Ellagic Acid Inclusion Complex-Loaded Hydrogels as an Efficient Controlled Release System: Design, Fabrication and In Vitro Evaluation
Abstract
1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Synthesis of HP-βCD and Ellagic Acid Inclusion Complexes (EIC)
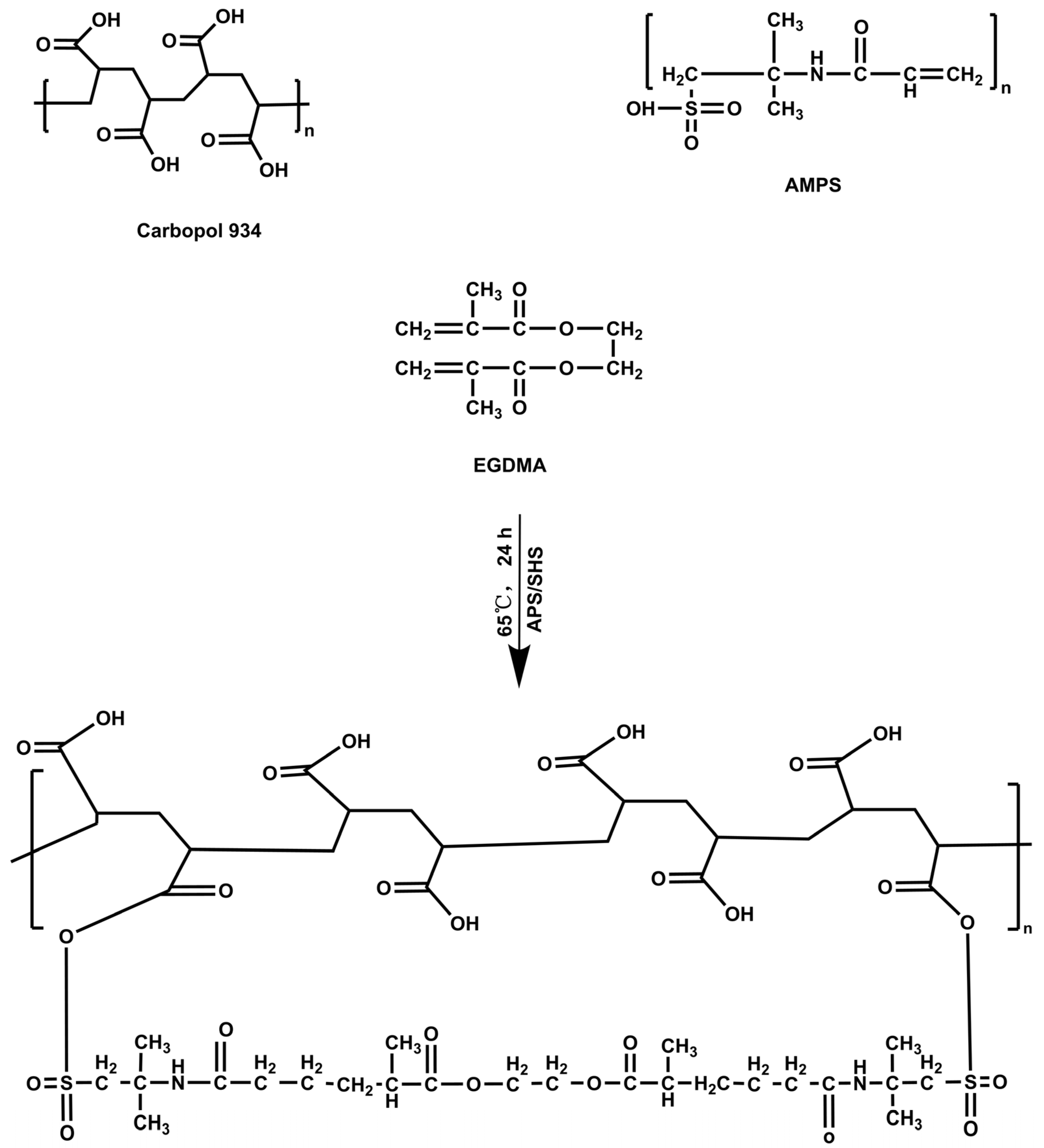
2.3. Fabrication of CP-g-AMPS Hydrogels
EIC Loading into Hydrogels
2.4. In Vitro Characterization
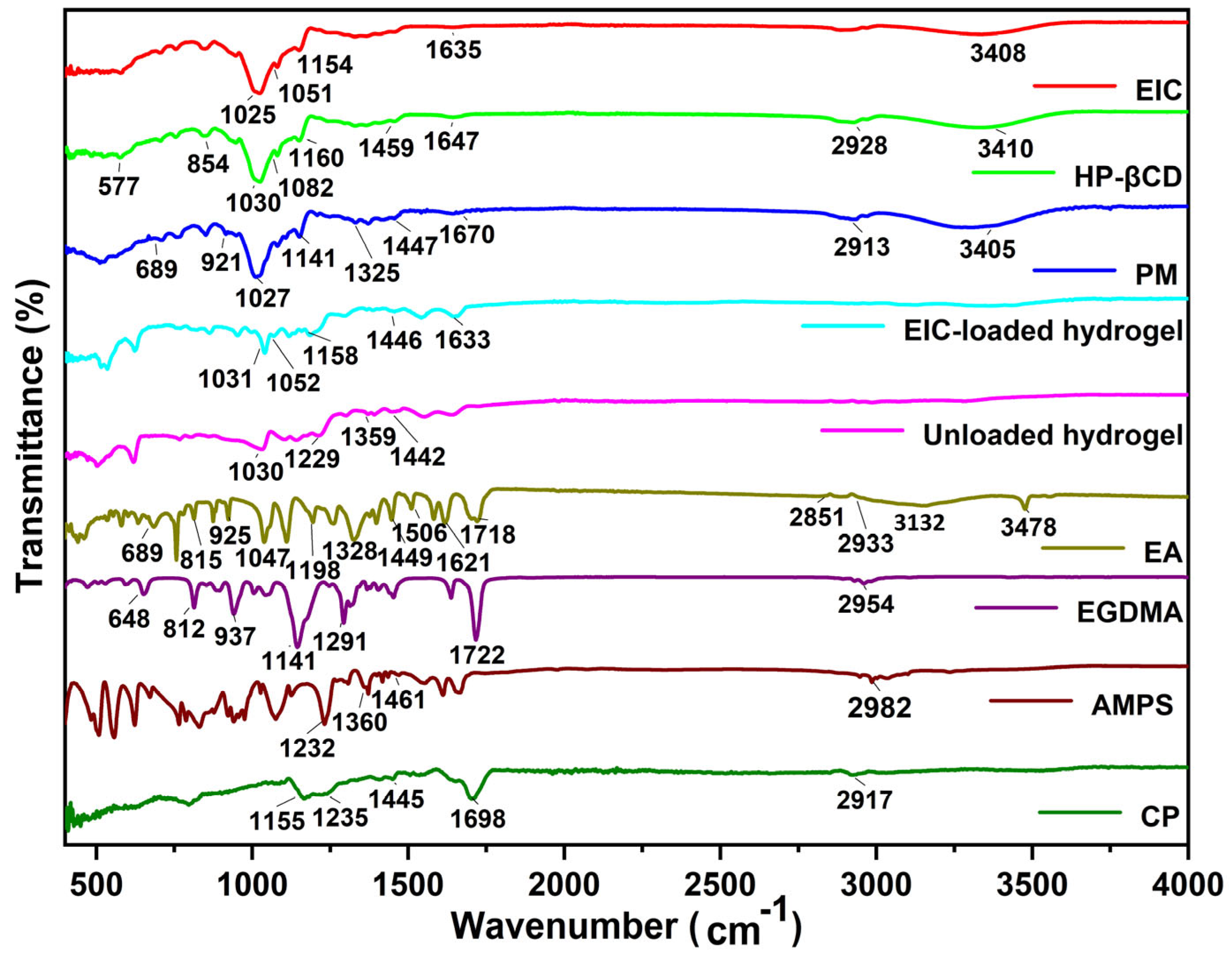
2.4.1. FTIR Spectroscopy
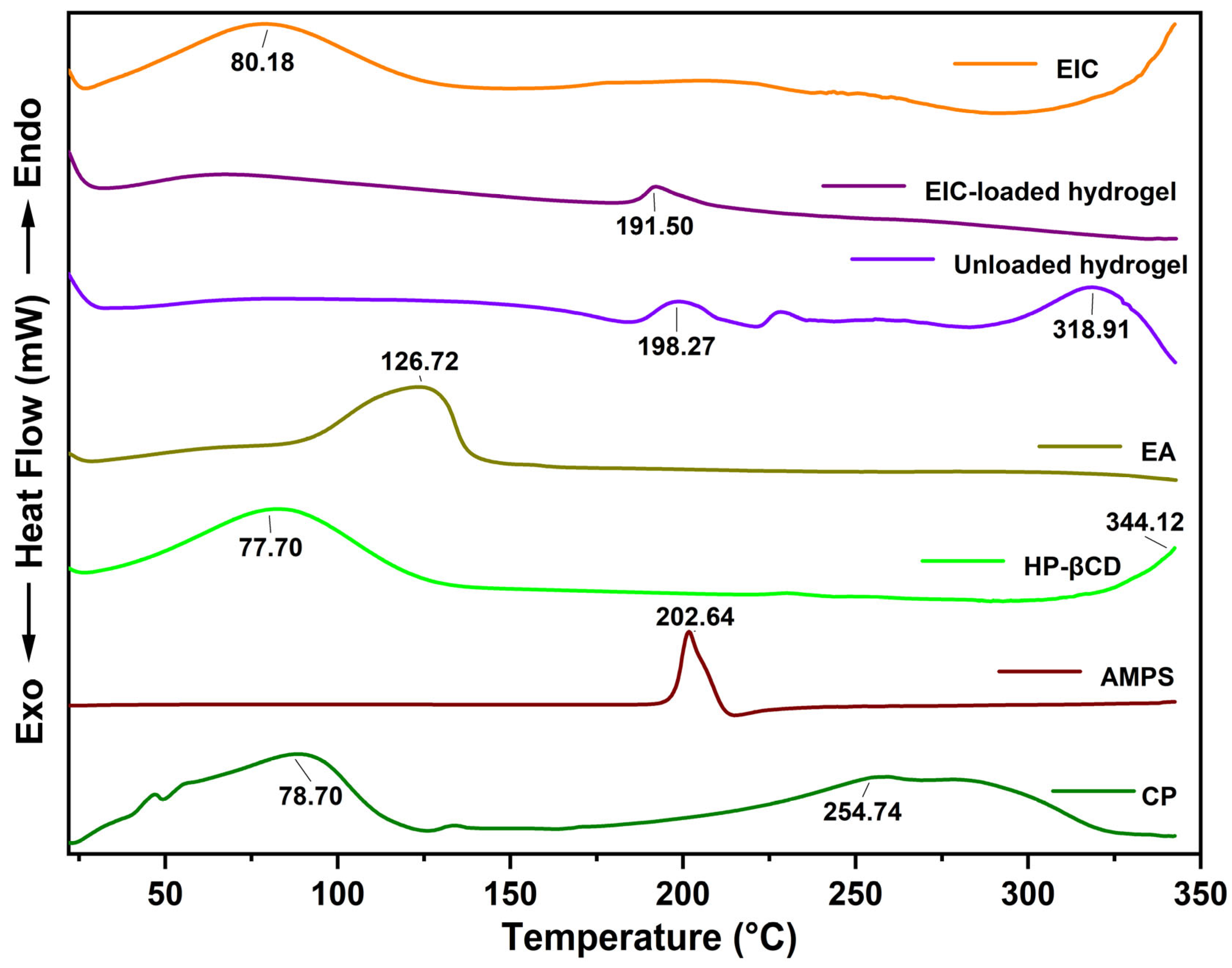
2.4.2. Thermal Analysis
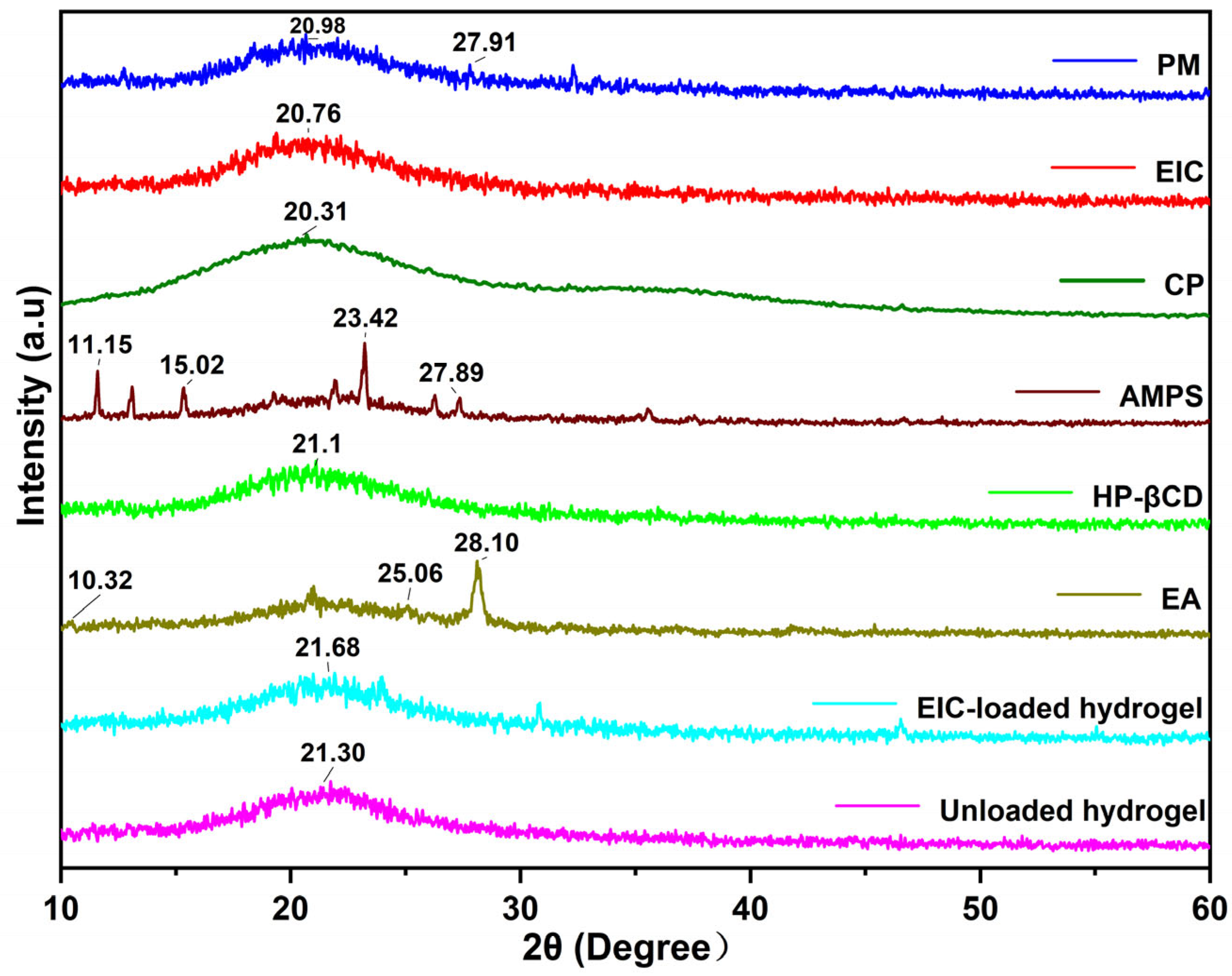
2.4.3. X-ray Diffraction
2.4.4. Scanning Electron Microscopy
2.4.5. Mechanical Characteristics
2.4.6. Sol-Gel Fraction Determination
2.4.7. Porosity Study
2.4.8. Polymer Network Parameters of CP-g-AMPS Hydrogels
2.4.9. Swelling Studies
2.4.10. In Vitro Release and Kinetics
2.4.11. Biodegradation Study
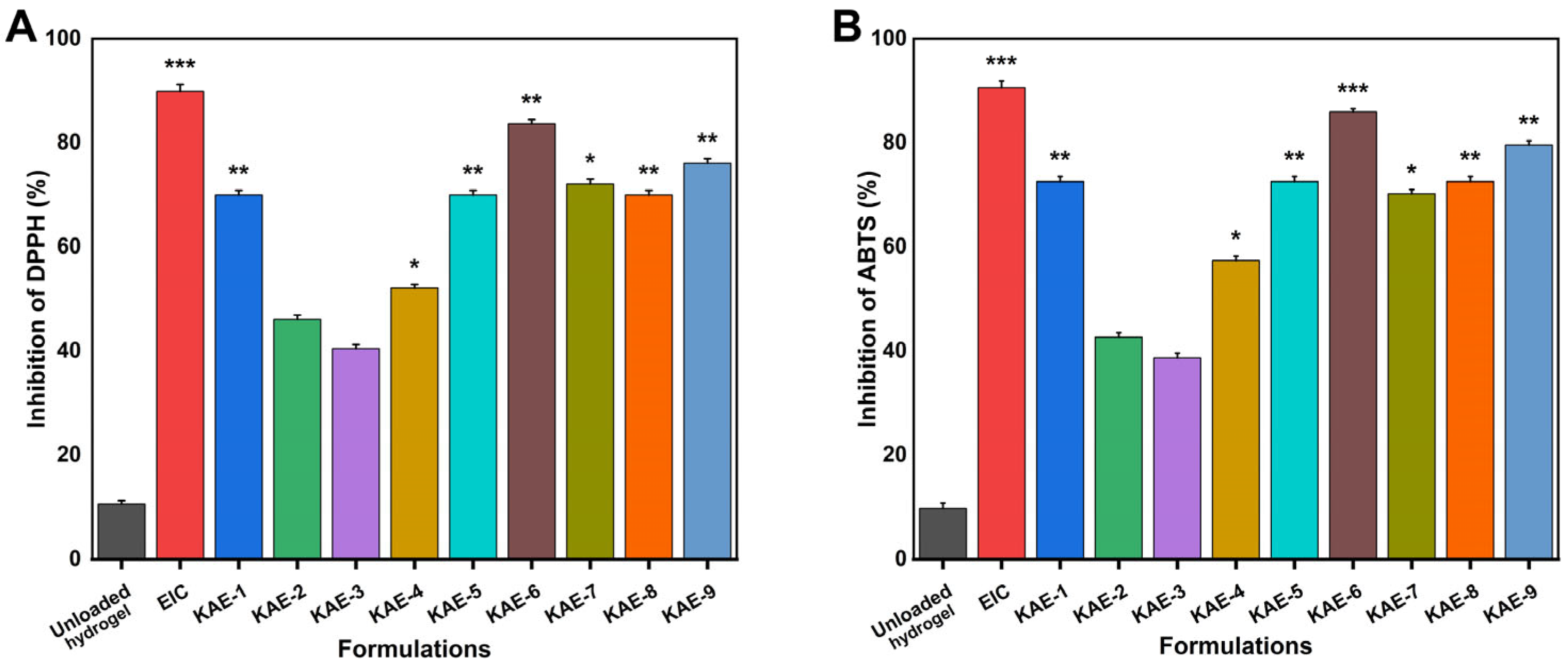
2.5. Antioxidant Studies
2.5.1. DPPH Activity
2.5.2. ABTS Activity
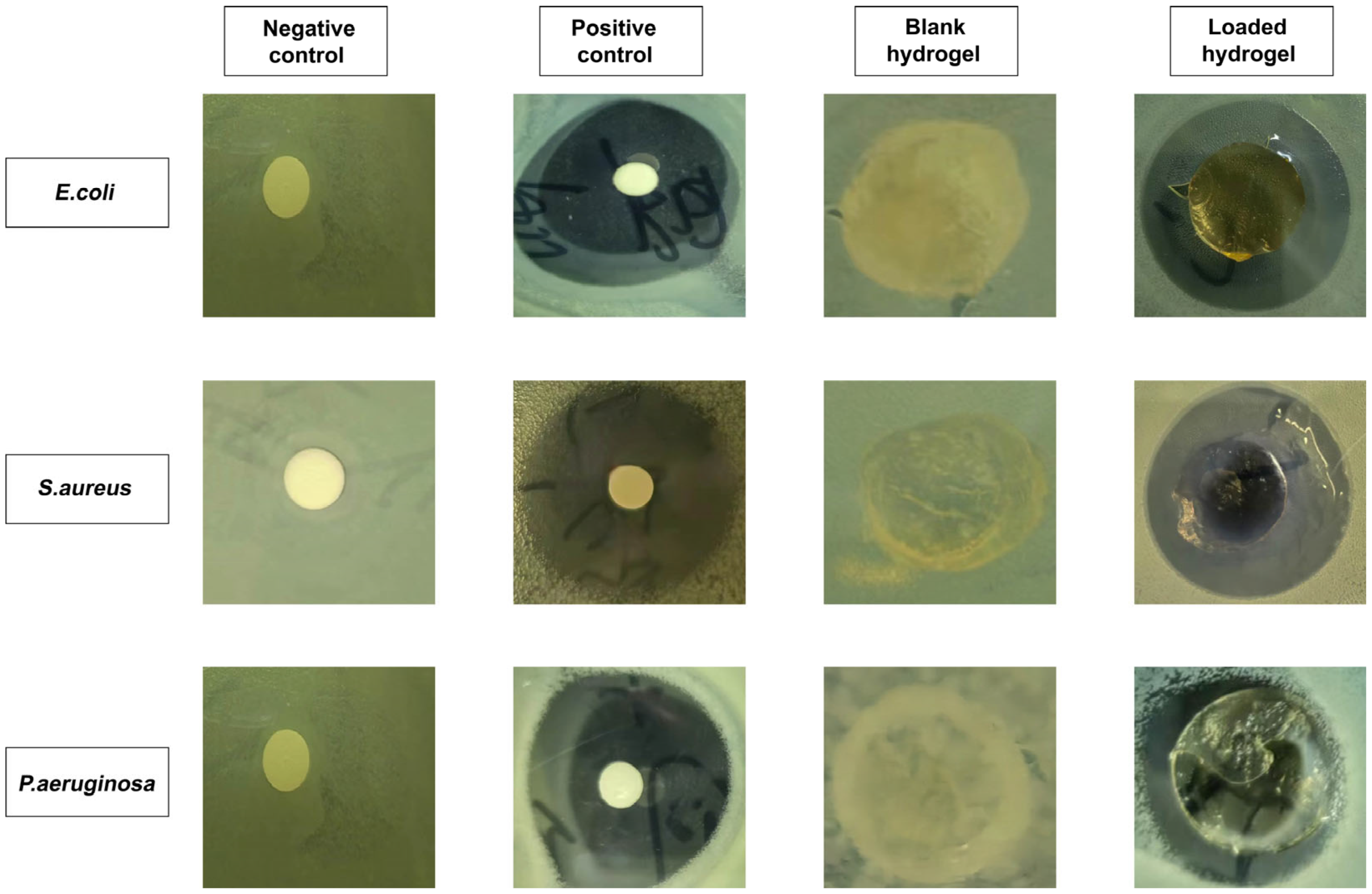
2.6. Antibacterial Activity
2.7. Statistical Analysis
3. Results and Discussion
3.1. FTIR Analysis
3.2. Thermal Analysis
3.3. XRD Study
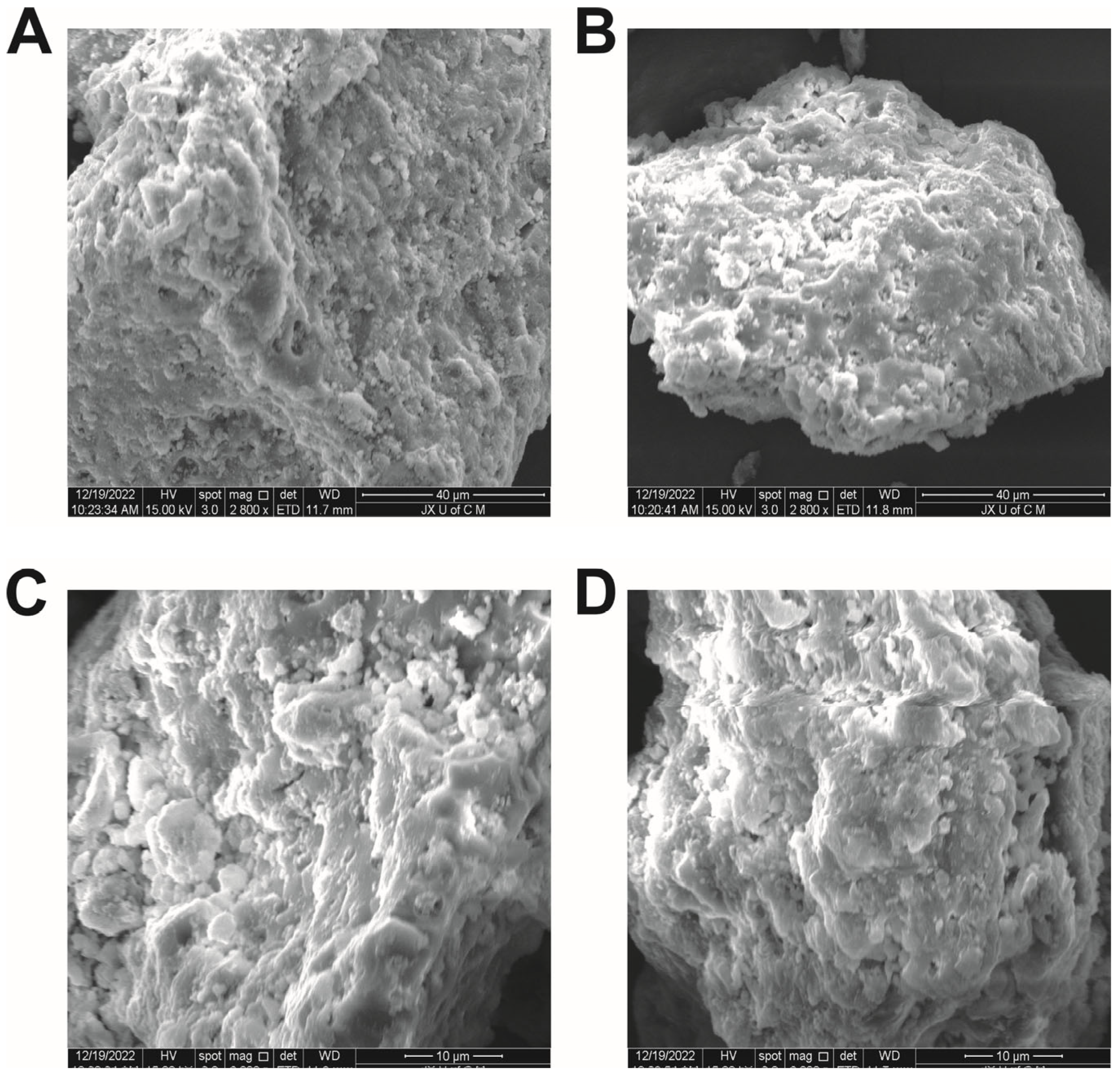
3.4. SEM Analysis
3.5. Mechanical Properties and Drug Loading
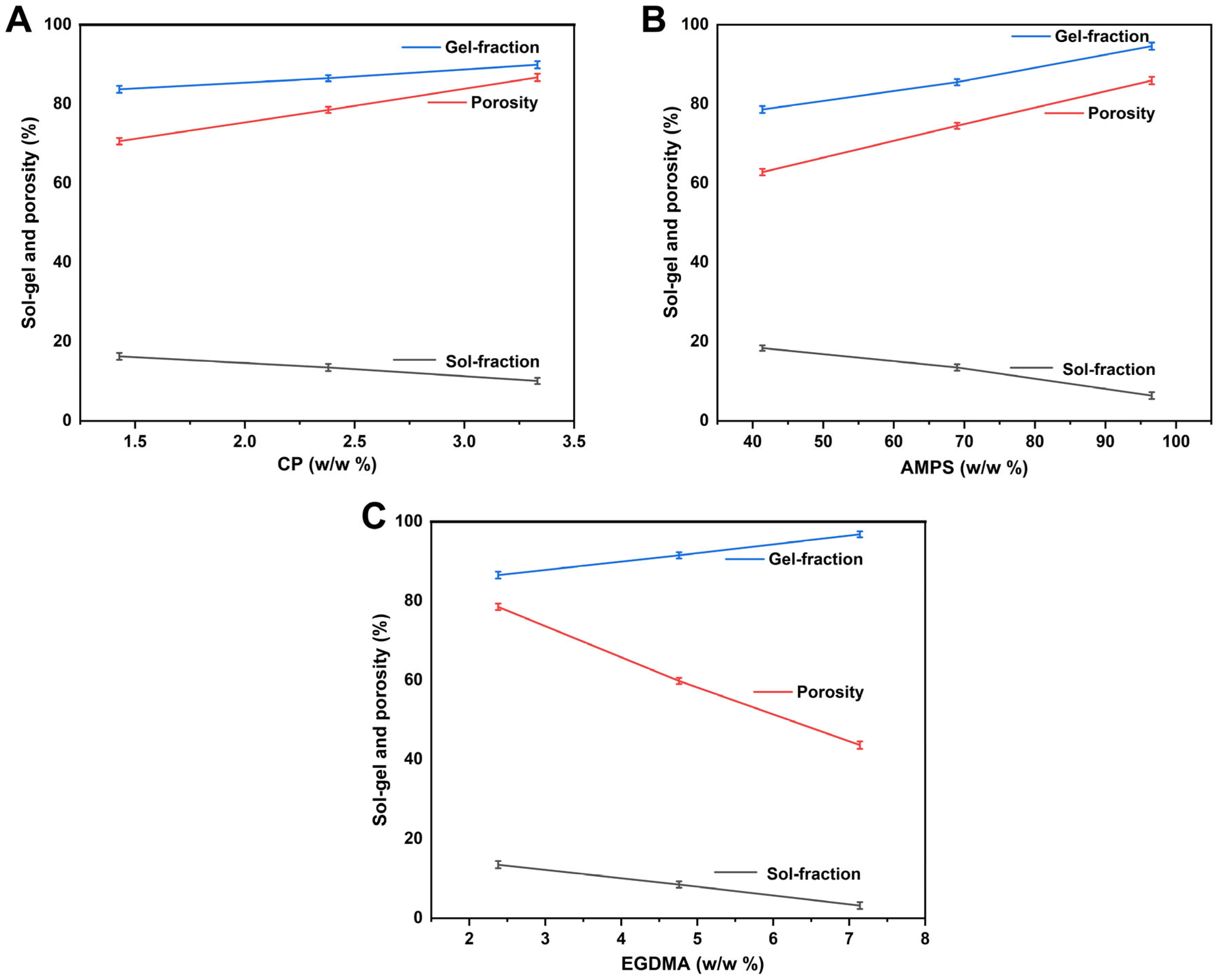
3.6. Sol–Gel Analysis
3.7. Porosity Evaluation
3.8. Biodegradation Study
3.9. Structural Parameters of Hydrogels
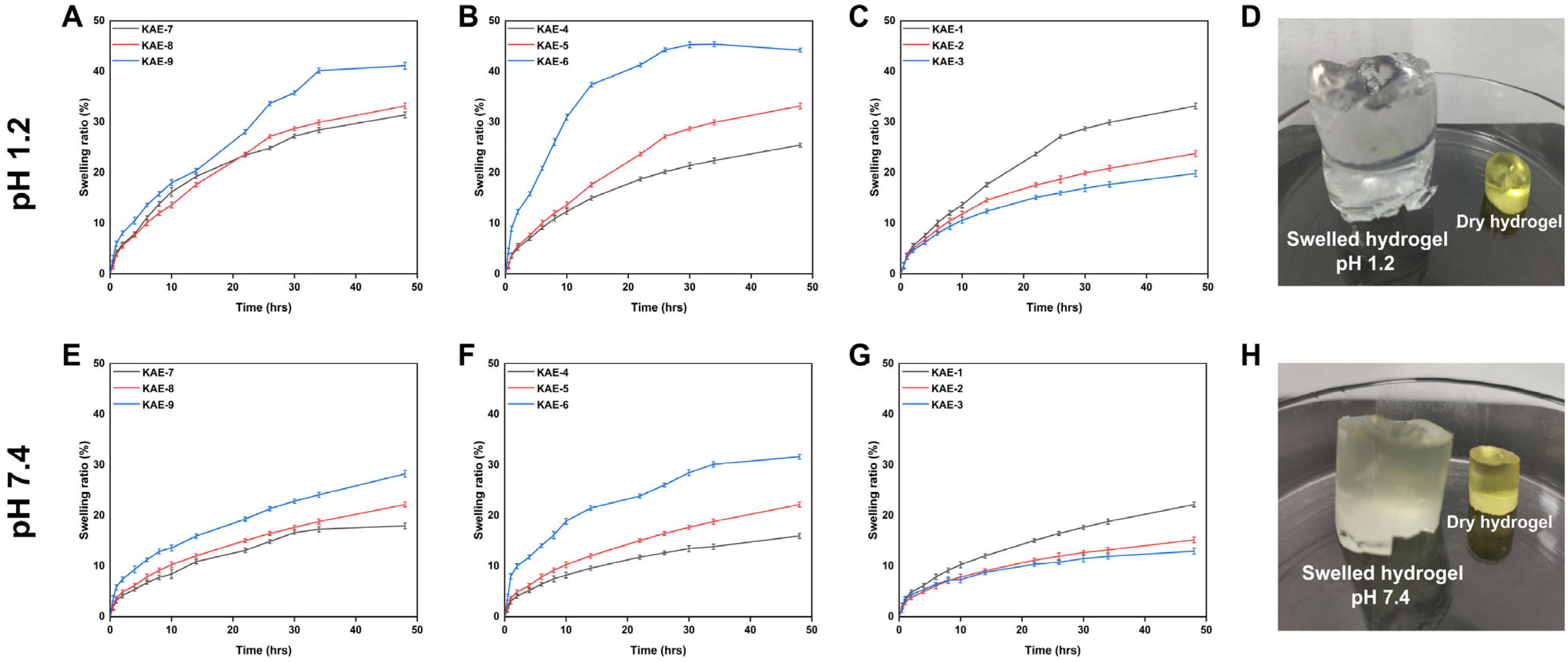
3.10. Swelling Behavior
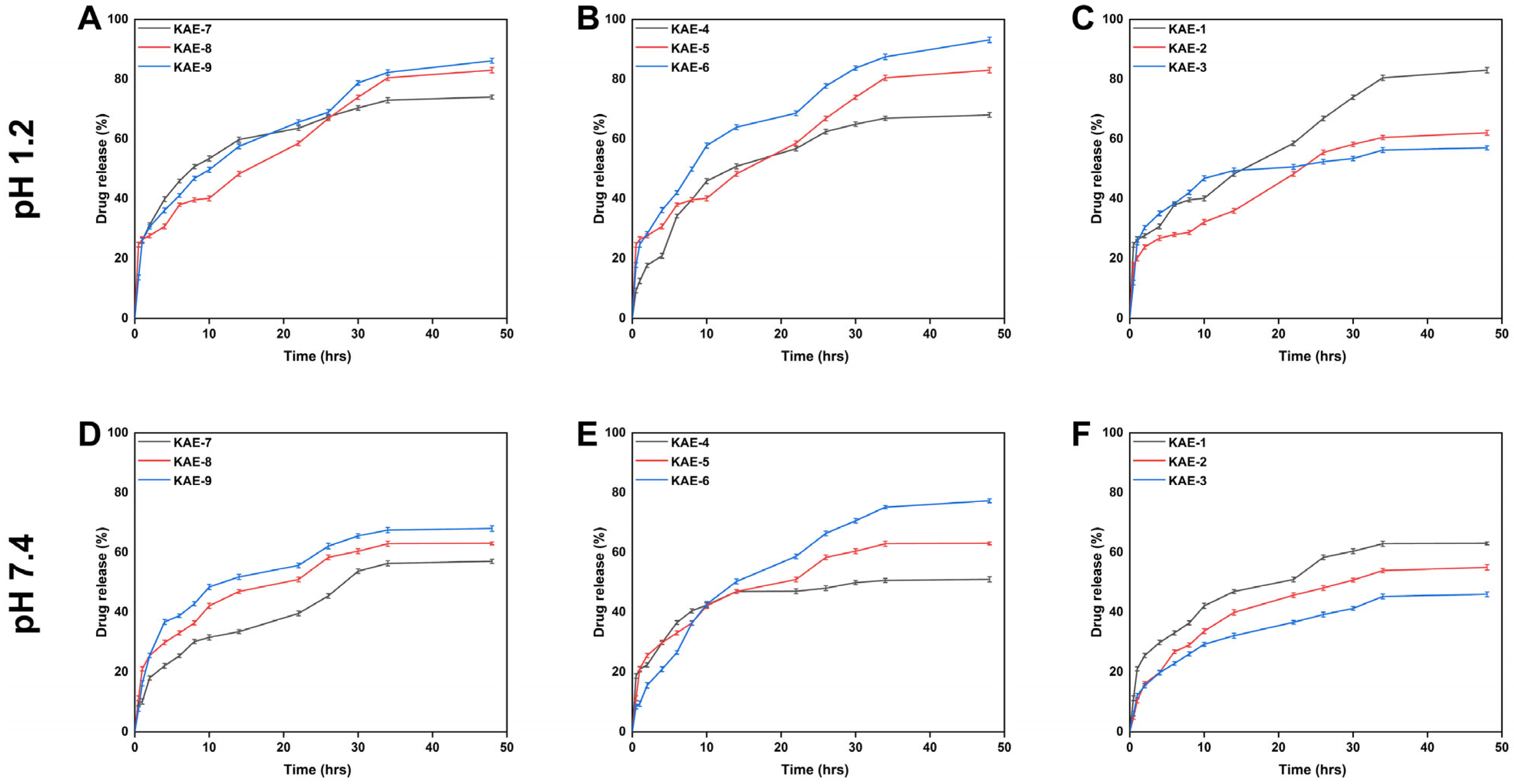
3.11. Release and Kinetic Modelling Analysis
3.12. Antioxidation Analysis
3.13. Antibacterial Study
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ortenzi, M.A.; Antenucci, S.; Marzorati, S.; Panzella, L.; Molino, S.; Rufián-Henares, J.Á.; Napolitano, A.; Verotta, L. Pectin-based formulations for controlled release of an ellagic acid salt with high solubility profile in physiological media. Molecules 2021, 26, 433. [Google Scholar] [CrossRef] [PubMed]
- Seeram, N.P.; Zhang, Y.; McKeever, R.; Henning, S.M.; Lee, R.-P.; Suchard, M.A.; Li, Z.; Chen, S.; Thames, G.; Zerlin, A. Pomegranate juice and extracts provide similar levels of plasma and urinary ellagitannin metabolites in human subjects. J. Med. Food 2008, 11, 390–394. [Google Scholar] [CrossRef]
- González-Sarrías, A.; García-Villalba, R.; Núñez-Sánchez, M.Á.; Tomé-Carneiro, J.; Zafrilla, P.; Mulero, J.; Tomás-Barberán, F.A.; Espín, J.C. Identifying the limits for ellagic acid bioavailability: A crossover pharmacokinetic study in healthy volunteers after consumption of pomegranate extracts. J. Funct. Foods 2015, 19, 225–235. [Google Scholar] [CrossRef]
- Alfei, S.; Marengo, B.; Zuccari, G. Oxidative stress, antioxidant capabilities, and bioavailability: Ellagic acid or urolithins? Antioxidants 2020, 9, 707. [Google Scholar] [CrossRef]
- Djedjibegovic, J.; Marjanovic, A.; Panieri, E.; Saso, L. Ellagic acid-derived urolithins as modulators of oxidative stress. Oxid. Med. Cell. Longev. 2020, 2020, 5194508. [Google Scholar] [CrossRef]
- Hussein, M.Z.; Al Ali, S.H.; Zainal, Z.; Hakim, M.N. Development of antiproliferative nanohybrid compound with controlled release property using ellagic acid as the active agent. Int. J. Nanomed. 2011, 6, 1373–1383. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Zhang, Y.; Tian, Z.; Ma, J.; Kang, M.; Ding, C.; Ming, D. Preparation of β-CD-ellagic acid microspheres and their effects on HepG2 cell proliferation. Molecules 2017, 22, 2175. [Google Scholar] [CrossRef] [PubMed]
- Avachat, A.M.; Patel, V.G. Self nanoemulsifying drug delivery system of stabilized ellagic acid–phospholipid complex with improved dissolution and permeability. Saudi Pharm. J. 2015, 23, 276–289. [Google Scholar] [CrossRef]
- Arulmozhi, V.; Pandian, K.; Mirunalini, S. Ellagic acid encapsulated chitosan nanoparticles for drug delivery system in human oral cancer cell line (KB). Colloids Surf. B Biointerfaces 2013, 110, 313–320. [Google Scholar] [CrossRef]
- Sampaio, A.D.G.; Gontijo, A.V.L.; Lima, G.D.M.G.; de Oliveira, M.A.C.; Lepesqueur, L.S.S.; Koga-Ito, C.Y. Ellagic acid–cyclodextrin complexes for the treatment of oral candidiasis. Molecules 2021, 26, 505. [Google Scholar] [CrossRef]
- Liu, Z.; Ye, L.; Xi, J.; Wang, J.; Feng, Z.-G. Cyclodextrin polymers: Structure, synthesis, and use as drug carriers. Prog. Polym. Sci. 2021, 118, 101408. [Google Scholar] [CrossRef]
- Carneiro, S.B.; Costa Duarte, F.Í.; Heimfarth, L.; Siqueira Quintans, J.D.S.; Quintans-Júnior, L.J.; Veiga Júnior, V.F.D.; Neves de Lima, Á.A. Cyclodextrin–drug inclusion complexes: In vivo and in vitro approaches. Int. J. Mol. Sci. 2019, 20, 642. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.-H.; Lee, S.-E.; Pyo, Y.-C.; Tran, P.; Park, J.-S. Solubility enhancement and application of cyclodextrins in local drug delivery. J. Pharm. Investig. 2020, 50, 17–27. [Google Scholar] [CrossRef]
- Ding, S.; Khan, A.I.; Cai, X.; Song, Y.; Lyu, Z.; Du, D.; Dutta, P.; Lin, Y. Overcoming blood–brain barrier transport: Advances in nanoparticle-based drug delivery strategies. Mater. Today 2020, 37, 112–125. [Google Scholar] [CrossRef] [PubMed]
- Sabbagh, F.; Kim, B.S. Recent advances in polymeric transdermal drug delivery systems. J. Control. Release 2022, 341, 132–146. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Yang, H.Y.; Lee, D.S. Advances in biodegradable and injectable hydrogels for biomedical applications. J. Control. Release 2021, 330, 151–160. [Google Scholar] [CrossRef]
- Mahmood, A.; Patel, D.; Hickson, B.; DesRochers, J.; Hu, X. Recent progress in biopolymer-based hydrogel materials for biomedical applications. Int. J. Mol. Sci. 2022, 23, 1415. [Google Scholar] [CrossRef]
- Dreiss, C.A. Hydrogel design strategies for drug delivery. Curr. Opin. Colloid Interface Sci. 2020, 48, 1–17. [Google Scholar] [CrossRef]
- Acharya, S.; Patra, S.; Pani, N.R. Optimization of HPMC and carbopol concentrations in non-effervescent floating tablet through factorial design. Carbohydr. Polym. 2014, 102, 360–368. [Google Scholar] [CrossRef]
- Safitri, F.I.; Nawangsari, D.; Febrina, D. Overview: Application of carbopol 940 in gel. In Proceedings of the International Conference on Health and Medical Sciences (AHMS 2020); Atlantis Press: Amsterdam, Netherlands, 2021; pp. 80–84. [Google Scholar]
- Seo, H.-S.; Bae, J.-Y.; Kwon, K.; Shin, S. Synthesis and assessment of amps-based copolymers prepared via electron-beam irradiation for ionic conductive hydrogels. Polymers 2022, 14, 2547. [Google Scholar] [CrossRef]
- Naeem, A.; Yu, C.; Zhu, W.; Zang, Z.; Guan, Y. Study of Hydroxypropyl β-Cyclodextrin and Puerarin Inclusion Complexes Encapsulated in Sodium Alginate-Grafted 2-Acrylamido-2-Methyl-1-Propane Sulfonic Acid Hydrogels for Oral Controlled Drug Delivery. Gels 2023, 9, 246. [Google Scholar] [CrossRef] [PubMed]
- Krstic, M.; Miladinovic, Z.R.; Barudzija, T.; Mladenovic, A.; Suljovrujic, E. Stimuli-responsive copolymeric hydrogels based on oligo (ethylene glycol) dimethacrylate for biomedical applications: An optimisation study of pH and thermoresponsive behaviour. React. Funct. Polym. 2022, 170, 105140. [Google Scholar] [CrossRef]
- Savic, I.M.; Jocic, E.; Nikolic, V.D.; Popsavin, M.M.; Rakic, S.J.; Savic-Gajic, I.M. The effect of complexation with cyclodextrins on the antioxidant and antimicrobial activity of ellagic acid. Pharm. Dev. Technol. 2019, 24, 410–418. [Google Scholar] [CrossRef] [PubMed]
- Naeem, A.; Yu, C.; Zang, Z.; Zhu, W.; Deng, X.; Guan, Y. Synthesis and Evaluation of Rutin–Hydroxypropyl β-Cyclodextrin Inclusion Complexes Embedded in Xanthan Gum-Based (HPMC-g-AMPS) Hydrogels for Oral Controlled Drug Delivery. Antioxidants 2023, 12, 552. [Google Scholar] [CrossRef]
- Li, Z.; Jiang, X.; Huang, H.; Liu, A.; Liu, H.; Abid, N.; Ming, L. Chitosan/zein films incorporated with essential oil nanoparticles and nanoemulsions: Similarities and differences. Int. J. Biol. Macromol. 2022, 208, 983–994. [Google Scholar] [CrossRef] [PubMed]
- Siddiqua, A.; Ranjha, N.M.; Rehman, S.; Shoukat, H.; Ramzan, N.; Sultana, H. Preparation and characterization of methylene bisacrylamide crosslinked pectin/acrylamide hydrogels. Polym. Bull. 2022, 79, 7655–7677. [Google Scholar] [CrossRef]
- Ghumman, S.A.; Noreen, S.; Hameed, H.; Elsherif, M.A.; Shabbir, R.; Rana, M.; Junaid, K.; Bukhari, S.N.A. Synthesis of pH-Sensitive Cross-Linked Basil Seed Gum/Acrylic Acid Hydrogels by Free Radical Copolymerization Technique for Sustained Delivery of Captopril. Gels 2022, 8, 291. [Google Scholar] [CrossRef]
- Chang, A.; Ye, Z.; Ye, Z.; Deng, J.; Lin, J.; Wu, C.; Zhu, H. Citric acid crosslinked sphingan WL gum hydrogel films supported ciprofloxacin for potential wound dressing application. Carbohydr. Polym. 2022, 291, 119520. [Google Scholar] [CrossRef]
- Guan, Y.; Yu, C.; Zang, Z.; Wan, X.; Naeem, A.; Zhang, R.; Zhu, W. Chitosan/xanthan gum-based (Hydroxypropyl methylcellulose-co-2-Acrylamido-2-methylpropane sulfonic acid) interpenetrating hydrogels for controlled release of amorphous solid dispersion of bioactive constituents of Pueraria lobatae. Int. J. Biol. Macromol. 2023, 224, 380–395. [Google Scholar] [CrossRef] [PubMed]
- Jozaghkar, M.R.; Sepehrian Azar, A.; Ziaee, F. Preparation, Characterization, and swelling study of N, N’-dimethylacrylamide/acrylic acid amphiphilic hydrogels in different conditions. Polym. Bull. 2022, 79, 5183–5195. [Google Scholar] [CrossRef]
- Khan, M.A.; Azad, A.K.; Safdar, M.; Nawaz, A.; Akhlaq, M.; Paul, P.; Hossain, M.K.; Rahman, M.H.; Baty, R.S.; El-Kott, A.F. Synthesis and Characterization of Acrylamide/Acrylic Acid Co-Polymers and Glutaraldehyde Crosslinked pH-Sensitive Hydrogels. Gels 2022, 8, 47. [Google Scholar] [CrossRef]
- Naeem, A.; Yu, C.; Zhu, W.; Chen, X.; Wu, X.; Chen, L.; Zang, Z.; Guan, Y. Gallic Acid-Loaded Sodium Alginate-Based (Polyvinyl Alcohol-Co-Acrylic Acid) Hydrogel Membranes for Cutaneous Wound Healing: Synthesis and Characterization. Molecules 2022, 27, 8397. [Google Scholar] [CrossRef] [PubMed]
- Tapdiqov, S.; Tagiyev, D.; Zeynalov, N.; Safaraliyeva, S.; Fatullayeva, S.; Hummetov, A.; Raucci, M.; Mustafayev, M.; Jafarova, R.; Shirinova, K. Cumulative release kinetics of levothyroxine-Na pentahydrate from chitosan/arabinogalactane based pH sensitive hydrogel and it’s toxicology. React. Funct. Polym. 2022, 178, 105334. [Google Scholar] [CrossRef]
- Xu, Z.; Liu, G.; Li, Q.; Wu, J. A novel hydrogel with glucose-responsive hyperglycemia regulation and antioxidant activity for enhanced diabetic wound repair. Nano Res. 2022, 15, 5305–5315. [Google Scholar] [CrossRef]
- Lorz, L.R.; Yoo, B.C.; Kim, M.-Y.; Cho, J.Y. Anti-wrinkling and anti-melanogenic effect of Pradosia mutisii methanol extract. Int. J. Mol. Sci. 2019, 20, 1043. [Google Scholar] [CrossRef] [PubMed]
- Abbasi, A.R.; Sohail, M.; Minhas, M.U.; Khaliq, T.; Kousar, M.; Khan, S.; Hussain, Z.; Munir, A. Bioinspired sodium alginate based thermosensitive hydrogel membranes for accelerated wound healing. Int. J. Biol. Macromol. 2020, 155, 751–765. [Google Scholar] [CrossRef] [PubMed]
- Mady, F.M.; Shaker, M.A. Enhanced anticancer activity and oral bioavailability of ellagic acid through encapsulation in biodegradable polymeric nanoparticles. Int. J. Nanomed. 2017, 12, 7405. [Google Scholar] [CrossRef]
- Ali, A.; Khalid, I.; Minhas, M.U.; Barkat, K.; Khan, I.U.; Syed, H.K.; Umar, A. Preparation and in vitro evaluation of Chondroitin sulfate and carbopol based mucoadhesive controlled release polymeric composites of Loxoprofen using factorial design. Eur. Polym. J. 2019, 121, 109312. [Google Scholar] [CrossRef]
- Yu, C.; Chen, X.; Zhu, W.; Li, L.; Peng, M.; Zhong, Y.; Naeem, A.; Zang, Z.; Guan, Y. Synthesis of Gallic Acid-Loaded Chitosan-Grafted-2-Acrylamido-2-Methylpropane Sulfonic Acid Hydrogels for Oral Controlled Drug Delivery: In Vitro Biodegradation, Antioxidant, and Antibacterial Effects. Gels 2022, 8, 806. [Google Scholar] [CrossRef] [PubMed]
- Maciejewska, M.; Rogulska, M.; Józwicki, M.; Głodowska, N. Synthesis and characterization of porous copolymers of 2-hydroxyethyl methacrylate with ethylene glycol dimethacrylate. Polym. Adv. Technol. 2021, 32, 2566–2575. [Google Scholar] [CrossRef]
- Sarfraz, M.; Iqbal, R.; Khan, K.U.; Minhas, M.U. Carbopol Based Hydrogels for ITOPRIDE Hydrochloride Delivery; Synthesis, Characterization and Comparative Assessment with Various Monomers. J. Funct. Biomater. 2022, 13, 295. [Google Scholar] [CrossRef] [PubMed]
- Hussein-Al-Ali, S.H.; Abudoleh, S.M.; Hussein, M.Z.; Bullo, S.; Palanisamy, A. Graphene oxide-ellagic acid nanocomposite as effective anticancer and antimicrobial agent. IET Nanobiotechnol. 2021, 15, 79–89. [Google Scholar] [CrossRef] [PubMed]
- Khan, S.A.; Azam, W.; Ashames, A.; Fahelelbom, K.M.; Ullah, K.; Mannan, A.; Murtaza, G. β-Cyclodextrin-based (IA-co-AMPS) Semi-IPNs as smart biomaterials for oral delivery of hydrophilic drugs: Synthesis, characterization, in-Vitro and in-Vivo evaluation. J. Drug Deliv. Sci. Technol. 2020, 60, 101970. [Google Scholar] [CrossRef]
- Sun, C.; Cao, J.; Wang, Y.; Chen, J.; Huang, L.; Zhang, H.; Wu, J.; Sun, C. Ultrasound-mediated molecular self-assemble of thymol with 2-hydroxypropyl-β-cyclodextrin for fruit preservation. Food Chem. 2021, 363, 130327. [Google Scholar] [CrossRef]
- Abarca, R.L.; Rodriguez, F.J.; Guarda, A.; Galotto, M.J.; Bruna, J.E. Characterization of beta-cyclodextrin inclusion complexes containing an essential oil component. Food Chem. 2016, 196, 968–975. [Google Scholar] [CrossRef] [PubMed]
- Sakurai, H.; Suzuki, M.; Itakura, S.; Todo, H.; Arce, F., Jr.; See, G.L.; Tanikawa, T.; Inoue, Y. Preparation, characterization, solubility, and antioxidant capacity of ellagic acid-urea complex. Materials 2022, 15, 2836. [Google Scholar] [CrossRef]
- Dudhipala, N.; Ettireddy, S.; Youssef, A.A.A.; Puchchakayala, G. Cyclodextrin complexed lipid nanoparticles of irbesartan for oral applications: Design, development, and in vitro characterization. Molecules 2021, 26, 7538. [Google Scholar] [CrossRef]
- Suhail, M.; Fang, C.-W.; Khan, A.; Minhas, M.U.; Wu, P.-C. Fabrication and in vitro evaluation of pH-sensitive polymeric hydrogels as controlled release carriers. Gels 2021, 7, 110. [Google Scholar] [CrossRef]
- Wang, J.; Yang, F. Preparation of 2-hydroxypropyl-β-cyclodextrin polymers crosslinked by poly(acrylic acid) for efficient removal of ibuprofen. Mater. Lett. 2021, 284, 128882. [Google Scholar] [CrossRef]
- Li, Y.; Mei, L.; Guan, X.; Hu, Y. Ellagic acid solid dispersion: Characterization and bioactivity in the hydroxyl radical oxidation system. Food Res. Int. 2021, 142, 110184. [Google Scholar] [CrossRef] [PubMed]
- Khan, S.; Anwar, N. Gelatin/carboxymethyl cellulose based stimuli-responsive hydrogels for controlled delivery of 5-fluorouracil, development, in vitro characterization, in vivo safety and bioavailability evaluation. Carbohydr. Polym. 2021, 257, 117617. [Google Scholar] [CrossRef]
- Park, D.W.; Haam, S.; Lee, T.G.; Kim, H.S.; Kim, W.S. Chemoenzymatic synthesis of sugar-containing biocompatible hydrogels: Crosslinked poly(β-methylglucoside acrylate) and poly(β-methylglucoside methacrylate). J. Biomed. Mater. Res. Part A 2004, 71, 497–507. [Google Scholar] [CrossRef]
- Liu, C.; Tripathi, A.K.; Gao, W.; Tsavalas, J.G. Crosslinking in Semi-Batch Seeded Emulsion Polymerization: Effect of Linear and Non-Linear Monomer Feeding Rate Profiles on Gel Formation. Polymers 2021, 13, 596. [Google Scholar] [CrossRef] [PubMed]
- Tabassum, M.; Pervaiz, F.; Shoukat, H. Fabrication and evaluation of gelatin-PVA-co-poly(2-acrylamido-2-methylpropane sulfonic acid)-based hydrogels for extended-release of sitagliptin and metformin by employing response surface methodology. Chem. Pap. 2022, 76, 4081–4097. [Google Scholar] [CrossRef]
- Khanum, H.; Ullah, K.; Murtaza, G.; Khan, S.A. Fabrication and in vitro characterization of HPMC-g-poly (AMPS) hydrogels loaded with loxoprofen sodium. Int. J. Biol. Macromol. 2018, 120, 1624–1631. [Google Scholar] [CrossRef]
- Suhail, M.; Liu, J.-Y.; Hung, M.-C.; Chiu, I.-H.; Minhas, M.U.; Wu, P.-C. Preparation, In Vitro Characterization, and Cytotoxicity Evaluation of Polymeric pH-Responsive Hydrogels for Controlled Drug Release. Pharmaceutics 2022, 14, 1864. [Google Scholar] [CrossRef] [PubMed]
- Jalil, A.; Khan, S.; Naeem, F.; Haider, M.S.; Sarwar, S.; Riaz, A.; Ranjha, N.M. The structural, morphological and thermal properties of grafted pH-sensitive interpenetrating highly porous polymeric composites of sodium alginate/acrylic acid copolymers for controlled delivery of diclofenac potassium. Des. Monomers Polym. 2017, 20, 308–324. [Google Scholar] [CrossRef] [PubMed]
- Singh, B.; Sharma, V. Influence of polymer network parameters of tragacanth gum-based pH responsive hydrogels on drug delivery. Carbohydr. Polym. 2014, 101, 928–940. [Google Scholar] [CrossRef]
- Wang, W.; Wang, A. Synthesis and swelling properties of pH-sensitive semi-IPN superabsorbent hydrogels based on sodium alginate-g-poly(sodium acrylate) and polyvinylpyrrolidone. Carbohydr. Polym. 2010, 80, 1028–1036. [Google Scholar] [CrossRef]
- Richbourg, N.; Wancura, M.; Gilchrist, A.; Toubbeh, S.; Harley, B.; Cosgriff-Hernandez, E.; Peppas, N. Precise control of synthetic hydrogel network structure via linear, independent synthesis-swelling relationships. Sci. Adv. 2021, 7, eabe3245. [Google Scholar] [CrossRef]
- Khalid, I.; Ahmad, M.; Minhas, M.U.; Barkat, K. Synthesis and evaluation of chondroitin sulfate based hydrogels of loxoprofen with adjustable properties as controlled release carriers. Carbohydr. Polym. 2018, 181, 1169–1179. [Google Scholar] [CrossRef] [PubMed]
- Suhail, M.; Shih, C.-M.; Liu, J.-Y.; Hsieh, W.-C.; Lin, Y.-W.; Minhas, M.U.; Wu, P.-C. Synthesis, Characterization, In-Vitro and In-Vivo Evaluation of Ketorolac Tromethamine-Loaded Hydrogels of Glutamic Acid as Controlled Release Carrier. Polymers 2021, 13, 3541. [Google Scholar] [CrossRef] [PubMed]
- Li, D.-Q.; Wang, S.-Y.; Meng, Y.-J.; Guo, Z.-W.; Cheng, M.-M.; Li, J. Fabrication of self-healing pectin/chitosan hybrid hydrogel via Diels-Alder reactions for drug delivery with high swelling property, pH-responsiveness, and cytocompatibility. Carbohydr. Polym. 2021, 268, 118244. [Google Scholar] [CrossRef]
- Khan, M.U.A.; Yaqoob, Z.; Ansari, M.N.M.; Razak, S.I.A.; Raza, M.A.; Sajjad, A.; Haider, S.; Busra, F.M. Chitosan/poly vinyl alcohol/graphene oxide based pH-responsive composite hydrogel films: Drug release, anti-microbial and cell viability studies. Polymers 2021, 13, 3124. [Google Scholar] [CrossRef] [PubMed]
- Hanna, D.H.; Lotfy, V.F.; Basta, A.H.; Saad, G.R. Comparative evaluation for controlling release of niacin from protein-and cellulose-chitosan based hydrogels. Int. J. Biol. Macromol. 2020, 150, 228–237. [Google Scholar] [CrossRef]
- Ritger, P.L.; Peppas, N.A. A simple equation for description of solute release I. Fickian and non-fickian release from non-swellable devices in the form of slabs, spheres, cylinders or discs. J. Control. Release 1987, 5, 23–36. [Google Scholar] [CrossRef]
- Derosa, G.; Maffioli, P.; Sahebkar, A. Ellagic acid and its role in chronic diseases. In Anti-Nutraceuticals and Chronic Diseases; Springer: Cham, Switzerland, 2016; pp. 473–479. [Google Scholar]
- Yayan, J.; Ghebremedhin, B.; Rasche, K. Cefepime shows good efficacy and no antibiotic resistance in pneumonia caused by Serratia marcescens and Proteus mirabilis–An observational study. BMC Pharmacol. Toxicol. 2016, 17, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Kamaci, M.; Kaya, I. Melamine-based poly(azomethine) hydrogels: Mechanical, biodegradability, drug loading and antibacterial properties. Eur. Polym. J. 2018, 108, 107–115. [Google Scholar] [CrossRef]


| Formulation Codes | Carbopol-934 (g) | APS/SHS (g) | AMPS (g) | EGDMA (g) |
|---|---|---|---|---|
| KAE-1 | 0.5/15 | 0.3/0.3/4 | 20/15 | 0.5 |
| KAE-2 | 0.5/15 | 0.3/0.3/4 | 20/15 | 1 |
| KAE-3 | 0.5/15 | 0.3/0.3/4 | 20/15 | 1.5 |
| KAE-4 | 0.5/15 | 0.3/0.3/4 | 12/15 | 0.5 |
| KAE-5 | 0.5/15 | 0.3/0.3/4 | 20/15 | 0.5 |
| KAE-6 | 0.5/15 | 0.3/0.3/4 | 28/15 | 0.5 |
| KAE-7 | 0.3/15 | 0.3/0.3/4 | 20/15 | 0.5 |
| KAE-8 | 0.5/15 | 0.3/0.3/4 | 20/15 | 0.5 |
| KAE-9 | 0.7/15 | 0.3/0.3/4 | 20/15 | 0.5 |
| F. Codes | Thickness (mm) | TS (N/m2) | EAB (%) | EIC-Loaded per 1 g Hydrogel (g) |
|---|---|---|---|---|
| KAE-1 | 1.15 ± 0.005 | 0.502 ± 0.103 | 46.3 ± 1.056 | 0.487 ± 0.013 |
| KAE-2 | 1.25 ± 0.007 | 0.676 ± 0.086 | 59.9 ± 1.687 | 0.417 ± 0.006 |
| KAE-3 | 1.37 ± 0.004 | 1.107 ± 0.076 | 72.6 ± 1.551 | 0.329 ± 0.010 |
| KAE-4 | 1.05 ± 0.003 | 0.816 ± 0.059 | 63.2 ± 2.922 | 0.460 ± 0.008 |
| KAE-5 | 1.15 ± 0.005 | 0.502 ± 0.103 | 46.3 ± 1.056 | 0.487 ± 0.013 |
| KAE-6 | 1.08 ± 0.008 | 0.413 ± 0.237 | 38.6 ± 1.687 | 0.596 ± 0.098 |
| KAE-7 | 1.09 ± 0.004 | 0.517 ± 0.211 | 50.8 ± 2.398 | 0.499 ± 0.069 |
| KAE-8 | 1.15 ± 0.005 | 0.502 ± 0.103 | 46.3 ± 1.056 | 0.487 ± 0.013 |
| KAE-9 | 1.47 ± 0.007 | 0.581 ± 0.051 | 60.7 ± 1.201 | 0.518 ± 0.029 |
| F. Codes | V2,s | χ | Mc | Mr | N | D × 10−5 (cm2 s−1) |
|---|---|---|---|---|---|---|
| KAE-1 | 0.030 | 0.510 | 3773.9 | 203.571 | 37.076 | 0.023 |
| KAE-2 | 0.042 | 0.514 | 2356.7 | 224.307 | 21.013 | 0.031 |
| KAE-3 | 0.050 | 0.517 | 1444.4 | 203.318 | 14.208 | 0.037 |
| KAE-4 | 0.039 | 0.513 | 2358.4 | 201.461 | 23.412 | 0.028 |
| KAE-5 | 0.030 | 0.510 | 3773.9 | 203.571 | 37.076 | 0.023 |
| KAE-6 | 0.022 | 0.507 | 4363.8 | 204.517 | 42.674 | 0.015 |
| KAE-7 | 0.031 | 0.510 | 2589.6 | 204.836 | 25.284 | 0.021 |
| KAE-8 | 0.030 | 0.510 | 3773.9 | 203.571 | 37.076 | 0.023 |
| KAE-9 | 0.024 | 0.508 | 3311.8 | 202.330 | 32.736 | 0.018 |
| F. Codes | pH | Zero Order. | First Order | Higuchi Model | Korsmeyer-Peppas Model | ||||
|---|---|---|---|---|---|---|---|---|---|
| Ko (h−1) | r2 | K1 (h−1) | r2 | K2 (h−1) | r2 | r2 | n | ||
| KAE-1 | 1.2 | 0.890 | 0.9640 | 0.011 | 0.9801 | 4.897 | 0.9942 | 0.9949 * | 0.482 |
| 7.4 | 0.576 | 0.9624 | 0.007 | 0.9714 | 3.218 | 0.9997 | 0.9998 * | 0.495 | |
| KAE-2 | 1.2 | 0.644 | 0.9467 | 0.007 | 0.9599 | 3.609 | 0.9972 | 0.9976 * | 0.484 |
| 7.4 | 0.411 | 0.9424 | 0.005 | 0.9505 | 2.324 | 0.9970 | 0.9988 * | 0.444 | |
| KAE-3 | 1.2 | 0.547 | 0.9372 | 0.006 | 0.9492 | 3.090 | 0.9956 | 0.9974 * | 0.454 |
| 7.4 | 0.372 | 0.9129 | 0.004 | 0.9215 | 2.138 | 0.9878 | 0.9983 * | 0.360 | |
| KAE-4 | 1.2 | 0.687 | 0.9513 | 0.008 | 0.9650 | 3.839 | 0.9978 * | 0.9977 | 0.498 |
| 7.4 | 0.434 | 0.9421 | 0.005 | 0.9507 | 2.450 | 0.9969 | 0.9987 * | 0.445 | |
| KAE-5 | 1.2 | 0.890 | 0.9640 | 0.011 | 0.9801 | 4.897 | 0.9942 | 0.9949 * | 0.482 |
| 7.4 | 0.576 | 0.9624 | 0.007 | 0.9714 | 3.218 | 0.9997 | 0.9998 * | 0.495 | |
| KAE-6 | 1.2 | 1.406 | 0.8748 | 0.021 | 0.9294 | 8.087 | 0.9669 * | 0.9963 | 0.401 |
| 7.4 | 0.835 | 0.8536 | 0.010 | 0.8689 | 4.801 | 0.9918 | 0.9937 * | 0.356 | |
| KAE-7 | 1.2 | 0.860 | 0.9462 | 0.011 | 0.9469 | 4.808 | 0.9954 | 0.9952 * | 0.479 |
| 7.4 | 0.445 | 0.9422 | 0.005 | 0.9510 | 2.515 | 0.9973 | 0.9993 * | 0.435 | |
| KAE-8 | 1.2 | 0.890 | 0.9640 | 0.011 | 0.9801 | 4.897 | 0.9942 | 0.9949 * | 0.482 |
| 7.4 | 0.576 | 0.9624 | 0.007 | 0.9714 | 3.218 | 0.9997 | 0.9998 * | 0.495 | |
| KAE-9 | 1.2 | 1.119 | 0.9638 | 0.015 | 0.9825 | 6.179 | 0.9919 | 0.9927 * | 0.459 |
| 7.4 | 0.746 | 0.9530 | 0.008 | 0.9652 | 4.206 | 0.9982 | 0.9992 * | 0.437 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yu, C.; Naeem, A.; Liu, Y.; Guan, Y. Ellagic Acid Inclusion Complex-Loaded Hydrogels as an Efficient Controlled Release System: Design, Fabrication and In Vitro Evaluation. J. Funct. Biomater. 2023, 14, 278. https://doi.org/10.3390/jfb14050278
Yu C, Naeem A, Liu Y, Guan Y. Ellagic Acid Inclusion Complex-Loaded Hydrogels as an Efficient Controlled Release System: Design, Fabrication and In Vitro Evaluation. Journal of Functional Biomaterials. 2023; 14(5):278. https://doi.org/10.3390/jfb14050278
Chicago/Turabian StyleYu, Chengqun, Abid Naeem, Yali Liu, and Yongmei Guan. 2023. "Ellagic Acid Inclusion Complex-Loaded Hydrogels as an Efficient Controlled Release System: Design, Fabrication and In Vitro Evaluation" Journal of Functional Biomaterials 14, no. 5: 278. https://doi.org/10.3390/jfb14050278
APA StyleYu, C., Naeem, A., Liu, Y., & Guan, Y. (2023). Ellagic Acid Inclusion Complex-Loaded Hydrogels as an Efficient Controlled Release System: Design, Fabrication and In Vitro Evaluation. Journal of Functional Biomaterials, 14(5), 278. https://doi.org/10.3390/jfb14050278






