Virtual Interactive Environment for Low-Cost Treatment of Mechanical Strabismus and Amblyopia
Abstract
1. Introduction
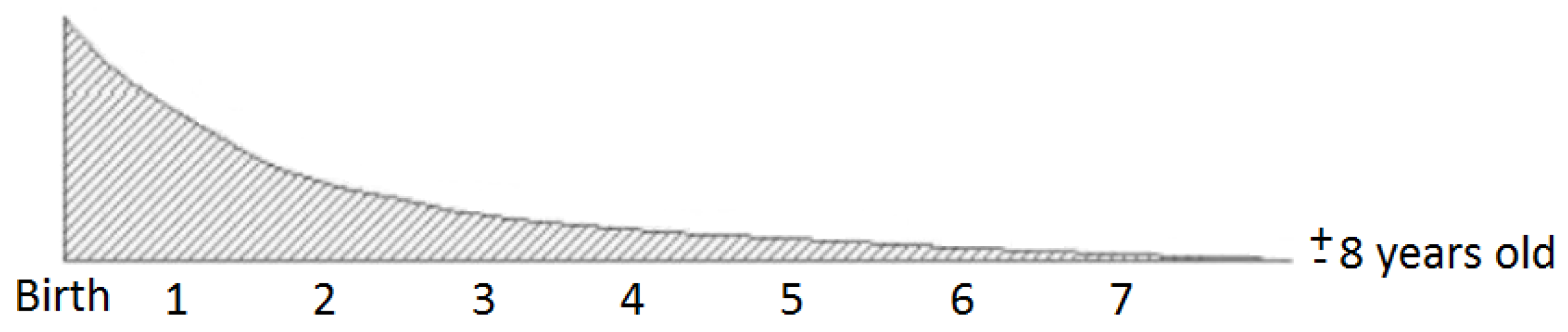
2. Strabismus
3. Amblyopia
4. Strabismus Treatment
4.1. Strabismus Surgical Treatment
4.2. Non-Surgical Treatment for Strabismus
4.2.1. Miotics
4.2.2. Pleoptica
4.2.3. Video Games
5. Interactive Virtual Environment for the Treatment of Mechanical Structure and Ambliopia
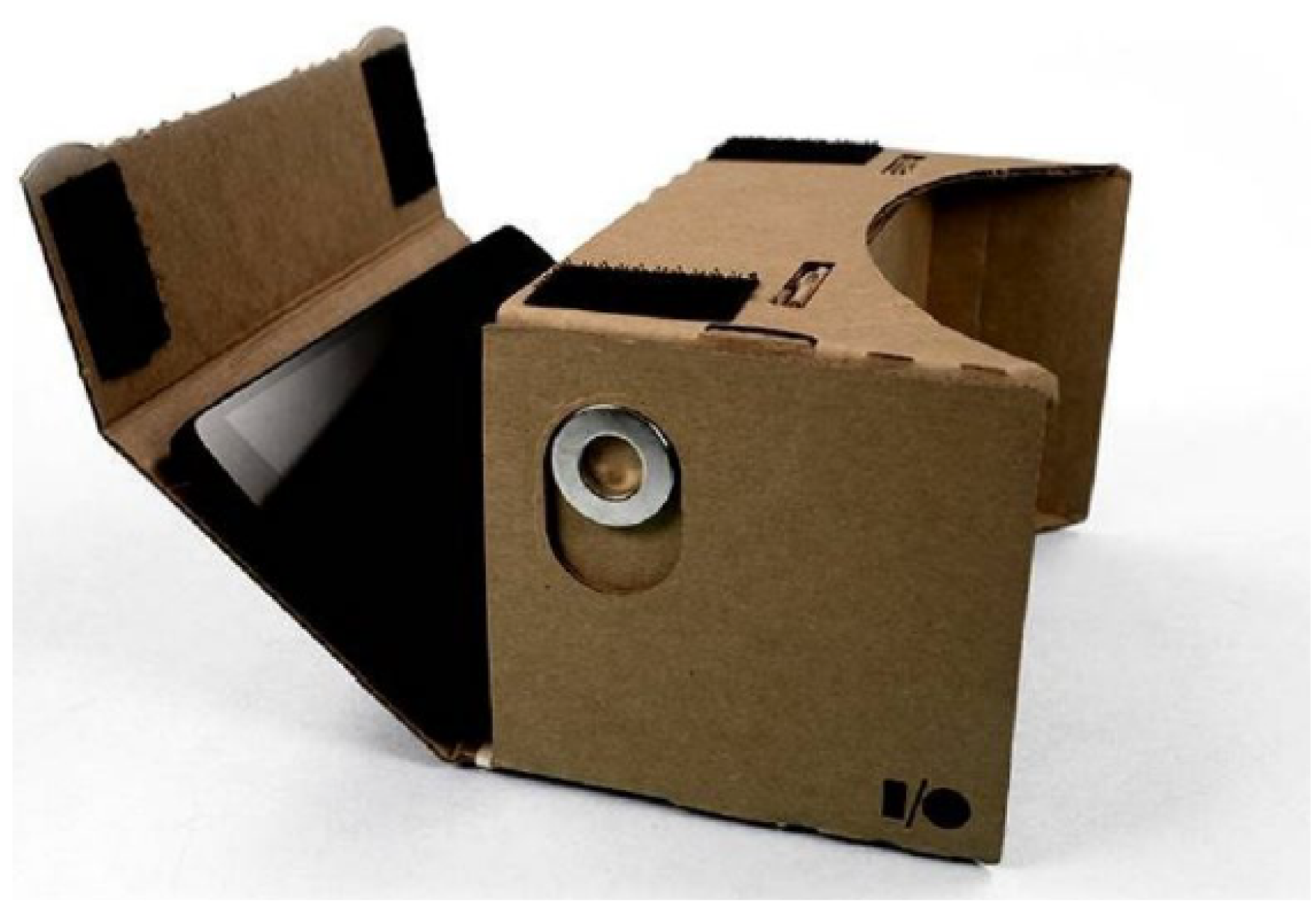
5.1. Virtual Reality and Google Cardboard
Google Cardboard
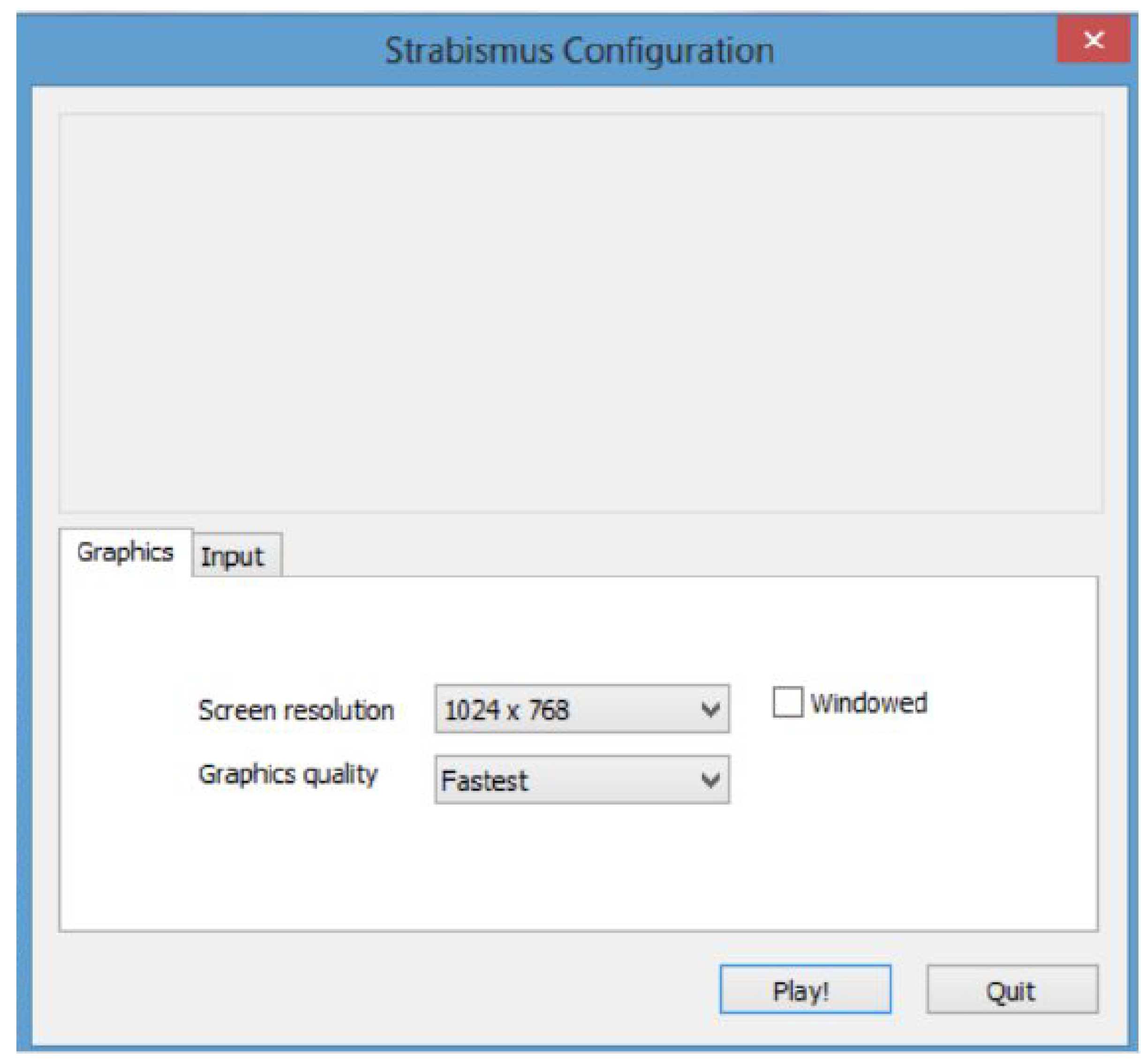
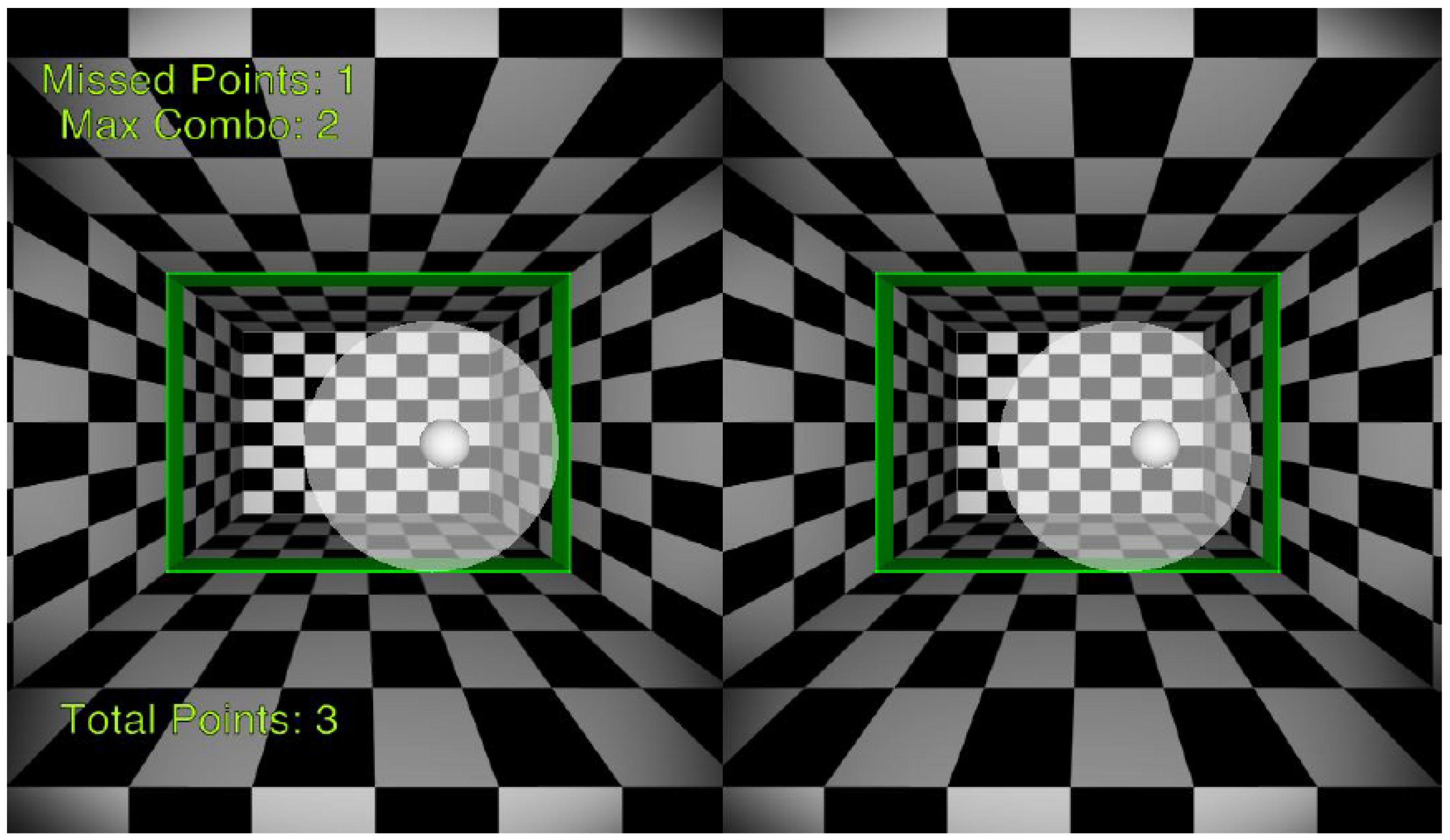
5.2. The Games Developed for the Treatment
- Easy-to-handle activities to reach all ages, especially those of advanced age who have difficulty assimilating commands and understanding activities.
- Colorful activities to stimulate visual activity and attract attention.
- Activities that include a score regarding patient time and which are challenging for the patient to try to overcome each section.
- Educational activities without the use of scenarios that may deviate from the characteristics of the patient, especially in regard to age group.
6. Methodology
6.1. Description of the Virtual Environment
6.2. Adaptation of the Virtual Environment
6.3. Virtual Environmental Activity
6.4. Relaxation of the Virtual Environment
7. Results
8. Discussion
9. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Von Noorden, G.K.; Campos, E.C. Binocular Vision and Ocular Motility: Theory and Management of Strabismus; Mosby: St. Louis, MO, USA, 1990; Volume 6. [Google Scholar]
- Rosenwasser, G.O.; Nicholson, W.J. Introduction to Eye Banking: A Handbook and Atlas: A Guide to Eye Bank Techniques, Corneal Evaluation, and Grading; The Authors: Hershey, PA, USA, 2003. [Google Scholar]
- Helveston, E.M. Surgical Management of Strabismus; Wayenborgh: Amsterdam, The Netherlands, 2005. [Google Scholar]
- Von Noorden, G.K.; Helveston, E.M. Strabismus: A Decision Making Approach; Mosby: St. Louis, MO, USA, 1994. [Google Scholar]
- Ruttum, M.; von Noorden, G. Orbital and Facial Anthropometry in a and v Pattern Strabismus; Strabismus II: New York, NY, USA, 1984; p. 363. [Google Scholar]
- Ejzenbaum, F.; Goldchmit, M.; Souza-Dias, C.; Gaal Vadas, M. Correçäo cirúrgica do estrabismo horizontal em portadores de alta miopia. Arq. Bras. Oftalmol. 2001, 64, 97–101. [Google Scholar] [CrossRef]
- Kanski, J.J. Clinical Ophtalmology, A Pocket Textebook Atlas, 2nd ed.; Thieme: Stuttgart, Germany, 2006. [Google Scholar]
- Kushner, B.J. Functional amblyopia associated with abnormalities of the optic nerve. Arch. Ophthalmol. 1984, 102, 683–685. [Google Scholar] [CrossRef] [PubMed]
- Black, J.M.; Hess, R.F.; Cooperstock, J.R.; To, L.; Thompson, B. The measurement and treatment of suppression in amblyopia. J. Vis. Exp. JoVE 2012, 70. [Google Scholar] [CrossRef] [PubMed]
- Procianoy, E.; Procianoy, L.; Procianoy, F. Resultados do tratamento da ambliopia com levodopa combinada à oclusão. Arq. Bras. Oftalmol. 2004, 67, 717–720. [Google Scholar] [CrossRef]
- Sasaki, Y.; Nanez, J.E.; Watanabe, T. Advances in visual perceptual learning and plasticity. Nat. Rev. Neurosci. 2010, 11, 53–60. [Google Scholar] [CrossRef] [PubMed]
- Hess, R.; Mansouri, B.; Thompson, B. Restoration of binocular vision in amblyopia. Strabismus 2011, 19, 110–118. [Google Scholar] [CrossRef] [PubMed]
- Tour, R.L. Nonsurgical treatment of convergent strabismus. Calif. Med. 1959, 90, 429. [Google Scholar] [PubMed]
- Von Noorden, G.K.; Almeida, H.C. The History of Strabismology; Schmidt, G., Ed.; Wayenborgh: Amsterdam, The Netherlands, 2002. [Google Scholar]
- Velter, D.E. Thérapeutique Chirurgicale Ophtalmologique; Masson: Hongkong, China, 1950. [Google Scholar]
- Loudon, S. Improvement of Therapy for Amblyopia; Erasmus MC, University Medical Center Rotterdam: Rotterdam, The Netherlands, 2007. [Google Scholar]
- Wheatstone, C. Contributions to the physiology of vision—Part the first. Philos. Trans. R. Soc. Lond. 1838, 128, 371–394. [Google Scholar] [CrossRef]
- Koskinen, K. Experiments with the use of miotics in convergent strabismus. Acta Ophthalmol. 1957, 35, 521–527. [Google Scholar] [CrossRef]
- Abraham, S.V. The use of miotics in the treatment of convergent strabismus and anisometropia: A preliminary report. Am. J. Ophthalmol. 1949, 32, 233–240. [Google Scholar] [CrossRef]
- Achtman, R.L.; Green, C.S.; Bavelier, D. Video games as a tool to train visual skills. Restor. Neurol. Neurosci. 2008, 26, 435–446. [Google Scholar] [PubMed]
- Bavelier, D.; Green, C.S.; Pouget, A. Brain plasticity through the life span: Learning to learn and action video games. Annu. Rev. Neurosci. 2012, 35, 391–416. [Google Scholar] [CrossRef] [PubMed]
- Green, C.S.; Bavelier, D. Learning, attentional control, and action video games. Curr. Biol. 2012, 22, 197–206. [Google Scholar] [CrossRef] [PubMed]
- Li, R.; Polat, U.; Scalzo, F.; Bavelier, D. Reducing backward masking through action game training. J. Vis. 2010, 10, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Li, R.W.; Ngo, C.; Nguyen, J.; Levi, D.M. Video-game play induces plasticity in the visual system of adults with amblyopia. PLoS Biol. 2011, 9. [Google Scholar] [CrossRef] [PubMed]
- Li, R.W.; Ngo, C.; Nguyen, J.; Levi, D.M. Relieving the attentional blink in the amblyopic brain with video games. Sci. Rep. 2015, 8483, e1001135. [Google Scholar] [CrossRef] [PubMed]
- Hussain, Z.; Astle, A.T.; Webb, B.S.; McGraw, P.V. The challenges of developing a contrast-based video game for treatment of amblyopia. Front. Psychol. 2014, 5, 1210. [Google Scholar] [CrossRef] [PubMed]
- Baker, D.H.; Meese, T.S.; Hess, R.F. Contrast masking in strabismic amblyopia: Attenuation, noise, interocular suppression and binocular summation. Vis. Res. 2008, 48, 1625–1640. [Google Scholar] [CrossRef] [PubMed]
- Bi, H.; Zhang, B.; Tao, X.; Harwerth, R.S.; Smith, E.L., III; Chino, Y.M. Neuronal responses in visual area v2 (v2) of macaque monkeys with strabismic amblyopia. Cereb. Cortex 2011, 21, 2033–2045. [Google Scholar] [CrossRef] [PubMed]
- Ding, J.; Klein, S.A.; Levi, D.M. Binocular combination in abnormal binocular vision. J. Vis. 2013, 13, 14. [Google Scholar] [CrossRef] [PubMed]
- Ding, J.; Levi, D.M. Rebalancing binocular vision in amblyopia. ophthalmic physiology optics. J. Br. Coll. Ophthalmic Opt. 2014, 34, 199–213. [Google Scholar] [CrossRef] [PubMed]
- Hess, R.F.; Thompson, B.; Baker, D.H. Binocular vision in amblyopia: Structure, suppression and plasticity. Ophthalmic Physiol. Opt. 2014, 34, 146–162. [Google Scholar] [CrossRef] [PubMed]
- Maehara, G.; Thompson, B.; Mansouri, B.; Farivar, R.; Hess, R.F. The perceptual consequences of interocular suppression in amblyopia. Investig. Ophthalmol. Vis. Sci. 2011, 52, 9011–9017. [Google Scholar] [CrossRef] [PubMed]
- Zhang, P.; Bobier, W.R.; To, L.; Cooperstock, J. An ipod treatment of amblyopia: An updated binocular approach. Optometry 2012, 83, 87–94. [Google Scholar]
- Li, J.; Thompson, B.; Deng, D.; Chan, L.Y.; Yu, M.; Hess, R.F. Dichoptic training enables the adult amblyopic brain to learn. Curr. Biol. 2013, 23, 308–309. [Google Scholar] [CrossRef] [PubMed]
- To, L.; Thompson, B.; Blum, J.R.; Maehara, G.; Hess, R.F.; Cooperstock, J.R. A game platform for treatment of amblyopia. IEEE Trans. Neural Syst. Rehabil. Eng. 2011, 19, 280–289. [Google Scholar] [PubMed]
- Gargantini, A.; Terzi, F.; Zambelli, M.; Bonfanti, S. A low-cost virtual reality game for amblyopia rehabilitation. In Proceedings of the 3rd 2015 Workshop on ICTs for Improving Patients Rehabilitation Research Techniques, Lisbon, Portugal, 1–2 October 2015; pp. 81–84. [Google Scholar]
- Nallour Raveendran, R. Fixational Eye Movements in Strabismic Amblyopia. Master’s Thesis, University of Waterloo, Waterloo, ON, Canada, 2013. [Google Scholar]
- Craig, A.B.; Sherman, W.R.; Will, J.D. Developing Virtual Reality Applications: Foundations of Effective Design; Morgan Kaufmann: Burlington, MA, USA, 2009. [Google Scholar]
- Lee, P.-W.; Wang, H.-Y.; Tung, Y.-C.; Lin, J.-W.; Valstar, A. Transection: Hand-based interaction for playing a game within a virtual reality game. In Proceedings of the 33rd Annual ACM Conference Extended Abstracts on Human Factors in Computing Systems, Seoul, Korea, 18–23 April 2015; pp. 73–76. [Google Scholar]
- Goradia, I.; Doshi, J.; Kurup, L. A review paper on oculus rift & project morpheus. Int. J. Curr. Eng. Technol. 2014, 4, 3196–3200. [Google Scholar]
- Google Cardboard. Available online: https://cardboard.withgoogle.com/ (accessed on 12 July 2018).
- MacIsaac, D. (Ed.) Google cardboard: A virtual reality headset for $10? Phys. Teach. 2015, 53, 125. [Google Scholar]
- Engadget. The New Oculus Rift Costs $350 and This Is What It’s Like. Available online: http://www.engadget.com/2014/03/19/oculus-rift-development-kit-2/ (accessed on 12 July 2018).
- Saraiva, A.A.; Fonseca Ferreira, N.M.; Soares, S.; Valente, A. Application of virtual reality for the treatment of Strabismus and Amblyopia. In Proceedings of the 6th International Conference on Serious Games and Applications for Health (IEEE SeGAH 2018), Vienna, Austria, 16–8 May 2018; pp. 1–7. [Google Scholar] [CrossRef]
- Laver, K.; George, S.; Thomas, S.; Deutsch, J.E.; Crotty, M. Virtual reality for stroke rehabilitation. Stroke 2012, 43, 20–21. [Google Scholar] [CrossRef]
- McMahan, R.P.; Bowman, D.A.; Zielinski, D.J.; Brady, R.B. Evaluating display fidelity and interaction fidelity in a virtual reality game. IEEE Trans. Vis. Comput. Graph. 2012, 18, 626–633. [Google Scholar] [CrossRef] [PubMed]
- Zeigelboim, B.S.; de Souza, S.D.; Mengelberg, H.; Teive, H.A.G.; Liberalesso, P.B.N. Reabilitação vestibular com realidade virtual na ataxia espinocerebelar. Audiol. Commun. Res. 2013, 18, 143–147. [Google Scholar] [CrossRef]
- Purdue University. Virtual Nose May Reduce Simulator Sickness in Video Games. Available online: http://www.purdue.edu/newsroom/releases/2015/Q1/virtual-nose-may-reduce-simulator-sickness-in-video-games.html (accessed on 12 July 2018).
- Foss, M.L.; Keteyian, S.J.; Taranto, G. Fox: Bases Fisiológicas do Exercício e Do Esporte; Guanabara Koogan: Rio de Janeiro, Brazil, 2000. [Google Scholar]
- Almeida, T.T.D.; Jabur, M.N. Mitos e verdades sobre flexibilidade: Reflexões sobre o treinamento de flexibilidade na saúde dos seres humanos. Motricidade 2007, 3, 337–344. [Google Scholar] [CrossRef]
- Archer, S.M.; Archer, X.N.; Helveston, E.M. Strabismus in infancy. Ophthalmology 1989, 96, 133–137. [Google Scholar] [CrossRef]




| Patient | Age | Sex | No. of Sessions | Success |
|---|---|---|---|---|
| 1 | 8 | M | 10 | Yes |
| 2 | 18 | F | 10 | Yes |
| 3 | 12 | F | 10 | Yes |
| 4 | 19 | F | 10 | Yes |
| 5 | 16 | F | 10 | Yes |
| 6 | 16 | F | 10 | Yes |
| 7 | 9 | F | 10 | Yes |
| 8 | 27 | M | 10 | Yes |
| 9 | 32 | F | 10 | Yes |
| 10 | 24 | F | 10 | Yes |
| 11 | 20 | F | 10 | Yes |
| 12 | 14 | F | 10 | Yes |
| 13 | 35 | F | 10 | Yes |
| 14 | 8 | F | 10 | Yes |
| 15 | 8 | F | 10 | Yes |
| 16 | 36 | F | 10 | Yes |
| 17 | 18 | F | 20 | Yes |
| 18 | 09 | F | 10 | No |
| 19 | 24 | M | 10 | Yes |
| 20 | 18 | F | 10 | Yes |
| 21 | 8 | F | 20 | Yes |
| 22 | 6 | F | 6 | Yes |
| 23 | 13 | F | 10 | Yes |
| 24 | 20 | M | 10 | Yes |
| 25 | 32 | F | 10 | Yes |
| 26 | 14 | M | 10 | Yes |
| 27 | 21 | F | 10 | Yes |
| 28 | 17 | F | 10 | Yes |
| 29 | 33 | F | 10 | Yes |
| 30 | 8 | F | 10 | Yes |
| 31 | 18 | F | 10 | Yes |
| 32 | 22 | F | 6 | Yes |
| 33 | 16 | M | 10 | Yes |
| 34 | 18 | F | 10 | Yes |
| 35 | 12 | F | 10 | Yes |
| 36 | 16 | M | 10 | Yes |
| 37 | 27 | M | 10 | Yes |
| 38 | 8 | F | 10 | Yes |
| 39 | 21 | F | 10 | Yes |
| 40 | 27 | F | 10 | Yes |
| 41 | 39 | F | 10 | Yes |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Saraiva, A.A.; Barros, M.P.; Nogueira, A.T.; Fonseca Ferreira, N.M.; Valente, A. Virtual Interactive Environment for Low-Cost Treatment of Mechanical Strabismus and Amblyopia. Information 2018, 9, 175. https://doi.org/10.3390/info9070175
Saraiva AA, Barros MP, Nogueira AT, Fonseca Ferreira NM, Valente A. Virtual Interactive Environment for Low-Cost Treatment of Mechanical Strabismus and Amblyopia. Information. 2018; 9(7):175. https://doi.org/10.3390/info9070175
Chicago/Turabian StyleSaraiva, Aratã Andrade, Matheus Pereira Barros, Alexandre Tolstenko Nogueira, N. M. Fonseca Ferreira, and Antonio Valente. 2018. "Virtual Interactive Environment for Low-Cost Treatment of Mechanical Strabismus and Amblyopia" Information 9, no. 7: 175. https://doi.org/10.3390/info9070175
APA StyleSaraiva, A. A., Barros, M. P., Nogueira, A. T., Fonseca Ferreira, N. M., & Valente, A. (2018). Virtual Interactive Environment for Low-Cost Treatment of Mechanical Strabismus and Amblyopia. Information, 9(7), 175. https://doi.org/10.3390/info9070175







