Melanin and Melanin-Like Hybrid Materials in Regenerative Medicine
Abstract
1. Introduction
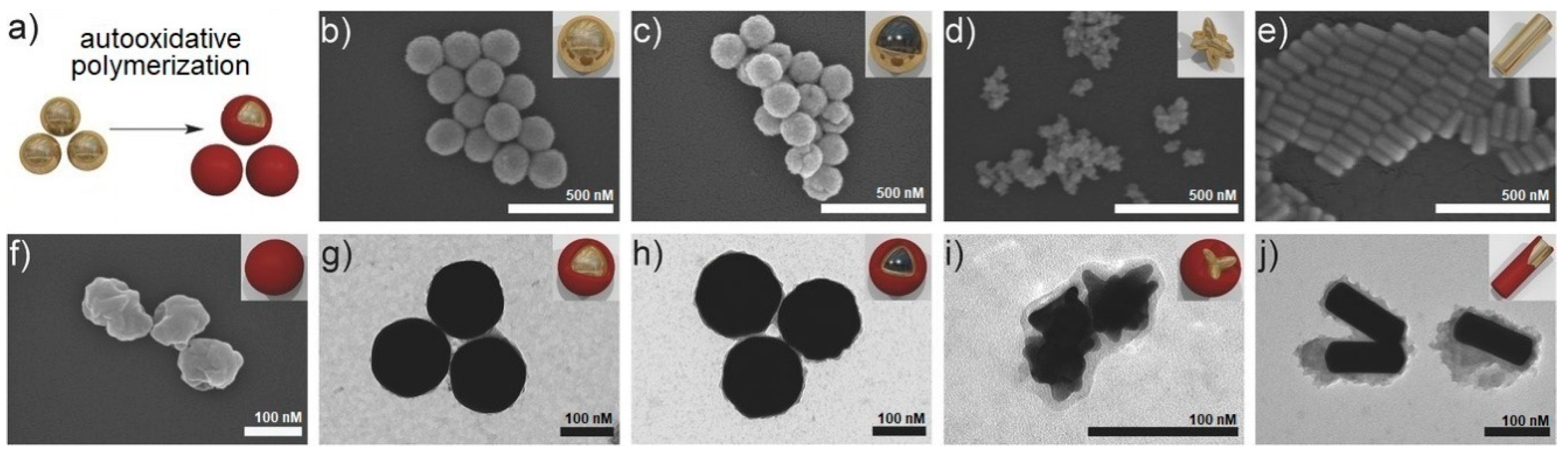
2. Synthetic Melanin-Like Materials: Opportunities and Issues of Biomimetic Approaches
2.1. From Physicochemical to Biomedical Properties of Melanins and Melanin-Like Hybrid Materials
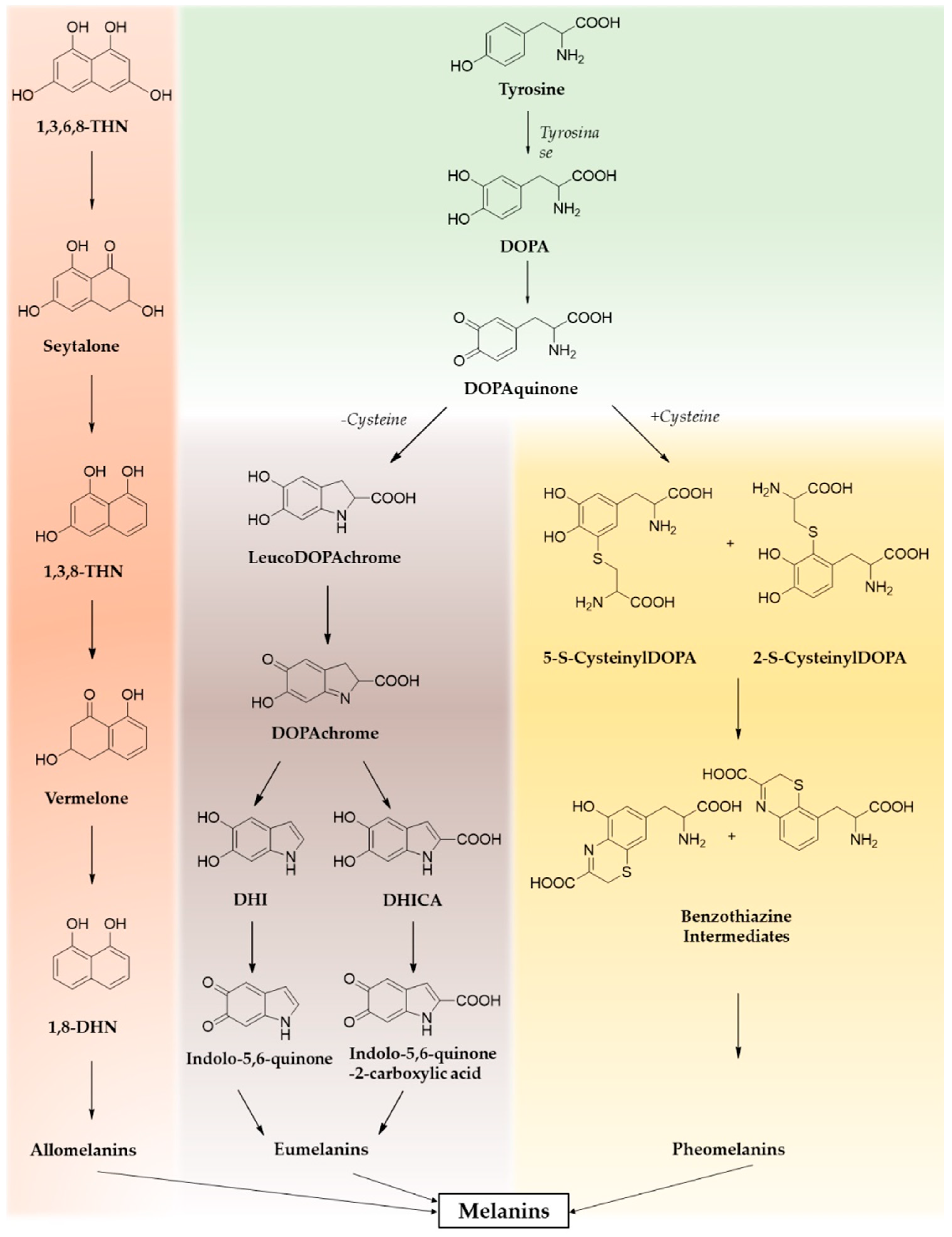
2.1.1. Versatile Chemistry and Easy Chemical Coupling
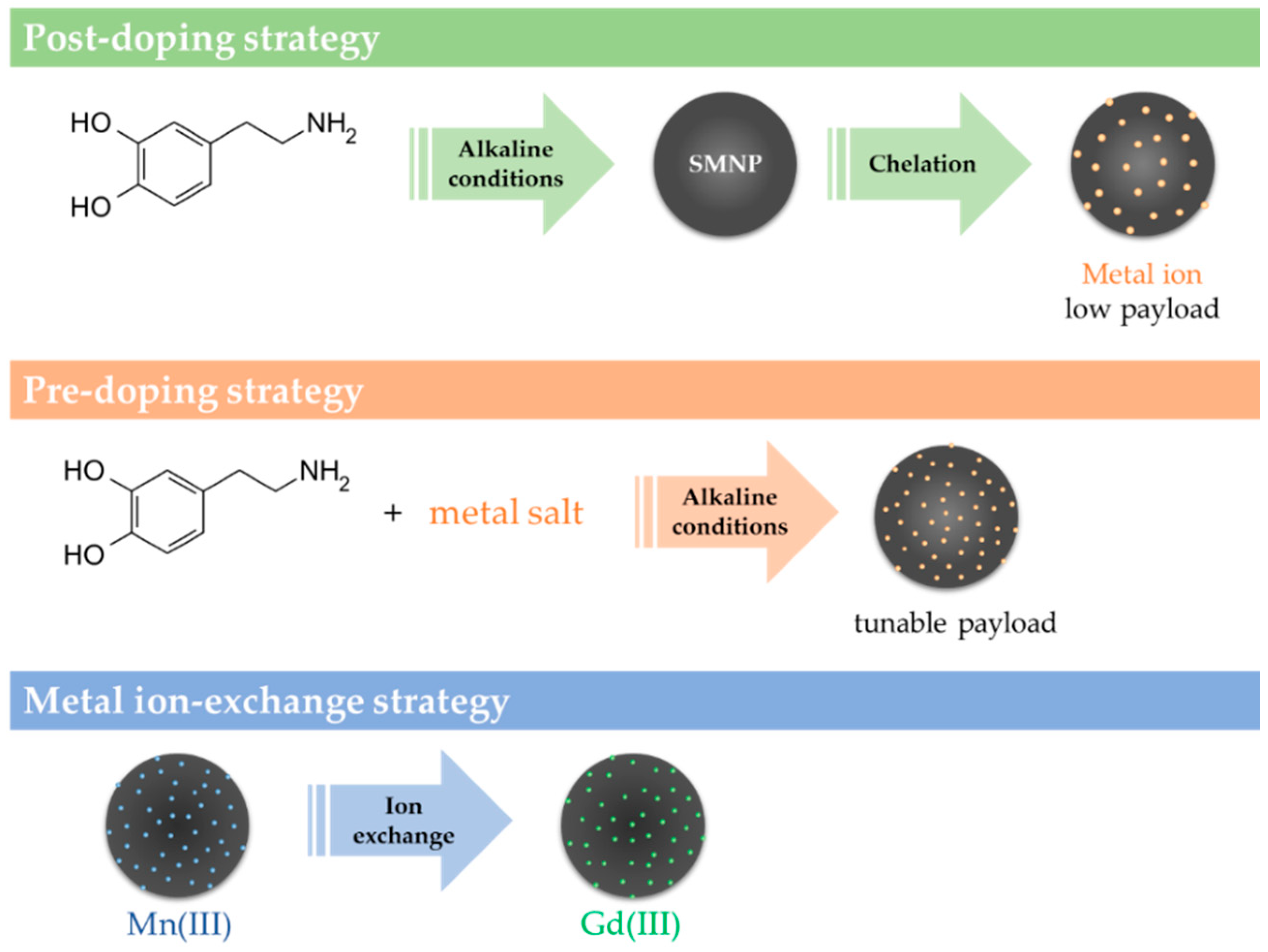
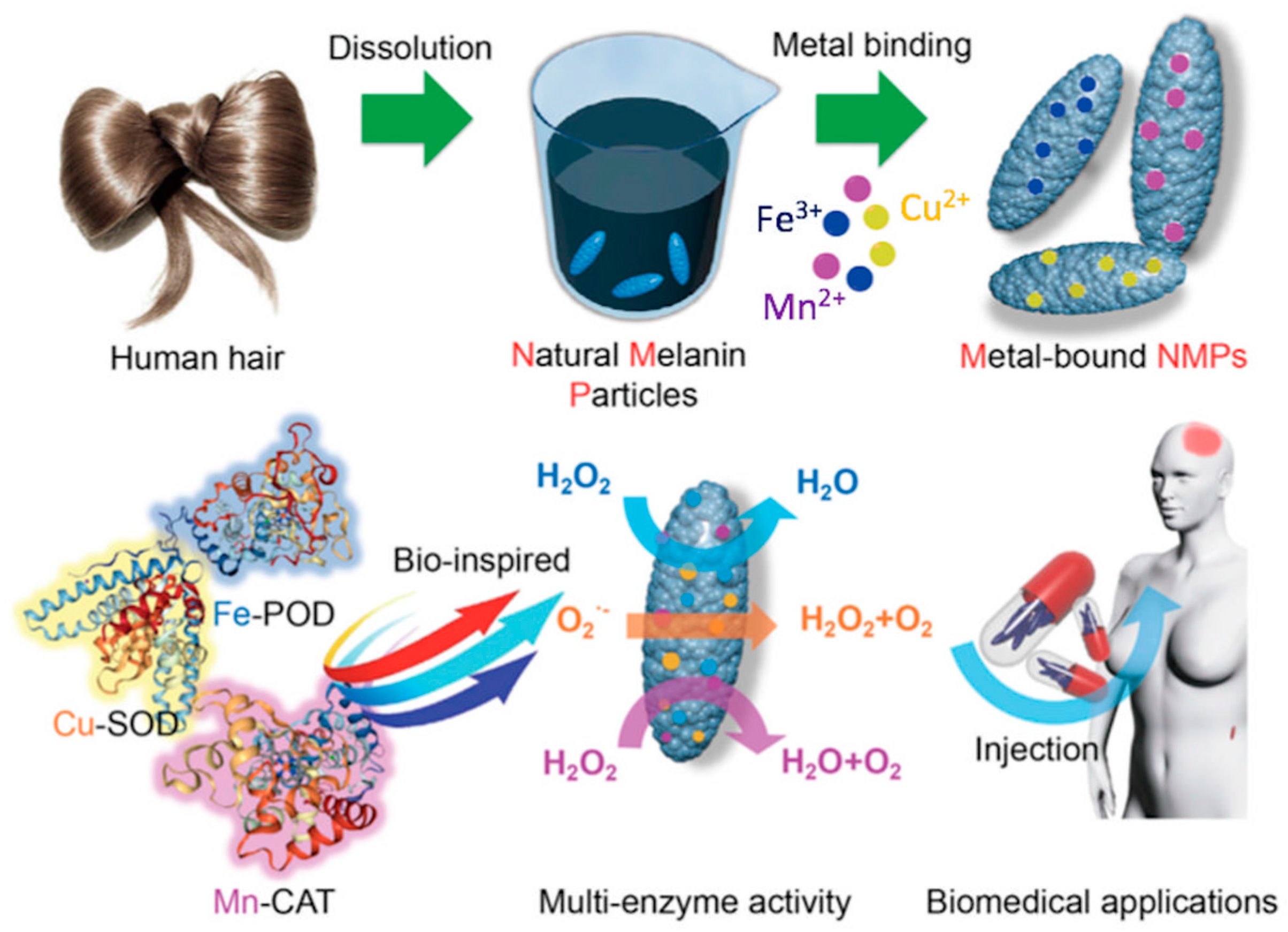
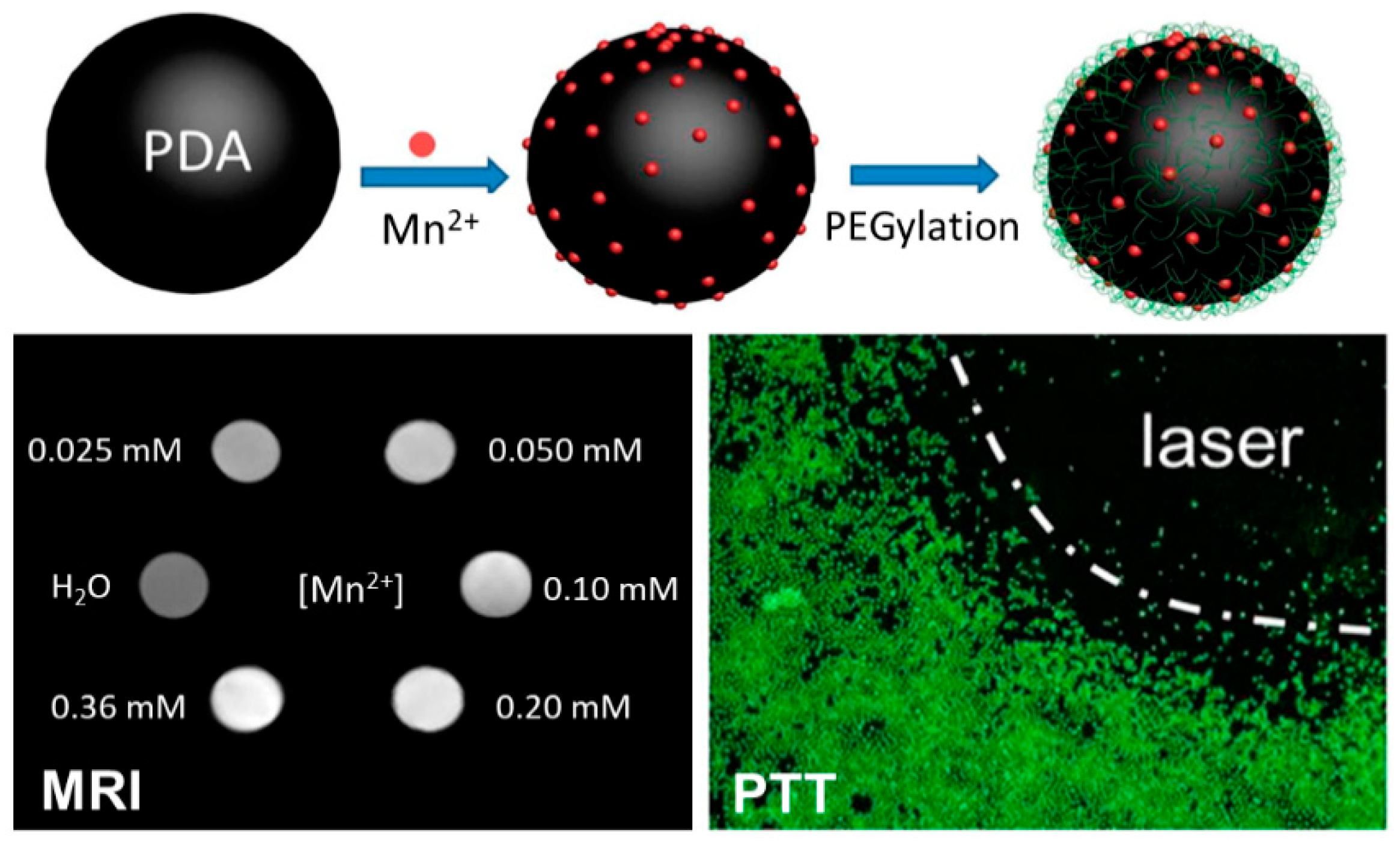
2.1.2. Metal Ions Chelating Action
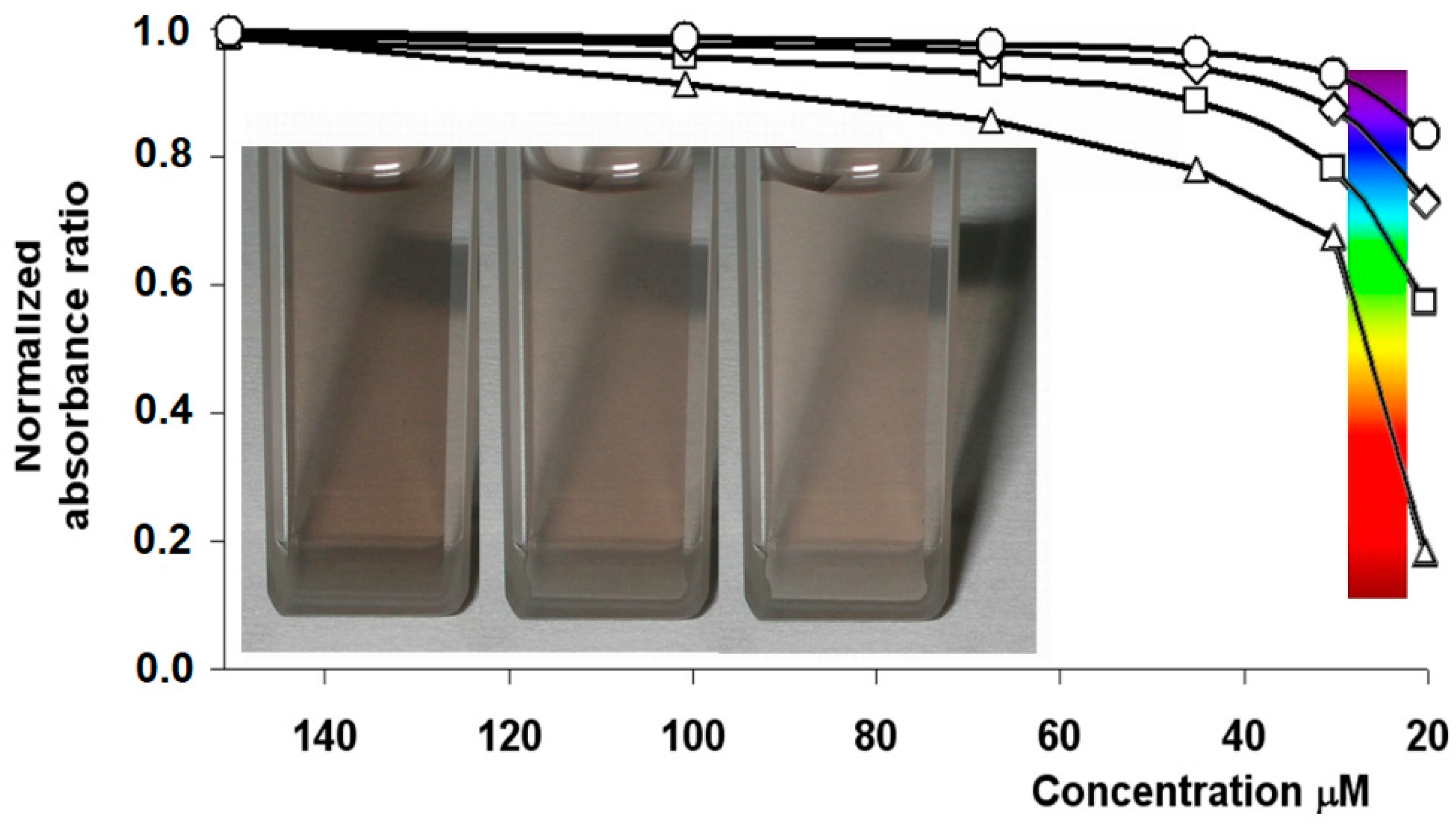
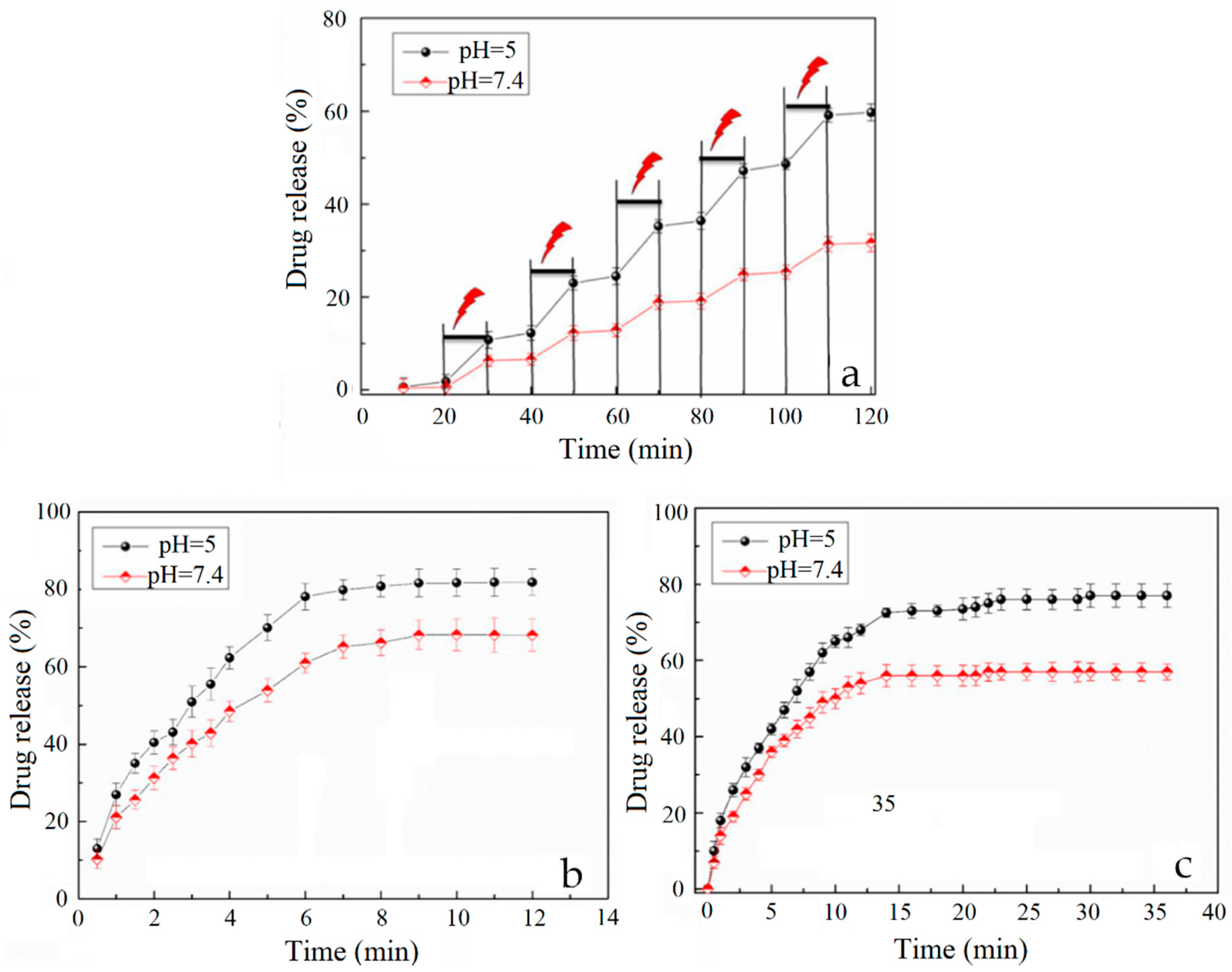
2.1.3. Broad Light Absorption
2.1.4. Paramagnetic and Red-Ox Properties
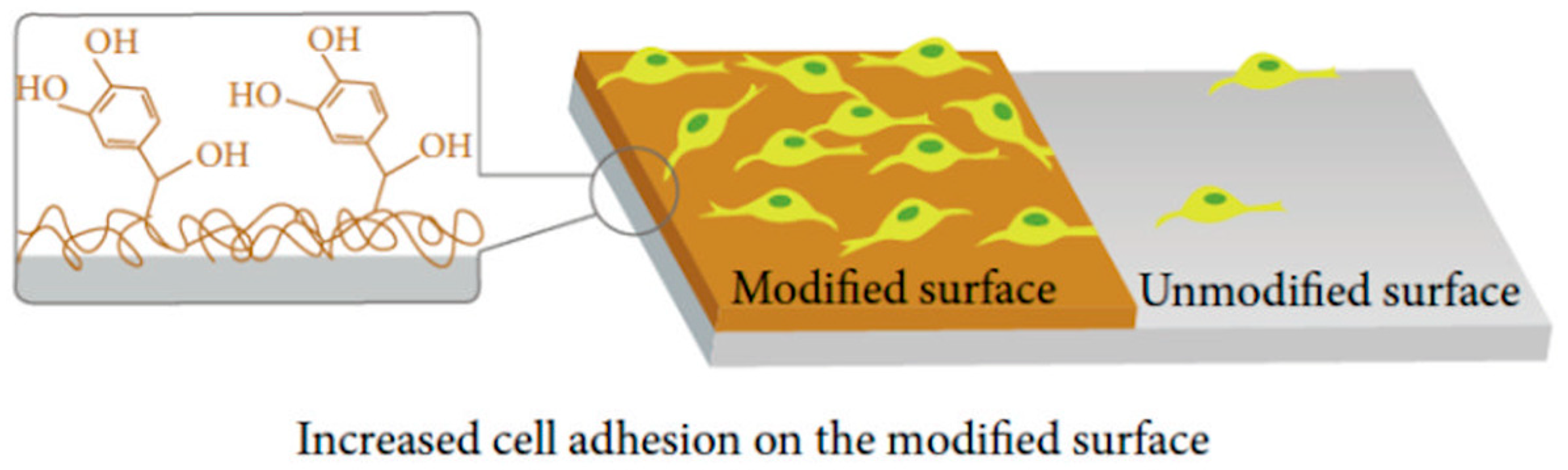
2.1.5. Adhesive Properties
3. Melanins and Melanin-Like Materials in Tissue Engineering
3.1. Wound Healing
3.1.1. Hydrogels
3.1.2. Films and Membranes
3.2. Bone and Cartilage Tissue Engineering
3.2.1. Fibrous Scaffolds
3.2.2. 3D Printed Scaffolds
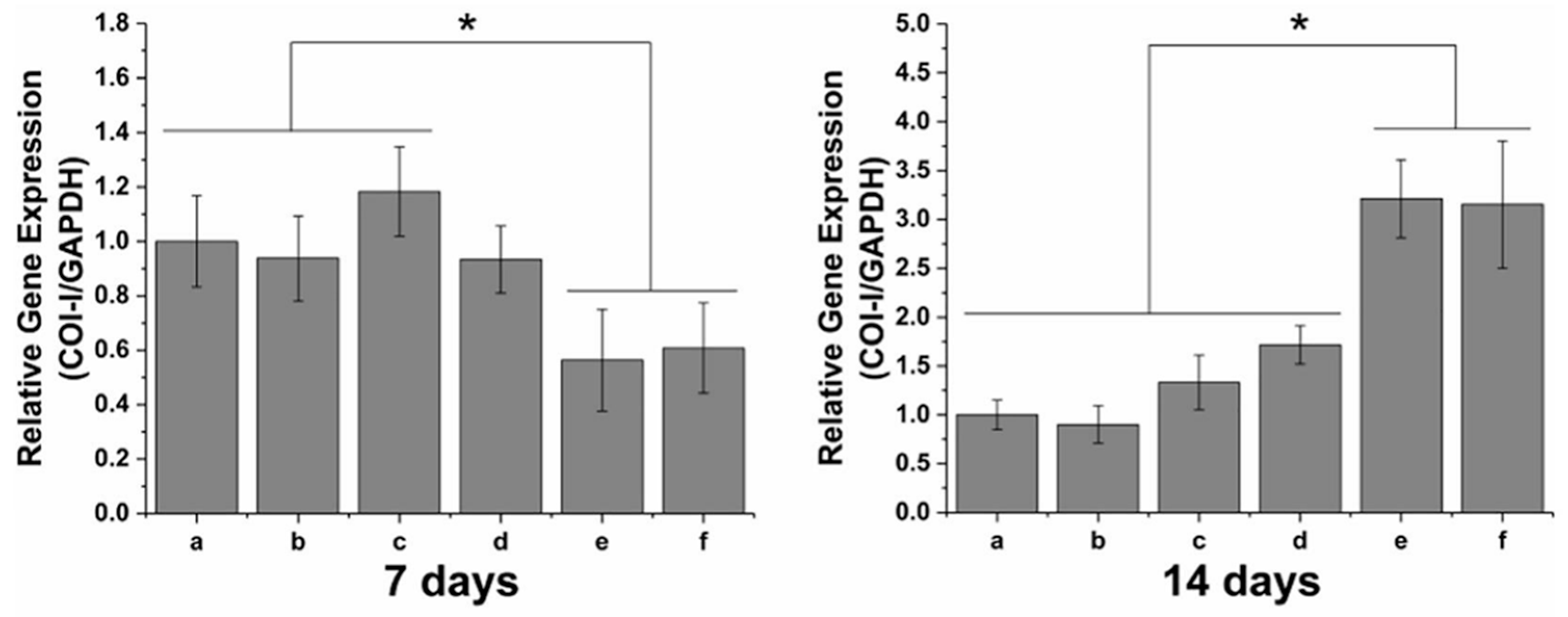
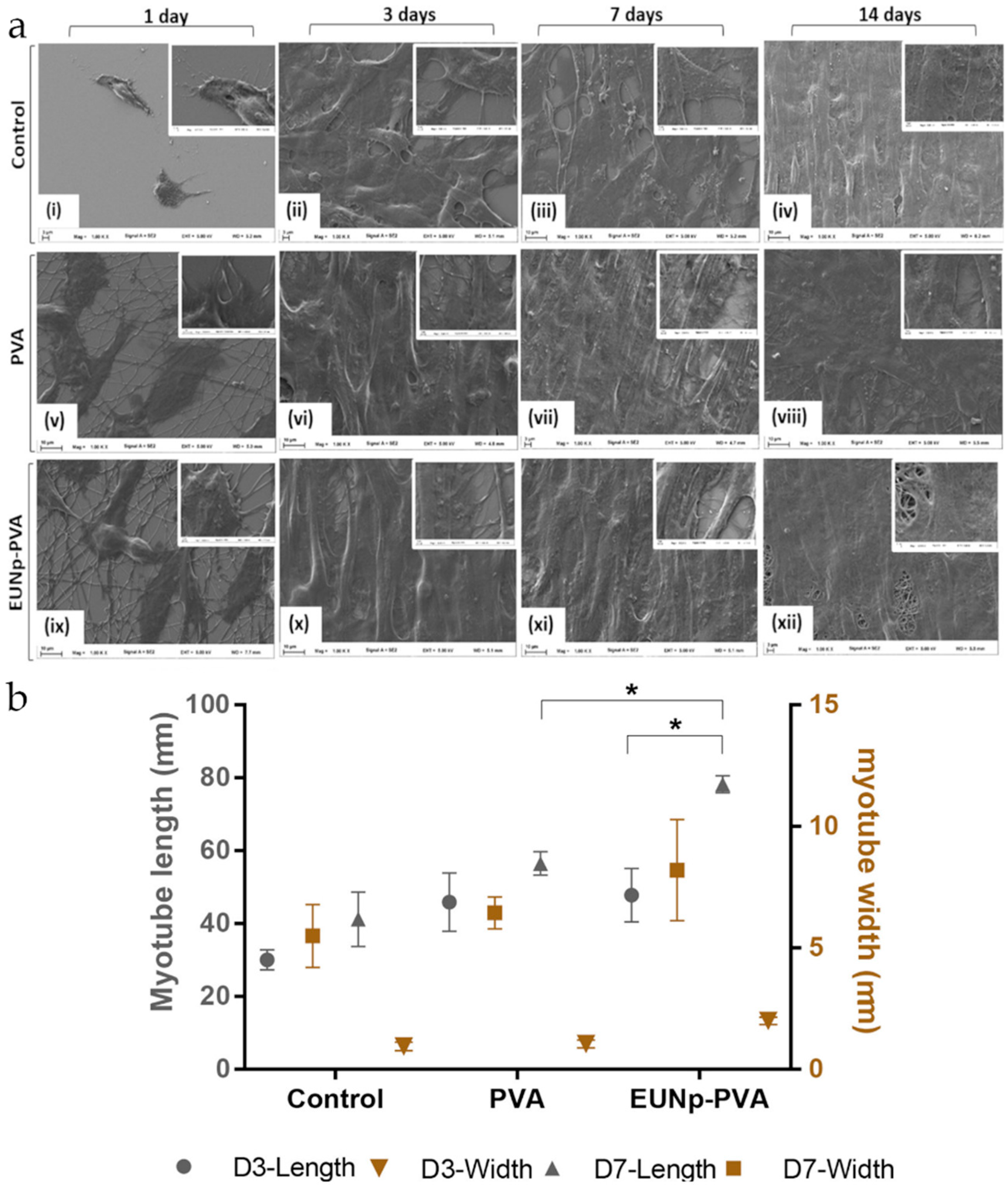
3.3. Nerve and Muscular Tissue Engineering
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| 3DP | 3D printed |
| ALP | alkaline phosphatase |
| bFGF | basic fibroblast growth factor |
| CS | Chitosan |
| CT | computed tomography |
| Cyp | Ciprofloxacin |
| DA | Dopamine |
| DHI | 5,6-dihydroxyindole |
| DHICA | 5,6-dihydroxyindole-2-carboxylic acid |
| EDC | 1-ethyl-3-(3-dimethylaminopropyl)carbodiimide |
| EGF | epidermal growth factor |
| G-C | glycol-chitosan |
| GO | graphene oxide |
| hKCs | human keratinocytes |
| L-DOPA | L-3,4-dihydroxyphenylalanine |
| LMCT | ligand to metal charge transfer |
| MRI | magnetic resonance imaging |
| NGF | nerve growth factor |
| NIR | near-infrared |
| PAI | photoacoustic imaging |
| PAM | Polyacrylamide |
| PANI | Polyaniline |
| PCL | poly(e-caprolactone) |
| PDA | Polydopamine |
| pDHN | poly-1,8-dihydroxynaphthalene |
| PEG | poly(ethylene glycol) |
| PET | positron emission tomography |
| pGO | polydopamine-reduced graphene oxide |
| PLA | poly(lactic acid) |
| PLG | poly(L-lactide-co-glycolide) |
| PLGA | poly(lactic-co-glycolic acid) |
| PMPDA NPs | PEGylated Mn2+−PDA nanoparticles |
| PNIPAM | poly(N-isopropylacrylamide-co-acrylamide) |
| PonG1 | ponericin G1 |
| PTT | photothermal therapy |
| PU | Polyurethane |
| PUE | Puerarin |
| PVA | polyvinyl alcohol |
| qPCR | quantitative polymerase chain reaction |
| RONS | reactive oxygen and nitrogen species |
| ROS | reactive oxygen species |
| SEM | scanning electron micrographs |
| SF | silk fibroin |
| SMNP | synthetic melanin nanoparticles |
| SNpc | substantia nigra pars compacta |
| TCP | β-tricalcium phosphate |
| TEM | transmission electron microscopy |
| TH | tetracycline hydrochloride |
| UV | Ultraviolet |
References
- Solano, F. Melanins: Skin Pigments and Much More—Types, Structural Models, Biological Functions, and Formation Routes. New J. Sci. 2014, 2014, 498276. [Google Scholar] [CrossRef]
- Brenner, M.; Hearing, V.J. The Protective Role of Melanin Against UV Damage in Human Skin. Photochem. Photobiol. 2008, 84, 539–549. [Google Scholar] [CrossRef]
- Lin, J.Y.; Fisher, D.E. Melanocyte biology and skin pigmentation. Nature 2007, 445, 843–850. [Google Scholar] [CrossRef]
- Ito, S.; Wakamatsu, K. Chemistry of Mixed Melanogenesis—Pivotal Roles of Dopaquinone†. Photochem. Photobiol. 2008, 84, 582–592. [Google Scholar] [CrossRef]
- Mitra, D.; Luo, X.; Morgan, A.; Wang, J.; Hoang, M.P.; Lo, J.; Guerrero, C.R.; Lennerz, J.K.; Mihm, M.C.; Wargo, J.A.; et al. An ultraviolet-radiation-independent pathway to melanoma carcinogenesis in the red hair/fair skin background. Nature 2012, 491, 449–453. [Google Scholar] [CrossRef] [PubMed]
- Greco, G.; Panzella, L.; Napolitano, A.; d’Ischia, M. The fundamental building blocks of red human hair pheomelanin are isoquinoline-containing dimers. Pigment Cell Melanoma Res. 2012, 25, 110–112. [Google Scholar] [CrossRef] [PubMed]
- Haining, R.L.; Achat-Mendes, C. Neuromelanin, one of the most overlooked molecules in modern medicine, is not a spectator. Neural Regen. Res. 2017, 12, 372–375. [Google Scholar] [CrossRef] [PubMed]
- Bush, W.D.; Garguilo, J.; Zucca, F.A.; Albertini, A.; Zecca, L.; Edwards, G.S.; Nemanich, R.J.; Simon, J.D. The surface oxidation potential of human neuromelanin reveals a spherical architecture with a pheomelanin core and a eumelanin surface. Proc. Natl. Acad. Sci. USA 2006, 103, 14785–14789. [Google Scholar] [CrossRef] [PubMed]
- d’Ischia, M.; Wakamatsu, K.; Cicoira, F.; Mauro, E.D.; Garcia-Borron, J.C.; Commo, S.; Galván, I.; Ghanem, G.; Kenzo, K.; Meredith, P.; et al. Melanins and melanogenesis: From pigment cells to human health and technological applications. Pigment Cell Melanoma Res. 2015, 28, 520–544. [Google Scholar] [CrossRef] [PubMed]
- Taborda, C.P.; da Silva, M.B.; Nosanchuk, J.D.; Travassos, L.R. Melanin as a virulence factor of Paracoccidioides brasiliensis and other dimorphic pathogenic fungi. Mycopathologia 2008, 165, 331–339. [Google Scholar] [CrossRef]
- Kollias, N.; Baqer, A.H. Absorption Mechanisms of Human Melanin in the Visible, 400–720nm. J. Investig. Dermatol. 1987, 89, 384–388. [Google Scholar] [CrossRef] [PubMed]
- Kalia, S.; Zhao, J.; Zeng, H.; McLean, D.; Kollias, N.; Lui, H. Melanin quantification by in vitro and in vivo analysis of near-infrared fluorescence. Pigment Cell Melanoma Res. 2018, 31, 31–38. [Google Scholar] [CrossRef] [PubMed]
- Ou-Yang, H.; Stamatas, G.; Kollias, N. Spectral Responses of Melanin to Ultraviolet A Irradiation. J. Investig. Dermatol. 2004, 122, 492–496. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Ai, K.; Ji, X.; Askhatova, D.; Du, R.; Lu, L.; Shi, J. Comprehensive Insights into the Multi-Antioxidative Mechanisms of Melanin Nanoparticles and Their Application to Protect Brain from Injury in Ischemic Stroke. J. Am. Chem. Soc. 2017, 139, 856–862. [Google Scholar] [CrossRef] [PubMed]
- Panzella, L.; Gentile, G.; D’Errico, G.; Vecchia, N.F.D.; Errico, M.E.; Napolitano, A.; Carfagna, C.; d’Ischia, M. Atypical Structural and π-Electron Features of a Melanin Polymer That Lead to Superior Free-Radical-Scavenging Properties. Angew. Chem. Int. Ed. Engl. 2013, 52, 12684–12687. [Google Scholar] [CrossRef]
- Kollias, N.; Sayre, R.M.; Zeise, L.; Chedekel, M.R. New trends in photobiology: Photoprotection by melanin. J. Photochem. Photobiol. B Biol. 1991, 9, 135–160. [Google Scholar] [CrossRef]
- Mostert, A.B.; Powell, B.J.; Pratt, F.L.; Hanson, G.R.; Sarna, T.; Gentle, I.R.; Meredith, P. Role of semiconductivity and ion transport in the electrical conduction of melanin. Proc. Natl. Acad. Sci. USA 2012, 109, 8943–8947. [Google Scholar] [CrossRef]
- Meredith, P.; Sarna, T. The physical and chemical properties of eumelanin. Pigment Cell Res. 2006, 19, 572–594. [Google Scholar] [CrossRef]
- Mauro, E.D.; Xu, R.; Soliveri, G.; Santato, C. Natural melanin pigments and their interfaces with metal ions and oxides: Emerging concepts and technologies. MRS Commun. 2017, 7, 141–151. [Google Scholar] [CrossRef]
- Zucca, F.A.; Segura-Aguilar, J.; Ferrari, E.; Muñoz, P.; Paris, I.; Sulzer, D.; Sarna, T.; Casella, L.; Zecca, L. Interactions of iron, dopamine and neuromelanin pathways in brain aging and Parkinson’s disease. Prog. Neurobiol. 2017, 155, 96–119. [Google Scholar] [CrossRef]
- Zucca, F.A.; Basso, E.; Cupaioli, F.A.; Ferrari, E.; Sulzer, D.; Casella, L.; Zecca, L. Neuromelanin of the Human Substantia Nigra: An Update. Neurotox. Res. 2014, 25, 13–23. [Google Scholar] [CrossRef] [PubMed]
- Vitiello, G.; Melone, P.; Silvestri, B.; Pezzella, A.; Donato, P.D.; D’Errico, G.; Napoli, M.D.; Zanfardino, A.; Varcamonti, M.; Luciani, G. Titanium based complexes with melanin precursors as a tool for directing melanogenic pathways. Pure Appl. Chem. 2019, 91, 1605–1616. [Google Scholar] [CrossRef]
- Cho, S.; Kim, S.-H. Hydroxide ion-mediated synthesis of monodisperse dopamine–melanin nanospheres. J. Colloid Interface Sci. 2015, 458, 87–93. [Google Scholar] [CrossRef] [PubMed]
- Huang, L.; Liu, M.; Huang, H.; Wen, Y.; Zhang, X.; Wei, Y. Recent Advances and Progress on Melanin-like Materials and Their Biomedical Applications. Biomacromolecules 2018, 19, 1858–1868. [Google Scholar] [CrossRef] [PubMed]
- d’Ischia, M. Melanin-Based Functional Materials. Int. J. Mol. Sci. 2018, 19, 228. [Google Scholar] [CrossRef]
- Büngeler, A.; Hämisch, B.; Strube, O.I. The Supramolecular Buildup of Eumelanin: Structures, Mechanisms, Controllability. Int. J. Mol. Sci. 2017, 18, 1901. [Google Scholar] [CrossRef]
- Wei, Q.; Zhang, F.; Li, J.; Li, B.; Zhao, C. Oxidant-induced dopamine polymerization for multifunctional coatings. Polym. Chem. 2010, 1, 1430–1433. [Google Scholar] [CrossRef]
- Zhang, C.; Ou, Y.; Lei, W.-X.; Wan, L.-S.; Ji, J.; Xu, Z.-K. CuSO4/H2O2-Induced Rapid Deposition of Polydopamine Coatings with High Uniformity and Enhanced Stability. Angew. Chem. Int. Ed. Engl. 2016, 55, 3054–3057. [Google Scholar] [CrossRef]
- Lee, M.; Lee, S.-H.; Oh, I.-K.; Lee, H. Microwave-Accelerated Rapid, Chemical Oxidant-Free, Material-Independent Surface Chemistry of Poly(dopamine). Small 2017, 13, 1600443. [Google Scholar] [CrossRef]
- Kim, J.Y.; Kim, W.I.; Youn, W.; Seo, J.; Kim, B.J.; Lee, J.K.; Choi, I.S. Enzymatic film formation of nature-derived phenolic amines. Nanoscale 2018, 10, 13351–13355. [Google Scholar] [CrossRef]
- Lee, H.; Dellatore, S.M.; Miller, W.M.; Messersmith, P.B. Mussel-Inspired Surface Chemistry for Multifunctional Coatings. Science 2007, 318, 426–430. [Google Scholar] [CrossRef] [PubMed]
- Caldas, M.; Santos, A.C.; Veiga, F.; Rebelo, R.; Reis, R.L.; Correlo, V.M. Melanin nanoparticles as a promising tool for biomedical applications—A review. Acta Biomater. 2020, 105, 26–43. [Google Scholar] [CrossRef] [PubMed]
- d’Ischia, M.; Napolitano, A.; Ball, V.; Chen, C.-T.; Buehler, M.J. Polydopamine and Eumelanin: From Structure–Property Relationships to a Unified Tailoring Strategy. Acc. Chem. Res. 2014, 47, 3541–3550. [Google Scholar] [CrossRef] [PubMed]
- Lu, Z.; Douek, A.M.; Rozario, A.M.; Tabor, R.F.; Kaslin, J.; Follink, B.; Teo, B.M. Bioinspired polynorepinephrine nanoparticles as an efficient vehicle for enhanced drug delivery. J. Mater. Chem. B 2020, 8, 961–968. [Google Scholar] [CrossRef]
- Park, M.; Shin, M.; Kim, E.; Lee, S.; Park, K.I.; Lee, H.; Jang, J.-H. The Promotion of Human Neural Stem Cells Adhesion Using Bioinspired Poly(norepinephrine) Nanoscale Coating. J. Nanomater. 2014, 2014, 793052. [Google Scholar] [CrossRef]
- Manini, P.; Lino, V.; Franchi, P.; Gentile, G.; Sibillano, T.; Giannini, C.; Picardi, E.; Napolitano, A.; Valgimigli, L.; Chiappe, C.; et al. A Robust Fungal Allomelanin Mimic: An Antioxidant and Potent π-Electron Donor with Free-Radical Properties that can be Tuned by Ionic Liquids. ChemPlusChem 2019, 84, 1331–1337. [Google Scholar] [CrossRef] [PubMed]
- Manini, P.; Lucci, V.; Lino, V.; Sartini, S.; Rossella, F.; Falco, G.; Chiappe, C.; d’Ischia, M. Synthetic mycomelanin thin films as emergent bio-inspired interfaces controlling the fate of embryonic stem cells. J. Mater. Chem. B 2020, 8, 4412–4418. [Google Scholar] [CrossRef] [PubMed]
- Ouyang, R.; Lei, J.; Ju, H.; Xue, Y. A Molecularly Imprinted Copolymer Designed for Enantioselective Recognition of Glutamic Acid. Adv. Funct. Mater. 2007, 17, 3223–3230. [Google Scholar] [CrossRef]
- El Yakhlifi, S.; Ball, V. Polydopamine as a stable and functional nanomaterial. Colloids Surf. B 2020, 186, 110719. [Google Scholar] [CrossRef]
- Schneider, A.; Hemmerlé, J.; Allais, M.; Didierjean, J.; Michel, M.; d’Ischia, M.; Ball, V. Boric Acid as an Efficient Agent for the Control of Polydopamine Self-Assembly and Surface Properties. ACS Appl. Mater. Interfaces 2018, 10, 7574–7580. [Google Scholar] [CrossRef]
- della Vecchia, N.F.; Cerruti, P.; Gentile, G.; Errico, M.E.; Ambrogi, V.; D’Errico, G.; Longobardi, S.; Napolitano, A.; Paduano, L.; Carfagna, C.; et al. Artificial Biomelanin: Highly Light-Absorbing Nano-Sized Eumelanin by Biomimetic Synthesis in Chicken Egg White. Biomacromolecules 2014, 15, 3811–3816. [Google Scholar] [CrossRef] [PubMed]
- Vij, M.; Grover, R.; Gotherwal, V.; Wani, N.A.; Joshi, P.; Gautam, H.; Sharma, K.; Chandna, S.; Gokhale, R.S.; Rai, R.; et al. Bioinspired Functionalized Melanin Nanovariants with a Range of Properties Provide Effective Color Matched Photoprotection in Skin. Biomacromolecules 2016, 17, 2912–2919. [Google Scholar] [CrossRef] [PubMed]
- della Vecchia, N.F.; Luchini, A.; Napolitano, A.; D’Errico, G.; Vitiello, G.; Szekely, N.; d’Ischia, M.; Paduano, L. Tris buffer modulates polydopamine growth, aggregation, and paramagnetic properties. Langmuir 2014, 30, 9811–9818. [Google Scholar] [CrossRef] [PubMed]
- Lemaster, J.E.; Jeevarathinam, A.S.; Kumar, A.; Chandrasekar, B.; Chen, F.; Jokerst, J.V. Synthesis of Ultrasmall Synthetic Melanin Nanoparticles by UV Irradiation in Acidic and Neutral Conditions. ACS Appl. Bio Mater. 2019, 2, 4667–4674. [Google Scholar] [CrossRef] [PubMed]
- Vitiello, G.; Pezzella, A.; Zanfardino, A.; Varcamonti, M.; Silvestri, B.; Costantini, A.; Branda, F.; Luciani, G. Titania as a driving agent for DHICA polymerization: A novel strategy for the design of bioinspired antimicrobial nanomaterials. J. Mater. Chem. B 2015, 3, 2808–2815. [Google Scholar] [CrossRef] [PubMed]
- Vitiello, G.; Zanfardino, A.; Tammaro, O.; Napoli, M.D.; Caso, M.F.; Pezzella, A.; Varcamonti, M.; Silvestri, B.; D’Errico, G.; Costantini, A.; et al. Bioinspired hybrid eumelanin–TiO2 antimicrobial nanostructures: The key role of organo–inorganic frameworks in tuning eumelanin’s biocide action mechanism through membrane interaction. RSC Adv. 2018, 8, 28275–28283. [Google Scholar] [CrossRef]
- Vitiello, G.; Pezzella, A.; Calcagno, V.; Silvestri, B.; Raiola, L.; D’Errico, G.; Costantini, A.; Branda, F.; Luciani, G. 5,6-Dihydroxyindole-2-carboxylic Acid-TiO2 Charge Transfer Complexes in the Radical Polymerization of Melanogenic Precursor(s). J. Phys. Chem. C 2016, 120, 6262–6268. [Google Scholar] [CrossRef]
- Xie, W.; Pakdel, E.; Liang, Y.; Kim, Y.J.; Liu, D.; Sun, L.; Wang, X. Natural Eumelanin and Its Derivatives as Multifunctional Materials for Bioinspired Applications: A Review. Biomacromolecules 2019, 20, 4312–4331. [Google Scholar] [CrossRef]
- Liu, H.; Yang, Y.; Liu, Y.; Pan, J.; Wang, J.; Man, F.; Zhang, W.; Liu, G. Melanin-Like Nanomaterials for Advanced Biomedical Applications: A Versatile Platform with Extraordinary Promise. Adv. Sci. 2020, 7, 1903129. [Google Scholar] [CrossRef]
- Cho, S.; Park, W.; Kim, D.-H. Silica-Coated Metal Chelating-Melanin Nanoparticles as a Dual-Modal Contrast Enhancement Imaging and Therapeutic Agent. ACS Appl. Mater. Interfaces 2017, 9, 101–111. [Google Scholar] [CrossRef]
- Silvestri, B.; Armanetti, P.; Sanità, G.; Vitiello, G.; Lamberti, A.; Calì, G.; Pezzella, A.; Luciani, G.; Menichetti, L.; Luin, S.; et al. Silver-nanoparticles as plasmon-resonant enhancers for eumelanin’s photoacoustic signal in a self-structured hybrid nanoprobe. Mater. Sci. Eng. C 2019, 102, 788–797. [Google Scholar] [CrossRef] [PubMed]
- Zou, Y.; Wu, T.; Li, N.; Guo, X.; Li, Y. Photothermal-enhanced synthetic melanin inks for near-infrared imaging. Polymer 2020, 186, 122042. [Google Scholar] [CrossRef]
- Hong, S.; Zhang, Q.-L.; Zheng, D.-W.; Zhang, C.; Zhang, Y.; Ye, J.-J.; Cheng, H.; Zhang, X.-Z. Enzyme Mimicking Based on the Natural Melanin Particles from Human Hair. iScience 2020, 23, 100778. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Xie, Y.; Wang, Z.; Zang, N.; Carniato, F.; Huang, Y.; Andolina, C.M.; Parent, L.R.; Ditri, T.B.; Walter, E.D.; et al. Structure and Function of Iron-Loaded Synthetic Melanin. ACS Nano 2016, 10, 10186–10194. [Google Scholar] [CrossRef] [PubMed]
- Ha, S.-W.; Cho, H.-S.; Yoon, Y.I.; Jang, M.-S.; Hong, K.S.; Hui, E.; Lee, J.H.; Yoon, T.-J. Ions doped melanin nanoparticle as a multiple imaging agent. J. Nanobiotechnol. 2017, 15, 73. [Google Scholar] [CrossRef]
- Hong, S.H.; Sun, Y.; Tang, C.; Cheng, K.; Zhang, R.; Fan, Q.; Xu, L.; Huang, D.; Zhao, A.; Cheng, Z. Chelator-Free and Biocompatible Melanin Nanoplatform with Facile-Loading Gadolinium and Copper-64 for Bioimaging. Bioconjug. Chem. 2017, 28, 1925–1930. [Google Scholar] [CrossRef]
- Lemaster, J.E.; Wang, Z.; Hariri, A.; Chen, F.; Hu, Z.; Huang, Y.; Barback, C.V.; Cochran, R.; Gianneschi, N.C.; Jokerst, J.V. Gadolinium Doping Enhances the Photoacoustic Signal of Synthetic Melanin Nanoparticles: A Dual Modality Contrast Agent for Stem Cell Imaging. Chem. Mater. 2019, 31, 251–259. [Google Scholar] [CrossRef]
- Wang, C.; Wang, D.; Dai, T.; Xu, P.; Wu, P.; Zou, Y.; Yang, P.; Hu, J.; Li, Y.; Cheng, Y. Skin Pigmentation-Inspired Polydopamine Sunscreens. Adv. Funct. Mater. 2018, 28, 1802127. [Google Scholar] [CrossRef]
- Pezzella, A.; Iadonisi, A.; Valerio, S.; Panzella, L.; Napolitano, A.; Adinolfi, M.; d’Ischia, M. Disentangling Eumelanin “Black Chromophore”: Visible Absorption Changes as Signatures of Oxidation State- and Aggregation-Dependent Dynamic Interactions in a Model Water-Soluble 5,6-Dihydroxyindole Polymer. J. Am. Chem. Soc. 2009, 131, 15270–15275. [Google Scholar] [CrossRef]
- Huang, Y.; Li, Y.; Hu, Z.; Yue, X.; Proetto, M.T.; Jones, Y.; Gianneschi, N.C. Mimicking Melanosomes: Polydopamine Nanoparticles as Artificial Microparasols. ACS Cent. Sci. 2017, 3, 564–569. [Google Scholar] [CrossRef]
- Huijser, A.; Pezzella, A.; Sundström, V. Functionality of epidermal melanin pigments: Current knowledge on UV-dissipative mechanisms and research perspectives. Phys. Chem. Chem. Phys. 2011, 13, 9119–9127. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Z.; Yan, Y.; Zhang, Q.; Cheng, Y. Melanin-like nanoparticles loaded with an angiotensin antagonist for an improved photothermal cancer therapy. Biomater. Sci. 2020, 8, 1658–1668. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.A.; Yoon, S.D.; Kim, E.-M.; Jeong, H.-J.; Lee, C.-M. Natural melanin-loaded nanovesicles for near-infrared mediated tumor ablation by photothermal conversion. Nanotechnology 2018, 29, 415101. [Google Scholar] [CrossRef] [PubMed]
- Ma, H.; Zhou, Q.; Chang, J.; Wu, C. Grape Seed-Inspired Smart Hydrogel Scaffolds for Melanoma Therapy and Wound Healing. ACS Nano 2019, 13, 4302–4311. [Google Scholar] [CrossRef]
- Awad, B.; Aly, A.A.; Ghannam, M.M. Melanin Doping Potential Effect on the Optical Properties Polyvinyl Alcohol. Int. J. Adv. Res. Chem. Sci. 2018, 5, 24–32. [Google Scholar]
- Ninh, C.; Cramer, M.J.; Bettinger, C. Photoresponsive hydrogel networks using melanin nanoparticle photothermal sensitizers. Biomater. Sci. 2014, 2, 766–774. [Google Scholar] [CrossRef]
- Kim, M.A.; Yoon, S.D.; Lee, C.-M. A drug release system induced by near infrared laser using alginate microparticles containing melanin. Int. J. Biol. Macromol. 2017, 103, 839–844. [Google Scholar] [CrossRef]
- Kim, Y.S.; Kim, M.A.; Lee, C.-M. Controlled drug release from PNIPAM-incorporated melanin nanovesicles by photo-stimulation. Mater. Technol. 2019, 34, 639–644. [Google Scholar] [CrossRef]
- Miao, Z.-H.; Wang, H.; Yang, H.; Li, Z.-L.; Zhen, L.; Xu, C.-Y. Intrinsically Mn2+-Chelated Polydopamine Nanoparticles for Simultaneous Magnetic Resonance Imaging and Photothermal Ablation of Cancer Cells. ACS Appl. Mater. Interfaces 2015, 7, 16946–16952. [Google Scholar] [CrossRef]
- Liu, F.; He, X.; Zhang, J.; Chen, H.; Zhang, H.; Wang, Z. Controllable synthesis of polydopamine nanoparticles in microemulsions with pH-activatable properties for cancer detection and treatment. J. Mater. Chem. B 2015, 3, 6731–6739. [Google Scholar] [CrossRef]
- Repenko, T.; Rix, A.; Nedilko, A.; Rose, J.; Hermann, A.; Vinokur, R.; Moli, S.; Cao-Milàn, R.; Mayer, M.; von Plessen, G.; et al. Strong Photoacoustic Signal Enhancement by Coating Gold Nanoparticles with Melanin for Biomedical Imaging. Adv. Funct. Mater. 2018, 28, 1705607. [Google Scholar] [CrossRef]
- Dong, Z.; Feng, L.; Hao, Y.; Chen, M.; Gao, M.; Chao, Y.; Zhao, H.; Zhu, W.; Liu, J.; Liang, C.; et al. Synthesis of Hollow Biomineralized CaCO3-Polydopamine Nanoparticles for Multimodal Imaging-Guided Cancer Photodynamic Therapy with Reduced Skin Photosensitivity. J. Am. Chem. Soc. 2018, 140, 2165–2178. [Google Scholar] [CrossRef] [PubMed]
- Cheng, Y.; Zhang, S.; Kang, N.; Huang, J.; Lv, X.; Wen, K.; Ye, S.; Chen, Z.; Zhou, X.; Ren, L. Polydopamine-Coated Manganese Carbonate Nanoparticles for Amplified Magnetic Resonance Imaging-Guided Photothermal Therapy. ACS Appl. Mater. Interfaces 2017, 9, 19296–19306. [Google Scholar] [CrossRef] [PubMed]
- Roy, S.; Rhim, J.-W. Agar-based antioxidant composite films incorporated with melanin nanoparticles. Food Hydrocoll. 2019, 94, 391–398. [Google Scholar] [CrossRef]
- Roy, S.; Hai, L.V.; Kim, H.C.; Zhai, L.; Kim, J. Preparation and characterization of synthetic melanin-like nanoparticles reinforced chitosan nanocomposite films. Carbohydr. Polym. 2020, 231, 115729. [Google Scholar] [CrossRef]
- Khemakhem, M.; Papadimitriou, V.; Sotiroudis, G.; Zoumpoulakis, P.; Arbez-Gindre, C.; Bouzouita, N.; Sotiroudis, T.G. Melanin and humic acid-like polymer complex from olive mill waste waters. Part I. Isolation and characterization. Food Chem. 2016, 203, 540–547. [Google Scholar] [CrossRef]
- Gurme, S.T.; Aware, C.B.; Surwase, S.N.; Chavan, C.S.; Jadhav, J.P. Synthesis of Melanin Mediated Silver Nanoparticles from Aeromonas sp. SNS Using Response Surface Methodology: Characterization with the Biomedical Applications and Photocatalytic Degradation of Brilliant Green. J. Polym. Environ. 2019, 27, 2428–2438. [Google Scholar] [CrossRef]
- Luo, H.; Gu, C.; Zheng, W.; Dai, F.; Wang, X.; Zheng, Z. Facile synthesis of novel size-controlled antibacterial hybrid spheres using silver nanoparticles loaded with poly-dopamine spheres. RSC Adv. 2015, 5, 13470–13477. [Google Scholar] [CrossRef]
- Pezzella, A.; Barra, M.; Musto, A.; Navarra, A.; Alfè, M.; Manini, P.; Parisi, S.; Cassinese, A.; Criscuolo, V.; d’Ischia, M. Stem cell-compatible eumelanin biointerface fabricated by chemically controlled solid state polymerization. Mater. Horiz. 2015, 2, 212–220. [Google Scholar] [CrossRef]
- Alfieri, M.L.; Panzella, L.; Oscurato, S.L.; Salvatore, M.; Avolio, R.; Errico, M.E.; Maddalena, P.; Napolitano, A.; D’Ischia, M. The Chemistry of Polydopamine Film Formation: The Amine-Quinone Interplay. Biomimetics 2018, 3, 26. [Google Scholar] [CrossRef]
- Iacomino, M.; Paez, J.I.; Avolio, R.; Carpentieri, A.; Panzella, L.; Falco, G.; Pizzo, E.; Errico, M.E.; Napolitano, A.; Del Campo, A.; et al. Multifunctional Thin Films and Coatings from Caffeic Acid and a Cross-Linking Diamine. Langmuir 2017, 33, 2096–2102. [Google Scholar] [CrossRef] [PubMed]
- Fasolino, I.; Bonadies, I.; Ambrosio, L.; Raucci, M.G.; Carfagna, C.; Caso, F.M.; Cimino, F.; Pezzella, A. Eumelanin Coated PLA Electrospun Micro Fibers as Bioinspired Cradle for SH-SY5Y Neuroblastoma Cells Growth and Maturation. ACS Appl. Mater. Interfaces 2017, 9, 40070–40076. [Google Scholar] [CrossRef] [PubMed]
- Gargiulo, V.; Alfè, M.; Capua, R.D.; Togna, A.R.; Cammisotto, V.; Fiorito, S.; Musto, A.; Navarra, A.; Parisi, S.; Pezzella, A. Supplementing π-systems: Eumelanin and graphene-like integration towards highly conductive materials for the mammalian cell culture bio-interface. J. Mater. Chem. B 2015, 3, 5070–5079. [Google Scholar] [CrossRef] [PubMed]
- Barra, M.; Bonadies, I.; Carfagna, C.; Cassinese, A.; Cimino, F.; Crescenzi, O.; Criscuolo, V.; d’Ischia, M.; Maglione, M.G.; Manini, P.; et al. Eumelanin-Based Organic Bioelectronics: Myth or Reality? MRS Adv. 2016, 1, 3801–3810. [Google Scholar] [CrossRef]
- Lee, H.; Rho, J.; Messersmith, P.B. Facile Conjugation of Biomolecules onto Surfaces via Mussel Adhesive Protein Inspired Coatings. Adv. Mater. 2009, 21, 431–434. [Google Scholar] [CrossRef] [PubMed]
- Tan, J.; Xie, Z.; Zhang, Z.; Sun, Y.; Shi, W.; Ge, D. Dopamine modified polyaniline with improved adhesion, dispersibility, and biocompatibility. J. Mater. Sci. 2018, 53, 447–455. [Google Scholar] [CrossRef]
- Wang, D.; Wu, H.; Zhou, J.; Xu, P.; Wang, C.; Shi, R.; Wang, H.; Wang, H.; Guo, Z.; Chen, Q. In Situ One-Pot Synthesis of MOF–Polydopamine Hybrid Nanogels with Enhanced Photothermal Effect for Targeted Cancer Therapy. Adv. Sci. 2018, 5, 1800287. [Google Scholar] [CrossRef]
- Nune, M.; Manchineella, S.; Govindaraju, T.; Narayan, K.S. Melanin incorporated electroactive and antioxidant silk fibroin nanofibrous scaffolds for nerve tissue engineering. Mater. Sci. Eng. C 2019, 94, 17–25. [Google Scholar] [CrossRef]
- Junker, J.P.E.; Kamel, R.A.; Caterson, E.J.; Eriksson, E. Clinical Impact Upon Wound Healing and Inflammation in Moist, Wet, and Dry Environments. Adv. Wound Care 2013, 2, 348–356. [Google Scholar] [CrossRef]
- Zarrintaj, P.; Moghaddam, A.S.; Manouchehri, S.; Atoufi, Z.; Amiri, A.; Amirkhani, M.A.; Nilforoushzadeh, M.A.; Saeb, M.R.; Hamblin, M.R.; Mozafari, M. Can regenerative medicine and nanotechnology combine to heal wounds? The search for the ideal wound dressing. Nanomedicine 2017, 12, 2403–2422. [Google Scholar] [CrossRef]
- ’t Veld, R.C.O.; Walboomers, X.F.; Jansen, J.A.; Wagener, F.A.D.T.G. Design Considerations for Hydrogel Wound Dressings: Strategic and Molecular Advances. Tissue Eng. Part B Rev. 2020, 26, 230–248. [Google Scholar] [CrossRef]
- Gupta, A.; Kowalczuk, M.; Heaselgrave, W.; Britland, S.T.; Martin, C.; Radecka, I. The production and application of hydrogels for wound management: A review. Eur. Polym. J. 2019, 111, 134–151. [Google Scholar] [CrossRef]
- Zhao, X.; Wu, H.; Guo, B.; Dong, R.; Qiu, Y.; Ma, P.X. Antibacterial anti-oxidant electroactive injectable hydrogel as self-healing wound dressing with hemostasis and adhesiveness for cutaneous wound healing. Biomaterials 2017, 122, 34–47. [Google Scholar] [CrossRef] [PubMed]
- Han, L.; Lu, X.; Liu, K.; Wang, K.; Fang, L.; Weng, L.-T.; Zhang, H.; Tang, Y.; Ren, F.; Zhao, C.; et al. Mussel-Inspired Adhesive and Tough Hydrogel Based on Nanoclay Confined Dopamine Polymerization. ACS Nano 2017, 11, 2561–2574. [Google Scholar] [CrossRef]
- Zhang, S.; Ou, Q.; Xin, P.; Yuan, Q.; Wang, Y.; Wu, J. Polydopamine/puerarin nanoparticle-incorporated hybrid hydrogels for enhanced wound healing. Biomater. Sci. 2019, 7, 4230–4236. [Google Scholar] [CrossRef]
- Han, L.; Zhang, Y.; Lu, X.; Wang, K.; Wang, Z.; Zhang, H. Polydopamine Nanoparticles Modulating Stimuli-Responsive PNIPAM Hydrogels with Cell/Tissue Adhesiveness. ACS Appl. Mater. Interfaces 2016, 8, 29088–29100. [Google Scholar] [CrossRef]
- Liang, Y.; Zhao, X.; Hu, T.; Chen, B.; Yin, Z.; Ma, P.X.; Guo, B. Adhesive Hemostatic Conducting Injectable Composite Hydrogels with Sustained Drug Release and Photothermal Antibacterial Activity to Promote Full-Thickness Skin Regeneration During Wound Healing. Small 2019, 15, 1900046. [Google Scholar] [CrossRef]
- Zhao, Y.; Li, Z.; Song, S.; Yang, K.; Liu, H.; Yang, Z.; Wang, J.; Yang, B.; Lin, Q. Skin-Inspired Antibacterial Conductive Hydrogels for Epidermal Sensors and Diabetic Foot Wound Dressings. Adv. Funct. Mater. 2019, 29, 1901474. [Google Scholar] [CrossRef]
- da Silva, L.P.; Oliveira, S.; Pirraco, R.P.; Santos, T.C.; Reis, R.L.; Marques, A.P.; Correlo, V.M. Eumelanin-releasing spongy-like hydrogels for skin re-epithelialization purposes. Biomed. Mater. 2017, 12, 025010. [Google Scholar] [CrossRef]
- Cheng, G.; Li, B. Nanoparticle-based photodynamic therapy: New trends in wound healing applications. Mater. Today Adv. 2020, 6, 100049. [Google Scholar] [CrossRef]
- Han, L.; Li, P.; Tang, P.; Wang, X.; Zhou, T.; Wang, K.; Ren, F.; Guo, T.; Lu, X. Mussel-inspired cryogels for promoting wound regeneration through photobiostimulation, modulating inflammatory responses and suppressing bacterial invasion. Nanoscale 2019, 11, 15846–15861. [Google Scholar] [CrossRef] [PubMed]
- Liang, Y.; Zhao, X.; Hu, T.; Han, Y.; Guo, B. Mussel-inspired, antibacterial, conductive, antioxidant, injectable composite hydrogel wound dressing to promote the regeneration of infected skin. J. Colloid Interface Sci. 2019, 556, 514–528. [Google Scholar] [CrossRef] [PubMed]
- Kloth, L.C. Electrical Stimulation for Wound Healing: A Review of Evidence from In Vitro Studies, Animal Experiments, and Clinical Trials. Int. J. Lower Extrem. Wounds 2016, 4, 23–44. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Sui, Y.; Liu, C.; Liu, C.; Wu, M.; Li, B.; Li, Y. A physically crosslinked polydopamine/nanocellulose hydrogel as potential versatile vehicles for drug delivery and wound healing. Carbohydr. Polym. 2018, 188, 27–36. [Google Scholar] [CrossRef]
- Gao, G.; Jiang, Y.-W.; Jia, H.-R.; Wu, F.-G. Near-infrared light-controllable on-demand antibiotics release using thermo-sensitive hydrogel-based drug reservoir for combating bacterial infection. Biomaterials 2019, 188, 83–95. [Google Scholar] [CrossRef]
- Desmet, K.D.; Paz, D.A.; Corry, J.J.; Eells, J.T.; Wong-Riley, M.T.T.; Henry, M.M.; Buchmann, E.V.; Connelly, M.P.; Dovi, J.V.; Liang, H.L.; et al. Clinical and Experimental Applications of NIR-LED Photobiomodulation. Photomed. Laser Surg. 2006, 24, 121–128. [Google Scholar] [CrossRef]
- Khan, A.A.; Banwell, P.E.; Bakker, M.C.; Gillespie, P.G.; McGrouther, D.A.; Roberts, A.H.N. Topical radiant heating in wound healing: An experimental study in a donor site wound model*. Int. Wound J. 2004, 1, 233–240. [Google Scholar] [CrossRef]
- Gao, Y.; Du, H.; Xie, Z.; Li, M.; Zhu, J.; Xu, J.; Zhang, L.; Tao, J.; Zhu, J. Self-adhesive photothermal hydrogel films for solar-light assisted wound healing. J. Mater. Chem. B 2019, 7, 3644–3651. [Google Scholar] [CrossRef]
- Boateng, J. Therapeutic Dressings and Wound Healing Applications; John Wiley & Sons: Hoboken, NJ, USA, 2020; ISBN 978-1-119-43326-2. [Google Scholar]
- La, S.; Liu, X.; Ma, P.X. Tissue Engineering with Nano-Fibrous Scaffolds. Soft Matter 2008, 4, 2144–2149. [Google Scholar] [CrossRef]
- Zhang, Y.; Lu, L.; Chen, Y.; Wang, J.; Chen, Y.; Mao, C.; Yang, M. Polydopamine modification of silk fibroin membranes significantly promotes their wound healing effect. Biomater. Sci. 2019, 7, 5232–5237. [Google Scholar] [CrossRef]
- Wang, J.; Chen, Y.; Zhou, G.; Chen, Y.; Mao, C.; Yang, M. Polydopamine-Coated Antheraea pernyi (A. pernyi) Silk Fibroin Films Promote Cell Adhesion and Wound Healing in Skin Tissue Repair. ACS Appl. Mater. Interfaces 2019, 11, 34736–34743. [Google Scholar] [CrossRef] [PubMed]
- Tang, P.; Han, L.; Li, P.; Jia, Z.; Wang, K.; Zhang, H.; Tan, H.; Guo, T.; Lu, X. Mussel-Inspired Electroactive and Antioxidative Scaffolds with Incorporation of Polydopamine-Reduced Graphene Oxide for Enhancing Skin Wound Healing. ACS Appl. Mater. Interfaces 2019, 11, 7703–7714. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Wang, X.; Wang, S.; Zhang, X.; Yu, J.; Wang, C. Mussel-inspired polydopamine-assisted bromelain immobilization onto electrospun fibrous membrane for potential application as wound dressing. Mater. Sci. Eng. C 2020, 110624. [Google Scholar] [CrossRef] [PubMed]
- Muhammad, Z.A.; Ahmad, T. Therapeutic uses of pineapple-extracted bromelain in surgical care—A review. J. Pak. Med. Assoc. 2017, 67, 6. [Google Scholar]
- Maurer, H.R. Bromelain: Biochemistry, pharmacology and medical use. Cell. Mol. Life Sci. 2001, 58, 1234–1245. [Google Scholar] [CrossRef] [PubMed]
- Zhan, J.; Xu, H.; Zhong, Y.; Wu, Q.; Liu, Z. Surface modification of patterned electrospun nanofibrous films via the adhesion of DOPA-bFGF and DOPA-ponericin G1 for skin wound healing. Mater. Des. 2020, 188, 108432. [Google Scholar] [CrossRef]
- Oryan, A.; Alidadi, S.; Moshiri, A.; Maffulli, N. Bone regenerative medicine: Classic options, novel strategies, and future directions. J. Orthop. Surg. Res. 2014, 9, 18. [Google Scholar] [CrossRef]
- Huang, J. Chapter 20—Design and Development of Ceramics and Glasses. In Biology and Engineering of Stem Cell Niches; Vishwakarma, A., Karp, J.M., Eds.; Academic Press: Boston, MA, USA, 2017; pp. 315–329. ISBN 978-0-12-802734-9. [Google Scholar]
- Albrektsson, T.; Johansson, C. Osteoinduction, osteoconduction and osseointegration. Eur. Spine J. 2001, 10, S96–S101. [Google Scholar] [CrossRef]
- Di silvio, L. 15—Bone tissue engineering and biomineralization. In Tissue Engineering Using Ceramics and Polymers; Boccaccini, A.R., Gough, J.E., Eds.; Woodhead Publishing Series in Biomaterials; Woodhead Publishing: Sawston, Cambridge, UK, 2007; pp. 319–331. ISBN 978-1-84569-176-9. [Google Scholar]
- Steeves, A.J.; Atwal, A.; Schock, S.C.; Variola, F. Evaluation of the direct effects of poly(dopamine) on the in vitro response of human osteoblastic cells. J. Mater. Chem. B 2016, 4, 3145–3156. [Google Scholar] [CrossRef]
- Ku, S.H.; Ryu, J.; Hong, S.K.; Lee, H.; Park, C.B. General functionalization route for cell adhesion on non-wetting surfaces. Biomaterials 2010, 31, 2535–2541. [Google Scholar] [CrossRef]
- Ryu, J.; Ku, S.H.; Lee, H.; Park, C.B. Mussel-Inspired Polydopamine Coating as a Universal Route to Hydroxyapatite Crystallization. Adv. Funct. Mater. 2010, 20, 2132–2139. [Google Scholar] [CrossRef]
- Ge, L.; Li, Q.; Huang, Y.; Yang, S.; Ouyang, J.; Bu, S.; Zhong, W.; Liu, Z.; Xing, M.M.Q. Polydopamine-coated paper-stack nanofibrous membranes enhancing adipose stem cells’ adhesion and osteogenic differentiation. J. Mater. Chem. B 2014, 2, 6917–6923. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.-C.; Fu, S.-J. Osteogenesis of human adipose-derived stem cells on poly(dopamine)-coated electrospun poly(lactic acid) fiber mats. Mater. Sci. Eng. C 2016, 58, 254–263. [Google Scholar] [CrossRef]
- Cui, Z.; Lin, J.; Zhan, C.; Wu, J.; Shen, S.; Si, J.; Wang, Q. Biomimetic composite scaffolds based on surface modification of polydopamine on ultrasonication induced cellulose nanofibrils (CNF) adsorbing onto electrospun thermoplastic polyurethane (TPU) nanofibers. J. Biomater. Sci. Polym. Ed. 2020, 31, 561–577. [Google Scholar] [CrossRef] [PubMed]
- Massoumi, B.; Abbasian, M.; Jahanban-Esfahlan, R.; Mohammad-Rezaei, R.; Khalilzadeh, B.; Samadian, H.; Rezaei, A.; Derakhshankhah, H.; Jaymand, M. A novel bio-inspired conductive, biocompatible, and adhesive terpolymer based on polyaniline, polydopamine, and polylactide as scaffolding biomaterial for tissue engineering application. Int. J. Biol. Macromol. 2020, 147, 1174–1184. [Google Scholar] [CrossRef]
- Zuppolini, S.; Cruz-Maya, I.; Guarino, V.; Borriello, A. Optimization of Polydopamine Coatings onto Poly–ε–Caprolactone Electrospun Fibers for the Fabrication of Bio-Electroconductive Interfaces. J. Funct. Biomater. 2020, 11, 19. [Google Scholar] [CrossRef]
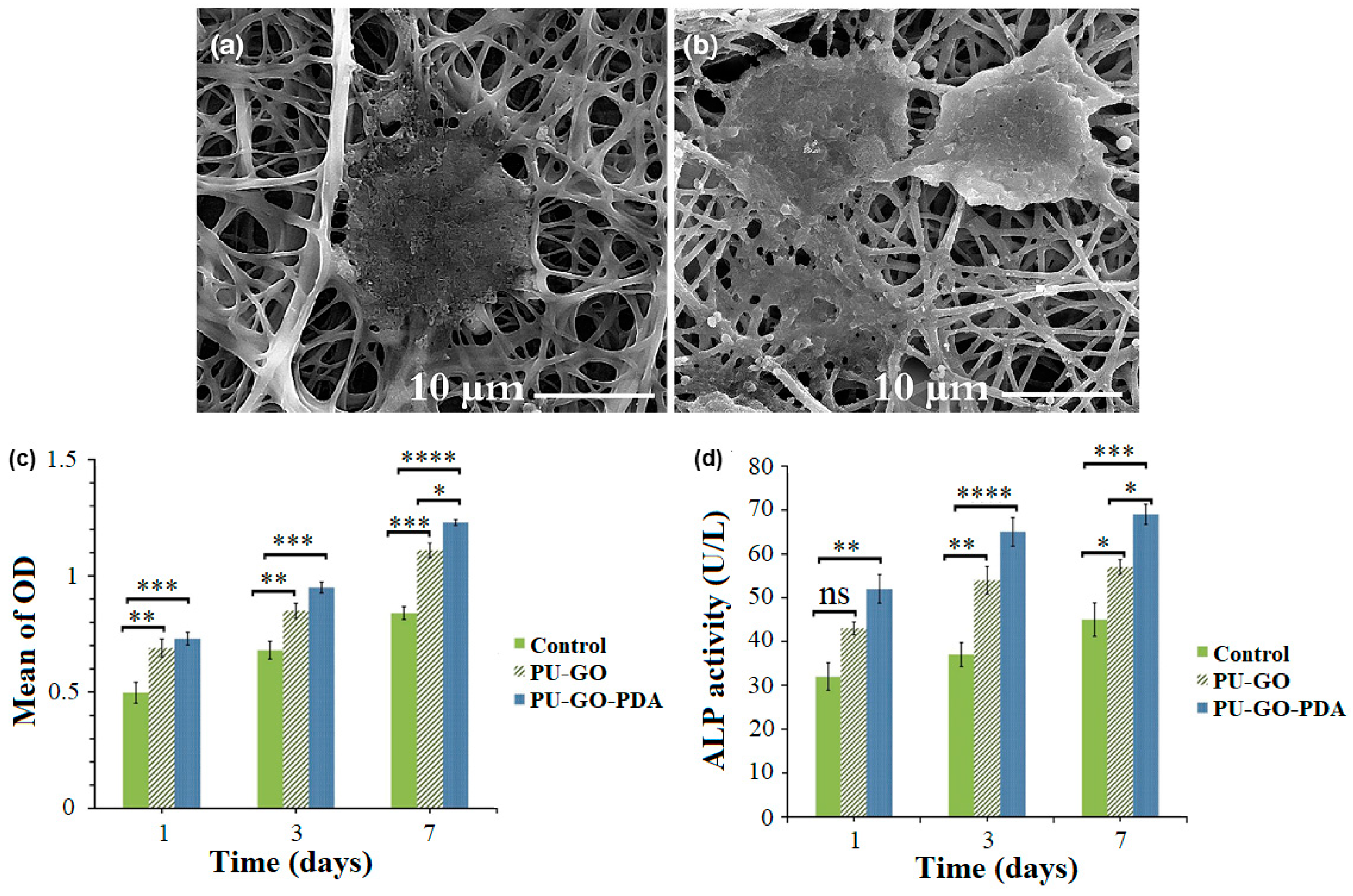
- Ghorbani, F.; Zamanian, A.; Aidun, A. Bioinspired polydopamine coating-assisted electrospun polyurethane-graphene oxide nanofibers for bone tissue engineering application. J. Appl. Polym. Sci. 2019, 136, 47656. [Google Scholar] [CrossRef]
- Hasani-Sadrabadi, M.M.; Sarrion, P.; Nakatsuka, N.; Young, T.D.; Taghdiri, N.; Ansari, S.; Aghaloo, T.; Li, S.; Khademhosseini, A.; Weiss, P.S.; et al. Hierarchically Patterned Polydopamine-Containing Membranes for Periodontal Tissue Engineering. ACS Nano 2019, 13, 3830–3838. [Google Scholar] [CrossRef]
- Bao, X.; Zhao, J.; Sun, J.; Hu, M.; Yang, X. Polydopamine Nanoparticles as Efficient Scavengers for Reactive Oxygen Species in Periodontal Disease. ACS Nano 2018, 12, 8882–8892. [Google Scholar] [CrossRef]
- Jin, L.; Yuan, F.; Chen, C.; Wu, J.; Gong, R.; Yuan, G.; Zeng, H.; Pei, J.; Chen, T. Degradation Products of Polydopamine Restrained Inflammatory Response of LPS-Stimulated Macrophages Through Mediation TLR-4-MYD88 Dependent Signaling Pathways by Antioxidant. Inflammation 2019, 42, 658–671. [Google Scholar] [CrossRef]
- Deng, Y.; Yang, W.-Z.; Shi, D.; Wu, M.; Xiong, X.-L.; Chen, Z.-G.; Wei, S.-C. Bioinspired and osteopromotive polydopamine nanoparticle-incorporated fibrous membranes for robust bone regeneration. NPG Asia Mater. 2019, 11, 1–13. [Google Scholar] [CrossRef]
- Lee, S.J.; Lee, D.; Yoon, T.R.; Kim, H.K.; Jo, H.H.; Park, J.S.; Lee, J.H.; Kim, W.D.; Kwon, I.K.; Park, S.A. Surface modification of 3D-printed porous scaffolds via mussel-inspired polydopamine and effective immobilization of rhBMP-2 to promote osteogenic differentiation for bone tissue engineering. Acta Biomater. 2016, 40, 182–191. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Yang, G.; Johnson, B.N.; Jia, X. Three-dimensional (3D) printed scaffold and material selection for bone repair. Acta Biomater. 2019, 84, 16–33. [Google Scholar] [CrossRef]
- Wang, C.; Huang, W.; Zhou, Y.; He, L.; He, Z.; Chen, Z.; He, X.; Tian, S.; Liao, J.; Lu, B.; et al. 3D printing of bone tissue engineering scaffolds. Bioact. Mater. 2020, 5, 82–91. [Google Scholar] [CrossRef] [PubMed]
- Domingos, M.; Intranuovo, F.; Gloria, A.; Gristina, R.; Ambrosio, L.; Bártolo, P.J.; Favia, P. Improved osteoblast cell affinity on plasma-modified 3-D extruded PCL scaffolds. Acta Biomater. 2013, 9, 5997–6005. [Google Scholar] [CrossRef] [PubMed]
- Bergemann, C.; Cornelsen, M.; Quade, A.; Laube, T.; Schnabelrauch, M.; Rebl, H.; Weißmann, V.; Seitz, H.; Nebe, B. Continuous cellularization of calcium phosphate hybrid scaffolds induced by plasma polymer activation. Mater. Sci. Eng. C 2016, 59, 514–523. [Google Scholar] [CrossRef]
- Cools, P.; Mota, C.; Lorenzo-Moldero, I.; Ghobeira, R.; De Geyter, N.; Moroni, L.; Morent, R. Acrylic Acid Plasma Coated 3D Scaffolds for Cartilage tissue engineering applications. Sci. Rep. 2018, 8, 1–15. [Google Scholar] [CrossRef]
- Sobral, J.M.; Caridade, S.G.; Sousa, R.A.; Mano, J.F.; Reis, R.L. Three-dimensional plotted scaffolds with controlled pore size gradients: Effect of scaffold geometry on mechanical performance and cell seeding efficiency. Acta Biomater. 2011, 7, 1009–1018. [Google Scholar] [CrossRef]
- Teixeira, B.N.; Aprile, P.; Mendonça, R.H.; Kelly, D.J.; Thiré, R.M.d.S.M. Evaluation of bone marrow stem cell response to PLA scaffolds manufactured by 3D printing and coated with polydopamine and type I collagen. J. Biomed. Mater. Res. Part B Appl. Biomater. 2019, 107, 37–49. [Google Scholar] [CrossRef]
- Chen, S.; Zhu, L.; Wen, W.; Lu, L.; Zhou, C.; Luo, B. Fabrication and Evaluation of 3D Printed Poly(l-lactide) Scaffold Functionalized with Quercetin-Polydopamine for Bone Tissue Engineering. ACS Biomater. Sci. Eng. 2019, 5, 2506–2518. [Google Scholar] [CrossRef]
- Xu, Z.; Wang, N.; Liu, P.; Sun, Y.; Wang, Y.; Fei, F.; Zhang, S.; Zheng, J.; Han, B. Poly(Dopamine) Coating on 3D-Printed Poly-Lactic-Co-Glycolic Acid/β-Tricalcium Phosphate Scaffolds for Bone Tissue Engineering. Molecules 2019, 24, 4397. [Google Scholar] [CrossRef] [PubMed]
- Zhong, W.; Li, J.; Hu, C.; Quan, Z.; Jiang, D.; Huang, G.; Wang, Z. 3D-printed titanium implant-coated polydopamine for repairing femoral condyle defects in rabbits. J. Orthop. Surg. Res. 2020, 15, 102. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.J.; Lee, H.-J.; Kim, S.-Y.; Seok, J.M.; Lee, J.H.; Kim, W.D.; Kwon, I.K.; Park, S.-Y.; Park, S.A. In situ gold nanoparticle growth on polydopamine-coated 3D-printed scaffolds improves osteogenic differentiation for bone tissue engineering applications: In vitro and in vivo studies. Nanoscale 2018, 10, 15447–15453. [Google Scholar] [CrossRef] [PubMed]
- Xiang, Z.; Wang, K.; Zhang, W.; Teh, S.W.; Peli, A.; Mok, P.L.; Higuchi, A.; Kumar, S.S. Gold Nanoparticles Inducing Osteogenic Differentiation of Stem Cells: A Review. J. Clust. Sci. 2018, 29, 1–7. [Google Scholar] [CrossRef]
- Gu, X.; Ding, F.; Williams, D.F. Neural tissue engineering options for peripheral nerve regeneration. Biomaterials 2014, 35, 6143–6156. [Google Scholar] [CrossRef]
- Bettinger, C.J.; Bruggeman, J.P.; Misra, A.; Borenstein, J.T.; Langer, R. Biocompatibility of biodegradable semiconducting melanin films for nerve tissue engineering. Biomaterials 2009, 30, 3050–3057. [Google Scholar] [CrossRef]
- Kang, K.; Choi, I.S.; Nam, Y. A biofunctionalization scheme for neural interfaces using polydopamine polymer. Biomaterials 2011, 32, 6374–6380. [Google Scholar] [CrossRef]
- Chen, Y.-W.; Chen, C.-C.; Ng, H.Y.; Lou, C.-W.; Chen, Y.-S.; Shie, M.-Y. Additive Manufacturing of Nerve Decellularized Extracellular Matrix-Contained Polyurethane Conduits for Peripheral Nerve Regeneration. Polymers 2019, 11, 1612. [Google Scholar] [CrossRef]
- Chen, C.-H.; Tsai, C.-C.; Wu, P.-T.; Wang, I.-K.; Yu, J.; Tsai, W.-B. Modulation of Neural Differentiation through Submicron-Grooved Topography Surface with Modified Polydopamine. ACS Appl. Bio Mater. 2019, 2, 205–216. [Google Scholar] [CrossRef]
- Qian, Y.; Song, J.; Zheng, W.; Zhao, X.; Ouyang, Y.; Yuan, W.; Fan, C. 3D Manufacture of Gold Nanocomposite Channels Facilitates Neural Differentiation and Regeneration. Adv. Funct. Mater. 2018, 28, 1707077. [Google Scholar] [CrossRef]
- Qian, Y.; Zhao, X.; Han, Q.; Chen, W.; Li, H.; Yuan, W. An integrated multi-layer 3D-fabrication of PDA/RGD coated graphene loaded PCL nanoscaffold for peripheral nerve restoration. Nat. Commun. 2018, 9, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Pan, S.; Zhao, Y.; Qiao, X.; Qi, Z.; Fu, C.; Kong, W.; Liu, Q.; Yang, X. PLGA porous scaffolds by polydopamine-assisted immobilization of NGF for spinal cord injury repair. Mater. Res. Express 2019, 6, 045024. [Google Scholar] [CrossRef]
- Manchineella, S.; Thrivikraman, G.; Khanum, K.K.; Ramamurthy, P.C.; Basu, B.; Govindaraju, T. Pigmented Silk Nanofibrous Composite for Skeletal Muscle Tissue Engineering. Adv. Healthc. Mater. 2016, 5, 1222–1232. [Google Scholar] [CrossRef] [PubMed]
- Kai, D.; Prabhakaran, M.P.; Jin, G.; Ramakrishna, S. Biocompatibility evaluation of electrically conductive nanofibrous scaffolds for cardiac tissue engineering. J. Mater. Chem. B 2013, 1, 2305–2314. [Google Scholar] [CrossRef]
- Srisuk, P.; Bishi, D.K.; Berti, F.V.; Silva, C.J.R.; Kwon, I.K.; Correlo, V.M.; Reis, R.L. Eumelanin Nanoparticle-Incorporated Polyvinyl Alcohol Nanofibrous Composite as an Electroconductive Scaffold for Skeletal Muscle Tissue Engineering. ACS Appl. Bio Mater. 2018, 1, 1893–1905. [Google Scholar] [CrossRef]
- Jing, X.; Mi, H.-Y.; Napiwocki, B.N.; Peng, X.-F.; Turng, L.-S. Mussel-inspired electroactive chitosan/graphene oxide composite hydrogel with rapid self-healing and recovery behavior for tissue engineering. Carbon 2017, 125, 557–570. [Google Scholar] [CrossRef]





| Materials | Organic Component | Functionality | Application | Ref. |
|---|---|---|---|---|
| SiO2 shell coated/gadolinium-chelated melanin nanoparticles | Synthetic melanin from DA | Heat transduction efficiency | In vivo bimodal MRI/fluorescent imaging | [50] |
| Ag/melanin/SiO2 hybrid nanostructures | Synthetic melanin from DHICA | Photoacoustic properties under long irradiation | PAI | [51] |
| Melanin/TiO2 hybrid nanostructures | Synthetic melanin from DHICA | Reactive oxygen species (ROS) production and bacteria killing | Antimicrobial agents | [22,45,46] |
| Metal ion-loaded synthetic melanin | Synthetic melanin from DA | NIR light absorption | NIR imaging | [52] |
| Metal-bound natural melanin particles | Natural melanin | Enzyme mimicking activity | ROS scavengers and in anti-inflammatory agents | [53] |
| PEGylated-ions doped melanin nanoparticle | Synthetic melanin from DA | Theranostic properties | In vitro and in vivo MRI/computed tomography (CT) imaging agents | [55] |
| Metal ion-synthetic melanin nanoparticles | Synthetic melanin from DA | Metal ion chelating/light absorption ability and photothermal effects | NIR imaging | [52,54,55,56,69,70,87] |
| Gd3+-loading melanin dots | Commercial melanin | Higher T1 relaxivity | PAI | [44,56] |
| PDA gels/nanoparticles | PDA | Photoprotection | Sunscreen | [58,60] |
| Melanin-loaded nanovesicles | Natural melanin | High photothermal conversion | NIR imaging/PTT | [68] |
| Hydrogel scaffolds | Grape extracts oligomeric proanthocyanidins | Photothermal conversion | Melanoma therapy and wound healing | [64] |
| Polymer based-melanin hydrogels | Natural/synthetic melanin | Biocompatibility | Biomedical application | [65,66,67,68] |
| Gold core-melanin shell nanoparticles | Synthetic melanin from DA | Enhanced photoacoustic conversion | PAI | [71] |
| Metal carbonates-melanin nanoparticles | PDA | Metal ion chelating/light absorption ability and photothermal effects | MRI/PTT theranostic agents | [72,73] |
| Melanin-nanoparticles incorporated agar-based composites | Natural melanin from Sepia ink | ROS scavenging | Films with antioxidant activity | [74] |
| CS/melanin-like nanocomposites | Synthetic melanin from DA | ROS scavenging (antioxidants) | Films for food packaging and biomedical packaging | [75] |
| Melanin-like polymer complex | Natural melanins from olive mill wastewaters | High radical scavenging activity | Antioxidant agents | [76] |
| Silk/melanin nanofibrous scaffolds | Commercial melanin | Antioxidant and radical scavenging properties | Nerve tissue engineering | [88] |
| Hybrid silver-loaded/melanin spheres. | Synthetic melanin from DA | ROS generation | Antibacterial agents | [78] |
| Bioinspired coatings | Mussel melanin | Adhesive properties | Active biointerfaces | [85] |
| Poly(norepinephrine) coatings | Norepinephrine polymerization | Biocompatibility and adhesive properties | Human neural stem cells adhesion | [35] |
| DA modified PANI hybrids | Synthetic melanin from DA | Adhesion, dispersibility, and biocompatibility | Conductive platforms in tissue engineering | [86] |
| Matrix | Melanin/Melanin-Like Material | Additives | Experimental Model(s) | Ref. | |
|---|---|---|---|---|---|
| In Vitro | In Vivo | ||||
| PAM, nanoclay | PDA | EGF | NIH-3T3 fibroblasts (mouse) | Full-thickness skin excision (rat) | [94] |
| PEG | PDA | PUE | Dental pulp stem cells, periodontal ligament stem cells | Full-thickness skin excision (rat) | [95] |
| CS/SF | PDA | – | NIH-3T3 fibroblasts (mouse) | Full-thickness skin excision (rat) | [101] |
| Gelatin, carbon nanotubes | PDA | – | L929 fibroblasts (mouse) | Bleeding liver, full-thickness skin excision (mouse) | [102] |
| Hyaluronic acid, GO | PDA | – | L929 fibroblasts (mouse) | Bleeding liver, full-thickness skin excision (mouse) | [97] |
| Nanocellulose | PDA | TH | – | Full-thickness skin excision (rat) | [104] |
| G-C | PDA | Cyp | Normal lung cells (AT-II) (human) | S. aureus-infection model, full-thickness skin excision (mouse) | [105] |
| PNIPAM | PDA | – | NIH-3T3 fibroblasts (mouse) | Full-thickness skin excision (rat) | [96] |
| PANI, PVA | PDA | Silver | – | S. aureus- and E. coli-infected diabetic wound (rat) | [98] |
| PAM, GO | PDA | – | – | Full-thickness skin excision (mouse) | [108] |
| Gellan gum | Eumelanin nanoparticles (Sepia officinalis) | – | Primary keratinocytes (human), C3H/a fibroblast-like cells (mouse) | Subcutaneous implantation (mouse) | [99] |
| SF | PDA | - | L929 fibroblasts (mouse) | Full-thickness skin excision (mouse) | [111] |
| SF | PDA | - | Mesenchymal stem cells (rat) | Full-thickness skin excision (rat) | [112] |
| SF, CS, GO | PDA | - | C2C12 myoblasts (mouse) | Full-thickness skin excision (rat) | [113] |
| PCL | PDA | Bromelain | L929 fibroblasts (mouse) | Full-thickness skin excision (rat) | [114] |
| PLGA | DOPA | bFGF PonG1 | BALB/c 3T3 fibroblasts (mouse embryonic) | Full-thickness skin excision (rat) | [117] |
| Matrix | Melanin/Melanin-Like Material | Additives | Experimental Model(s) | Ref. | |
|---|---|---|---|---|---|
| In Vitro | In Vivo | ||||
| PCL, gelatin | PDA | – | Adipose-derived stem cells (mouse) | – | [125] |
| PLA | PDA | – | Adipose-derived stem cells (human) | – | [126] |
| PU cellulose nanofibers | PDA | – | MC3T3-E1 embryonic osteoblasts (mouse) | – | [127] |
| PANI poly(d,l-lactide) | PDA | – | MC3T3-E1 embryonic osteoblasts (mouse) | – | [128] |
| PCL | PDA | – | Mesenchymal stem cells (human) | – | [129] |
| PU, GO | PDA | MG-63 osteosarcoma cells (human) | – | [130] | |
| PCL | PDA | – | Dental-derived stem cells (human) | Periodontal defect (rat) | [131] |
| PCL | PDA | – | Mesenchymal stem cells (human) | Skull defect (mouse) | [134] |
| PCL | PDA | recombinant human bone morphogenetic protein-2 | MC3T3-E1 embryonic osteoblasts (mouse) | – | [135] |
| PLA, type I collagen | PDA | – | Bone marrow stem cells (pig) | [142] | |
| Poly(lactide) | PDA | quercetin | MC3T3-E1 embryonic osteoblasts (mouse) | – | [143] |
| PLGA/TCP | PDA | – | MC3T3-E1 embryonic osteoblasts (mouse) | Critical size skull defect (mouse) | [144] |
| porous titanium | PDA | – | Femoral condyle defect (rabbit) | [145] | |
| PCL | PDA | GNPs | Adipose-derived stem cells (human) | Skull defect (rabbit) | [146] |
| Matrix | Melanin/Melanin-Like Material | Additives | Experimental Model(s) | Ref. | |
|---|---|---|---|---|---|
| In Vitro | In Vivo | ||||
| – | Synthetic melanin film | – | Schwann cells (rat) | Implantation on top of the sciatic nerve (rat) | [149] |
| Glass, platinum, indium tin oxide | PDA | – | Hippocampal neurons (rat) | – | [150] |
| PU, decellularized ECM | PDA | – | L929 fibroblasts (mouse), Schwann cells (human) | – | [151] |
| Polystyrene | PDA | – | PC12 pheochromocytoma cells (rat), adipose-derived stem cells (human) | – | [152] |
| PCL, gold | PDA | – | Bone marrow stem cells, Schwann cells (rat) | Sciatic nerve dissection (rat) | [153] |
| PCL, graphene | PDA | – | Schwann cells (rat) | Sciatic nerve dissection (rat) | [154] |
| PLGA | PDA | NGF | Neural stem cells (mouse) | Spinal cord injury (rat) | [155] |
| SF | Synthetic melanin | – | SH-SY5Y neuroblastoma cells (human) | – | [88] |
| SF | Synthetic melanin | – | C2C12 myoblast cells (mouse) | – | [156] |
| poly(L-lactide-co-ε-caprolactone), gelatin | Synthetic melanin | – | Cardiac myocytes (human) | – | [157] |
| PVA | Eumelanin nanoparticles from Sepia ink | – | C2C12 myoblast cells (mouse) | – | [158] |
| CS, GO | PDA | – | HEF1 fibroblast cells, cardiomyocytes (human) | – | [159] |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cavallini, C.; Vitiello, G.; Adinolfi, B.; Silvestri, B.; Armanetti, P.; Manini, P.; Pezzella, A.; d’Ischia, M.; Luciani, G.; Menichetti, L. Melanin and Melanin-Like Hybrid Materials in Regenerative Medicine. Nanomaterials 2020, 10, 1518. https://doi.org/10.3390/nano10081518
Cavallini C, Vitiello G, Adinolfi B, Silvestri B, Armanetti P, Manini P, Pezzella A, d’Ischia M, Luciani G, Menichetti L. Melanin and Melanin-Like Hybrid Materials in Regenerative Medicine. Nanomaterials. 2020; 10(8):1518. https://doi.org/10.3390/nano10081518
Chicago/Turabian StyleCavallini, Chiara, Giuseppe Vitiello, Barbara Adinolfi, Brigida Silvestri, Paolo Armanetti, Paola Manini, Alessandro Pezzella, Marco d’Ischia, Giuseppina Luciani, and Luca Menichetti. 2020. "Melanin and Melanin-Like Hybrid Materials in Regenerative Medicine" Nanomaterials 10, no. 8: 1518. https://doi.org/10.3390/nano10081518
APA StyleCavallini, C., Vitiello, G., Adinolfi, B., Silvestri, B., Armanetti, P., Manini, P., Pezzella, A., d’Ischia, M., Luciani, G., & Menichetti, L. (2020). Melanin and Melanin-Like Hybrid Materials in Regenerative Medicine. Nanomaterials, 10(8), 1518. https://doi.org/10.3390/nano10081518












