The Effect of Polishing, Glazing, and Aging on Optical Characteristics of Multi-Layered Dental Zirconia with Different Degrees of Translucency
Abstract
1. Introduction
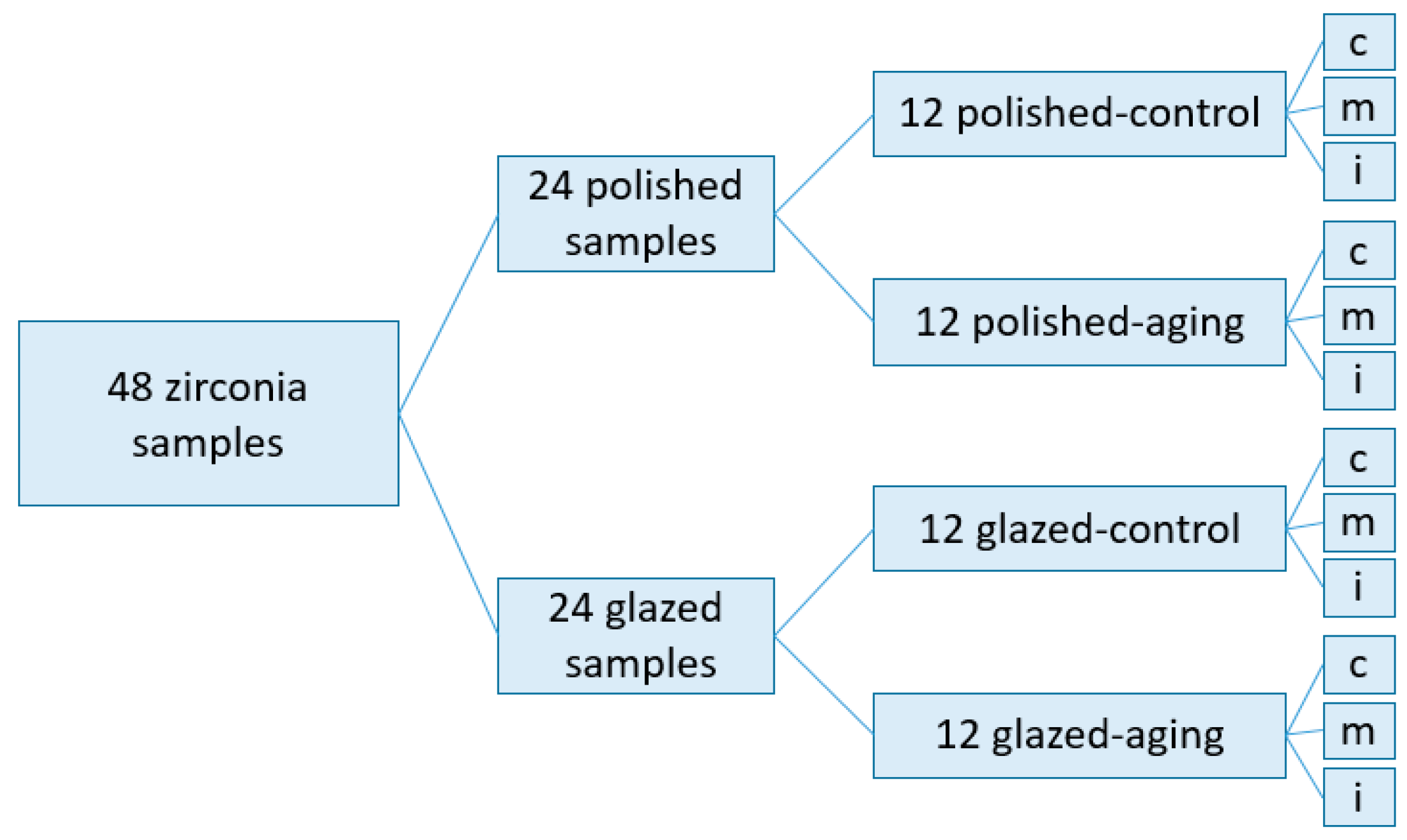
2. Materials and Methods
2.1. Specimen Preparation
2.2. Hydrothermal Aging Protocol
2.3. Optical and Color Change Measurements
2.4. Statistical Analysis
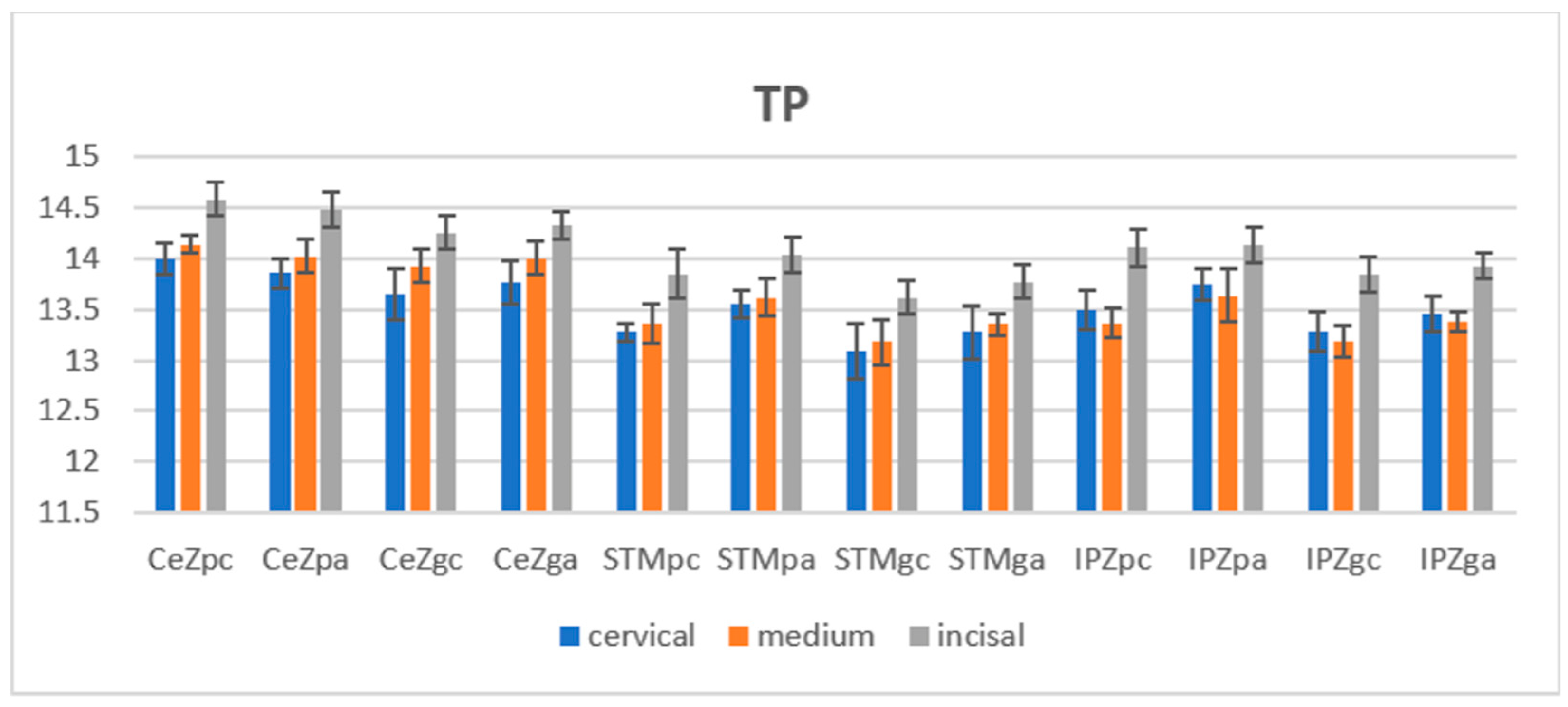
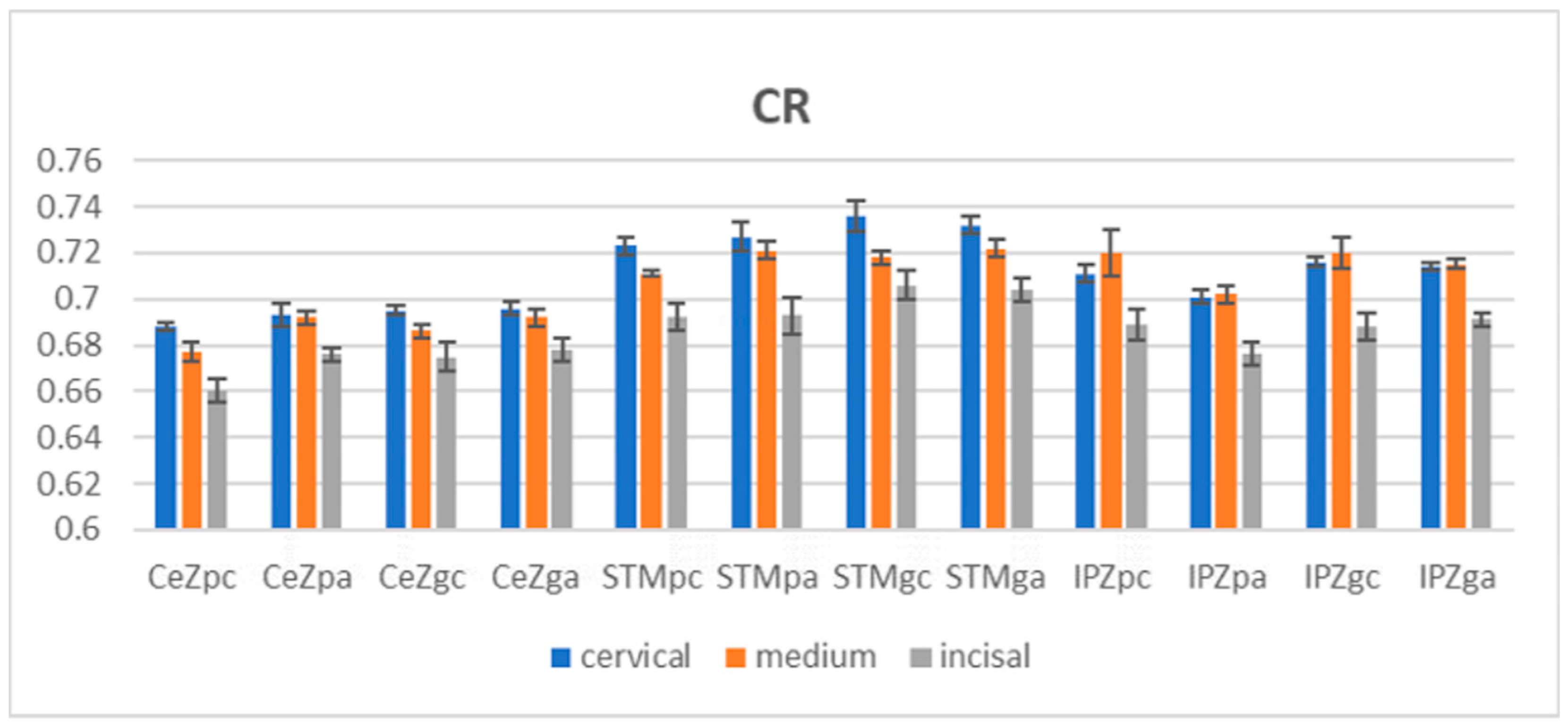
3. Results
4. Discussion
5. Conclusions
- Polishing and glazing, as surface treatments, influence the optical properties of zirconia; the translucency of the polished samples was higher than that of the glazed samples before and after aging.
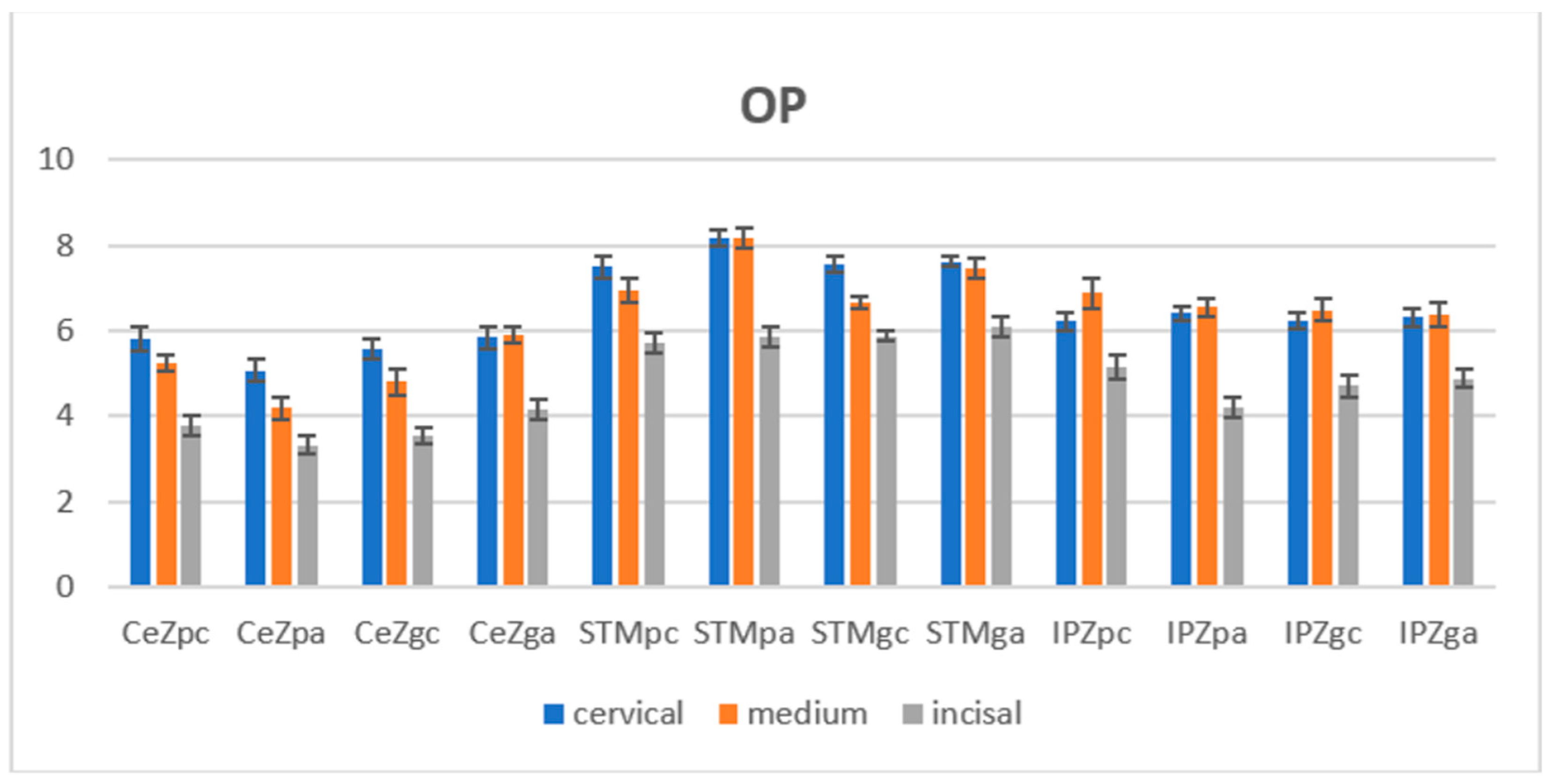
- After aging, the mean TP and OP values were increased for all materials except polished CeZ; the super-high translucent zirconia was less affected by LTD.
- The levels of color change were between extremely slight to perceivable.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Salmang, H.; Scholze, H. Keramik Vollständing Neuarbeitete und Erweiterte Auflage; Springer: Berlin/Heidelberg, Germany, 2007; Volume 7, pp. 817–838. [Google Scholar]
- Holleman-Wiberg, E. Lehrbuch der Anorganischen Chemie, 101st ed.; Walterde Gruyter & Co.: Berlin, Germany, 1995; pp. 918–985. [Google Scholar]
- Malkondu, Ö.; Tinastepe, N.; Akan, E.; Kazazoglu, E. An overview of monolithic zirconia in dentistry. Biotechnol. Biotecnol. Equip. 2016, 30, 644–652. [Google Scholar] [CrossRef]
- Acar, O.; Yilmaz, B.; Altintas, S.H.; Chandrasekaran, I.; Johnston, W.M. Color Stainability of CAD/CAM and Nanocomposite Resin Materials. J. Prosthet. Dent. 2016, 115, 71–75. [Google Scholar] [CrossRef]
- Zhang, Y.; Lawn, B.R. Novel zirconia materials in dentistry. J. Dent. Res. 2018, 97, 140–147. [Google Scholar] [CrossRef]
- Scientific Documentation. Microsoft Word–WissDok IPS e.max ZirCADenglisch aktualisiert 30112017.docx. Available online: https://www.ivoclar.com/ (accessed on 3 March 2022).
- Zhang, Y. Making Yttria-stabilized tetragonal zirconia translucent. Dent. Mater. 2014, 30, 1195–1203. [Google Scholar] [CrossRef]
- Inokoshi, M.; Shimizu, H.; Nozaki, K.; Yoshihara, K.; Nagaoka, N.; Zhang, F.; Vleugels, J.; Van Meerbeek, B.; Minakuchi, S. Crystallographic and morphological analysis of sandblasted highly translucent dental zirconia. Dent. Mater. 2018, 34, 508–518. [Google Scholar] [CrossRef]
- Sheng, Y.; Shi, Y.; Wang, L.; Narasimhan, S.G. Translucent radiosity: Efficiently combining diffuse inter-reflection and subsurface scattering. IEEE Trans. Vis. Comput. Graph. 2014, 20, 1009–1021. [Google Scholar] [CrossRef]
- Sulaiman, T.A.; Abdulmajeed, A.A.; Donovan, T.E.; Ritter, A.V.; Vallittu, P.K.; Närhi, T.O.; Lassila, L.V. Optical properties and light irradiance of monolithic zirconia at variable thicknesses. Dent. Mater. 2015, 31, 1180–1187. [Google Scholar] [CrossRef]
- Kumari, R.V.; Nagaraj, H.; Siddaraju, K.; Poluri, R.K. Evaluation of the Effect of Surface Polishing, Oral Beverages and Food Colorants on Color Stability and Surface Roughness of Nanocomposite Resins. J. Int. Oral Health 2015, 7, 63–70. [Google Scholar]
- Pereira, G.K.R.; Guilardi, L.F.; Dapieve, K.S.; Kleverlaan, C.J.; Rippe, M.P.; Valandro, L.F. Mechanical reliability, fatigue strength and survival analysis of new polycrystalline translucent zirconia ceramics for monolithic restorations. J. Mech. Behav. Biomed. Mater. 2018, 85, 57–65. [Google Scholar] [CrossRef]
- Ueda, K.; Güth, J.F.; Erdelt, K.; Stimmelmayr, M.; Kappert, H.; Beuer, F. Light transmittance by a multi-coloured zirconia material. Dent. Mater. J. 2015, 34, 310–314. [Google Scholar] [CrossRef]
- Kolakarnprasert, N.; Kaiser, M.R.; Kim, D.K.; Zhang, Y. New multi-layered zirconia: Composition, microstructure and translucency. Dent. Mater. 2019, 35, 797–806. [Google Scholar] [CrossRef] [PubMed]
- Gomez, I.; Lopez, L.P.; Fonseca, M.; Portugal, J. Effect of zirconia pigmentation on translucency. Eur. J. Proshodont. Restor. Dent. 2018, 26, 136–142. [Google Scholar]
- Zhang, F.; Vanmeensel, K.; Inokoshi, M.; Batuk, M.; Hadermann, J.; Van Meerbeek, B.; Naert, I.; Vleugels, J. Critical influence of alumina content on the low temperature degradation of 2–3 mol% yttria-stabilized TZP for dental restorations. J. Eur. Ceram. Soc. 2015, 35, 741–750. [Google Scholar] [CrossRef]
- Hallmann, L.; Ulmer, P.; Reusser, E.; Louvel, M.; Hämmerle, C.H. Effect of dopants and sintering temperature on microstructure and low temperature degradation of dental Y-TZP zirconia. J. Eur. Ceram. Soc. 2012, 32, 4091–4104. [Google Scholar] [CrossRef]
- Holz, L.; Macias, J.; Vitorino, N.; Fernandes, A.J.S.; Costa, F.M.; Almeida, M.M. Effect of Fe2O3 doping on colour and mechanical properties of Y-TZP ceramics. Ceram. Int. 2018, 44, 17962–17971. [Google Scholar] [CrossRef]
- Standard, O.C.; Sorrell, C.C. Densification of zirconia—Conventional methods. Key Eng. Mater. 1998, 153–154, 251–300. [Google Scholar]
- Powell, L.J.; Paulsen, P.J. Determination of hafnium in zirconium metal and zircaloy 4 metal standard reference materials by isotope dilution spark source mass spectrometry. Anal. Chem. 1984, 58, 376–378. [Google Scholar] [CrossRef]
- Aykent, F.; Yondem, I.; Ozyesil, A.G.; Gunal, S.K.; Avunduk, M.C.; Ozkan, S. Effect of different finishing techniques for restaurative materials on surface roughness and bacterial adhesion. J. Prosthet. Dent. 2010, 103, 221–227. [Google Scholar] [CrossRef]
- Alghazzawi, T.F.; Lemons, J.; Liu, P.R.; Essig, M.E.; Bartoluccci, A.A.; Janowski, G.M. Influence of low-temperature environmental exposure on the mechanical properties and structural stability of dental zirconia. J. Prosthodont. 2012, 21, 362–368. [Google Scholar] [CrossRef]
- Anusavice, K.J.; Shen, C.; Rawls, H.R. Phillip’s Science of Dental Materials, 12th ed.; Elsevier: St. Luis, MO, USA, 2012; pp. 231–255. [Google Scholar]
- Sarac, D.; Sarac, Y.S.; Yuzbasioglu, E. The effect of porcelain polishing systems on the color and surface texture of feldspathic porcelain. J. Prosthet. Dent. 2006, 96, 122–128. [Google Scholar] [CrossRef]
- Kohorst, P.; Borchers, L.; Strempel, J.; Stiesch, M.; Hassel, T.; Bach, F.W.; Hubsch, C. Low-temperature degradation of different zirconia ceramics for dental application. Acta Biomater. 2012, 8, 1213–1220. [Google Scholar] [CrossRef]
- Park, C.; Vang, M.S.; Park, S.W.; Lim, H.P. Effect of various polishing system on the surface roughness and phase transformation of zirconia and the durability of the polishing systems. J. Prosthet. Dent. 2017, 117, 430–437. [Google Scholar] [CrossRef]
- Hjerppe, J.; Narhi, T.O.; Vallittu, P.K.; Lassila, L.V. Surface roughness and the flexural and bend strength of zirconia after different surface treatments. J. Prosthet. Dent. 2016, 116, 577–583. [Google Scholar] [CrossRef]
- Amaral, M.; Valandro, L.F.; Bottino, M.A.; Souza, R.O. Low-temperature degradation of a Y-TPZ ceramic after surface treatments. J. Biomed. Mater. Res. B Appl. Biomater. 2013, 101, 1387–1392. [Google Scholar] [CrossRef]
- Pereira, G.K.R.; Venturini, A.B.; Silvestri, T.; Dapieve, K.S.; Montagner, A.F.; Soares, F.Z.M.; Valandro, L.F. Low-temperature degradation of Y-TZP ceramics: A systematic review and meta-analysis. Mech. Behav. Biomed. Mater. 2015, 55, 151–163. [Google Scholar] [CrossRef]
- Deville, S.; Gremillard, L.; Chevalier, J.; Fantozzi, G. A critical comparison of methods for the determination of aging sensitivity in biomedical grade yttria-stabilized zirconia. J. Biomed. Mater. Res. Part B Appl. Biomater. 2005, 72, 239–245. [Google Scholar] [CrossRef]
- Kelly, J.; Denry, I. Stabilized zirconia as a structural ceramic: An overview. Dent. Mater. 2008, 24, 289–298. [Google Scholar] [CrossRef]
- Harada, A.; Shishido, S.; Barkarmo, S.; Inagaki, R.; Kanno, T.; Örtengren, U.; Egusa, H.; Nakamura, K. Mechanical and microstructural properties of ultra-translucent zirconia ceramic stabilized with 5 mol % yttria. J. Mech. Behav. Biomed. Mater. 2020, 111, 103974. [Google Scholar] [CrossRef]
- Ivoclar-Vivadent IPS e.max ZirCAD Labside Gebrauchsinformation 2019-06-27, Rev3a. Available online: https://www.cadstar.dental/download/87/materialdokumentation-de/5667919/ipse-maxzircadlabside.pdf (accessed on 18 February 2022).
- Kuraray Noritake—Technical Guide Katana Zirconia Multi-Layered Series. 201805-brochure-katana-zirconia-technical-guide-web-en_2.pdf. Available online: https://www.kuraraynoritake.eu/ (accessed on 21 February 2022).
- Amann Girrbach-Verarbaitungstehnik—Zolid DNA Generation. 976109DE, 03/2021. Indikationsleitfaden_Zirkon_DE.pdf. Available online: https://www.Amanngirrbach.com (accessed on 25 January 2022).
- Chevalier, J.; Cales, B.; Drouin, J.M. Low-temperature aging of Y-TZP ceramics. J. Am. Ceram. Soc. 1999, 82, 2150–2154. [Google Scholar] [CrossRef]
- Akl, M.A.; Sim, C.P.C.; Nunn, M.E.; Zeng, L.L.; Hamza, T.A.; Wee, A.G. Validation of two clinical color measuring instruments for use in dental research. J. Dent. 2022, 125, 104223. [Google Scholar] [CrossRef]
- CIE. Colorimetry; CIE 15:2004; Commission Internationale de l′Eclairage: Vienna, Austria, 2004. [Google Scholar]
- Elsaka, S.E. Optical and Mechanical Properties of Newly Developed Multilayer Zirconia. J. Prosthodont. 2019, 28, 279–284. [Google Scholar] [CrossRef]
- Paravina, R.; Powers, J. Esthetic Color Training in Dentistry; Mosby: St. Louis, MO, USA, 2004; pp. 51–78. [Google Scholar]
- De Araújo-Júnior, E.N.S.; Bergamo, E.T.P.; Bastos, T.M.C.; Benalcázar Jalkh, E.B.; Lopes, A.C.O.; Monteiro, K.N.; Cesar, P.F.; Tognolo, F.C.; Migliati, R.; Tanaka, R.; et al. Ultra-translucent zirconia processing and aging effect on microstructural, optical, and mechanical properties. Dent. Mater. 2022, 38, 587–600. [Google Scholar] [CrossRef]
- Kim, H.K.; Kim, S.H.; Lee, J.B.; Han, J.S.; Yeo, I.S. Effect of polishing and glazing on the color and spectral distribution of monolithic zirconia. J. Adv. Prosthodont. 2013, 5, 296–304. [Google Scholar] [CrossRef]
- Toma, F.R.; Birdeanu, M.I.; Utu, I.D.; Vasiliu, R.D.; Moleriu, L.C.; Porojan, L. Surface characteristics of high translucent zirconia related to aging. Materials 2022, 15, 3606. [Google Scholar] [CrossRef]
- Sedda, M.; Vichi, A.; Carrabba, M.; Capperucci, A.; Louca, C.; Ferrari, M. Influence of coloring procedure on flexural resistance of zirconia blocks. J. Prosthet. Dent. 2015, 114, 98–102. [Google Scholar] [CrossRef]
- Al-Juaila, E.; Osman, E.; Segaan, L.; Shrebaty, M.; Farghaly, E.A. Comparison of translucency for different thickness of recent types of esthetic zirconia ceramics versus conventional ceramics… (in vitro study). Future Dent. J. 2018, 4, 297–301. [Google Scholar] [CrossRef]
- Lee, Y.K. Translucency of human teeth and dental restorative materials and its clinical relevance. J. Biomed. Opt. 2015, 20, 45002. [Google Scholar] [CrossRef]
- Wang, F.; Takahasi, H.; Iwasaki, N. Translucency of dental ceramics with different thicknesses. J. Prosthet. Dent. 2013, 110, 14–20. [Google Scholar] [CrossRef]
- Liu, M.-C.; Aquilino, S.A.; Lund, P.S.; Vargas, M.A.; Diaz-Arnold, A.M.; Gratton, D.G.; Qian, F. Human perception of dental porcelain translucency correlated to spectrophotometric measurements. J. Prosthodont. 2010, 19, 187–193. [Google Scholar] [CrossRef]
- Juntavee, N.; Attashu, S. Effect of sintering process on color parameters of nano-sized yttria partially stabilized tetragonal monolithic zirconia. J. Clin. Exp. Dent. 2018, 10, e794–e804. [Google Scholar] [CrossRef]
- Camposilvan, E.; Leone, R.; Gremillard, L.; Sorrentino, R.; Zarone, F.; Ferrari, M.; Chevalier, J. Aging resistance, mechanical properties and translucency of different yttria-stabilized zirconia ceramics for monolithic dental crown applications. Dent. Mater. 2018, 34, 879–890. [Google Scholar] [CrossRef] [PubMed]
- Alghazzawi, T.F. The effect of extended aging on the optical properties of different zirconia materials. J. Prosthodont. Res. 2017, 61, 305–314. [Google Scholar] [CrossRef] [PubMed]
- Lumkemann, N.; Stawarczyk, B. Impact of hydrothermal aging on the light transmittance and flexural strength of colored yttria-stabilized zirconia materials of different formulations. J. Prosthet. Dent. 2021, 125, 518–526. [Google Scholar] [CrossRef] [PubMed]
- Baldi, A.; Comba, A.; Ferrero, G.; Italia, E.; Dds, R.M.T.; Paolone, G.; Mazzoni, A.; Breschi, L.; Scotti, N. External gap progression after cyclic fatigue of adhesive overlays and crowns made with high translucency zirconia or lithium silicate. J. Esthet. Restor. Dent. 2022, 34, 557–564. [Google Scholar] [CrossRef]
- Ziyad, T.A.; Abu-Naba’a, L.A.; Almohammed, S.N. Optical properties of CAD/CAM monolithic system compared: Three multi-layered zirconia and one lithium disilicate system. J. Heliyon 2021, 7, e08151. [Google Scholar] [CrossRef] [PubMed]
| Material/Manufacturer | Y2O3 Content | Other Components | Grain Size | Shade/Translucency |
|---|---|---|---|---|
| Ceramill Zolid fx ML/ Amman Girrbach, AG, Koblach, Austria (CeZ) | 5 mol% (8.5–9.5 wt%) | Hf O2 ≤ 5.0 wt% Al2O3 ≤ 0.5 wt% other oxides ≤ 1.0 wt% | - | Super-high translucency (A2/A3) |
| STML/Katana, Kuraray Noritake Dental, Tokio, Japan (STM) | 4 mol% (7–10.0 wt%) | Hf O2 ≤ 5.0 wt% Al2O3 0.26 wt% other oxides < 2% | 0.2–0.5 µm | Super translucency (A2) |
| IPS e.max Zir CAD/ Ivoclar Vivadent AG, Schaan, Liechtenstein (IPZ) | 4 mol%-cervical (7.10 wt%) 4 + 5 mol%-transition 5 mol%-incisal (8.80 wt%) | Hf O2 ≤ 5.0 wt% Al2O3 ≤ 0.05 wt% other oxides ≤ 1.0 wt% | 0.65 µm 0.85 µm | Super-high translucency + Super translucency (A2) |
| Variable | Area | CeZ pc | CeZ gc | STM pc | STM gc | IPZ pc | IPZ gc |
|---|---|---|---|---|---|---|---|
| L* | c | 78.213 ± 0.271 | 80.813 ± 0.217 | 76.650 ± 0.288 | 83.613 ± 0.187 | 83.288 ± 0.289 | 83.613 ± 0.278 |
| m | 77.888 ± 0.267 | 81.700 ± 0.269 | 78.613 ± 0.289 | 83.988 ± 0.278 | 82.100 ± 0.234 | 83.988 ± 0.348 | |
| i | 79.825 ± 0.288 | 82.825 ± 0.219 | 80.488 ± 0.219 | 84.075 ± 0.234 | 83.463 ± 0.267 | 84.075 ± 0.234 | |
| a* | c | 0.013 ± 0.054 | −0.075 ± 0.005 | −0.738 ± 0.005 | 0.438 ± 0.005 | 0.413 ± 0.005 | 0.438 ± 0.005 |
| m | −0.850 ± 0.024 | −0.938 ± 0.054 | −1.363 ± 0.003 | 0.175 ± 0.109 | 0.275 ± 0.109 | 0.175 ± 0.004 | |
| i | −1.113 ± 0.005 | −1.025 ± 0.101 | −2.388 ± 0.014 | −1.413 ± 0.102 | −1.613 ± 0.109 | −1.413 ± 0.109 | |
| b* | c | 10.675 ± 0.218 | 10.413 ± 0.250 | 26.000 ± 0.207 | 16.638 ± 0.218 | 17.125 ± 0.280 | 16.638 ± 0.267 |
| m | 5.700 ± 0.250 | 5.850 ± 0.187 | 20.763 ± 0.267 | 15.738 ± 0.234 | 17.825 ± 0.267 | 15.738 ± 0.207 | |
| i | 1.825 ± 0.207 | 1.938 ± 0.207 | 12.738 ± 0.280 | 5.575 ± 0.278 | 4.538 ± 0.188 | 5.575 ± 0.256 | |
| TP | c | 13.996 ± 0.158 | 13.656 ± 0.25 | 13.274 ± 0.185 | 13.083 ± 0.271 | 13.491 ± 0.191 | 13.284 ± 0.197 |
| m | 14.139± 0.119 | 13.929 ± 0.166 | 13.353 ± 0.16 | 13.178 ± 0.215 | 13.366 ± 0.147 | 13.188 ± 0.16 | |
| i | 14.587 ± 0.167 | 14.258 ± 0.168 | 13.846 ± 0.24 | 13.612 ± 0.165 | 14.108 ± 0.189 | 13.838 ± 0.175 | |
| CR | c | 0.688 ± 0.002 | 0.695 ± 0.002 | 0.723 ± 0.004 | 0.736 ± 0.007 | 0.711 ± 0.004 | 0.716 ± 0.002 |
| m | 0.677 ± 0.004 | 0.686 ± 0.003 | 0.711 ± 0.001 | 0.718 ± 0.003 | 0.724 ± 0.01 | 0.720 ± 0.007 | |
| i | 0.66 ± 0.005 | 0.675 ± 0.006 | 0.692 ± 0.006 | 0.706 ± 0.006 | 0.689 ± 0.007 | 0.688 ± 0.006 | |
| OP | c | 5.802 ± 0.192 | 5.581 ± 0.236 | 7.486 ± 0.273 | 7.555 ± 0.203 | 6.207 ± 0.201 | 6.239 ± 0.177 |
| m | 5.218 ± 0.18 | 4.791 ± 0.296 | 6.929 ± 0.298 | 6.651 ± 0.143 | 6.867 ± 0.350 | 6.486 ± 0.237 | |
| i | 3.787 ± 0.217 | 3.529 ± 0.189 | 5.704 ± 0.222 | 5.855 ± 0.116 | 5.159 ± 0.279 | 4.706 ± 0.268 |
| Variable | Area | CeZ pa | CeZ ga | STM pa | STM ga | IPZ pa | IPZ ga |
|---|---|---|---|---|---|---|---|
| L* | c | 77.688 ± 0.213 | 81.038 ± 0.217 | 76.938 ± 0.269 | 79.075 ± 0.267 | 77.688 ± 0.218 | 84.025 ± 0.219 |
| m | 78.463 ± 0.326 | 81.463 ± 0.278 | 78.575 ± 0.187 | 80.513 ± 0.288 | 78.463 ± 0.348 | 83.225 ± 0.278 | |
| i | 79.863 ± 0.234 | 83.175 ± 0.219 | 82.025 ± 0.267 | 82.925 ± 0.218 | 79.863 ± 0.289 | 83.563 ± 0.219 | |
| a* | c | −0.025 ± 0.015 | 0.038 ± 0.005 | −0.550 ± 0.005 | −0.525 ± 0.028 | −0.025 ± 0.008 | 0.275 ± 0.102 |
| m | −0.088 ± 0.028 | −0.675 ± 0.003 | −1.413 ± 0.024 | −1.875 ± 0.109 | −0.888 ± 0.102 | 0.100 ± 0.014 | |
| i | −1.088 ± 0.109 | −1.013 ± 0.005 | −1.988 ± 0.054 | −2.663 ± 0.101 | −1.088 ± 0.004 | −1.538 ± 0.005 | |
| b* | c | 9.538 ± 0.267 | 11.000 ± 0.188 | 27.613 ± 0.185 | 26.950 ± 0.26 | 9.538 ± 0.317 | 16.375 ±0.280 |
| m | 5.125 ± 0.234 | 5.925 ± 0.207 | 23.550 ± 0.218 | 21.700 ± 0.187 | 5.125 ± 0.218 | 16.725 ±0.250 | |
| i | 1.625 ± 0.154 | 2.200 ± 0.250 | 15.425 ± 0.207 | 12.200 ± 0.267 | 1.625 ± 0.280 | 5.525 ± 0.280 | |
| TP | c | 13.854 ± 0.142 | 13.766 ± 0.21 | 13.551 ± 0.132 | 13.277 ± 0.26 | 13.749 ± 0.153 | 13.462 ± 0.187 |
| m | 14.022 ± 0.163 | 14.007 ± 0.166 | 13.617 ± 0.188 | 13.351 ± 0.109 | 13.636 ± 0.165 | 13.374 ± 0.188 | |
| i | 14.486 ± 0.176 | 14.325 ± 0.14 | 14.034 ± 0.174 | 13.773 ± 0.158 | 14.135 ± 0.182 | 13.929 ± 0.128 | |
| CR | c | 0.693 ± 0.005 | 0.696 ± 0.003 | 0.727 ± 0.006 | 0.732 ± 0.004 | 0.701 ± 0.003 | 0.714 ± 0.002 |
| m | 0.692 ± 0.008 | 0.692 ± 0.004 | 0.721 ± 0.004 | 0.722 ± 0.004 | 0.702 ± 0.004 | 0.715 ± 0.002 | |
| i | 0.676 ± 0.003 | 0.678 ± 0.005 | 0.693 ± 0.008 | 0.704 ± 0.005 | 0.676 ± 0.005 | 0.691 ± 0.003 | |
| OP | c | 5.071 ± 0.269 | 5.842 ± 0.267 | 8.184 ± 0.187 | 7.619 ± 0.126 | 6.405 ± 0.154 | 6.314 ± 0.218 |
| m | 4.186 ± 0.250 | 5.896 ± 0.185 | 8.170 ± 0.218 | 7.452 ± 0.234 | 6.540 ± 0.217 | 6.383 ± 0.277 | |
| i | 3.313 ± 0.207 | 4.135 ± 0.126 | 5.852 ± 0.248 | 6.109 ± 0.236 | 4.179 ± 0.248 | 4.865 ± 0.213 |
| Material | L* | a* | b* |
|---|---|---|---|
| STM p, c | very weak, r = 0.196 | moderate, r = 0.547 | weak, r = 0.235 |
| r2 = 0.038 = 3.84% | r2 = 0.299 = 29.9% | r2 = 0.055 = 5.5% | |
| p = 0.043 | p = 0.003 | p = 0.026 | |
| STM p, m | weak, r = −0.341 | weak, r = − 0.235 | moderate, r = 0.460 |
| r2= 0.116 = 11.6%, | r2 = 0.055 = 5.5%, | r2 = 0.211 =21.1%, | |
| p = 0.913 | p = 0.026 | p = 0.002 | |
| IPZ p, c | very strong, r = −0.867 | moderate, r = −0.435 | very strong, r = 0.800 |
| r2 = 0.751 = 75.1% | r2 = 0.189 | r2 = 0.640 =64% | |
| p < 0.001 | p < 0.001 | p < 0.001 | |
| IPZ p, m | very weak, r = −0.180 | very weak, r = −0.116 | very weak, r = 0.068 |
| r2= 0.032 = 3.2% | r2 = 0.013 = 1.3% | r2 = 0.004 = 0.4% | |
| p = 0.233 | p = 0.150 | p = 0.055 |
| Material | a* | b* |
|---|---|---|
| CeZ p, c | weak, r = −0.203, r2 = 0.041 = 4.1%, p = 0.830 | moderate, r = 0.567, r2 = −0.321 = 32.1%, p = 0.001 |
| CeZ p, m | moderate, r = −0.044, r2 = 0.002 = 0.2%, p = 0.246 | weak, r = −0.313, r2 = 0.098 = 0.98%, p = 0.820 |
| STM p, c | moderate, r = 0.547, r2= 0.299 = 29.9%, p = 0.003 | weak, r = 0.235, r2 = 0.055 = 5.5%, p = 0.026 |
| STM p, m | weak, r = −0.235, r2 = 0.055 = 5.5%, p = 0.026 | moderate, r = 0.460, r2= 0.211 = 21.1%, p = 0.002 |
| IPZ p, i | very weak, r = −0.096, r2 = 0.009= 0.9%, p = 0.147 | moderate, r = 0.424, r2 = 0.180 = 18%, p = 0.053 |
| CeZ g, m | weak, r = 0.020, r2 < 0.001 p < 0.001 | very weak, r = 0.009, r2 < 0.001, p < 0.001 |
| STM g, m | weak, r = −0.323, r2 = 0.104 = 10.4%, p = 0.662 | strong, r = 623, r2 = 0.389 = 38.9%, p = 0.031 |
| ΔE | CeZ p | CeZ p | STM p | STM g | IPZ p | IPZ g | |
|---|---|---|---|---|---|---|---|
| black | c | 1.152 | 0.587 | 1.517 | 0.872 | 2.239 | 0.573 |
| m | 0.748 | 0.337 | 2.564 | 1.162 | 2.473 | 1.15 | |
| i | 0.188 | 0.402 | 2.871 | 1.132 | 2.474 | 0.486 | |
| white | c | 1.486 | 0.635 | 1.644 | 0.922 | 2.259 | 0.598 |
| m | 0.938 | 0.465 | 2.642 | 1.381 | 1.989 | 1.114 | |
| i | 0.141 | 0.289 | 2.964 | 1.07 | 2.141 | 0.952 |
 ΔE*—The total color change value. CeZ = Ceramill Zolid fx ML, STM = STML, IPZ = IPS e.max ZirCAD CEREC/in Lab MT Multi, p = polished, g = glazed, m = medium, c = cervical, i = incisal.
ΔE*—The total color change value. CeZ = Ceramill Zolid fx ML, STM = STML, IPZ = IPS e.max ZirCAD CEREC/in Lab MT Multi, p = polished, g = glazed, m = medium, c = cervical, i = incisal.Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Toma, F.R.; Porojan, S.D.; Vasiliu, R.D.; Porojan, L. The Effect of Polishing, Glazing, and Aging on Optical Characteristics of Multi-Layered Dental Zirconia with Different Degrees of Translucency. J. Funct. Biomater. 2023, 14, 68. https://doi.org/10.3390/jfb14020068
Toma FR, Porojan SD, Vasiliu RD, Porojan L. The Effect of Polishing, Glazing, and Aging on Optical Characteristics of Multi-Layered Dental Zirconia with Different Degrees of Translucency. Journal of Functional Biomaterials. 2023; 14(2):68. https://doi.org/10.3390/jfb14020068
Chicago/Turabian StyleToma, Flavia Roxana, Sorin Daniel Porojan, Roxana Diana Vasiliu, and Liliana Porojan. 2023. "The Effect of Polishing, Glazing, and Aging on Optical Characteristics of Multi-Layered Dental Zirconia with Different Degrees of Translucency" Journal of Functional Biomaterials 14, no. 2: 68. https://doi.org/10.3390/jfb14020068
APA StyleToma, F. R., Porojan, S. D., Vasiliu, R. D., & Porojan, L. (2023). The Effect of Polishing, Glazing, and Aging on Optical Characteristics of Multi-Layered Dental Zirconia with Different Degrees of Translucency. Journal of Functional Biomaterials, 14(2), 68. https://doi.org/10.3390/jfb14020068






