Enhancing Healthcare Management during COVID-19: A Patient-Centric Architectural Framework Enabled by Hyperledger Fabric Blockchain
Abstract
1. Introduction
- (1)
- What specific procedures are used to improve data security and privacy for COVID-19 patients in the proposed Hyperledger blockchain-based lightweight access control system?
- (2)
- What are the essential components and design concepts of the architectural framework designed for the application, and how does it permit seamless integration with the Hyperledger blockchain to ensure effective access control for COVID-19 patient data?
- (3)
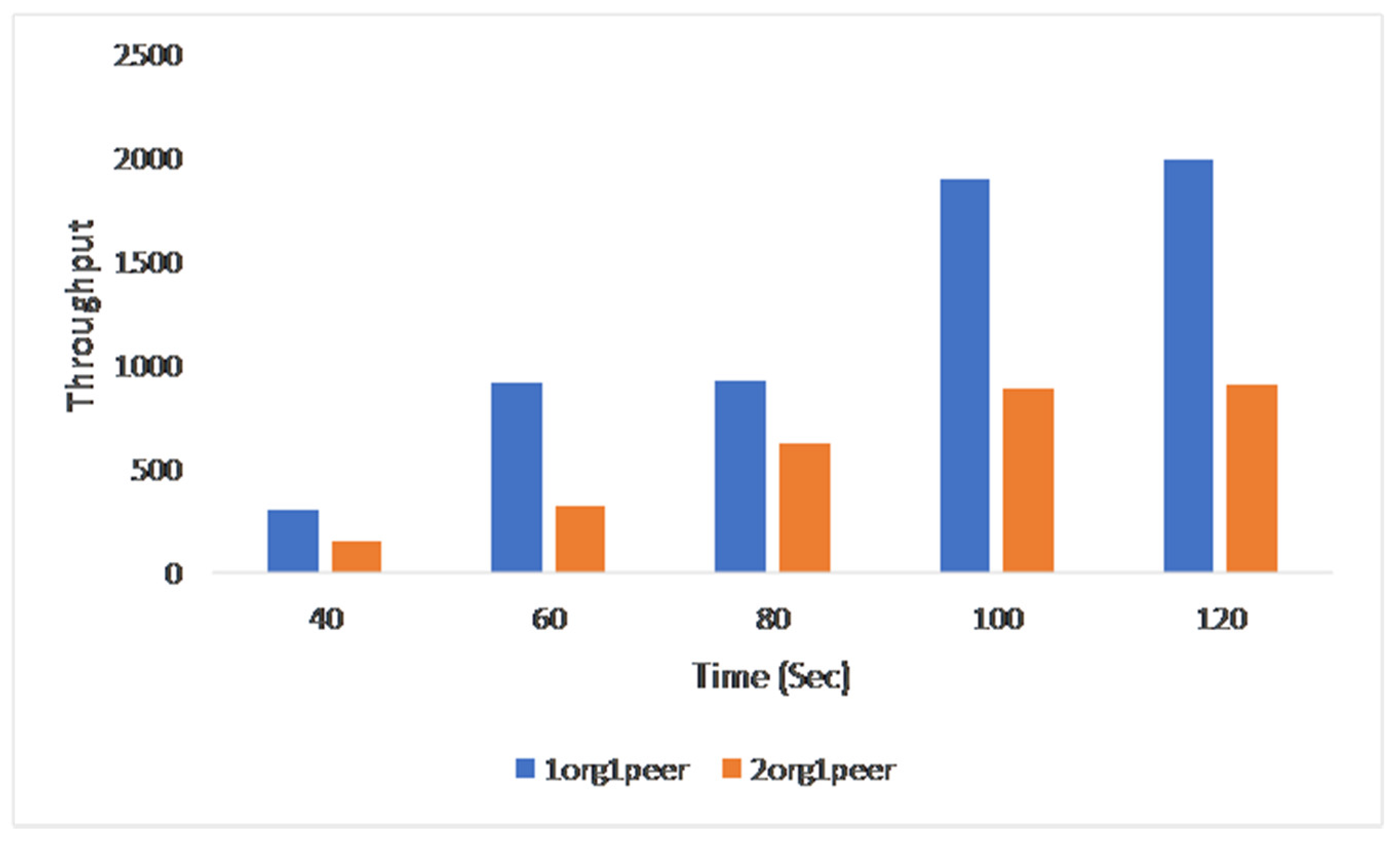
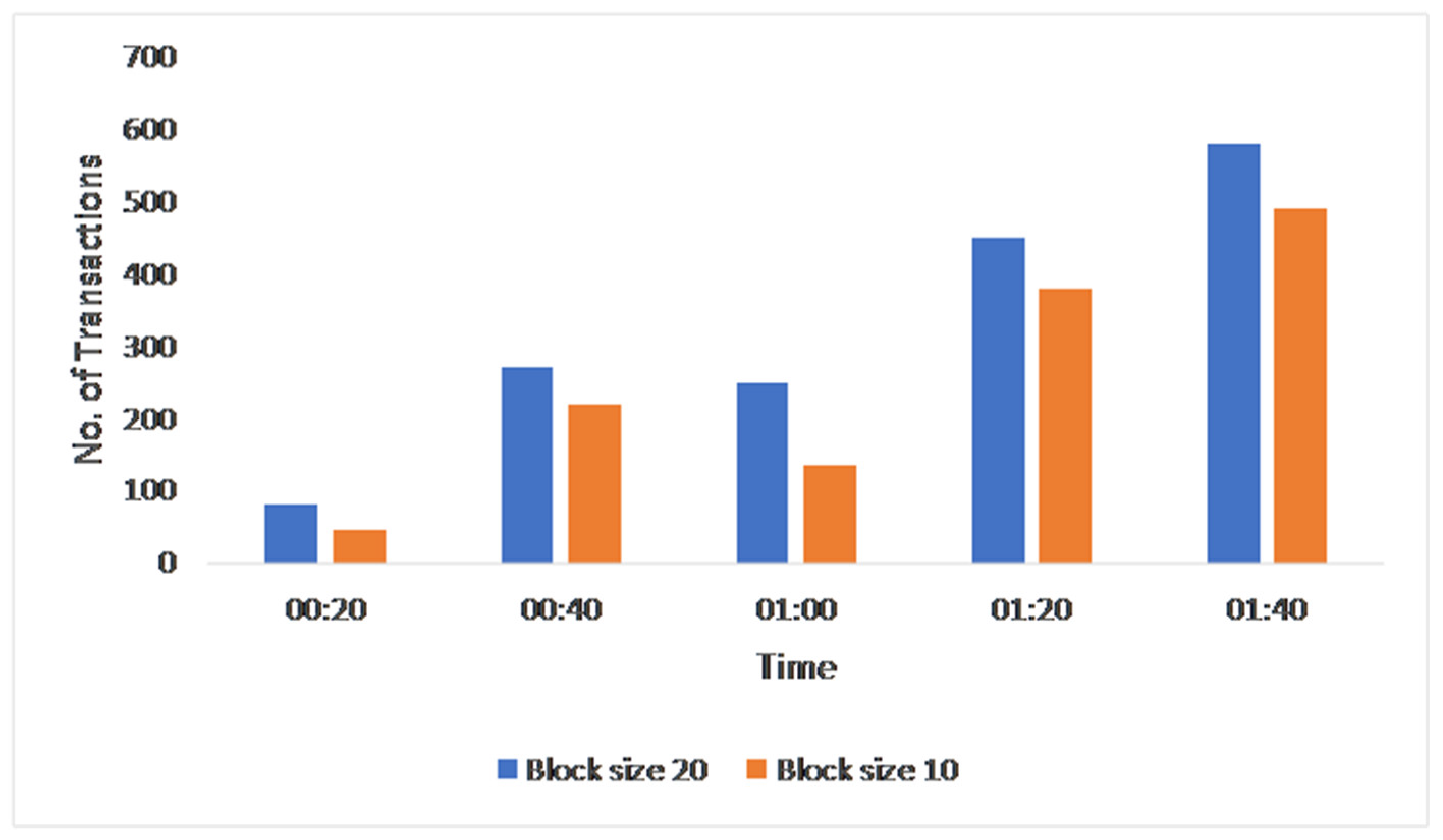
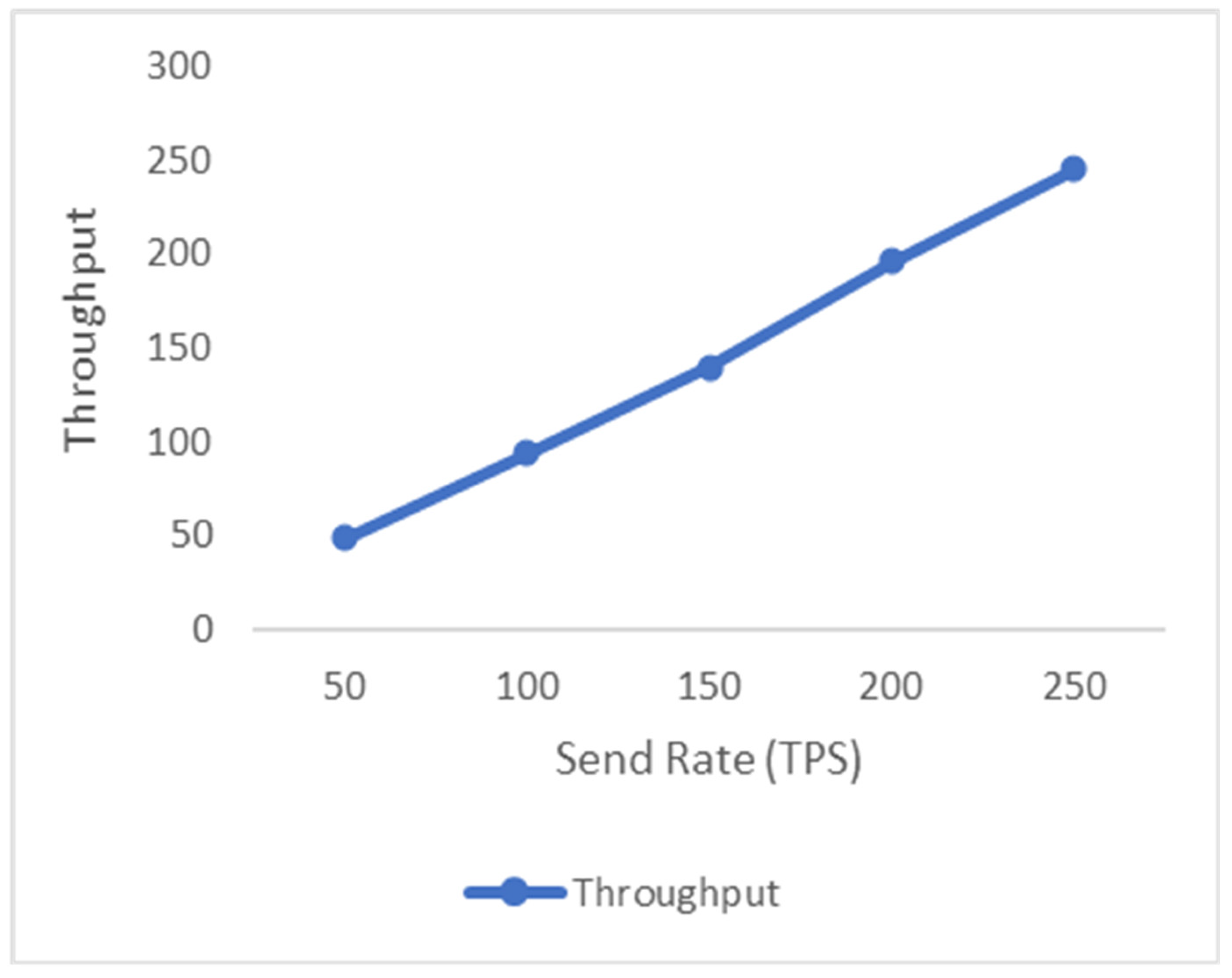
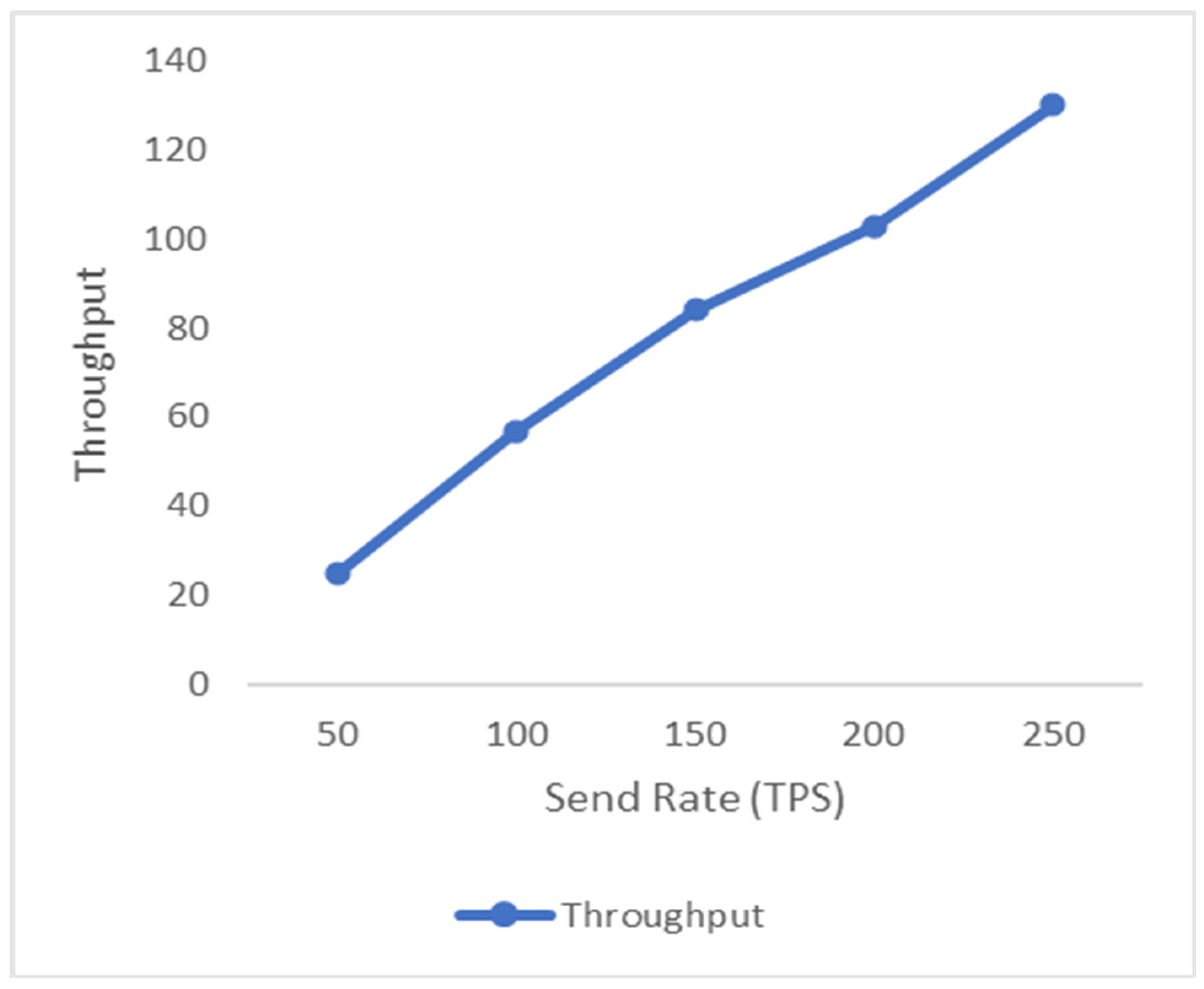
- How does the proposed solution compare to standard access control systems in terms of resource utilization, latency, as well as throughput for managing COVID-19 patient data? What performance measures and benchmarks are utilized to assess the system’s efficiency and scalability?
2. Related Work
- (1)
- The study proposes a Hyperledger blockchain-based, lightweight access control system for COVID-19 patients.
- (2)
- The study enlists the design and development of an architectural framework for such an application.
- (3)
- The study demonstrates the effectiveness of the suggested method in terms of resource utilization, latency, and throughput, among others.
3. Proposed Framework and System Architecture
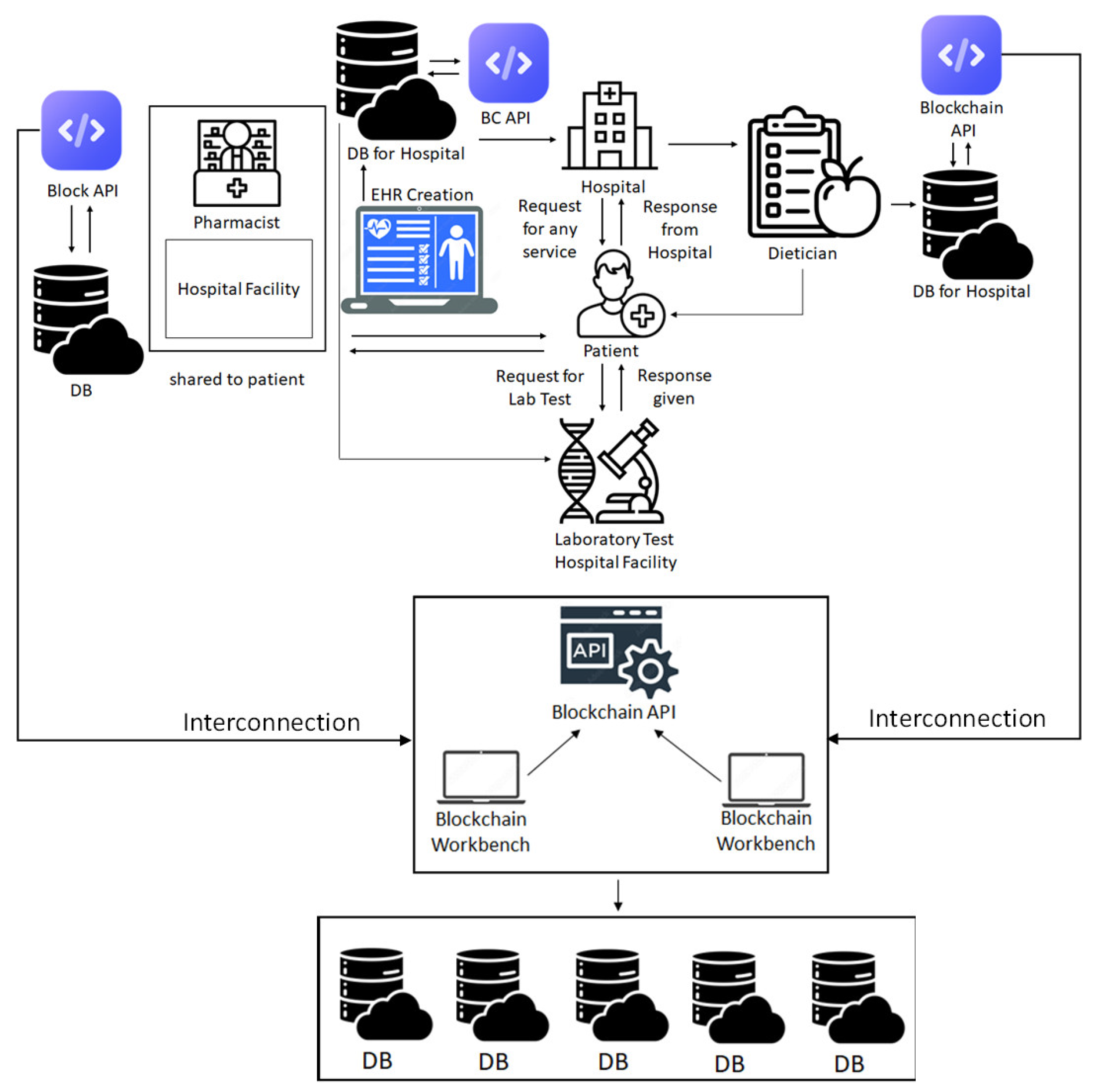
3.1. System Architecture
3.2. Transactions, Participants, and Related Assets in the Proposed Research Work
- (1)
- Participants: Participants represent an individual or group of individuals or organizations. A member who is present in the network has the ability to create assets as well as to exchange assets with the other network participants. Figure 2 shows a list of the participants who have already signed up for our application.
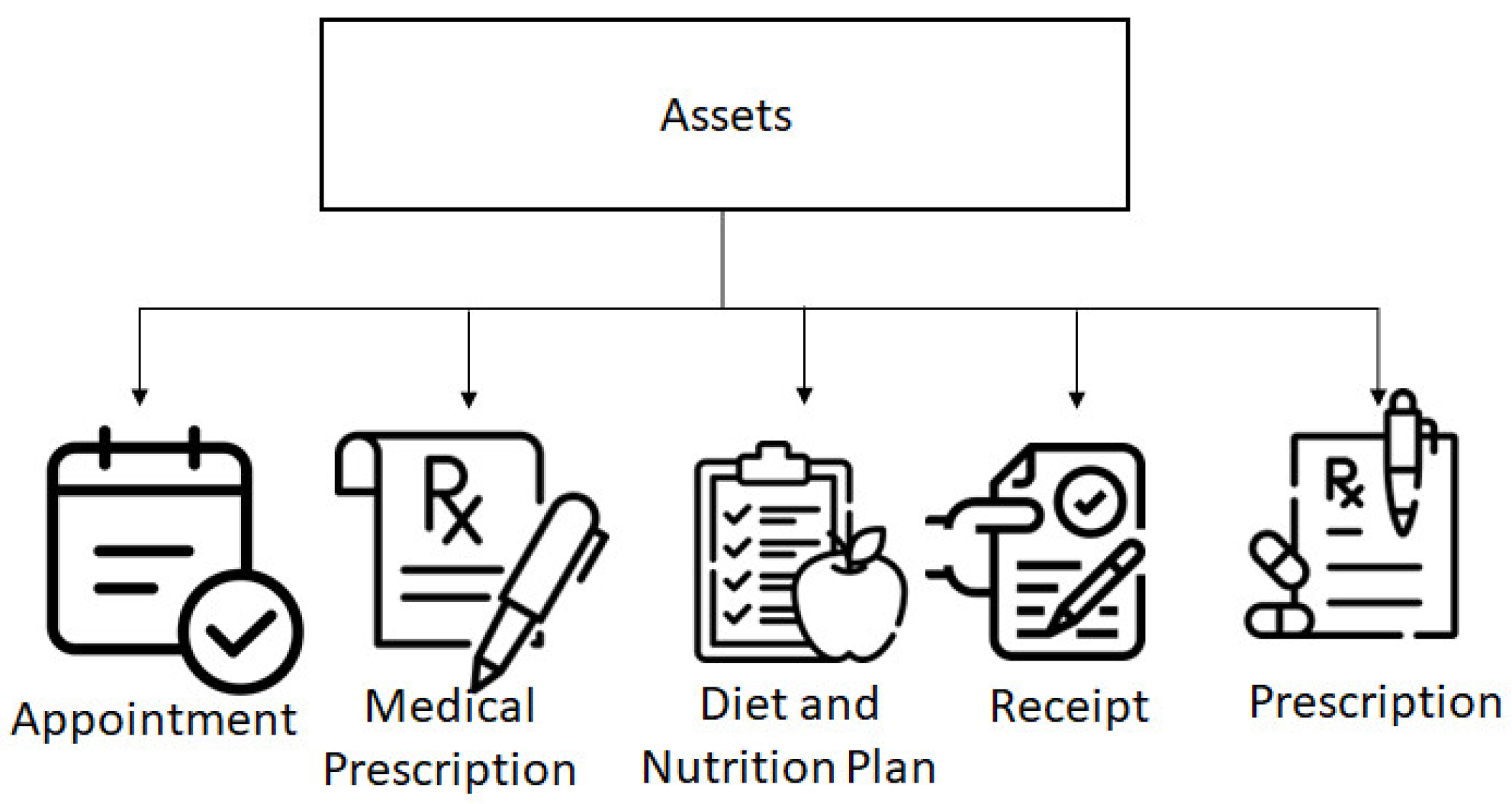
- (2)
- Assets: Assets are any tangible or intangible things that can be used to generate income. To give an example, a receipt is a physical object. Transactions, which are different from one another, can be used to modify these assets. Figure 3 depicts a list of all of the assets associated with our application.
- (3)
- Transactions: Whenever the request for reading and writing from the ledger is made, a transaction is initiated, which further initializes the chain code on a channel. Through the endorsement of peers, application clients can collect, invoke, or instantiate replies. Furthermore, the clients can encapsulate the endorsed results in a transaction, which will then be submitted for committing, validating, and ordering.
3.3. Interaction among the Participants
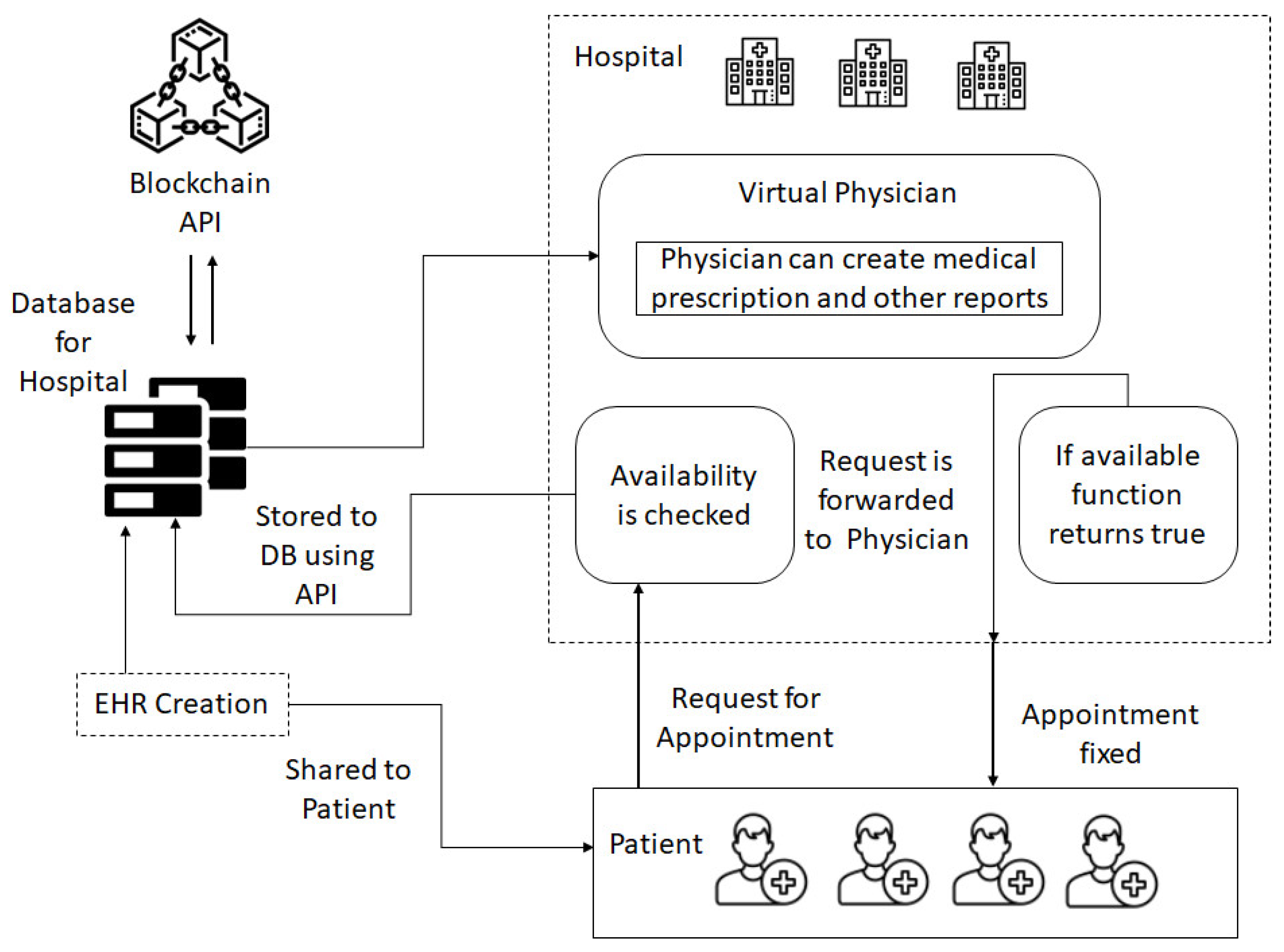
3.3.1. Virtual Physician and Patient Appointment
3.3.2. Virtual Physician Consultation
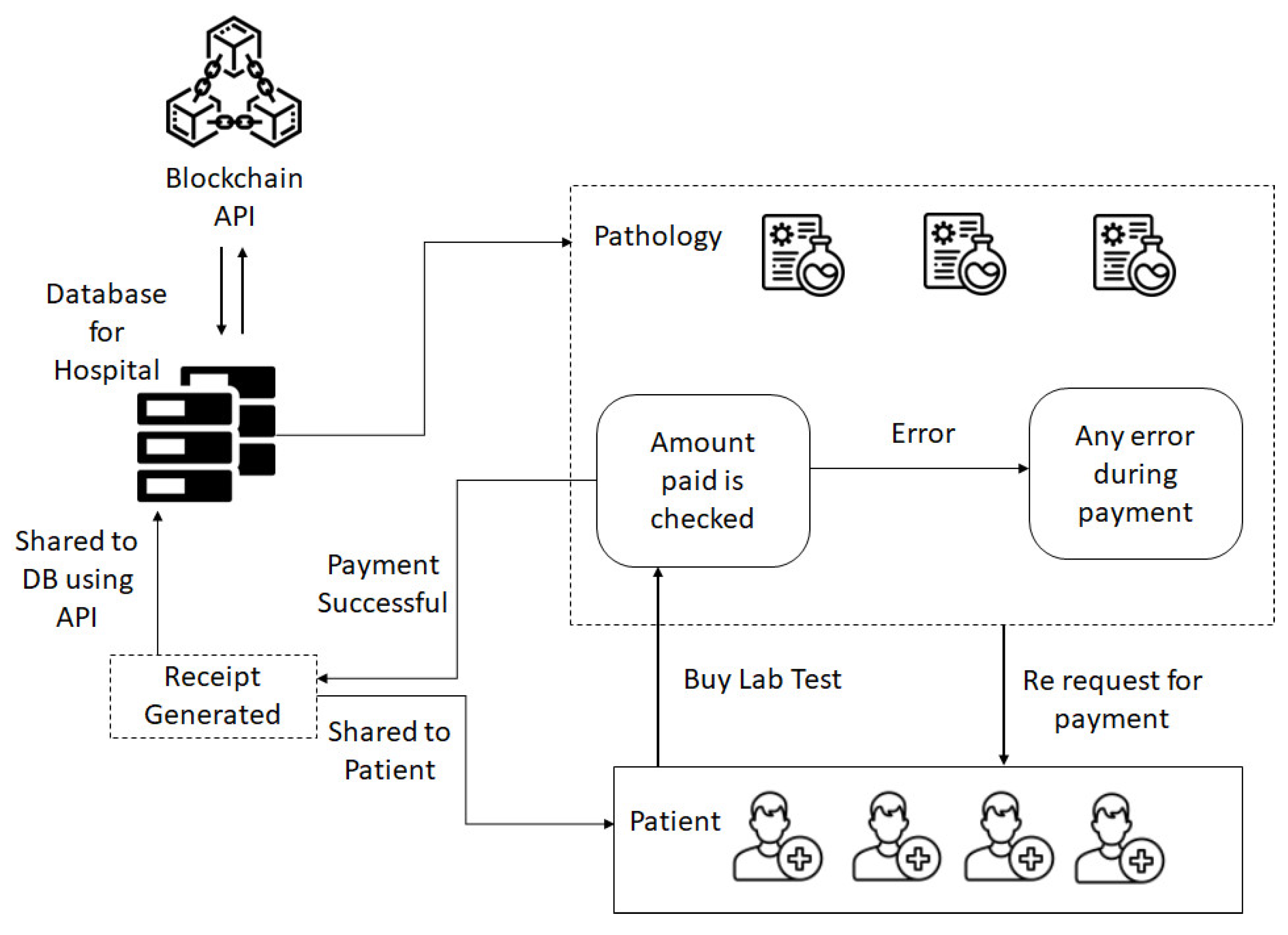
3.3.3. Pathology and Interaction among Patients
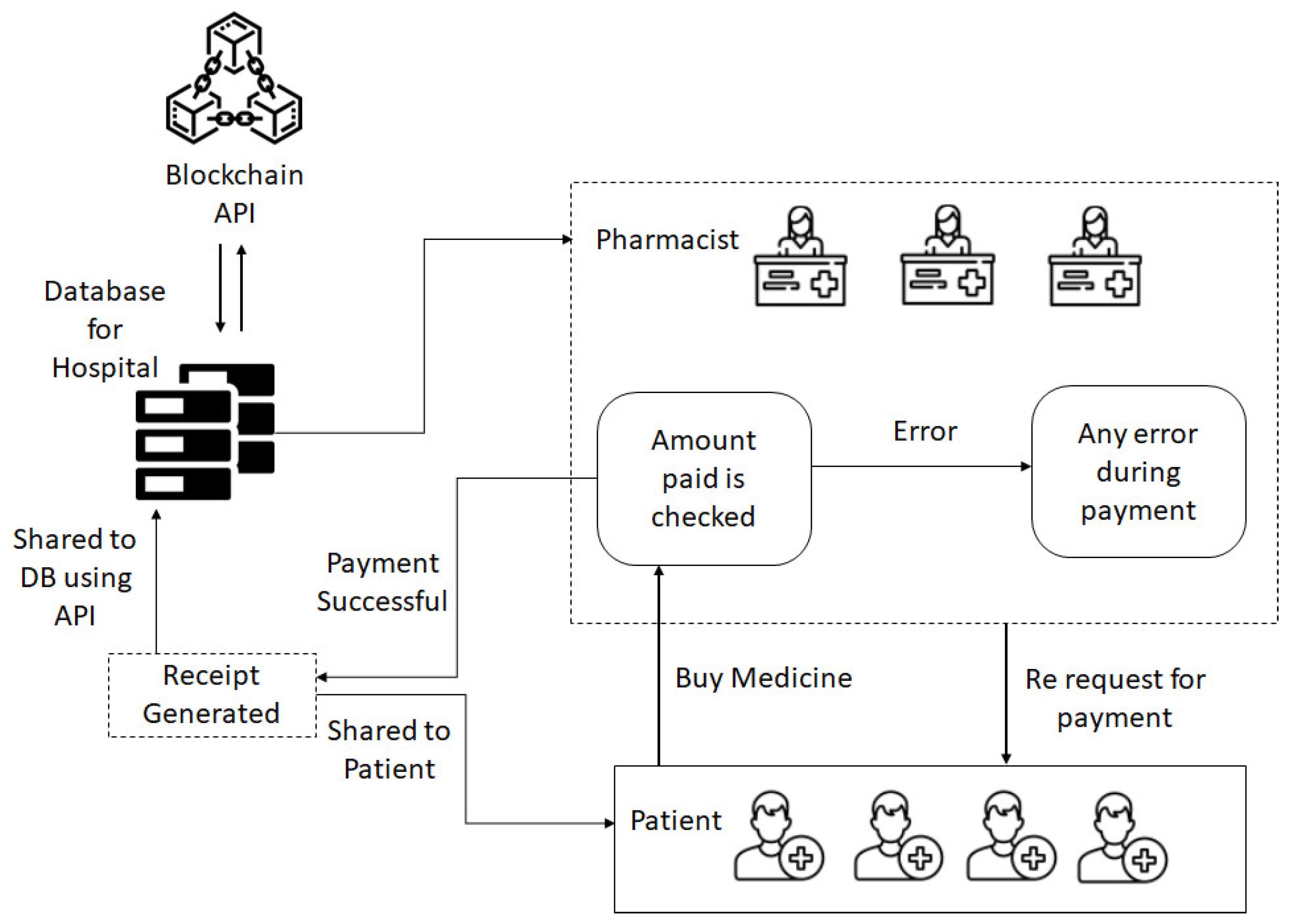
3.3.4. Pharmacist and Patient Interaction
3.3.5. Dietician and Patient Interaction
4. Implementation
4.1. Deployment Phase
- The first phase of network implementation includes designing participants and assets. Business network creation allows application coding. After application coding, the authors created a.bna file (banana file). Hyperledger’s online playground was used to test this file.
- In the second phase, the appointment, buying medicine, pathology test, dietician, and physician’s diagnosis are tested with the framework.
- In the third phase, the patient and virtual physician confirmed appointments as a module in the framework. Testing1 creates a participant patient. The authors also developed an asset appointment for participants. Testing 2 creates the asset. Testing 3 shows an appointment transaction between the patient and the virtual physician IDs.
 |
| Algorithm 1: Enrollment of Participant and Admin. |
| Input: Registration Certificate (RC) request from certificate authority (CA) Output: Transaction Access to ∀ (V, P, H, T, I) ∈ BN Initialization: Nadmin node = valid Nadmin Permissions are (Read, Write, Update, Removal) of V, P, H, T, I Procedure ADMIN (V, P, H, T, I) 1 While (true) do 2 if Vid found valid then BN 3 Add_V to BN 4 Add_V (BN, Vid); 5 Grant_access (Vid); 6 Else 7 Not_exist (VN) 8 End 9 If PID found valid then 10 Add_P to BN 11 Add_P (BN, PID); 12 Grant_access (PID); 13 Else 14 Not_exist(PID); 15 End 16 If HID = found valid then 17 Add_H to BN 18 Add_H(BN, HID); 19 Grant_access(HID); 20 Else 21 Not_exist(HID); 22 End 23 If TID = found valid then 24 Add_T to BN 25 Add_T(BN, TID); 26 Grant_access(TID); 27 Else 28 Not_exist(TID); 29 End 30 If IID = found valid then 31 Add_I to BN 32 Add_I (BN, TID) 33 Grant_access (IID); 34 Else 35 Not_exist (IID); 36 End 37 End 38 Int N: (found malicious 1 not malicious 0) 39 For all (*) do 40 If (node found malicious) then 41 Not update (VID, PID, HID, TID, IID) 42 Else 44 Update (VID, PID, HID, TID, IID) 45 End 46 End For End Procedure |
| Algorithm 2: Working of Participant, fixing of appointment, buying medicine and lab record, dietician consultation. |
| Input: initiate request from N admin for keys & IDS Output: get access to transaction Initialization: VN, PN, HN, TN, IN should be valid node Procedure Appointment (AID) 1 While (true) do 2 If (PN ∈ BN) then 3 If PID = not in BN then 4 Create record (PID, PREC, BN); 5 Else 6 Read records (PID, PREC, BN); 7 Update records (PID, PREC, BN); 8 End 9 Else 10 Not_valid (PID) 11 End 12 If VN ∈ BN then 13 If VID not in BN then 14 Create records (VID, VREC, BN); 15 Else 16 Read_records (VID, VREC, BN); 17 Update_records (VID, VREC, BN); 18 End 19 Else 20 Not_valid(VID) 21 End 22 If HN ∈ BN then 23 If HID not in BN then 24 Create records (HID, HREC, BN); 25 Else 26 Read records (HID, HREC, BN); 27 Update_records (HID, HREC, BN); 28 End 29 Else 30 Not_valid(HID) 31 End 32 If TN ∈ BN then 33 If TID not in BN then 34 Create records (TID, TREC, BN); 35 Else 36 Read records (TID, TREC, BN); 37 Update records (TID, TREC, BN); 38 End 39 Else 40 Not valid(TID) 41 End 42 If DN ∈ BN then 43 If DID not in BN then 44 Create records (DID, DREC, BN); 45 Else 46 Read_records (DID, DREC, BN); 47 Update_records (DID, DREC, BN); 48 End 49 Else 50 Not_exist(DID); 51 End 52 End 53 N = 0 (participant non availability) 0 or 1 (participants availablilty); 54 If (Appointment (VID, PID)) then 55 MPID = Drug Record (PID, VID); 56 If N = 1 then 57 Generate permission for record (MPID) 58 Reciept_Generation (PID, VID); 59 Else 60 Notify (“Error”); 61 End 62 Else 63 End 64 Int N: 0 (payment status invalid) or 1 (payment status valid); 65 If (purchase drugs (HID, PID) then 66 If N = 1 then 67 Generate permission for record (MPID) 68 Receipt Generate (PID, HID); 69 Else 70 Display (“Found Error”); 71 End 72 Else 73 End 74 Int N: 0 (participant’s non availability) or 1 (participants’ availability); 75 If (Appointment (VID, PID) then 76 LID = Lab Record (PID, VID); 77 If N then 78 Grant records (LPID) 79 Else 80 Display (“Error Found”); 81 End 82 Else 83 End 84 Int N: 0 (payment status false) or 1 (payment status true); 85 If (purchase testing (PID, TID) then 86 LID = Lab record (PID, TID); 87 If N then 88 Grant permission for records (LID) 89 Receipt Generation (PID, VID); 90 Else 91 Display (“Error found”); 92 End 93 Else 94 End 95 Int N: 0 (participants availability false) or 1: (participants availability true); 96 If (Appointment (IID, PID) then 97 CID = dietician (IID, VID); 98 If N then 99 Grant permission for records (CID) 100 Receipt Generation (PID, IID); 101 Else 102 Display (“Error found”); 103 End 104 Else 105 End 106 Int N: 0 (payment status false) or 1: (payment status true); 107 If (taking consultation (IID, PID) then 108 CID = Diet Chart (PID, IID); 109 If N then 110 Grant Chart (CID) 111 Generate receipt (PID, IID); 112 Else 113 Notify (“Error”); 114 End 115 Else 116 End Procedure |
4.2. REST Server Implementation
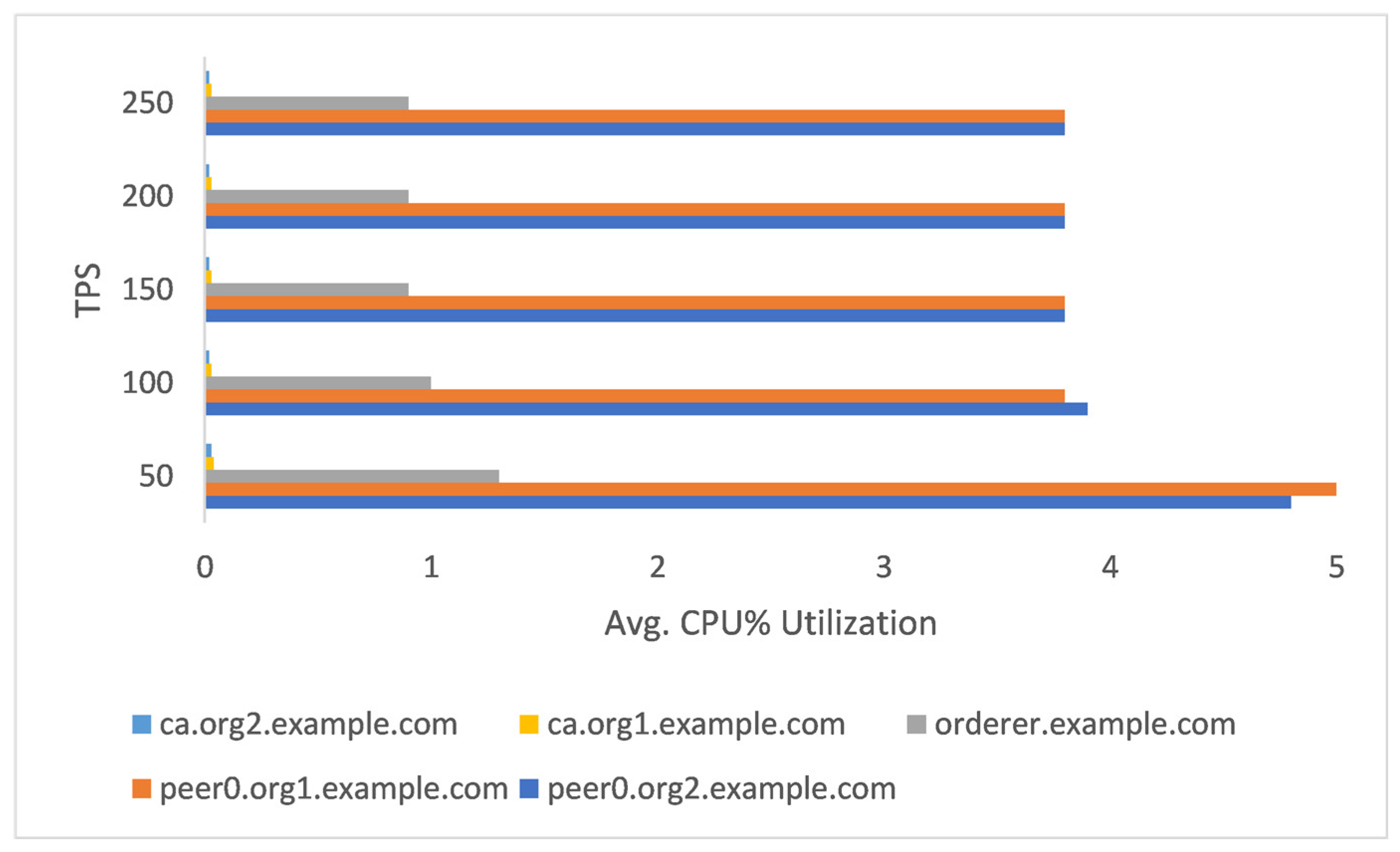
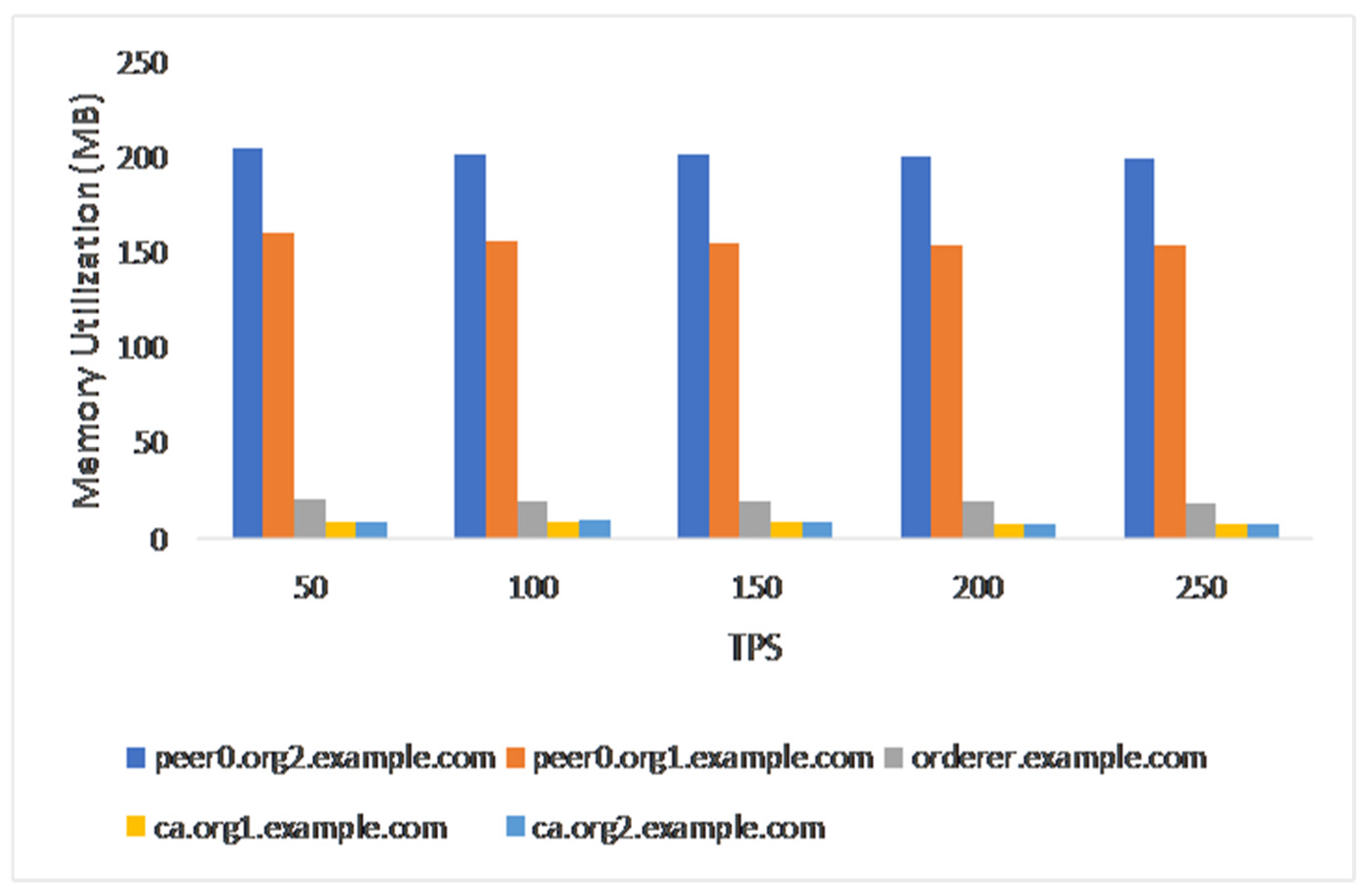
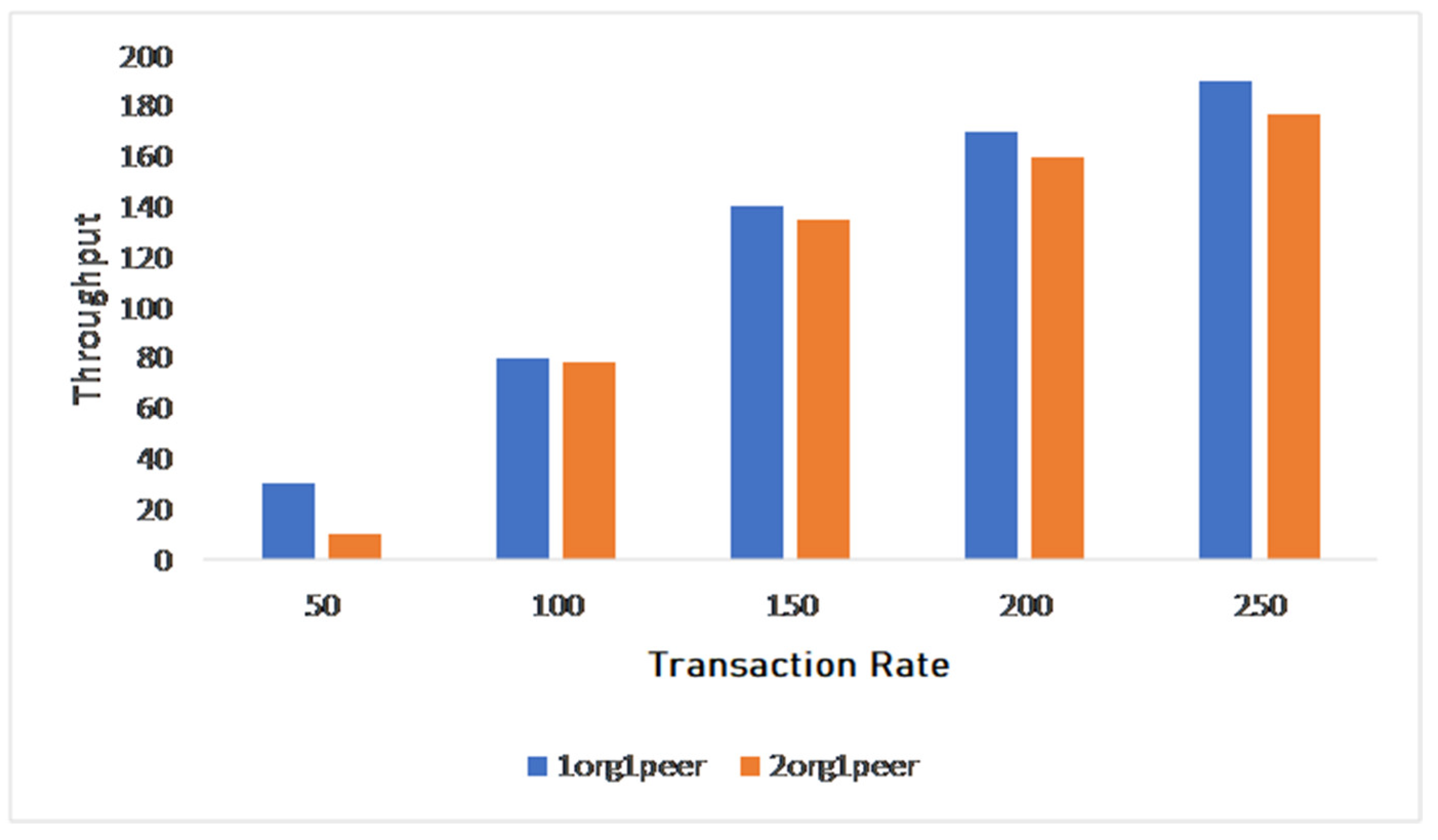
5. Performance Analysis of Proposed Solution and Findings
6. Discussion
7. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Pham, Q.-V.; Nguyen, D.C.; Huynh-The, T.; Hwang, W.-J.; Pathirana, P.N. Artificial Intelligence (AI) and Big Data for Coronavirus (COVID-19) Pandemic: A Survey on the State-of-the-Arts. IEEE Access 2020, 8, 130820–130839. [Google Scholar] [CrossRef]
- Al-Rakhami, M.S.; Al-Amri, A.M. Lies Kill, Facts Save: Detecting COVID-19 Misinformation in Twitter. IEEE Access 2020, 8, 155961–155970. [Google Scholar] [CrossRef]
- Khatri, S.; Alzahrani, F.A.; Ansari, M.T.J.; Agrawal, A.; Kumar, R.; Khan, R.A. A Systematic Analysis on Blockchain Integration with Healthcare Domain: Scope and Challenges. IEEE Access 2021, 9, 84666–84687. [Google Scholar] [CrossRef]
- Marbouh, D.; Abbasi, T.; Maasmi, F.; Omar, I.A.; Debe, M.S.; Salah, K.; Jayaraman, R.; Ellahham, S. Blockchain for COVID-19: Review, Opportunities, and a Trusted Tracking System. Arab. J. Sci. Eng. 2020, 45, 9895–9911. [Google Scholar] [CrossRef]
- Xu, H.; Zhang, L.; Onireti, O.; Fang, Y.; Buchanan, W.J.; Imran, M.A. BeepTrace: Blockchain-Enabled Privacy-Preserving Contact Tracing for COVID-19 Pandemic and Beyond. IEEE Internet Things J. 2021, 8, 3915–3929. [Google Scholar] [CrossRef]
- Baz, M.; Khatri, S.; Baz, A.; Alhakami, H.; Agrawal, A.; Ahmad Khan, R. Blockchain and Artificial Intelligence Applications to Defeat COVID-19 Pandemic. Comput. Syst. Sci. Eng. 2022, 40, 691–702. [Google Scholar] [CrossRef]
- Celesti, A.; Amft, O.; Villari, M. Guest Editorial Special Section on Cloud Computing, Edge Computing, Internet of Things, and Big Data Analytics Applications for Healthcare Industry 4.0. IEEE Trans. Ind. Inform. 2019, 15, 454–456. [Google Scholar] [CrossRef]
- Ismail, L.; Materwala, H.; Zeadally, S. Lightweight Blockchain for Healthcare. IEEE Access 2019, 7, 149935–149951. [Google Scholar] [CrossRef]
- Kim, M.; Yu, S.; Lee, J.; Park, Y.; Park, Y. Design of Secure Protocol for Cloud-Assisted Electronic Health Record System Using Blockchain. Sensors 2020, 20, 2913. [Google Scholar] [CrossRef]
- Augot, D.; Chabanne, H.; Chenevier, T.; George, W.; Lambert, L. A User-Centric System for Verified Identities on the Bitcoin Blockchain. In Lecture Notes in Computer Science; Springer International Publishing: Cham, Switzerland, 2017; pp. 390–407. ISBN 9783319678153. [Google Scholar]
- Fan, K.; Wang, S.; Ren, Y.; Li, H.; Yang, Y. MedBlock: Efficient and Secure Medical Data Sharing via Blockchain. J. Med. Syst. 2018, 42, 136. [Google Scholar] [CrossRef]
- Guo, R.; Shi, H.; Zhao, Q.; Zheng, D. Secure Attribute-Based Signature Scheme with Multiple Authorities for Blockchain in Electronic Health Records Systems. IEEE Access 2018, 6, 11676–11686. [Google Scholar] [CrossRef]
- Biswas, S.; Sharif, K.; Li, F.; Latif, Z.; Kanhere, S.S.; Mohanty, S.P. Interoperability and Synchronization Management of Blockchain-Based Decentralized e-Health Systems. IEEE Trans. Eng. Manag. 2020, 67, 1363–1376. [Google Scholar] [CrossRef]
- Valenta, M.; Sandner, P. Comparison of Ethereum, Hyperledger Fabric and Corda. Frankf. Sch. Blockchain Cent. 2017, 8, 1–8. [Google Scholar]
- Sajana, P.; Sindhu, M.; Sethumadhavan, M. On Blockchain Applications: Hyperledger Fabric and Ethereum. Int. J. Pure Appl. Math. 2018, 118, 2965–2970. [Google Scholar]
- Uddin, M.A.; Stranieri, A.; Gondal, I.; Balasubramanian, V. A Patient Agent to Manage Blockchains for Remote Patient Monitoring. Stud. Health Technol. Inform. 2018, 254, 105–115. [Google Scholar] [CrossRef]
- Wang, S.; Wang, J.; Wang, X.; Qiu, T.; Yuan, Y.; Ouyang, L.; Guo, Y.; Wang, F.-Y. Blockchain-Powered Parallel Healthcare Systems Based on the ACP Approach. IEEE Trans. Comput. Soc. Syst. 2018, 5, 942–950. [Google Scholar] [CrossRef]
- Daraghmi, E.-Y.; Daraghmi, Y.-A.; Yuan, S.-M. MedChain: A Design of Blockchain-Based System for Medical Records Access and Permissions Management. IEEE Access 2019, 7, 164595–164613. [Google Scholar] [CrossRef]
- Al Omar, A.; Rahman, M.S.; Basu, A.; Kiyomoto, S. MediBchain: A Blockchain Based Privacy Preserving Platform for Healthcare Data. In Security, Privacy, and Anonymity in Computation, Communication, and Storage; Springer International Publishing: Cham, Switzerland, 2017; pp. 534–543. ISBN 9783319723945. [Google Scholar]
- Dubovitskaya, A.; Baig, F.; Xu, Z.; Shukla, R.; Zambani, P.S.; Swaminathan, A.; Jahangir, M.M.; Chowdhry, K.; Lachhani, R.; Idnani, N.; et al. ACTION-EHR: Patient-Centric Blockchain-Based Electronic Health Record Data Management for Cancer Care. J. Med. Internet Res. 2020, 22, e13598. [Google Scholar] [CrossRef]
- Abou Jaoude, J.; George Saade, R. Blockchain Applications—Usage in Different Domains. IEEE Access 2019, 7, 45360–45381. [Google Scholar] [CrossRef]
- Ahir, S.; Telavane, D.; Thomas, R. The Impact of Artificial Intelligence, Blockchain, Big Data and Evolving Technologies in Coronavirus Disease—2019 (COVID-19) Curtailment. In Proceedings of the 2020 International Conference on Smart Electronics and Communication (ICOSEC), Trichy, India, 10–12 September 2020; IEEE: New York, NY, USA, 2020. [Google Scholar]
- Lv, W.; Wu, S.; Jiang, C.; Cui, Y.; Qiu, X.; Zhang, Y. Towards Large-Scale and Privacy-Preserving Contact Tracing in COVID-19 Pandemic: A Blockchain Perspective. IEEE Trans. Netw. Sci. Eng. 2022, 9, 282–298. [Google Scholar] [CrossRef]
- Liu, X.; Barenji, A.V.; Li, Z.; Montreuil, B.; Huang, G.Q. Blockchain-Based Smart Tracking and Tracing Platform for Drug Supply Chain. Comput. Ind. Eng. 2021, 161, 107669. [Google Scholar] [CrossRef]
- Krittanawong, C.; Rogers, A.J.; Aydar, M.; Choi, E.; Johnson, K.W.; Wang, Z.; Narayan, S.M. Integrating Blockchain Technology with Artificial Intelligence for Cardiovascular Medicine. Nat. Rev. Cardiol. 2020, 17, 1–3. [Google Scholar] [CrossRef]
- Mashamba-Thompson, T.P.; Crayton, E.D. Blockchain and Artificial Intelligence Technology for Novel Coronavirus Disease 2019 Self-Testing. Diagnostics 2020, 10, 198. [Google Scholar] [CrossRef]
- Du, M.; Chen, Q.; Chen, J.; Ma, X. An Optimized Consortium Blockchain for Medical Information Sharing. IEEE Trans. Eng. Manag. 2021, 68, 1677–1689. [Google Scholar] [CrossRef]
- Tan, L.; Yu, K.; Shi, N.; Yang, C.; Wei, W.; Lu, H. Towards Secure and Privacy-Preserving Data Sharing for COVID-19 Medical Records: A Blockchain-Empowered Approach. IEEE Trans. Netw. Sci. Eng. 2022, 9, 271–281. [Google Scholar] [CrossRef]
- Huang, H.; Gong, T.; Ye, N.; Wang, R.; Dou, Y. Private and Secured Medical Data Transmission and Analysis for Wireless Sensing Healthcare System. IEEE Trans. Ind. Inform. 2017, 13, 1227–1237. [Google Scholar] [CrossRef]
- Resiere, D.; Resiere, D.; Kallel, H. Implementation of Medical and Scientific Cooperation in the Caribbean Using Blockchain Technology in Coronavirus (COVID-19) Pandemics. J. Med. Syst. 2020, 44, 123. [Google Scholar] [CrossRef]
- Bansal, A.; Garg, C.; Padappayil, R.P. Optimizing the Implementation of COVID-19 “Immunity Certificates” Using Blockchain. J. Med. Syst. 2020, 44, 140. [Google Scholar] [CrossRef]
- Tanwar, S.; Parekh, K.; Evans, R. Blockchain-Based Electronic Healthcare Record System for Healthcare 4.0 Applications. J. Inf. Secur. Appl. 2020, 50, 102407. [Google Scholar] [CrossRef]
- Bhattacharya, P.; Tanwar, S.; Bodkhe, U.; Tyagi, S.; Kumar, N. BinDaaS: Blockchain-Based Deep-Learning as-a-Service in Healthcare 4.0 Applications. IEEE Trans. Netw. Sci. Eng. 2021, 8, 1242–1255. [Google Scholar] [CrossRef]
- Singh, A.P.; Pradhan, N.R.; Luhach, A.K.K.; Agnihotri, S.; Jhanjhi, N.Z.; Verma, S.; Kavita; Ghosh, U.; Roy, D.S. A Novel Patient-Centric Architectural Framework for Blockchain-Enabled Healthcare Applications. IEEE Trans. Ind. Inform. 2021, 17, 5779–5789. [Google Scholar] [CrossRef]
- Jabarulla, M.Y.; Lee, H.-N. A blockchain and artificial intelligence-based, patient-centric healthcare system for combating the COVID-19 pandemic: Opportunities and applications. Healthcare 2021, 9, 1019. [Google Scholar] [CrossRef]
- Nabipour, M.; Ülkü, M.A. On deploying blockchain technologies in supply chain strategies and the COVID-19 pandemic: A systematic literature review and research outlook. Sustainability 2021, 13, 10566. [Google Scholar] [CrossRef]
- Xia, Q.; Sifah, E.B.; Smahi, A.; Amofa, S.; Zhang, X. BBDS: Blockchain-based data sharing for electronic medical records in cloud environments. Information 2017, 8, 44. [Google Scholar] [CrossRef]
- Caldarelli, G. Understanding the blockchain oracle problem: A call for action. Information 2020, 11, 509. [Google Scholar] [CrossRef]
- Alshahrani, H.M.; Alotaibi, S.S.; Ansari, M.T.J.; Asiri, M.M.; Agrawal, A.; Khan, R.A.; Mohsen, H.; Hilal, A.M. Analysis and ranking of IT risk factors using fuzzy TOPSIS-based approach. Appl. Sci. 2022, 12, 5911. [Google Scholar] [CrossRef]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Khatri, S.; al-Sulbi, K.; Attaallah, A.; Ansari, M.T.J.; Agrawal, A.; Kumar, R. Enhancing Healthcare Management during COVID-19: A Patient-Centric Architectural Framework Enabled by Hyperledger Fabric Blockchain. Information 2023, 14, 425. https://doi.org/10.3390/info14080425
Khatri S, al-Sulbi K, Attaallah A, Ansari MTJ, Agrawal A, Kumar R. Enhancing Healthcare Management during COVID-19: A Patient-Centric Architectural Framework Enabled by Hyperledger Fabric Blockchain. Information. 2023; 14(8):425. https://doi.org/10.3390/info14080425
Chicago/Turabian StyleKhatri, Sabita, Khalil al-Sulbi, Abdulaziz Attaallah, Md Tarique Jamal Ansari, Alka Agrawal, and Rajeev Kumar. 2023. "Enhancing Healthcare Management during COVID-19: A Patient-Centric Architectural Framework Enabled by Hyperledger Fabric Blockchain" Information 14, no. 8: 425. https://doi.org/10.3390/info14080425
APA StyleKhatri, S., al-Sulbi, K., Attaallah, A., Ansari, M. T. J., Agrawal, A., & Kumar, R. (2023). Enhancing Healthcare Management during COVID-19: A Patient-Centric Architectural Framework Enabled by Hyperledger Fabric Blockchain. Information, 14(8), 425. https://doi.org/10.3390/info14080425











