Short-Term Bone Healing in Anterior Maxillary Sockets Using L-PRF With or Without Synthetic HA/β-TCP: A Randomized Clinical Trial
Abstract
1. Introduction
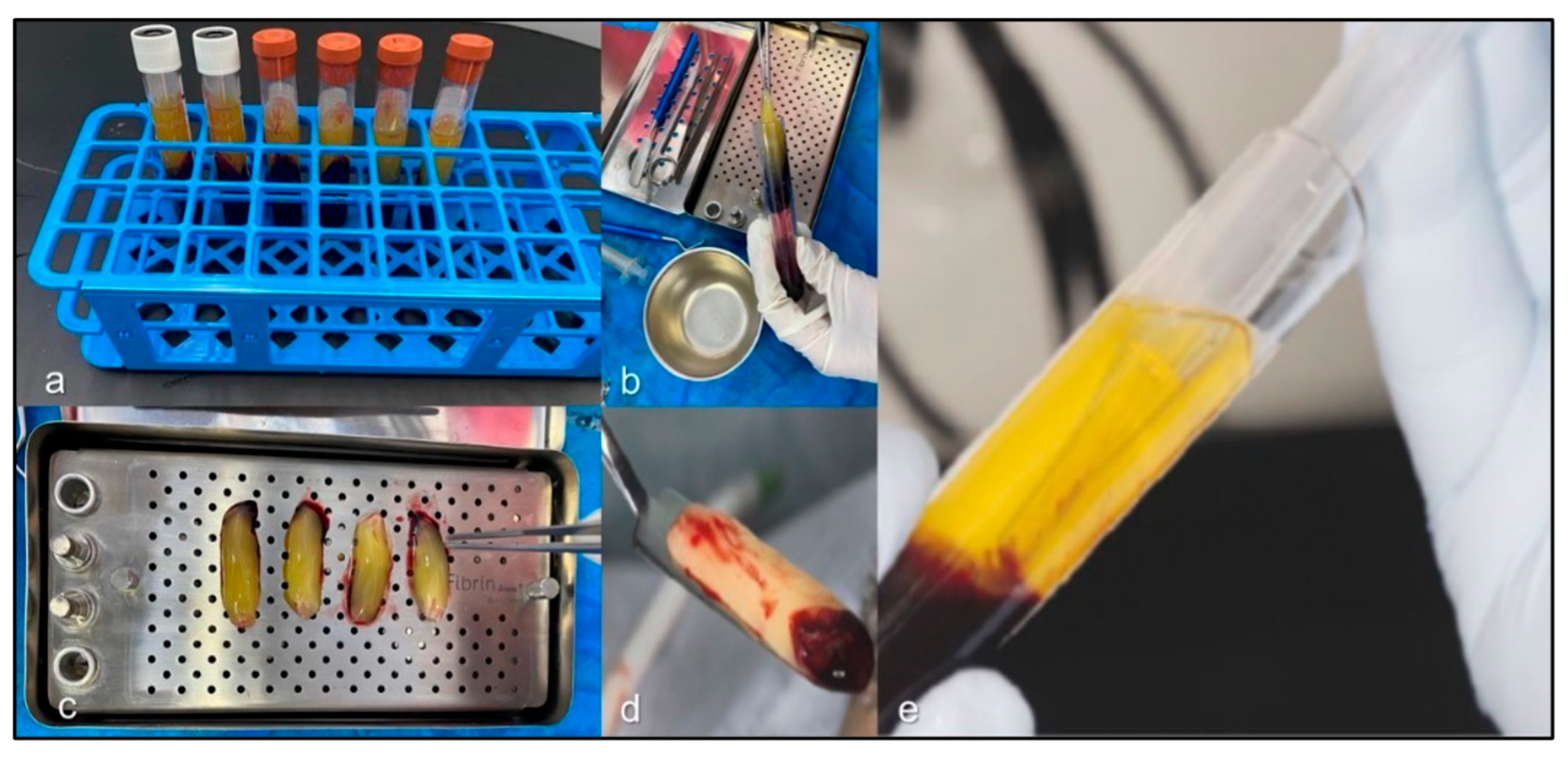
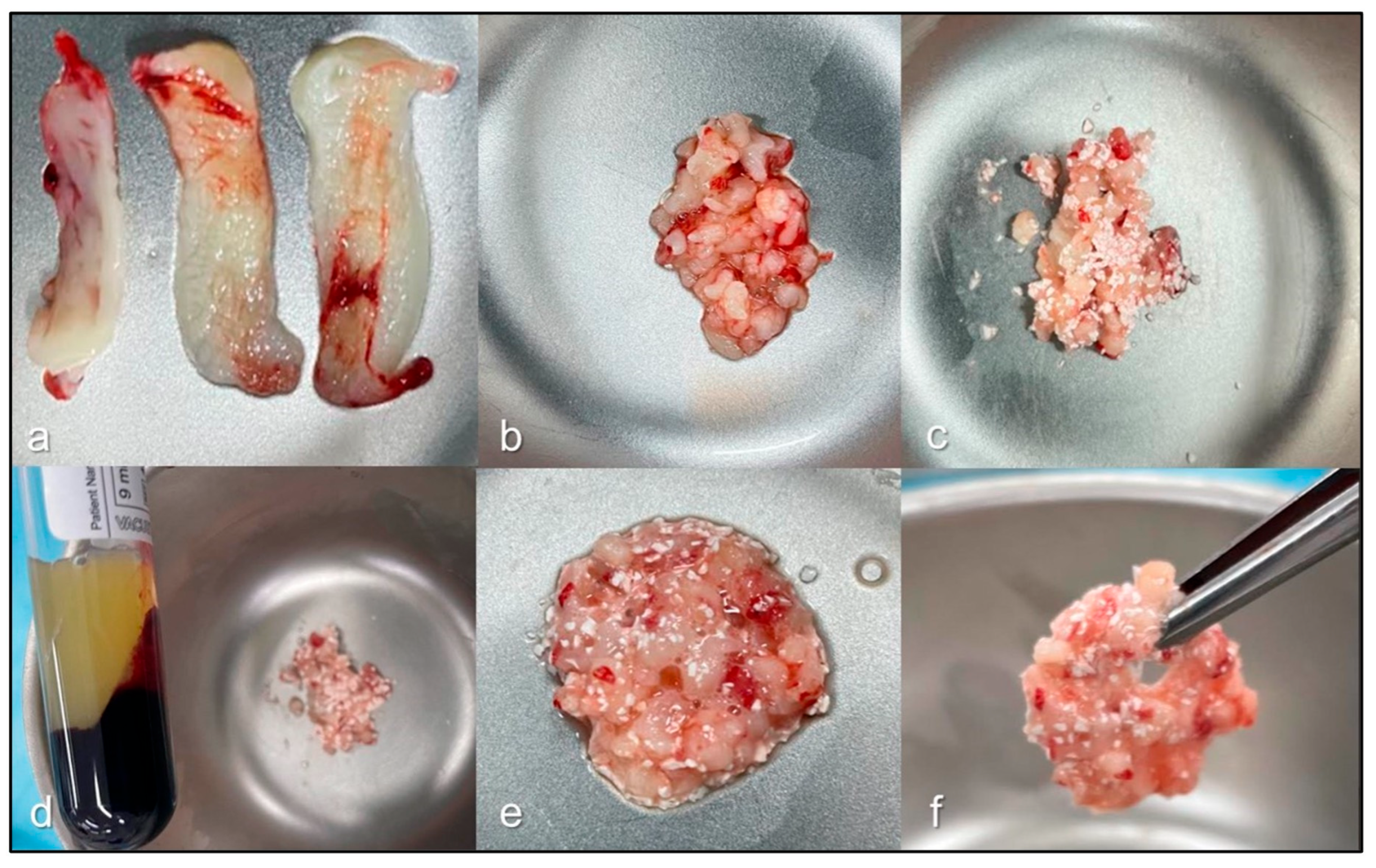
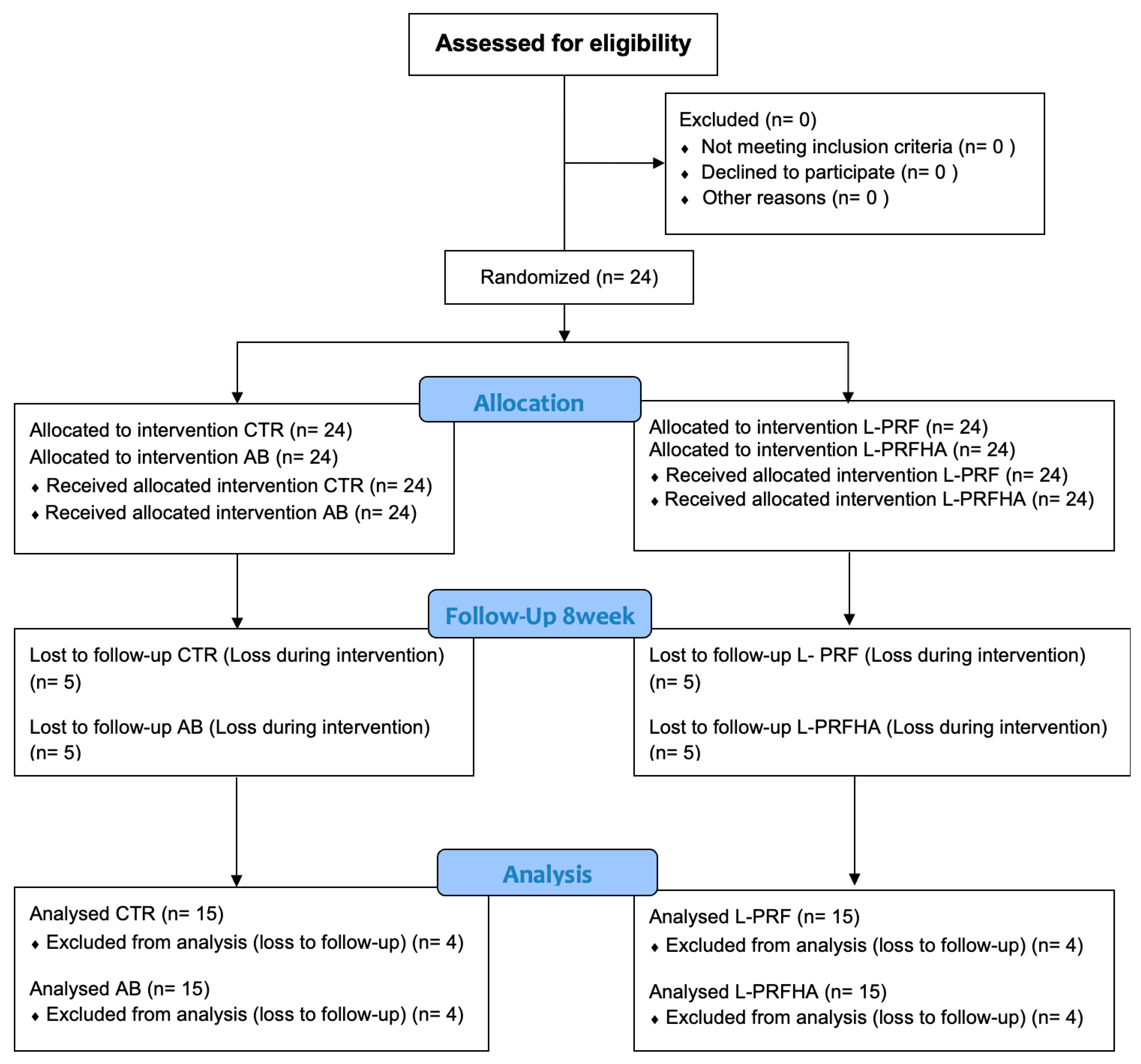
2. Materials and Methods
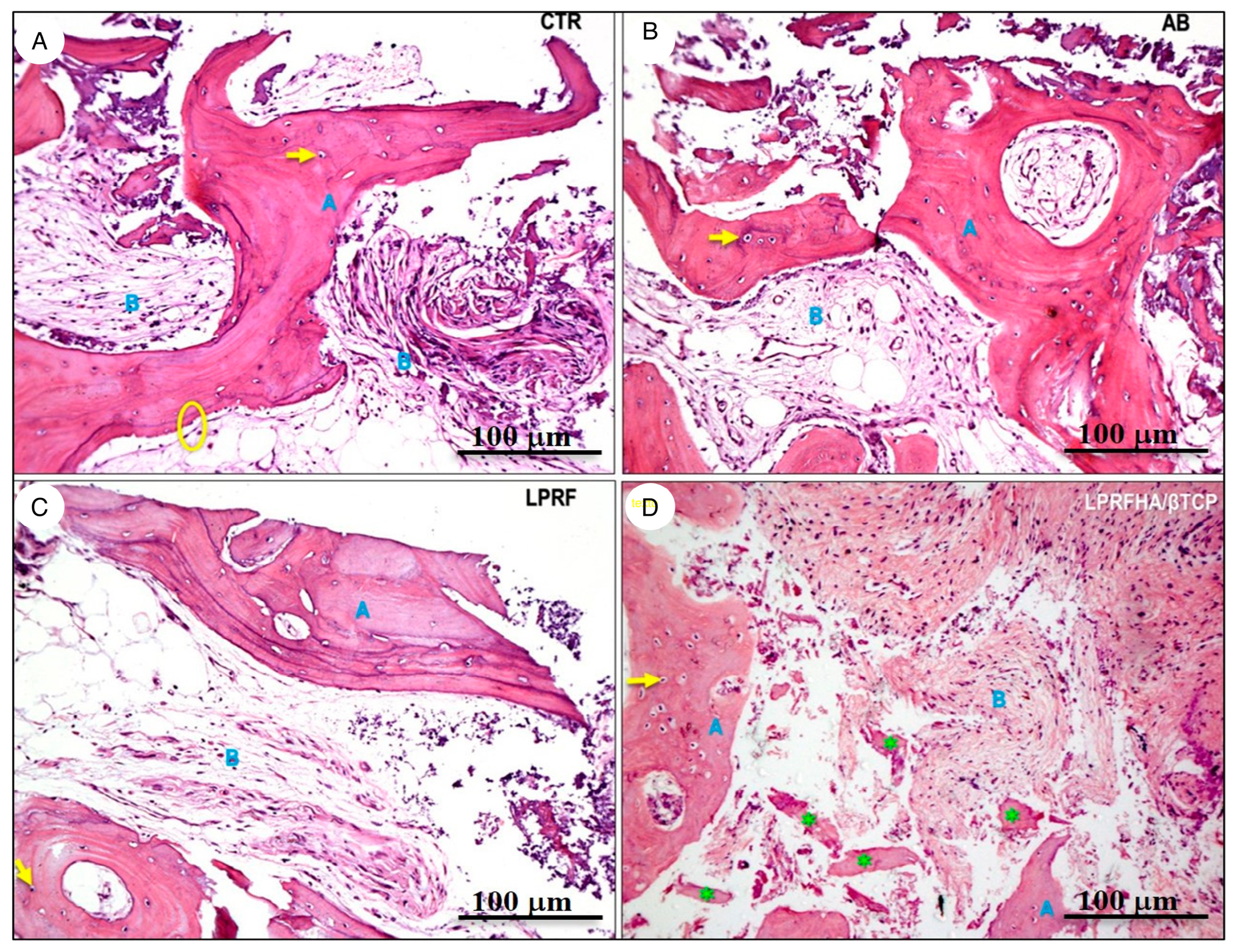
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Alghamdi, H.S. Methods to Improve Osseointegration of Dental Implants in Low Quality (Type-IV) Bone: An Overview. J. Funct. Biomater. 2018, 9, 7. [Google Scholar] [CrossRef]
- Chappuis, V.; Engel, O.; Reyes, M.; Shahim, K.; Nolte, L.P.; Buser, D. Ridge alterations post-extraction in the esthetic zone: A 3D analysis with CBCT. J. Dent. Res. 2013, 92, 195–201. [Google Scholar] [CrossRef]
- De Angelis, P.; De Angelis, S.; Passarelli, P.C.; Liguori, M.G.; Manicone, P.F.; D’Addona, A. Hard and Soft Tissue Evaluation of Different Socket Preservation Procedures Using Leukocyte and Platelet-Rich Fibrin: A Retrospective Clinical and Volumetric Analysis. J. Oral Maxillofac. Surg. 2019, 77, 1807–1815. [Google Scholar] [CrossRef] [PubMed]
- Dipalma, G.; Inchingolo, A.M.; Colonna, V.; Marotti, P.; Carone, C.; Ferrante, L.; Inchingolo, F.; Palermo, A.; Inchingolo, A.D. Autologous and Heterologous Minor and Major Bone Regeneration with Platelet-Derived Growth Factors. J. Funct. Biomater. 2025, 16, 16. [Google Scholar] [CrossRef] [PubMed]
- Janjua, O.S.; Qureshi, S.M.; Shaikh, M.S.; Alnazzawi, A.; Rodriguez-Lozano, F.J.; Pecci-Lloret, M.P.; Zafar, M.S. Autogenous Tooth Bone Grafts for Repair and Regeneration of Maxillofacial Defects: A Narrative Review. Int. J. Environ. Res. Public Health 2022, 19, 3690. [Google Scholar] [CrossRef] [PubMed]
- Zhao, R.; Yang, R.; Cooper, P.R.; Khurshid, Z.; Shavandi, A.; Ratnayake, J. Bone Grafts and Substitutes in Dentistry: A Review of Current Trends and Developments. Molecules 2021, 26, 3007. [Google Scholar] [CrossRef]
- Yang, N.; Liu, Y. The Role of the Immune Microenvironment in Bone Regeneration. Int. J. Med. Sci. 2021, 18, 3697–3707. [Google Scholar] [CrossRef]
- Sohn, H.S.; Oh, J.K. Review of bone graft and bone substitutes with an emphasis on fracture surgeries. Biomater. Res. 2019, 23, 9. [Google Scholar] [CrossRef]
- Choukroun, J.; Diss, A.; Simonpieri, A.; Girard, M.O.; Schoeffler, C.; Dohan, S.L.; Dohan, A.J.; Mouhyi, J.; Dohan, D.M. Platelet-rich fibrin (PRF): A second-generation platelet concentrate. Part V: Histologic evaluations of PRF effects on bone allograft maturation in sinus lift. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2006, 101, 299–303. [Google Scholar] [CrossRef]
- Choukroun, J.; Diss, A.; Simonpieri, A.; Girard, M.O.; Schoeffler, C.; Dohan, S.L.; Dohan, A.J.; Mouhyi, J.; Dohan, D.M. Platelet-rich fibrin (PRF): A second-generation platelet concentrate. Part IV: Clinical effects on tissue healing. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2006, 101, e56–e60. [Google Scholar] [CrossRef]
- Zhao, J.H.; Tsai, C.H.; Chang, Y.C. Clinical application of platelet-rich fibrin as the sole grafting material in maxillary sinus augmentation. J. Formos. Med. Assoc. 2015, 114, 779–780. [Google Scholar] [CrossRef]
- Canellas, J.V.D.S.; da Costa, R.C.; Breves, R.C.; de Oliveira, G.P.; Figueredo, C.M.D.S.; Fischer, R.G.; Thole, A.A.; Medeiros, P.J.D.; Ritto, F.G. Tomographic and histomorphometric evaluation of socket healing after tooth extraction using leukocyte- and platelet-rich fibrin: A randomized, single-blind, controlled clinical trial. J. Craniomaxillofac. Surg. 2020, 48, 24–32. [Google Scholar] [CrossRef] [PubMed]
- Walia, K.D.; Belludi, S.A.; Pradhan, N.; Jain, V.; Shaik, S. Evaluation of Platelet-Rich Fibrin Matrix as a Regenerative Material in the Surgical Management of Human Periodontal Intraosseous Defects—A Randomized Controlled Trial. Contemp. Clin. Dent. 2022, 13, 9–17. [Google Scholar] [CrossRef]
- Nacopoulos, C.; Dontas, I.; Lelovas, P.; Galanos, A.; Vesalas, A.M.; Raptou, P.; Mastoris, M.; Chronopoulos, E.; Papaioannou, N. Enhancement of bone regeneration with the combination of platelet-rich fibrin and synthetic graft. J. Craniofac. Surg. 2014, 25, 2164–2168. [Google Scholar] [CrossRef] [PubMed]
- Galav, S.; Chandrashekar, K.T.; Mishra, R.; Tripathi, V.; Agarwal, R.; Galav, A. Comparative evaluation of platelet-rich fibrin and autogenous bone graft for the treatment of infrabony defects in chronic periodontitis: Clinical, radiological, and surgical reentry. Indian J. Dent. Res. 2016, 27, 502–507. [Google Scholar] [CrossRef]
- Weingart, D.; Chen, S.T. International Team for Implantology (ITI). In Proceedings of the 4th International Team for Implantology (ITI) Consensus Conference, Stuttgart, Germany, 26–28 August 2008; Quintessence Publishing: Batavia, IL, USA, 2009; Volume 24, pp. 7–278. [Google Scholar]
- Caplanis, N.; Lozada, J.L.; Kan, J.Y. Extraction defect assessment, classification, and management. J. Calif. Dent. Assoc. 2005, 33, 853–863. [Google Scholar] [CrossRef]
- Sheikh, Z.; Sima, C.; Glogauer, M. Bone Replacement Materials and Techniques Used for Achieving Vertical Alveolar Bone Augmentation. Materials 2015, 8, 2953–2993. [Google Scholar] [CrossRef]
- Wang, W.; Yeung, K.W.K. Bone grafts and biomaterials substitutes for bone defect repair: A review. Bioact. Mater. 2017, 2, 224–247. [Google Scholar] [CrossRef] [PubMed]
- Montero, J.; Becerro, A.; Dib, A.; Quispe-López, N.; Borrajo, J.; Benito Garzón, L. Preliminary results of customized bone graft made by robocasting hydroxyapatite and tricalcium phosphates for oral surgery. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2023, 135, 192–203. [Google Scholar] [CrossRef]
- Kucko, S.K.; Raeman, S.M.; Keenan, T.J. Current Advances in Hydroxyapatite- and β-Tricalcium Phosphate-Based Composites for Biomedical Applications: A Review. Biomed. Mater. Devices 2023, 1, 49–65. [Google Scholar] [CrossRef]
- Helaehil, J.V.; Huang, B.; Bartolo, P.; Santamaria, M., Jr.; Caetano, G.F. Bone regeneration: The influence of composite HA/TCP scaffolds and electrical stimulation on TGF/BMP and RANK/RANKL/OPG pathways. Injury 2025, 56, 112158. [Google Scholar] [CrossRef]
- Acar, A.H.; Yolcu, Ü.; Gül, M.; Keleş, A.; Erdem, N.F.; Altundag Kahraman, S. Micro-computed tomography and histomorphometric analysis of the effects of platelet-rich fibrin on bone regeneration in the rabbit calvarium. Arch. Oral Biol. 2015, 60, 606–614. [Google Scholar] [CrossRef]
- Oliveira, M.R.; deC Silva, A.; Ferreira, S.; Avelino, C.C.; Garcia, I.R., Jr.; Mariano, R.C. Influence of the association between platelet-rich fibrin and bovine bone on bone regeneration. A histomorphometric study in the calvaria of rats. Int. J. Oral Maxillofac. Surg. 2015, 44, 649–655. [Google Scholar] [CrossRef]
- Maia, P.W.; Teixeira, M.L.; Scavone de Macedo, L.G.; Aloise, A.C.; Passos Junior, C.A.; Aragoneses, J.M.; Calvo-Guirado, J.L.; Pelegrine, A.A. Use of Platelet-Rich Fibrin Associated with Xenograft in Critical Bone Defects: Histomorphometric Study in Rabbits. Symmetry 2019, 11, 1293. [Google Scholar] [CrossRef]
- Baghele, O.; Thorat, M.; Malpani, P. Clinical and radiographic evaluation of platelet-rich fibrin and bone graft material (β-tricalcium phosphate + hydroxyapatite) in the treatment of intrabony defects of periodontitis patients: A randomized controlled trial. Quintessence Int. 2023, 54, 472–483. [Google Scholar]
- Gaur, S.; Chugh, A.; Chaudhry, K.; Bajpayee, A.; Jain, G.; Chugh, V.K.; Kumar, P.; Singh, S. Efficacy and Safety of Concentrated Growth Factors and Platelet- Rich Fibrin on Stability and Bone Regeneration in Patients with Immediate Dental Implants: A Randomized Controlled Trial. Int. J. Oral Maxillofac. Implant. 2022, 37, 784–792. [Google Scholar] [CrossRef]
- Anapu, M.P.; Atluri, K.R.; Chandra Tripuraneni, S.; Issrani, R.; Bader, A.K.; Alkhalaf, Z.A.; Sghaireen, M.G.; Prabhu, N.; Rbea Dh Alshammari, R.; Khalid, G.; et al. Evaluation of effect on stability of implants with and without platelet rich fibrin using a resonance frequency analyzer—An in-vivo study. Heliyon 2024, 10, e27971. [Google Scholar] [CrossRef] [PubMed]
- Elsheikh, H.A.; Abdelsameaa, S.E.; Elbahnasi, A.A.; Abdel-Rahman, F.H. Comparison between platelet rich fibrin as space filling material versus xenograft and alloplastic bone grafting materials in immediate implant placement: A randomized clinical trial. BMC Oral Health 2023, 23, 977. [Google Scholar] [CrossRef] [PubMed]
- Shahbaz-Alam, M.; Dhiman, A.; Jain, V.; Bhutia, O.; Pruthi, G. Vertical Bone Implant Contact Around Anterior Immediate Implants and Their Stability After Using Either Alloplast or L-PRF or Both in Peri-Implant Gap: A Prospective Randomized Trial. J. Maxillofac. Oral Surg. 2022, 21, 533–541. [Google Scholar] [CrossRef]
- Giammarinaro, E.; Baldini, N.; Covani, U.; Menini, M.; Pesce, P.; Marconcini, S. Does platelet-rich fibrin enhance the outcomes of peri-implant soft tissues? A systematic review. BMC Oral Health 2025, 25, 615. [Google Scholar] [CrossRef]
- Miron, R.J.; Moraschini, V.; Del Fabbro, M.; Piattelli, A.; Fujioka-Kobayashi, M.; Zhang, Y.; Saulacic, N.; Schaller, B.; Kawase, T.; Cosgarea, R.; et al. Use of platelet-rich fibrin for the treatment of gingival recessions: A systematic review and meta-analysis. Clin. Oral Investig. 2020, 24, 2543–2557. [Google Scholar] [CrossRef]
- Hajibagheri, P.; Basirat, M.; Tabari-Khomeiran, Z.; Asadi-Aria, A. The efficacy of platelet-rich fibrin (PRF) in post-extraction hard and soft tissue healing and associated complications: A systematic review and meta-analysis of split-mouth randomized clinical trials. BMC Oral Health 2025, 25, 869. [Google Scholar] [CrossRef]
- Castro, A.B.; Meschi, N.; Temmerman, A.; Pinto, N.; Lambrechts, P.; Teughels, W.; Quirynen, M. Regenerative potential of leucocyte- and platelet-rich fibrin. Part B: Sinus floor elevation, alveolar ridge preservation and implant therapy. A systematic review. J. Clin. Periodontol. 2017, 44, 225–234. [Google Scholar] [CrossRef]
- Ustaoğlu, G.; Göller Bulut, D.; Gümüş, K.Ç. Evaluation of different platelet-rich concentrates effects on early soft tissue healing and socket preservation after tooth extraction. J. Stomatol. Oral Maxillofac. Surg. 2020, 121, 539–544. [Google Scholar] [CrossRef] [PubMed]
- Abdullah, W.A. Evaluation of bone regenerative capacity in rats claverial bone defect using platelet rich fibrin with and without beta tri calcium phosphate bone graft material. Saudi Dent. J. 2016, 28, 109–117. [Google Scholar] [CrossRef]
- Clark, D.; Rajendran, Y.; Paydar, S.; Ho, S.; Cox, D.; Ryder, M.; Dollard, J.; Kao, R.T. Advanced platelet-rich fibrin and freeze-dried bone allograft for ridge preservation: A randomized controlled clinical trial. J. Periodontol. 2018, 89, 379–387. [Google Scholar] [CrossRef]
- Wei, L.; Sun, Y.; Yu, D.; Pieterse, H.; Wismeijer, D.; Liu, Y.; Wu, Y. The Clinical Efficacy and Safety of ErhBMP-2/BioCaP/β-TCP as a Novel Bone Substitute Using the Tooth-Extraction-Socket-Healing Model: A Proof-of-Concept Randomized Controlled Trial. J. Clin. Periodontol. 2025, 52, 299–309. [Google Scholar] [CrossRef] [PubMed]
- Kollati, P.; Koneru, S.; Dwarakanath, C.D.; Gottumukkala, S.N.V.S. Effectiveness of naturally derived bovine hydroxyapatite (Cerabone™) combined with platelet-rich fibrin matrix in socket preservation: A randomized controlled clinical trial. J. Indian Soc. Periodontol. 2019, 23, 145–151. [Google Scholar] [CrossRef] [PubMed]
- Brouwers, J.E.I.G.; van der Vorm, L.N.; Buis, S.; Haumann, R.; Karanzai, A.; Konings, J.; de Groot, P.G.; de Laat, B.; Remijn, J.A. Implant stability in patients treated with platelet-rich fibrin and bovine bone substitute for alveolar ridge preservation is associated with peripheral blood cells and coagulation factors. Clin. Exp. Dent. Res. 2020, 6, 236–243. [Google Scholar] [CrossRef]
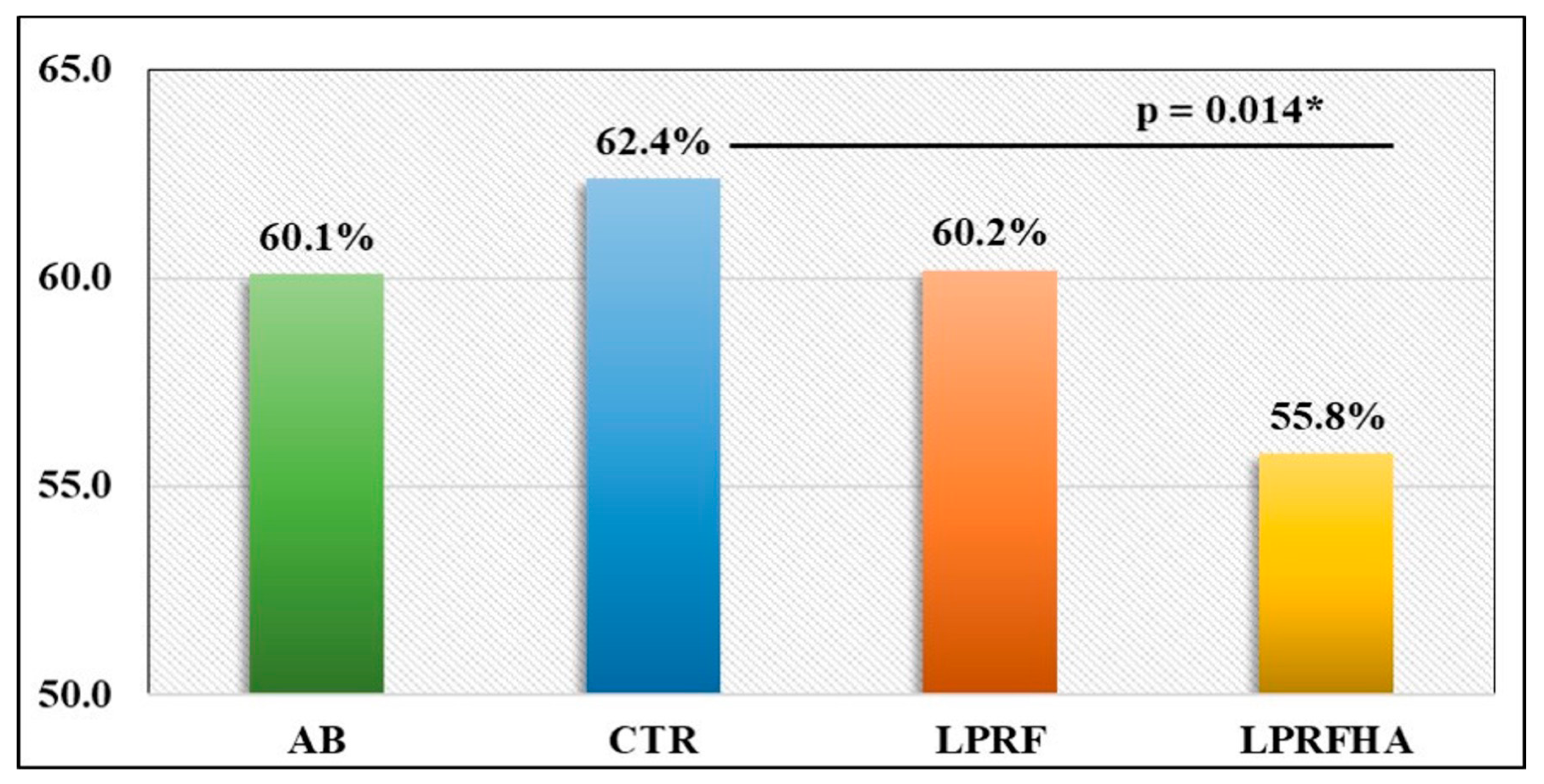
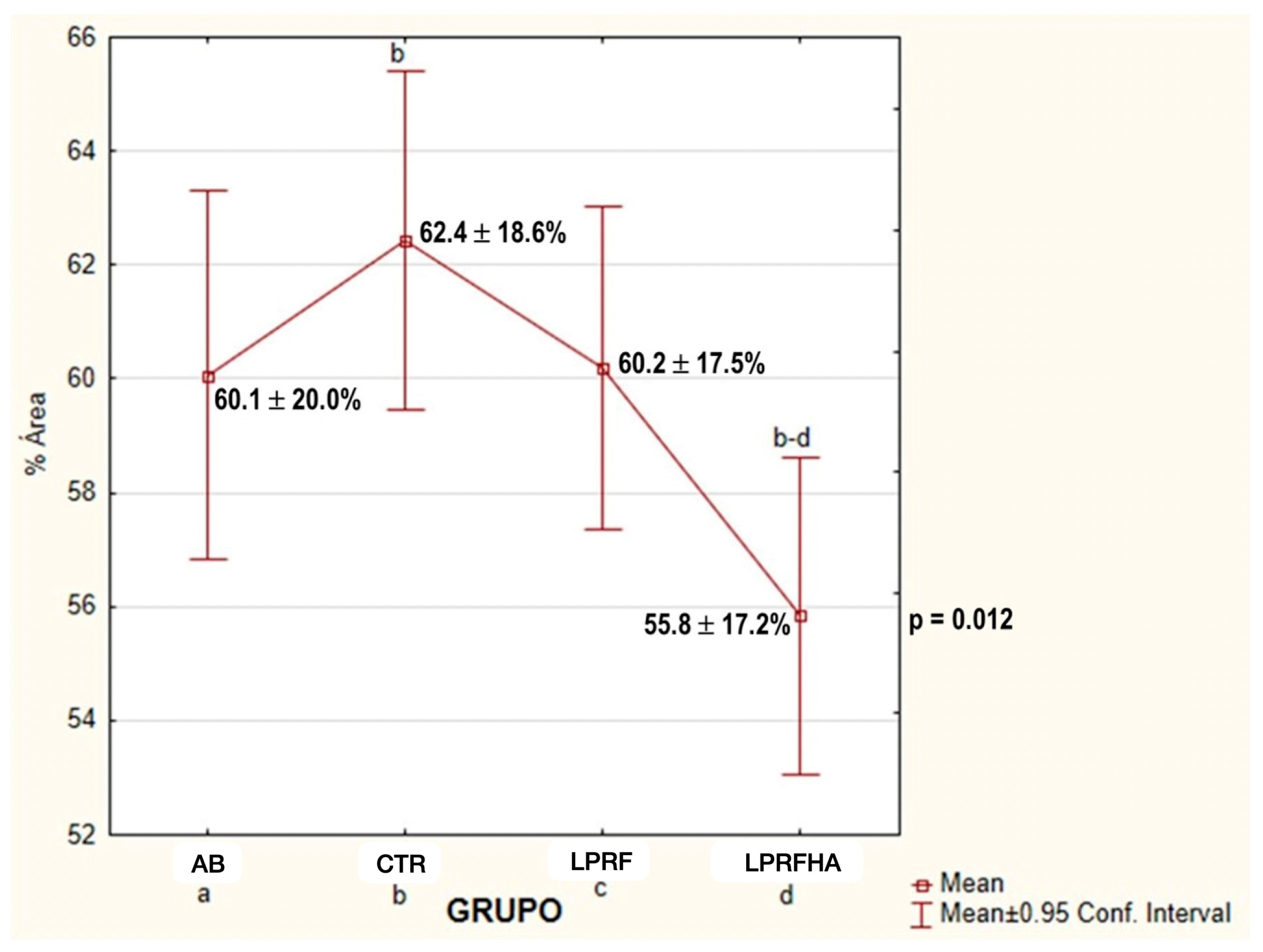
| Grupos | NBF (%) | p-Value | ||
|---|---|---|---|---|
| Mean ± SD | Median | Minimum–Maximum | ||
| AB | 60.1 ± 20.0 | 58.4 | 15.6–99.2 | 0.014 * |
| CTR | 62.4 ± 18.6 * | 64.2 | 21.6–97.6 | |
| LPRF | 60.2 ± 17.5 | 63.8 | 17.2–92.9 | |
| LPRFHA | 55.8 ± 17.2 * | 54.9 | 12.7–96.1 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.
Share and Cite
Gusmão, P.d.S.; Silva, C.P.d.; Ravelo, V.; Nagato, A.C.; Olate, S.; Duque, H. Short-Term Bone Healing in Anterior Maxillary Sockets Using L-PRF With or Without Synthetic HA/β-TCP: A Randomized Clinical Trial. J. Funct. Biomater. 2026, 17, 6. https://doi.org/10.3390/jfb17010006
Gusmão PdS, Silva CPd, Ravelo V, Nagato AC, Olate S, Duque H. Short-Term Bone Healing in Anterior Maxillary Sockets Using L-PRF With or Without Synthetic HA/β-TCP: A Randomized Clinical Trial. Journal of Functional Biomaterials. 2026; 17(1):6. https://doi.org/10.3390/jfb17010006
Chicago/Turabian StyleGusmão, Pricila da Silva, Cássia Pereira da Silva, Víctor Ravelo, Akinori Cardozo Nagato, Sergio Olate, and Henrique Duque. 2026. "Short-Term Bone Healing in Anterior Maxillary Sockets Using L-PRF With or Without Synthetic HA/β-TCP: A Randomized Clinical Trial" Journal of Functional Biomaterials 17, no. 1: 6. https://doi.org/10.3390/jfb17010006
APA StyleGusmão, P. d. S., Silva, C. P. d., Ravelo, V., Nagato, A. C., Olate, S., & Duque, H. (2026). Short-Term Bone Healing in Anterior Maxillary Sockets Using L-PRF With or Without Synthetic HA/β-TCP: A Randomized Clinical Trial. Journal of Functional Biomaterials, 17(1), 6. https://doi.org/10.3390/jfb17010006







