Structural Integrity of Anterior Ceramic Resin-Bonded Fixed Partial Denture: A Finite Element Analysis Study
Abstract
1. Introduction
2. Materials and Methods
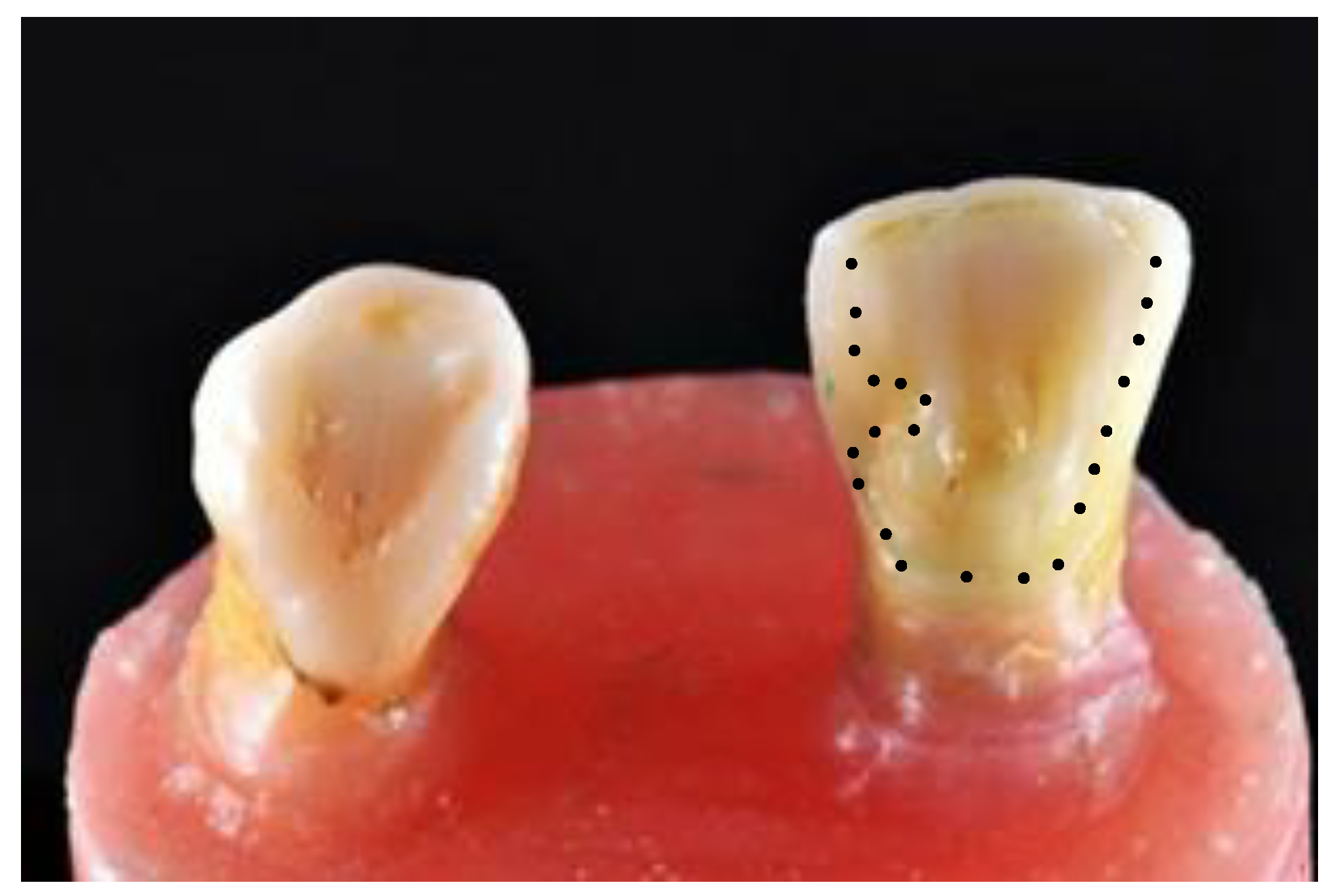
2.1. Set Up of Master Model
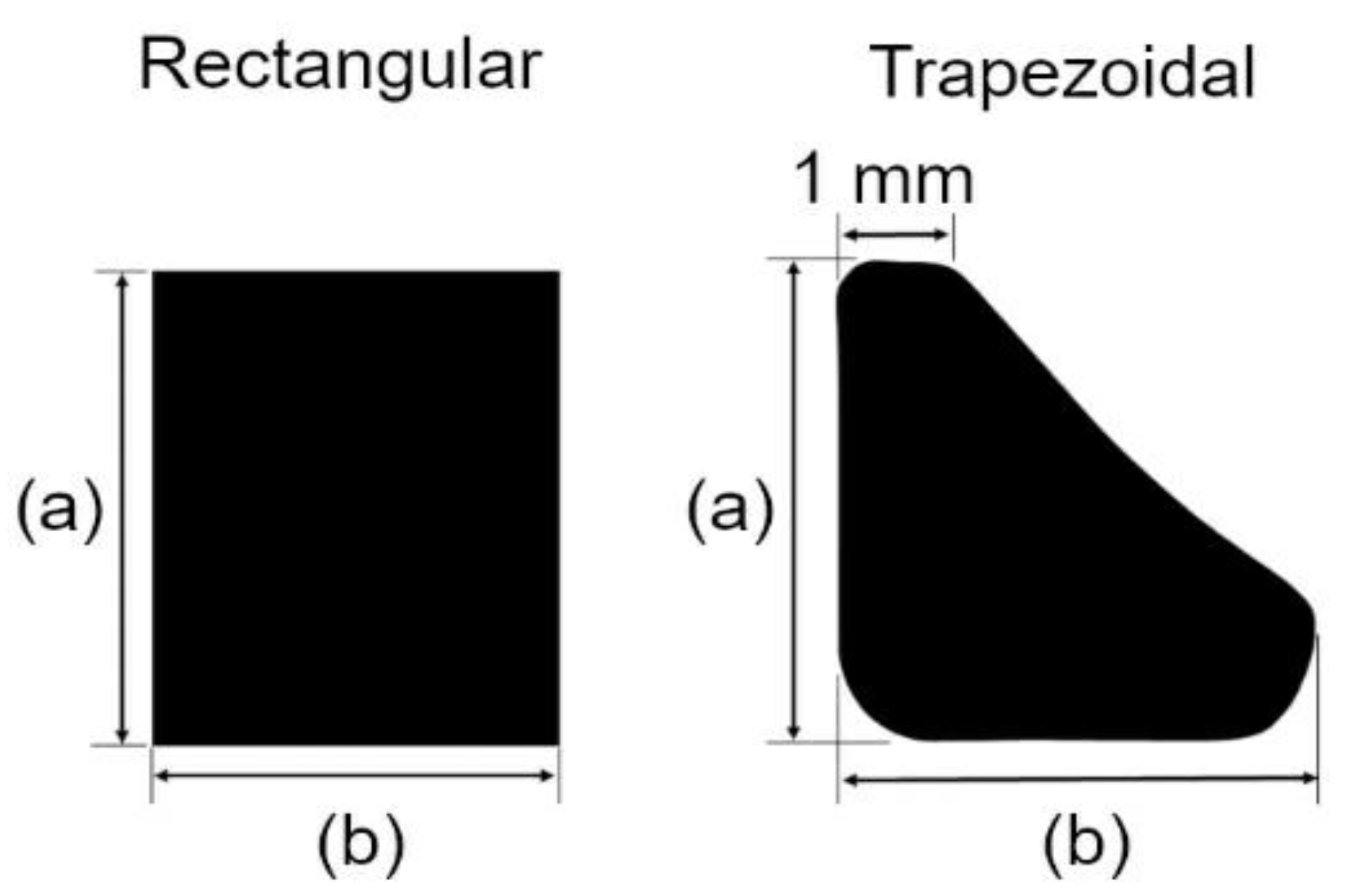
2.2. Preparation of Abutment and Prostheses
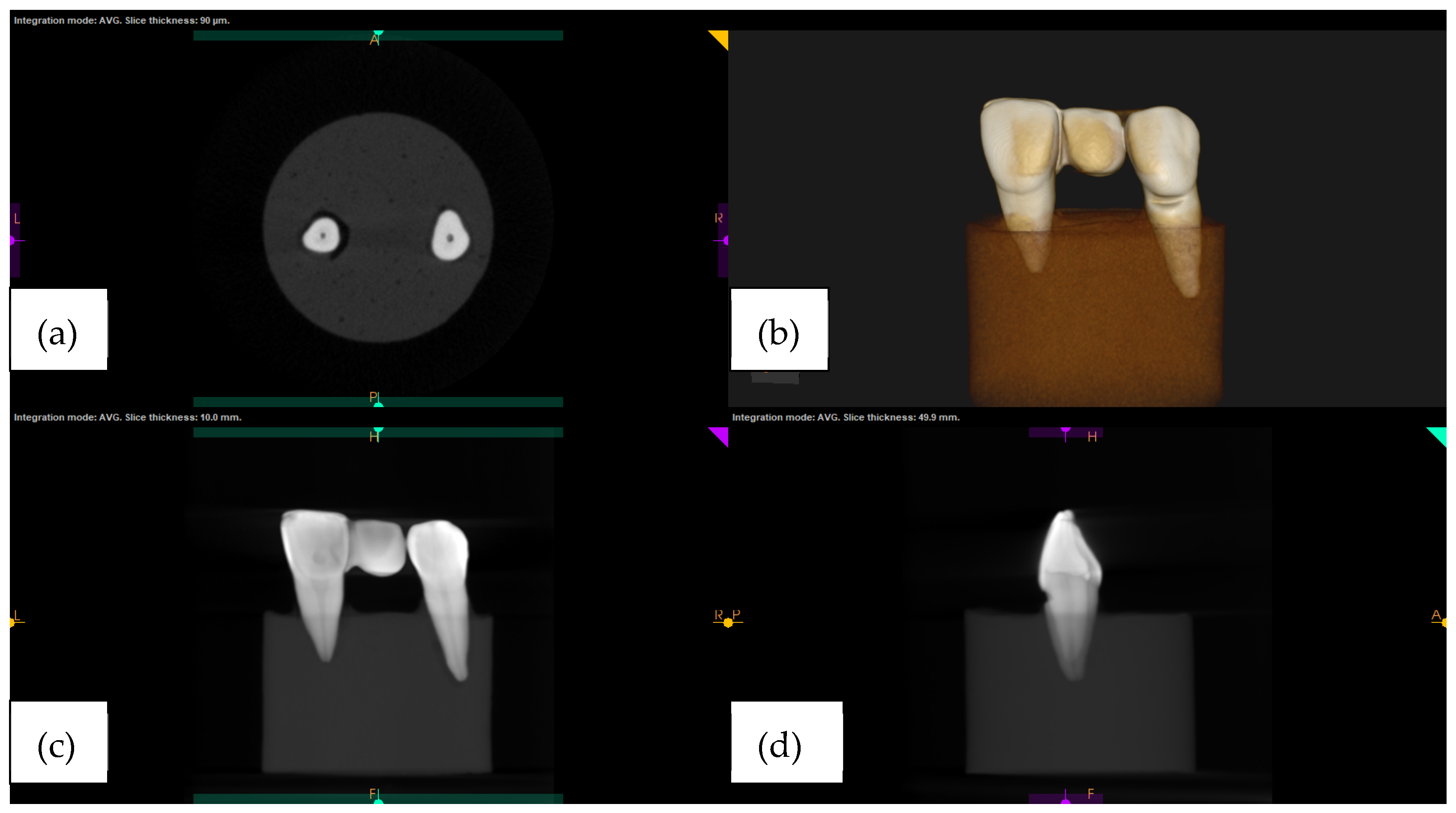
2.3. Radiographic Imaging of the Master Model
2.4. Finite Element Modelling and Simulation
3. Results
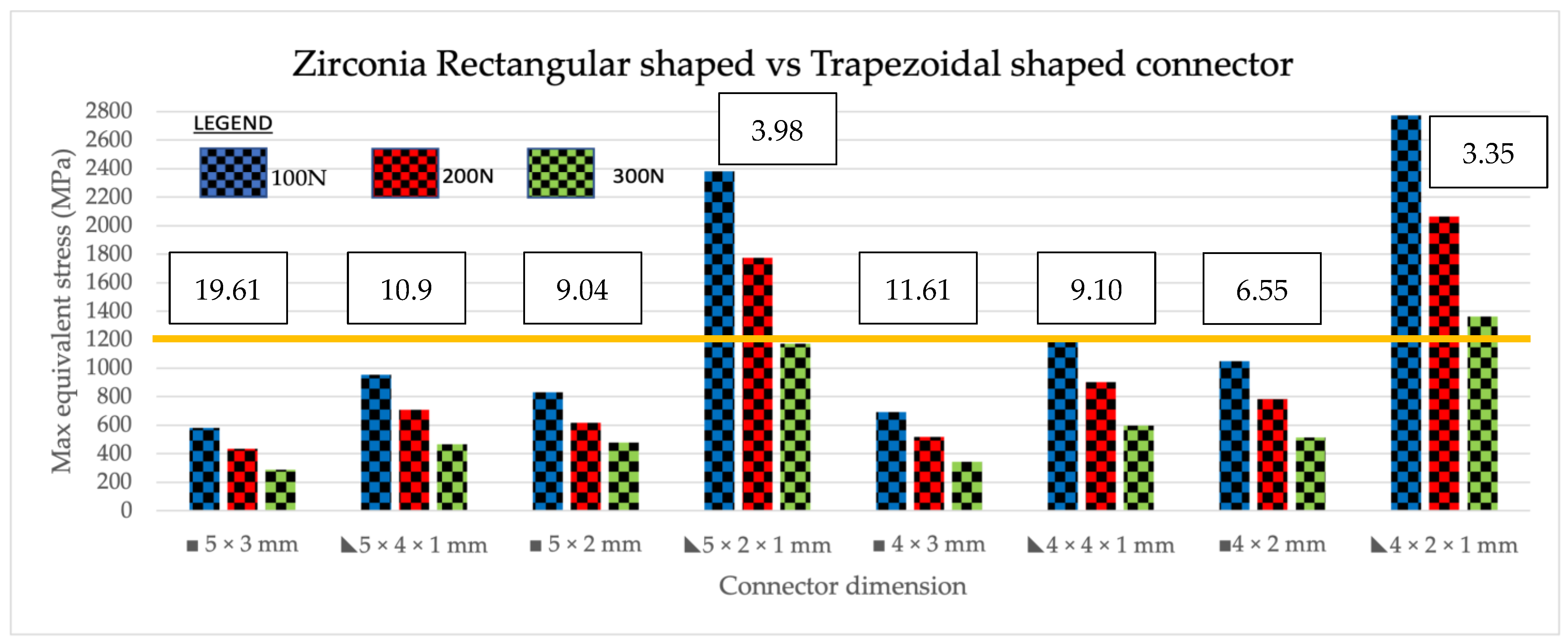
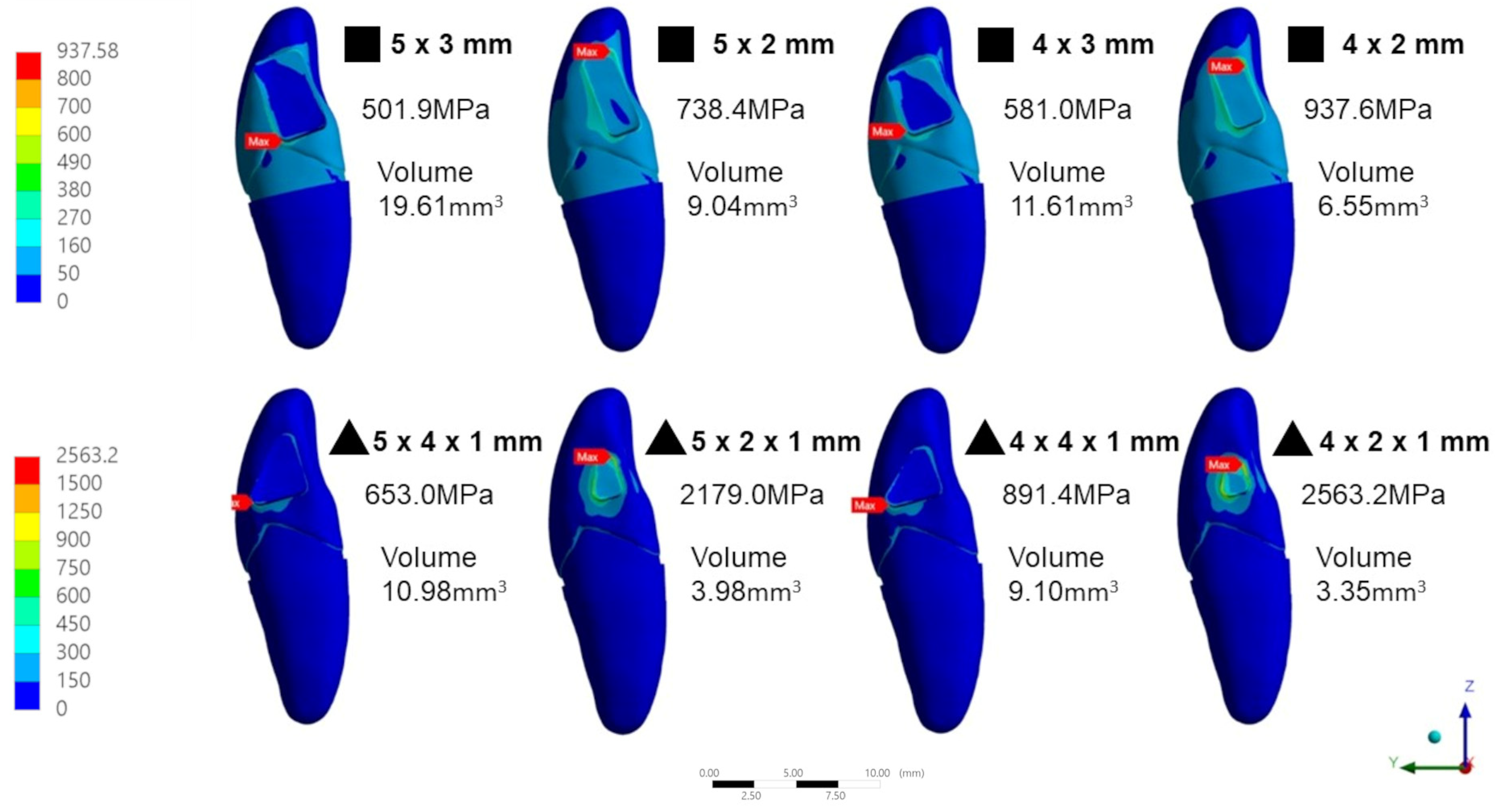
3.1. Volume of Tested Connector
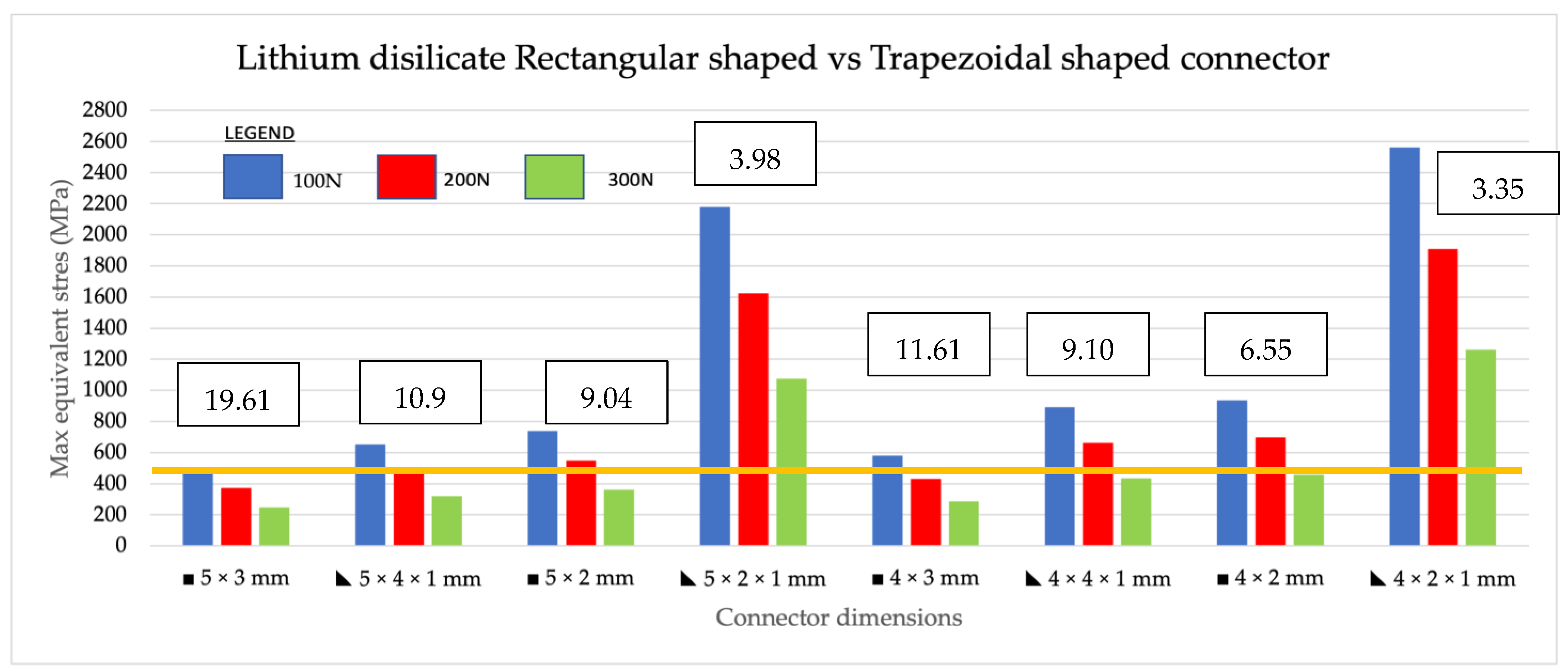
3.2. Intracomparison of the Maximum Equivalent Stress (MES) between Trapezoidal and Rectangular Shape within the Same Material
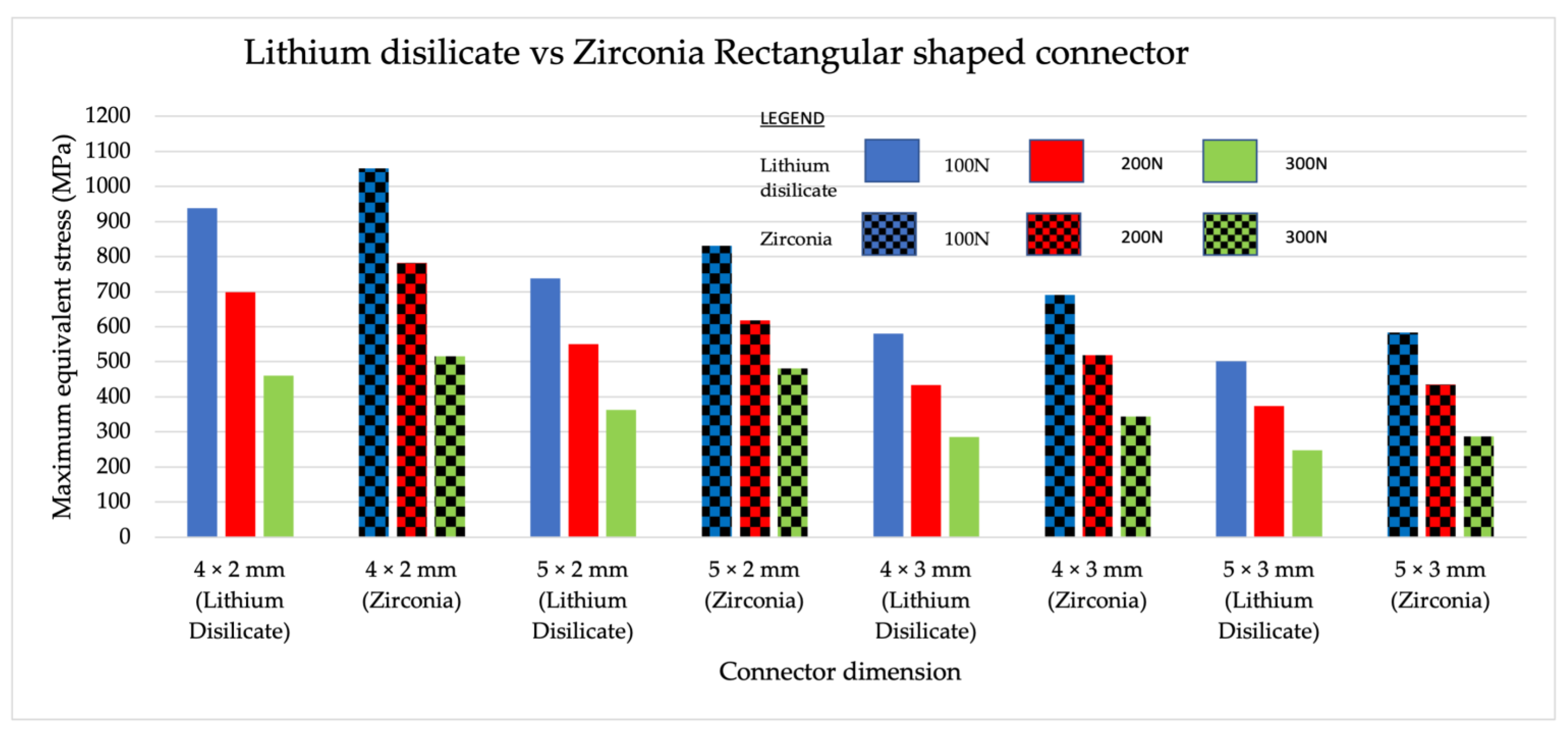
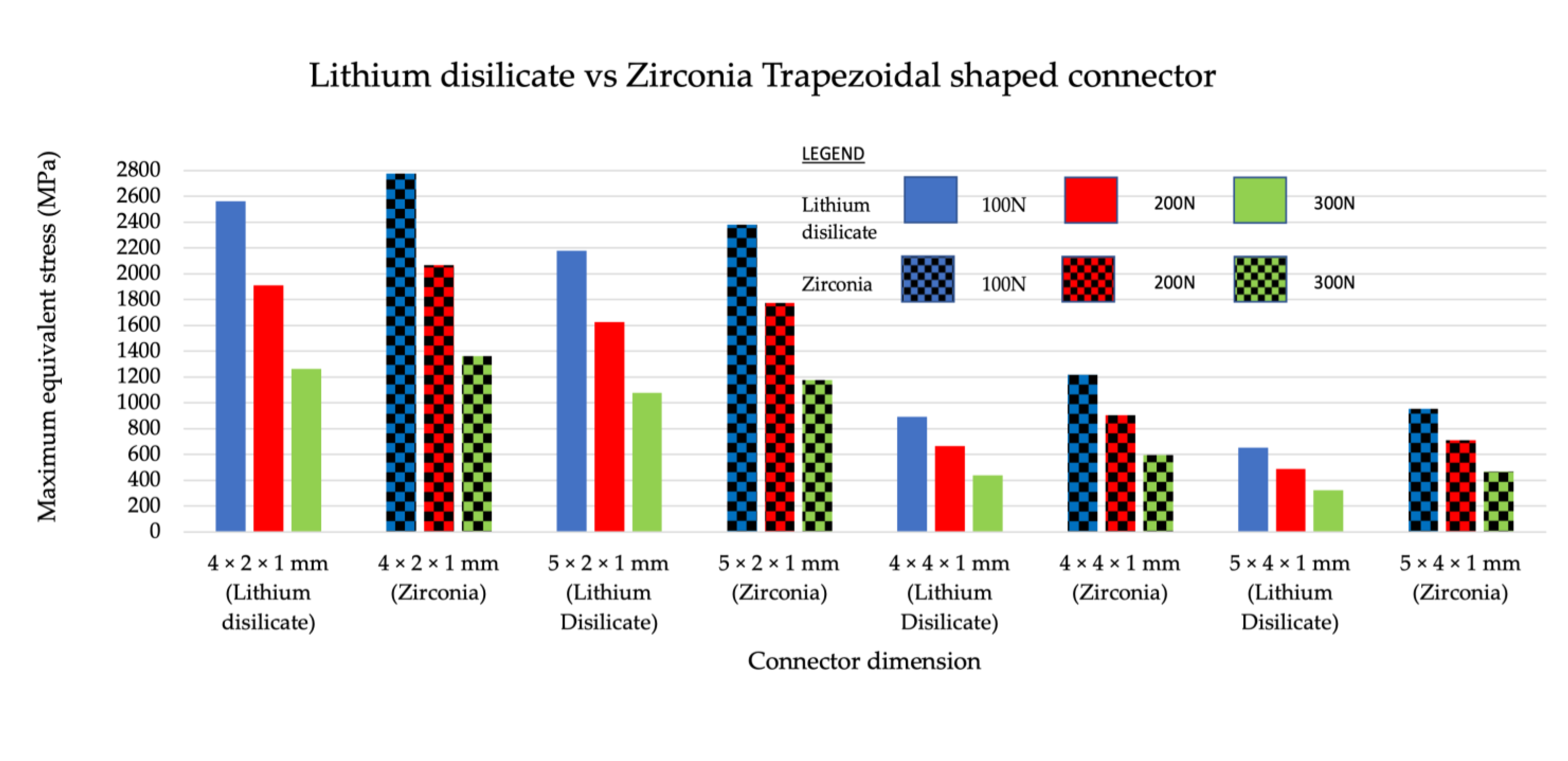
3.3. Intercomparison of Maximum Equivalent Stress between Different Materials with the Same Shape
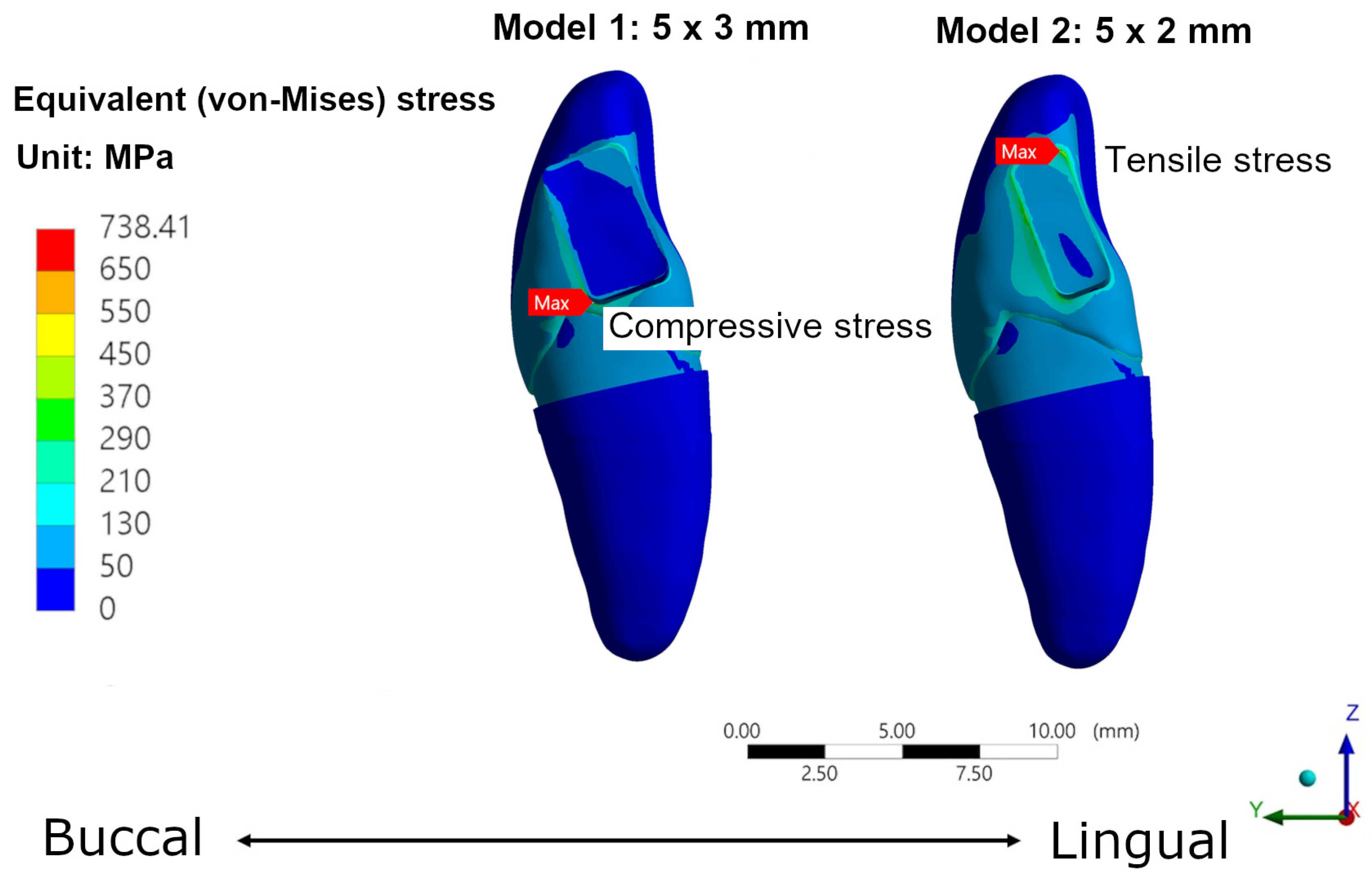
3.4. Patterns of Stress
4. Discussion
5. Conclusions
- The base of the connector serves as a vital variable that significantly influences fracture strength of the materials tested. Regardless of the connector shape, the base of the connector must be of a sufficient size to be able to resist crack propagation and failure of the prostheses. A small sized connector base may induce more tensile stress concentration on the lingual side compared to a larger sized connector base.
- When the height of the connector was altered and the width was fixed, there was a higher amount of stress on the prostheses. A higher degree of stress was imposed on the prostheses, as a result of fixed connector width and altered connector height.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lim, T.W.; Abdul Ghani, S.M.; Mustaza, T.A. Resin bonded bridges. Malays. Dent. J. 2014, 36, 24–29. [Google Scholar]
- Yoshida, T.; Kurosaki, Y.; Mine, A.; Kimura-Ono, A.; Mino, T.; Osaka, S. Fifteen-year survival of resin-bonded vs full-coverage fixed dental prostheses. J. Prosthodont. Res. 2019, 63, 374–382. [Google Scholar] [CrossRef] [PubMed]
- Conrad, H.J.; Seong, W.J.; Pesun, I.J. Current ceramic materials and systems with clinical recommendations: A systematic review. J. Prosthet. Dent. 2007, 98, 389–404. [Google Scholar] [CrossRef]
- Edelhoff, D.; Sorensen, J.A. Tooth structure removal associated with various preparation designs for anterior teethD. J. Prosthet. Dent. 2002, 87, 503–509. [Google Scholar] [CrossRef] [PubMed]
- Block, M.S. Dental implants: The last 100 years. J. Oral Maxillofac. Surg. 2018, 76, 11–26. [Google Scholar] [CrossRef] [PubMed]
- Okuni, S.; Maekawa, K.; Mino, T.; Kurosaki, Y.; Kuboki, T. A retrospective comparison of the survival of vital teeth adjacent to single, bounded edentulous spaces rehabilitated using implant-supported, resin-bonded, and conventional fixed dental prostheses. J. Dent. 2022, 116, 103911. [Google Scholar] [CrossRef] [PubMed]
- Lim, T.W.; Ariff, T. Single tooth implant versus resin-bonded bridge: A study of patient’s satisfaction. Eur. J. Gen. Dent. 2020, 9, 90–95. [Google Scholar] [CrossRef]
- Alraheam, I.A.; Ngoc, C.N.; Wiesen, C.A.; Donovan, T.E. Five year success rate of resin-bonded fixed partial dentures: A systematic review. J. Esthet. Restor. Dent. 2019, 31, 40–50. [Google Scholar] [CrossRef]
- Mine, A.; Fujisawa, M.; Miura, S.; Yumitate, M.; Ban, S.; Yamanaka, A.; Ishida, M.; Takebe, J.; Yatani, H. Critical review about two myths in fixed dental prostheses: Full-Coverage vs. Resin-Bonded, non-Cantilever vs. Cantilever. Jpn. Dent. Sci. Rev. 2021, 57, 33–38. [Google Scholar] [CrossRef]
- Rochette, A.L. Attachment of a splint to enamel of lower anterior teeth. J. Prosthet. Dent. 1973, 30, 418–423. [Google Scholar] [CrossRef]
- Chan, A.W.K.; Barnes, I.E. A prospective study of cantilever resin-bonded bridges: An initial report. Aust. Dent. J. 2000, 45, 31–36. [Google Scholar] [CrossRef] [PubMed]
- Hussey, D.L.; Linden, G.J. The clinical performance of cantilevered resin-bonded bridgework. J. Dent. 1996, 24, 251–256. [Google Scholar] [CrossRef] [PubMed]
- Wel, Y.R.; Wang, X.D.; Zhang, Q.; Li, X.X.; Blatz, M.B.; Jian, Y.T.; Zhao, K. Clinical performance of anterior resin-bonded fixed dental prostheses with different framework designs: A systematic review and meta-analysis. J. Dent. 2016, 47, 1–7. [Google Scholar]
- Balasubramaniam, G.R. Predictability of resin bonded bridges-a systematic review. Br. Dent. J. 2017, 222, 849–858. [Google Scholar] [CrossRef] [PubMed]
- Zarone, F.; Di Mauro, M.I.; Ausiello, P.; Ruggiero, G.; Sorrentino, R. Current status on lithium disilicate and zirconia: A narrative review. BMC Oral Health 2019, 19, 1–14. [Google Scholar] [CrossRef]
- Solá-Ruiz, M.F.; Leon-Martine, R.; Labaig-Rueda, C.; Selva-Otalaorrouchi, E.; Agustin-Panadero, R. Clinical outcomes of veneered zirconia anterior partial fixed dental prostheses: A 12-year prospective clinical trial. J. Prosthet. Dent. 2021, 127, 846–851. [Google Scholar] [CrossRef]
- Sailer, I.; Balmer, M.; Hüsler, J.; Hämmerle, C.H.F.; Känel, S.; Thoma, D.S. 10-year randomized trial (RCT) of zirconia-ceramic and metal-ceramic fixed dental prostheses. J. Dent. 2018, 76, 32–39. [Google Scholar] [CrossRef]
- Miettinen, M.; Millar, B.J. A review of the success and failure characteristics of resin-bonded bridges. Br. Dent. J. 2013, 215, E3. [Google Scholar] [CrossRef]
- Mendes, J.M.; Bentata, A.L.G.; De Sá, J.; Silva, A.S. Survival Rates of Anterior-Region Resin-Bonded Fixed Dental Prostheses: An Integrative Review. Eur. J. Dent. 2021, 15, 788–797. [Google Scholar] [CrossRef]
- Pattaratiwanont, R.; Piemjai, M.; Garcia-Godoy, F. Survival of posterior fixed partial dentures with minimal tooth reduction and improved esthetics: An in vitro study. J. Prosthet. Dent. 2021, 127, 585–592. [Google Scholar] [CrossRef]
- Mohd Osman, M.; Lim, T.W.; Ab Ghani, A.R.; Ab Ghani, S.M. A Narrative Review on the In-Vitro Performance of Anterior All-Ceramic Resin Bonded Bridges. In Proceedings of the 21th Annual Scientific Meeting & 23rd Annual General Meeting IADR Malaysian Section, Selangor, Malaysia, 24 September 2022; Volume 3, pp. 25–31. [Google Scholar]
- Kern, M.; Fechtig, T.; Strub, J.R. Influence of water storage and thermal cycling on the fracture strength of all-porcelain, resin-bonded fixed partial dentures. J. Prosthet. Dent. 1994, 71, 251–256. [Google Scholar] [CrossRef]
- Botelho, M.G.; Leung, K.C.M.; Ng, H.; Chan, K. A retrospective clinical evaluation of two-unit cantilevered resin-bonded fixed partial dentures. J. Am. Dent. Assoc. 2006, 137, 783–788. [Google Scholar] [CrossRef] [PubMed]
- Idris, R.I.; Shoji, Y.; Lim, T.W. Occlusal force and occlusal contact reestablishment with resin-bonded fixed partial dental prostheses using the Dahl concept: A. clinical study. J. Prosthet. Dent. 2021, 127, 737–743. [Google Scholar] [CrossRef] [PubMed]
- Lim, T.W.; Ab Ghani, S.M.; Mahmud, M. Occlusal re-establishment and clinical complications of resin-bonded fixed partial dental prostheses cemented at an increased occlusal vertical dimension: A retrospective study. J. Prosthet. Dent. 2020, 127, 258–265. [Google Scholar] [CrossRef] [PubMed]
- Ouuldyerou, A.; Merdji, A.; Aminallah, L.; Roy, S.; Mehboob, H.; Ozcan, M. Biomechanical performance of Ti-PEEK dental implants in bone: An in-silico analysis. J. Mech. Behav. Biomed. Mater. 2022, 134, 105422. [Google Scholar] [CrossRef]
- Trindade, F.Z.; Valandro, L.F.; de Jager, D.; Bottino, M.A.; Kleverlaan, C.J. Elastic Properties of Lithium Disilicate Versus Feldspathic Inlays: Effect on the Bonding by 3D Finite Element Analysis. J. Prosthodont. 2016, 27, 741–747. [Google Scholar] [CrossRef]
- Pospiech, P.; Rammelsberg, P.; Goldhofer, G.; Gernet, W. All-ceramic resin-bonded bridges: A3-D finite element analysis study. Eur. J. Oral Sci. 1996, 104, 390–395. [Google Scholar] [CrossRef]
- Keulemans, F.; Shinya, A.; Lassila, L.V.J.; Vallittu, P.K.; Kleverlaan, C.J.; Feilzer, A.J.; De Moor, R.J.G. Three-dimensional finite element analysis of anterior two-unit cantilever resin-bonded fixed dental prostheses. Sci. World J. 2015, 2015, 864389. [Google Scholar] [CrossRef]
- Wang, C.H.; Du, J.K.; Li, H.Y.; Chang, H.C.; Chen, K.K. Factorial analysis of variables influencing mechanical characteristics of a post used to restore a root filled premolar using the finite element stress analysis combined with the Taguchi method. Int. Endod. J. 2016, 49, 690–699. [Google Scholar] [CrossRef]
- Chang, H.C.; Chang, C.H.; Li, H.Y.; Wang, C.H. Biomechanical analysis of the press-fit effect in a conical Morse taper implant system by using an in vitro experimental test and finite element analysis. J. Prosthet. Dent. 2022, 127, 601–608. [Google Scholar] [CrossRef]
- Uraba, A.; Nemoto, R.; Nozaki, K.; Inagaki, T.; Omori, S.; Miura, H. Biomechanical behavior of adhesive cement layer and periodontal tissues on the restored teeth with zirconia RBFDPs using three-kinds of framework design: 3D FEA study. J. Prosthodont. Res. 2018, 62, 227–233. [Google Scholar] [CrossRef]
- Ferrario, V.F.; Sforza, C.; Zanotti, G.; Tartaglia, G.M. Maximal bite forces in healthy young adults as predicted by surface electromyography. J. Dent. 2004, 32, 451–457. [Google Scholar] [CrossRef]
- Magne, P.; Gallucci, G.O.; Belser, U.C. Anatomic crown width/length ratios of unworn and worn maxillary teeth in white subjects. J. Prosthet. Dent. 2003, 89, 453–461. [Google Scholar] [CrossRef] [PubMed]
- Sterrett, J.D.; Oliver, T.; Robinson, F.; Fortson, W.; Knaak, B.; Russell, C.M. Width/length ratios of normal clinical crowns of the maxillary anterior dentition in man. J. Clin. Periodontol. 1999, 26, 153–157. [Google Scholar] [CrossRef] [PubMed]
- Hossain, M.Z.; Munawar Khalil, M.M.; Rahim Zubaidah, H.A.; Mohd Bakri, R.M. Can stature be estimated from tooth crown dimensions? A study in a sample of South-East Asians. Arch. Oral Biol. 2016, 64, 85–91. [Google Scholar] [CrossRef]
- Kelly, J.R.; Tesk, J.A.; Sorensen, J.A. Failure of All-ceramic Fixed Partial Dentures in vitro and in vivo: Analysis and Modeling. J. Dent. Res. 1995, 74, 1253–1258. [Google Scholar] [CrossRef]
- Wang, F.; Yu, T.; Chen, J. Biaxial flexural strength and translucent characteristics of dental lithium disilicate glass ceramics with different translucencies. J. Prosthodont. Res. 2020, 64, 71–77. [Google Scholar] [CrossRef]
- Ghodsi, S.; Jafarian, Z. A review on translucent zirconia. Eur. J. Prosthodont. Restor. Dent. 2018, 26, 62–74. [Google Scholar] [PubMed]
- Wang, C.C.; Fu, P.S.; Wang, J.C.; Lan, T.H.; Lai, P.L.; Du, J.K.; Chen, W.C.; Hung, H.H. Comparison of optical and crystal properties of three translucent yttria-stabilized tetragonal zirconia polycrystals with those of lithium disilicate glass-ceramic material. J. Dent. Sci. 2021, 16, 1247–1254. [Google Scholar] [CrossRef]
- Fabian Fonzar, R.; Carrabba, M.; Sedda, M.; Ferrari, M.; Goracci, C.; Vichi, A. Flexural resistance of heat-pressed and CAD-CAM lithium disilicate with different translucencies. Dent. Mater. 2016, 33, 63–70. [Google Scholar] [CrossRef]
- Kwon, S.J.; Lawson, N.C.; McLaren, E.E.; Nejat, A.H.; Burgess, J.O. Comparison of the mechanical properties of translucent zirconia and lithium disilicate. J. Prosthet. Dent. 2018, 120, 132–137. [Google Scholar] [CrossRef] [PubMed]
- Oh, W.; Götzen, N.; Anusavice, K.J. Influence of connector design on fracture probability of ceramic fixed-partial dentures. J. Dent. Res. 2002, 81, 623–627. [Google Scholar] [CrossRef] [PubMed]
- Raigrodski, A.J.; Hillstead, M.B.; Meng, G.K.; Chung, K.H. Survival and complications of zirconia-based fixed dental prostheses: A systematic review. J. Prosthet. Dent. 2012, 107, 170–177. [Google Scholar] [CrossRef] [PubMed]
- Sailer, I.; Fehér, A.; Filser, F.; Gauckler, L.J.; Lüthy, H.; Hämmerle, C.H.F. Five-year clinical results of zirconia frameworks for posterior fixed partial dentures. Int. J. Prosthodont. 2007, 20, 383–388. [Google Scholar]
- Manda, M.; Galanis, C.; Georgiopoulos, V.; Provatidis, C.; Koidis, P. Effect of varying the vertical dimension of connectors of cantilever cross-arch fixed dental prostheses in patients with severely reduced osseous support: A three-dimensional finite element analysis. J. Prosthet. Dent. 2010, 103, 91–100. [Google Scholar] [CrossRef] [PubMed]
- Sasse, M.; Kern, M. CAD/CAM single retainer zirconia-ceramic resin-bonded fixed dental prostheses: Clinical outcome after 5 years. Int. J. Comput. Dent. 2013, 16, 109–118. [Google Scholar]
- Kern, M. Fifteen-year survival of anterior all-ceramic cantilever resin-bonded fixed dental prostheses. J. Dent. 2017, 56, 133–135. [Google Scholar] [CrossRef]
- Sailer, I.; Hämmerle, C. Zirconia Ceramic Single-Retainer Resin-Bonded Fixed Dental Prostheses (RBFDPs) after 4 Years of Clinical Service: A Retrospective Clinical and Volumetric Study. Int. J. Periodontics Restor. Dent. 2014, 34, 333–343. [Google Scholar] [CrossRef]
- Zhang, X.; Li, T.; Wang, X.; Yang, L.; Wu, J. Glass-ceramic resin-bonded fixed partial dentures for replacing a single premolar tooth: A prospective investigation with a 4-year follow-up. J. Prosthet. Dent. 2020, 124, 53–59. [Google Scholar] [CrossRef]




| Material | Element Size (mm) | Young’s Modulus (MPa) | Poisson Ratio (υ) | Compression (MPa) | Tensile Strength (MPa) | References |
|---|---|---|---|---|---|---|
| Enamel | 0.4 | 95,000 | 0.3 | - | - | [27] |
| Dentine | 0.4 | 18,600 | 0.31 | - | - | [27,28] |
| 5/3-Yttria stabilized Tetragonal zirconia | 0.2 | 205,000 | 0.24 | 192–316 | 27–70 | [29] |
| Lithium disilicate | 0.2 | 83,500 | 0.21 | 1378 | 82 | [27] |
| Periodontal ligament | 0.2 | 68.9 | 0.45 | [30] | ||
| Cortical bone | 0.8 | 13,700 | 0.3 | - | - | [31] |
| Cancellous bone | 0.8 | 1370 | 0.3 | - | - | [31] |
| Lithium Disilicate | Zirconia | ||
|---|---|---|---|
| Rectangular (a) × (b) | Trapezoidal (a) × (b) × 1 mm | Rectangular (a) × (b) | Trapezoidal (a) × (b) × 1 mm |
| 5 × 3 mm | 5 × 4 × 1 mm | 5 × 3 mm | 5 × 4 × 1 mm |
| 5 × 2 mm | 5 × 2 × 1 mm | 5 × 2 mm | 5 × 2 × 1 mm |
| 4 × 3 mm | 4 × 4 × 1 mm | 4 × 3 mm | 4 × 4 × 1 mm |
| 4 × 2 mm | 4 × 2 × 1 mm | 4 × 2 mm | 4 × 2 × 1 mm |
| Connector Type | Dimensions | Connector Volume (mm3) |
|---|---|---|
| Rectangular | 5 × 3 mm | 19.61 |
| 5 × 2 mm | 9.04 | |
| 4 × 3 mm | 11.61 | |
| 4 × 2 mm | 6.55 | |
| Trapezoidal | 5 × 4 × 1 mm | 10.98 |
| 5 × 2 × 1 mm | 3.98 | |
| 4 × 4 × 1 mm | 9.10 | |
| 4 × 2 × 1 mm | 3.35 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Osman, M.L.M.; Lim, T.W.; Chang, H.-C.; Ab Ghani, A.R.; Tsoi, J.K.H.; Ab Ghani, S.M. Structural Integrity of Anterior Ceramic Resin-Bonded Fixed Partial Denture: A Finite Element Analysis Study. J. Funct. Biomater. 2023, 14, 108. https://doi.org/10.3390/jfb14020108
Osman MLM, Lim TW, Chang H-C, Ab Ghani AR, Tsoi JKH, Ab Ghani SM. Structural Integrity of Anterior Ceramic Resin-Bonded Fixed Partial Denture: A Finite Element Analysis Study. Journal of Functional Biomaterials. 2023; 14(2):108. https://doi.org/10.3390/jfb14020108
Chicago/Turabian StyleOsman, Mas Linda Mohd, Tong Wah Lim, Hung-Chih Chang, Amir Radzi Ab Ghani, James Kit Hon Tsoi, and Siti Mariam Ab Ghani. 2023. "Structural Integrity of Anterior Ceramic Resin-Bonded Fixed Partial Denture: A Finite Element Analysis Study" Journal of Functional Biomaterials 14, no. 2: 108. https://doi.org/10.3390/jfb14020108
APA StyleOsman, M. L. M., Lim, T. W., Chang, H.-C., Ab Ghani, A. R., Tsoi, J. K. H., & Ab Ghani, S. M. (2023). Structural Integrity of Anterior Ceramic Resin-Bonded Fixed Partial Denture: A Finite Element Analysis Study. Journal of Functional Biomaterials, 14(2), 108. https://doi.org/10.3390/jfb14020108








