Abstract
MHealth strategies have been used in various health areas, and mobile apps have been used in the context of health self-management. They can be considered an adjuvant intervention in oral health literacy, mainly for people with special health needs. Thus, the aim of this study was to identify the improvement of oral health literacy in patients with special needs when using digital platforms. A systematic literature review, based on the Joanna Briggs Institute (JBI) guidelines, was the main research method employed in this study. A search was undertaken in PubMed/MEDLINE and Cochrane Central Register of Controlled Trials (CENTRAL) databases, according to the relevant Mesh descriptors, their synonyms, and free terms (Entry Terms). Studies published between the years 2012 and 2023 were included. Two researchers independently assessed the quality of the included studies by completing the Newcastle–Ottawa Quality Assessment Scale questionnaire. The analysis corpus comprised 5 articles among the 402 articles selected after applying the inclusion/exclusion criteria (k = 0.97). The evidence from the considered articles is consensual regarding the effectiveness of using new technologies and innovations in promoting oral health literacy in patients with special health needs. The interventions were based on using the Illustration Reinforcement Communication System, inspired by the Picture Exchange Communication System, Nintendo® Wii™ TV, virtual reality, smartphones, with software applications to read messages sent, Audio Tactile Performance technique, and Art package. One study had a low-quality assessment, and four had a high quality. The evidence from the articles included in this systematic review is consistent regarding the effectiveness of using new technologies and innovations in promoting oral health literacy in patients with special health needs.
1. Introduction
The World Health Organization (WHO) estimates that around 16% of the population of any country has some disability (around 1.3 billion people; 1 in 6 people). It is estimated that around 5% are people with mental disabilities, 2% with physical disabilities, 1.5% with hearing impairment, 0.5% with visual impairment, and 1% with multiple disabilities [1]. People with special needs encounter challenges such as physical barriers, social inclusion, educational adaptation, daily activities, and personal hygiene [2]. Encouraging healthy living and autonomy must be developed, using adaptations and alternatives. Therefore, maintaining adequate oral hygiene can be difficult for these individuals [2,3].
Chronic diseases have a pronounced worldwide prevalence and are an evident public health concern. Moreover, it was proposed that diseases from the oral cavity and systemic diseases have a bidirectional association [4,5,6,7,8]. While evidence of this bidirectional link is robust in diseases that limit oral self-care (either physical or cognitive incapacity), the association of oral diseases with other chronic noncommunicable diseases (NCDs) has increased, still without the proper consistency.
However, there is a need for programs that can develop methods of motivation and oral health literacy adapted for this part of the population so lacking in information and alternatives to adapt to their reality, establishing a routine of prevention, guidance, and knowledge about oral hygiene [9]. The development of oral health education programs and strategies is of utmost importance for patients with special needs, aiming to reduce the rates of tooth decay and periodontal disease rates, which are generally prevalent [2,3,9]. Adaptations and appropriate care can generate motivation for health and constitute autonomy for these patients. This encouragement of independence and self-care contributes to oral health and general health, which is the motivation and benefit of being healthy [2,3,9,10,11]. Thus, aiming to promote increased knowledge, oral health education programs help reduce risk factors for oral diseases, promoting the control of dental biofilm and the consumption of a healthy diet [10]. A significant barrier to preventing major oral diseases would be the lack of knowledge, inadequate eating habits, and poor oral hygiene, which are the main factors for the development of tooth decay and periodontal disease.
Oral health literacy strategies aim to increase knowledge and encourage behavior, self-care, and diet changes [12]. However, acquiring knowledge does not mean an immediate improvement in practices and attitudes. The complement includes education and prevention for oral health to be applied periodically [9,10,11,12]. Studies reveal that many people with special needs have never had adequate guidance on brushing and hygiene techniques, which is a worrying fact, as these individuals generally need special help or adaptations to learn how to perform their hygiene and, for example, adequately use a brush or dental floss [3,9,10,11]. Faced with the new global scenario, with the pandemic and social isolation, the internet has become an environment with an essential role in building connections, as well as bringing people together and spreading knowledge for the population, especially for those with some special needs [13]. When correctly used, it becomes a favorable way for educational and cultural activities [10,11], as the ease of access and sharing of information allows a large portion of the population to be reached without the need to travel to a specific location [12,13]. Thereby, important and safe information about oral and general health care can be disseminated through the virtual environment. On the other hand, the work can become more comprehensive and exhaustive, as new content is needed with a certain frequency and the audience becomes heterogeneous, given the scope and diversity of the internet environment [13,14].
Social and research networks provide an environment for searching for health information. Data show that 80% of searches and browsing activities on the internet are directed toward health-related knowledge. The YouTube platform is the most popular platform for patients to consult to find health-related information, including information on oral health. However, not all information contained on YouTube is true or accurate, which may have a negative impact on the population’s health [15]. Much of the dental content is published on digital platforms (Google, Facebook, YouTube, and Instagram), which may influence positively and/or negatively the patient’s vision, with reliable and unreliable information being available, which can lead to misunderstanding by the population. For this reason, it is essential to review these contents and check their reliability [16].
Also, the application of digital technologies, such as augmented reality, virtual reality, and mixed reality, has led to advances in oral health. These applications permit the development of specific oral health literacy strategies focused on the most vulnerable social risk groups [17].
Oral diseases affect almost half the world’s population, causing a substantial economic burden. Oral health promotion is one of the most cost-effective methods to overcome this problem. Digital media can play a fundamental role in reducing this burden, providing a broader platform to reach the entire population, regardless of their characteristics, and even in areas where oral health services are lacking [17,18]. Although oral health literacy is widely debated and has many heterogeneous conceptualizations, people with special health needs have often been neglected [18]. There are many different approaches to preventing oral disease, and the most effective method in terms of costs is health promotion and education [19]. As access to digital media continues to expand, it will increasingly serve as a valuable health resource in environments lacking specialized health knowledge. They are an alternative platform that can help reach people with special health needs, promoting greater oral health literacy. Evidence reveals that interactive digital interventions increase knowledge about oral health and change behaviors, constituting one of the main approaches to promoting oral health literacy [20].
Thus, within this context, this study aimed to systematically review the use of new technologies and digital innovations to improve health literacy in patients with special needs and in vulnerable communities.
2. Material and Methods
This systematic review followed the guidelines of the Cochrane Database of Systematic Reviews. It was written using the PRISMA criteria (Preferred Reporting Items for Systematic Reviews and Meta-analyses) [21,22,23,24]. It was registered at PROSPERO (CRD42023434469). The research question was developed based on the PICO (Participants, Intervention, Comparison, and Outcomes) strategy (Table 1): “Does the use of new technologies and digital innovations improve health literacy in patients with special needs and vulnerable communities?”.

Table 1.
Description of the acronym PICO.
2.1. Search and Selection of Articles
The articles were searched and selected through the PubMed/MEDLINE and Cochrane Central Register of Controlled Trials (CENTRAL). The following keywords were used: visually [All Fields] AND impaired [All Fields]; “hearing loss” [MeSH Terms] OR hearing-impaired [Text Word]; “autistic disorder” [MeSH Terms] OR autism [Text Word] Or Autism Spectrum Disorder; “cerebral palsy” [MeSH Terms] OR cerebral palsy [Text Word]; new [All Fields] AND (“technology” [MeSH Terms] OR technologies [Text Word]); app [All Fields]; “literacy” [MeSH Terms] OR literacy [Text Word]; and “oral health” [MeSH Terms] OR oral health [Text Word]. These were used as MeSH or DeCS terms, together with their synonyms, and also as free terms (Entry Terms). The search keys used were digital media OR eHealth OR MHealth OR mobile phones OR cell phones OR MHealth application OR telemedicine OR television, as well as videos AND oral health education OR oral health OR oral health promotion OR oral health literacy OR oral health knowledge AND special needs.
2.2. Inclusion and Exclusion Criteria
Studies published in English between 2012 and 2023 that were related to the criteria established in the PICO strategy and that have the full text available were included. Regarding the design of the studies, experimental, quasi-experimental, and cross-sectional analytical studies and controlled, randomized clinical trials, and randomized controlled exploratory studies were included.
Systematic, narrative, comprehensive, or critical reviews were excluded. Also excluded were articles published in another language; articles that included a population without special needs; and articles that used tools other than new technologies and digital innovations to achieve oral health literacy.
2.3. Selection of Studies
Two reviewers (LBC and NJV) selected the articles. The review was carried out in two phases: initially, the titles and abstracts were read, followed by the collection and evaluation of the complete articles based on the review criteria. The remnant studies were evaluated by two independent reviewers (LBC and NJV); a third evaluator was invited to make the final decision in case of any disagreement (PC). Identified references were evaluated, and duplicate studies were removed. Then, the titles and abstracts were analyzed according to the established inclusion and exclusion criteria to identify potentially eligible studies. Eligible studies were read in full to confirm their inclusion and analysis. Secondary articles and articles without comparison groups and/or without recording data at baseline vs. post-intervention were also excluded during the screening phase.
2.4. Data Extraction, Synthesis, and Quality Assessment
Data extraction from the final articles was conducted based on a data extraction form, considering the following: the author, article name, year/country of publication, study design, inclusion criteria, exclusion criteria, participants, and main results. The extracted data were summarized, including the collection, combination, and summary of the study’s results.
Two researchers (LBC and NJV) independently assessed the quality of the included studies by completing the Newcastle–Ottawa Quality Assessment Scale questionnaire. Thus, quality assessment scales for each selected study were applied to the full text of each article identified for inclusion in the review as part of the data extraction process. It provides a rating system ranging from 0 to 9 stars, with scores equal to or greater than 7 considered high quality and scores less than 7 regarded as low quality.
3. Results
In the first phase, 501 articles were identified, and the duplicated studies were removed (n = 99). In this way, 402 were selected, of which 299 were excluded by the inclusion/exclusion criteria when reading the title and abstract (k = 0.96). Thus, 103 articles were transferred to the next phase and were subject to a full-text reading. After reading, 98 were excluded, according to the following criteria: secondary articles (n = 39) and articles without comparison groups and/or without recording data at baseline vs. post-intervention (n = 59). Therefore, five articles [25,26,27,28,29] were included in this systematic review (k = 0.97) (Figure 1).
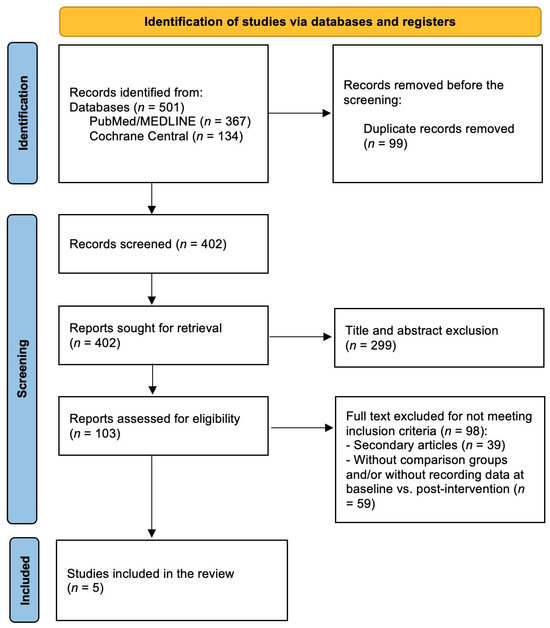
Figure 1.
Screening and inclusion of studies.
Studies Characteristics
Table 2, Table 3 and Table 4 present all the details of the articles included. Table 5 shows the quality assessment of the five articles included; only one [25] was low quality.

Table 2.
Identification of final articles.

Table 3.
Summary of results from included studies.

Table 4.
Drop-out, follow-up, summarized outcome(s), and problems and challenges found in the studies included.

Table 5.
Quality assessment for the included studies.
4. Discussion
The main objective of this study was to identify the improvement of oral health literacy in patients with special needs and vulnerable communities using new technologies and innovations. Five articles were considered in the systematic review, presenting con-sensual views on the effectiveness of new technologies and innovations in promoting oral health literacy in patients with special health needs. As the focus of health care has shifted from treating disease to preserving health (preventive approach), health promotion has emerged as a social issue that affects individuals in general and health care professionals, whatever their field of practice.
In recent decades, there has been an increase in the use of the internet and digital devices, which has led to their integration into oral health care [18]. Veiga et al. [30] showed that using technological resources in health is essential. They improve communication and the reception of new information, permit more accessible communication, and, for leisure, improve feelings of loneliness and/or social isolation. Thus, eHealth was defined as health services and information transmitted through electronic and digital means. The eHealth conceptual model adequately integrates technology and health care, the benefits of which include increasing the effectiveness and accessibility of medical and dental services, for example, the implementation of various mobile health applications. With the help of the internet, people who face difficulties in accessing medical services can obtain health information and receive assistance to manage their oral health [31,32,33]. This makes oral health care more accessible, especially for people living in remote areas or with mobility problems.
Additionally, eHealth technologies help reduce wait times, increase patient engagement in managing their oral health, and improve overall health outcomes [2]. Currently, the internet is considered an essential source of health information. People who have difficulty obtaining medical and dental care can access health information online and receive assistance in managing their health condition. However, obtaining health-related information on the internet requires specific skills and health literacy, such as reading, understanding, and evaluating the information found, particularly on the part of people with special health needs [2,3,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30]. Thus, the concept of eHealth Literacy emerged, defined as the ability to search, find, understand, and evaluate health information from electronic sources and apply the knowledge acquired to address or solve a health problem [33].
The studies included in the present systematic review agreed that, in the field of oral health, the concept of health literacy has gained significant importance and has been integrated into oral health literacy, encompassing various tools and resources. Research has shown that individual and systemic factors influence oral health literacy. Personal factors such as education level, socioeconomic and cultural conditions, proficiency, and health literacy can affect a person’s ability to understand and use oral health information, whereas systemic factors include the complexity of access to health care and health systems. According to the values obtained after interventions using new technologies and innovations, all studies showed a significant increase in patients’ oral health literacy with special health needs. In the study ID 5 by Sharifard et al. [29], the effectiveness of the ATP (audio-tactile performance) program for children/adolescents with visual impairments was demonstrated. Audio: verbal oral health education was offered to the target population on the importance of preventing oral diseases such as tooth decay and gum health. This program contained essential instructions for daily oral hygiene, with a verbal demonstration of techniques. The Art package consisted of an electronic game for oral health education based on music that complemented the ATP. Likewise, guidance/teaching to mothers via telephone completed the other interventions.
The study ID 1 by Pai Khot et al. [25] included patients aged between 7 and 18 years old with ASD. The PAIR communication system, inspired by the Picture Exchange Communication System (PECS), was a modified version of the same that is based on descriptive data. It was a new pictorial system based on behavior, created to develop communication skills and educate children with special health needs in terms of oral hygiene practices, serving as a link with everyday practices. The PAIR intervention is based on the concepts of applied behavioral analysis and uses differentiated teaching and different teaching, reinforcement, and chaining strategies. Furthermore, this system uses pictorial differentiation of oral hygiene aids and structured illustrations, demonstrating oral hygiene tasks in different patterns with increased oral health literacy. This new digital technique contained illustrations in a sequence of actions necessary to maintain oral hygiene. The steps included were the following: step 1 was the illustration and identification of images by children/adolescents; step 2 was the illustrated object given to the children/adolescents to choose the correct image; step 3 was that children/adolescents identify the correct and incorrect illustrations presented; and step 4 was that children/adolescents produced a sentence following the sequence of images.
In the study ID 2 by Álvareza et al. [26], the intervention was based on exercises with a Nintendo® Wii™ TV and a Wii balance board in an experimental group. In contrast, the control group continued with their normal daily activities. The games applied on the Wii balance board challenge the stability of children with trisomy 21 by balancing their body weight, as requested by the game, causing a sensory and motor stimulus, which led the experimental group, after the intervention, to improve their postural control, resulting in greater ease in improving your oral hygiene. The data provided in this study demonstrated that when using an intervention based on the Wii balance board with appropriate adaptations to the characteristics of each child, children with trisomy 21 increased their knowledge about oral health and adopted behaviors that are more conducive to good oral health. One study by Genaro et al. [34] found seeding results using virtual reality, where there was a significant increase in good oral hygiene practices. In the study ID 3 by Khalil et al. [27], oral health literacy was a predictive factor for self-efficacy in oral health throughout each period of interventions, using smartphones with software applications for elderly people to read oral health messages. Likewise, Carli et al. [28] found significant improvements between baseline and post-intervention values, that is, applying an oral health disease prevention program on personalized digital media, which significantly improved clinical parameters and patient behaviors.
As a limitation of this study, the low number of studies directly included that evaluated patients with special needs and technologies focused on oral health can be pointed out; moreover, it is possible to consider that the number of patients included in some of the articles was low and should be increased in future studies.
5. Conclusions
The results reveal that one of the strategies with the potential to promote more oral health literacy in people with special health needs is the use of new technologies and innovations. However, this study clearly has its limitations. The most obvious is that few studies were found in the literature, with the majority focusing on promoting health literacy in general. Many studies also do not have comparator elements, that is, pre- and post-assessment, mainly with a cross-sectional focus. Therefore, it is suggested that a primary, cluster-randomized controlled study be carried out as future research.
The result addresses the overall research objective and its practical implications. This is justified by consistent evidence from the articles in this systematic review regarding the effectiveness of using new technologies and innovations in promoting oral health literacy in patients with special health needs. It was found that the interventions were based on the use of the Illustration Reinforcement Communication System, inspired by the Picture Exchange Communication System, Nintendo® Wii™ TV, virtual reality, smartphones, with software applications to read sent messages, Audio Tactile Performance technique (tactile-audio performance) and Art package (electronic game). Even though the reported results were enlightening, it is desirable to carry out additional studies to confirm the effectiveness of using new technologies and innovations to promote oral health literacy in patients with special health needs; in addition, studies analyzing electronically the health or any urgent care necessities for this group should be better standardized and developed. This will enable an intervention that is more in line with each patient’s difficulties, considering their individual and clinical characteristics.
Author Contributions
L.B.C., P.C. (Patrícia Couto), P.C. (Patrícia Correia), and N.J.V. were responsible for the conceptualization and design of the project. L.B.C., P.C. (Patrícia Couto), P.C. (Patrícia Correia), P.C.L., J.C.H.F., G.V.O.F., and N.J.V. were responsible for the data collection. L.B.C., P.C. (Patrícia Couto), P.C. (Patrícia Correia), P.C.L., J.C.H.F., G.V.O.F., and N.J.V. were responsible for the analysis and interpretation of data. L.B.C., P.C. (Patrícia Couto), P.C. (Patrícia Correia), P.C.L., J.C.H.F., G.V.O.F., and N.J.V. participated in the investigation and data curation, drafted the manuscript, and made contributions to the revising of the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by National Funds through FCT—Fundação para a Ciência e a Tecnologia, I.P., under the project UIDP/04279/2020.
Data Availability Statement
The data used to generate and support this study’s findings are available from the corresponding author upon request.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- World Health Organization. Available online: https://www.who.int/health-topics/disability#tab=tab_1 (accessed on 22 August 2024).
- Silveira, E.R.; Schardosim, R.L.; Goettems, L.M.; Azevedo, S.M.; Dias, T.D. Oral health education aimed at the visually impaired. Rev. Bras. Educ. Spec. 2015, 21, 289–298. [Google Scholar] [CrossRef]
- Freitas-Fernandes, L.B.; Novaes, A.B., Jr.; Feitosa, A.C.; Novaes, A.B. Effectiveness of an oral hygiene program for Brazilian orphans. Braz. Dent. J. 2002, 13, 44–48. [Google Scholar] [PubMed]
- Meurman, J.H.; Bascones-Martinez, A. Oral infections and systemic health—More than just links to cardiovascular diseases. Oral. Health Prev. Dent. 2021, 19, 441–448. [Google Scholar] [PubMed]
- Tavares, L.T.R.; Saavedra-Silva, M.; Marcos, J.F.L.; Veiga, N.J.; Castilho, R.M.; Fernandes, G.V.O. Blood and salivary inflammatory biomarkers profile in patients with chronic kidney disease and periodontal disease: A systematic review. Diseases 2022, 10, 12. [Google Scholar] [CrossRef]
- Tonetti, M.S.; Jepsen, S.; Jin, L.; Otomo-Corgel, J. Impact of the global burden of periodontal diseases on health, nutrition and wellbeing of mankind: A call for global action. J. Clin. Periodontol. 2017, 44, 456–462. [Google Scholar] [CrossRef]
- Bastos, J.L.; Celeste, R.K.; Paradies, Y.C. Racial inequalities in oral health. J. Dent. Res. 2018, 97, 878–886. [Google Scholar] [CrossRef]
- Hajishengallis, G.; Chavakis, T. Local and systemic mechanisms linking periodontal disease and inflammatory comorbidities. Nat. Rev. Immunol. 2021, 21, 426–440. [Google Scholar] [CrossRef]
- Monteiro, L.P.; Monteiro, A.C.; Pereira, R.M.; Costa, C.C. The knowledge of visually impaired people in relation to oral health. Plural. Sc. Mag. 2018, 4, 44–66. [Google Scholar]
- Siqueira, R.; Ammari, M.; Andrade, M.R.C. Retention of Knowledge About Oral Health in a Sample of Schoolchildren from Nova Friburgo? Int. J. Sci. Dent. 2022, 2, 169–180. [Google Scholar]
- Garcia, C.L.; Uchida, H.T.; Lima, J.P.; Terada, S.G.R.; Pascotto, C.R.; Fujimaki, M. Health education practices for the prevention of tooth decay: A qualitative study with dental surgeons. Rev. Abeno 2018, 18, 62–74. [Google Scholar] [CrossRef]
- Araújo, M.T.B.; Pereira, C.S.; Dutra, C.E.S.V.; Melo, T.C.S.; Pimenta, I.A.; Carvalho, T.A. Videos as oral health education tools in times of pandemic in the integration of teaching and service at the Centro Universitário de Patos de Minas. Abeno Mag. 2021, 21, 1672. [Google Scholar] [CrossRef]
- Huss, A.B.M.; Bishop, C.G.C.; Mistrello, Y.; Rossetto, K.C.A.; Veltrini, V.C. The pandemic and the reformulation of an extension project on oral health education: Report of a year of experience with social media. Abeno Mag. 2021, 22, 1695. [Google Scholar] [CrossRef]
- Chen, S.; Xing, X.; Li, Z.; Zhang, W. Scoping review on the role of social media in oral health promotion. Eur. Rev. Med. Pharmacol. Sci. 2022, 26, 8256–8264. [Google Scholar] [PubMed]
- ElKarmi, R.; Hassona, Y.; Taimeh, D.; Scully, C. YouTube as a source for parents’ education on early childhood caries. Int. J. Paediatr. Dent. 2017, 27, 437–443. [Google Scholar] [CrossRef]
- Duman, C. YouTube™ quality as a source for parental education about the oral hygiene of children. Int. J. Dent. Hyg. 2020, 18, 261–267. [Google Scholar] [CrossRef]
- Monterubbianesi, R.; Tosco, V.; Vitiello, F.; Orilisi, G.; Fraccastoro, F.; Putignano, A.; Orsini, G. Augmented, Virtual and Mixed Reality in Dentistry: A Narrative Review on the Existing Platforms and Future Challenges. Appl. Sci. 2022, 12, 877. [Google Scholar] [CrossRef]
- Hakeem, F.F.; Abdouh, I.; Hamadallah, H.H.; Alarabi, Y.O.; Almuzaini, A.S.; Abdullah, M.M.; Altarjami, A.A. The Association between Electronic Health Literacy and Oral Health Outcomes among Dental Patients in Saudi Arabia: A Cross-Sectional Study. Healthcare 2023, 11, 1804. [Google Scholar] [CrossRef]
- Fonseca, M.H.; Kovaleski, F.; Picinin, C.T.; Pedroso, B.; Rubbo, P. E-health practices and technologies: A systematic review from 2014 to 2019. Healthcare 2021, 9, 1192. [Google Scholar] [CrossRef]
- Estai, M.; Kanagasingam, Y.; Tennant, M.; Bunt, S. A systematic review of the research evidence for the benefits of teledentistry. J. Telemed. Telecare 2018, 24, 147–156. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.; Thomas, J.; Chandler, J. Cochrane handbook for systematic reviews of interventions. In Cochrane Handbook for Systematic Reviews of Interventions; Wiley: Hoboken, NJ, USA, 2019. [Google Scholar]
- Morena, D.; Leitão-Almeida, B.; Pereira, M.; Resende, R.; Fernandes, J.C.H.; Fernandes, G.V.O.; Borges, T. Comparative Clinical Behavior of Zirconia versus Titanium Dental Implants: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J. Clin. Med. 2024, 13, 4488. [Google Scholar] [CrossRef]
- Maurotto, M.; Costa, L.G.; Manso, M.C.; Mosley, G.A.; Fernandes, J.C.H.; Fernandes, G.V.O.; Castro, F. Correlation Between Periodontitis and Gastritis Induced by Helicobacter Pylori: A Comprehensive Review. Microorganisms 2024, 12, 1579. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, A.; Brennan, S.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, 71. [Google Scholar] [CrossRef] [PubMed]
- Pai Khot, A.J.; Choudhury, A.R.; Ankola, A.V.; Sankeshwari, R.M.; Hampiholi, V.; Hebbal, M.; Jalihal, S.; Kumar, R.S.; Kabra, L.; Kotha, S.L. Evaluation of a “Picture Assisted Illustration Reinforcement” (PAIR) System for Oral Hygiene in Children with Autism: A Double-Blind Randomized Controlled Trial. Children 2023, 10, 369. [Google Scholar] [CrossRef] [PubMed]
- Álvarez, N.G.; Mortecinos, A.V.; Rodríguez, V.R.; Fontanilla, M.L.; Vásquez, M.M.; Pavez-Adasme, G.; Hemández- Mosqueira, C. Effect of an intervention based on virtual reality on motor development and postural control in children with Down Syndrome. Rev. Chil. Pediatr. 2018, 89, 747–752. [Google Scholar] [CrossRef]
- Khalil, M.; Sorour, D.; Mousa, E.; Shaala, R. Effect of Mobile-Based Educational Program Through Bluetooth and WhatsApp. Application on the Oral Health Values, Dental Literacy, and Oral Self-Efficacy among Older Adults. NILES J. Geriatr. Gerontol. 2020, 3, 42–64. [Google Scholar] [CrossRef]
- Carli, E.; Pasini, M.; Pardossi, F.; Capotosti, I.; Narzisi, A.; Lardani, L. Oral Health Preventive Program in Patients with Autism Spectrum Disorder. Children 2022, 9, 535. [Google Scholar] [CrossRef]
- Sharififard, N.; Sargeran, K.; Gholami, M.; Zayeri, F. A music- and game-based oral health education for visually impaired school children; multilevel analysis of a cluster randomized controlled trial. BMC Oral. Health 2020, 20, 144. [Google Scholar] [CrossRef]
- Veiga, N.; Lopes, P.C.; Pires, B.; Couto, P.; Correia, P.; Fernandes, J.C.H.; Fernandes, G.V.O. Application of Digital Technologies in Health Literacy in situations of Social Isolation: A systematic review. Int. J. Sci. Dent. 2024. [Google Scholar]
- Shaw, T.; McGregor, D.; Brunner, M.; Keep, M.; Janssen, A.; Barnet, S. What is eHealth (6)? Development of a Conceptual Model for eHealth: Qualitative Study with Key Informants. J. Med. Internet Res. 2017, 19, e324. [Google Scholar] [CrossRef]
- Ko, M.-S.; Kang, K.-J. Influence of health literacy and health empowerment on health behavior practice in elderly outpatients with coronary artery disease. J. Korean Clin. Nurs. Res. 2018, 24, 293–302. [Google Scholar]
- Norman, C.D.; Skinner, H.A. eHealth literacy: Essential skills for consumer health in a networked world. J. Med. Internet Res. 2006, 8, e506. [Google Scholar] [CrossRef]
- Genaro, L.E.; Marconato, J.V.; Hanai, D.; Gobbo-Pawloski, C.L.; Capote, T.S.O. Virtual Reality in Oral Hygiene Instruction: An Immersive Approach Virtual reality in oral hygiene teaching: An immersive approach. Odovtos-Int. J. Dent. Sci. 2022, 24, 177–187. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).