Clinical Efficacy of Clear Aligners in Class II Malocclusion: From Pediatric to Adult Cases–A Narrative Review
Abstract
1. Introduction
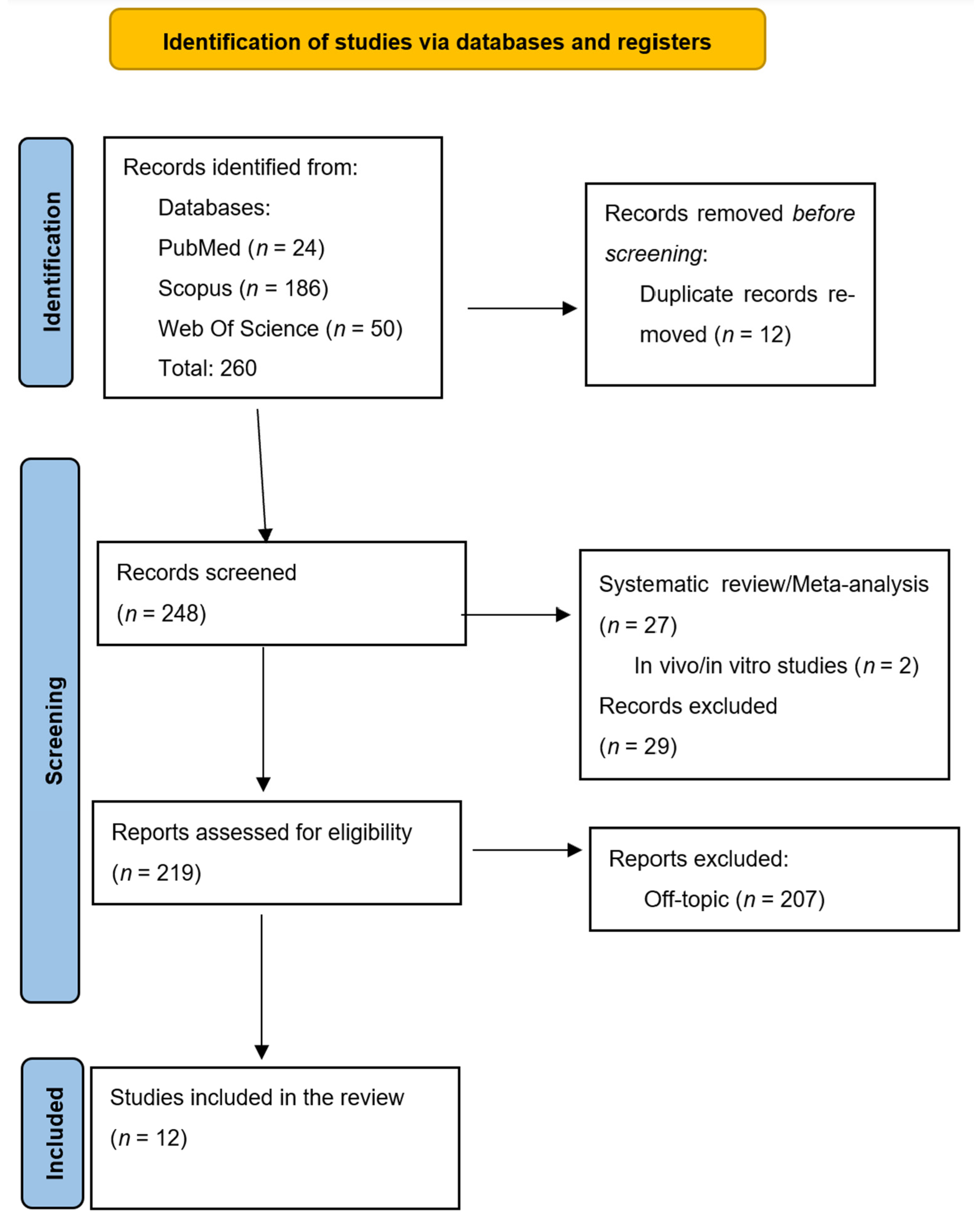
2. Materials and Methods
Search Process
3. Results
Quality Assessment and Risk of Bias of Included Articles
4. Discussion
4.1. Control of Mandibular Incisor Proclination
4.2. Deep Bite Correction and Vertical Movements
4.3. Torque Movements and Three-Dimensional Control
4.4. Class II Correction and Molar Distalization
4.5. Determinants of Predictability and the Role of Auxiliaries
4.6. Broader Considerations and Future Perspectives
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| Abbreviation | Definition |
| Class II | Class II (malocclusions according to Angle’s classification) |
| CAD/CAM | Computer-Aided Design/Computer-Aided Manufacturing |
| CBCT | Cone Beam Computed Tomography |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
| CAT | Clear aligner therapy |
| CAG | Clear Aligner Group |
| TADs | Temporary anchorage devices |
| CAD-CAM | Computer-Aided Design/Computer-Aided Manufacturing |
| OHRQoL | Oral-Health-Related Quality of Life |
| OJ | Overjet |
| OB | Overbite |
| TMD | Temporomandibular Disorder |
| CR | Centric Relation |
| MI | Maximum Intercuspation |
| VTO | Visual Treatment Objective |
| G8 | Invisalign G8 Protocol |
| PG | Pendulum Group |
| IBs | Intrusion bulbs |
| LII | Little’s Irregularity Index |
References
- Hakim, M.A.A.; Khatab, N.M.A.; Mohamed, K.M.G.; Elheeny, A.A.H. A Comparative Three-Dimensional Finite Element Study of Two Space Regainers in the Mixed Dentition Stage. Eur. J. Dent. 2020, 14, 107–114. [Google Scholar] [CrossRef][Green Version]
- Ke, Y.; Zhu, Y.; Zhu, M. A Comparison of Treatment Effectiveness between Clear Aligner and Fixed Appliance Therapies. BMC Oral Health 2019, 19, 24. [Google Scholar] [CrossRef]
- Amro, H.; Najjar, S.; Owda, M.; Elayyan, F. A Comprehensive National Survey on Malocclusion Prevalence among Palestinian Children. BMC Oral Health 2024, 24, 664. [Google Scholar] [CrossRef]
- Jiang, T.; Jiang, Y.-N.; Chu, F.-T.; Lu, P.-J.; Tang, G.-H. A Cone-Beam Computed Tomographic Study Evaluating the Efficacy of Incisor Movement with Clear Aligners: Assessment of Incisor Pure Tipping, Controlled Tipping, Translation, and Torque. Am. J. Orthod. Dentofac. Orthop. 2021, 159, 635–643. [Google Scholar] [CrossRef]
- Hennessy, J.; Garvey, T.; Al-Awadhi, E.A. A Randomized Clinical Trial Comparing Mandibular Incisor Proclination Produced by Fixed Labial Appliances and Clear Aligners. Angle Orthod. 2016, 86, 706–712. [Google Scholar] [CrossRef]
- Meade, M.J.; Weir, T. A Survey of Orthodontic Clear Aligner Practices among Orthodontists. Am. J. Orthod. Dentofac. Orthop. 2022, 162, e302–e311. [Google Scholar] [CrossRef]
- Keilig, L.; Fittgen, A.; Schneider, H.; Sifa, R.; Schwarze, J.; Bourauel, C.; Konermann, A. Accuracy of Digital Orthodontic Treatment Planning: Assessing Aligner-Directed Tooth Movements and Exploring Inherent Intramaxillary Side Effects. J. Clin. Med. 2024, 13, 2298. [Google Scholar] [CrossRef]
- Krieger, E.; Seiferth, J.; Saric, I.; Jung, B.A.; Wehrbein, H. Accuracy of Invisalign® Treatments in the Anterior Tooth Region. J. Orofac. Orthop. 2011, 72, 141–149. [Google Scholar] [CrossRef]
- Bollen, A.-M.; Huang, G.; King, G.; Hujoel, P.; Ma, T. Activation Time and Material Stiffness of Sequential Removable Orthodontic Appliances. Part 1: Ability to Complete Treatment. Am. J. Orthod. Dentofac. Orthop. 2003, 124, 496–501. [Google Scholar] [CrossRef]
- Baldwin, D.K.; King, G.; Ramsay, D.S.; Huang, G.; Bollen, A.-M. Activation Time and Material Stiffness of Sequential Removable Orthodontic Appliances. Part 3: Premolar Extraction Patients. Am. J. Orthod. Dentofacial Orthop. 2008, 133, 837–845. [Google Scholar] [CrossRef]
- Bridges, T.; King, G.; Mohammed, A. The Effect of Age on Tooth Movement and Mineral Density in the Alveolar Tissues of the Rat. Am. J. Orthod. Dentofacial Orthop. 1988, 93, 245–250. [Google Scholar] [CrossRef]
- Springate, S.D. The Effect of Sample Size and Bias on the Reliability of Estimates of Error: A Comparative Study of Dahlberg’s Formula. Eur. J. Orthod. 2012, 34, 158–163. [Google Scholar] [CrossRef]
- The Effectiveness of Pendulum, K-Loop, and Distal Jet Distalization Techniques in Growing Children and Its Effects on Anchor Unit: A Comparative Study. Available online: https://www.researchgate.net/publication/309921892_The_effectiveness_of_pendulum_K-loop_and_distal_jet_distalization_techniques_in_growing_children_and_its_effects_on_anchor_unit_A_comparative_study (accessed on 23 July 2025).
- Hilgers, J.J. The Pendulum Appliance for Class II Non-Compliance Therapy. J. Clin. Orthod. 1992, 26, 706–714. [Google Scholar]
- Kesling, H.D. The Philosophy of the Tooth Positioning Appliance. Am. J. Orthod. Oral Surg. 1945, 31, 297–304. [Google Scholar] [CrossRef]
- Lucchese, A.; Pilolli, G.P.; Petruzzi, M.; Crincoli, V.; Scivetti, M.; Favia, G. Analysis of Collagen Distribution in Human Crown Dentin by Confocal Laser Scanning Microscopy. Ultrastruct. Pathol. 2008, 32, 107–111. [Google Scholar] [CrossRef]
- Tortarolo, A.; Rotolo, R.; Nucci, L.; Tepedino, M.; Crincoli, V.; Piancino, M.G. Condylar Asymmetry in Children with Unilateral Posterior Crossbite Malocclusion: A Comparative Cross-Sectional Study. Children 2022, 9, 1772. [Google Scholar] [CrossRef]
- Giancotti, A.; Mampieri, G.; Greco, M. Correction of Deep Bite in Adults Using the Invisalign System. J. Clin. Orthod. 2008, 42, 719–726, quiz 728. [Google Scholar]
- Crincoli, V.; Ballini, A.; Fatone, L.; Bisceglie, M.B.D.; Nardi, G.; Grassi, F.R. Cytokine Genotype Distribution in Patients with Periodontal Disease and Rheumatoid Arthritis or Diabetes Mellitus. J. Biol. Regul. Homeost. Agents 2016, 30, 863–866. [Google Scholar]
- Crincoli, V.; Di Bisceglie, M.B.; Scivetti, M.; Favia, A.; Di Comite, M. Dens Invaginatus: A Qualitative-Quantitative Analysis. Case Report of an Upper Second Molar. Ultrastruct. Pathol. 2010, 34, 7–15. [Google Scholar] [CrossRef]
- Crincoli, V.; Cazzolla, A.P.; Di Comite, M.; Lo Muzio, L.; Ciavarella, D.; Dioguardi, M.; Bizzoca, M.E.; Palmieri, G.; Fontana, A.; Giustino, A.; et al. Evaluation of Vitamin D (25OHD), Bone Alkaline Phosphatase (BALP), Serum Calcium, Serum Phosphorus, Ionized Calcium in Patients with Mandibular Third Molar Impaction. An Observational Study. Nutrients 2021, 13, 1938. [Google Scholar] [CrossRef]
- Fuziy, A.; Rodrigues de Almeida, R.; Janson, G.; Angelieri, F.; Pinzan, A. Sagittal, Vertical, and Transverse Changes Consequent to Maxillary Molar Distalization with the Pendulum Appliance. Am. J. Orthod. Dentofacial Orthop. 2006, 130, 502–510. [Google Scholar] [CrossRef]
- Berg, R. Stability of Deep Overbite Correction. Eur. J. Orthod. 1983, 5, 75–83. [Google Scholar] [CrossRef]
- Mehta, S.; Patel, D.; Yadav, S.; Mehta, S.; Patel, D.; Yadav, S. Staging Orthodontic Aligners for Complex Orthodontic Tooth Movement. Turk. J. Orthod. 2021, 34, 202–206. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, O.M.; Saga, A.Y.; Pithon, M.M.; Argenta, M.A. Stresses in the Midpalatal Suture in the Maxillary Protraction Therapy: A 3D Finite Element Analysis. Prog. Orthod. 2016, 17, 8. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Lindauer, S.J. The Basics of Orthodontic Mechanics. Semin. Orthod. 2001, 7, 2–15. [Google Scholar] [CrossRef]
- Dioguardi, M.; Cantore, S.; Scacco, S.; Quarta, C.; Sovereto, D.; Spirito, F.; Alovisi, M.; Troiano, G.; Aiuto, R.; Garcovich, D.; et al. From Bench to Bedside in Precision Medicine: Diabetes Mellitus and Peri-Implantitis Clinical Indices with a Short-Term Follow-Up: A Systematic Review and Meta-Analysis. J. Pers. Med. 2022, 12, 235. [Google Scholar] [CrossRef]
- Dioguardi, M.; Cazzolla, A.P.; Arena, C.; Sovereto, D.; Caloro, G.A.; Dioguardi, A.; Crincoli, V.; Laino, L.; Troiano, G.; Lo Muzio, L. Innate Immunity in Children and the Role of ACE2 Expression in SARS-CoV-2 Infection. Pediatr. Rep. 2021, 13, 363–382. [Google Scholar] [CrossRef]
- Lucchese, A.; Serpico, R.; Guida, A.; Crincoli, V.; Scully, C.; Kanduc, D. Interkeratin Peptide-Protein Interactions That Promote HPV16 E7 Gene Expression. Int. J. Immunopathol. Pharmacol. 2010, 23, 857–864. [Google Scholar] [CrossRef]
- Miller, D.B. Invisalign in TMD Treatment. Int. J. Orthod. Milwaukee 2009, 20, 15–19. [Google Scholar]
- Crincoli, V.; Ballini, A.; Di Comite, M.; Tettamanti, L.; Coscia, M.F.; Mastrangelo, F.; De Vito, D. Microbiological Investigation of Medication-Related Osteonecrosis of the Jaw: Preliminary Results. J. Biol. Regul. Homeost. Agents 2015, 29, 977–983. [Google Scholar] [PubMed]
- Lacarbonara, M.; Lacarbonara, V.; Cazzolla, A.P.; Spinelli, V.; Crincoli, V.; Lacaita, M.G.; Capogreco, M. Odontomas in Developmental Age: Confocal Laser Scanning Microscopy Analysis of a Case. Eur. J. Paediatr. Dent. 2017, 18, 77–79. [Google Scholar] [CrossRef]
- Andrews, L.F. The Six Keys to Normal Occlusion. Am. J. Orthod. 1972, 62, 296–309. [Google Scholar] [CrossRef] [PubMed]
- Dianiskova, S.; Rongo, R.; Buono, R.; Franchi, L.; Michelotti, A.; D’Antò, V. Treatment of Mild Class II Malocclusion in Growing Patients with Clear Aligners versus Fixed Multibracket Therapy: A Retrospective Study. Orthod. Craniofacial Res. 2022, 25, 96–102. [Google Scholar] [CrossRef] [PubMed]
- Park, T.H.; Shen, C.; Chung, C.-H.; Li, C. Vertical Control in Molar Distalization by Clear Aligners: A Systematic Review and Meta-Analysis. J. Clin. Med. 2024, 13, 2845. [Google Scholar] [CrossRef]
- Balboni, A.; Lombardo, E.C.; Balboni, G.; Gazzani, F. Vertical Effects of Distalization Protocol with Clear Aligners in Class II Patients: A Prospective Study. Minerva Dent. Oral Sci. 2023, 72, 291–297. [Google Scholar] [CrossRef]
- Patano, A.; Cardarelli, F.; Montenegro, V.; Ceci, S.; Inchingolo, A.D.; Semjonova, A.; Palmieri, G.; Pede, C.D.; Mancini, A.; Maggiore, M.E.; et al. Early Functional Orthodontic Treatment of Bad Oral Habits with AMCOP® Bio-Activators. J. Biol. Regul. Homeost. Agents 2022, 36, 91–110. [Google Scholar] [CrossRef]
- Inchingolo, A.D.; Malcangi, G.; Ceci, S.; Patano, A.; Corriero, A.; Vimercati, L.; Azzollini, D.; Marinelli, G.; Coloccia, G.; Piras, F.; et al. Effectiveness of SARS-CoV-2 Vaccines for Short- and Long-Term Immunity: A General Overview for the Pandemic Contrast. Int. J. Mol. Sci. 2022, 23, 8485. [Google Scholar] [CrossRef] [PubMed]
- Patano, A.; Inchingolo, A.M.; Cardarelli, F.; Inchingolo, A.D.; Viapiano, F.; Giotta, M.; Bartolomeo, N.; Di Venere, D.; Malcangi, G.; Minetti, E.; et al. Effects of Elastodontic Appliance on the Pharyngeal Airway Space in Class II Malocclusion. J. Clin. Med. 2023, 12, 4280. [Google Scholar] [CrossRef]
- Inchingolo, A.D.; Pezzolla, C.; Patano, A.; Ceci, S.; Ciocia, A.M.; Marinelli, G.; Malcangi, G.; Montenegro, V.; Cardarelli, F.; Piras, F.; et al. Experimental Analysis of the Use of Cranial Electromyography in Athletes and Clinical Implications. Int. J. Environ. Res. Public Health 2022, 19, 7975. [Google Scholar] [CrossRef]
- Dipalma, G.; Inchingolo, A.D.; Inchingolo, F.; Charitos, I.A.; Di Cosola, M.; Cazzolla, A.P. Focus on the Cariogenic Process: Microbial and Biochemical Interactions with Teeth and Oral Environment. J. Biol. Regul. Homeost. Agents 2021, 35, 3942. [Google Scholar] [CrossRef]
- Functional Breastfeeding: From Nutritive Sucking to Oral Health. Available online: https://www.researchgate.net/publication/361633237_Functional_breastfeeding_from_nutritive_sucking_to_oral_health (accessed on 10 April 2025).
- Cirulli, N.; Ballini, A.; Cantore, S.; Farronato, D.; Inchingolo, F.; Dipalma, G.; Gatto, M.R.; Alessandri Bonetti, G. Mixed Dentition Space Analysis of a Southern Italian Population: New Regression Equations for Unerupted Teeth. J. Biol. Regul. Homeost. Agents 2015, 29, 515–520. [Google Scholar]
- MRONJ Treatment Strategies: A Systematic Review and Two Case Reports. Available online: https://www.mdpi.com/2076-3417/13/7/4370 (accessed on 10 April 2025).
- Navigation Systems in Maxillofacial Surgery and Neurosurgery and Their Potential Advantages. Available online: https://www.researchgate.net/publication/362780164_Navigation_systems_in_maxillofacial_surgery_and_neurosurgery_and_their_potential_advantages (accessed on 10 April 2025).
- Orthodontic Emergencies and Patients’ Perceptions of Orthodontic Patients during the COVID-19 Pandemic. Available online: https://www.researchgate.net/publication/362742614_Orthodontic_emergencies_and_patients%27_perceptions_of_orthodontic_patients_during_the_COVID-19_pandemic (accessed on 10 April 2025).
- Dipalma, G.; Inchingolo, A.D.; Mancini, A.; Maggiore, M.E.; Tartaglia, G.M.; Malcangi, G.; Ferrara, E.; Lorusso, F.; Scarano, A.; Bordea, I.R.; et al. Periodontal Disease and Clinical Association with COVID-19 Infection. J. Biol. Regul. Homeost. Agents 2022, 36, 139–150. [Google Scholar]
- Inchingolo, A.M.; Ceci, S.; Coloccia, G.; Azzollini, D.; Malcangi, G.; Mancini, A.; Inchingolo, F.; Trerotoli, P.; Dipalma, G.; Patano, A. Predictability and Effectiveness of Nuvola® Aligners in Dentoalveolar Transverse Changes: A Retrospective Study. Biomedicines 2023, 11, 1366. [Google Scholar] [CrossRef]
- Dipalma, G.; Inchingolo, A.M.; Malcangi, G.; Ferrara, I.; Viapiano, F.; Netti, A.; Patano, A.; Isacco, C.G.; Inchingolo, A.D.; Inchingolo, F. Sixty-Month Follow Up of Clinical MRONJ Cases Treated with CGF and Piezosurgery. Bioengineering 2023, 10, 863. [Google Scholar] [CrossRef] [PubMed]
- Gargiulo Isacco, C.; Inchingolo, A.D.; Nguyen Cao, K.D.; Malcangi, G.; Paduanelli, G.; Pham Hung, V.; Tran Cong, T.; Bordea, I.R.; Scarano, A.; Laforgia, A.; et al. The Bad Relationship, Osteo-Decay and Diabetes Type 2 Searching for a Link: A Literature Review. J. Biol. Regul. Homeost. Agents 2021, 35, 253–269. [Google Scholar] [CrossRef] [PubMed]
- Patano, A.; Inchingolo, A.M.; Laudadio, C.; Azzollini, D.; Marinelli, G.; Ceci, S.; Latini, G.; Rapone, B.; Inchingolo, A.D.; Mancini, A.; et al. Therapeutic Strategies of Primary Molar Infraocclusion: A Systematic Review. Children 2023, 10, 582. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Wang, P.; Jiang, C.; Liu, Y.; Ma, X.; Liu, Y.; Fan, C. Biomechanical Effects of Clear Aligners with Different Distal Coverage Designs Combined with Class II Elastic Traction for Maxillary First Molar Distalization: A Finite Element Study. BMC Oral Health 2025, 25, 1033. [Google Scholar] [CrossRef]
- Sandhya, V.; Arun, A.; Reddy, V.P.; Mahendra, S.; Chandrashekar, B.; Aravind. Biomechanical Effects of Torquing on Upper Central Incisor with Thermoplastic Aligner: A Comparative Three-Dimensional Finite Element Study with and Without Auxillaries. J. Indian Orthod. Soc. 2022, 56, 49–56. [Google Scholar] [CrossRef]
- Mossaz, C.F.; Byloff, F.K.; Kiliaridis, S. Cervical Headgear vs Pendulum Appliance for the Treatment of Moderate Skeletal Class II Malocclusion. Am. J. Orthod. Dentofacial Orthop. 2007, 132, 616–623. [Google Scholar] [CrossRef]
- Vukusić, N.; Lapter, M.; Muretić, Z. Change in the Inclination of the Occlusal Plane during Craniofacial Growth and Development. Coll. Antropol. 2000, 24, 145–150. [Google Scholar]
- Braun, S.; Legan, H.L. Changes in Occlusion Related to the Cant of the Occlusal Plane. Am. J. Orthod. Dentofacial Orthop. 1997, 111, 184–188. [Google Scholar] [CrossRef]
- Li, J.; Kau, C.; Wang, M. Changes of Occlusal Plane Inclination after Orthodontic Treatment in Different Dentoskeletal Frames. Prog. Orthod. 2014, 15, 41. [Google Scholar] [CrossRef]
- Bichu, Y.M.; Alwafi, A.; Liu, X.; Andrews, J.; Ludwig, B.; Bichu, A.Y.; Zou, B. Advances in Orthodontic Clear Aligner Materials. Bioact. Mater. 2023, 22, 384–403. [Google Scholar] [CrossRef]
- Align Technology Introduces One-Week Aligner Wear for Invisalign(R) Teen and Full Products|Align Technology. Available online: https://investor.aligntech.com/news-releases/news-release-details/align-technology-introduces-one-week-aligner-wear-invisalignr/ (accessed on 23 July 2025).
- Baccetti, T.; Franchi, L.; McNamara, J.A. An Improved Version of the Cervical Vertebral Maturation (CVM) Method for the Assessment of Mandibular Growth. Angle Orthod. 2002, 72, 316–323. [Google Scholar] [CrossRef]
- Analisi Degli Effetti Della Terapia Con Distalizzazione Molare—ScienceDirect. Available online: https://www.sciencedirect.com/science/article/abs/pii/S0391200010001019 (accessed on 23 July 2025).
- Staderini, E.; Ventura, V.; Meuli, S.; Maltagliati, L.Á.; Gallenzi, P. Analysis of the Changes in Occlusal Plane Inclination in a Class II Deep Bite “Teen” Patient Treated with Clear Aligners: A Case Report. Int. J. Environ. Res. Public Health 2022, 19, 651. [Google Scholar] [CrossRef] [PubMed]
- Elkholy, F.; Weber, S.; Repky, S.; Jäger, R.; Schmidt, F.; Lapatki, B.G. Are Aligners Capable of Inducing Palatal Bodily Translation or Palatal Root Torque of Upper Central Incisors? A Biomechanical in Vitro Study. Clin. Oral Investig. 2023, 27, 4289–4300. [Google Scholar] [CrossRef] [PubMed]
- Kuo, E.; Miller, R.J. Automated Custom-Manufacturing Technology in Orthodontics. Am. J. Orthod. Dentofacial Orthop. 2003, 123, 578–581. [Google Scholar] [CrossRef] [PubMed]
- Dioguardi, M.; Alovisi, M.; Crincoli, V.; Aiuto, R.; Malagnino, G.; Quarta, C.; Laneve, E.; Sovereto, D.; Lo Russo, L.; Troiano, G.; et al. Prevalence of the Genus Propionibacterium in Primary and Persistent Endodontic Lesions: A Systematic Review. J. Clin. Med. 2020, 9, 739. [Google Scholar] [CrossRef]
- Lacarbonara, M.; Cazzolla, A.P.; Lacarbonara, V.; Lo Muzio, L.; Ciavarella, D.; Testa, N.F.; Crincoli, V.; Di Venere, D.; De Franco, A.; Tripodi, D.; et al. Prosthetic Rehabilitation of Maxillary Lateral Incisors Agenesis Using Dental Mini-Implants: A Multicenter 10-Year Follow-Up. Clin. Oral Investig. 2022, 26, 1963–1974. [Google Scholar] [CrossRef]
- Tecco, S.; Crincoli, V.; Di Bisceglie, B.; Caputi, S.; Festa, F. Relation between Facial Morphology on Lateral Skull Radiographs and sEMG Activity of Head, Neck, and Trunk Muscles in Caucasian Adult Females. J. Electromyogr. Kinesiol. 2011, 21, 298–310. [Google Scholar] [CrossRef]
- Schour, I.; Massler, M. Studies in Tooth Development: The Growth Pattern of Human Teeth. J. Am. Dent. Assoc. 1940, 27, 1778–1793. [Google Scholar] [CrossRef]
- Crincoli, V.; Piancino, M.G.; Iannone, F.; Errede, M.; Di Comite, M. Temporomandibular Disorders and Oral Features in Systemic Lupus Erythematosus Patients: An Observational Study of Symptoms and Signs. Int. J. Med. Sci. 2020, 17, 153–160. [Google Scholar] [CrossRef]
- Dioguardi, M.; Spirito, F.; Sovereto, D.; Alovisi, M.; Aiuto, R.; Garcovich, D.; Crincoli, V.; Laino, L.; Cazzolla, A.P.; Caloro, G.A.; et al. The Prognostic Role of miR-31 in Head and Neck Squamous Cell Carcinoma: Systematic Review and Meta-Analysis with Trial Sequential Analysis. Int. J. Environ. Res. Public Health 2022, 19, 5334. [Google Scholar] [CrossRef]
- Crincoli, V.; Scivetti, M.; Di Bisceglie, M.B.; Pilolli, G.P.; Favia, G. Unusual Case of Adverse Reaction in the Use of Sodium Hypochlorite during Endodontic Treatment: A Case Report. Quintessence Int. 2008, 39, e70–73. [Google Scholar]
- Al-balaa, M.; Li, H.; Mohamed, A.M.; Xia, L.; Liu, W.; Chen, Y.; Omran, T.; Li, S.; Hua, X. Predicted and Actual Outcome of Anterior Intrusion with Invisalign Assessed with Cone-Beam Computed Tomography. Am. J. Orthod. Dentofac. Orthop. 2021, 159, e275–e280. [Google Scholar] [CrossRef]
- Lu, W.; Li, Y.; Mei, L.; Li, Y. Preformed Intrusion Bulbs on Clear Aligners Facilitate Active Vertical Control in a Hyperdivergent Skeletal Class II Case with Extraction: A Case Report with 4-Year Follow-Up. APOS-Trends Orthod. 2023, 13, 46–54. [Google Scholar] [CrossRef]
- De Ridder, L.; Aleksieva, A.; Willems, G.; Declerck, D.; Cadenas de Llano-Pérula, M. Prevalence of Orthodontic Malocclusions in Healthy Children and Adolescents: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 7446. [Google Scholar] [CrossRef]
- Kim, B.J.; Lee, E.-J.; Kwon, S.U.; Park, J.-H.; Kim, Y.-J.; Hong, K.-S.; Wong, L.K.S.; Yu, S.; Hwang, Y.-H.; Lee, J.S.; et al. Prevention of Cardiovascular Events in Asian Patients with Ischaemic Stroke at High Risk of Cerebral Haemorrhage (PICASSO): A Multicentre, Randomised Controlled Trial. Lancet Neurol. 2018, 17, 509–518. [Google Scholar] [CrossRef] [PubMed]
- Gaddam, R.; Freer, E.; Kerr, B.; Weir, T. Reliability of Torque Expression by the Invisalign® Appliance: A Retrospective Study. Australas. Orthod. J. 2021, 37, 3–13. [Google Scholar] [CrossRef]
- Schupp, W.; Haubrich, J.; Neumann, I. Class II Correction with the Invisalign System. J. Clin. Orthod. 2010, 44, 28–35. [Google Scholar] [PubMed]
- Jones, G.; Buschang, P.H.; Kim, K.B.; Oliver, D.R. Class II Non-Extraction Patients Treated with the Forsus Fatigue Resistant Device versus Intermaxillary Elastics. Angle Orthod. 2008, 78, 332–338. [Google Scholar] [CrossRef]
- Ghosh, J.; Nanda, R.S. Class II, Division 1 Malocclusion Treated with Molar Distalization Therapy. Am. J. Orthod. Dentofacial Orthop. 1996, 110, 672–677. [Google Scholar] [CrossRef]
- Meade, M.J.; Weir, T.; Seehra, J.; Fleming, P.S. Clear Aligner Therapy Practice among Orthodontists in the United Kingdom and the Republic of Ireland: A Cross-Sectional Survey of the British Orthodontic Society Membership. J. Orthod. 2024, 51, 120–129. [Google Scholar] [CrossRef]
- Meade, M.J.; Weir, T. Clear Aligner Therapy Procedures and Protocols of Orthodontists in New Zealand. Australas. Orthod. J. 2023, 39, 123–135. [Google Scholar] [CrossRef]
- Voudouris, J.C.; Voudouris, J.D.; Nicolay, O.; Glaser, B.; Nicozisis, J.; Theodoridis, G.; Carrillo, R.; Moshiri, M.; Masoud, M. Clear Aligners, Dentofacial Orthopedics, Physics and Supercorrection Prescription Biomechanics. A Meeting of the Minds. Semin. Orthod. 2022, 27, 202–258. [Google Scholar] [CrossRef]
- Stephens, C.; Weir, T.; Llewellyn, S.; Freer, E.; Kerr, B. Clinical Expression of Programmed Mandibular Canine Rotation Using Various Attachment Protocols and 1- vs 2-Week Wear Protocols with Invisalign SmartTrack Aligners: A Retrospective Cohort Study. Am. J. Orthod. Dentofac. Orthop. 2022, 162, e103–e115. [Google Scholar] [CrossRef] [PubMed]
- Makwana, K.P.; Malek, N.I.; Kailasa, S.K. Colloidal Perovskite Nanomaterials: New Insights on Synthetic Routes, Properties and Sensing Applications. Adv. Colloid Interface Sci. 2025, 344, 103587. [Google Scholar] [CrossRef] [PubMed]
- Bussick, T.J.; McNamara, J.A. Dentoalveolar and Skeletal Changes Associated with the Pendulum Appliance. Am. J. Orthod. Dentofacial Orthop. 2000, 117, 333–343. [Google Scholar] [CrossRef]
- Morton, J.; Derakhshan, M.; Kaza, S.; Li, C. Design of the Invisalign System Performance. Semin. Orthod. 2017, 23, 3–11. [Google Scholar] [CrossRef]
- Muro, M.P.; Caracciolo, A.C.A.; Patel, M.P.; Feres, M.F.N.; Roscoe, M.G. Effectiveness and Predictability of Treatment with Clear Orthodontic Aligners: A Scoping Review. Int. Orthod. 2023, 21, 100755. [Google Scholar] [CrossRef]
- Effectiveness of Clear Aligner Therapy for Orthodontic Treatment: A Systematic Review—Robertson—2020—Orthodontics & Craniofacial Research—Wiley Online Library. Available online: https://onlinelibrary.wiley.com/doi/10.1111/ocr.12353 (accessed on 23 July 2025).
- Kankam, H.; Madari, S.; Sawh-Martinez, R.; Bruckman, K.C.; Steinbacher, D.M. Comparing Outcomes in Orthognathic Surgery Using Clear Aligners Versus Conventional Fixed Appliances. J. Craniofacial Surg. 2019, 30, 1488. [Google Scholar] [CrossRef] [PubMed]
- Dai, F.-F.; Xu, T.-M.; Shu, G. Comparison of Achieved and Predicted Tooth Movement of Maxillary First Molars and Central Incisors: First Premolar Extraction Treatment with Invisalign. Angle Orthod. 2019, 89, 679–687. [Google Scholar] [CrossRef] [PubMed]
- Angelieri, F.; de Almeida, R.R.; Janson, G.; Castanha Henriques, J.F.; Pinzan, A. Comparison of the Effects Produced by Headgear and Pendulum Appliances Followed by Fixed Orthodontic Treatment. Eur. J. Orthod. 2008, 30, 572–579. [Google Scholar] [CrossRef]
- Moshiri, M. Considerations for Treatment of Patients Undergoing Orthognathic Surgery Using Clear Aligners. AJO-DO Clin. Companion 2022, 2, 229–239. [Google Scholar] [CrossRef]
- Janson, G.; Sathler, R.; Fernandes, T.M.F.; Branco, N.C.C.; Freitas, M.R. de Correction of Class II Malocclusion with Class II Elastics: A Systematic Review. Am. J. Orthod. Dentofacial Orthop. 2013, 143, 383–392. [Google Scholar] [CrossRef] [PubMed]
- Crossref Crossref. Available online: https://record.crossref.org/ (accessed on 23 July 2025).
- Blundell, H.L.; Weir, T.; Meade, M.J. Deep Overbite Reduction in Adolescent Patients Treated with Invisalign: A Retrospective Analysis. Am. J. Orthod. Dentofacial Orthop. 2024, 166, 515–523. [Google Scholar] [CrossRef]
- Baneshi, M.; O’Malley, L.; El-Angbawi, A.; Thiruvenkatachari, B. Effectiveness of Clear Orthodontic Aligners in Correcting Malocclusions: A Systematic Review and Meta-Analysis. J. Evid. Based Dent. Pract. 2025, 25, 102081. [Google Scholar] [CrossRef]
- Lione, R.; Franchi, L.; Laganà, G.; Cozza, P. Effects of Cervical Headgear and Pendulum Appliance on Vertical Dimension in Growing Subjects: A Retrospective Controlled Clinical Trial. Eur. J. Orthod. 2015, 37, 338–344. [Google Scholar] [CrossRef]
- Henick, D.; Dayan, W.; Dunford, R.; Warunek, S.; Al-Jewair, T. Effects of Invisalign (G5) with Virtual Bite Ramps for Skeletal Deep Overbite Malocclusion Correction in Adults. Angle Orthod. 2021, 91, 164–170. [Google Scholar] [CrossRef]
- Li, Y.; Wu, M.; Xing, X.; Chen, Y.; Zhang, C.; Hu, J.; Shi, C. Effects of Maxillary Molar Distalization Using Clear Aligners during the Mixed Dentition and Early Permanent Dentition with 3 Types of Class II Traction: A Three-Dimensional Finite Element Analysis. BMC Oral Health 2025, 25, 717. [Google Scholar] [CrossRef]
- Lione, R.; Balboni, A.; Di Fazio, V.; Pavoni, C.; Cozza, P. Effects of Pendulum Appliance versus Clear Aligners in the Vertical Dimension during Class II Malocclusion Treatment: A Randomized Prospective Clinical Trial. BMC Oral Health 2022, 22, 441. [Google Scholar] [CrossRef]
- De Almeida-Pedrin, R.R.; Henriques, J.F.C.; de Almeida, R.R.; de Almeida, M.R.; McNamara, J.A. Effects of the Pendulum Appliance, Cervical Headgear, and 2 Premolar Extractions Followed by Fixed Appliances in Patients with Class II Malocclusion. Am. J. Orthod. Dentofacial Orthop. 2009, 136, 833–842. [Google Scholar] [CrossRef]
- Rossini, G.; Parrini, S.; Castroflorio, T.; Deregibus, A.; Debernardi, C.L. Efficacy of Clear Aligners in Controlling Orthodontic Tooth Movement: A Systematic Review. Angle Orthod. 2015, 85, 881–889. [Google Scholar] [CrossRef]
- Rajan, N.; Weir, T.; Meade, M.J. Efficacy of Planned Moderate to Severe Torque Changes in Maxillary Central Incisors with the Invisalign Appliance: A Retrospective Investigation. Am. J. Orthod. Dentofac. Orthop. 2024, 166, 375–383. [Google Scholar] [CrossRef] [PubMed]
- Hong, Y.-Y.; Zhou, M.-Q.; Cai, C.-Y.; Han, J.; Ning, N.; Kang, T.; Chen, X.-P. Efficacy of Upper-Incisor Torque Control with Clear Aligners: A Retrospective Study Using Cone-Beam Computed Tomography. Clin. Oral Investig. 2023, 27, 3863–3873. [Google Scholar] [CrossRef] [PubMed]
- Saif, B.S.; Pan, F.; Mou, Q.; Han, M.; Bu, W.; Zhao, J.; Guan, L.; Wang, F.; Zou, R.; Zhou, H.; et al. Efficiency Evaluation of Maxillary Molar Distalization Using Invisalign Based on Palatal Rugae Registration. Am. J. Orthod. Dentofacial Orthop. 2022, 161, e372–e379. [Google Scholar] [CrossRef] [PubMed]
- Kinzinger, G.S.M.; Fritz, U.B.; Sander, F.-G.; Diedrich, P.R. Efficiency of a Pendulum Appliance for Molar Distalization Related to Second and Third Molar Eruption Stage. Am. J. Orthod. Dentofacial Orthop. 2004, 125, 8–23. [Google Scholar] [CrossRef]
- Hartshorne, J.; Wertheimer, M.B. Emerging Insights and New Developments in Clear Aligner Therapy: A Review of the Literature. AJO-DO Clin. Companion 2022, 2, 311–324. [Google Scholar] [CrossRef]
- Ricketts, R.M. Esthetics, Environment, and the Law of Lip Relation. Am. J. Orthod. 1968, 54, 272–289. [Google Scholar] [CrossRef]
- Whitehead, A.L.; Julious, S.A.; Cooper, C.L.; Campbell, M.J. Estimating the Sample Size for a Pilot Randomised Trial to Minimise the Overall Trial Sample Size for the External Pilot and Main Trial for a Continuous Outcome Variable. Stat. Methods Med. Res. 2016, 25, 1057–1073. [Google Scholar] [CrossRef]
- Ji, L.; Li, B.; Wu, X. Evaluation of Biomechanics Using Different Traction Devices in Distalization of Maxillary Molar with Clear Aligners: A Finite Element Study. Comput. Methods Biomech. Biomed. Engin. 2023, 26, 559–567. [Google Scholar] [CrossRef]
- Su, P.; Pei, W.; Wang, X.; Ma, Y.; Jiang, Q.; Liang, J.; Zhou, S.; Zhao, J.; Liu, J.; Lu, G.Q.M. Exceptional Electrochemical HER Performance with Enhanced Electron Transfer between Ru Nanoparticles and Single Atoms Dispersed on a Carbon Substrate. Angew. Chem. Int. Ed. 2021, 60, 16044–16050. [Google Scholar] [CrossRef]
- Haouili, N.; Kravitz, N.D.; Vaid, N.R.; Ferguson, D.J.; Makki, L. Has Invisalign Improved? A Prospective Follow-up Study on the Efficacy of Tooth Movement with Invisalign. Am. J. Orthod. Dentofac. Orthop. 2020, 158, 420–425. [Google Scholar] [CrossRef] [PubMed]
- Burstone, C.J.; Pryputniewicz, R.J. Holographic Determination of Centers of Rotation Produced by Orthodontic Forces. Am. J. Orthod. 1980, 77, 396–409. [Google Scholar] [CrossRef]
- Al-Tayar, B.; Al-Somairi, M.A.; ALshoaibi, L.H.; Wang, X.; Wang, J.; Liu, J.; Al-Tayar, B.; An, X.; Si, Q. Impact of Molar Teeth Distalization by Clear Aligners on Temporomandibular Joint: A Three-Dimensional Study. Prog. Orthod. 2023, 24, 25. [Google Scholar] [CrossRef]
- Caruso, S.; Nota, A.; Ehsani, S.; Maddalone, E.; Ojima, K.; Tecco, S. Impact of Molar Teeth Distalization with Clear Aligners on Occlusal Vertical Dimension: A Retrospective Study. BMC Oral Health 2019, 19, 182. [Google Scholar] [CrossRef] [PubMed]
- Faxén Sepanian, V.; Sonnesen, L. Incisor Root Resorption in Class II Division 2 Patients in Relation to Orthodontic Treatment. Eur. J. Orthod. 2018, 40, 337–342. [Google Scholar] [CrossRef]
- Miao, Z.; Zhang, H.; Yang, Y.; Han, Y.; Leng, J.; Wang, S. Influence of Maxillary Molar Distalization with Clear Aligners on Three-Dimensional Direction: Molar Distal Movement, Intrusion, Distal Tip and Crown Buccal Torque. Prog. Orthod. 2023, 24, 48. [Google Scholar] [CrossRef] [PubMed]
- Luder, H.U. Malformations of the Tooth Root in Humans. Front. Physiol. 2015, 6, 307. [Google Scholar] [CrossRef]
- Xiao, Z.; Yu, S.; Li, Y.; Ruan, S.; Kong, L.B.; Huang, Q.; Huang, Z.; Zhou, K.; Su, H.; Yao, Z.; et al. Materials Development and Potential Applications of Transparent Ceramics: A Review. Mater. Sci. Eng. R Rep. 2020, 139, 100518. [Google Scholar] [CrossRef]
- Antonarakis, G.S.; Kiliaridis, S. Maxillary Molar Distalization with Noncompliance Intramaxillary Appliances in Class II Malocclusion. A Systematic Review. Angle Orthod. 2008, 78, 1133–1140. [Google Scholar] [CrossRef]
- Smith, R.J.; Burstone, C.J. Mechanics of Tooth Movement. Am. J. Orthod. 1984, 85, 294–307. [Google Scholar] [CrossRef]
- Methods of Anterior Torque Control during Retraction: A Systematic Review. Available online: https://www.mdpi.com/2075-4418/12/7/1611 (accessed on 23 July 2025).
- Shen, C.; Park, T.H.; Chung, C.-H.; Li, C. Molar Distalization by Clear Aligners with Sequential Distalization Protocol: A Systematic Review and Meta-Analysis. J. Funct. Biomater. 2024, 15, 137. [Google Scholar] [CrossRef]
- Tepedino, M.; Paoloni, V.; Cozza, P.; Chimenti, C. Movement of Anterior Teeth Using Clear Aligners: A Three-Dimensional, Retrospective Evaluation. Prog. Orthod. 2018, 19, 9. [Google Scholar] [CrossRef]
- Fontana, M.; Cozzani, M.; Caprioglio, A. Non-Compliance Maxillary Molar Distalizing Appliances: An Overview of the Last Decade. Prog. Orthod. 2012, 13, 173–184. [Google Scholar] [CrossRef]
- Lux, C.J.; Dücker, B.; Pritsch, M.; Komposch, G.; Niekusch, U. Occlusal Status and Prevalence of Occlusal Malocclusion Traits among 9-Year-Old Schoolchildren. Eur. J. Orthod. 2009, 31, 294–299. [Google Scholar] [CrossRef] [PubMed]
- Orthodontic Aligners: Current Perspectives for the Modern Orthodontic Office. Available online: https://www.mdpi.com/1648-9144/59/10/1773 (accessed on 23 July 2025).
- Kyomen, S.; Tanne, K. Influences of Aging Changes in Proliferative Rate of PDL Cells during Experimental Tooth Movement in Rats. Angle Orthod. 1997, 67, 67–72. [Google Scholar] [PubMed]
- Chang, S.; Condon, B.; Smith, J.; Nam, S. Innovative Approach to Flame Retardant Cotton Fabrics with Phosphorus Rich Casein via Layer-by-Layer Processing. Int. J. Mater. Sci. Appl. 2019, 8, 81–89. [Google Scholar] [CrossRef]
- Pinho, T.; Rocha, D.; Ribeiro, S.; Monteiro, F.; Pascoal, S.; Azevedo, R. Interceptive Treatment with Invisalign® First in Moderate and Severe Cases: A Case Series. Children 2022, 9, 1176. [Google Scholar] [CrossRef] [PubMed]
- Xun, C.-L.; Zhao, H.; Zeng, X.-L.; Wang, X. Intrusion of Overerupted Maxillary Molars with Miniscrew Implant Anchorage: A Radiographic Evaluation. J. Huazhong Univ. Sci. Technol. Med. Sci. 2013, 33, 780–785. [Google Scholar] [CrossRef]
- Krieger, E.; Seiferth, J.; Marinello, I.; Jung, B.A.; Wriedt, S.; Jacobs, C.; Wehrbein, H. Invisalign® Treatment in the Anterior Region: Were the Predicted Tooth Movements Achieved? J. Orofac. Orthop. 2012, 73, 365–376. [Google Scholar] [CrossRef]
- Caprioglio, A.; Fontana, M.; Longoni, E.; Cozzani, M. Long-Term Evaluation of the Molar Movements Following Pendulum and Fixed Appliances. Angle Orthod. 2013, 83, 447–454. [Google Scholar] [CrossRef]
- Tanaka, E.M.; Sato, S. Longitudinal Alteration of the Occlusal Plane and Development of Different Dentoskeletal Frames during Growth. Am. J. Orthod. Dentofacial Orthop. 2008, 134, 602.e1–602.e11, discussion 602–603. [Google Scholar] [CrossRef] [PubMed]
- Grippaudo, C.; Pantanali, F.; Paolantonio, E.G.; Saulle, R.; Latorre, G.; Deli, R. Orthodontic Treatment Timing in Growing Patients. Eur. J. Paediatr. Dent. 2013, 14, 231–236. [Google Scholar] [PubMed]
- Tamer, İ.; Öztaş, E.; Marşan, G.; Tamer, İ.; Öztaş, E.; Marşan, G. Orthodontic Treatment with Clear Aligners and The Scientific Reality Behind Their Marketing: A Literature Review. Turk. J. Orthod. 2019, 32, 241–246. [Google Scholar] [CrossRef]
- Kirjavainen, M.; Kirjavainen, T.; Hurmerinta, K.; Haavikko, K. Orthopedic Cervical Headgear with an Expanded Inner Bow in Class II Correction. Angle Orthod. 2000, 70, 317–325. [Google Scholar] [PubMed]
- Borda, A.F.; Garfinkle, J.S.; Covell, D.A.; Wang, M.; Doyle, L.; Sedgley, C.M. Outcome Assessment of Orthodontic Clear Aligner vs Fixed Appliance Treatment in a Teenage Population with Mild Malocclusions. Angle Orthod. 2020, 90, 485–490. [Google Scholar] [CrossRef]
- Bräscher, A.-K.; Zuran, D.; Feldmann, R.E.; Benrath, J. Patient Survey on Invisalign® Treatment Comparen the SmartTrack® Material to the Previous Aligner Material. J. Orofac. Orthop. 2016, 77, 432–438. [Google Scholar] [CrossRef]
- Al-Thomali, Y.; Basha, S.; Mohamed, R.N. Pendulum and Modified Pendulum Appliances for Maxillary Molar Distalization in Class II Malocclusion—A Systematic Review. Acta Odontol. Scand. 2017, 75, 394–401. [Google Scholar] [CrossRef]
- Rossini, G.; Parrini, S.; Castroflorio, T.; Deregibus, A.; Debernardi, C.L. Periodontal Health during Clear Aligners Treatment: A Systematic Review. Eur. J. Orthod. 2015, 37, 539–543. [Google Scholar] [CrossRef]
- Greco, M.; Rombolà, A. Precision Bite Ramps and Aligners: An Elective Choice for Deep Bite Treatment. J. Orthod. 2022, 49, 213–220. [Google Scholar] [CrossRef] [PubMed]
- Castroflorio, T.; Sedran, A.; Parrini, S.; Garino, F.; Reverdito, M.; Capuozzo, R.; Mutinelli, S.; Grybauskas, S.; Vaitiekūnas, M.; Deregibus, A. Predictability of Orthodontic Tooth Movement with Aligners: Effect of Treatment Design. Prog. Orthod. 2023, 24, 2. [Google Scholar] [CrossRef] [PubMed]
- Shahabuddin, N.; Kang, J.; Jeon, H.H. Predictability of the Deep Overbite Correction Using Clear Aligners. Am. J. Orthod. Dentofacial Orthop. 2023, 163, 793–801. [Google Scholar] [CrossRef] [PubMed]


| Studio (Autore, Anno) | D1 | D2 | D3 | D4 | D5 | D6 | D7 | D8 |
|---|---|---|---|---|---|---|---|---|
| J. Hennessy et al. (2016) [5] |  High risk High risk |  Low risk Low risk |  Some concerns Some concerns |  Some concerns Some concerns |  Low risk Low risk |  Low risk Low risk |  Some concerns Some concerns |  High risk High risk |
| S. Dianiskova et al. (2022) [34] |  Some concerns Some concerns |  Low risk Low risk |  Low risk Low risk |  Some concerns Some concerns |  Low risk Low risk |  Low risk Low risk |  Low risk Low risk |  Low risk Low risk |
| R. Lione et al. (2022) [100] |  Low risk Low risk |  Low risk Low risk |  Low risk Low risk |  Low risk Low risk |  Low risk Low risk |  Low risk Low risk |  Low risk Low risk |  Low risk Low risk |
| A. Balboni et al. (2023) [36] |  High risk High risk |  Low risk Low risk |  Some concerns Some concerns |  Some concerns Some concerns |  Low risk Low risk |  Low risk Low risk |  Some concerns Some concerns |  High risk High risk |
| Y. Li et al. (2025) [99] |  Some concerns Some concerns |  Low risk Low risk |  Some concerns Some concerns |  Some concerns Some concerns |  Low risk Low risk |  Low risk Low risk |  Some concerns Some concerns |  Some concerns Some concerns |
| M. Tepedino et al. (2018) [124] |  Low risk Low risk |  Low risk Low risk |  Low risk Low risk |  Low risk Low risk |  Low risk Low risk |  Low risk Low risk |  Low risk Low risk |  Low risk Low risk |
| W. Lu et al. (2023) [73] |  Low risk Low risk |  Low risk Low risk |  Low risk Low risk |  Some concerns Some concerns |  Low risk Low risk |  Low risk Low risk |  Low risk Low risk |  Low risk Low risk |
| T. Castroflorio et al. (2023) [143] |  Low risk Low risk |  Low risk Low risk |  Low risk Low risk |  Some concerns Some concerns |  Low risk Low risk |  Low risk Low risk |  Low risk Low risk |  Low risk Low risk |
| B. Al-Tayar et al. (2023) [114] |  High risk High risk |  Low risk Low risk |  Some concerns Some concerns |  Some concerns Some concerns |  Low risk Low risk |  Low risk Low risk |  Some concerns Some concerns |  High risk High risk |
| L. Keilig et al. (2024) [7] |  Low risk Low risk |  Low risk Low risk |  Low risk Low risk |  Some concerns Some concerns |  Low risk Low risk |  Low risk Low risk |  Low risk Low risk |  Low risk Low risk |
| N. Shahabuddin et al. (2023) [144] |  Low risk Low risk |  Low risk Low risk |  Low risk Low risk |  Low risk Low risk |  Low risk Low risk |  Low risk Low risk |  Low risk Low risk |  Low risk Low risk |
| N. Rajan et al. (2024) [103] |  Low risk Low risk |  Low risk Low risk |  Low risk Low risk |  Low risk Low risk |  Low risk Low risk |  Low risk Low risk |  Low risk Low risk |  Low risk Low risk |
 high;
high;  some concerns;
some concerns;  low.
low.Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dipalma, G.; Marinelli, G.; Inchingolo, F.; Longo, M.; Di Giulio Cesare, M.; Di Serio, S.; Palermo, A.; Del Fabbro, M.; Inchingolo, A.D.; Inchingolo, A.M. Clinical Efficacy of Clear Aligners in Class II Malocclusion: From Pediatric to Adult Cases–A Narrative Review. J. Funct. Biomater. 2025, 16, 354. https://doi.org/10.3390/jfb16090354
Dipalma G, Marinelli G, Inchingolo F, Longo M, Di Giulio Cesare M, Di Serio S, Palermo A, Del Fabbro M, Inchingolo AD, Inchingolo AM. Clinical Efficacy of Clear Aligners in Class II Malocclusion: From Pediatric to Adult Cases–A Narrative Review. Journal of Functional Biomaterials. 2025; 16(9):354. https://doi.org/10.3390/jfb16090354
Chicago/Turabian StyleDipalma, Gianna, Grazia Marinelli, Francesco Inchingolo, Marialuisa Longo, Maral Di Giulio Cesare, Sharon Di Serio, Andrea Palermo, Massimo Del Fabbro, Alessio Danilo Inchingolo, and Angelo Michele Inchingolo. 2025. "Clinical Efficacy of Clear Aligners in Class II Malocclusion: From Pediatric to Adult Cases–A Narrative Review" Journal of Functional Biomaterials 16, no. 9: 354. https://doi.org/10.3390/jfb16090354
APA StyleDipalma, G., Marinelli, G., Inchingolo, F., Longo, M., Di Giulio Cesare, M., Di Serio, S., Palermo, A., Del Fabbro, M., Inchingolo, A. D., & Inchingolo, A. M. (2025). Clinical Efficacy of Clear Aligners in Class II Malocclusion: From Pediatric to Adult Cases–A Narrative Review. Journal of Functional Biomaterials, 16(9), 354. https://doi.org/10.3390/jfb16090354












