Investigation of the Global Fear Associated with COVID-19 Using Subjectivity Analysis and Deep Learning
Abstract
1. Introduction
1.1. Overview of COVID-19 and Its Effect on Humans
1.2. An Overview of the Fear Related to COVID-19 on a Global Scale
2. Literature Review
2.1. Review of Recent Works Based on Machine Learning Algorithms and Their Applications
2.2. Review of Recent Works Based on Data Analysis and Content Analysis
2.3. Review of Recent Works Based on Subjectivity Analysis
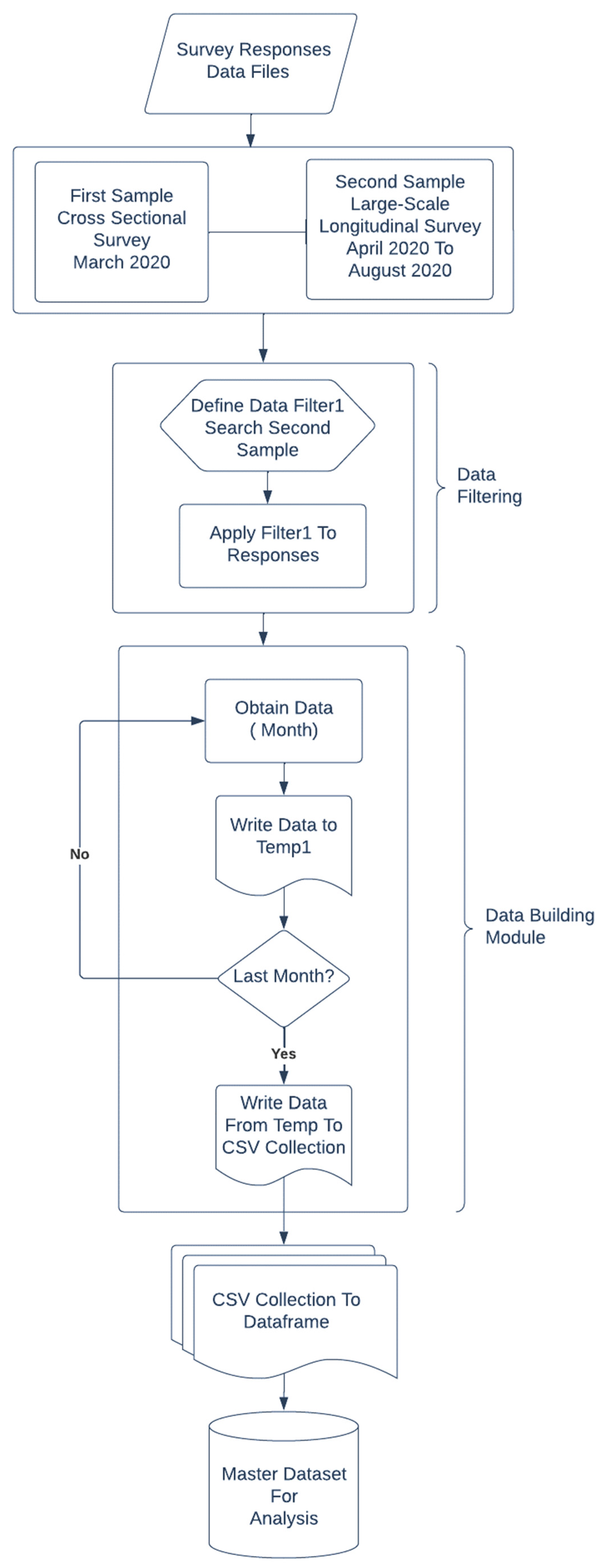
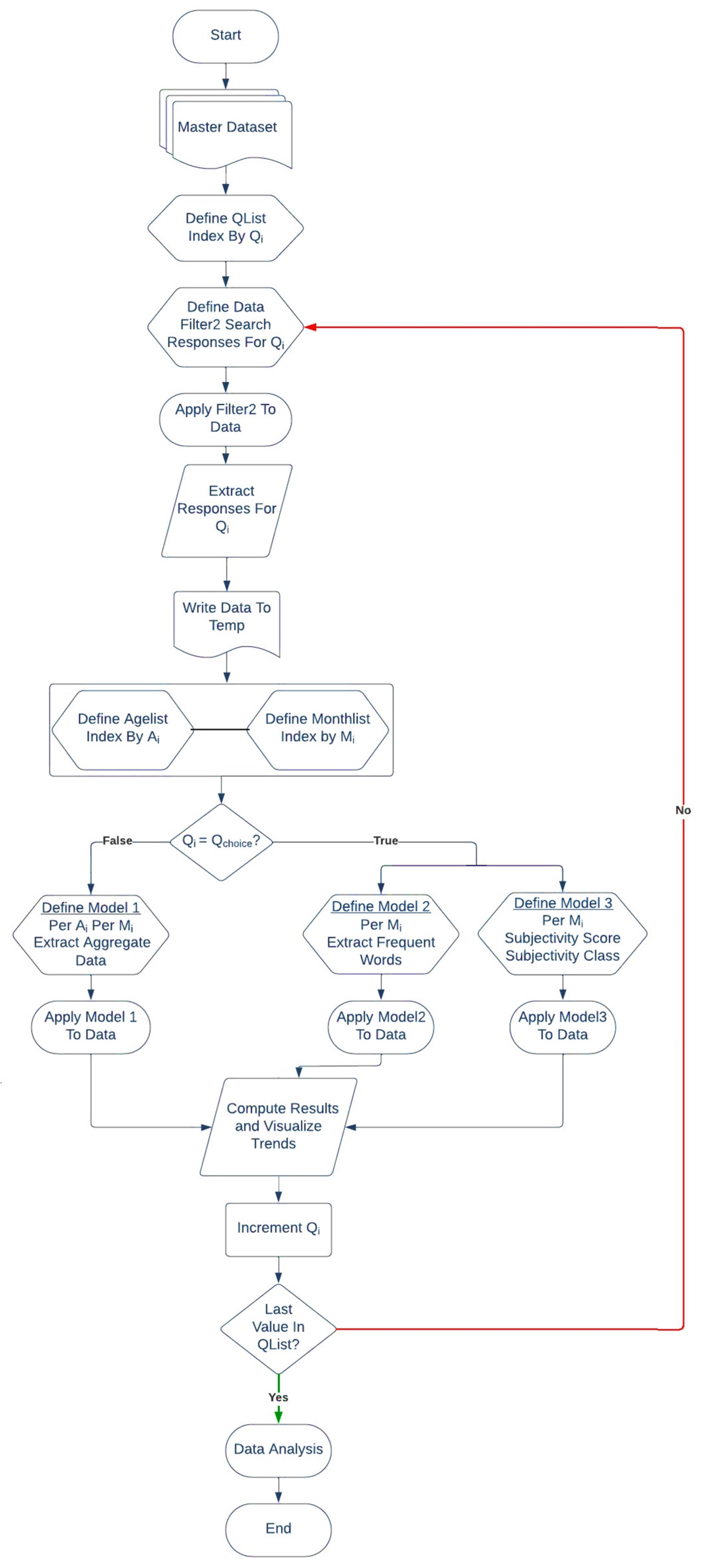
3. Methodology
| Algorithm 1: Subjectivity Analysis of responses indicating the biggest concern about COVID-19 |
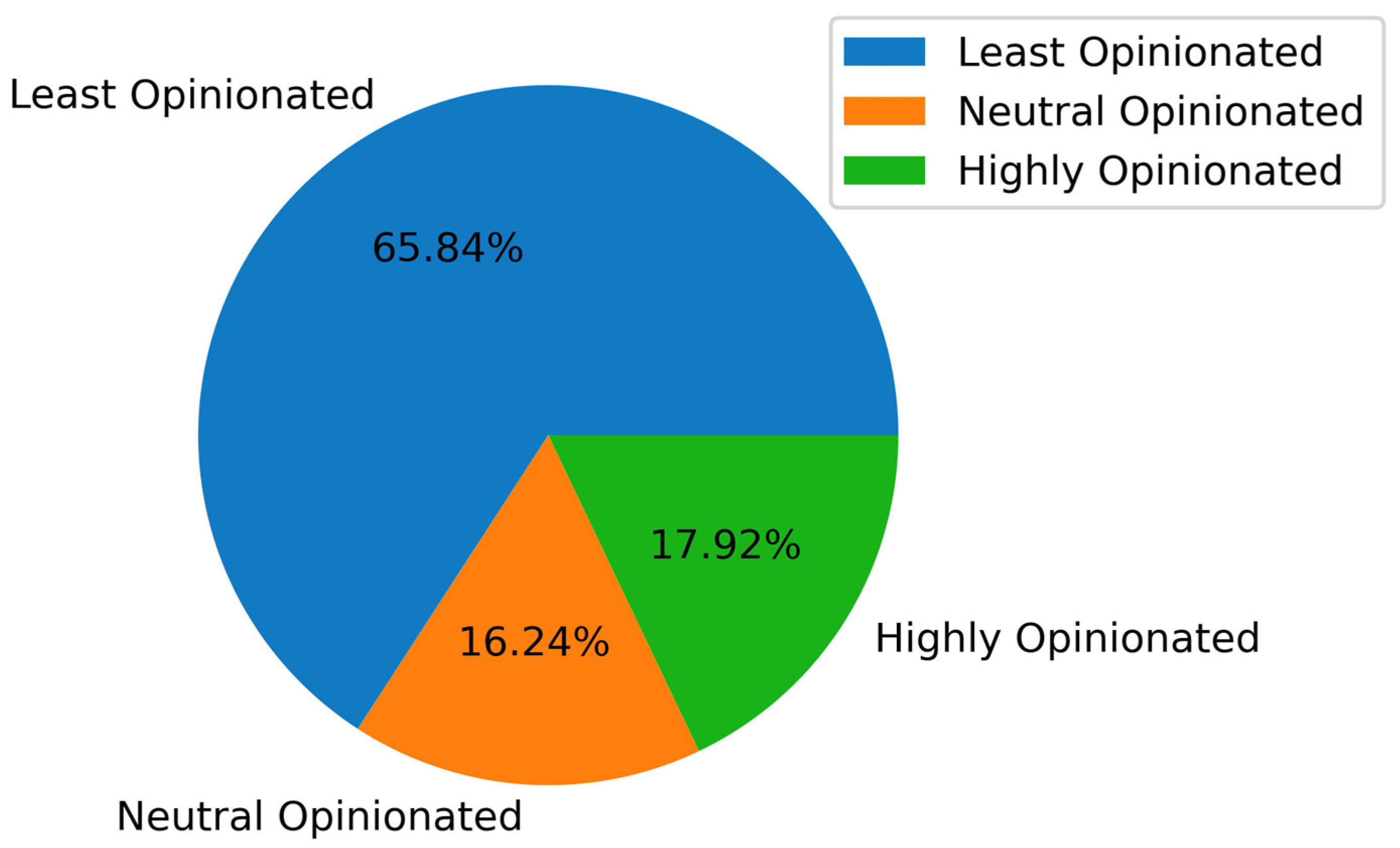
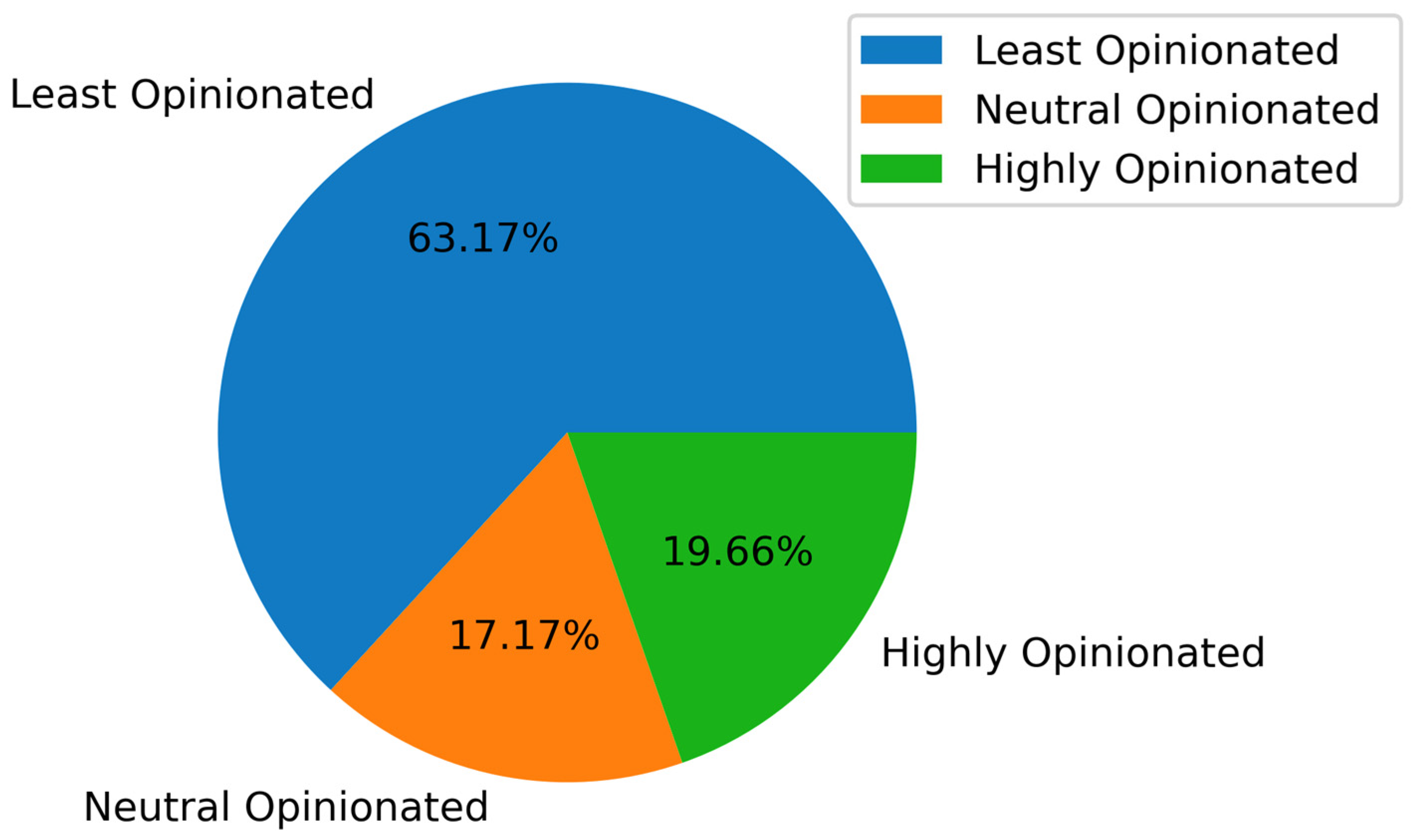
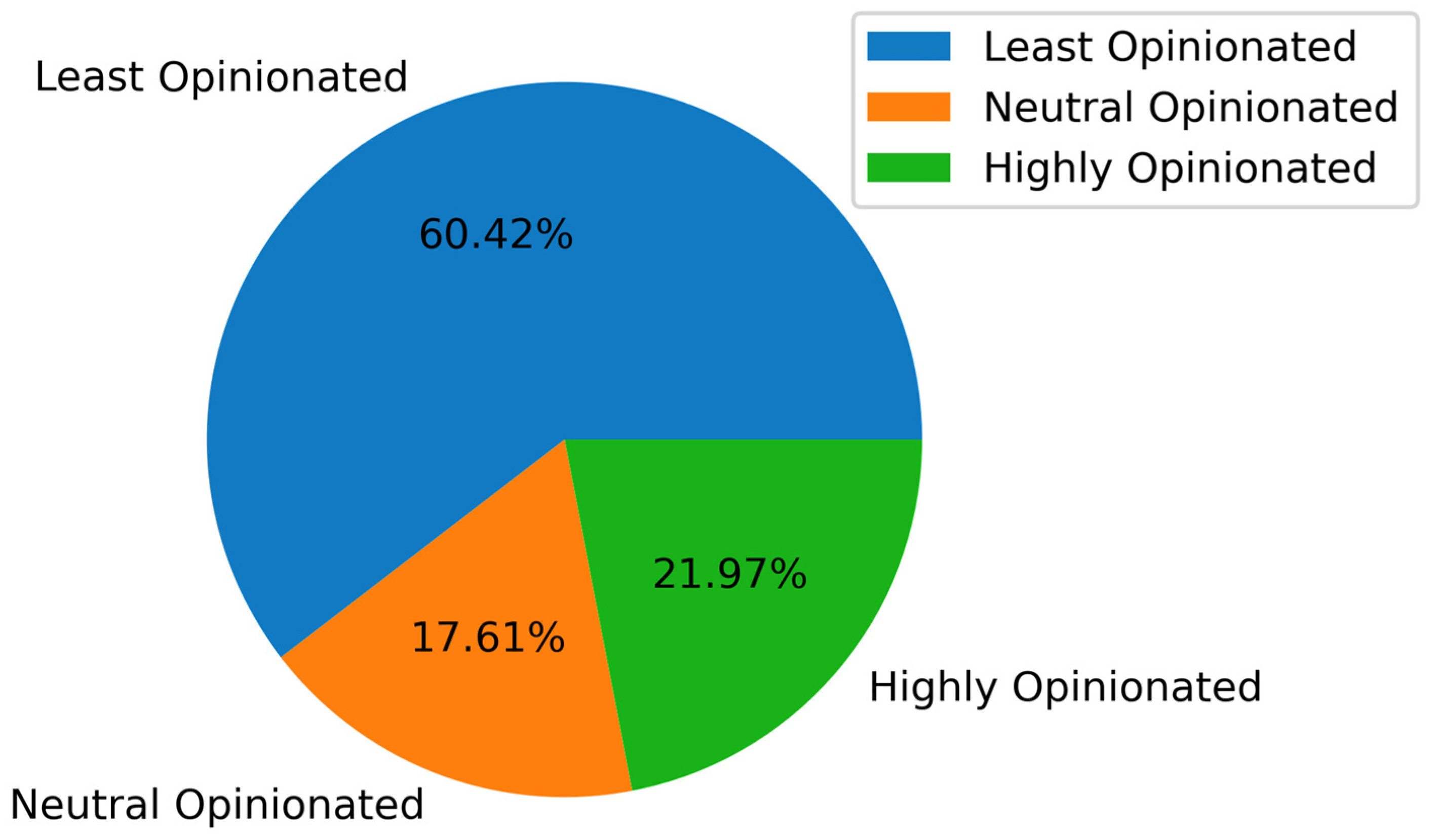
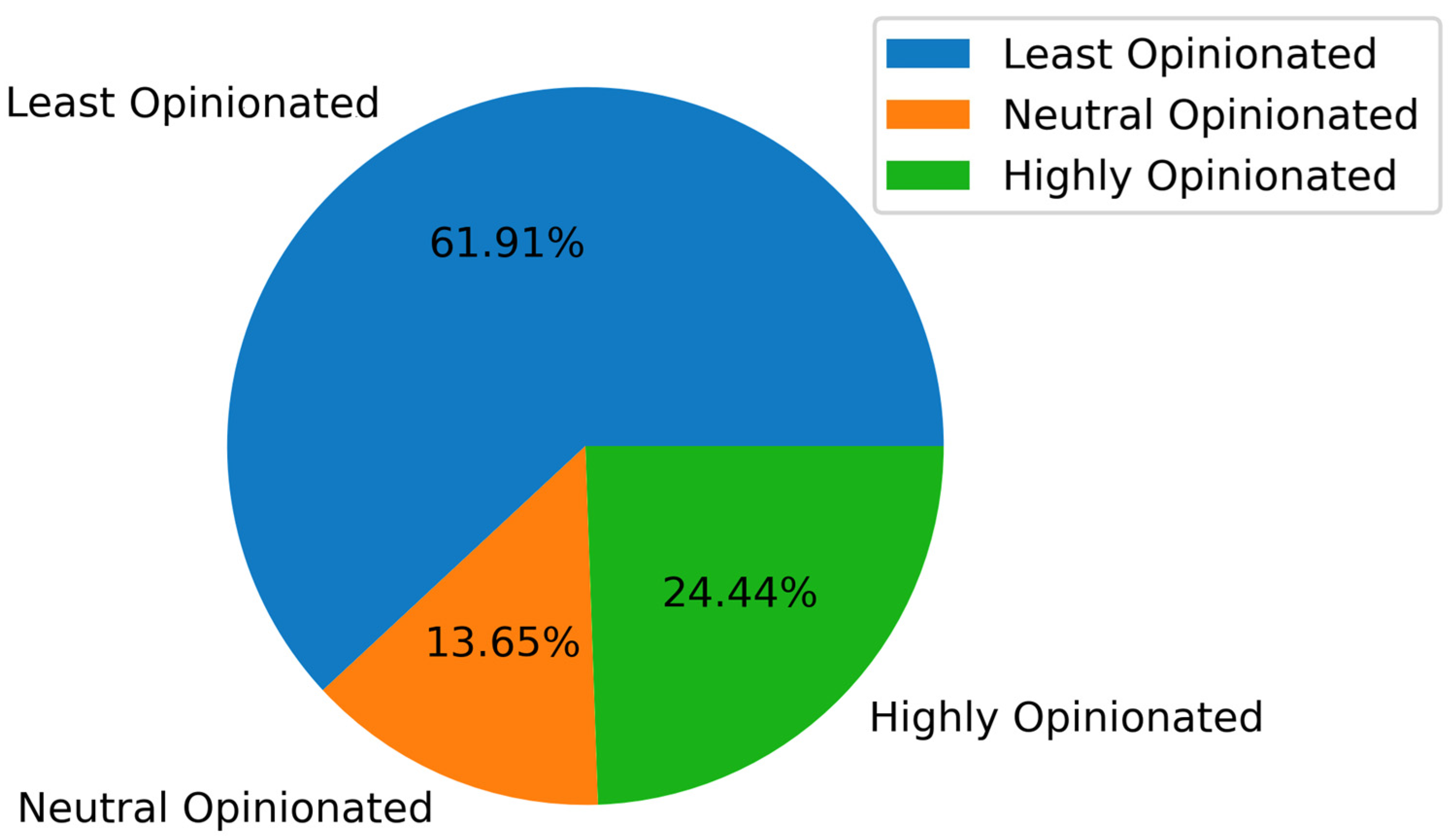
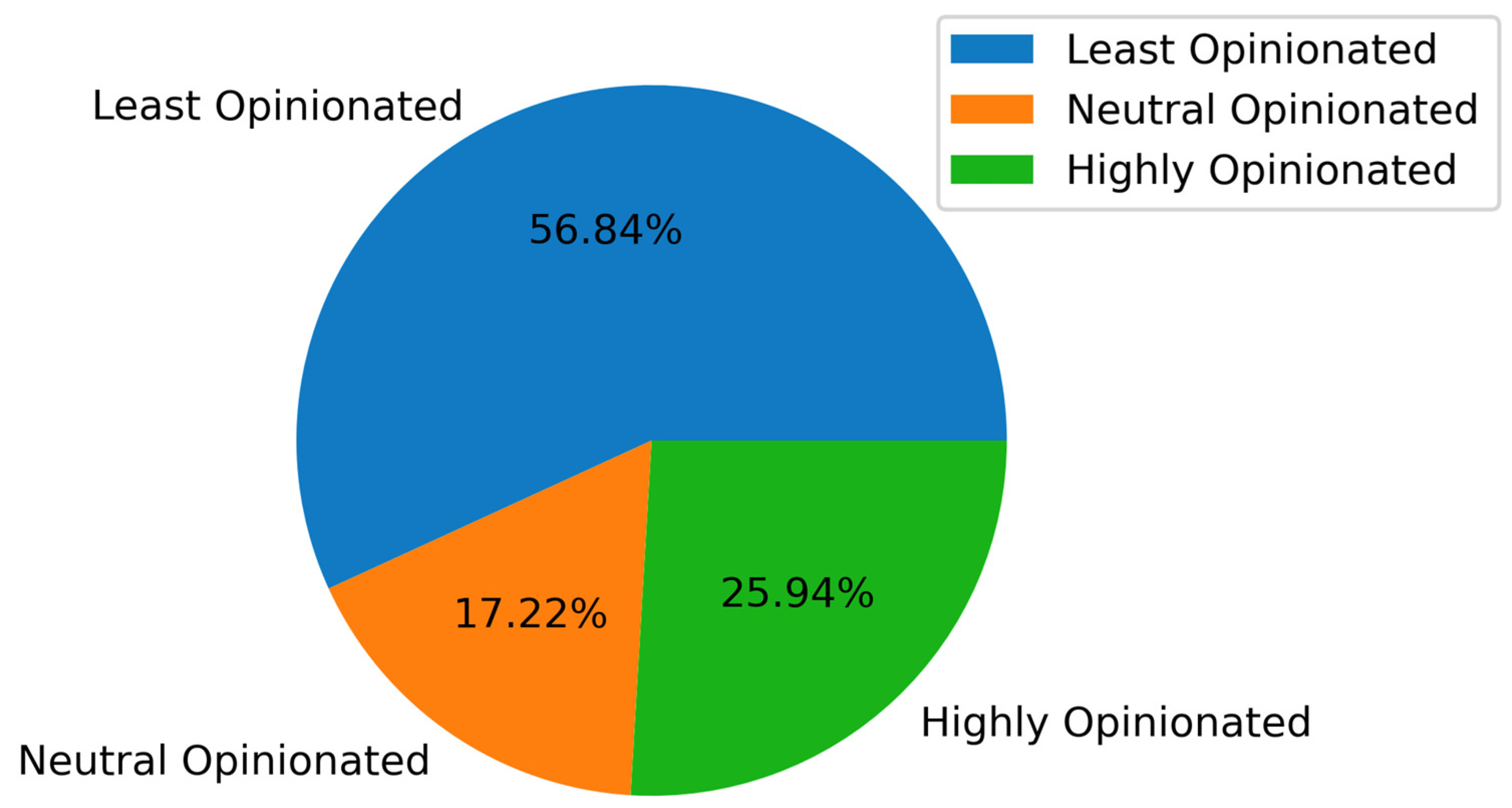
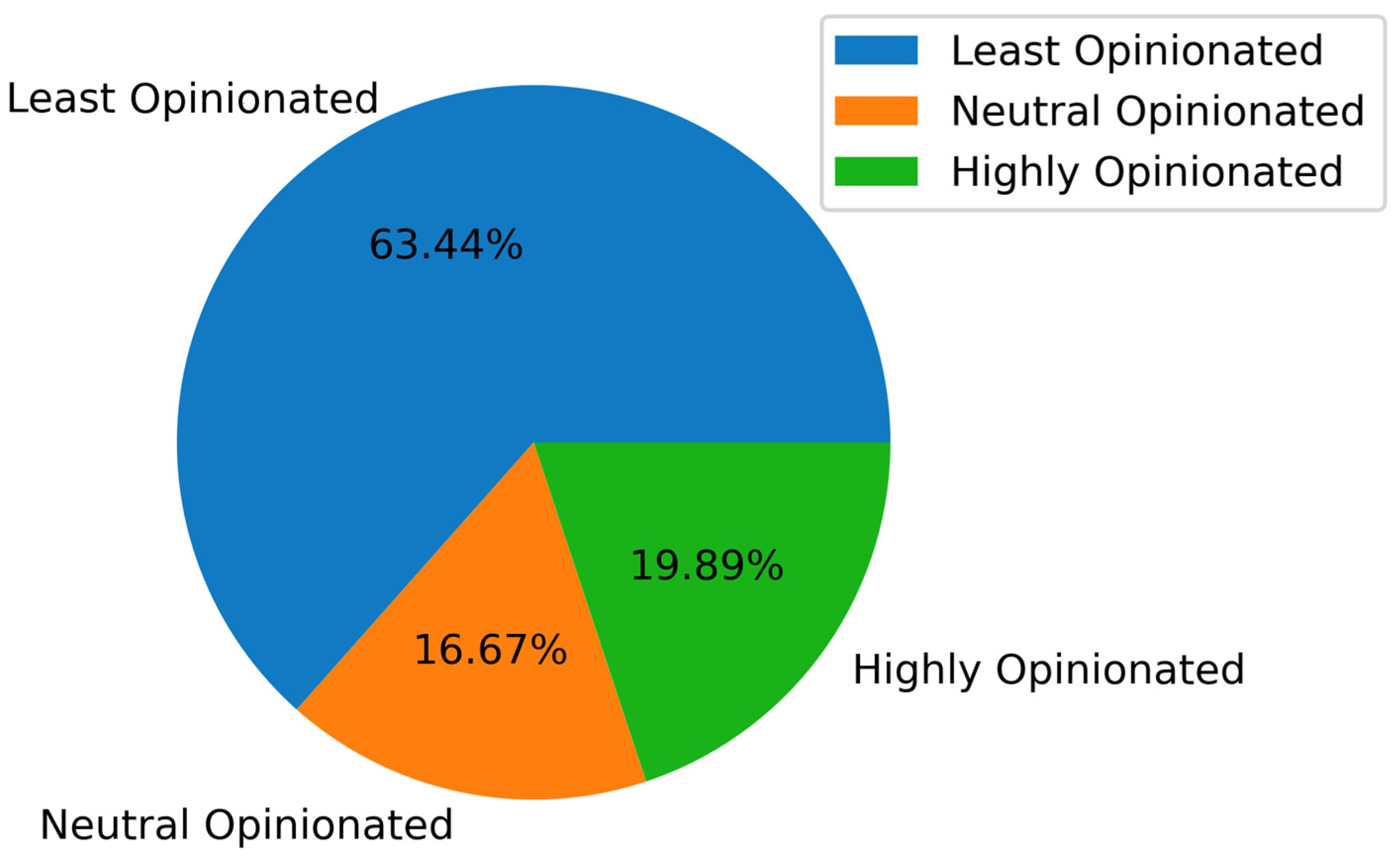
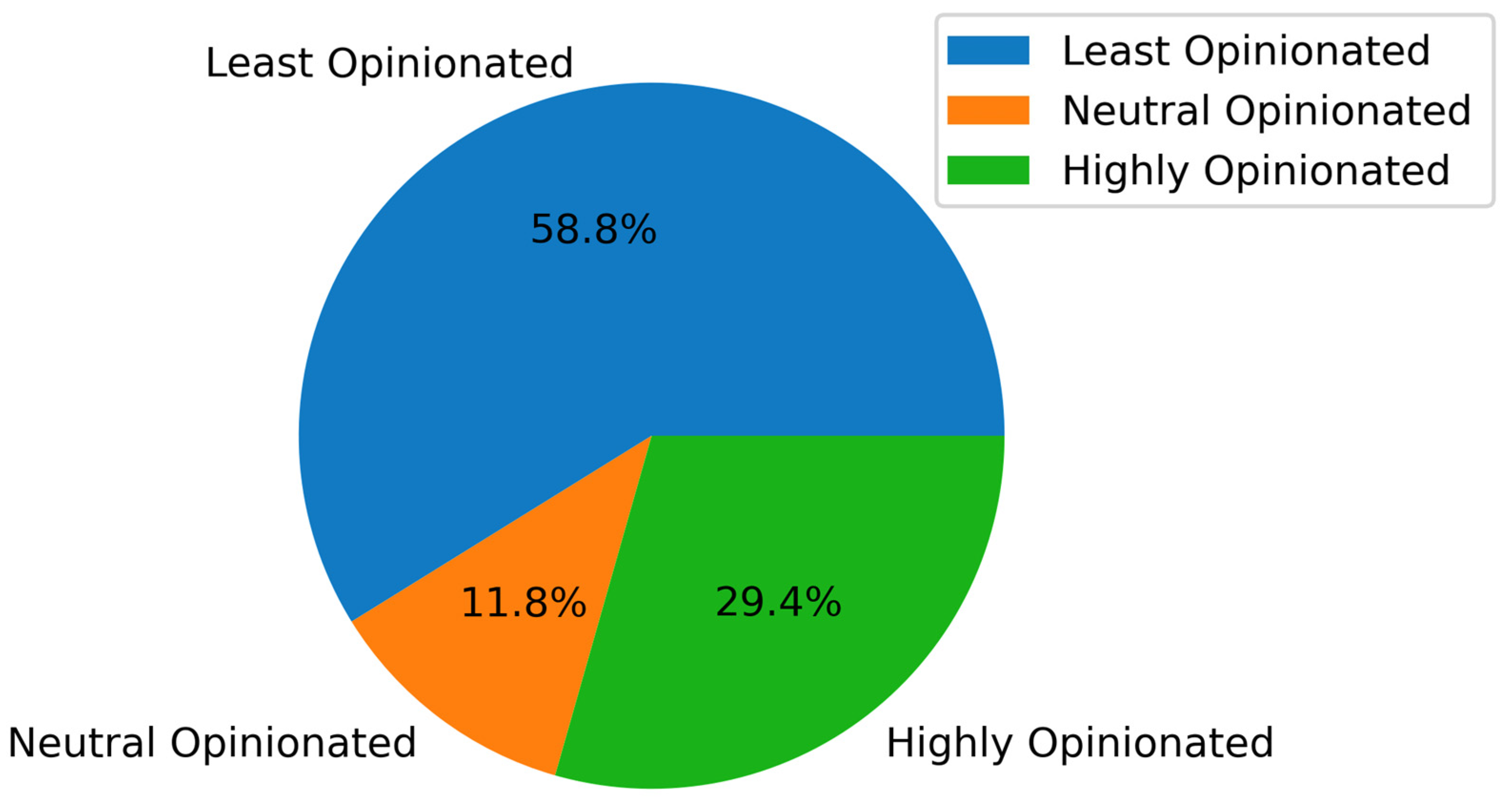
| Input: Master Dataset Output: Pie Charts and a Line Graph to represent the variation of Subjectivity per Age Group Local variables: words, corpus, corpus2, corpus3, Ai, Mi def DataPreprocessing(data) for each record in response do: record = replace non-alphabetic characters with space record = remove URLs, hashtags, and user mentions, from the dataset using RegEx record = remove digits record.lowercase() split record to words ps = porterstemmer all_stopwords = list of English stopwords record = perform stemming exclude those in the stopword list end of for loop end of function def CalculateSubjectivity(data) for each month in months do: data = getresponses (month) preprocessed_data = DataPreprocessing(data) for each item in the data do: testimonial = TextBlob(item) subjectivity = extract subjectivity score from testimonial corpus3 ← append(subjectivity) if subjectivity is less than 0.4 then: subjectivity_class = least opinionated else if subjectivity is greater than 0.6 then: subjectivity_class = high opinionated else: subjectivity_class = neutral corpus2 ← append(subjectivity_class) end of for loop for each item in the data do: tmp ← append(month) tmp ← append(corpus) tmp ← append(corpus2[item]) tmp ← append(corpus3[item]) data ← append(tmp) end of for loop end of for loop end of function def SubjectivityAnalysis_PerAgeGroup(data) for each month in months do: for each row in the month do: index AgeList by <Ai> if age is <Ai> then: if subjectivity_class is least opinionated then: increment least_opinion_<Ai> by 1 else if subjectivity_class is neutral then: increment neutral_<Ai> by 1 else if subjectivity_class is highly opinionated then: increment highly_opinion_<Ai> by 1 end of for loop end of for loop fig: = pie charts with these values save fig as an image end of function def SubjectivityVariation_PerAgeGroup(data) for each month in months do: for each row in the month do: subj_score = numerical value from subjectivity_value age = numerical value for age group index AgeList by <Ai> if age is <Ai> then: total_month_scores_<Ai> ← add subj_score mean_month_scores_<Ai> ← avg(total_month_scores_<Ai>) end of for loop end of for loop fig: = line graph with these values save fig as an image end of function |
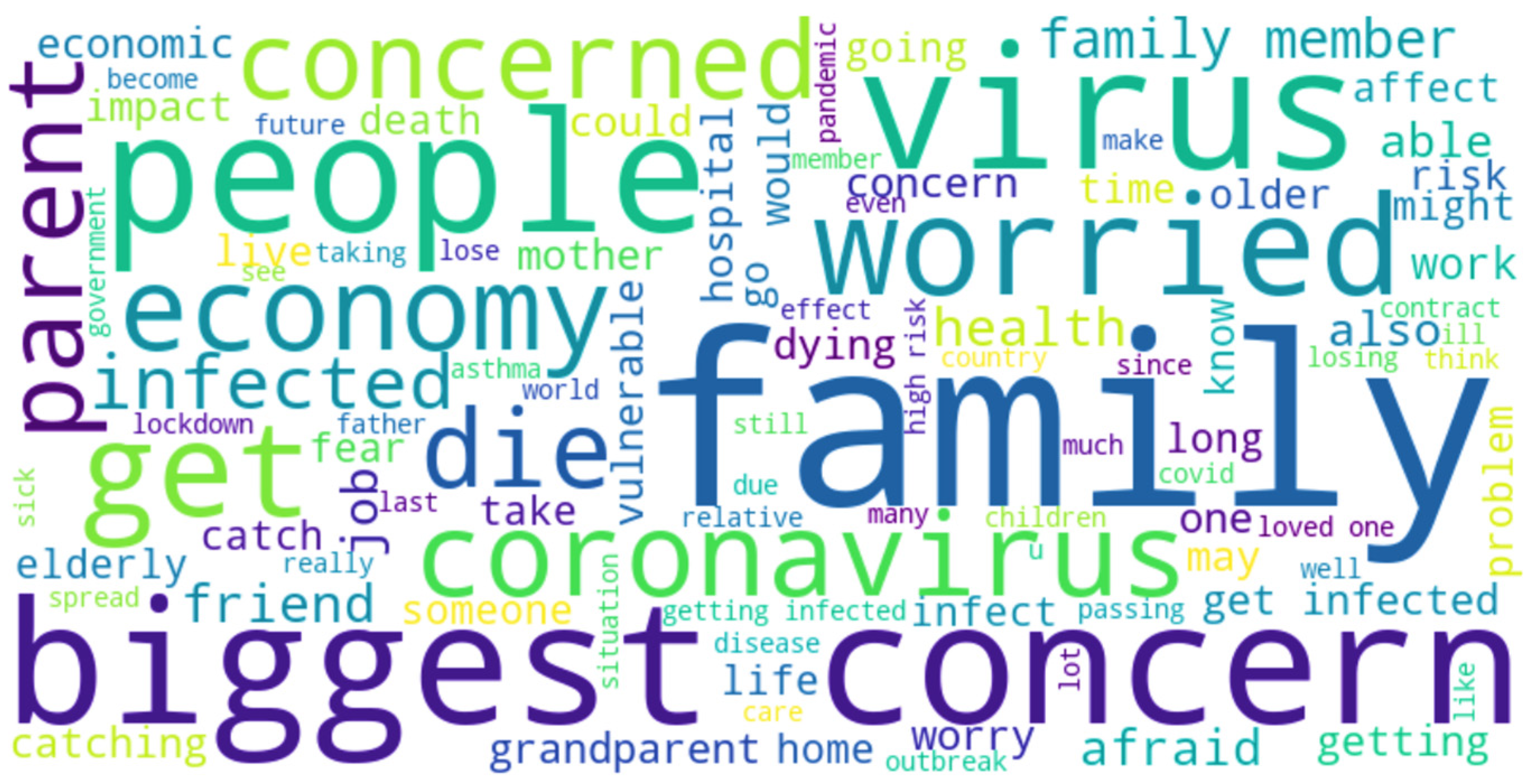
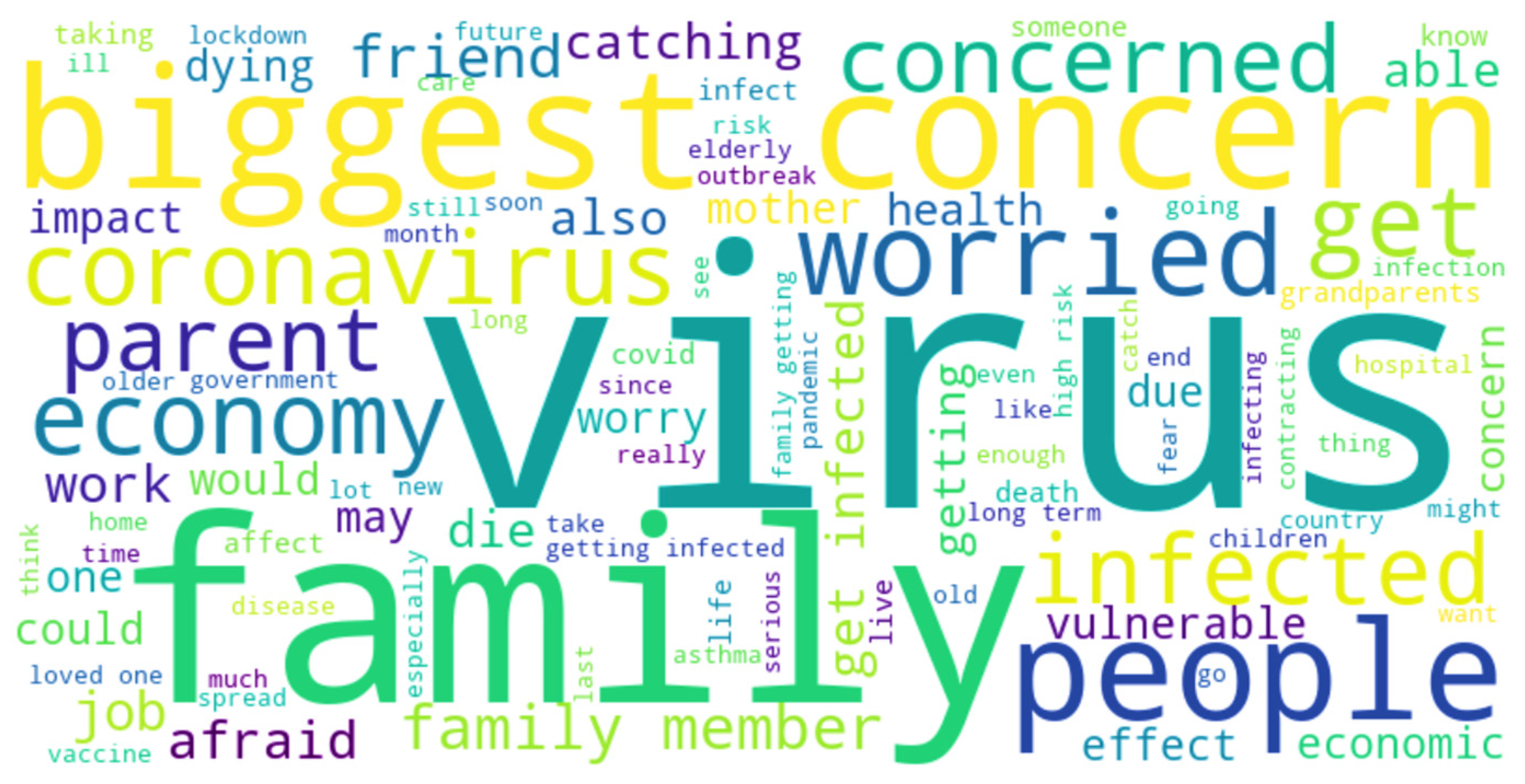
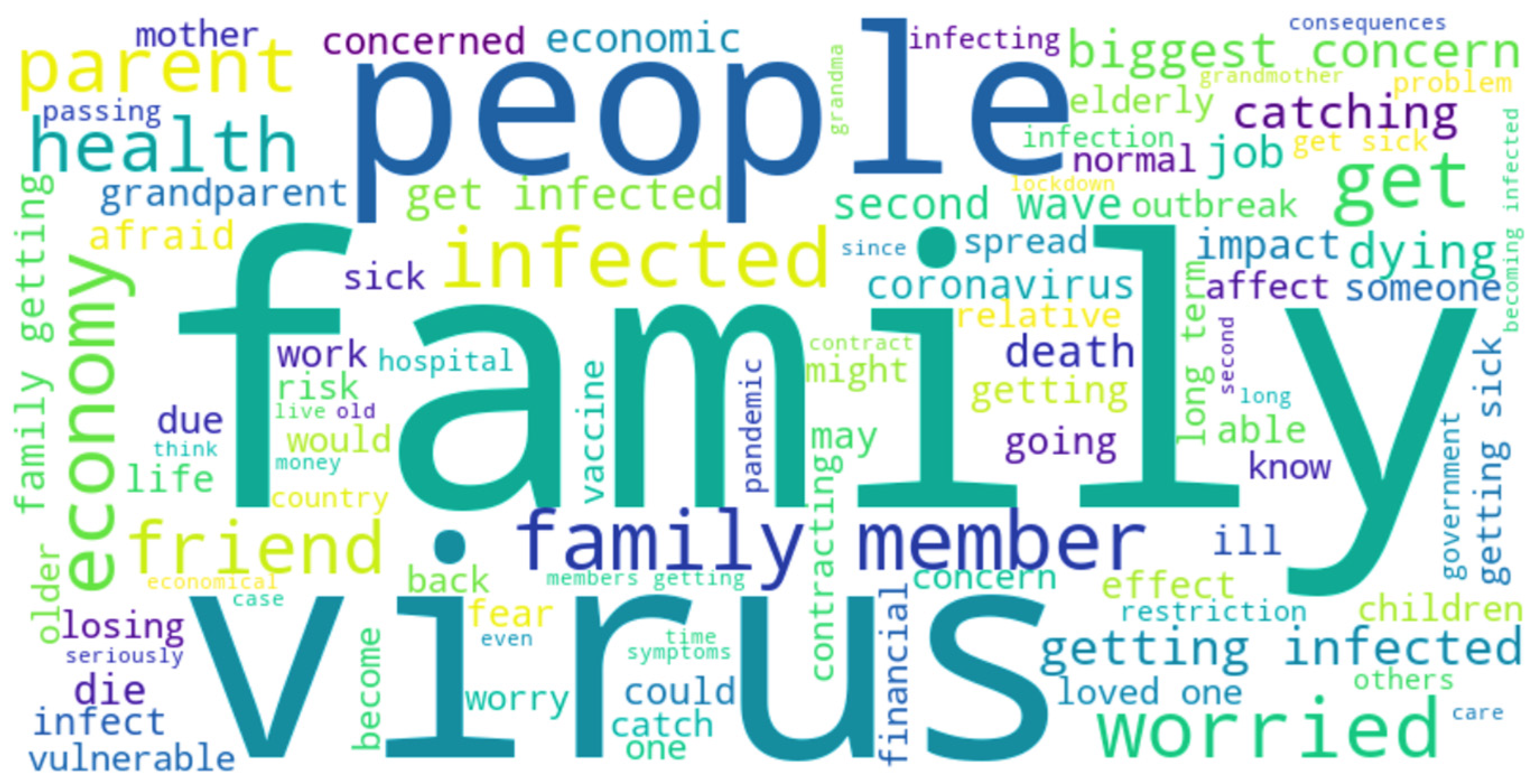
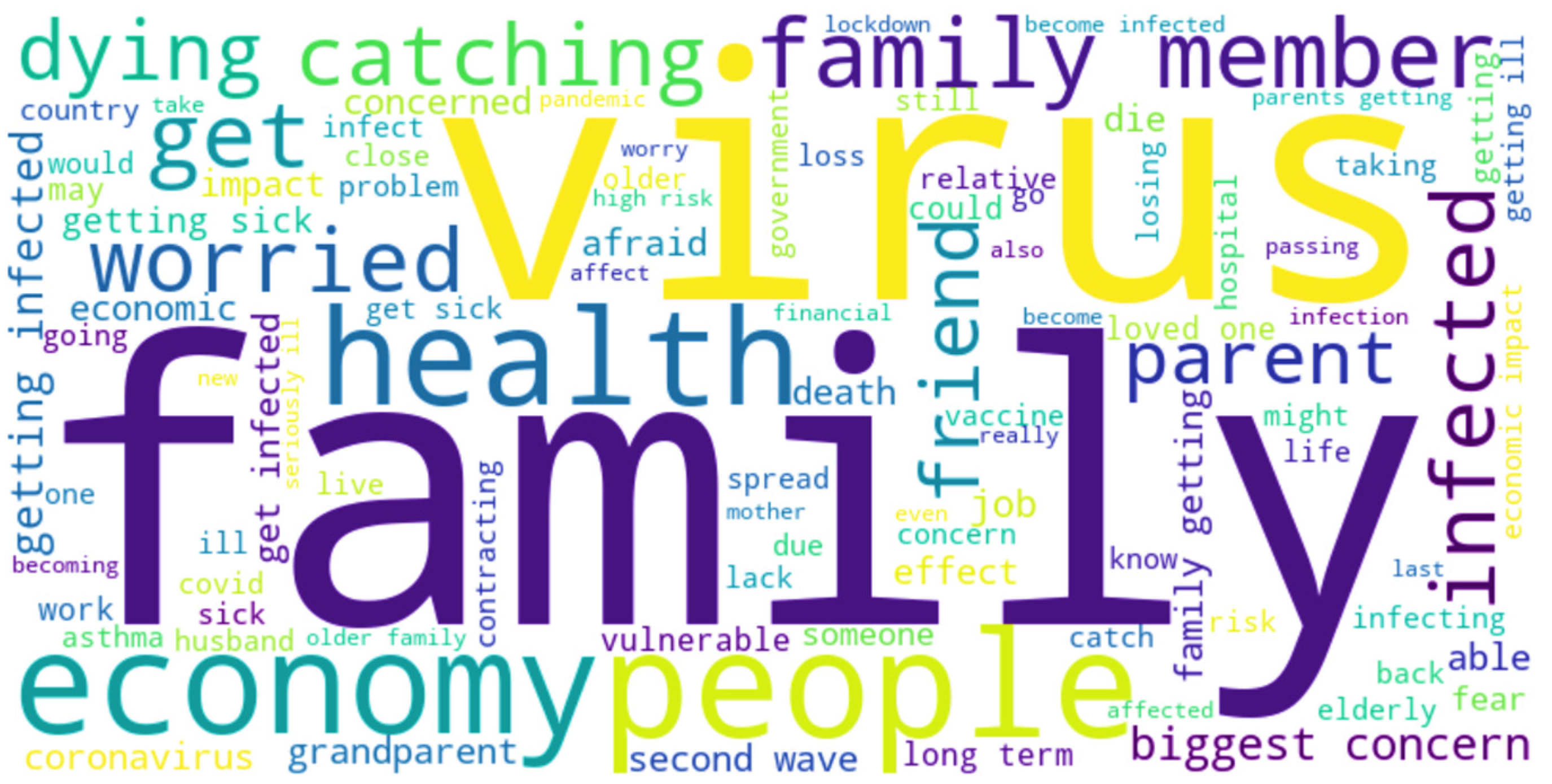
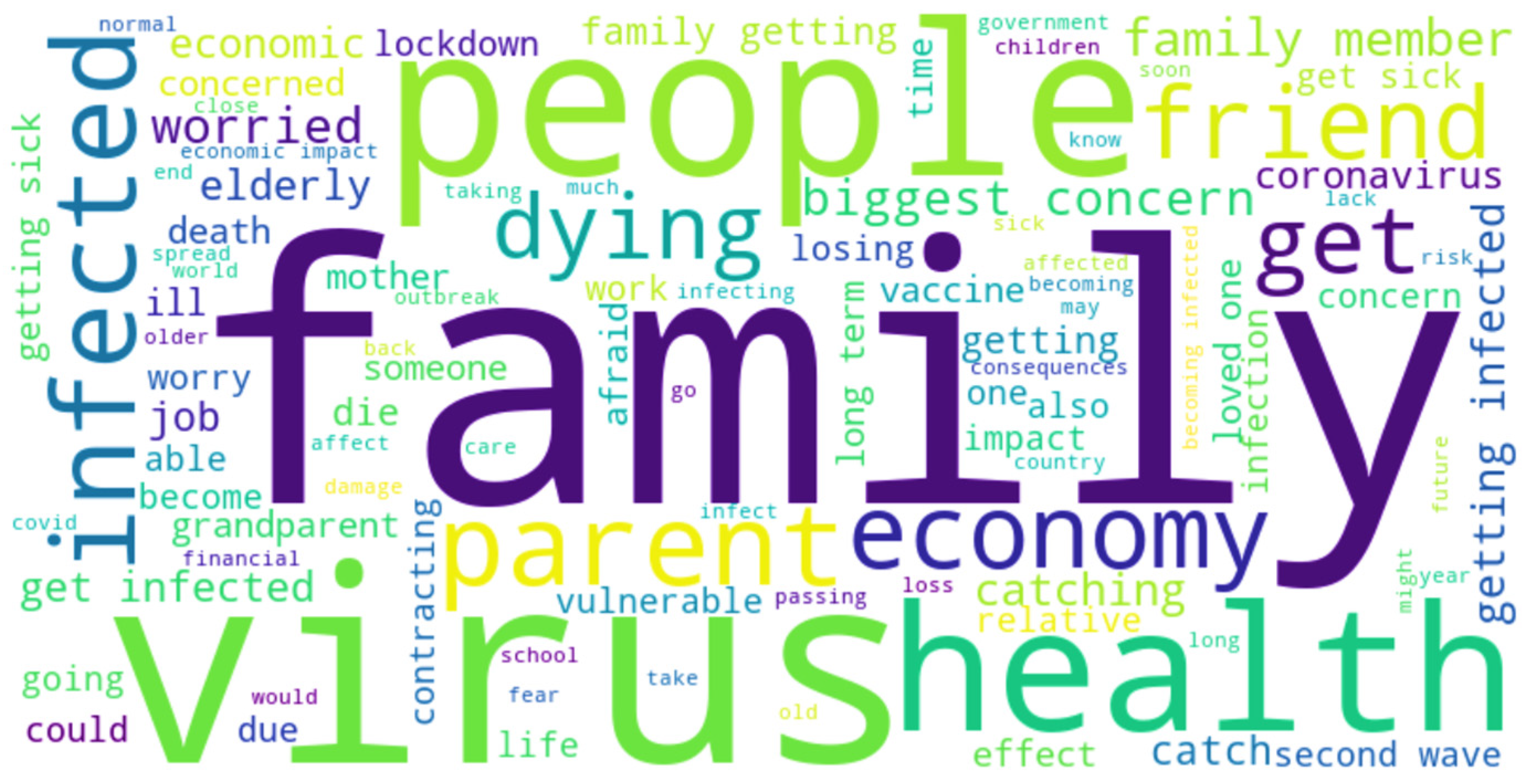
| Algorithm 2: Word Cloud of responses indicating the biggest concern about COVID-19 per month |
| Input: Master Dataset Output: One Word Cloud per month based on the responses Local variables: stopwords, new_stopwords import stopwords from nltk download stopwords from nltk stopwords = English stopwords list new_stopwords = added words add ‘new_stopwords’ to the ‘stopwords’ list for each val in column month of dataframe do: val = covert val to string tokens = split val into words for each index i in the range length of tokens do: tokens[i] ← convert the token to lowercase end of for loop join tokens with space, append data end of for loop wordcloud = instantiate wordcloud object with data generate wordcloud |
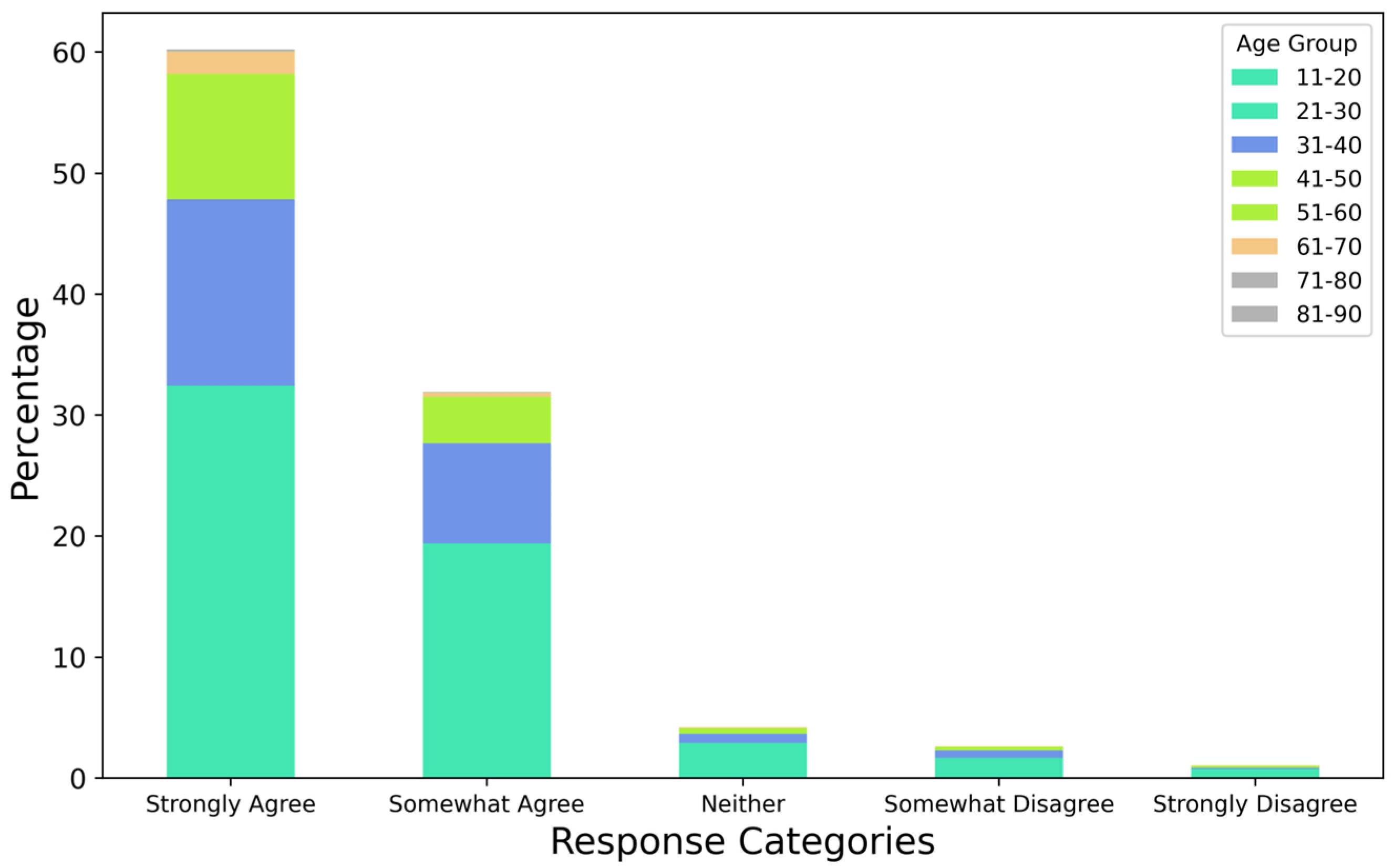
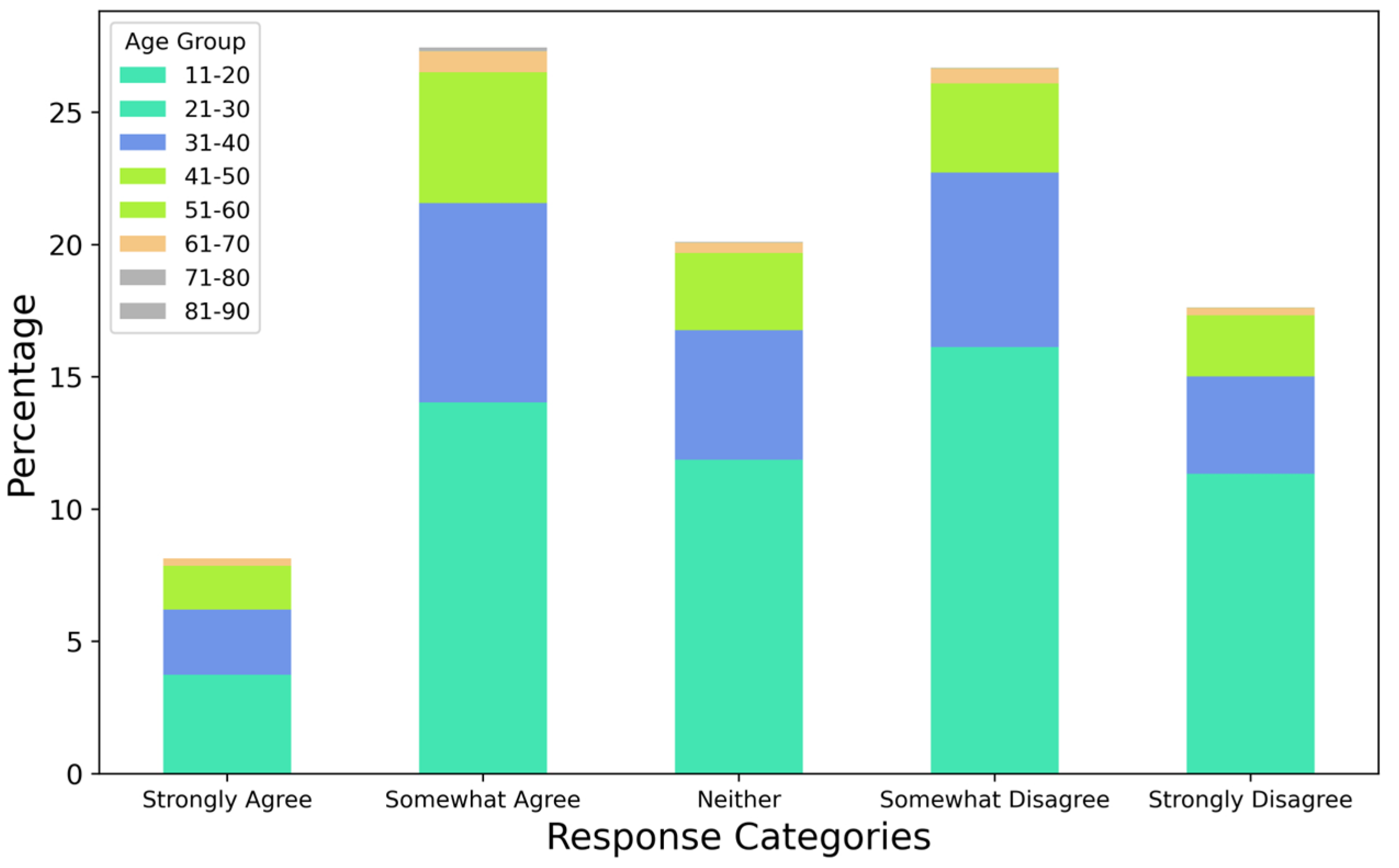
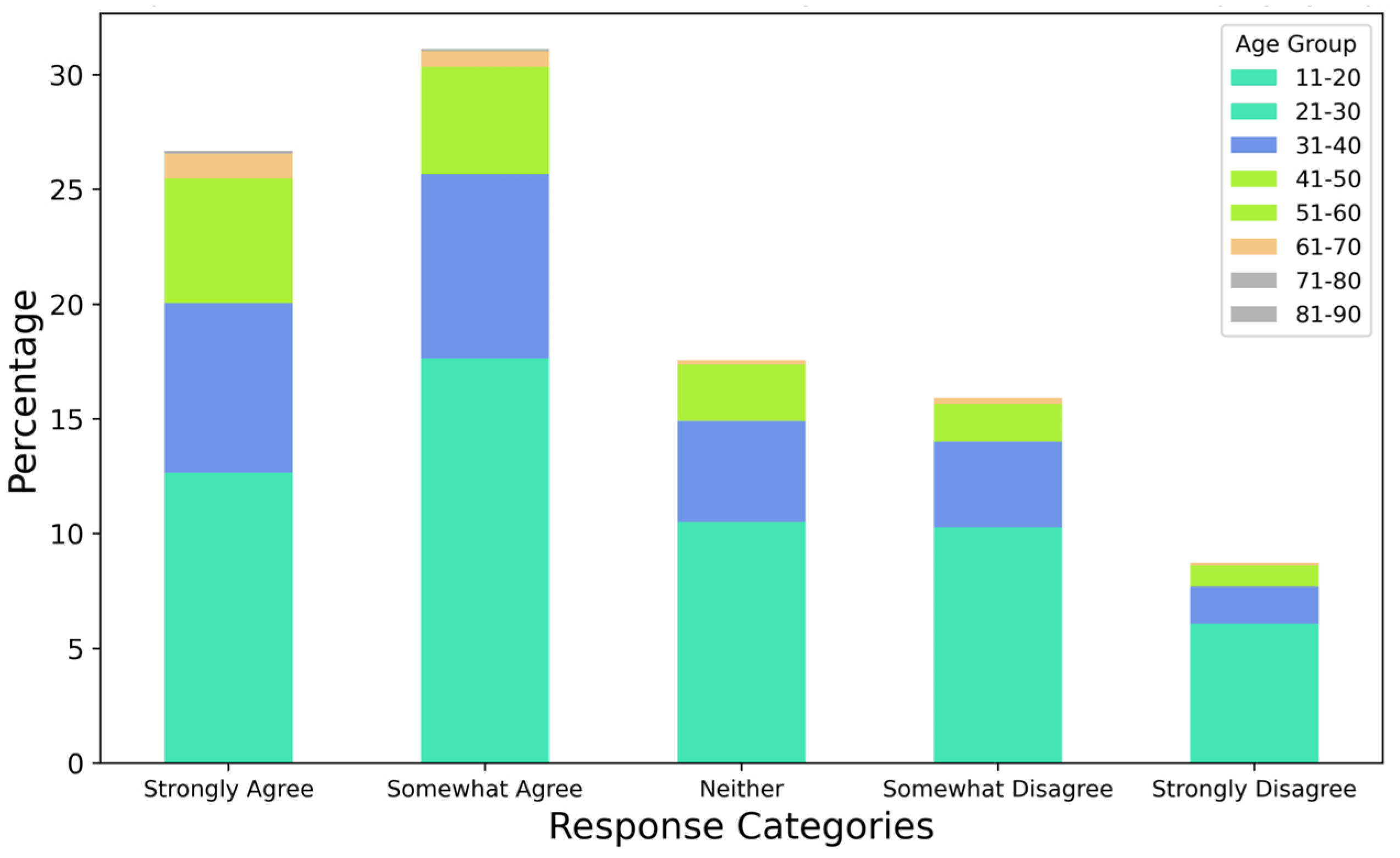
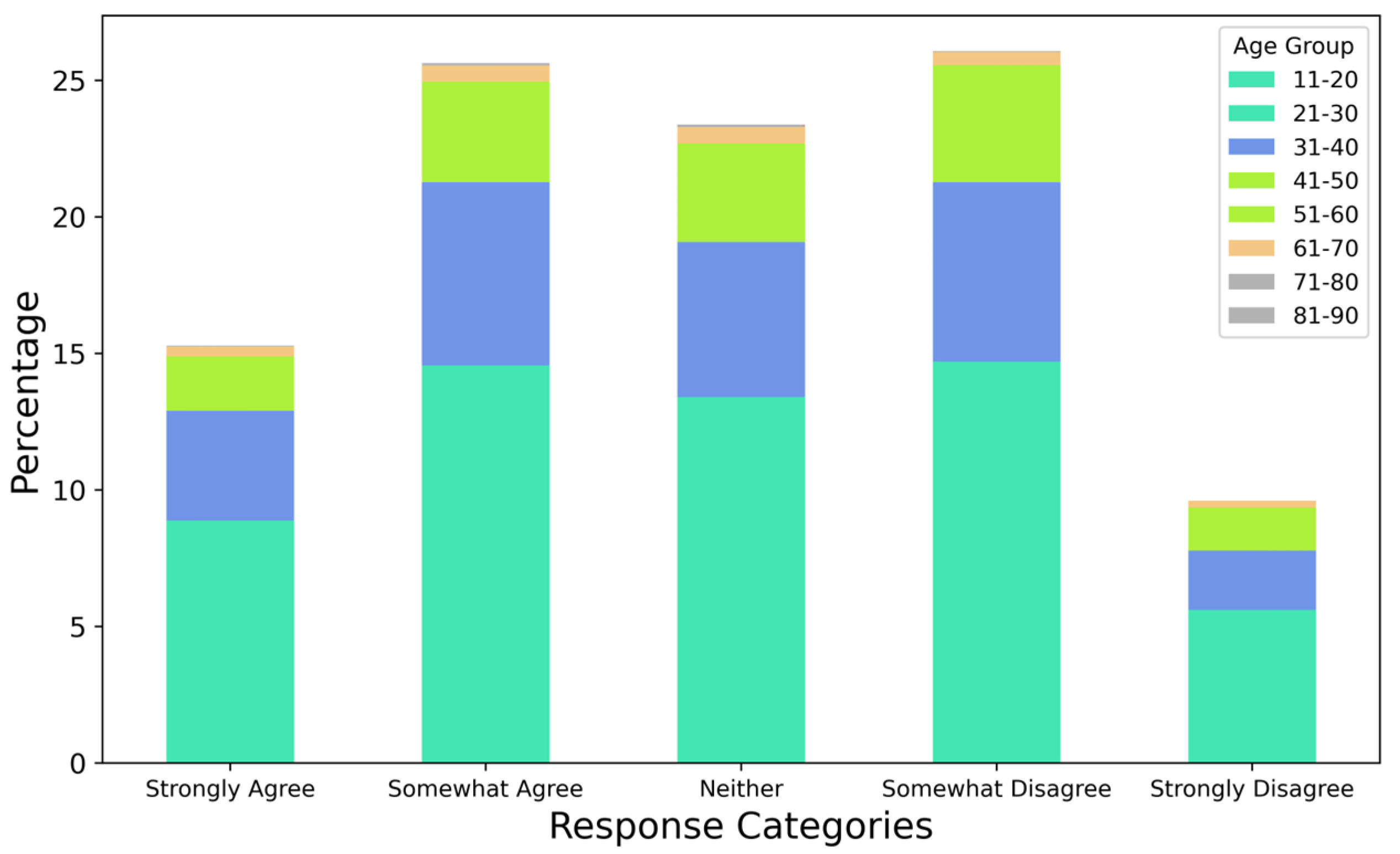
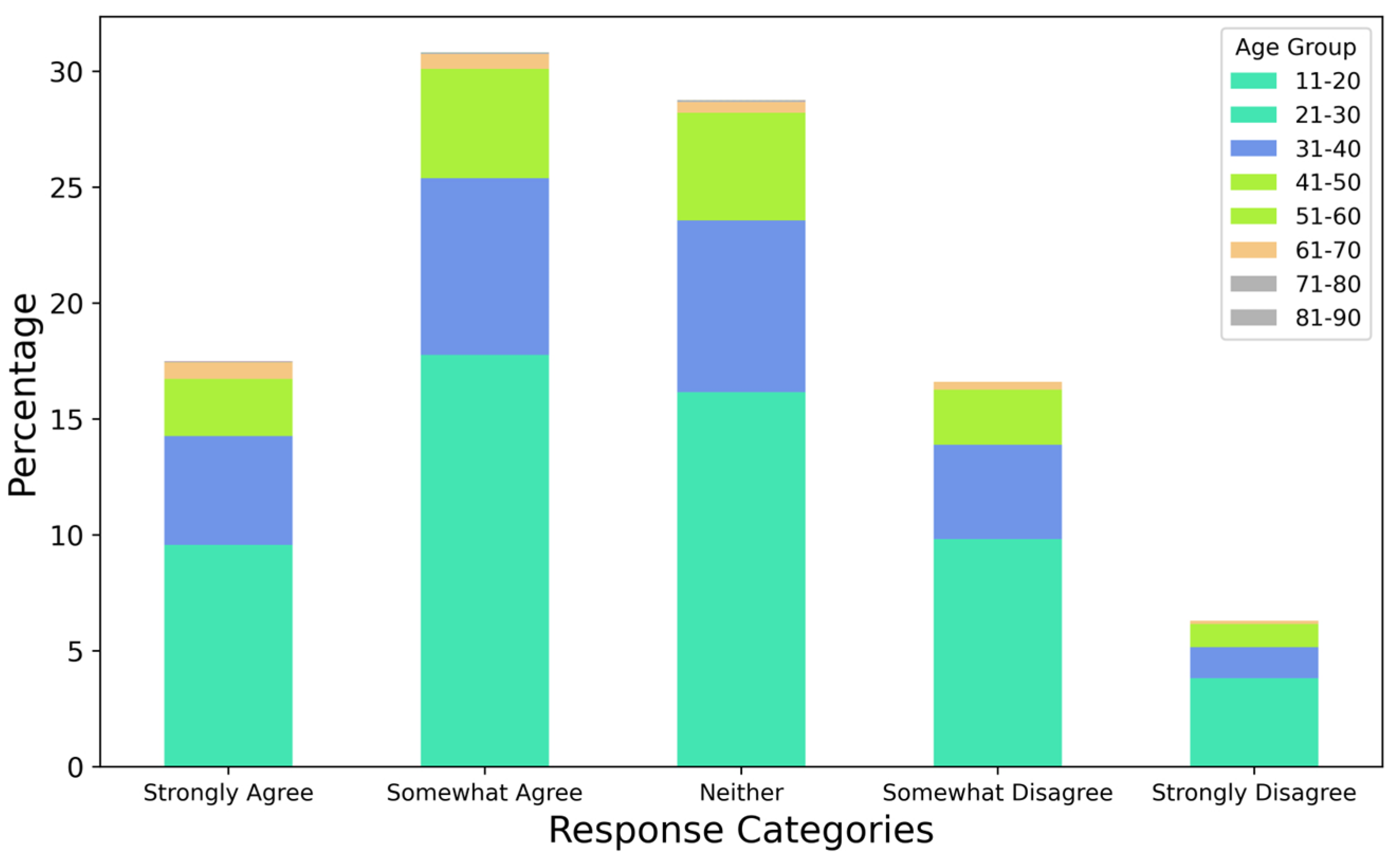
| Algorithm 3: Analysis of Responses per Age Group per Question (from Qlist) |
| Input: Master Dataset Output: Stacked Graphs (aggregate) per Q from Qlist per Age group Local variables: response_type, ages response_type = strong_agree, somewhat_agree, neither, somewhat_disagree, strong_disagree for each record in response_type do: for each row in the record do: total = 0 age ← row[0] for each month in months do: total ← add the value of row[month] end of for loop result[response_type][age] = total end of for loop end of for loop df_trans = result.transpose() df_percentage = df_trans.div(df_trans.sum().sum()) * 100 num_age_groups ← length of df_percentage.index ax = df_percentage with stacked = true fig: = stacked bar graph with these values save fig as an image |
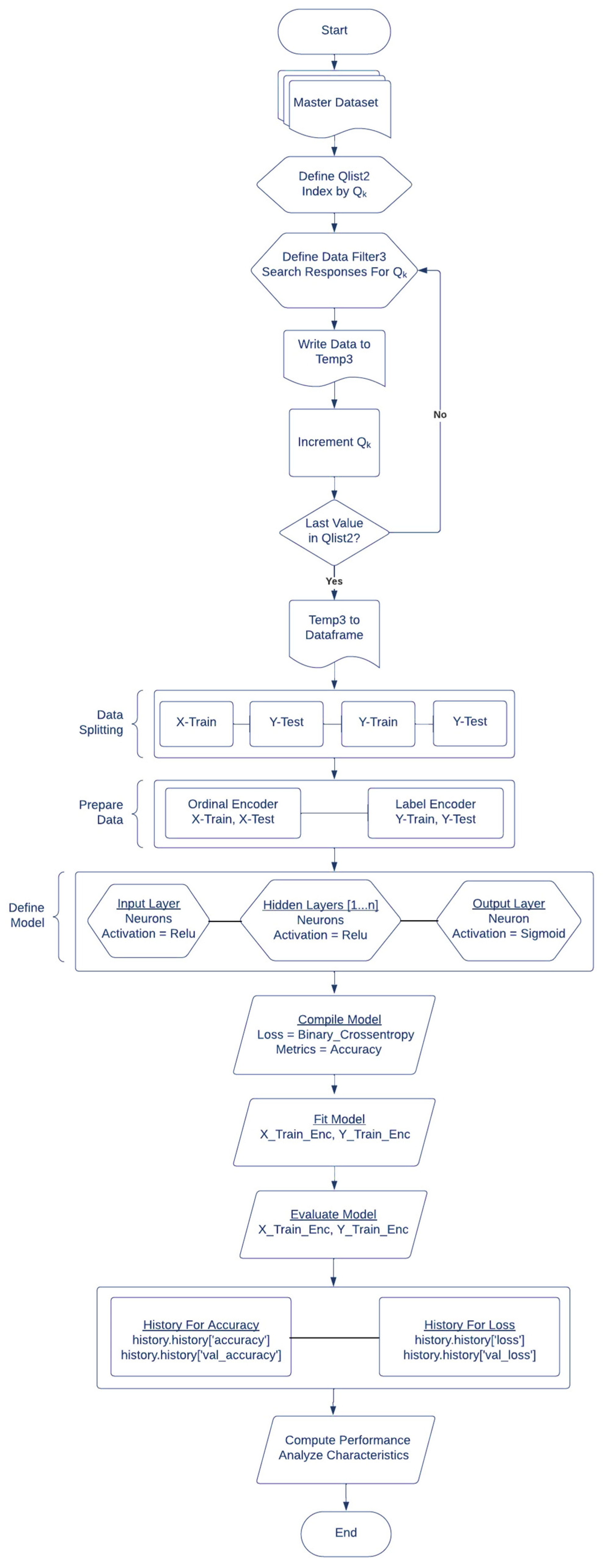
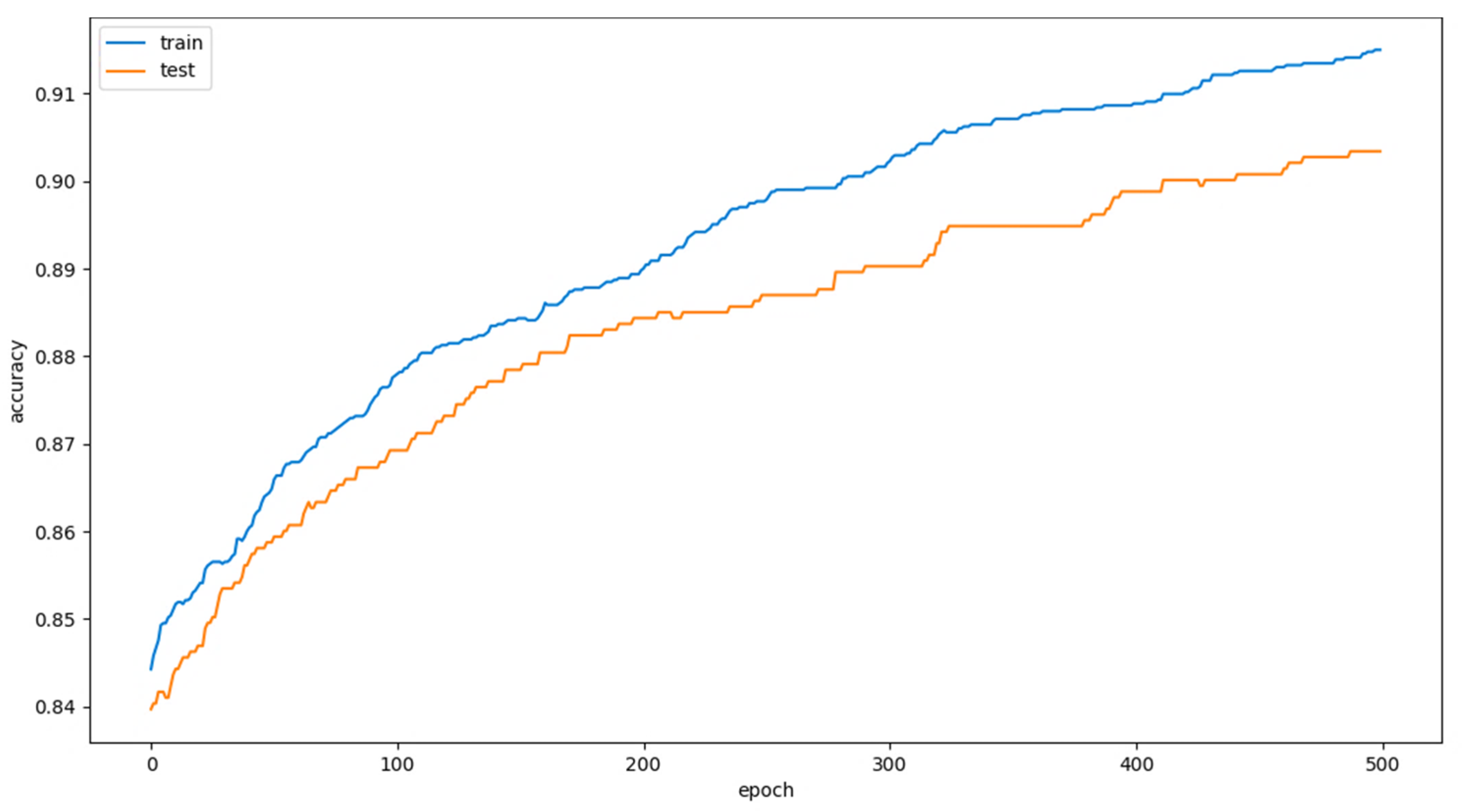
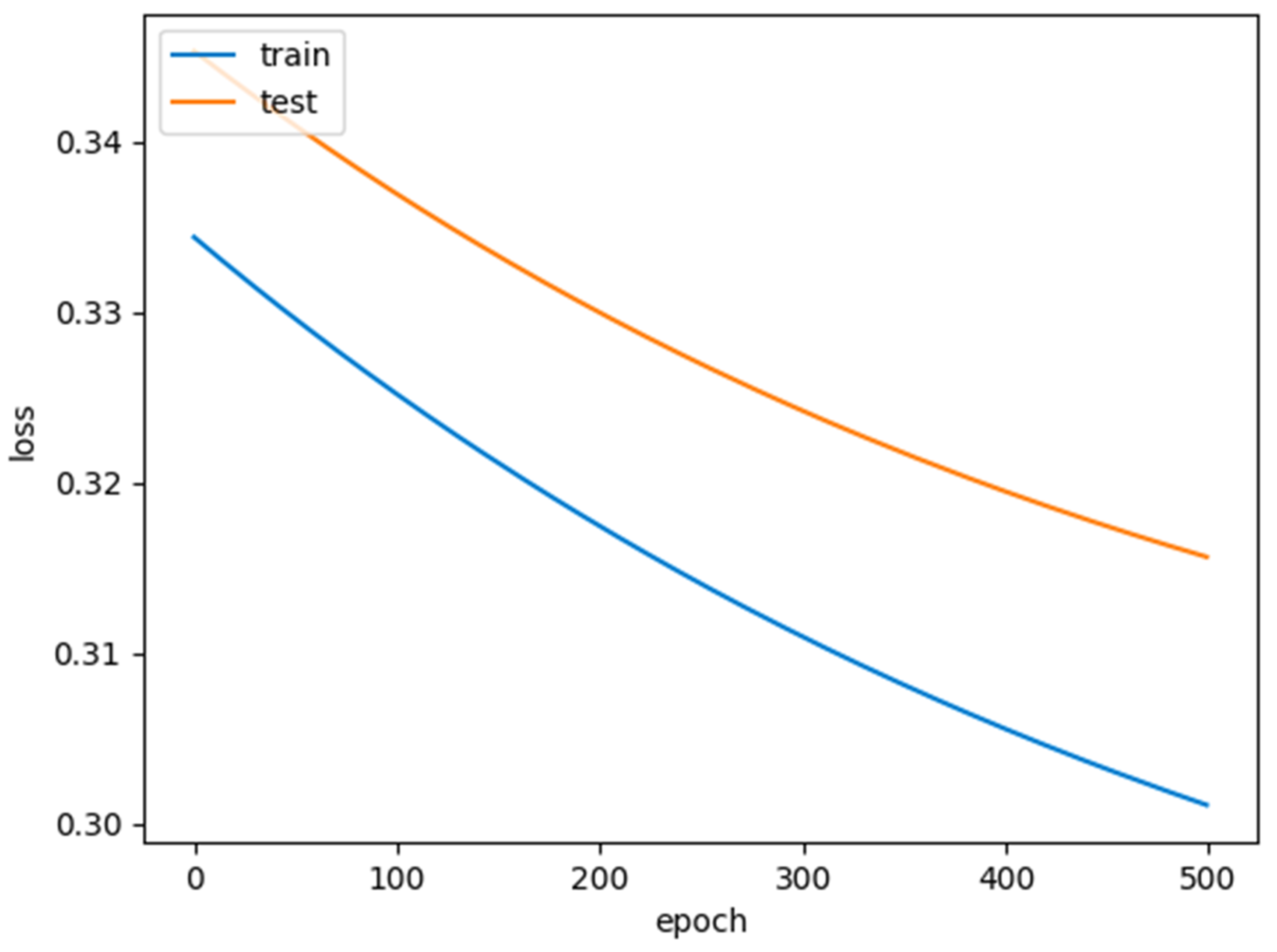
| Algorithm 4: Deep Learning Model to Detect the Responses for QSpecific |
| Input: Master Dataset Output: Performance characteristics of the Deep Learning model Local variables: X_train, X_test, y_train, y_test def prepare_inputs(X_train, X_test): oe ← OrdinalEncoder() X_train_enc ← transform X_train using oe X_test_enc ← transform X_test using oe return X_train_enc, X_test_enc end of function def prepare_targets(y_train, y_test): le ← LabelEncoder() y_train_enc ← transform y_train using le y_test_enc ← transform y_test using le return y_train_enc, y_test_enc end of function X, y = load_dataset from input X_train, X_test, y_train, y_test = train_test_split(split ratio) X_train_enc, X_test_enc = prepare_inputs(X_train, X_test) y_train_enc, y_test_enc = prepare_targets(y_train, y_test) model = Sequential() model ← add(input layer, activation = relu, kernel_initializer = he_normal) model ← add(hidden layers, activation = relu) model ← add(output layer, activation = sigmoid) model.compile(loss = binary_crossentropy, optimizer = SGD, metrics = accuracy) model ← fit(X_train_enc, y_train_enc, epochs, batch_size, verbose) accuracy = model.evaluate(X_test_enc, y_test_enc, verbose) fig: = graph with model history using history.history.keys() save fig as an image |
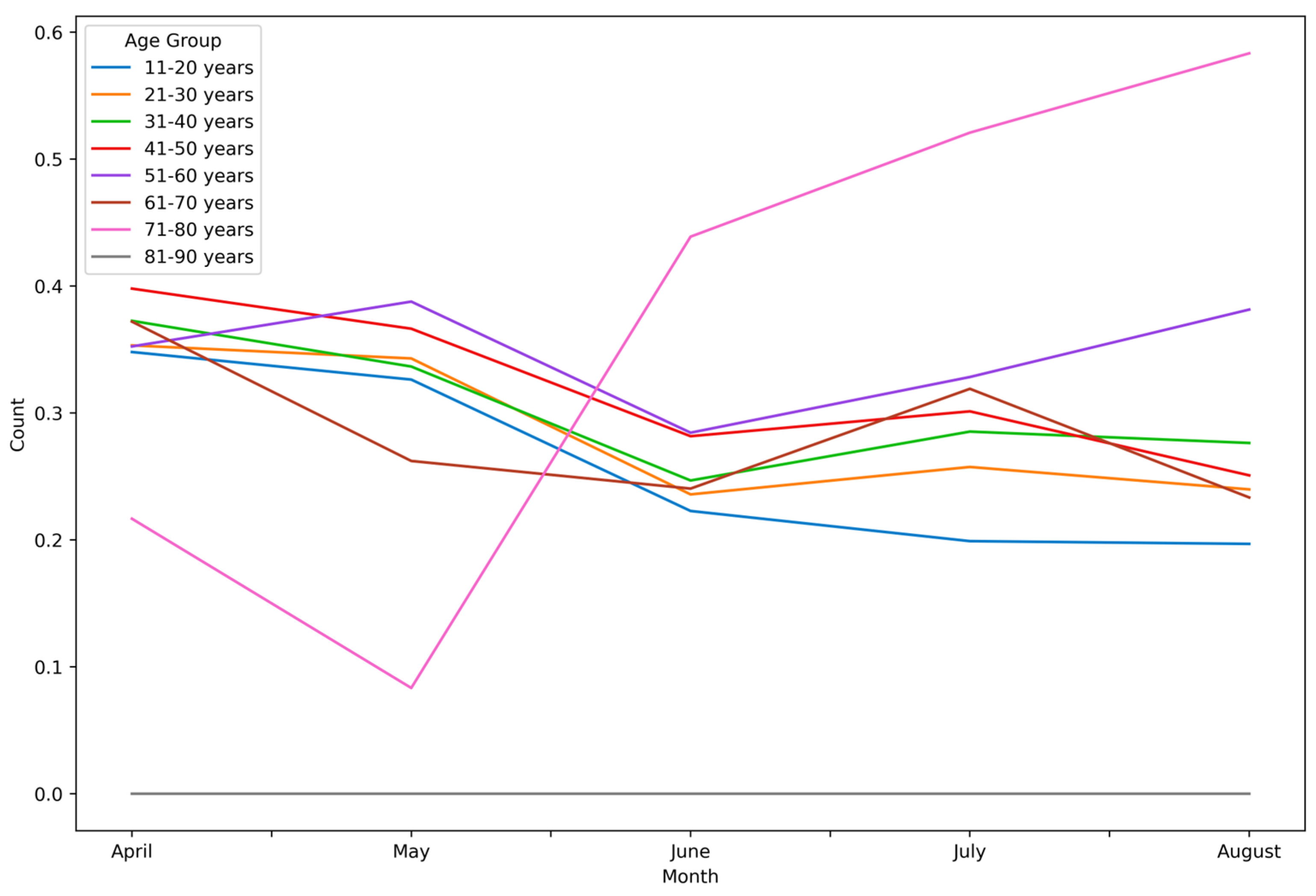
4. Results and Discussion
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Shi, Y.; Wang, G.; Cai, X.-P.; Deng, J.-W.; Zheng, L.; Zhu, H.-H.; Zheng, M.; Yang, B.; Chen, Z. An Overview of COVID-19. J. Zhejiang Univ. Sci. B 2020, 21, 343–360. [Google Scholar] [CrossRef] [PubMed]
- WHO Coronavirus (COVID-19) Dashboard. Available online: https://covid19.who.int/ (accessed on 19 December 2023).
- Reardon, S. Ebola’s Mental-Health Wounds Linger in Africa. Nature 2015, 519, 13–14. [Google Scholar] [CrossRef] [PubMed]
- Mamun, M.A. Suicide and Suicidal Behaviors in the Context of COVID-19 Pandemic in Bangladesh: A Systematic Review. Psychol. Res. Behav. Manag. 2021, 14, 695–704. [Google Scholar] [CrossRef] [PubMed]
- al Mamun, F.; Hosen, I.; Misti, J.M.; Kaggwa, M.M.; Mamun, M.A. Mental Disorders of Bangladeshi Students during the COVID-19 Pandemic: A Systematic Review. Psychol. Res. Behav. Manag. 2021, 14, 645–654. [Google Scholar] [CrossRef] [PubMed]
- Thakur, N.; Cho, H.; Cheng, H.; Lee, H. Analysis of User Diversity-Based Patterns of Public Discourse on Twitter about Mental Health in the Context of Online Learning during COVID-19. In Proceedings of the 2023 Human Computer Interaction International Conference (HCII), Copenhagen, Denmark, 23–28 July 2023. [Google Scholar]
- Mental Health. Available online: https://www.who.int/publications/i/item/WHO-2019-nCoV-Sci_Brief-Mental_health-2022.1 (accessed on 19 December 2023).
- Rogers, A.H.; Shepherd, J.M.; Garey, L.; Zvolensky, M.J. Psychological Factors Associated with Substance Use Initiation during the COVID-19 Pandemic. Psychiatry Res. 2020, 293, 113407. [Google Scholar] [CrossRef] [PubMed]
- Ogueji, I.A.; Asagba, R.B.; Constantine-Simms, D. The Fear of COVID-19, Demographic Factors, and Substance Use in a Multinational Sample amid the COVID-19 Pandemic. Eur. Rev. Appl. Sociol. 2021, 14, 43–54. [Google Scholar] [CrossRef]
- Dumas, T.M.; Ellis, W.; Litt, D.M. What Does Adolescent Substance Use Look like during the COVID-19 Pandemic? Examining Changes in Frequency, Social Contexts, and Pandemic-Related Predictors. J. Adolesc. Health 2020, 67, 354–361. [Google Scholar] [CrossRef] [PubMed]
- Roberts, A.; Rogers, J.; Mason, R.; Siriwardena, A.N.; Hogue, T.; Whitley, G.A.; Law, G.R. Alcohol and Other Substance Use during the COVID-19 Pandemic: A Systematic Review. Drug Alcohol Depend. 2021, 229, 109150. [Google Scholar] [CrossRef] [PubMed]
- Zhu, N.; Zhang, D.; Wang, W.; Li, X.; Yang, B.; Song, J.; Zhao, X.; Huang, B.; Shi, W.; Lu, R.; et al. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N. Engl. J. Med. 2020, 382, 727–733. [Google Scholar] [CrossRef]
- Wang, L.-F.; Shi, Z.; Zhang, S.; Field, H.; Daszak, P.; Eaton, B. Review of Bats and SARS. Emerg. Infect. Dis. 2006, 12, 1834–1840. [Google Scholar] [CrossRef]
- Ge, X.-Y.; Li, J.-L.; Yang, X.-L.; Chmura, A.A.; Zhu, G.; Epstein, J.H.; Mazet, J.K.; Hu, B.; Zhang, W.; Peng, C.; et al. Isolation and Characterization of a Bat SARS-like Coronavirus That Uses the ACE2 Receptor. Nature 2013, 503, 535–538. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Guo, D. Molecular Mechanisms of Coronavirus RNA Capping and Methylation. Virol. Sin. 2016, 31, 3–11. [Google Scholar] [CrossRef]
- King, A.M.Q.; Lefkowitz, E.; Adams, M.J.; Carstens, E.B. Virus Taxonomy: Ninth Report of the International Committee on Taxonomy of Viruses; Elsevier: Amsterdam, The Netherlands, 2011; ISBN 9780123846853. [Google Scholar]
- Zhou, P.; Yang, X.-L.; Wang, X.-G.; Hu, B.; Zhang, L.; Zhang, W.; Si, H.-R.; Zhu, Y.; Li, B.; Huang, C.-L.; et al. A Pneumonia Outbreak Associated with a New Coronavirus of Probable Bat Origin. Nature 2020, 579, 270–273. [Google Scholar] [CrossRef] [PubMed]
- Chan, J.F.-W.; Yuan, S.; Kok, K.-H.; To, K.K.-W.; Chu, H.; Yang, J.; Xing, F.; Liu, J.; Yip, C.C.-Y.; Poon, R.W.-S.; et al. A Familial Cluster of Pneumonia Associated with the 2019 Novel Coronavirus Indicating Person-to-Person Transmission: A Study of a Family Cluster. Lancet 2020, 395, 514–523. [Google Scholar] [CrossRef] [PubMed]
- Liu, P.; Chen, W.; Chen, J.-P. Viral Metagenomics Revealed Sendai Virus and Coronavirus Infection of Malayan Pangolins (Manis javanica). Viruses 2019, 11, 979. [Google Scholar] [CrossRef] [PubMed]
- Cui, H.; Gao, Z.; Liu, M.; Lu, S.; Mo, S.; Mkandawire, W.; Narykov, O.; Srinivasan, S.; Korkin, D. Structural Genomics and Interactomics of 2019 Wuhan Novel Coronavirus, 2019-nCoV, Indicate Evolutionary Conserved Functional Regions of Viral Proteins. bioRxiv 2020. [Google Scholar] [CrossRef]
- Chan, J.F.-W.; Kok, K.-H.; Zhu, Z.; Chu, H.; To, K.K.-W.; Yuan, S.; Yuen, K.-Y. Genomic Characterization of the 2019 Novel Human-Pathogenic Coronavirus Isolated from a Patient with Atypical Pneumonia after Visiting Wuhan. Emerg. Microbes Infect. 2020, 9, 221–236. [Google Scholar] [CrossRef] [PubMed]
- Ceraolo, C.; Giorgi, F.M. Genomic Variance of the 2019-nCoV Coronavirus. J. Med. Virol. 2020, 92, 522–528. [Google Scholar] [CrossRef] [PubMed]
- Dong, N.; Yang, X.; Ye, L.; Chen, K.; Chan, E.W.-C.; Yang, M.; Chen, S. Genomic and Protein Structure Modelling Analysis Depicts the Origin and Infectivity of 2019-nCoV, a New Coronavirus Which Caused a Pneumonia Outbreak in Wuhan, China. bioRxiv 2020. [Google Scholar] [CrossRef]
- Hofmann, H.; Pöhlmann, S. Cellular Entry of the SARS Coronavirus. Trends Microbiol. 2004, 12, 466–472. [Google Scholar] [CrossRef]
- Li, F.; Li, W.; Farzan, M.; Harrison, S.C. Structure of SARS Coronavirus Spike Receptor-Binding Domain Complexed with Receptor. Science 2005, 309, 1864–1868. [Google Scholar] [CrossRef] [PubMed]
- Wrapp, D.; Wang, N.; Corbett, K.S.; Goldsmith, J.A.; Hsieh, C.-L.; Abiona, O.; Graham, B.S.; McLellan, J.S. Cryo-EM Structure of the 2019-nCoV Spike in the Prefusion Conformation. Science 2020, 367, 1260–1263. [Google Scholar] [CrossRef] [PubMed]
- Li, F. Structure, Function, and Evolution of Coronavirus Spike Proteins. Annu. Rev. Virol. 2016, 3, 237–261. [Google Scholar] [CrossRef] [PubMed]
- Huang, Q.; Herrmann, A. Fast Assessment of Human Receptor-Binding Capability of 2019 Novel Coronavirus (2019-nCoV). bioRxiv 2020. [Google Scholar] [CrossRef]
- Meng, T.; Cao, H.; Zhang, H.; Kang, Z.; Xu, D.; Gong, H.; Wang, J.; Li, Z.; Cui, X.; Xu, H.; et al. The Insert Sequence in SARS-CoV-2 Enhances Spike Protein Cleavage by TMPRSS. bioRxiv 2020. [Google Scholar] [CrossRef]
- Walls, A.C.; Park, Y.-J.; Tortorici, M.A.; Wall, A.; McGuire, A.T.; Veesler, D. Structure, Function, and Antigenicity of the SARS-CoV-2 Spike Glycoprotein. Cell 2020, 181, 281–292.e6. [Google Scholar] [CrossRef] [PubMed]
- Jaimes, J.A.; André, N.M.; Millet, J.K.; Whittaker, G.R. Structural Modeling of 2019-Novel Coronavirus (nCoV) Spike Protein Reveals a Proteolytically-Sensitive Activation Loop as a Distinguishing Feature Compared to SARS-CoV and Related SARS-like Coronaviruses. bioRxiv 2020. [Google Scholar] [CrossRef] [PubMed]
- Saha, A.; Saha, B. Novel Coronavirus SARS-CoV-2 (Covid-19) Dynamics inside the Human Body. Rev. Med. Virol. 2020, 30, e2140. [Google Scholar] [CrossRef] [PubMed]
- Zaim, S.; Chong, J.H.; Sankaranarayanan, V.; Harky, A. COVID-19 and Multiorgan Response. Curr. Probl. Cardiol. 2020, 45, 100618. [Google Scholar] [CrossRef]
- Chowdhury, M.A.; Hossain, N.; Kashem, M.A.; Shahid, M.A.; Alam, A. Immune Response in COVID-19: A Review. J. Infect. Public Health 2020, 13, 1619–1629. [Google Scholar] [CrossRef]
- Tabary, M.; Khanmohammadi, S.; Araghi, F.; Dadkhahfar, S.; Tavangar, S.M. Pathologic Features of COVID-19: A Concise Review. Pathol. Res. Pract. 2020, 216, 153097. [Google Scholar] [CrossRef] [PubMed]
- Quadros, S.; Garg, S.; Ranjan, R.; Vijayasarathi, G.; Mamun, M.A. Fear of COVID 19 Infection across Different Cohorts: A Scoping Review. Front. Psychiatry 2021, 12, 708430. [Google Scholar] [CrossRef] [PubMed]
- Pakpour, A.H.; Griffiths, M.D. The Fear of COVID-19 and Its Role in Preventive Behaviors. J. Concurr. Disord. 2020, 2, 58–63. [Google Scholar] [CrossRef]
- Troisi, A. Fear of Covid-19: Insights from Evolutionary Behavioral Science. Clin. Neuropsychiatry 2020, 17, 72. [Google Scholar] [CrossRef]
- LeDoux, J. Anxious: Using the Brain to Understand and Treat Fear and Anxiety; Penguin: New York, NY, USA, 2016; ISBN 9780143109044. [Google Scholar]
- Erbiçer, E.S.; Metin, A.; Çetinkaya, A.; Şen, S. The Relationship between Fear of COVID-19 and Depression, Anxiety, and Stress: A Meta-Analysis. Eur. Psychol. 2021, 26, 323–333. [Google Scholar] [CrossRef]
- Banerjee, D. The COVID-19 Outbreak: Crucial Role the Psychiatrists Can Play. Asian J. Psychiatr. 2020, 50, 102014. [Google Scholar] [CrossRef]
- Smits, M.; Staal, J.B.; van Goor, H. Could Virtual Reality Play a Role in the Rehabilitation after COVID-19 Infection? BMJ Open Sport Exerc. Med. 2020, 6, e000943. [Google Scholar] [CrossRef]
- Sampaio, M.; Navarro Haro, M.V.; De Sousa, B.; Vieira Melo, W.; Hoffman, H.G. Therapists Make the Switch to Telepsychology to Safely Continue Treating Their Patients during the COVID-19 Pandemic. Virtual Reality Telepsychology May Be Next. Front. Virtual Real. 2021, 1, 576421. [Google Scholar] [CrossRef]
- Garcia, D.; Blizzard, A.M.; Peskin, A.; Rothenberg, W.A.; Schmidt, E.; Piscitello, J.; Espinosa, N.; Salem, H.; Rodriguez, G.M.; Sherman, J.A.; et al. Rapid, Full-Scale Change to Virtual PCIT during the COVID-19 Pandemic: Implementation and Clinical Implications. Prev. Sci. 2021, 22, 269–283. [Google Scholar] [CrossRef]
- Dantas, L.O.; Barreto, R.P.G.; Ferreira, C.H.J. Digital Physical Therapy in the COVID-19 Pandemic. Braz. J. Phys. Ther. 2020, 24, 381–383. [Google Scholar] [CrossRef]
- Liu, S.; Yang, L.; Zhang, C.; Xiang, Y.-T.; Liu, Z.; Hu, S.; Zhang, B. Online Mental Health Services in China during the COVID-19 Outbreak. Lancet Psychiatry 2020, 7, e17–e18. [Google Scholar] [CrossRef]
- Angermeyer, M.C.; Matschinger, H.; Riedel-Heller, S.G. Whom to Ask for Help in Case of a Mental Disorder? Preferences of the Lay Public. Soc. Psychiatry Psychiatr. Epidemiol. 1999, 34, 202–210. [Google Scholar] [CrossRef]
- Glueckauf, R.L.; Maheu, M.M.; Drude, K.P.; Wells, B.A.; Wang, Y.; Gustafson, D.J.; Nelson, E.-L. Survey of Psychologists’ Telebehavioral Health Practices: Technology Use, Ethical Issues, and Training Needs. Prof. Psychol. Res. Pract. 2018, 49, 205–219. [Google Scholar] [CrossRef]
- Elhai, J.D.; Yang, H.; McKay, D.; Asmundson, G.J.G.; Montag, C. Modeling Anxiety and Fear of COVID-19 Using Machine Learning in a Sample of Chinese Adults: Associations with Psychopathology, Sociodemographic, and Exposure Variables. Anxiety Stress Coping 2021, 34, 130–144. [Google Scholar] [CrossRef] [PubMed]
- Eder, S.J.; Steyrl, D.; Stefańczyk, M.; Pieniak, M.; Molina, J.M.; Pešout, O.; Binter, J.; Smela, P.; Scharnowski, F.; Nicholson, A. Predicting Fear and Perceived Health during the COVID-19 Pandemic Using Machine Learning: A Cross-National Longitudinal Study. PLoS ONE 2021, 16, e0247997. [Google Scholar] [CrossRef] [PubMed]
- Albagmi, F.M.; Alansari, A.; Al Shawan, D.S.; AlNujaidi, H.Y.; Olatunji, S.O. Prediction of Generalized Anxiety Levels during the Covid-19 Pandemic: A Machine Learning-Based Modeling Approach. Inform. Med. Unlocked 2022, 28, 100854. [Google Scholar] [CrossRef]
- Feng, P.; Chen, Z.; Becker, B.; Liu, X.; Zhou, F.; He, Q.; Qiu, J.; Lei, X.; Chen, H.; Feng, T. Predisposing Variations in Fear-Related Brain Networks Prospectively Predict Fearful Feelings during the 2019 Coronavirus (COVID-19) Pandemic. Cereb. Cortex 2022, 32, 540–553. [Google Scholar] [CrossRef] [PubMed]
- Roy, D.; Roy, T.J.; Mahmud, I.; Alvi, N. An Efficient Approach to Predict Fear of Human’s Mind during COVID-19 Outbreaks Utilizing Data Mining Technique. In Advances in Intelligent Systems and Computing; Springer: Singapore, 2022; pp. 41–51. ISBN 9789811625961. [Google Scholar]
- Kalita, M.; Hussain, G.I. Determining the Influencing Factors of COVID 19 on Mental Health Using Neural Network. Int. Res. J. Adv. Sci. Hub 2021, 3, 126–129. [Google Scholar] [CrossRef]
- Fitzpatrick, K.M.; Harris, C.; Drawve, G. Fear of COVID-19 and the Mental Health Consequences in America. Psychol. Trauma 2020, 12, S17–S21. [Google Scholar] [CrossRef]
- Mistry, S.K.; Ali, A.R.M.M.; Akther, F.; Yadav, U.N.; Harris, M.F. Exploring Fear of COVID-19 and Its Correlates among Older Adults in Bangladesh. Glob. Health 2021, 17, 47. [Google Scholar] [CrossRef]
- Avazzadeh, S.; Gilani, N.; Jahangiry, L. Predictors of Fear Control Related to COVID-19 among Older Population: An Investigation on COVID-19 Risk Perception and Health Related Quality of Life during the Pandemic. Health Qual. Life Outcomes 2023, 21, 79. [Google Scholar] [CrossRef] [PubMed]
- Demirbas, N.; Kutlu, R. Effects of COVID-19 Fear on Society’s Quality of Life. Int. J. Ment. Health Addict. 2022, 20, 2813–2822. [Google Scholar] [CrossRef] [PubMed]
- Suhail, A.; Dar, K.A.; Iqbal, N. COVID-19 Related Fear and Mental Health in Indian Sample: The Buffering Effect of Support System. Curr. Psychol. 2022, 41, 480–491. [Google Scholar] [CrossRef] [PubMed]
- Chair, S.Y.; Chien, W.T.; Liu, T.; Lam, L.; Cross, W.; Banik, B.; Rahman, M.A. Psychological Distress, Fear and Coping Strategies among Hong Kong People during the COVID-19 Pandemic. Curr. Psychol. 2023, 42, 2538–2557. [Google Scholar] [CrossRef] [PubMed]
- Elhessewi, G.M.S.; Almoayad, F.; Mahboub, S.; Alhashem, A.M.; Fiala, L. Psychological Distress and Its Risk Factors during COVID-19 Pandemic in Saudi Arabia: A Cross-Sectional Study. Middle East Curr. Psychiatr. 2021, 28, 7. [Google Scholar] [CrossRef]
- Ambelu, A.; Birhanu, Z.; Yitayih, Y.; Kebede, Y.; Mecha, M.; Abafita, J.; Belay, A.; Fufa, D. Psychological Distress during the COVID-19 Pandemic in Ethiopia: An Online Cross-Sectional Study to Identify the Need for Equal Attention of Intervention. Ann. Gen. Psychiatry 2021, 20, 22. [Google Scholar] [CrossRef] [PubMed]
- Traunmüller, C.; Stefitz, R.; Gaisbachgrabner, K.; Schwerdtfeger, A. Psychological Correlates of COVID-19 Pandemic in the Austrian Population. BMC Public Health 2020, 20, 1395. [Google Scholar]
- Lee, J.; Jeong, H.J.; Kim, S. Stress, Anxiety, and Depression among Undergraduate Students during the COVID-19 Pandemic and Their Use of Mental Health Services. Innov. High. Educ. 2021, 46, 519–538. [Google Scholar] [CrossRef] [PubMed]
- Verma, H.; Verma, G.; Kumar, P. Depression, Anxiety, and Stress during Times of COVID-19: An Analysis of Youngsters Studying in Higher Education in India. Rev. Socionetw. Strateg. 2021, 15, 471–488. [Google Scholar] [CrossRef]
- Villani, L.; Pastorino, R.; Molinari, E.; Anelli, F.; Ricciardi, W.; Graffigna, G.; Boccia, S. Impact of the COVID-19 Pandemic on Psychological Well-Being of Students in an Italian University: A Web-Based Cross-Sectional Survey. Glob. Health 2021, 17, 39. [Google Scholar] [CrossRef]
- Fodjo, J.N.S.; Ngarka, L.; Njamnshi, Y.W.; Nfor, L.N.; Mengnjo, M.K.; Mendo, E.L.; Angwafor, S.A.; Basseguin, J.G.A.; Nkouonlack, C.; Njit, E.N.; et al. Fear and Depression during the COVID-19 Outbreak in Cameroon: A Nation-Wide Observational Study. BMC Psychiatry 2021, 21, 356. [Google Scholar] [CrossRef] [PubMed]
- Sakib, N.; Akter, T.; Zohra, F.; Bhuiyan, A.K.M.I.; Mamun, M.A.; Griffiths, M.D. Fear of COVID-19 and Depression: A Comparative Study among the General Population and Healthcare Professionals during COVID-19 Pandemic Crisis in Bangladesh. Int. J. Ment. Health Addict. 2023, 21, 976–992. [Google Scholar] [CrossRef] [PubMed]
- Khalaf, O.O.; Abdalgeleel, S.A.; Mostafa, N. Fear of COVID-19 Infection and Its Relation to Depressive and Anxiety Symptoms among Elderly Population: Online Survey. Middle East Curr. Psychiatr. 2022, 29, 7. [Google Scholar] [CrossRef]
- Kabasakal, E.; Özpulat, F.; Akca, A.; Özcebe, L.H. COVID-19 Fear and Compliance in Preventive Measures Precautions in Workers during the COVID-19 Pandemic. Int. Arch. Occup. Environ. Health 2021, 94, 1239–1247. [Google Scholar] [CrossRef] [PubMed]
- Malik, S.; Ullah, I.; Irfan, M.; Ahorsu, D.K.; Lin, C.-Y.; Pakpour, A.H.; Griffiths, M.D.; Rehman, I.U.; Minhas, R. Fear of COVID-19 and Workplace Phobia among Pakistani Doctors: A Survey Study. BMC Public Health 2021, 21, 833. [Google Scholar] [CrossRef]
- Jue, J.; Ha, J.H. Art Therapists’ Fear of COVID-19, Subjective Well-Being, and Mindfulness. Arts Psychother. 2022, 77, 101881. [Google Scholar] [CrossRef] [PubMed]
- Satici, S.A.; Kayis, A.R.; Satici, B.; Griffiths, M.D.; Can, G. Resilience, Hope, and Subjective Happiness among the Turkish Population: Fear of COVID-19 as a Mediator. Int. J. Ment. Health Addict. 2023, 21, 803–818. [Google Scholar] [CrossRef]
- Blasco-Belled, A.; Tejada-Gallardo, C.; Torrelles-Nadal, C.; Alsinet, C. The Costs of the COVID-19 on Subjective Well-Being: An Analysis of the Outbreak in Spain. Sustainability 2020, 12, 6243. [Google Scholar] [CrossRef]
- Gritzka, S.; Angerer, P.; Diebig, M. The Mediating Role of Fear of COVID-19 in the Association between COVID-19-Related Work Stressors and Subjective Well-Being: Cross-Sectional Evidence in the Child Care Sector across Three Samples. Res. Sq. 2022. [Google Scholar] [CrossRef]
- Mertens, G.; Lodder, P.; Smeets, T.; Duijndam, S. Fear of COVID-19: Data of a Large Longitudinal Survey Conducted between March 2020 and June 2021. Data Brief 2023, 48, 109177. [Google Scholar] [CrossRef]
- Vos, L.M.W.; Habibović, M.; Nyklíček, I.; Smeets, T.; Mertens, G. Optimism, Mindfulness, and Resilience as Potential Protective Factors for the Mental Health Consequences of Fear of the Coronavirus. Psychiatry Res. 2021, 300, 113927. [Google Scholar] [CrossRef] [PubMed]
- Tzur Bitan, D.; Grossman-Giron, A.; Bloch, Y.; Mayer, Y.; Shiffman, N.; Mendlovic, S. Fear of COVID-19 Scale: Psychometric Characteristics, Reliability and Validity in the Israeli Population. Psychiatry Res. 2020, 289, 113100. [Google Scholar] [CrossRef] [PubMed]
- TextBlob. Available online: https://media.readthedocs.org/pdf/textblob/latest/textblob.pdf (accessed on 22 December 2023).
- Sindhu, C.; Sasmal, B.; Gupta, R.; Prathipa, J. Subjectivity Detection for Sentiment Analysis on Twitter Data. In Artificial Intelligence Techniques for Advanced Computing Applications; Springer: Singapore, 2021; pp. 467–476. ISBN 9789811553288. [Google Scholar]
- Yaqub, U.; Sharma, N.; Pabreja, R.; Chun, S.A.; Atluri, V.; Vaidya, J. Analysis and Visualization of Subjectivity and Polarity of Twitter Location Data. In Proceedings of the 19th Annual International Conference on Digital Government Research: Governance in the Data Age, Delft, The Netherlands, 30 May–1 June 2018; ACM: New York, NY, USA, 2018. [Google Scholar]
- Thakur, N.; Cui, S.; Khanna, K.; Knieling, V.; Duggal, Y.N.; Shao, M. Investigation of the Gender-Specific Discourse about Online Learning during COVID-19 on Twitter Using Sentiment Analysis, Subjectivity Analysis, and Toxicity Analysis. Computers 2023, 12, 221. [Google Scholar] [CrossRef]
- Chihab, M.; Chiny, M.; Mabrouk, N.; Boussatta, H.; Chihab, Y.; Hadi, M.Y. BiLSTM and Multiple Linear Regression Based Sentiment Analysis Model Using Polarity and Subjectivity of a Text. Int. J. Adv. Comput. Sci. Appl. 2022, 13, 436–442. [Google Scholar] [CrossRef]
- Melton, C.A.; Olusanya, O.A.; Ammar, N.; Shaban-Nejad, A. Public Sentiment Analysis and Topic Modeling Regarding COVID-19 Vaccines on the Reddit Social Media Platform: A Call to Action for Strengthening Vaccine Confidence. J. Infect. Public Health 2021, 14, 1505–1512. [Google Scholar] [CrossRef] [PubMed]
- Melton, C.A. Mining Public Opinion on COVID-19 Vaccines Using Unstructured Social Media Data. Available online: https://trace.tennessee.edu/utk_graddiss/7624/ (accessed on 28 January 2024).
- Heimerl, F.; Lohmann, S.; Lange, S.; Ertl, T. Word Cloud Explorer: Text Analytics Based on Word Clouds. In Proceedings of the 2014 47th Hawaii International Conference on System Sciences, Waikoloa, HI, USA, 6–9 January 2014. [Google Scholar]
- Goodfellow, I.; Bengio, Y.; Courville, A. Deep Learning; MIT Press: London, UK, 2016; ISBN 9780262337373. [Google Scholar]
- LeCun, Y.; Bengio, Y.; Hinton, G. Deep Learning. Nature 2015, 521, 436–444. [Google Scholar] [CrossRef] [PubMed]
- Chauhan, N.K.; Singh, K. A Review on Conventional Machine Learning vs. Deep Learning. In Proceedings of the 2018 International Conference on Computing, Power and Communication Technologies (GUCON), Greater Noida, India, 28–29 September 2018. [Google Scholar]
- Buduma, N.; Buduma, N.; Papa, J. Fundamentals of Deep Learning; O’Reilly Media, Inc.: Sebastopol, CA, USA, 2022; ISBN 9781492082132. [Google Scholar]
- Ahmed, S.F.; Alam, M.S.B.; Hassan, M.; Rozbu, M.R.; Ishtiak, T.; Rafa, N.; Mofijur, M.; Shawkat Ali, A.B.M.; Gandomi, A.H. Deep Learning Modelling Techniques: Current Progress, Applications, Advantages, and Challenges. Artif. Intell. Rev. 2023, 56, 13521–13617. [Google Scholar] [CrossRef]
- Thakur, N.; Han, C. An Exploratory Study of Tweets about the SARS-CoV-2 Omicron Variant: Insights from Sentiment Analysis, Language Interpretation, Source Tracking, Type Classification, and Embedded URL Detection. COVID 2022, 2, 1026–1049. [Google Scholar] [CrossRef]
- Rahman, M.A.; Islam, S.M.S.; Tungpunkom, P.; Sultana, F.; Alif, S.M.; Banik, B.; Salehin, M.; Joseph, B.; Lam, L.; Watts, M.C.; et al. COVID-19: Factors Associated with Psychological Distress, Fear, and Coping Strategies among Community Members across 17 Countries. Glob. Health 2021, 17, 117. [Google Scholar] [CrossRef]
- Roma, P.; Monaro, M.; Colasanti, M.; Ricci, E.; Biondi, S.; Di Domenico, A.; Verrocchio, M.C.; Napoli, C.; Ferracuti, S.; Mazza, C. A 2-Month Follow-up Study of Psychological Distress among Italian People during the COVID-19 Lockdown. Int. J. Environ. Res. Public Health 2020, 17, 8180. [Google Scholar] [CrossRef]
- Chu, I.Y.-H.; Alam, P.; Larson, H.J.; Lin, L. Social Consequences of Mass Quarantine during Epidemics: A Systematic Review with Implications for the COVID-19 Response. J. Travel Med. 2020, 27, taaa192. [Google Scholar] [CrossRef] [PubMed]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The Psychological Impact of Quarantine and How to Reduce It: Rapid Review of the Evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef] [PubMed]
- Baiano, C.; Zappullo, I.; Conson, M.; The LabNPEE Group. Tendency to Worry and Fear of Mental Health during Italy’s COVID-19 Lockdown. Int. J. Environ. Res. Public Health 2020, 17, 5928. [Google Scholar] [CrossRef] [PubMed]
- Han, M.F.Y.; Mahendran, R.; Yu, J. Associations between Fear of COVID-19, Affective Symptoms and Risk Perception among Community-Dwelling Older Adults during a COVID-19 Lockdown. Front. Psychol. 2021, 12, 638831. [Google Scholar] [CrossRef] [PubMed]
- Fearon, J.D. Ethnic and Cultural Diversity by Country. J. Econ. Growth 2003, 8, 195–222. [Google Scholar] [CrossRef]
- Ibanez, A.; Sisodia, G.S. The Role of Culture on 2020 SARS-CoV-2 Country Deaths: A Pandemic Management Based on Cultural Dimensions. GeoJournal 2022, 87, 1175–1191. [Google Scholar] [CrossRef] [PubMed]
- Huynh, T.L.D. Does Culture Matter Social Distancing under the COVID-19 Pandemic? Saf. Sci. 2020, 130, 104872. [Google Scholar] [CrossRef]
- Furlong, Y.; Finnie, T. Culture Counts: The Diverse Effects of Culture and Society on Mental Health amidst COVID-19 Outbreak in Australia. Ir. J. Psychol. Med. 2020, 37, 237–242. [Google Scholar] [CrossRef]



| Work | Focus Areas of the Works | ||
|---|---|---|---|
| Machine Learning or Applications of Machine Learning | Data Analysis or Content Analysis | Subjectivity Analysis | |
| Elhai et al. [49] | √ | ||
| Eder et al. [50] | √ | ||
| Albagmi et al. [51] | √ | ||
| Feng et al. [52] | √ | ||
| Roy et al. [53] | √ | ||
| Kalita et al. [54] | √ | ||
| Fitzpatrick et al. [55] | √ | ||
| Mistry et al. [56] | √ | ||
| Avazzadeh et al. [57] | √ | ||
| Demirbas et al. [58] | √ | ||
| Suhail et al. [59] | √ | ||
| Chair et al. [60] | √ | ||
| Elhessewi et al. [61] | √ | ||
| Ambelu et al. [62] | √ | ||
| Traunmüller et al. [63] | √ | ||
| Lee et al. [64] | √ | ||
| Verma et al. [65] | √ | ||
| Villani et al. [66] | √ | ||
| Fodjo et al. [67] | √ | ||
| Sakib et al. [68] | √ | ||
| Khalaf et al. [69] | √ | ||
| Kabasakal et al. [70] | √ | ||
| Malik et al. [71] | √ | ||
| Jue et al. [72] | √ | ||
| Satici et al. [73] | √ | ||
| Blasco et al. [74] | √ | ||
| Gritzka et al. [75] | √ | ||
| Thakur et al. [this work] | √ | √ | √ |
| Work | Information about the Represented Countries in the Survey Data | |
|---|---|---|
| Names of Countries | Number of Countries | |
| Elhai et al. [49] | China | 1 |
| Feng et al. [52] | China | 1 |
| Fitzpatrick et al. [55] | United States | 1 |
| Mistry et al. [56] | Bangladesh | 1 |
| Avazzadeh et al. [57] | Iran | 1 |
| Demirbas et al. [58] | Turkey | 1 |
| Suhail et al. [59] | India | 1 |
| Chair et al. [60] | Hong Kong | 1 |
| Elhessewi et al. [61] | Saudi Arabia | 1 |
| Ambelu et al. [62] | Ethiopia | 1 |
| Traunmüller et al. [63] | Austria | 1 |
| Lee et al. [64] | United States | 1 |
| Verma et al. [65] | India | 1 |
| Villani et al. [66] | Italy | 1 |
| Fodjo et al. [67] | Cameroon | 1 |
| Sakib et al. [68] | Bangladesh | 1 |
| Kabasakal et al. [70] | Turkey | 1 |
| Malik et al. [71] | Pakistan | 1 |
| Jue et al. [72] | Korea | 1 |
| Satici et al. [73] | Turkey | 1 |
| Blasco et al. [74] | Spain | 1 |
| Gritzka et al. [75] | Germany | 1 |
| Eder et al. [50] | Austria, Spain, Poland, and Czech Republic | 4 |
| Thakur et al. [this work] | Australia, Austria, Belgium, Canada, Chile, Cyprus, Czech Republic, Denmark, Estonia, Finland, France, Germany, Greece, Hong Kong (S.A.R.), Hungary, India, Ireland, Israel, Italy, Japan, Latvia, Mexico, Netherlands, New Zealand, Norway, Peru, Poland, Portugal, Romania, Russian Federation, Slovenia, South Africa, South Korea, Spain, Sweden, Switzerland, Turkey, United Arab Emirates, United Kingdom, and USA | 40 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Thakur, N.; Patel, K.A.; Poon, A.; Shah, R.; Azizi, N.; Han, C. Investigation of the Global Fear Associated with COVID-19 Using Subjectivity Analysis and Deep Learning. Computation 2024, 12, 118. https://doi.org/10.3390/computation12060118
Thakur N, Patel KA, Poon A, Shah R, Azizi N, Han C. Investigation of the Global Fear Associated with COVID-19 Using Subjectivity Analysis and Deep Learning. Computation. 2024; 12(6):118. https://doi.org/10.3390/computation12060118
Chicago/Turabian StyleThakur, Nirmalya, Kesha A. Patel, Audrey Poon, Rishika Shah, Nazif Azizi, and Changhee Han. 2024. "Investigation of the Global Fear Associated with COVID-19 Using Subjectivity Analysis and Deep Learning" Computation 12, no. 6: 118. https://doi.org/10.3390/computation12060118
APA StyleThakur, N., Patel, K. A., Poon, A., Shah, R., Azizi, N., & Han, C. (2024). Investigation of the Global Fear Associated with COVID-19 Using Subjectivity Analysis and Deep Learning. Computation, 12(6), 118. https://doi.org/10.3390/computation12060118







