Multi-Stimulus Responsive Multilayer Coating for Treatment of Device-Associated Infections
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials and Instrumentation
2.2. Synthesis of PPPB
2.3. Synthesis of (MMT-PPPB-CHA)n Coating
2.4. Characterization of Polymers PPPB
2.5. Characterization of (MMT-PPPB-CHA)n Coating
2.6. The Standard Curve of CHA
2.7. CHA Loading Capacity of (MMT-PPPB-CHA)n Coating
2.8. Sustained Drug-Releasing Capacity of (MMT-PPPB-CHA)3 Coating
2.9. Multi-Stimulus Responsive Ability of (MMT-PPPB-CHA)3 Coating
2.10. Preparation of Bacteria Suspensions
2.11. In Vitro Antibacterial Activity of (MMT-PPPB-CHA)3 Coating
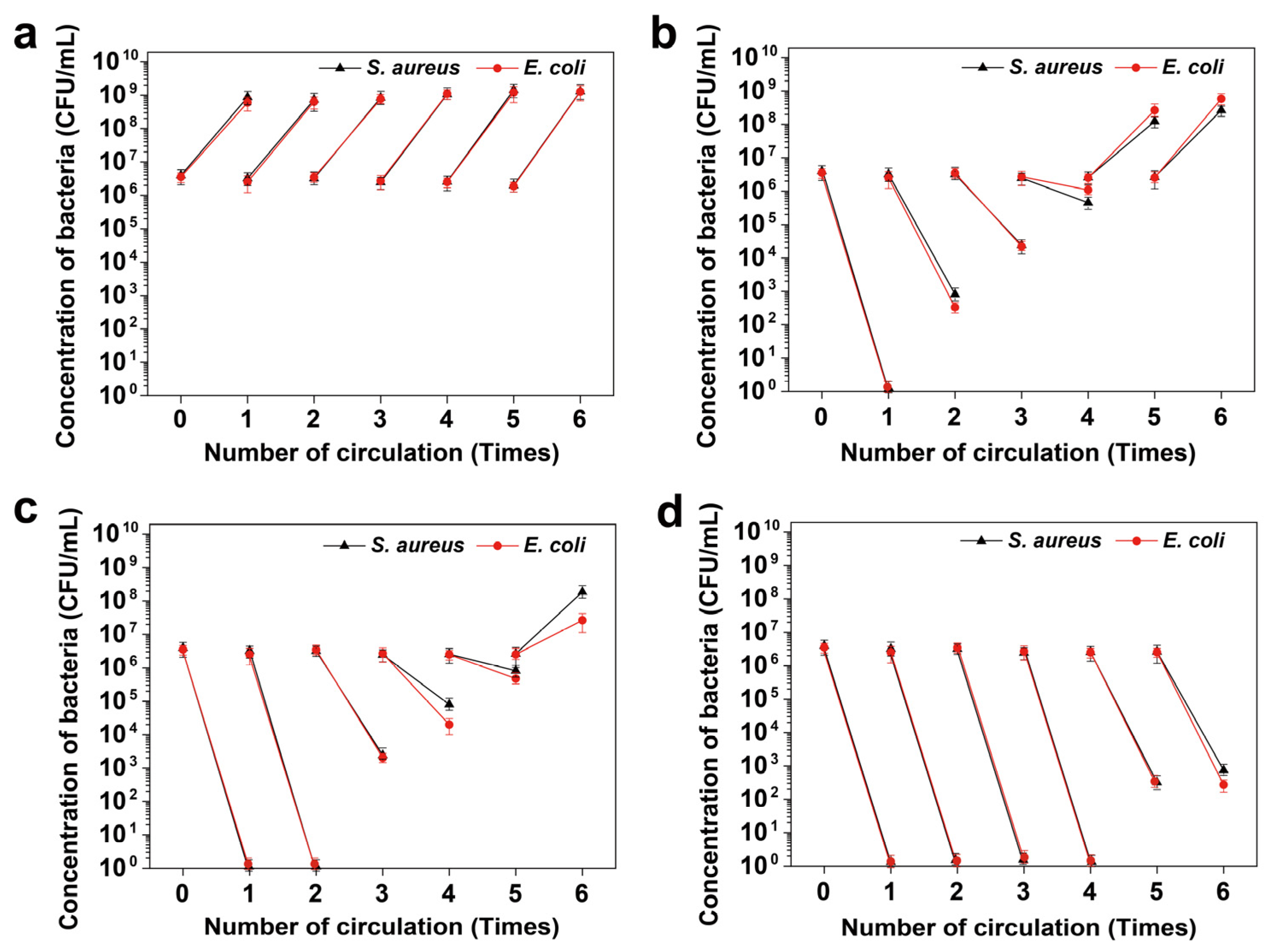
2.12. Long-Term Antibacterial Performance of (MMT-PPPB-CHA)3 Coating
2.13. In Vivo Antibacterial Activity and Full-Thickness Skin Defect Healing
2.14. Statistical Analysis
3. Results and Discussion
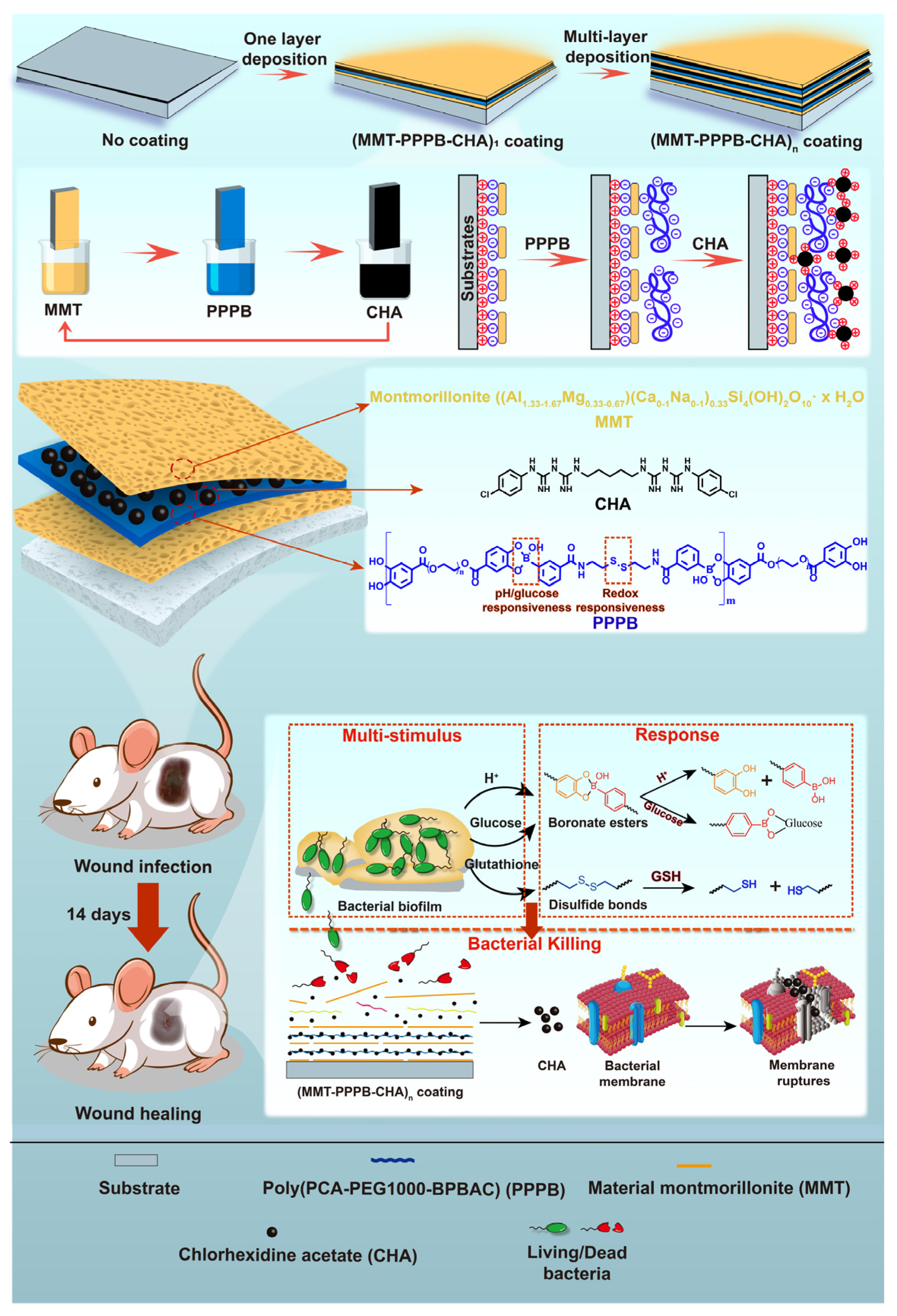
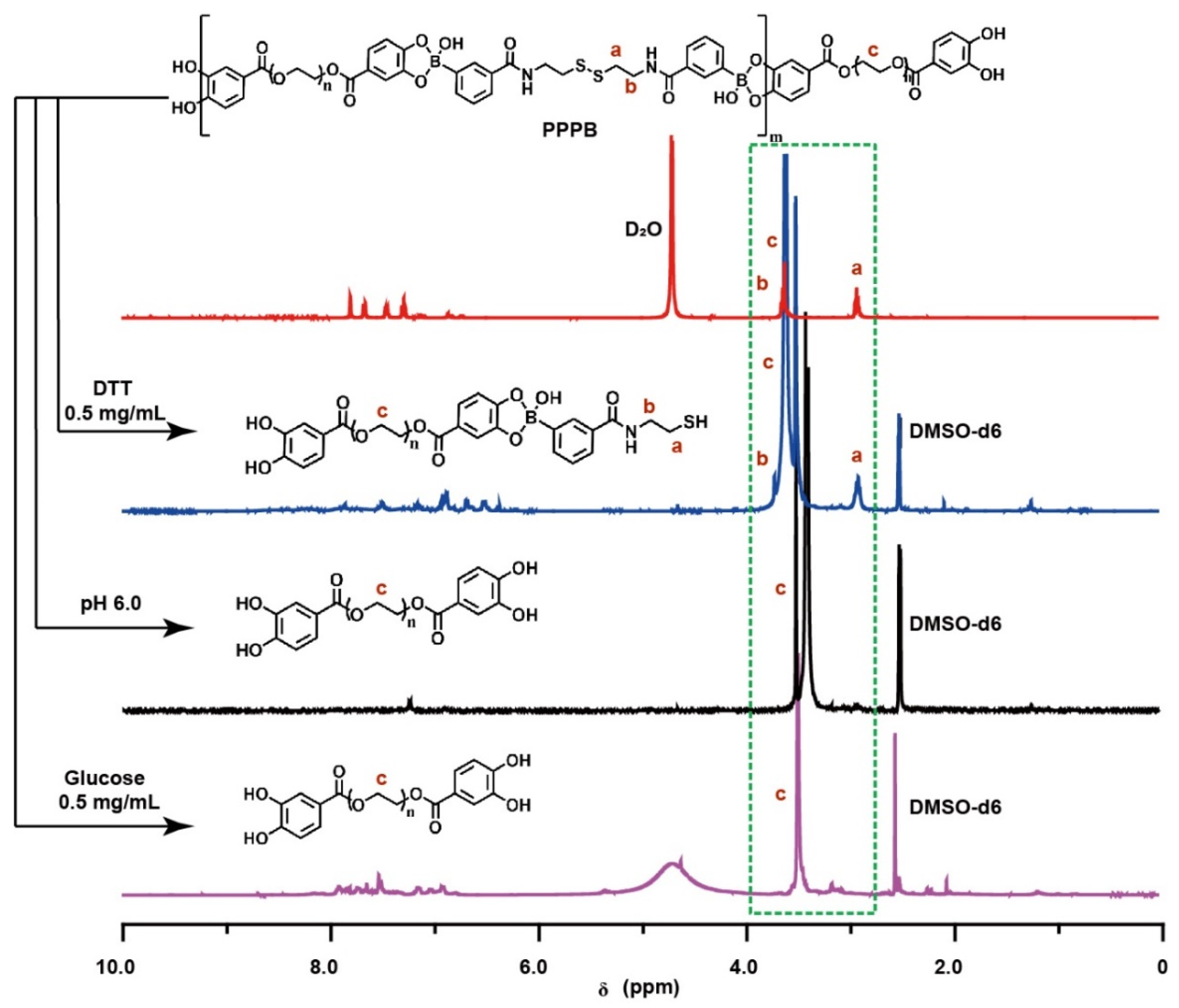
3.1. Synthesis of the Multi-Stimulus Responsive Polymer PPPB
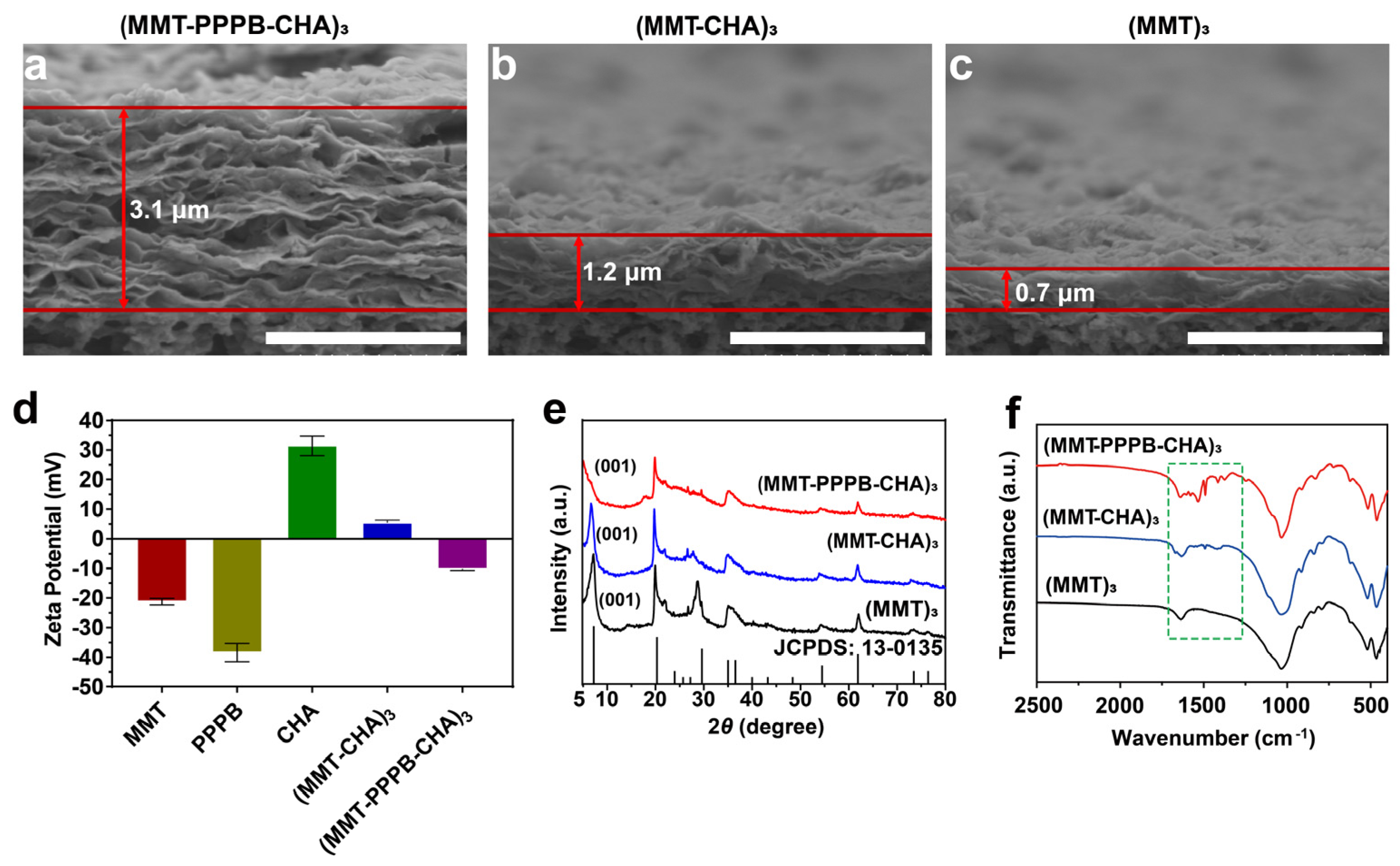
3.2. Construction of the of (MMT-PPPB-CHA)n Coating
3.3. CHA Loading Capacity and Releasing Kinetics of (MMT-PPPB-CHA)n Coating
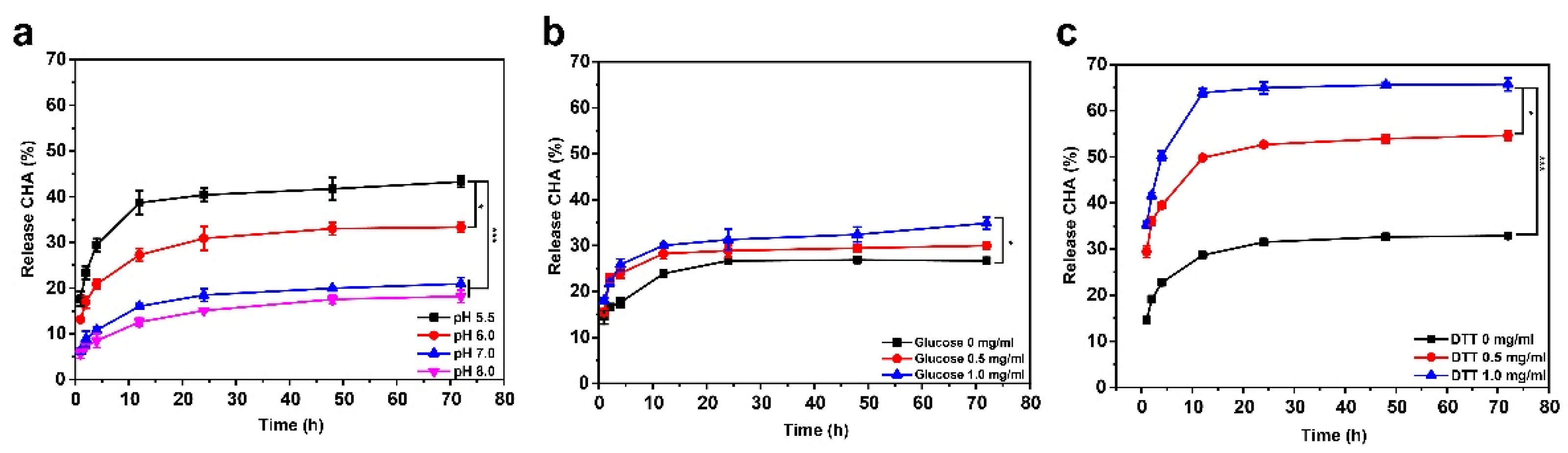
3.4. Multistimulus-Responsive Drug Release Behavior of (MMT-PPPB-CHA)n Coating
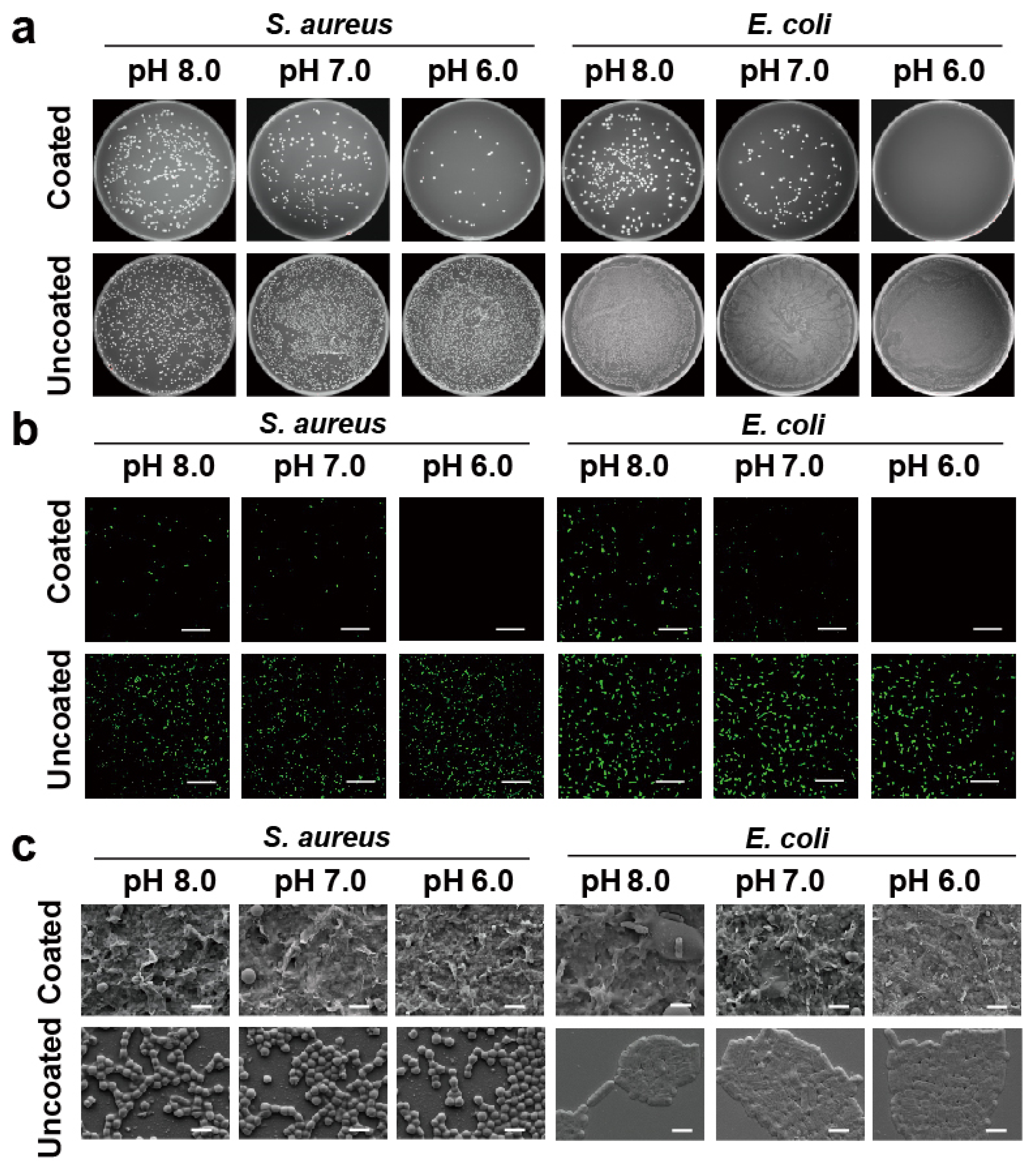
3.5. In Vitro Antibacterial Activity of (MMT-PPPB-CHA)n Coating
3.6. In Vivo Antibacterial Activity and Full-Thickness Skin Defect Healing of (MMT-PPPB CHA)n Coating
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Brooks, B.; Olm, M.R.; Firek, B.A.; Baker, R.; Geller-McGrath, D.; Reimer, S.R.; Soenjoyo, K.R.; Yip, J.S.; Dahan, D.; Thomas, B.C.; et al. The developing premature infant gut microbiome is a major factor shaping the microbiome of neonatal intensive care unit rooms. Microbiome 2018, 6, 12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Burny, F.; Donkerwolcke, M.; Moulart, F.; Bourgois, R.; Puers, R.; Van Schuylenbergh, K.; Barbosa, M.; Paiva, O.; Rodes, F.; Begueret, J.B.; et al. Concept, design and fabrication of smart orthopedic implants. Med. Eng. Phys. 2000, 22, 469–479. [Google Scholar] [CrossRef]
- Arciola, C.R.; Campoccia, D.; Montanaro, L. Implant infections: Adhesion, biofilm formation and immune evasion. Nat. Rev. Microbiol. 2018, 16, 397–409. [Google Scholar] [CrossRef] [PubMed]
- Weiner-Lastinger, L.M.; Abner, S.; Edwards, J.R.; Kallen, A.J.; Karlsson, M.; Magill, S.S.; Pollock, D.; See, I.; Soe, M.M.; Walters, M.S.; et al. Antimicrobial-resistant pathogens associated with adult healthcare-associated infections: Summary of data reported to the National Healthcare Safety Network, 2015–2017. Infect. Control. Hosp. Epidemiol. 2020, 41, 1–18. [Google Scholar] [CrossRef] [Green Version]
- Zhou, C.; Wu, Y.; Thappeta, K.R.V.; Subramanian, J.T.L.; Pranantyo, D.; Kang, E.T.; Duan, H.W.; Kline, K.; Chan-Park, M.B. In Vivo Anti-Biofilm and Anti-Bacterial Non-Leachable Coating Thermally Polymerized on Cylindrical Catheter. ACS Appl. Mater. Interfaces 2017, 9, 36269–36280. [Google Scholar] [CrossRef]
- Wang, B.L.; Liu, H.H.; Wang, Z.F.; Shi, S.; Nan, K.H.; Xu, Q.W.; Ye, Z.; Chen, H. A self-defensive antibacterial coating acting through the bacteria-triggered release of a hydrophobic antibiotic from layer-by-layer films. J. Mat. Chem. B 2017, 5, 1498–1506. [Google Scholar] [CrossRef]
- Wei, T.; Yu, Q.; Chen, H. Responsive and Synergistic Antibacterial Coatings: Fighting against Bacteria in a Smart and Effective Way. Adv. Healthc. Mater. 2019, 8, 1801381. [Google Scholar] [CrossRef]
- Chen, R.; Shi, C.; Xi, Y.; Zhao, P.; He, H. Fabrication of cationic polymer surface through plasma polymerization and layer-by-layer assembly. Mater. Manuf. Processes 2020, 35, 221–229. [Google Scholar] [CrossRef]
- Liu, P.; Fu, K.; Zeng, X.; Chen, N.; Wen, X. Fabrication and Characterization of Composite Meshes Loaded with Antimicrobial Peptides. ACS Appl. Mater. Interfaces 2019, 11, 24609–24617. [Google Scholar] [CrossRef]
- Liu, Z.; Ma, S.; Duan, S.; Deng, X.; Sun, Y.; Zhang, X.; Xu, X.; Guan, B.; Wang, C.; Hu, M.; et al. Modification of Titanium Substrates with Chimeric Peptides Comprising Antimicrobial and Titanium-Binding Motifs Connected by Linkers To Inhibit Biofilm Formation. ACS Appl. Mater. Interfaces 2016, 8, 5124–5136. [Google Scholar] [CrossRef]
- Bhaskara, U.R.; Warmoeskerken, M.; Nabers, M.G.D.; Nanomi, B.V. Antimicrobial Functionalization of beta-Cyclodextrin Treated Fabrics. AATCC J. Res. 2016, 3, 15–24. [Google Scholar] [CrossRef]
- Zhou, C.; Wang, F.; Chen, H.; Li, M.; Qiao, F.; Liu, Z.; Hou, Y.; Wu, C.; Fan, Y.; Liu, L.; et al. Selective Antimicrobial Activities and Action Mechanism of Micelles Self-Assembled by Cationic Oligomeric Surfactants. ACS Appl. Mater. Interfaces 2016, 8, 4242–4249. [Google Scholar] [CrossRef]
- Yao, Q.Q.; Ye, Z.; Sun, L.; Jin, Y.Y.; Xu, Q.W.; Yang, M.; Wang, Y.; Zhou, Y.L.; Ji, J.; Chen, H.; et al. Bacterial infection microenvironment-responsive enzymatically degradable multilayer films for multifunctional antibacterial properties. J. Mat. Chem. B 2017, 5, 8532–8541. [Google Scholar] [CrossRef]
- Saha, K.; Butola, B.S.; Joshi, M. Synthesis and characterization of chlorhexidine acetate drug-montmorillonite intercalates for antibacterial applications. Appl. Clay Sci. 2014, 101, 477–483. [Google Scholar] [CrossRef]
- Datta, S.M. Clay-polymer nanocomposites as a novel drug carrier: Synthesis, characterization and controlled release study of Propranolol Hydrochloride. Appl. Clay Sci. 2013, 80–81, 85–92. [Google Scholar] [CrossRef]
- Fillion, M.; Goudreault, M.; Voyer, N.; Bechinger, B.; Auger, M. Amphiphilicity Is a Key Determinant in the Membrane Interactions of Synthetic 14-mer Cationic Peptide Analogues. Biochemistry 2016, 55, 6919–6930. [Google Scholar] [CrossRef]
- Chen, H.; Jin, Y.Y.; Wang, J.J.; Wang, Y.Q.; Jiang, W.Y.; Dai, H.D.; Pang, S.Y.; Lei, L.; Ji, J.; Wang, B.L. Design of smart targeted and responsive drug delivery systems with enhanced antibacterial properties. Nanoscale 2018, 10, 20946–20962. [Google Scholar] [CrossRef]
- Li, M.; Wang, H.Q.; Chen, X.M.; Jin, S.N.; Chen, W.; Meng, Y.C.; Liu, Y.; Guo, Y.S.; Jiang, W.Y.; Xu, X.; et al. Chemical grafting of antibiotics into multilayer films through Schiff base reaction for self-defensive response to bacterial infections. Chem. Eng. J. 2020, 382, 122973. [Google Scholar] [CrossRef]
- Xu, Q.W.; Li, X.; Jin, Y.Y.; Sun, L.; Ding, X.X.; Liang, L.; Wang, L.; Nan, K.H.; Ji, J.; Chen, H.; et al. Bacterial self-defense antibiotics release from organic-inorganic hybrid multilayer films for long-term anti-adhesion and biofilm inhibition properties. Nanoscale 2017, 9, 19245–19254. [Google Scholar] [CrossRef]
- Zhao, Y.Q.; Sun, Y.J.; Zhang, Y.D.; Ding, X.K.; Zhao, N.N.; Yu, B.R.; Zhao, H.; Duan, S.; Xu, F.J. Well-Defined Gold Nanorod/Polymer Hybrid Coating with Inherent Antifouling and Photothermal Bactericidal Properties for Treating an Infected Hernia. ACS Nano 2020, 14, 2265–2275. [Google Scholar] [CrossRef]
- Wei, T.; Zhan, W.J.; Yu, Q.; Chen, H. Smart Biointerface with Photoswitched Functions between Bactericidal Activity and Bacteria-Releasing Ability. ACS Appl. Mater. Interfaces 2017, 9, 25767–25774. [Google Scholar] [CrossRef] [PubMed]
- Nastyshyn, S.; Raczkowska, J.; Stetsyshyn, Y.; Orzechowska, B.; Bernasik, A.; Shymborska, Y.; Brzychczy-Wloch, M.; Gosiewski, T.; Lishchynskyi, O.; Ohar, H.; et al. Non-cytotoxic, temperature-responsive and antibacterial POEGMA based nanocomposite coatings with silver nanoparticles. RSC Adv. 2020, 10, 10155–10166. [Google Scholar] [CrossRef]
- Zhou, Y.; Zheng, Y.J.; Wei, T.; Qu, Y.C.; Wang, Y.R.; Zhan, W.J.; Zhang, Y.X.; Pan, G.Q.; Li, D.; Yu, Q.; et al. Multistimulus Responsive Biointerfaces with Switchable Bioadhesion and Surface Functions. ACS Appl. Mater. Interfaces 2020, 12, 5447–5455. [Google Scholar] [CrossRef] [PubMed]
- Chouirfa, H.; Bouloussa, H.; Migonney, V.; Falentin-Daudre, C. Review of titanium surface modification techniques and coatings for antibacterial applications. Acta Biomater. 2019, 83, 37–54. [Google Scholar] [CrossRef]
- Wang, B.L.; Jin, T.W.; Xu, Q.W.; Liu, H.H.; Ye, Z.; Chen, H. Direct Loading and Tunable Release of Antibiotics from Polyelectrolyte Multilayers To Reduce Bacterial Adhesion and Biofilm Formation. Bioconjugate Chem. 2016, 27, 1305–1313. [Google Scholar] [CrossRef]
- Manyi-Loh, C.; Mamphweli, S.; Meyer, E.; Okoh, A. Antibiotic Use in Agriculture and Its Consequential Resistance in Environmental Sources: Potential Public Health Implications. Molecules 2018, 23, 795. [Google Scholar] [CrossRef] [Green Version]
- Iler, R.K. Multilayers of colloidal particles. J. Colloid Interface Sci. 1966, 21, 569–594. [Google Scholar] [CrossRef]
- Richardson, J.J.; Cui, J.W.; Bjornmalm, M.; Braunger, J.A.; Ejima, H.; Caruso, F. Innovation in Layer-by-Layer Assembly. Chem. Rev. 2016, 116, 14828–14867. [Google Scholar] [CrossRef] [Green Version]
- Zhang, X.H.; Ou-yang, S.; Wang, J.L.; Liao, L.; Wu, R.F.; Wei, J.C. Construction of Antibacterial Surface Via Layer-by-Layer Method. Curr. Pharm. Des. 2018, 24, 926–935. [Google Scholar] [CrossRef]
- Singh, A.V.; Baylan, S.; Park, B.W.; Richter, G.; Sitti, M. Hydrophobic pinning with copper nanowhiskers leads to bactericidal properties. PLoS ONE 2017, 12, e0175428. [Google Scholar] [CrossRef] [Green Version]
- Yu, H.-C.; Kim, Y.-K. Fractures of implant fixtures: A retroscccpective clinical study. Maxillofac. Plast. Reconstr. Surg. 2020, 42, 13. [Google Scholar] [CrossRef]
- Lobato-Aguilar, H.; Uribe-Calderon, J.A.; Herrera-Kao, W.; Duarte-Aranda, S.; Baas-Lopez, J.M.; Escobar-Morales, B.; Cauich-Rodriguez, J.V.; Cervantes-Uc, J.M. Synthesis, characterization and chlorhexidine release from either montmorillonite or palygorskite modified organoclays for antibacterial applications. J. Drug Deliv. Sci. Technol. 2018, 46, 452–460. [Google Scholar] [CrossRef]
- Song, X.P.; Tang, J. Extraction Optimization, Preliminary Characterization and Bioactivities in Vitro of Ligularia hodgsonii Polysaccharides. Int. J. Mol. Sci. 2016, 17, 788. [Google Scholar] [CrossRef] [Green Version]
- Wang, W.T.; Wu, B.; Qin, H.; Liu, P.T.; Qin, Y.; Duan, G.W.; Hu, G.Q.; He, M.X. Genome shuffling enhances stress tolerance of Zymomonas mobilis to two inhibitors. Biotechnol. Biofuels 2019, 12, 288. [Google Scholar] [CrossRef] [Green Version]
- Fan, W.; Sun, Q.; Li, Y.Y.; Tay, F.R.; Fan, B. Synergistic mechanism of Ag+-Zn2+ in anti-bacterial activity against Enterococcus faecalis and its application against dentin infection. J. Nanobiotechnol. 2018, 16, 10. [Google Scholar] [CrossRef]
- Li, W.T.; Zhang, H.X.; Li, X.L.; Yu, H.; Che, C.Y.; Luan, S.F.; Ren, Y.F.; Li, S.; Liu, P.; Yu, X.T.; et al. Multifunctional Antibacterial Materials Comprising Water Dispersible Random Copolymers Containing a Fluorinated Block and Their Application in Catheters. ACS Appl. Mater. Interfaces 2020, 12, 7617–7630. [Google Scholar] [CrossRef]
- Joshi, K.M.; Shelar, A.; Kasabe, U.; Nikam, L.K.; Pawar, R.A.; Sangshetti, J.; Kale, B.B.; Singh, A.V.; Patil, R.; Chaskar, M.G. Biofilm inhibition in Candida albicans with biogenic hierarchical zinc-oxide nanoparticles. Mater. Sci. Eng. C 2021, 112592. [Google Scholar] [CrossRef]



| Groups | Factors | CHA Release Rate (%) | ||
|---|---|---|---|---|
| pH | Glucose (mg/mL) | DTT (mg/mL) | ||
| a | 6.0 | 0 | 0 | 56.0 ± 3.2 |
| b | 6.0 | 0.5 | 0.5 | 60.1 ± 2.0 |
| c | 6.0 | 1.0 | 1.0 | 70.1 ± 1.3 |
| d | 7.0 | 0 | 0.5 | 56.7 ± 1.7 |
| e | 7.0 | 0.5 | 1.0 | 62.0 ± 2.3 |
| f | 7.0 | 1.0 | 0 | 53.9 ± 1.1 |
| g | 8.0 | 0 | 1.0 | 43.3 ± 1.6 |
| h | 8.0 | 0.5 | 0 | 34.3 ± 1.8 |
| i | 8.0 | 1.0 | 0.5 | 50.7 ± 2.8 |
| K1 | 186.2 | 156.0 | 144.2 | |
| K2 | 172.6 | 156.4 | 167.8 | |
| K3 | 128.3 | 174.7 | 175.4 | |
| k1 | 62.1 | 52.0 | 48.1 | |
| k2 | 57.5 | 52.1 | 55.9 | |
| k3 | 42.8 | 58.2 | 58.5 | |
| R | 19.3 | 6.2 | 10.4 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, W.; Hua, G.; Cai, J.; Zhou, Y.; Zhou, X.; Wang, M.; Wang, X.; Fu, B.; Ren, L. Multi-Stimulus Responsive Multilayer Coating for Treatment of Device-Associated Infections. J. Funct. Biomater. 2022, 13, 24. https://doi.org/10.3390/jfb13010024
Li W, Hua G, Cai J, Zhou Y, Zhou X, Wang M, Wang X, Fu B, Ren L. Multi-Stimulus Responsive Multilayer Coating for Treatment of Device-Associated Infections. Journal of Functional Biomaterials. 2022; 13(1):24. https://doi.org/10.3390/jfb13010024
Chicago/Turabian StyleLi, Wenlong, Guanping Hua, Jingfeng Cai, Yaming Zhou, Xi Zhou, Miao Wang, Xiumin Wang, Baoqing Fu, and Lei Ren. 2022. "Multi-Stimulus Responsive Multilayer Coating for Treatment of Device-Associated Infections" Journal of Functional Biomaterials 13, no. 1: 24. https://doi.org/10.3390/jfb13010024
APA StyleLi, W., Hua, G., Cai, J., Zhou, Y., Zhou, X., Wang, M., Wang, X., Fu, B., & Ren, L. (2022). Multi-Stimulus Responsive Multilayer Coating for Treatment of Device-Associated Infections. Journal of Functional Biomaterials, 13(1), 24. https://doi.org/10.3390/jfb13010024








