Salivary Fistula as a Complication After the ORIF of a Mandibular Condylar Process Fracture: A Single-Centre Retrospective Study
Abstract
1. Introduction
2. Materials and Methods
- -
- A diagnosis of mandibular condylar process fracture;
- -
- ORIF treatment;
- -
- Complete medical history and personal data;
- -
- Patients attending follow-up appointments.
- -
- Close treatment;
- -
- Incomplete medical history;
- -
- Lack of follow-up appointments;
- -
- Patients with a history of cancer of the head and neck region.
- Disinfection, a tasteless diet, and pressure dressing;
- Chemical cauterization with a 10% solution of AgNO3, a cholinolytic drug, a tasteless diet, and pressure dressing;
- Surgical treatment—plastic surgery of the fistula.
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ORIF | Open Rigid Internal Fixation |
| BMI | Body Mass Index |
| CRP | C-reactive Protein Level |
| WBC | White Blood Cells |
References
- Wusiman, P.; Maimaitituerxun, B.; Guli Saimaiti, A.; Moming, A. Epidemiology and Pattern of Oral and Maxillofacial Trauma. J. Craniofac. Surg. 2020, 31, 517–520. [Google Scholar] [CrossRef]
- Ascani, G.; Di Cosimo, F.; Costa, M.; Mancini, P.; Caporale, C. Maxillofacial Fractures in the Province of Pescara, Italy: A Retrospective Study. ISRN Otolaryngol. 2014, 2014, 101370. [Google Scholar] [CrossRef]
- Kozakiewicz, M.; Walczyk, A. Current Frequency of Mandibular Condylar Process Fractures. J. Clin. Med. 2023, 12, 1394. [Google Scholar] [CrossRef] [PubMed]
- Wayiso, G.T.; Tola, F.S.; Erba, M.S.; Desta, D. Etiology and Pattern of Maxillofacial Fractures among Patients Who Visited Jimma Medical Center Dental Clinic, Jimma, Southwest Ethiopia. Medicine 2025, 104, e42569. [Google Scholar] [CrossRef] [PubMed]
- Kozakiewicz, M.; Zieliński, R.; Krasowski, M.; Okulski, J. Forces Causing One-Millimeter Displacement of Bone Fragments of Condylar Base Fractures of the Mandible after Fixation by All Available Plate Designs. Materials 2019, 12, 3122. [Google Scholar] [CrossRef] [PubMed]
- Sikora, M.; Chęciński, M.; Nowak, Z.; Chęcińska, K.; Olszowski, T.; Chlubek, D. The Use of Titanium 3D Mini-Plates in the Surgical Treatment of Fractures of the Mandibular Condyle: A Systematic Review and Meta-Analysis of Clinical Trials. J. Clin. Med. 2021, 10, 3604. [Google Scholar] [CrossRef]
- Kolk, A.; Scheunemann, L.M.; Grill, F.; Stimmer, H.; Wolff, K.D.; Neff, A. Prognostic Factors for Long-Term Results after Condylar Head Fractures: A Comparative Study of Non-Surgical Treatment versus Open Reduction and Osteosynthesis. J. Cranio-Maxillofac. Surg. 2020, 48, 1138–1145. [Google Scholar] [CrossRef]
- Valiati, R.; Ibrahim, D.; Abreu, M.E.; Heitz, C.; de Oliveira, R.B.; Pagnoncelli, R.M.; Silva, D.N. The Treatment of Condylar Fractures: To Open or Not to Open? A Critical Review of This Controversy. Int. J. Med. Sci. 2008, 5, 313–318. [Google Scholar] [CrossRef]
- Neff, A. Open Reduction and Internal Fixation in Temporomandibular Joint Traumatology: Current Concepts and Future Perspectives. Stomatol. Dis. Sci. 2019, 3, 2. [Google Scholar] [CrossRef]
- Bhutia, O.; Kumar, L.; Jose, A.; Roychoudhury, A.; Trikha, A. Evaluation of Facial Nerve Following Open Reduction and Internal Fixation of Subcondylar Fracture through Retromandibular Transparotid Approach. Br. J. Oral Maxillofac. Surg. 2014, 52, 236–240. [Google Scholar] [CrossRef]
- Ellis, E., 3rd; McFadden, D.; Simon, P.; Throckmorton, G. Surgical Complications with Open Treatment of Mandibular Condylar Process Fractures. J. Oral Maxillofac. Surg. 2000, 58, 950–958. [Google Scholar] [CrossRef]
- Ghezta, N.K.; Ram, R.; Bhardwaj, Y.; Sreevidya, S.; Sharma, M.; Bhatt, R. Operator Experience and Fracture Location Affects the Rate of Facial Nerve Injury in Condylar Fractures: An Analysis of 89 Cases. J. Oral Maxillofac. Surg. 2021, 79, e1-1104. [Google Scholar] [CrossRef]
- Neff, A.; Neff, F.; Kolk, A.; Horch, H.H. Risiken und perioperative Komplikationen bei offenen gelenkchirurgischen Eingriffen. Dtsch. Zahnärztl. Z. 2001, 56, 258–262. [Google Scholar]
- Tandon, S.; Verma, V.; Rashid, M.; Srivastava, S.; Singh, A.K.; Sharma, N.K. Is the Facial Nerve at Risk Following Surgical Correction of Mandibular Condylar Fracture: A Systematic Review and Meta-Analysis. Natl. J. Maxillofac. Surg. 2022, 13, S1–S10. [Google Scholar] [CrossRef]
- Agier, P.; Kozakiewicz, M.; Tyszkiewicz, S.; Gabryelczak, I. Risk of Permanent Dysfunction of Facial Nerves After Open Rigid Internal Fixation in the Treatment of Mandibular Condylar Process Fracture. Med. Sci. 2025, 13, 121. [Google Scholar] [CrossRef]
- Anehosur, V.; Kulkarni, K.; Shetty, S.; Kumar, N. Clinical outcomes of endoscopic vs retromandibular approach for the treatment of condylar fractures-a randomized clinical trial. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2019, 128, 479–484. [Google Scholar] [CrossRef] [PubMed]
- Balasundram, S.; Kovilpillai, F.J.; Royan, S.J.; Ma, B.C.; Gunarajah, D.R.; Adnan, T.H. A 4-Year Multicentre Audit of Complications Following ORIF Treatment of Mandibular Fractures. J. Maxillofac. Oral Surg. 2020, 19, 289–297. [Google Scholar] [CrossRef] [PubMed]
- Sikora, M.; Olszowski, T.; Sielski, M.; Stąpor, A.; Janiszewska-Olszowska, J.; Chlubek, D. The use of the transparotid approach for surgical treatment of condylar fractures—Own experience. J. Craniomaxillofac. Surg. 2015, 43, 1961–1965. [Google Scholar] [CrossRef]
- Sverzut, C.E.; Trivellato, A.E.; Sverzut, A.T.; de Moraes, M. Frey’s Syndrome after Condylar Fracture: Case Report. Braz. Dent. J. 2004, 15, 159–162. [Google Scholar] [CrossRef]
- Bouchard, C.; Perreault, M.H. Postoperative Complications Associated with the Retromandibular Approach: A Retrospective Analysis of 118 Subcondylar Fractures. J. Oral Maxillofac. Surg. 2014, 72, 370–375. [Google Scholar] [CrossRef]
- Rozeboom, A.V.J.; Dubois, L.; Boss, R.R.M.; Spijker, R.; de Lange, J. Open Treatment of Condylar Fractures via Extraoral Approaches: A Review of Complications. J. Cranio-Maxillofac. Surg. 2018, 46, 1232–1240. [Google Scholar] [CrossRef] [PubMed]
- Al Hasani, K.M.; Bakathir, A.A.; Al-Hashmi, A.K.; Albakri, A.M. Complications of Open Reduction and Internal Fixation of Mandibular Condyle Fractures in Oman. Sultan. Qaboos. Univ. Med. J. 2024, 24, 338–344. [Google Scholar] [CrossRef] [PubMed]
- García-Guerrero, I.; Ramírez, J.M.; Gómez de Diego, R.; Martínez-González, J.M.; Poblador, M.S.; Lancho, J.L. Complications in the Treatment of Mandibular Condylar Fractures: Surgical versus Conservative Treatment. Ann. Anat. 2018, 216, 60–68. [Google Scholar] [CrossRef]
- Lu, X.W.; Liu, X.G. Risk of Complications with Retromandibular Transparotid vs. Anteroparotid Approach for Condylar Fractures: A Systematic Review and Meta-Analysis. Eur. Rev. Med. Pharmacol. Sci. 2022, 26, 799–809. [Google Scholar] [CrossRef]
- Kim, B.K.; Kwon, Y.D.; Ohe, J.Y.; Choi, Y.H.; Choi, B.J. Usefulness of the Retromandibular Transparotid Approach for Condylar Neck and Condylar Base Fractures. J. Craniofac. Surg. 2012, 23, 712–715. [Google Scholar] [CrossRef]
- Vesnaver, A.; Ahčan, U.; Rozman, J. Evaluation of Surgical Treatment in Mandibular Condyle Fractures. J. Cranio-Maxillofac. Surg. 2012, 40, 647–653. [Google Scholar] [CrossRef] [PubMed]
- Belcastro, A.; Reed, W.; Puscas, L. The Management of Salivary Fistulas. Semin. Plast. Surg. 2022, 37, 4–8. [Google Scholar] [CrossRef]
- Gurukeerthi, B.; Thiagarajan, S.; Chidambaranathan, N.; Chaukar, D. Parotid fistula and/or salivary collection: An underrecognized and underreported preventable complication following surgery for oral cancer. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2022, 134, 442–448. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gotzsche, P.C.; Vandenbroucke, J.P.; STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for Reporting Observational Studies. Lancet 2007, 370, 1453–1457. [Google Scholar] [CrossRef]
- Kozakiewicz, M. Classification Proposal for Fractures of the Processus Condylaris Mandibulae. Clin. Oral Investig. 2019, 23, 485–491. [Google Scholar] [CrossRef]
- Neff, A.; Cornelius, C.P.; Rasse, M.; Torre, D.D.; Audigé, L. The Comprehensive AOCMF Classification System: Condylar Process Fractures—Level 3 Tutorial. Craniomaxillofac. Trauma Reconstr. 2014, 7, 44–58. [Google Scholar] [CrossRef]
- Loukota, R.A.; Rasse, M. Nomenclature/Classification of Fractures of the Mandibular Condylar Head. Br. J. Oral Maxillofac. Surg. 2010, 48, 477–478. [Google Scholar] [CrossRef]
- Cederholm, T.; Jensen, G.L.; Ballesteros-Pomar, M.D.; Blaauwe, R.; Correia, M.I.T.D.; Cuerda, C.; David, C.; Fukushima, R.; Gautier, J.B.O.; Gonzalez, M.C.; et al. Guidance for Assessment of the Inflammation Etiologic Criterion for the GLIM Diagnosis of Malnutrition: A Modified Delphi Approach. Clin. Nutr. 2024, 43, 1025–1032. [Google Scholar] [CrossRef] [PubMed]
- Hyman, J.; Disa, J.J.; Cordiero, P.G.; Mehrara, B.J. Management of Salivary Fistulas after Microvascular Head and Neck Reconstruction. Ann. Plast. Surg. 2006, 57, 270–274. [Google Scholar] [CrossRef] [PubMed]
- Weissler, J.M.; Mohamed, O.; Gryskiewicz, J.M.; Chopra, K. An Algorithmic Approach to Managing Parotid Duct Injury Following Buccal Fat Pad Removal. Aesthetic Surg. J. Open Forum 2022, 4, ojac032. [Google Scholar] [CrossRef]
- Al-Taki, M.; Sukkarieh, H.G.; Hoballah, J.J.; Jamali, S.F.; Habbal, M.; Masrouha, K.Z.; Abi-Melhem, R.; Tamim, H. Effect of Gender on Postoperative Morbidity and Mortality Outcomes: A Retrospective Cohort Study. Am. Surg. 2018, 84, 377–386. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Liu, M.; Wang, Y.; Li, W.; Guo, C.; Zhang, Y. Predictors of Sialocele or Salivary Fistula after Partial Superficial Parotidectomy for Benign Parotid Tumor: A Retrospective Study. J. Oral Maxillofac. Surg. 2022, 80, 526–532. [Google Scholar] [CrossRef]
- Paksoy, Z.B.; Sazak Kundi, F.C. Impact of the Prognostic Nutritional Index on the Development of Sialocele or Salivary Fistula After Parotidectomy. Clin. Otolaryngol. 2024, 50, 107–112. [Google Scholar] [CrossRef]
- Britt, C.J.; Stein, A.P.; Gessert, T.; Pflum, Z.; Saha, S.; Hartig, G.K. Factors Influencing Sialocele or Salivary Fistula Formation Postparotidectomy. Head Neck 2017, 39, 387–391. [Google Scholar] [CrossRef]
- Oehl, M.; Hummer, M.; Fleischhacker, W.W. Compliance with Antipsychotic Treatment. Acta Psychiatr. Scand. Suppl. 2000, 407, 83–86. [Google Scholar] [CrossRef]
- Nosé, M.; Barbui, C.; Tansella, M. How Often Do Patients with Psychosis Fail to Adhere to Treatment Programmes? A Systematic Review. Psychol. Med. 2003, 33, 1149–1160. [Google Scholar] [CrossRef]
- Backer, P. Men’s Health: An Overlooked Inequality. Br. J. Nurs. 2016, 25, 1054. [Google Scholar] [CrossRef] [PubMed]
- Imamura, F.; Micha, R.; Khatibzadeh, S.; Fahimi, S.; Shi, P.; Powles, J.; Mozaffarian, D. Dietary Quality among Men and Women in 187 Countries in 1990 and 2010: A Systematic Assessment. Lancet Glob. Health 2015, 3, 132–142. [Google Scholar] [CrossRef]
- Abe, M.; Mitani, A.; Hoshi, K.; Yanagimoto, S. Large Gender Gap in Oral Hygiene Behavior and Its Impact on Gingival Health in Late Adolescence. Int. J. Environ. Res. Public Health 2020, 17, 4394. [Google Scholar] [CrossRef] [PubMed]
- Olczak-Kowalczyk, D.; Gozdowski, D.; Kaczmarek, U. Oral Health in Polish Fifteen-year-old Adolescents. Oral Health Prev. Dent. 2019, 17, 139–146. [Google Scholar]
- Almas, K.; Al-Hawish, A.; Al-Khamis, W. Oral Hygiene Practices, Smoking Habit, and Self-Perceived Oral Malodor among Dental Students. J. Contemp. Dent. Pract. 2003, 4, 77–90. [Google Scholar] [CrossRef]
- Eurostat. The Lives of Women and Men in Europe—A Statistical Portrait; European Union: Luxembourg, 2017. [Google Scholar] [CrossRef]
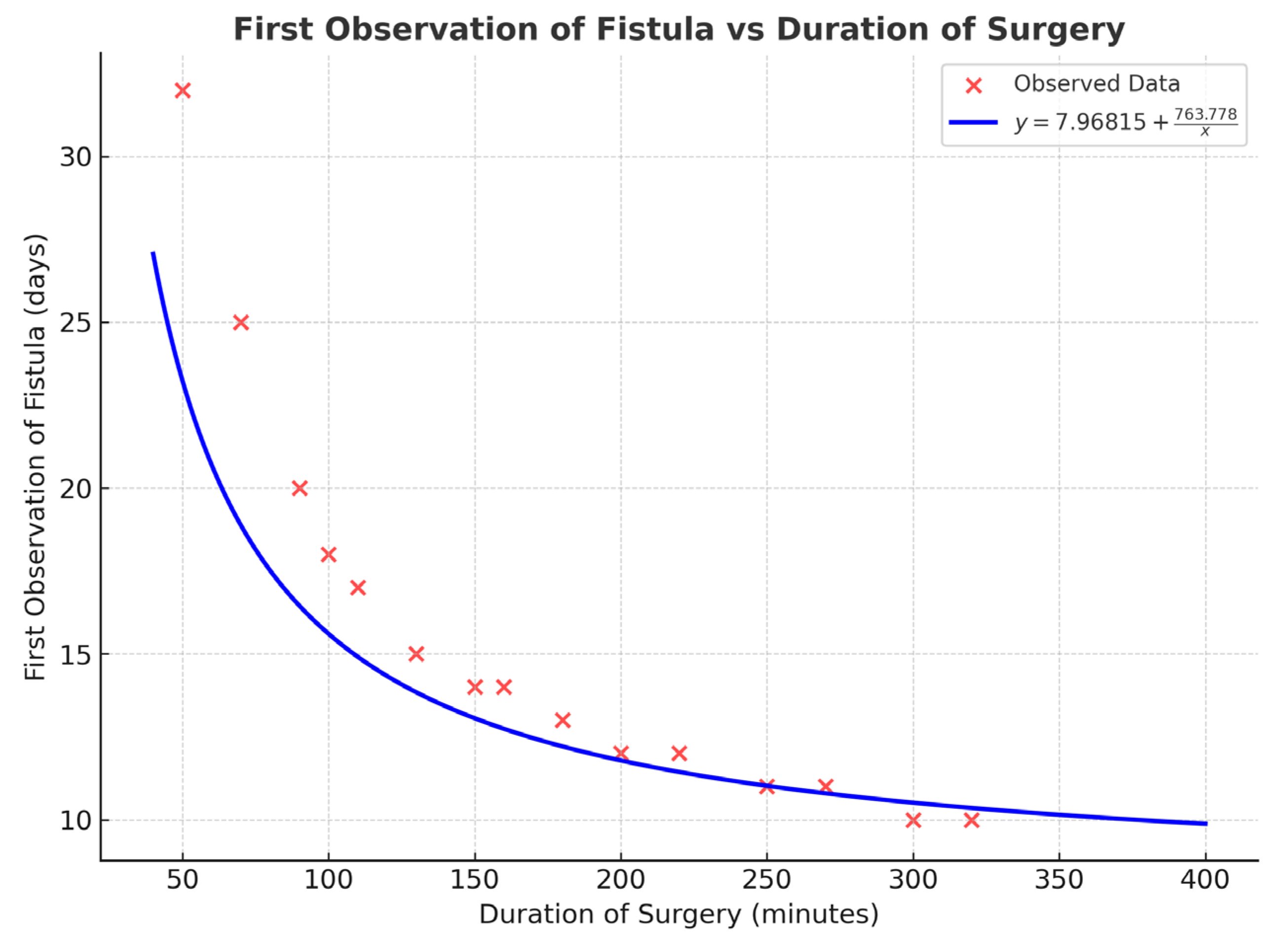
- Pienkohs, S.P.; Meisgeier, A.; Herrmann, J.; Graf, L.; Reichert, C.S.; Trento, G.; Neff, A. Factors Affecting the Duration of Surgery in the Management of Condylar Head Fractures. J. Clin. Med. 2023, 12, 7172. [Google Scholar] [CrossRef] [PubMed]
- Damrongsirirat, N.; Kaboosaya, B.; Siriwatana, K.; Subbalekha, K.; Jansisyanont, P.; Pimkhaokham, A. Complications Related to Orthognathic Surgery: A 10-Year Experience in Oral and Maxillofacial Training Center. J. Craniomaxillofac. Surg. 2022, 50, 197–203. [Google Scholar] [CrossRef] [PubMed]
- Chow, L.K.; Singh, B.; Chiu, W.K.; Samman, N. Prevalence of Postoperative Complications after Orthognathic Surgery: A 15-Year Review. J. Oral Maxillofac. Surg. 2007, 65, 984–992. [Google Scholar] [CrossRef]
- Yano, K.; Ikari, K.; Takatsuki, Y.; Taniguchi, A.; Yamanaka, H.; Momohara, S. Longer Operative Time Is the Risk for Delayed Wound Healing after Forefoot Surgery in Patients with Rheumatoid Arthritis. Mod. Rheumatol. 2016, 26, 211–215. [Google Scholar] [CrossRef]
- Cheng, H.; Clymer, J.W.; Po-Han Chen, B.; Sadeghirad, B.; Ferko, N.C.; Cameron, C.G.; Hinoul, P. Prolonged Operative Duration Is Associated with Complications: A Systematic Review and Meta-Analysis. J. Surg. Res. 2018, 229, 134–144. [Google Scholar] [CrossRef] [PubMed]
- El Sheikh, Y.M.; Seleem, M.F.M.A.; Fawzy, H.H. Compare between intraoral and extraoral approaches of subcondylar mandibular fracture management. Int. J. Health Sci. 2023, 7, 2746–2767. [Google Scholar] [CrossRef]
- Nam, S.M.; Kim, Y.B.; Lee, S.J.; Kim, S.M.; Huh, J.K. A comparative study of intraoral versus retromandibular approach in the management of subcondylar fracture. BMC Surg. 2019, 19, 28. [Google Scholar] [CrossRef] [PubMed]
- Kulkarni, V.; Chowdhury, S.K.R.; Ghosh, S.; Rajkumar, K. Incidence of Facial Nerve Injury and Sialocele Formation Following Mandibular Condylar and Sub-Condyle Fracture Fixation. J. Maxillofac. Oral Surg. 2024, 23, 380–386. [Google Scholar] [CrossRef]
- Caruso, C. When Recovery Goes Awry, New findings reveal how recovery progresses following inflammation triggered by injury or illness. In News Research; Harvard Medical School: Boston, MA, USA, 2022; Available online: https://hms.harvard.edu/news/when-recovery-goes-awry (accessed on 2 September 2025).
- Mank, W.; Waqas Azhar, W.; Brown, K. Leukocytosis. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2025. Available online: https://www.ncbi.nlm.nih.gov/books/NBK560882/ (accessed on 23 July 2025).
- Foy, B.H.; Sundt, T.M.; Carlson, J.C.T.; Aguirre, A.D.; Higgins, J.M. Human acute inflammatory recovery is defined by co-regulatory dynamics of white blood cell and platelet populations. Nat Commun. 2022, 13, 4705. [Google Scholar] [CrossRef]
- Julier, Z.; Park, A.J.; Briquez, P.S.; Martino, M.M. Promoting Tissue Regeneration by Modulating the Immune System. Acta Biomater. 2017, 53, 13–28. [Google Scholar] [CrossRef]
- Tsirpanlis, G. Inflammation in Atherosclerosis and Other Conditions: A Response to Danger. Kidney Blood Press. Res. 2005, 28, 211–217. [Google Scholar] [CrossRef] [PubMed]
- Kiran, D.N.; Desai, R. Estimation of C-Reactive Protein Associated with Mandibular Fracture. J. Maxillofac. Oral Surg. 2012, 11, 67–71. [Google Scholar] [CrossRef]
- Elbromboly, Y.; Esawy, M.A. Post-Operative C-Reactive Protein and White Blood Cells Changes Pattern Following Spinal Deformity Surgery and Its Clinical Correlation. J. Orthop. Surg. Res. 2023, 18, 790. [Google Scholar] [CrossRef]
- Horwich, T.B.; Kalantar-Zadeh, K.; MacLellan, R.W.; Fonarow, G.C. Albumin Levels Predict Survival in Patients with Systolic Heart Failure. Am. Heart J. 2008, 155, 883–889. [Google Scholar] [CrossRef]
- Saucedo, J.M.; Marecek, G.S.; Wanke, T.R.; Lee, J.; Stulberg, S.D.; Puri, L. Understanding Readmission after Primary Total Hip and Knee Arthroplasty: Who’s at Risk? J. Arthroplast. 2014, 29, 256–260. [Google Scholar] [CrossRef] [PubMed]
- Qin, P.; Wang, Z.; Liu, L.; Xiong, Q.; Liu, D.; Min, S.; Wei, K. The association between BMI and Postoperative Pulmonary Complications in Adults Undergoing Non-Cardiac, Non-Obstetric Surgery: A Retrospective Cohort Study. Assoc. Anaest. 2025, 80. [Google Scholar] [CrossRef]
- Heo, Y.H.; Yagi, S.; Toriyama, K.; Urken, M.L.; Nabili, V.; Kiyokawa, K.; Takushima, A. Relationship between BMI and postoperative complications with free flap in anterolateral craniofacial reconstruction. Plast. Reconstr. Surg. Glob. Open 2016, 4, e636. [Google Scholar] [CrossRef]
- Ebenezer, V.; Ramalingam, B. Comparison of Approaches for the Rigid Fixation of Sub-condylar Fractures. J. Maxillofac. Oral Surg. 2011, 10, 38–44. [Google Scholar] [CrossRef]
- Khoo, M.J.W.; Ooi, A.S.H. Management of postreconstructive head and neck salivary fistulae: A review of current practices. J. Plast. Reconstr. Aesthet. Surg. 2021, 74, 2120–2132. [Google Scholar] [CrossRef]
- Barrera, J.E. Parotid Duct Injures. Otolaryngol. Facial Plast. Surg. 2023. Available online: https://emedicine.medscape.com/article/868651-treatment#showall (accessed on 2 September 2025).
- Lim, J.C.; Choi, E.C. Treatment of an Acute Salivary Fistula after Parotid Surgery: Botulinum Toxin Type A Injection as Primary Treatment. Eur. Arch. Otorhinolaryngol. 2008, 265, 243–245. [Google Scholar] [CrossRef]
- Cohen, J.; Reed, W.; Foster, M.W.; Kahmke, R.R.; Rocke, D.J.; Puscas, L.; Cannon, T.Y.; Lee, W.T. Octreotide May Improve Pharyngocutaneous Fistula Healing through Downregulation of Cystatins: A Pilot Study. Laryngoscope Investig. Otolaryngol. 2022, 8, 113–119. [Google Scholar] [CrossRef]
- Mir, A.; Guys, N.; Arianpour, K.; Svider, P.F.; Rayess, H.; Zuliani, G.; Raza, S.N.; Lin, H. Negative Pressure Wound Therapy in the Head and Neck: An Evidence-Based Approach. Laryngoscope 2019, 129, 671–683. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.H.; Jeng, S.F.; Hsieh, C.H.; Feng, G.M.; Chen, C.C. Vacuum-Assisted Closure for Complicated Wounds in Head and Neck Region after Reconstruction. J. Plast. Reconstr. Aesthet. Surg. 2013, 66, e209–e216. [Google Scholar] [CrossRef] [PubMed]
- Kaehn, K.; Eberlein, T. In-vitro test for comparing the efficacy of wound rinsing solutions. Br. J. Nurs. 2009, 18, 4–10. [Google Scholar] [CrossRef]
- Wilkins, R.G.; Unverdorben, M. Wound cleaning and wound healing: A concise review. Adv. Skin Wound Care 2013, 26, 160–163. [Google Scholar] [CrossRef] [PubMed]
- Alvarez-Marin, R.; Aires-de-Sousa, M.; Nordmann, P.; Kieffer, N.; Poirel, L. Antimicrobial activity of octenidine against multidrug-resistant Gram-negative pathogens. Eur. J. Clin. Microbiol. Infect. Dis. 2017, 36, 2379–2383. [Google Scholar] [CrossRef] [PubMed]
- Assadian, O. Octenidine dihydrochloride: Chemical characteristics and antimicrobial properties. J. Wound Care 2016, 25, 3–6. [Google Scholar] [CrossRef] [PubMed]
- Krasowski, G.; Junka, A.; Paleczny, J.; Czajkowska, J.; Makomaska-Szaroszyk, E.; Chodaczek, G.; Majkowski, M.; Migdał, P.; Fijałkowski, K.; Kowalska-Krochmal, B.; et al. In Vitro Evaluation of Polihexanide, Octenidine and NaClO/HClO-Based Antiseptics against Biofilm Formed by Wound Pathogens. Membranes 2021, 11, 62. [Google Scholar] [CrossRef]
- Dettenkofer, M.; Wilson, C.; Gratwohl, A.; Schmoor, C.; Bertz, H.; Frei, R.; Heim, D.; Luft, C.; Schultz, S.; Widmer, A.F.; et al. Skin disinfection with octenidine dihydrochloride for central venous catheter site care: A double-blind, randomized, controlled trial. Clin. Microbiol. Infect. 2010, 16, 600–606. [Google Scholar] [CrossRef]
- Krishna, B.V.; Gibb, A.P. Use of octenidine dihydrochloride in meticillin-resistant Staphylococcus aureus decolonisation regimens: A literature review. J. Hosp. Infect. 2010, 74, 199–203. [Google Scholar] [CrossRef]
- Jain, J.; Arora, S.; Rajwade, J.M.; Omray, P.; Khandelwal, S.; Paknikar, K.M. Silver nanoparticles in therapeutics: Development of an antimicrobial gel formulation for topical use. Mol. Pharm. 2009, 6, 1388–1401. [Google Scholar] [CrossRef]
- Allawadhi, P.; Singh, V.; Khurana, A.; Khurana, I.; Allwadhi, S.; Kumar, P.; Banothu, A.K.; Thalugula, S.; Barani, P.J.; Naik, R.R.; et al. Silver nanoparticle based multifunctional approach for combating COVID-19. Sens. Int. 2021, 2, 100101. [Google Scholar] [CrossRef]
- Lansdown, A.B.; Sampson, B.; Laupattarakasem, P.; Vuttivirojana, A. Silver aids healing in the sterile skin wound: Experimental studies in the laboratory rat. Br. J. Dermatol. 1997, 137, 728–735. [Google Scholar] [CrossRef]
- Lansdown, A.B. Silver in health care: Antimicrobial effects and safety in use. Curr. Probl. Dermatol. 2006, 33, 17–34. [Google Scholar] [CrossRef] [PubMed]
- Severing, A.L.; Rembe, J.D.; Koester, V.; Stuermer, E.K. Safety and efficacy profiles of different commercial sodium hypochlorite/hypochlorous acid solutions (NaClO/HClO): Antimicrobial efficacy, cytotoxic impact and physicochemical parameters in vitro. J. Antimicrob. Chemother. 2019, 74, 365–372. [Google Scholar] [CrossRef] [PubMed]
- Souza, M.A.; Steier, L.; Vanin, G.N.; Brondi, M.R.; de Melo Carvalho, F.; de Oliveira Lima, C.S.; Pinto, L.D.R.; Rodrigues, L.K.A.; Colombo, A.P.V.; de Almeida, R.R.; et al. Antimicrobial action, cytotoxicity and erosive potential of hypochlorous acid obtained from an electrolytic device compared with sodium hypochlorite. Clin. Oral Investig. 2024, 28, 282. [Google Scholar] [CrossRef]
- Farber, N.M.; Perez-Lloret, S.; Gamzu, E.R. Design and development of a novel supportive care product for the treatment of sialorrhea in Parkinson’s disease. Curr. Top. Med. Chem. 2015, 15, 939–954. [Google Scholar] [CrossRef]
- Naicker, P.; Anoopkumar-Dukie, S.; Grant, G.D.; Kavanagh, J.J. Anticholinergic activity in the nervous system: Consequences for visuomotor function. Physiol. Behav. 2017, 170, 6–11. [Google Scholar] [CrossRef] [PubMed]
- Gudis, D.A.; Soler, Z.M. Nasal Cauterization with Silver Nitrate for Recurrent Epistaxis. N. Engl. J. Med. 2021, 384, 101. [Google Scholar] [CrossRef] [PubMed]
- Linneman, P.K.; Litt, J. Hypertrophic Granulation Wounds Treated With Silver Nitrate Sticks or With Topical Steroid: Rate of Wound Closure. J. Burn Care Res. 2022, 43, 403–407. [Google Scholar] [CrossRef]
- Martinez, J.D.; Cardenas, J.A.; Soria, M.; Saenz, L.M.; Estrada, K.; Delgado, S.M.; Ionescu, M.-A.; Busila, C.; Tatu, A.L. Role of Silver Nitrate Spray for Skin Wound Care in Patients with Toxic Epidermal Necrolysis: Our Experience in 4 Patients. Life 2023, 13, 2341. [Google Scholar] [CrossRef]
- Hah, J.H.; Kim, B.J.; Sung, M.W.; Kim, K.H. Chemocauterization of congenital fistula from the accessory parotid gland. Clin. Exp. Otorhinolaryngol. 2008, 1, 113–115. [Google Scholar] [CrossRef]
- Blythe, J.N.; Koraitim, M.; Arcuri, F.; Brennan, P.A. Novel approach in the treatment of a persistent iatrogenic parotid fistula using AlloDerm®—An allogenic acellular dermal matrix. Br. J. Oral Maxillofac. Surg. 2016, 54, 109–110. [Google Scholar] [CrossRef]






| Intensity of Salivary Leakage | Clinical Manifestation and/or Patient’s Observations | Treatment Method |
|---|---|---|
| Slight | Clinically visible aperture in the skin of the affected area, clinically no leakage of saliva; patient reports history of saliva flow | Disinfection, tasteless diet, pressure dressing |
| Moderate | Clinically visible moist aperture in the skin of the affected area | Chemical cauterization, cholinolytic drug, tasteless diet, pressure dressing |
| Profuse | Clinically visible aperture in the skin of the affected area, clinically visible salivary flow | Plastic surgery procedure |
| Variable | Complication | Mean ± SD | p-Value |
|---|---|---|---|
| Age [years] | No Salivary Fistula | 40.16 ± 16.54 | 0.548 |
| Salivary Fistula | 40.43 ± 11.90 | ||
| BMI [kg/m2] | No Salivary Fistula | 23.04 ± 4.29 | 0.922 |
| Salivary Fistula | 22.89 ± 3.55 | ||
| Total Mandibular Fractures | No Salivary Fistula | 2.01 ± 0.82 | 0.389 |
| Salivary Fistula | 1.87 ± 0.81 | ||
| Delay of Surgery Delay [days] | No Salivary Fistula | 8.76 ± 11.89 | 0.990 |
| Salivary Fistula | 8.39 ± 6.86 | ||
| Co-Morbidity | No Salivary Fistula | 0.50 ± 0.87 | 0.254 |
| Salivary Fistula | 0.30 ± 0.63 | ||
| Hemoglobin Level [g/dL] | No Salivary Fistula | 14.02 ± 1.71 | 0.02 |
| Salivary Fistula | 14.83 ± 1.21 | ||
| White Blood Cell Count [109/L] | No Salivary Fistula | 7.94 ± 3.00 | 0.01 |
| Salivary Fistula | 9.80 ± 3.99 |
| Variable | Correlation Coefficient | p-Value |
|---|---|---|
| WBC [109/L] | 0.66 | p = 0.0006 |
| CRP [mg/L] | 0.76 | p = 0.0003 |
| BMI [kg/m2] | 0.43 | p = 0.0467 |
| Treatment Method | No of Patients | Mean ± SD | Median and IQR |
|---|---|---|---|
| Disinfection, tasteless diet, pressure dressing | 12 | 11.75 ± 9.41 | 10 (7–41) |
| Chemical cauterization, cholinolytic drug, tasteless diet, pressure dressing | 8 | 13.12 ± 11.56 | 7.5 (2–35) |
| Surgical plastic surgery | 3 | 13.33 ± 7.09 | 12 (7–21) |
| Total | 23 | 12.43 ± 9.59 | 10 (2–41) |
| Variable | Bypassing Approach (n = 39) | Transparotid Approach (n = 356) | p-Value |
|---|---|---|---|
| Type of fixation | p = 0.488 | ||
| Dedicated plate | 13 (33%) | 137 (38.5%) | |
| Standard plate | 26 (67%) | 219 (61.5%) | |
| Diagnosis | p = 0.202 | ||
| No salivary fistula | 39 (100%) | 333 (93.5%) | |
| Salivary fistula | 0 | 23 (6.5%) | |
| Estimated Regression Model (Maximum Likelihood) | |||
|---|---|---|---|
| Parameter | Estimate | Standard Error | Estimated Odds Ratio |
| Constant | −2.544 | 0.221 | |
| Sex = Female 1 | −1.978 | 1.030 | 0.138 |
| Analysis of Deviance | |||
| Source | Deviance | Df | p |
| Model | 6.766 | 1 | 0.0093 2 |
| Residual | 168.66 | 393 | 1 |
| Total (corr.) | 175.43 | 394 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Agier, P.; Kozakiewicz, M.; Szymor, P. Salivary Fistula as a Complication After the ORIF of a Mandibular Condylar Process Fracture: A Single-Centre Retrospective Study. J. Funct. Biomater. 2025, 16, 326. https://doi.org/10.3390/jfb16090326
Agier P, Kozakiewicz M, Szymor P. Salivary Fistula as a Complication After the ORIF of a Mandibular Condylar Process Fracture: A Single-Centre Retrospective Study. Journal of Functional Biomaterials. 2025; 16(9):326. https://doi.org/10.3390/jfb16090326
Chicago/Turabian StyleAgier, Paulina, Marcin Kozakiewicz, and Piotr Szymor. 2025. "Salivary Fistula as a Complication After the ORIF of a Mandibular Condylar Process Fracture: A Single-Centre Retrospective Study" Journal of Functional Biomaterials 16, no. 9: 326. https://doi.org/10.3390/jfb16090326
APA StyleAgier, P., Kozakiewicz, M., & Szymor, P. (2025). Salivary Fistula as a Complication After the ORIF of a Mandibular Condylar Process Fracture: A Single-Centre Retrospective Study. Journal of Functional Biomaterials, 16(9), 326. https://doi.org/10.3390/jfb16090326







