Molar Septum Expansion with Osseodensification for Immediate Implant Placement, Retrospective Multicenter Study with Up-to-5-Year Follow-Up, Introducing a New Molar Socket Classification
Abstract
:1. Introduction
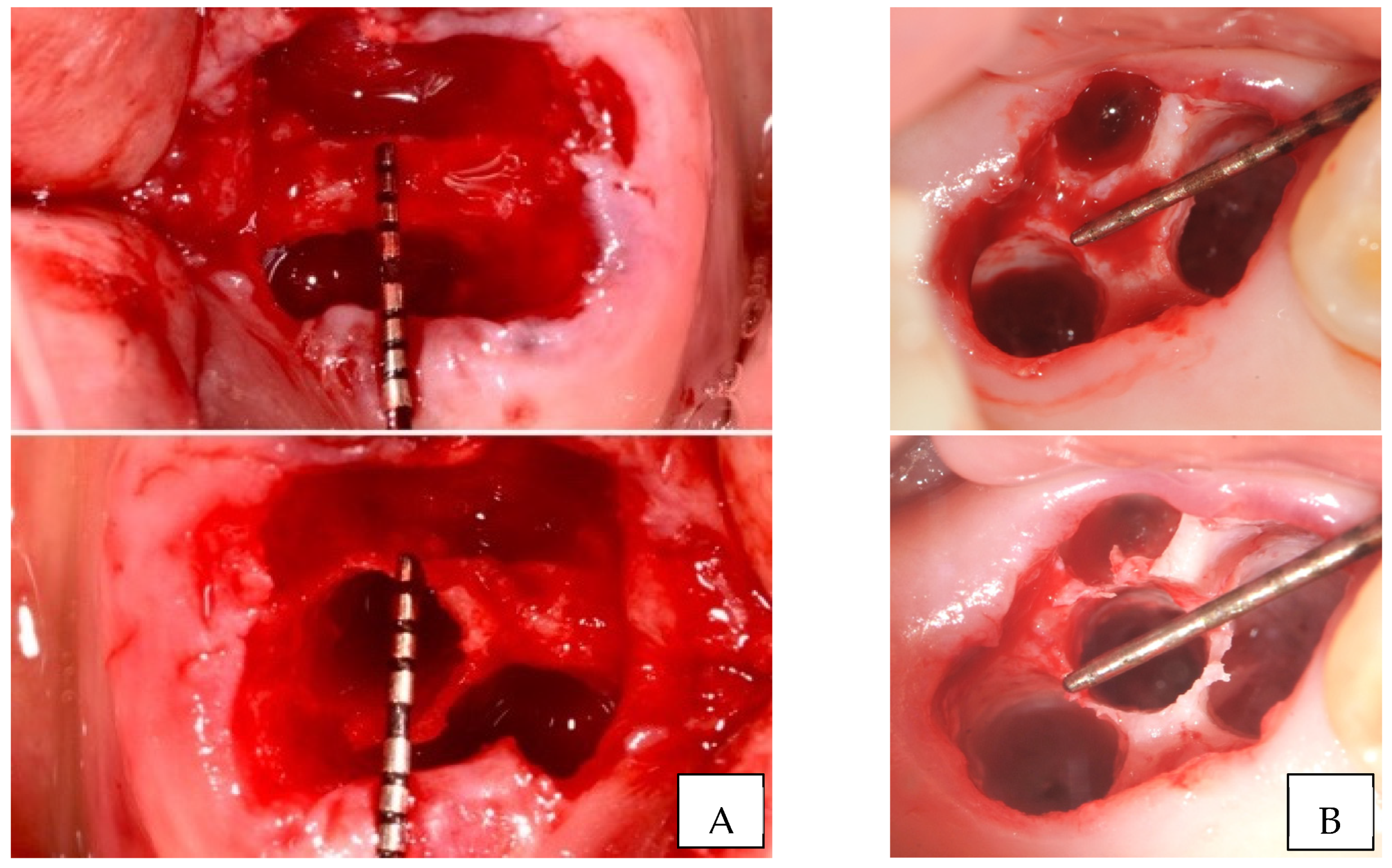
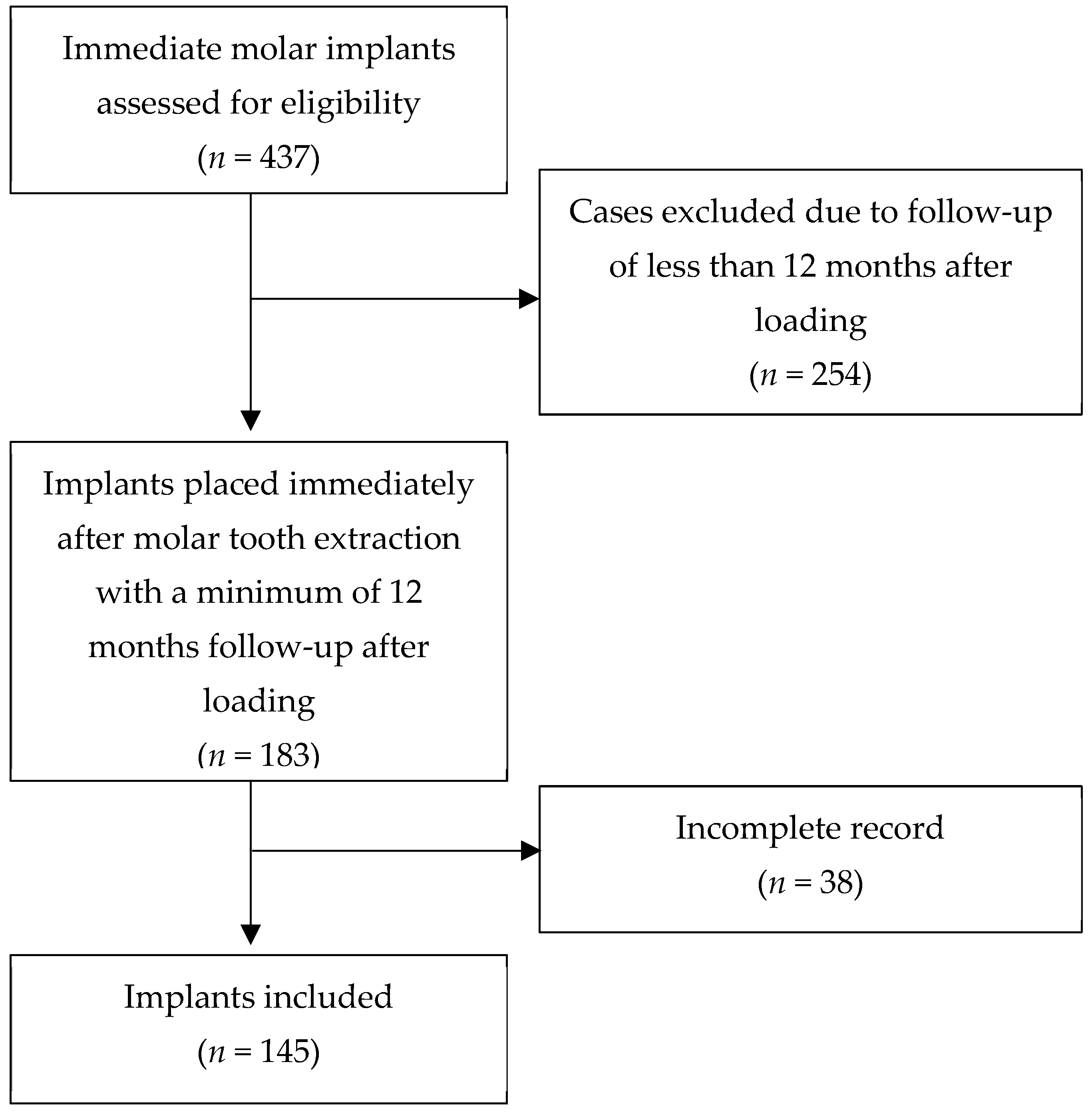
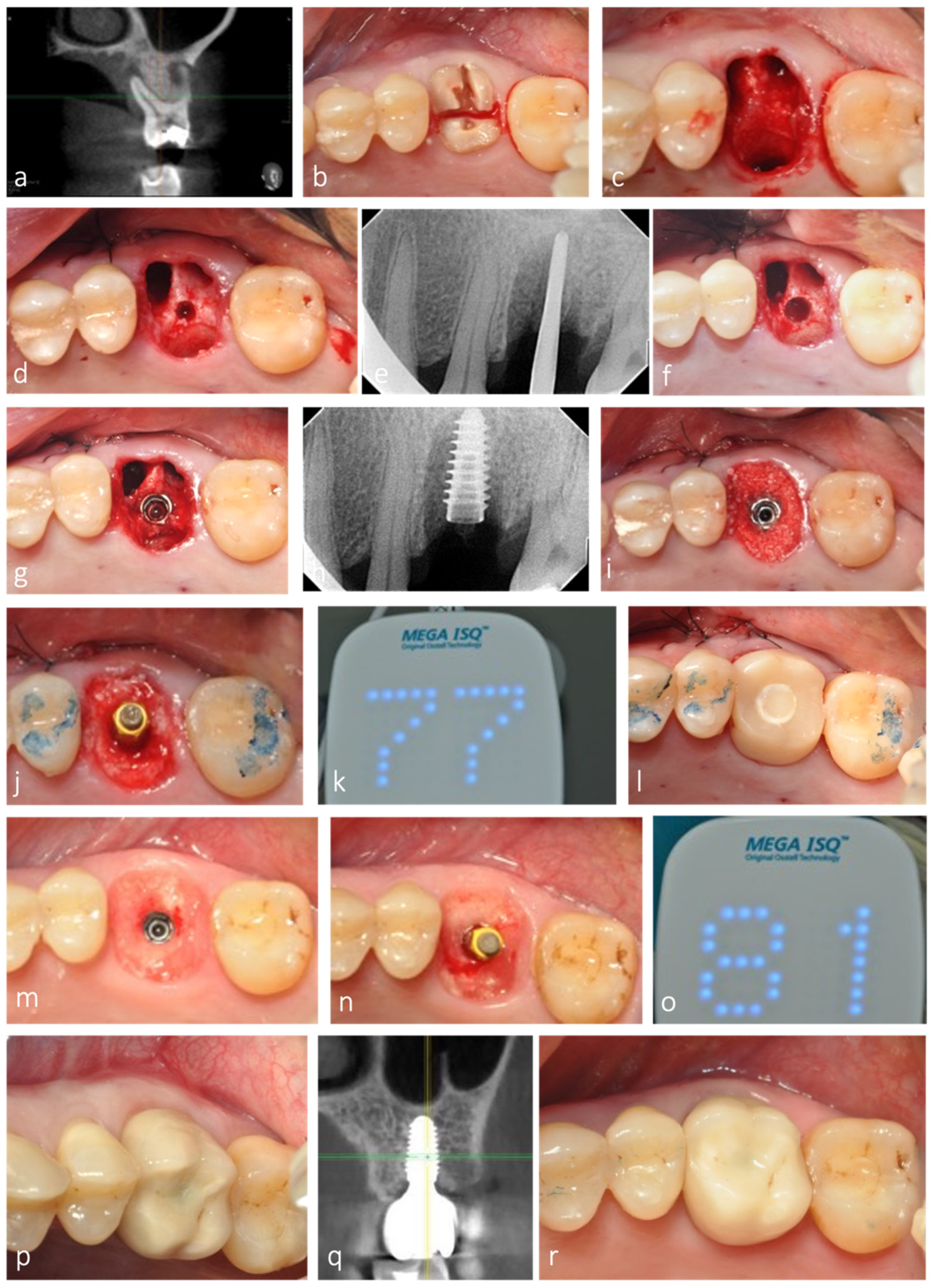
2. Materials and Methods
2.1. Selection Criteria and Surgical Technique
2.2. Variables and Statistics
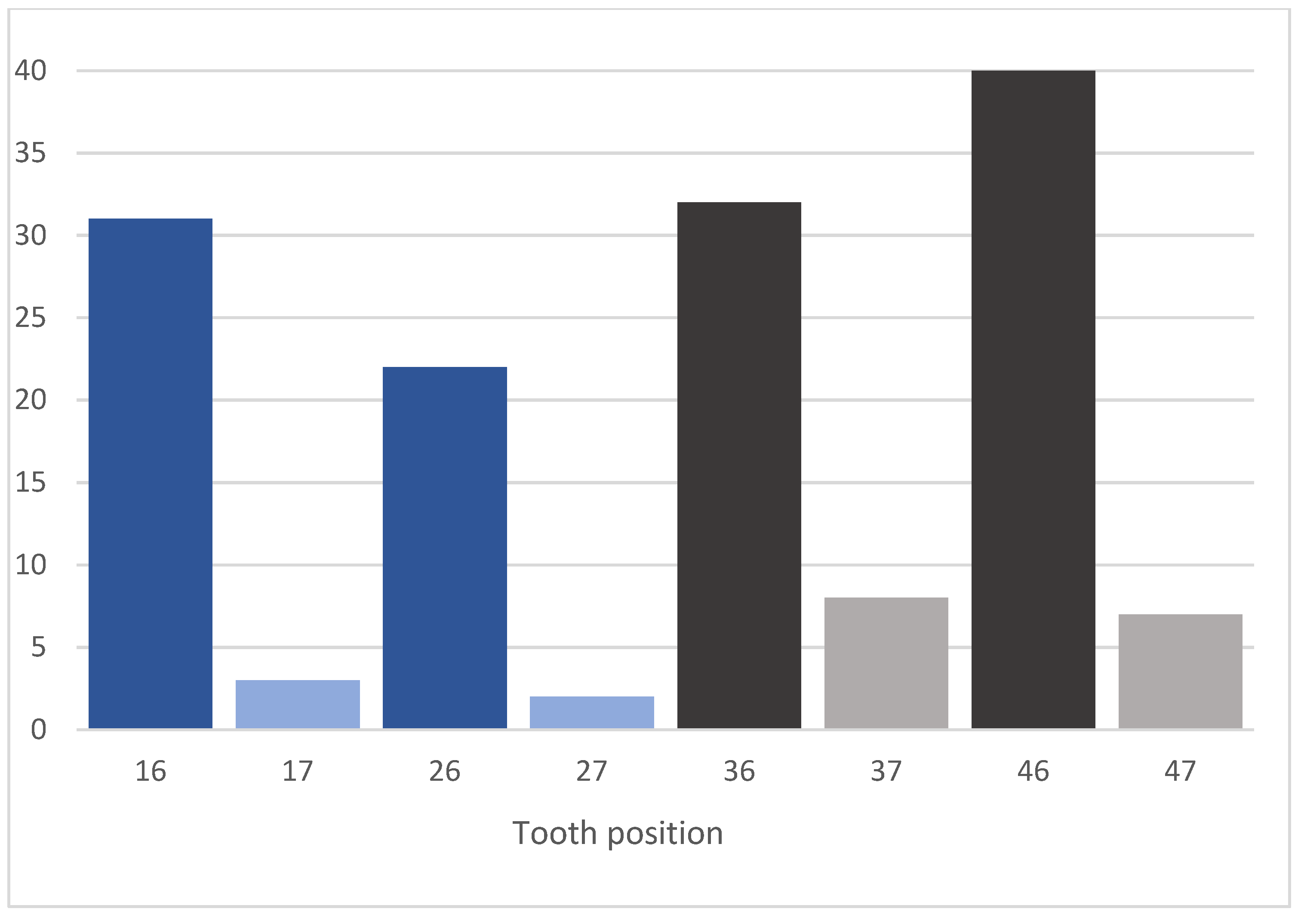
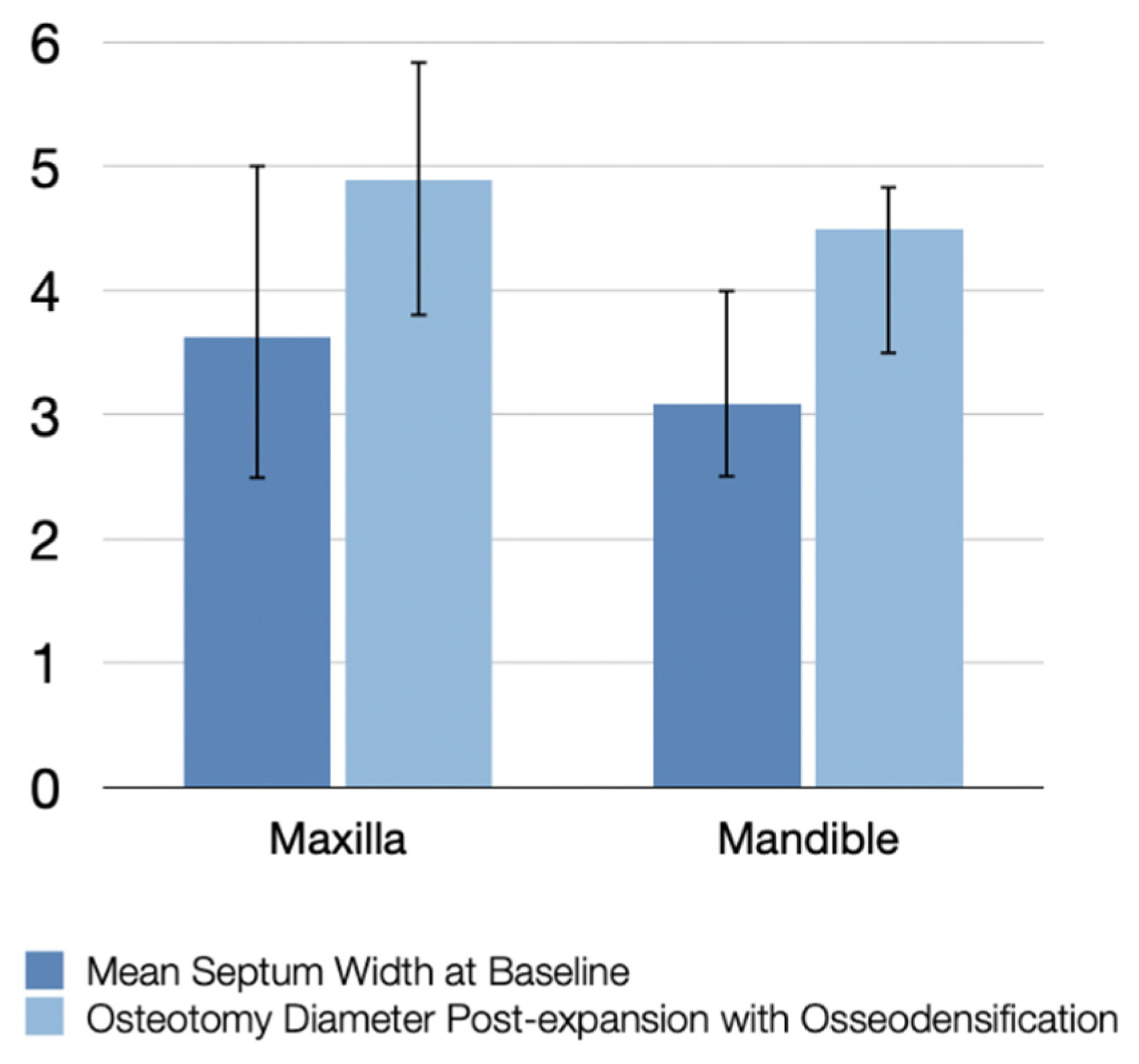
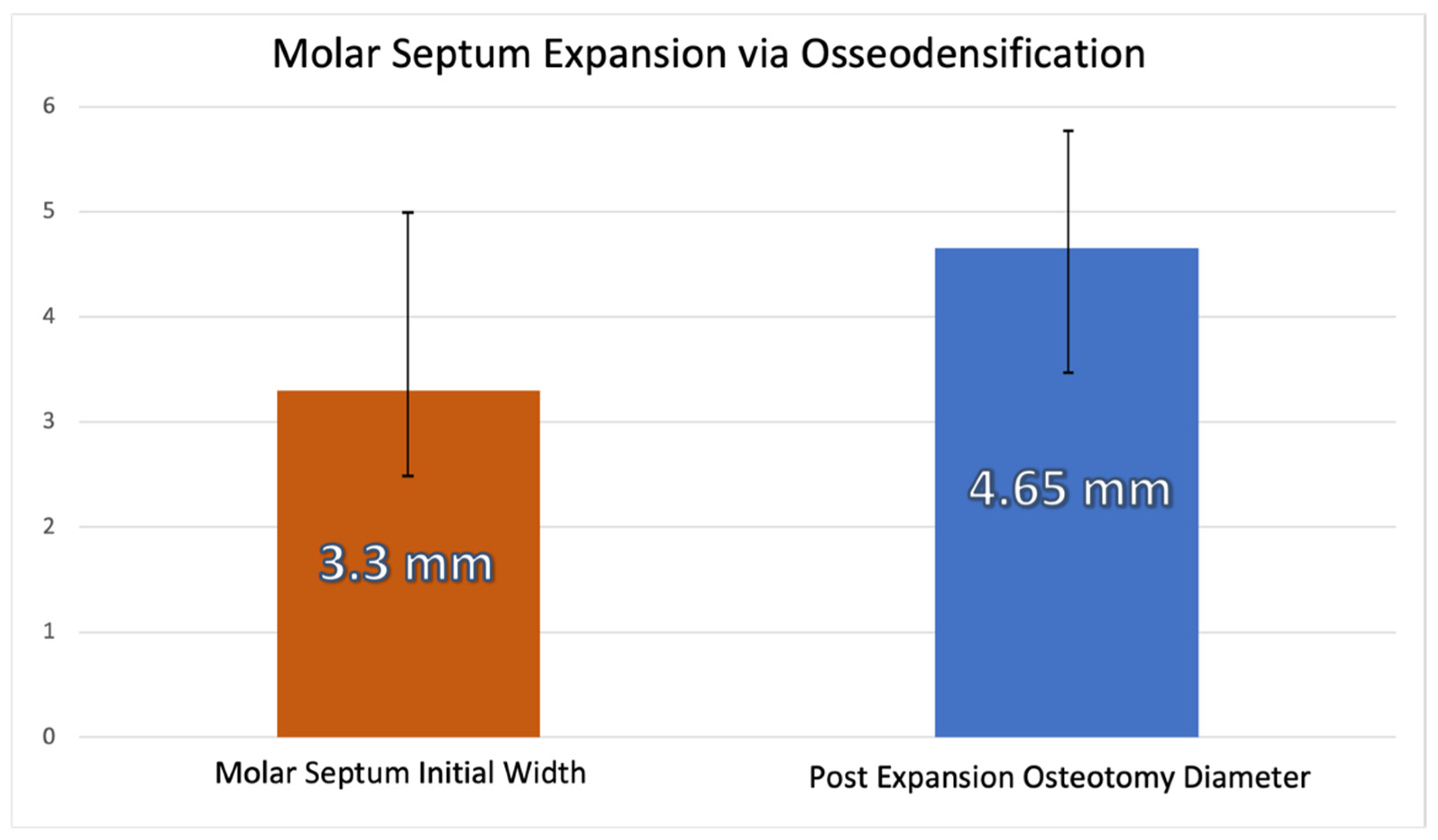
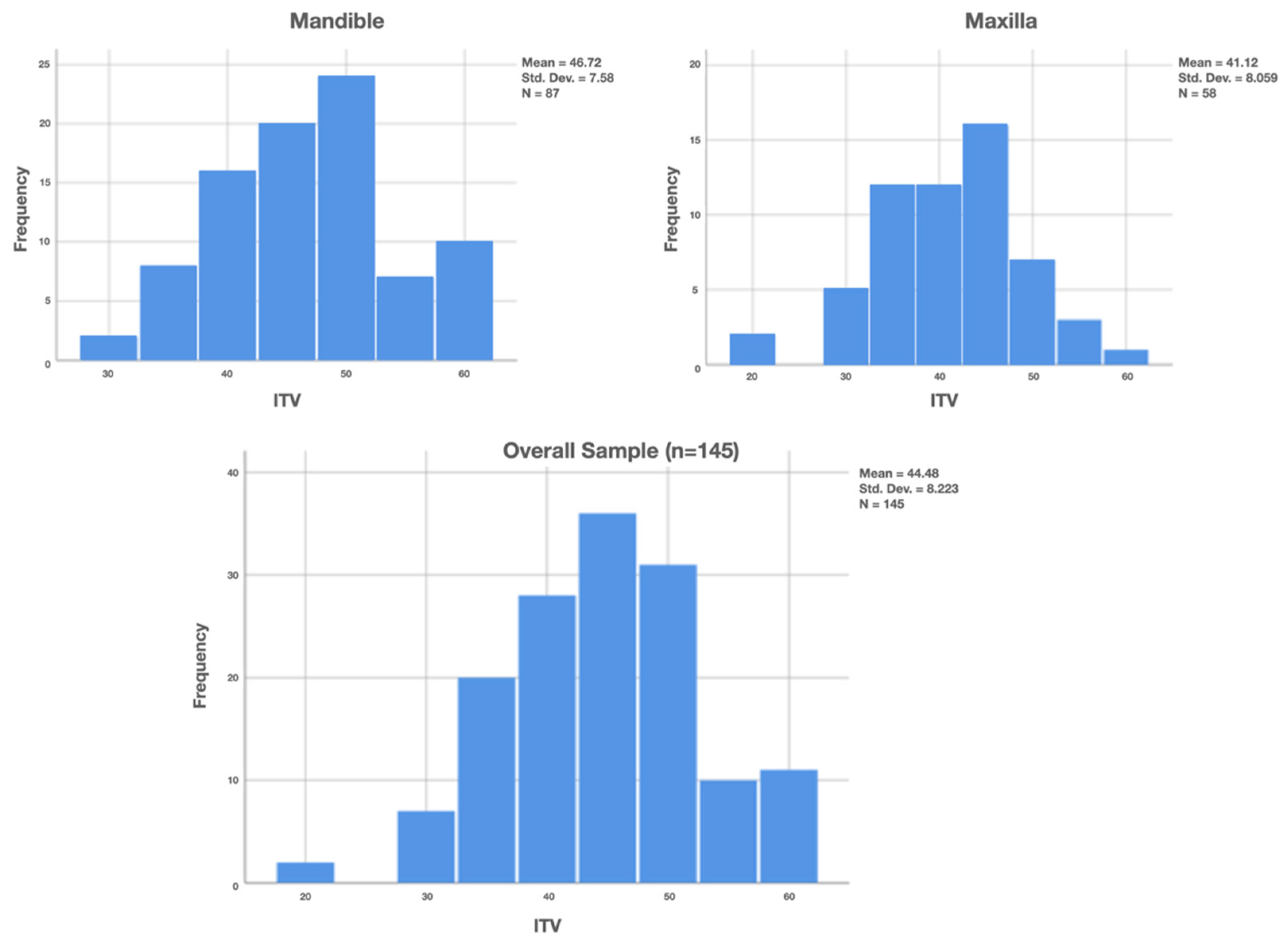
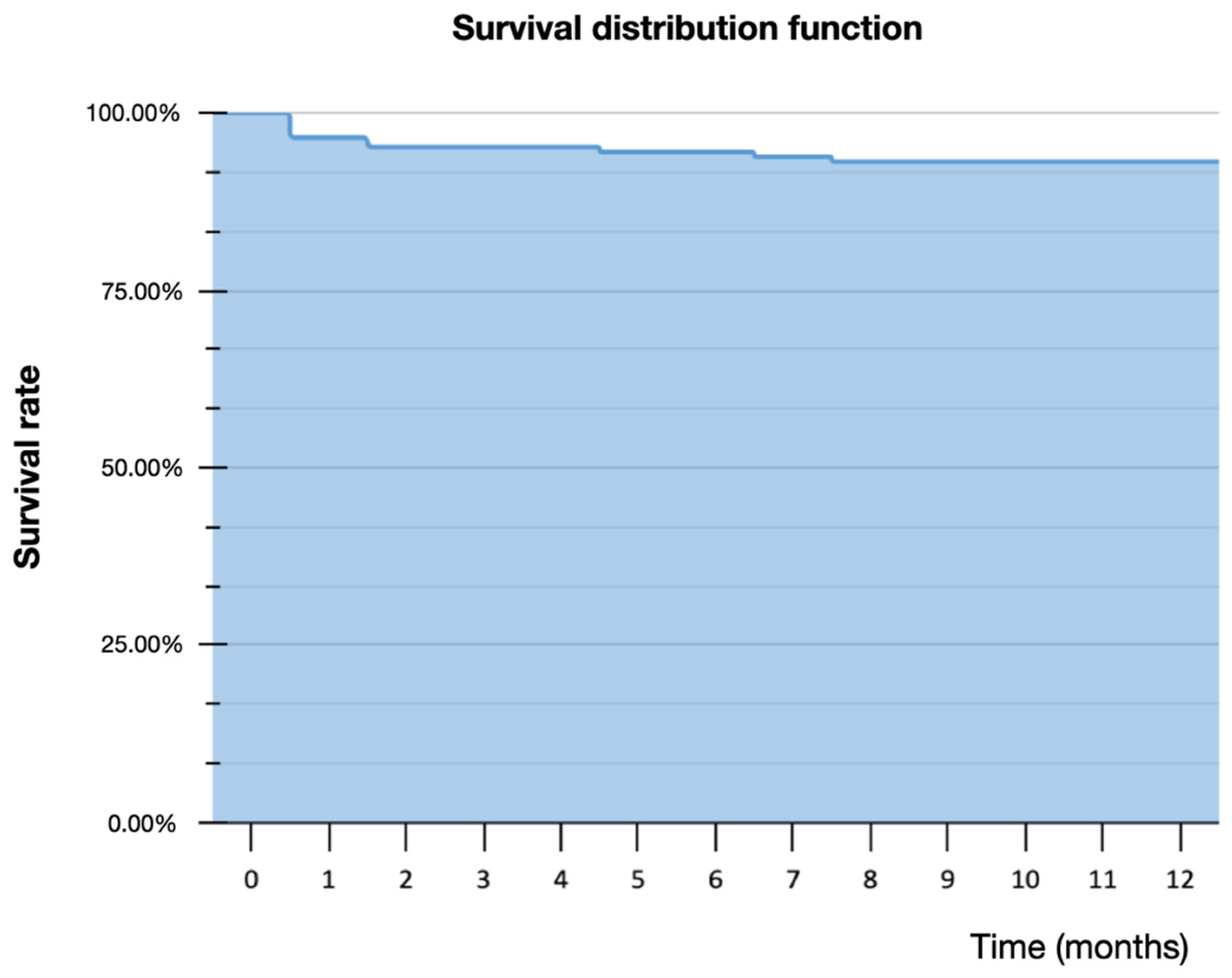
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Schulte, W.; Heimke, G. The Tübinger immediate implant. Quintessenz 1976, 27, 17–23. [Google Scholar]
- Lazzara, R. Immediate implant placement into extraction sites: Surgical and restorative advantages. Int. J. Periodontics Restor. Dent. 1989, 9, 332–343. [Google Scholar]
- Chen, S.; Wilson, T.J.; Hämmerle, C. Immediate or early placement of implants following tooth extraction: Review of biologic basis, clinical procedures, and outcomes. Int. J. Oral Maxillofac. Implant. 2004, 19, 12–25. [Google Scholar]
- Wagenberg, B.; Froum, S. A retrospective study of 1925 consecutively placed immediate implants from 1988 to 2004. Int. J. Oral Maxillofac. Implant. 2006, 21, 70–80. [Google Scholar]
- Schwartz-Arad, D.; Chaushu, G. The Ways and Wherefores of Immediate Placement of Implants into Fresh Extraction Sites: A Literature Review. J. Periodontol. 1997, 68, 915–923. [Google Scholar] [CrossRef] [PubMed]
- Smith, R.B.; Tarnow, D.P.; Sarnachiaro, G. Immediate Placement of Dental Implants in Molar Extraction Sockets: An 11-Year Retrospective Analysis. Compend. Contin. Educ. Dent. 2019, 40, 166–170. [Google Scholar]
- Ketabi, M.; Deporter, D.; Atenafu, E.G. A Systematic Review of Outcomes Following Immediate Molar Implant Placement Based on Recently Published Studies. Clin. Implant. Dent. Relat. Res. 2016, 18, 1084–1094. [Google Scholar] [CrossRef] [PubMed]
- Ragucci, G.M.; Elnayef, B.; Criado-Cámara, E.; Del Amo, F.S.-L.; Hernández-Alfaro, F. Immediate implant placement in molar extraction sockets: A systematic review and meta-analysis. Int. J. Implant. Dent. 2020, 6, 40. [Google Scholar] [CrossRef]
- Schwartz-Arad, D.; Grossman, Y.; Chaushu, G. The Clinical Effectiveness of Implants Placed Immediately into Fresh Extraction Sites of Molar Teeth. J. Periodontol. 2000, 71, 839–844. [Google Scholar] [CrossRef]
- Fugazzotto, P.A. Implant Placement at the Time of Mandibular Molar Extraction: Description of Technique and Preliminary Results of 341 Cases. J. Periodontol. 2008, 79, 737–747. [Google Scholar] [CrossRef]
- Walker, L.R.; Morris, G.A.; Novotny, P.J. Implant insertional torque values predict outcomes. J. Oral Maxillofac. Surg. 2011, 69, 1344–1349. [Google Scholar] [CrossRef]
- Bavetta, G.; Bavetta, G.; Randazzo, V.; Cavataio, A.; Paderni, C.; Grassia, V.; Dipalma, G.; Gargiulo Isacco, C.; Scarano, A.; De Vito, D.; et al. A retrospective study on insertion torque and implant stability quotient (isq) as stability parameters for immediate loading of implants in fresh extraction sockets. Biomed. Res. Int. 2019, 2019, 9720419. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Atieh, M.A.; Payne, A.G.T.; Duncan, W.J.; de Silva, R.K.; Cullinan, M.P. Immediate placement or immediate restoration/loading of single implants for molar tooth replacement: A systematic review and meta-analysis. Int. J. Oral Maxillofac. Implant. 2010, 25, 401–415. [Google Scholar]
- Smith, R.B.; Tarnow, D.P. Classification of Molar Extraction Sites for Immediate Dental Implant Placement: Technical Note. Int. J. Oral Maxillofac. Implant. 2013, 28, 911–916. [Google Scholar] [CrossRef] [Green Version]
- Marquezan, M.; Osório, A.; Sant’Anna, E.; Souza, M.M.; Maia, L. Does bone mineral density influence the primary stability of dental implants? A systematic review. Clin. Oral Implant. Res. 2012, 23, 767–774. [Google Scholar] [CrossRef]
- Farronato, D.; Manfredini, M.; Stocchero, M.; Caccia, M.; Azzi, L.; Farronato, M. Influence of Bone Quality, Drilling Protocol, Implant Diameter/Length on Primary Stability: An In Vitro Comparative Study on Insertion Torque and Resonance Frequency Analysis. J. Oral Implant. 2020, 46, 182–189. [Google Scholar] [CrossRef]
- Javed, F.; Ahmed, H.; Crespi, R.; Romanos, G. Role of primary stability for successful osseointegration of dental implants: Factors of influence and evaluation. Interv. Med. Appl. Sci. 2013, 5, 162–167. [Google Scholar] [CrossRef] [PubMed]
- Greenstein, G.; Cavallaro, J. Implant Insertion Torque: Its Role in Achieving Primary Stability of Restorable Dental Implants. Compend. Contin. Educ. Dent. 2017, 38, 88–95. [Google Scholar]
- Hattingh, A.; De Bruyn, H.; Vandeweghe, S. A retrospective study on ultra-wide diameter dental implants for immediate molar replacement. Clin. Implant. Dent. Relat. Res. 2019, 21, 879–887. [Google Scholar] [CrossRef]
- Hattingh, A.; Hommez, G.; De Bruyn, H.; Huyghe, M.; Vandeweghe, S. A prospective study on ultra-wide diameter dental implants for immediate molar replacement. Clin. Implant. Dent. Relat. Res. 2018, 20, 1009–1015. [Google Scholar] [CrossRef] [PubMed]
- Hattingh, A.; De Bruyn, H.; Ackermann, A.; Vandeweghe, S. Immediate Placement of Ultrawide-Diameter Implants in Molar Sockets: Description of a Recommended Technique. Int. J. Periodontics Restor. Dent. 2018, 38, 17–23. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huwais, S.; Meyer, E. A Novel Osseous Densification Approach in Implant Osteotomy Preparation to Increase Biomechanical Primary Stability, Bone Mineral Density, and Bone-to-Implant Contact. Int. J. Oral Maxillofac. Implant. 2017, 32, 27–36. [Google Scholar] [CrossRef] [PubMed]
- Trisi, P.; Berardini, M.; Falco, A.; Podaliri Vulpiani, M. New osseodensification implant site preparation method to increase bone density in low-density bone: In vivo evaluation in sheep. Implant. Dent. 2016, 25, 24–31. [Google Scholar] [CrossRef] [Green Version]
- Lahens, B.; Neiva, R.; Tovar, N.; Alifarag, A.M.; Jimbo, R.; Bonfante, E.A.; Bowers, M.M.; Cuppini, M.; Freitas, H.; Witek, L.; et al. Biomechanical and histologic basis of osseodensification drilling for endosteal implant placement in low density bone. An experimental study in sheep. J. Mech. Behav. Biomed. Mater. 2016, 63, 56–65. [Google Scholar] [CrossRef] [PubMed]
- Alifarag, A.M.; Lopez, C.D.; Neiva, R.F.; Tovar, N.; Witek, L.; Coelho, P.G. Atemporal osseointegration: Early biomechanical stability through osseodensification. J. Orthop. Res. 2018, 36, 2516–2523. [Google Scholar] [CrossRef] [Green Version]
- Kold, S.; Bechtold, J.E.; Ding, M.; Chareancholvanich, K.; Rahbek, O.; Søballe, K. Compacted cancellous bone has a spring-back effect. Acta Orthop. Scand. 2003, 74, 591–595. [Google Scholar] [CrossRef]
- Lopez, C.D.; Alifarag, A.M.; Torroni, A.; Tovar, N.; Diaz-Siso, J.R.; Witek, L.; Rodriguez, E.D.; Coelho, P.G. Osseodensification for enhancement of spinal surgical hardware fixation. J. Mech. Behav. Biomed. Mater. 2017, 69, 275–281. [Google Scholar] [CrossRef] [Green Version]
- Bergamo, E.T.; Zahoui, A.; Barrera, R.B.; Huwais, S.; Coelho, P.G.; Karateew, E.D.; Bonfante, E.A. Osseodensification effect on implants primary and secondary stability: Multicenter controlled clinical trial. Clin. Implant. Dent. Relat. Res. 2021, 23, 317–328. [Google Scholar] [CrossRef]
- Koutouzis, T.; Huwais, S.; Hasan, F.; Trahan, W.; Waldrop, T.; Neiva, R. Alveolar Ridge Expansion by Osseodensification-Mediated Plastic Deformation and Compaction Autografting: A Multicenter Retrospective Study. Implant. Dent. 2019, 28, 349–355. [Google Scholar] [CrossRef] [Green Version]
- Machado, R.; da Gama, C.; Batista, S.; Rizzo, D.; Valiense, H.; Moreira, R. Tomographic and clinical findings, pre-, trans-, and post-operative, of osseodensification in immediate loading. Int. J. Growth Factors Stem Cells Dent. 2018, 1, 101–105. [Google Scholar] [CrossRef]
- Neiva, R.; Tanello, B.; Duarte, W.; Coelho, P.G.; Witek, L.; Silva, F. Effects of osseodensification on Astra TX and EV implant systems. Clin. Oral Implant. Res. 2018, 29, 444. [Google Scholar] [CrossRef] [Green Version]
- Tanello, B.; Neiva, R.; Huwais, S. Osseodensification Protocols for Enhancement of Primary and Secondary Implant Stability- A Retrospective 5-year follow-up Multi-center Study. Clin. Oral Implant. Res. 2019, 30, 414. [Google Scholar] [CrossRef]
- Gaspar, J.; Esteves, T.; Gaspar, R.; Rua, J.; João Mendes, J. Osseodensification for implant site preparation in the maxilla- a prospective study of 97 implants. Clin. Oral Implants Res. 2018, 29, 163. [Google Scholar] [CrossRef] [Green Version]
- Kumar, B.; Narayan, V. Minimally invasive crestal approach sinus floor elevation using Densah burs, and Hydraulic lift utilising putty graft in cartridge delivery. Clin. Oral Implants Res. 2017, 28, 203. [Google Scholar]
- Huwais, S.; Mazor, Z.; Ioannou, A.; Gluckman, H.; Neiva, R. A Multicenter Retrospective Clinical Study with Up-to-5-Year Follow-up Utilizing a Method that Enhances Bone Density and Allows for Transcrestal Sinus Augmentation Through Compaction Grafting. Int. J. Oral Maxillofac. Implant. 2018, 33, 1305–1311. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Lancet 2007, 370, 1453–1457. [Google Scholar] [CrossRef]
- Tarnow, D.P.; Chu, S. Human histologic verification of osseointegration of an immediate implant placed into a fresh extraction socket with excessive gap distance without primary flap closure, graft, or membrane: A case report. Int. J. Periodontics Restor. Dent. 2011, 31, 515–521. [Google Scholar]
- Tarnow, D.P.; Chu, S.J.; Salama, M.A.; Stappert, C.F.J.; Salama, H.; Garber, D.A.; Sarnachiaro, G.O.; Sarnachiaro, E.; Luis Gotta, S.; Saito, H. Flapless Postextraction Socket Implant Placement in the Esthetic Zone: Part 1. The Effect of Bone Grafting and/or Provisional Restoration on Facial-Palatal Ridge Dimensional Change—A Retrospective Cohort Study. Int. J. Periodontics Restor. Dent. 2014, 34, 323–331. [Google Scholar] [CrossRef]
- Padhye, N.M.; Shirsekar, V.; Bhatavadekar, N.B. Three-Dimensional Alveolar Bone Assessment of Mandibular First Molars with Implications for Immediate Implant Placement. Int. J. Periodontics Restor. Dent. 2020, 40, e163–e167. [Google Scholar] [CrossRef]
- Hayacibara, R.M.; Gonçalves, C.S.; Garcez-Filho, J.; Magro-Filho, O.; Esper, H.; Hayacibara, M. The success rate of immediate implant placement of mandibular molars: A clinical and radiographic retrospective evaluation between 2 and 8 years. Clin. Oral Implant. Res. 2013, 24, 806–811. [Google Scholar] [CrossRef]
- Peñarrocha-Oltra, D.; Demarchi, C.; Maestre-Ferrín, L.; Peñarrocha-Diago, M.; Peñarrocha-Diago, M. Comparison of immediate and delayed implants in the maxillary molar region: A retrospective study of 123 implants. Int. J. Oral Maxillofac. Implant. 2012, 27, 604–610. [Google Scholar]
- Smith, R.B.; Rawdin, S.B.; Kagan, V. Influence of Implant-Tooth Proximity on Incidence of Caries in Teeth Adjacent to Implants in Molar Sites: A Retrospective Radiographic Analysis of 300 Consecutive Implants. Compend. Contin. Educ. Dent. 2020, 41, e1–e5. [Google Scholar] [PubMed]


| Implant Company | Number of Implants Placed | Number of Implants Failed |
|---|---|---|
| Dentium | 35 | 1 |
| Adin | 35 | 3 |
| Megagen | 26 | 1 |
| Neobiotech | 21 | 2 |
| Zimmer | 14 | 3 |
| Paltop | 6 | 0 |
| IDI | 5 | 0 |
| Nobel Biocare | 3 | 0 |
| Total | 145 | 10 |
| ISQS | ISQR | ||
|---|---|---|---|
| Maxilla | Mean | 71.47 | 77.26 |
| N | 58 | 54 | |
| Std. Deviation | 4.231 | 3.004 | |
| Mandible | Mean | 73.72 | 79.88 |
| N | 87 | 84 | |
| Std. Deviation | 4.358 | 3.730 | |
| Total | Mean | 72.82 | 78.86 |
| N | 145 | 138 | |
| Std. Deviation | 4.434 | 3.684 |
| Implant Company | Diameter | ITV | ISQ | Septum Pre | Septum Post | Timing of Failure |
|---|---|---|---|---|---|---|
| Neobiotech | 5 | 55 | 76 | 3.5 | 4.8 | After |
| Neobiotech | 5 | 35 | 65 | 3.4 | 4.8 | Before |
| Dentium | 5 | 40 | 68 | 2.8 | 4.5 | Before |
| Zimmer | 5.2 | 20 | 63 | 5 | 5.5 | Before |
| Zimmer | 5 | 20 | 62 | 4 | 5.5 | Before |
| Zimmer | 4.7 | 30 | 60 | 2.5 | 4.5 | After |
| Megagen | 5.0 | 30 | 70 | 3.5 | 4.8 | After |
| Adin | 4.3 | 50 | 75 | 3 | 4.5 | Before |
| Adin | 5 | 45 | 70 | 3 | 4.5 | Before |
| Adin | 4.3 | 50 | 74 | 2.5 | 3.8 | Before |
| Mean | 4.85 | 37.5 | 68.3 | 3.32 | 4.7 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bleyan, S.; Gaspar, J.; Huwais, S.; Schwimer, C.; Mazor, Z.; Mendes, J.J.; Neiva, R. Molar Septum Expansion with Osseodensification for Immediate Implant Placement, Retrospective Multicenter Study with Up-to-5-Year Follow-Up, Introducing a New Molar Socket Classification. J. Funct. Biomater. 2021, 12, 66. https://doi.org/10.3390/jfb12040066
Bleyan S, Gaspar J, Huwais S, Schwimer C, Mazor Z, Mendes JJ, Neiva R. Molar Septum Expansion with Osseodensification for Immediate Implant Placement, Retrospective Multicenter Study with Up-to-5-Year Follow-Up, Introducing a New Molar Socket Classification. Journal of Functional Biomaterials. 2021; 12(4):66. https://doi.org/10.3390/jfb12040066
Chicago/Turabian StyleBleyan, Samvel, João Gaspar, Salah Huwais, Charles Schwimer, Ziv Mazor, José João Mendes, and Rodrigo Neiva. 2021. "Molar Septum Expansion with Osseodensification for Immediate Implant Placement, Retrospective Multicenter Study with Up-to-5-Year Follow-Up, Introducing a New Molar Socket Classification" Journal of Functional Biomaterials 12, no. 4: 66. https://doi.org/10.3390/jfb12040066
APA StyleBleyan, S., Gaspar, J., Huwais, S., Schwimer, C., Mazor, Z., Mendes, J. J., & Neiva, R. (2021). Molar Septum Expansion with Osseodensification for Immediate Implant Placement, Retrospective Multicenter Study with Up-to-5-Year Follow-Up, Introducing a New Molar Socket Classification. Journal of Functional Biomaterials, 12(4), 66. https://doi.org/10.3390/jfb12040066







