Graphene Scaffolds: A Striking Approach to Combat Dermatophytosis
Abstract
1. Introduction
2. Materials and Methods
2.1. Materials
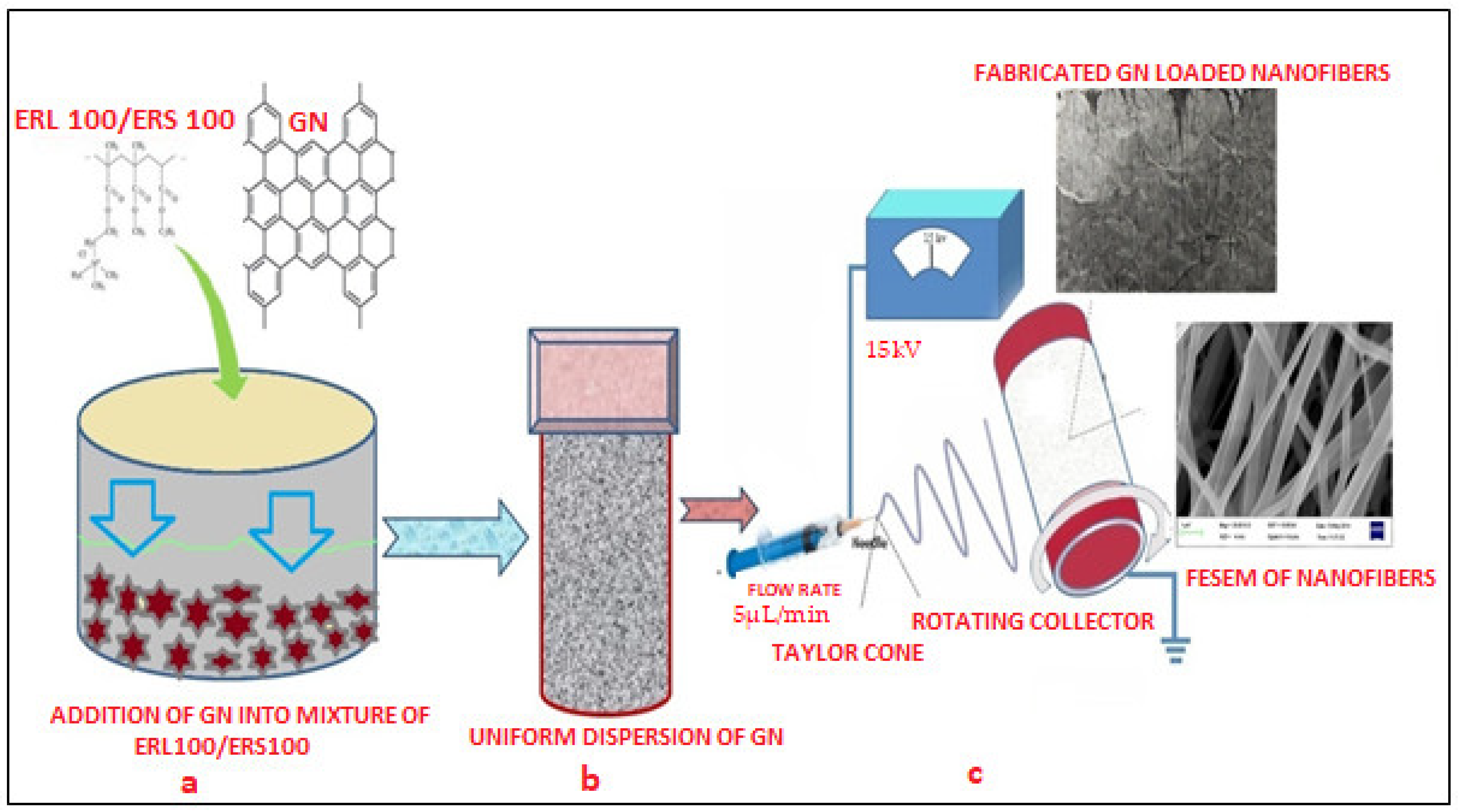
2.2. Fabrication of GN-Loaded Scaffolds
2.3. Characterizations
2.4. Surface Morphology
2.5. In Vitro Antifungal Assay
2.6. In Vivo Study
2.7. Stability Study
3. Results
3.1. Fabrication of GN-Loaded Scaffolds
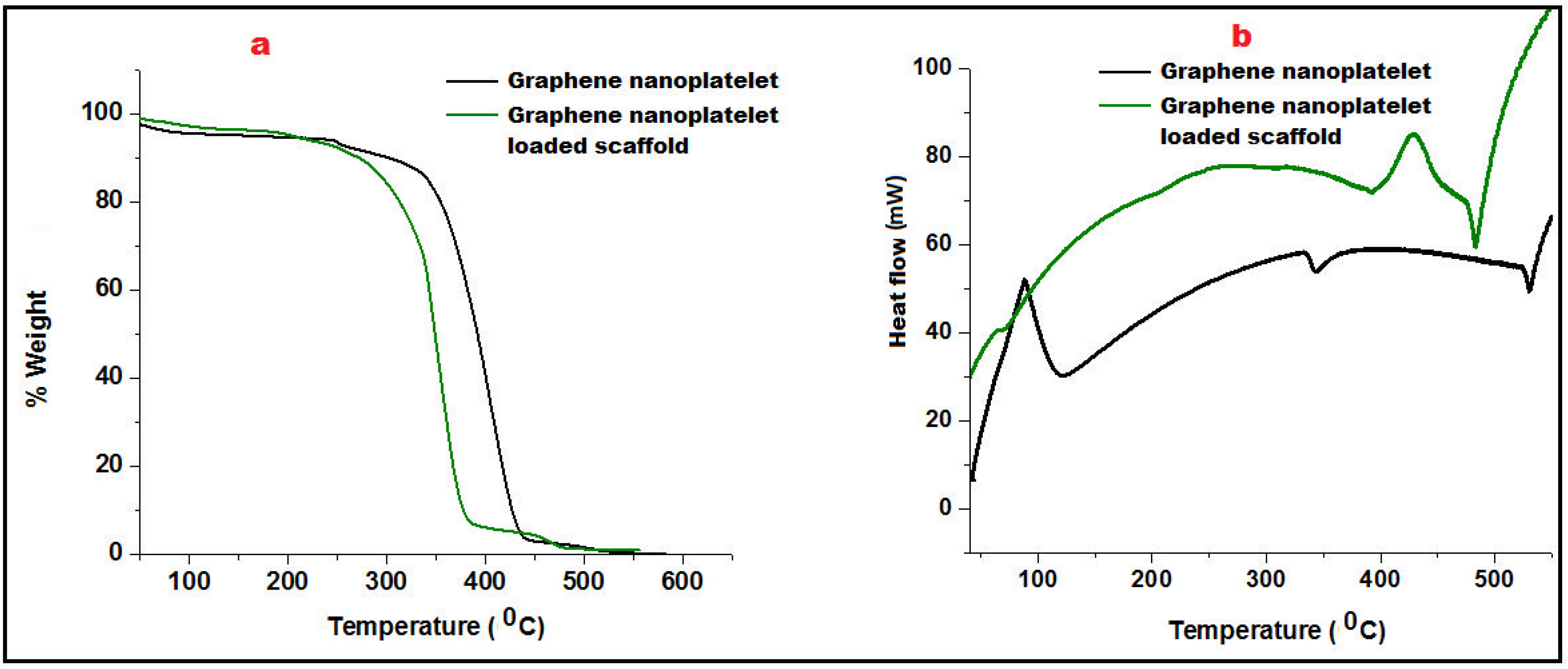
3.2. Characterization
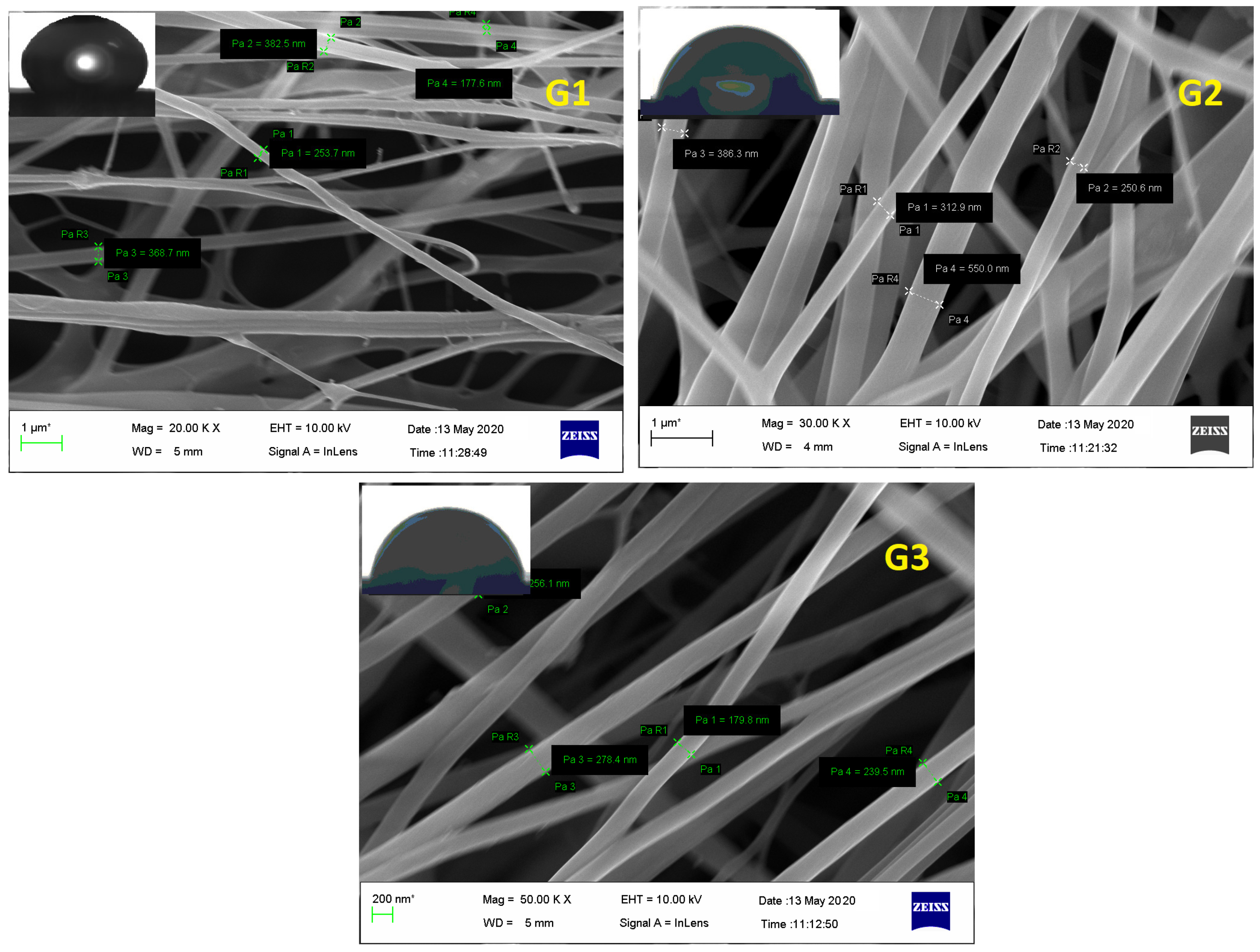
3.3. Surface Morphology
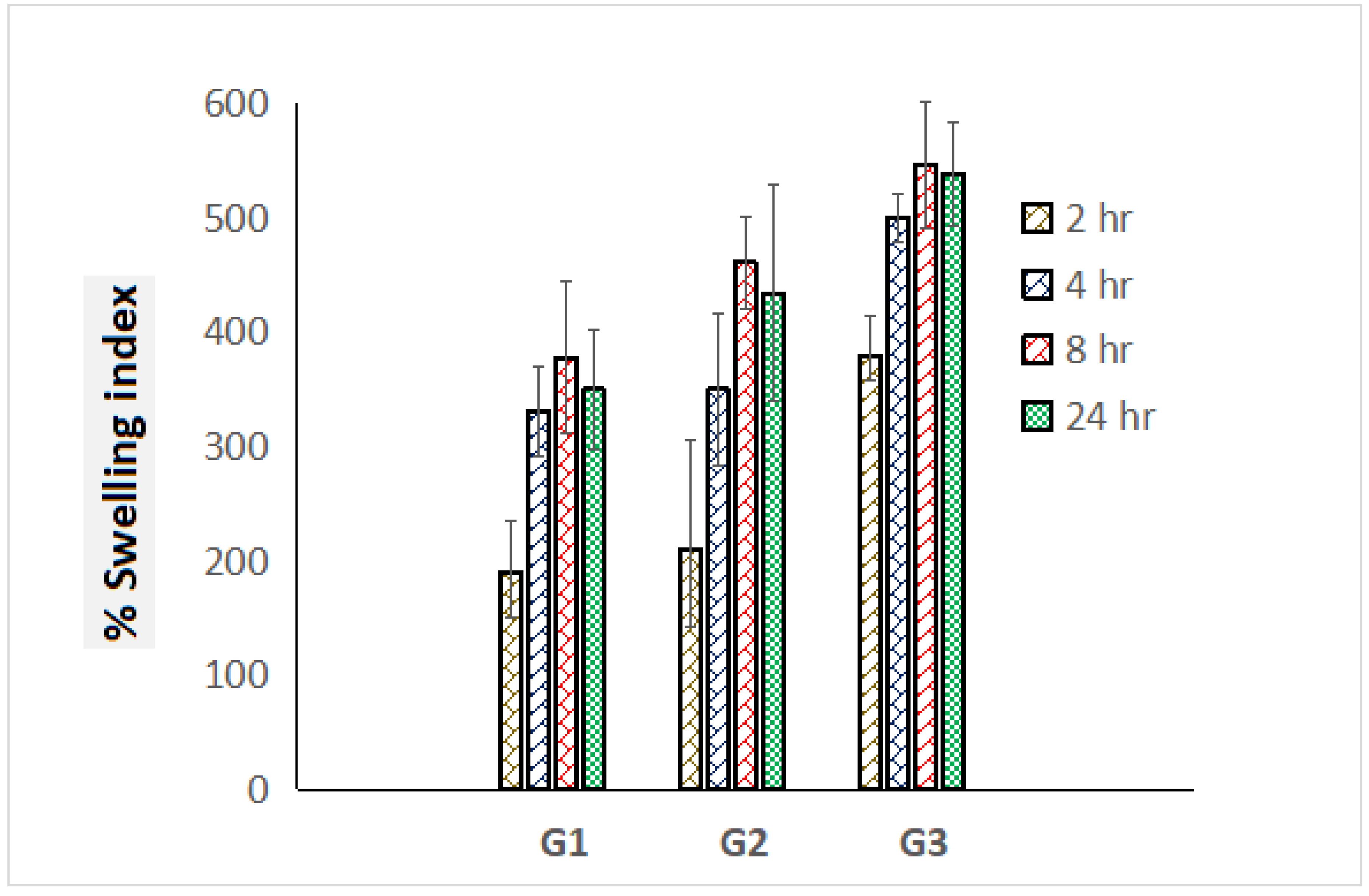
3.4. Swelling Index
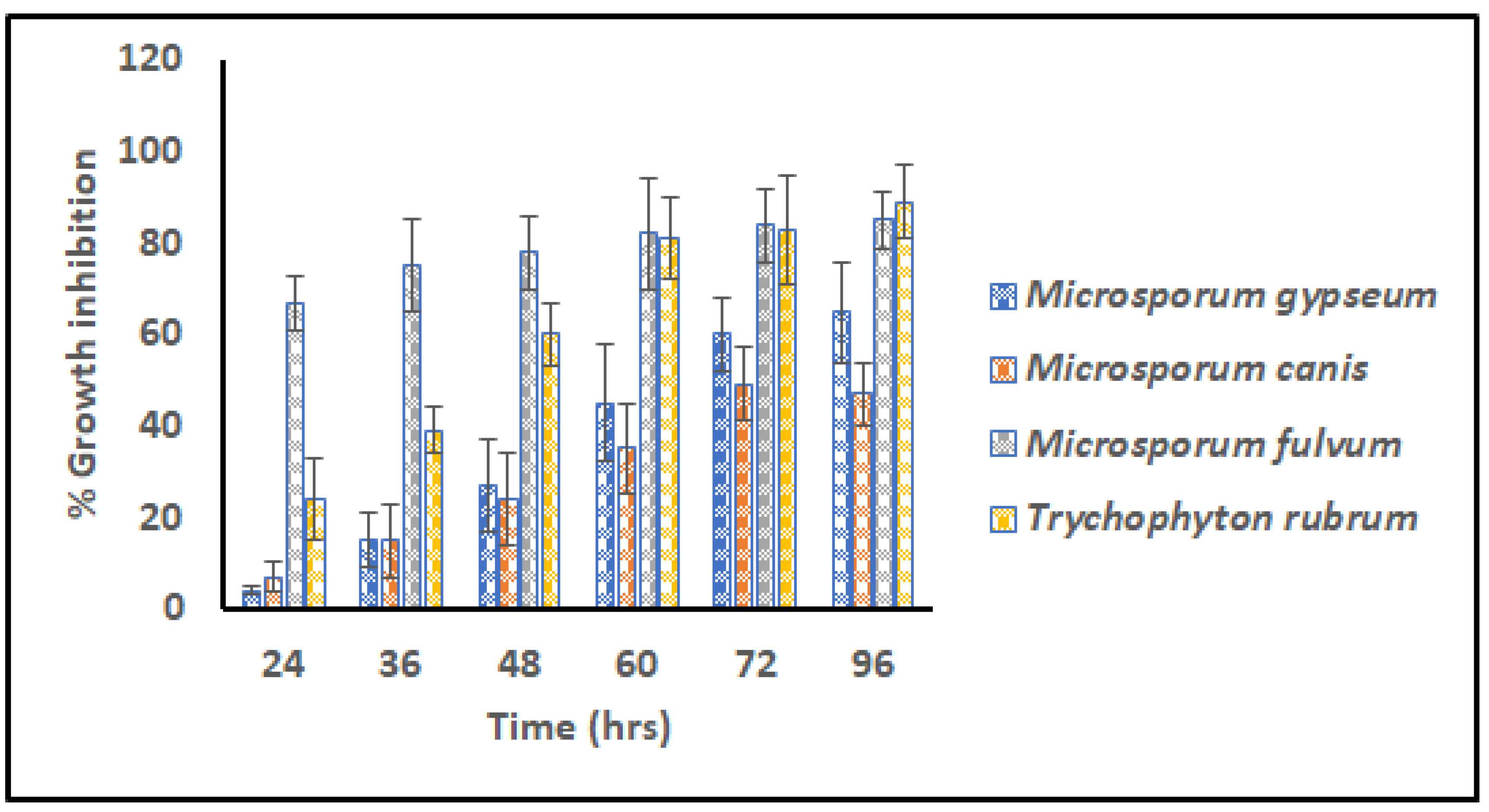
3.5. Microdilution Assay
3.6. Stability Study
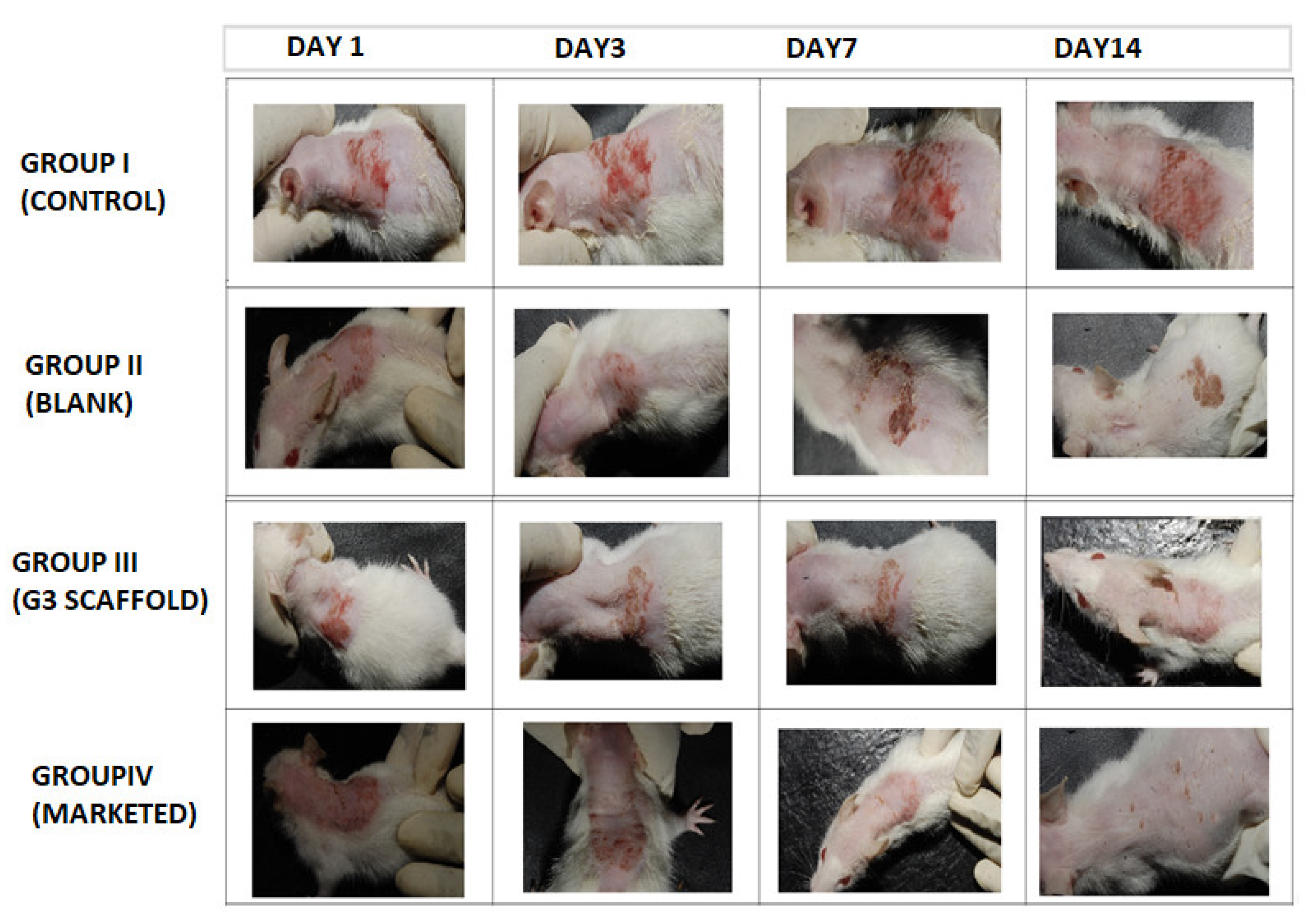
3.7. In Vivo Study
4. Discussion
5. Conclusions
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cataldi, P.; Athanassiou, A.; Bayer, I.S. Graphene Nanoplatelets-Based Advanced Materials and Recent Progress in Sustainable Applications. Appl. Sci. 2018, 8, 1438. [Google Scholar] [CrossRef]
- Kausar, A.; Ahmad, I.; Zhao, T.; Aldaghri, O.; Eisa, M.H. Graphene in Polymeric Nanocomposite Membranes—Current State and Progress. Processes 2023, 11, 927. [Google Scholar] [CrossRef]
- Kim, J.M.; Kim, J.; Kim, J. Covalent Decoration of Graphene Oxide with Dendrimer-Encapsulated Nanoparticles for Universal Attachment of Multiple Nanoparticles on Chemically Converted Graphene. Chem. Commun. 2012, 48, 9233–9235. [Google Scholar] [CrossRef] [PubMed]
- Geim, A.K.; Novoselov, K.S. The Rise of Graphene. Nat. Mater. 2007, 6, 183–191. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Sun, G.; Routh, P.; Kim, D.H.; Huang, W.; Chen, P. Heteroatom-Doped Graphene Materials: Syntheses, Properties and Applications. Chem. Soc. Rev. 2014, 43, 7067–7098. [Google Scholar] [CrossRef] [PubMed]
- Tatarskiy, V.V.; Zakharova, O.V.; Baranchikov, P.A.; Muratov, D.S.; Kuznetsov, D.V.; Gusev, A.A. Graphene Oxide Nanosurface Reduces Apoptotic Death of HCT116 Colon Carcinoma Cells Induced by Zirconium Trisulfide Nanoribbons. Int. J. Mol. Sci. 2023, 24, 2783. [Google Scholar] [CrossRef]
- Qin, Z.; Taylor, M.; Hwang, M.; Bertoldi, K.; Buehler, M.J. Effect of Wrinkles on the Surface Area of Graphene: Toward the Design of Nanoelectronics. Nano Lett. 2014, 14, 6520–6525. [Google Scholar] [CrossRef] [PubMed]
- Drieschner, S.; Weber, M.; Wohlketzetter, J.; Vieten, J.; Makrygiannis, E.; Blaschke, B.M.; Morandi, V.; Colombo, L.; Bonaccorso, F.; Garrido, J.A. High Surface Area Graphene Foams by Chemical Vapor Deposition. 2D Mater. 2016, 3, 45013. [Google Scholar] [CrossRef]
- Cherian, R.S. Graphene: A Multifaceted Nanomaterial for Cutting Edge Biomedical Application. Int. J. Med. Nano Res. 2014, 1, 3. [Google Scholar] [CrossRef]
- Snitka, V. Graphene Based Materials: Opportunities and Challenges in Nanomedicine. J. Nanomed. Res. 2015, 2, 103–104. [Google Scholar] [CrossRef]
- McCallion, C.; Burthem, J.; Rees-Unwin, K.; Golovanov, A.; Pluen, A. Graphene in Therapeutics Delivery: Problems, Solutions and Future Opportunities. Eur. J. Pharm. Biopharm. 2016, 104, 235–250. [Google Scholar] [CrossRef] [PubMed]
- Mohan, H.; Fagan, A.; Giordani, S. Carbon Nanomaterials (CNMs) in Cancer Therapy: A Database of CNM-Based Nanocarrier Systems. Pharmaceutics 2023, 15, 1545. [Google Scholar] [CrossRef] [PubMed]
- Al-Thani, R.F.; Patan, N.K.; Al-Maadeed, M.A. Raphene Oxide as Antimicrobial Against Two Gram-Positive And Two Gram-Negative Bacteria In Addition To One Fungus. Online J. Biol. Sci. 2014, 14, 230–239. [Google Scholar] [CrossRef]
- Liu, S.; Zeng, T.H.; Hofmann, M.; Burcombe, E.; Wei, J.; Jiang, R.; Kong, J.; Chen, Y. Antibacterial Activity of Graphite, Graphite Oxide, Graphene Oxide, and Reduced Graphene Oxide: Membrane and Oxidative Stress. ACS Nano 2011, 5, 6971–6980. [Google Scholar] [CrossRef] [PubMed]
- Mookherjee, N.; Anderson, M.A.; Haagsman, H.P.; Davidson, D.J. Antimicrobial Host Defence Peptides: Functions and Clinical Potential. Nat. Rev. Drug Discov. 2020, 19, 311–332. [Google Scholar] [CrossRef] [PubMed]
- Marsella, R. Dermatophytosis, 2nd ed.; Elsevier Inc.: Amsterdam, The Netherlands, 2013; ISBN 9781455708918. [Google Scholar]
- Sharma, V.; Kumawat, T.K.; Sharma, A.; Seth, R.; Chandra, S. Distribution and Prevalence of Dermatophytes in Semi-Arid Region of India. Adv. Microbiol. 2015, 5, 93–106. [Google Scholar] [CrossRef]
- Lakshmipathy, D.T.; Kannabiran, K. Review on Dermatomycosis: Pathogenesis and Treatment. Nat. Sci. 2010, 02, 726–731. [Google Scholar] [CrossRef]
- Araújo, C.R.; Miranda, K.C.; Fernandes, O.d.F.L.; Soares, A.J.; Silva, M.d.R.R. In Vitro Susceptibility Testing of Dermatophytes Isolated in Goiania, Brazil, against Five Antifungal Agents by Broth Microdilution Method. Rev. Inst. Med. Trop. Sao Paulo 2009, 51, 9–12. [Google Scholar] [CrossRef]
- Martinez-Rossi, N.M.; Persinoti, G.F.; Peres, N.T.A.; Rossi, A. Role of PH in the Pathogenesis of Dermatophytoses. Mycoses 2012, 55, 381–387. [Google Scholar] [CrossRef]
- Majeed, N.; Narayanankutty, S.; Rajan, R.; Theodore, R. Clinicomycological Study of Dermatophytosis in a Tertiary Care Centre YR—2016/7/1. J. Acad. Clin. Microbiol. 2016, 8, 110–113. [Google Scholar] [CrossRef]
- De Aguiar Peres, N.T.; Maranhão, F.C.A.; Rossi, A.; Martinez-Rossi, N.M. Dermatophytes: Host-Pathogen Interaction and Antifungal Resistance. An. Bras. Dermatol. 2010, 85, 657–667. [Google Scholar] [CrossRef]
- Dhivya, S.; Padma, V.V.; Santhini, E. Wound Dressings—A Review. BioMedicine 2015, 5, 22. [Google Scholar] [CrossRef] [PubMed]
- Sill, T.J.; von Recum, H.A. Electrospinning: Applications in Drug Delivery and Tissue Engineering. Biomaterials 2008, 29, 1989–2006. [Google Scholar] [CrossRef]
- McIvor, M.J.; Ó Maolmhuaidh, F.; Meenagh, A.; Hussain, S.; Bhattacharya, G.; Fishlock, S.; Ward, J.; McFerran, A.; Acheson, J.G.; Cahill, P.A.; et al. 3D Fabrication and Characterisation of Electrically Receptive PCL-Graphene Scaffolds for Bioengineered In Vitro Tissue Models. Materials 2022, 15, 9030. [Google Scholar] [CrossRef] [PubMed]
- Reda, R.I.; Wen, M.M.; El-Kamel, A.H. Ketoprofen-Loaded Eudragit Electrospun Nanofibers for the Treatment of Oral Mucositis. Int. J. Nanomed. 2017, 12, 2335–2351. [Google Scholar] [CrossRef]
- Lin, J.; Li, C.; Zhao, Y.; Hu, J.; Zhang, L.-M. Co-Electrospun Nanofibrous Membranes of Collagen and Zein for Wound Healing. ACS Appl. Mater. Interfaces 2012, 4, 1050–1057. [Google Scholar] [CrossRef]
- Bucolo, C.; Maltese, A.; Puglisi, G.; Pignatello, R. Enhanced Ocular Anti-Inflammatory Activity of Ibuprofen Carried by an Eudragit RS100 Nanoparticle Suspension. Ophthalmic Res. 2002, 34, 319–323. [Google Scholar] [CrossRef] [PubMed]
- Pendekal, M.S.; Tegginamat, P.K. Formulation and Evaluation of a Bioadhesive Patch for Buccal Delivery of Tizanidine. Acta Pharm. Sin. B 2012, 2, 318–324. [Google Scholar] [CrossRef]
- Pignatello, R.; Bucolo, C.; Ferrara, P.; Maltese, A.; Puleo, A.; Puglisi, G. Eudragit RS100 Nanosuspensions for the Ophthalmic Controlled Delivery of Ibuprofen. Eur. J. Pharm. Sci. 2002, 16, 53–61. [Google Scholar] [CrossRef]
- Huang, Z.-M.; Zhang, Y.Z.; Ramakrishna, S.; Lim, C.T. Electrospinning and Mechanical Characterization of Gelatin Nanofibers. Polymer 2004, 45, 5361–5368. [Google Scholar] [CrossRef]
- Tan, E.P.S.; Lim, C.T. Mechanical Characterization of Nanofibers—A Review. Compos. Sci. Technol. 2006, 66, 1102–1111. [Google Scholar] [CrossRef]
- Kchaou, M.; Alquraish, M.; Abuhasel, K.; Abdullah, A.; Ali, A.A. Electrospun Nanofibrous Scaffolds: Review of Current Progress in the Properties and Manufacturing Process, and Possible Applications for COVID-19. Polymers 2021, 13, 916. [Google Scholar] [CrossRef] [PubMed]
- Sharma, N.; Misra, S. Smart Gn-Keto Nanohybrid Embedded Topical System for Effective Management of Dermatophytosis. Drug Deliv. Lett. 2019, 9, 21–28. [Google Scholar] [CrossRef]
- Misra, S.K.; Pandey, H.; Patil, S.; Ramteke, P.W.; Pandey, A.C. Tolnaftate-Loaded PolyacrylateElectrospun Nanofibers for an Impressive Regimen on Dermatophytosis. Fibers 2017, 5, 41. [Google Scholar] [CrossRef]
- Misra, S.K.; Ramteke, P.W.; Patil, S.; Pandey, A.C.; Pandey, H. Tolnaftate–Graphene Composite-Loaded Nanoengineered Electrospun Scaffolds as Efficient Therapeutic Dressing Material for Regimen of Dermatomycosis. Appl. Nanosci. 2018, 8, 1629–1640. [Google Scholar] [CrossRef]
- Sahni, K.; Singh, S.; Dogra, S. Newer Topical Treatments in Skin and Nail Dermatophyte Infections. Indian Dermatol. Online J. 2018, 9, 149–158. [Google Scholar] [PubMed]
- Elzatahry, A.A.; Al-Enizi, A.M.; Elsayed, E.A.; Butorac, R.R.; Al-Deyab, S.S.; Wadaan, M.A.M.; Cowley, A.H. Nanofiber Composites Containing N-Heterocyclic Carbene Complexes with Antimicrobial Activity. Int. J. Nanomed. 2012, 7, 2829–2832. [Google Scholar] [CrossRef]
- Heunis, T.D.J.; Smith, C.; Dicks, L.M.T. Evaluation of a Nisin-Eluting Nanofiber Scaffold to Treat Staphylococcus Aureus-Induced Skin Infections in Mice. Antimicrob. Agents Chemother. 2013, 57, 3928–3935. [Google Scholar] [CrossRef]
- Tomar, Y.; Pandit, N.; Priya, S.; Singhvi, G. Evolving Trends in Nanofibers for Topical Delivery of Therapeutics in Skin Disorders. ACS Omega 2023, 8, 18340–18357. [Google Scholar] [CrossRef]
- Lammel, T.; Navas, J.M. Graphene nanoplatelets spontaneously translocate into the cytosol and physically interact with cellular organelles in the fish cell line PLHC-1. Aquat. Toxicol. 2014, 150, 55–65. [Google Scholar] [CrossRef]
- Zhang, B.; Wei, P.; Zhou, Z.; Wei, T. Interactions of graphene with mammalian cells: Molecular mechanisms and biomedical insights. Adv. Drug Deliv. Rev. 2016, 105 Pt B, 145–162. [Google Scholar] [CrossRef]


| Parameters | Diameter of Nanofiber | Contact Angle | Percentage Swelling Index | In Vitro Antifungal Responses | |||
|---|---|---|---|---|---|---|---|
| G3 Nanofiber (nm) | G3 Nanofibers | % | M. gypseum | M. fulvum | M. canis | T. rubrum | |
| 0 month | 280 ± 90 nm | 48.8 ± 2.8° | 646 ± 23% | 65.888 ± 11.45% | 85.004 ± 6.34% | 47.017 ± 7.03% | 89.703 ± 8.06% |
| 3 months | 423 ± 60 nm | 67.5 ± 4.2° | 426 ± 19% | 60. 564 ± 8.88% | 81.002 ± 12.34% | 43.419 ± 7.67% | 86.453 ± 9.54% |
| Score | Magnitude of Lesion |
|---|---|
| 0 | Absence of lesion |
| 1 | Appearance of erythema at infection site |
| 2 | Moderate erythema and spread |
| 3 | Erythema, abrasion and scaling |
| 4 | Severe erythema with lesion and scars |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Misra, S.K.; Pandey, H.; Patil, S.; Virmani, T.; Virmani, R.; Kumar, G.; Alhalmi, A.; Noman, O.M.; Alshahrani, S.S.; Mothana, R.A. Graphene Scaffolds: A Striking Approach to Combat Dermatophytosis. Nanomaterials 2023, 13, 2305. https://doi.org/10.3390/nano13162305
Misra SK, Pandey H, Patil S, Virmani T, Virmani R, Kumar G, Alhalmi A, Noman OM, Alshahrani SS, Mothana RA. Graphene Scaffolds: A Striking Approach to Combat Dermatophytosis. Nanomaterials. 2023; 13(16):2305. https://doi.org/10.3390/nano13162305
Chicago/Turabian StyleMisra, Shashi Kiran, Himanshu Pandey, Sandip Patil, Tarun Virmani, Reshu Virmani, Girish Kumar, Abdulsalam Alhalmi, Omar M. Noman, Saad S. Alshahrani, and Ramzi A. Mothana. 2023. "Graphene Scaffolds: A Striking Approach to Combat Dermatophytosis" Nanomaterials 13, no. 16: 2305. https://doi.org/10.3390/nano13162305
APA StyleMisra, S. K., Pandey, H., Patil, S., Virmani, T., Virmani, R., Kumar, G., Alhalmi, A., Noman, O. M., Alshahrani, S. S., & Mothana, R. A. (2023). Graphene Scaffolds: A Striking Approach to Combat Dermatophytosis. Nanomaterials, 13(16), 2305. https://doi.org/10.3390/nano13162305









