]
- Cao, X.; Ashfaq, R.; Cheng, F.; Maharjan, S.; Li, J.; Ying, G.; Hassan, S.; Xiao, H.; Yue, K.; Zhang, Y.S. A Tumor-on-a-Chip System with Bioprinted Blood and Lymphatic Vessel Pair. Adv. Funct. Mater. 2019, 29, 1807173. [Google Scholar] [CrossRef]
- Xie, M.; Gao, Q.; Fu, J.; Chen, Z.; He, Y. Bioprinting of novel 3D tumor array chip for drug screening. Bio-Design Manuf. 2020, 3, 175–188. [Google Scholar] [CrossRef]



Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chliara, M.A.; Elezoglou, S.; Zergioti, I. Bioprinting on Organ-on-Chip: Development and Applications. Biosensors 2022, 12, 1135. https://doi.org/10.3390/bios12121135
Chliara MA, Elezoglou S, Zergioti I. Bioprinting on Organ-on-Chip: Development and Applications. Biosensors. 2022; 12(12):1135. https://doi.org/10.3390/bios12121135
Chicago/Turabian StyleChliara, Maria Anna, Stavroula Elezoglou, and Ioanna Zergioti. 2022. "Bioprinting on Organ-on-Chip: Development and Applications" Biosensors 12, no. 12: 1135. https://doi.org/10.3390/bios12121135
APA StyleChliara, M. A., Elezoglou, S., & Zergioti, I. (2022). Bioprinting on Organ-on-Chip: Development and Applications. Biosensors, 12(12), 1135. https://doi.org/10.3390/bios12121135







