Design and Execution of Integrated Clinical Pathway: A Simplified Meta-Model and Associated Methodology
Abstract
1. Introduction
2. Theoretical Background
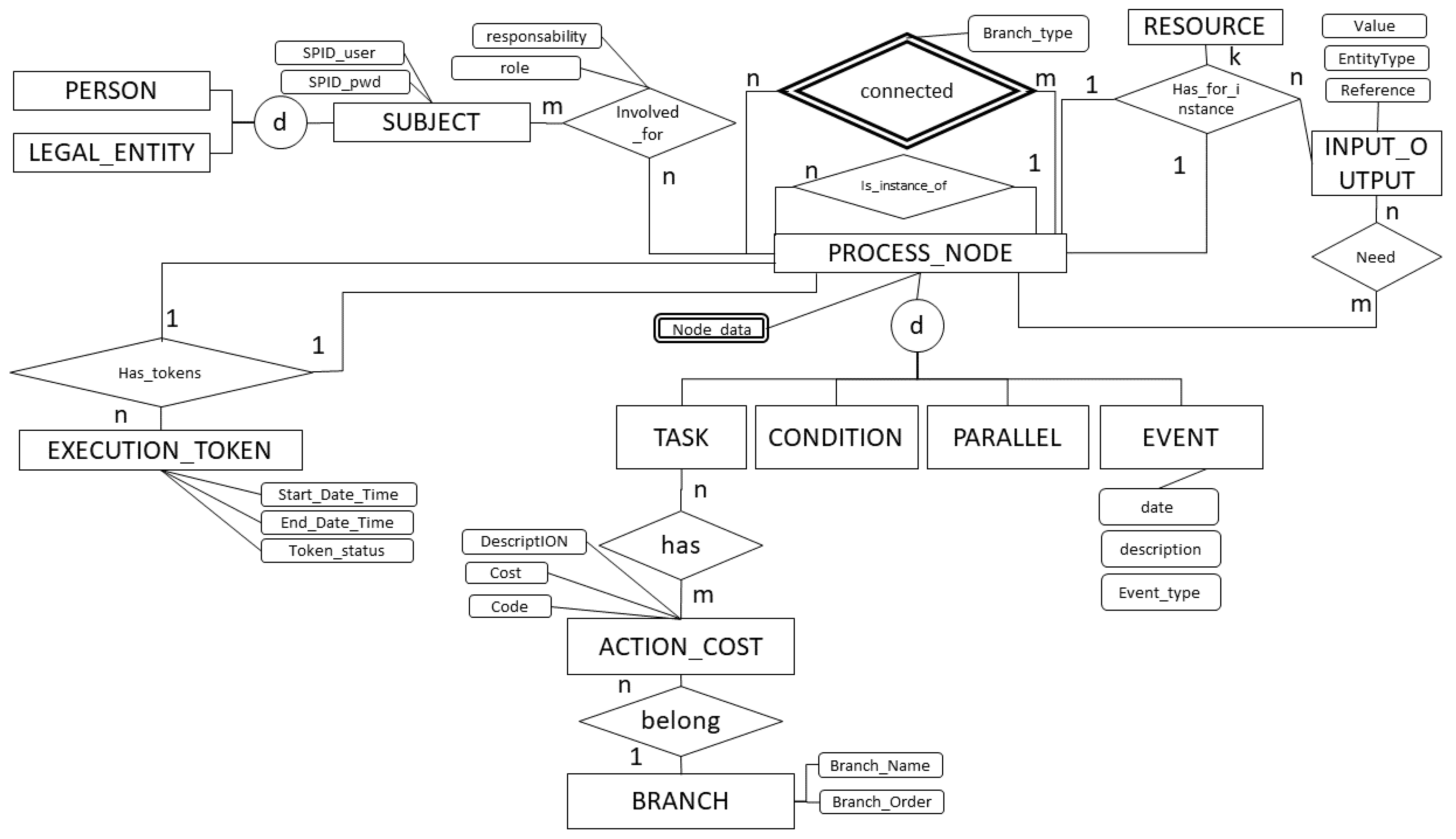
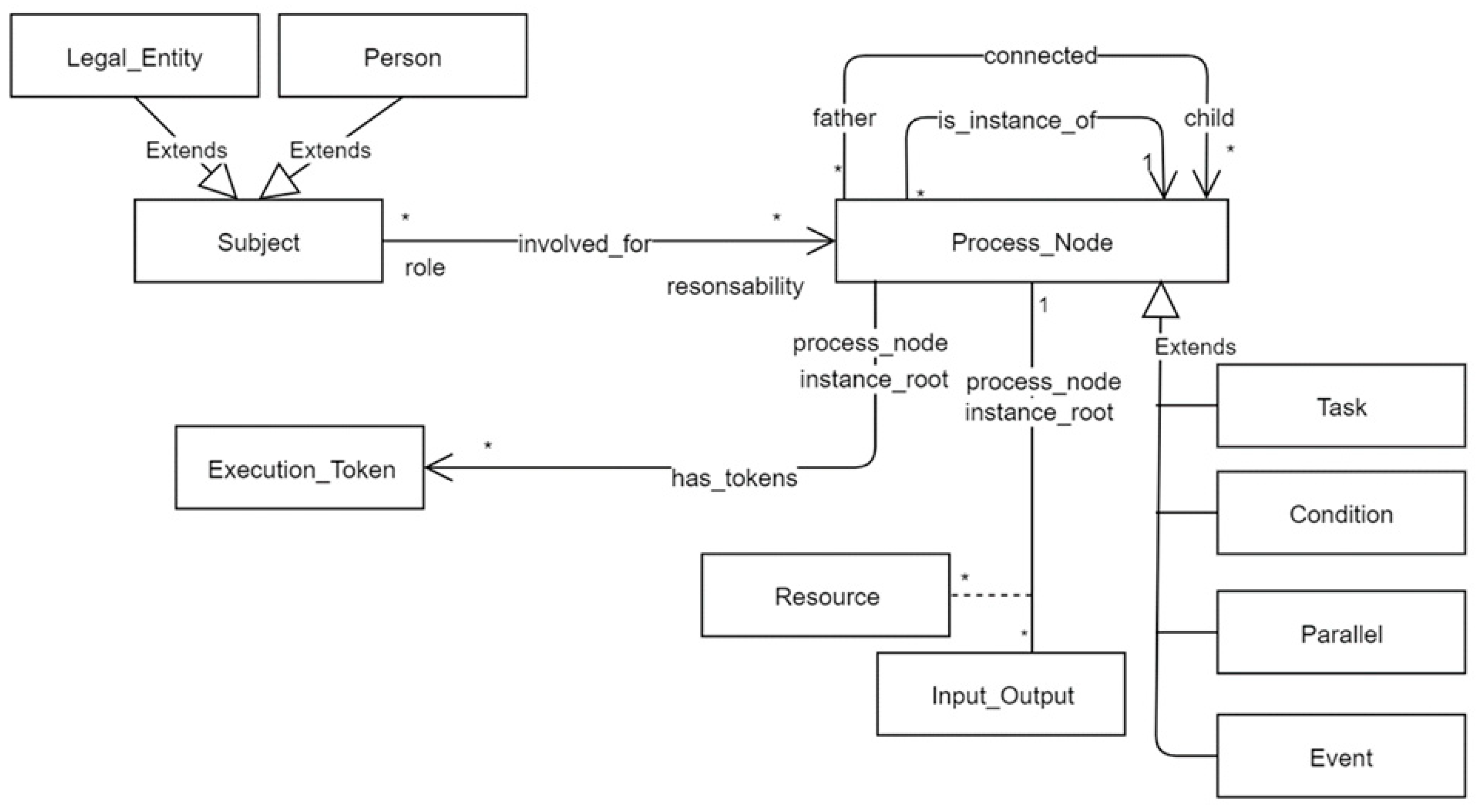
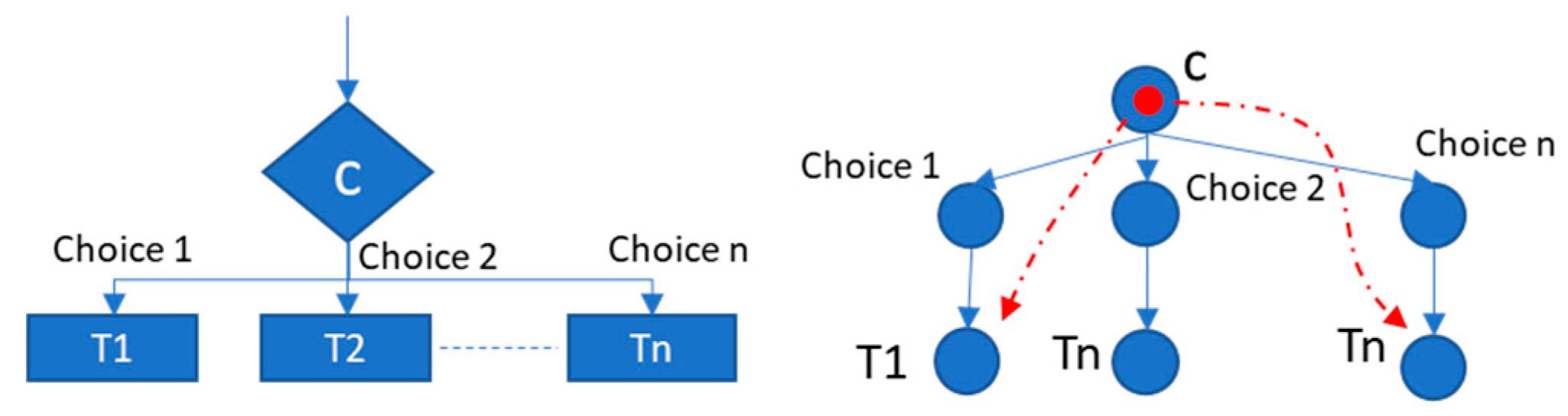
3. A Simplified Meta-Model for Process Knowledge Management
- The number of constructs of the process model must be not too large.
- Features that can be derived from the context of an element of the model should not lead to the definition of specialized subtypes.
- Features that may evolve during the lifecycle of an element should be represented as properties, not as types.
- Multi-dimensional classification is more efficiently represented by properties than by types.
- Pure notational differences should not be reflected in the data model.
- Req. 01: The data model must map the complete process structure.
- Req. 02: When a patient enters in a clinical pathway, the related process instance has to be assigned to him/her.
- Req. 03: The data model should contain the clinical pathway process template and its instances when assigned to a specific patient.
- Req. 04: It is necessary to track and/or reconstruct all the documentation that belongs to each task for the specific clinical pathway process instance.
- Req. 05: The data model should contain information about the costs that belong to each phase/task of the process.
- Req. 06: The data model should include the minimal set of process descriptors such as task sequences, parallel flow, iterations, conditions and events.
- Req. 07: It is mandatory to assign responsibility to each task.
- Req. 08: It is mandatory to track timing perspective information about each task.
- “TR”: If the node is a Template Root.
- “IR”: If the node is an Instance Root.
- “PN”: If the node is a template Process Node.
- “LN”: If the node is a Log Node (these are events related to tasks performed but not planned in the template process).
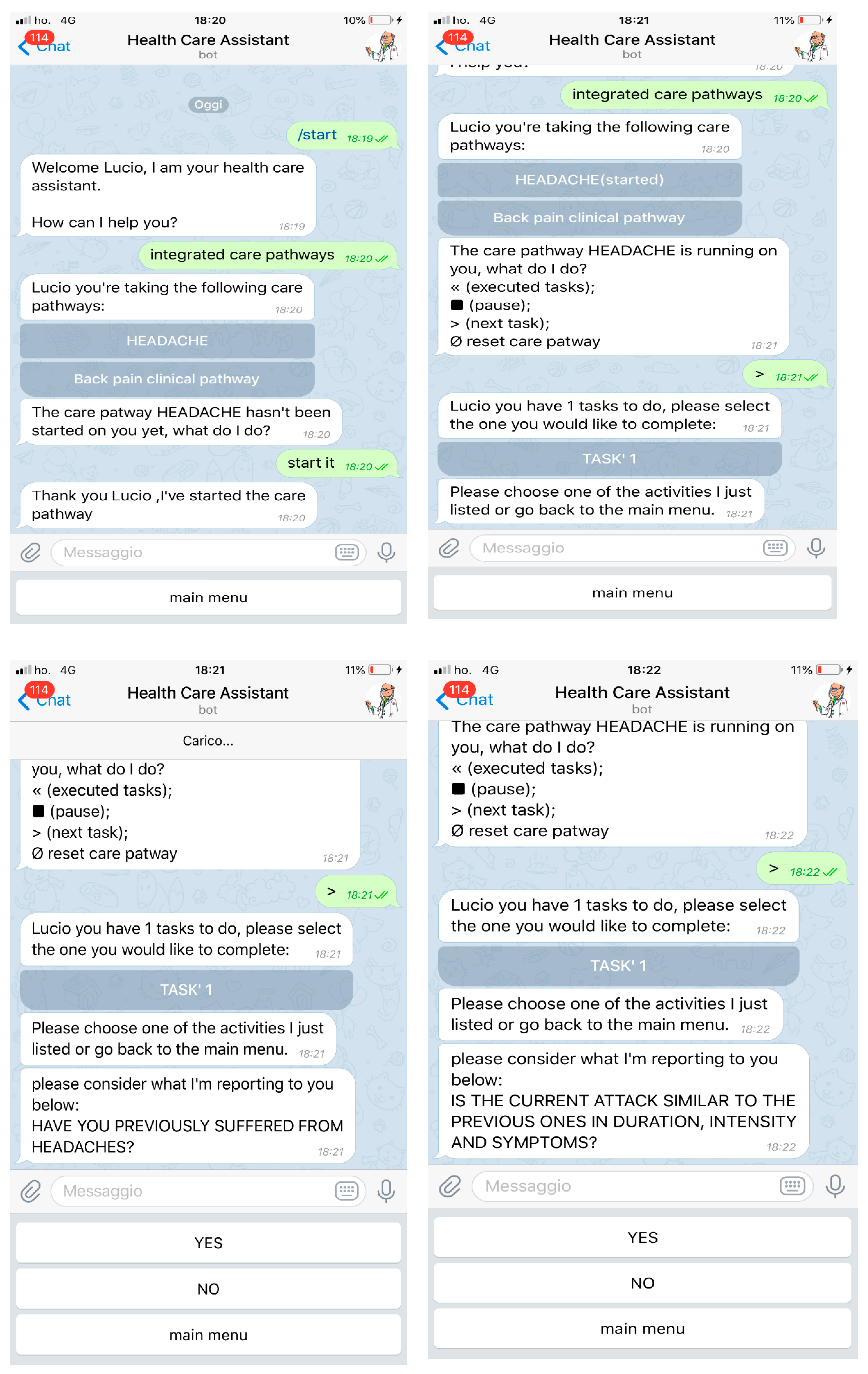
4. ICP Process Execution Assisted by a Chatbot
4.1. ICP Execution: What Really Matters
- Proactively involving the patient at every stage of the process.
- Suggesting what the next step to be performed is (meaning to govern the state of the process).
- Making teamwork agile.
- Eliminating redundancies.
- Reducing conflicts.
- Suggesting actions that will reduce costs and still have the same outcome.
- Optimizing the use of resources.
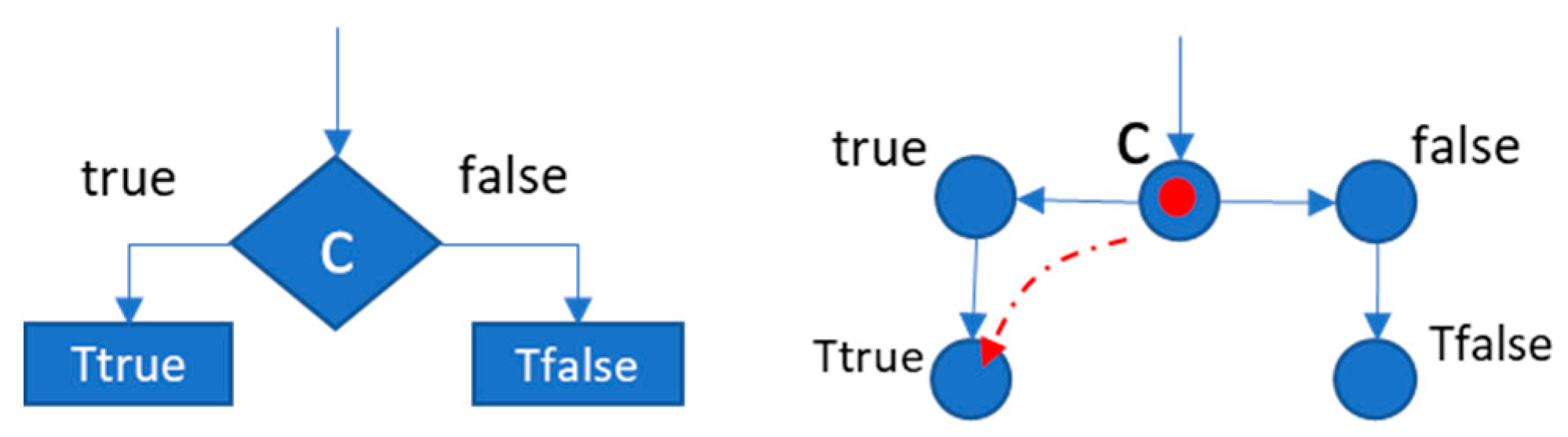
4.2. ICP Execution Strategy
- Assigning a clinical path template to a patient.
- Continuously monitoring the process status.
- Automating the status changes for each task in the process.
- Identifying actions that deviate from the standard path.
- Proposing or suggesting future actions envisaged by the standard route.
- Reminding those responsible for task execution and possibly making them aware of delays.
- Asking for feedback on the state of task execution.
- Asking for feedback on the quality of the template process, in order to improve it.
- Sharing results both at the task level and at the process level as a whole.
- -
- Informative task: A task that aims to provide information and does not require the production of specific results. The chatbot sends the information message stored in patient_description and then moves the execution token to the next task;
- -
- Processing task: In this case, the task requires the production of specific outputs. The chatbot guides the user to produce the expected results. When all the results have been produced, the chatbot independently moves the execution token to the next task.
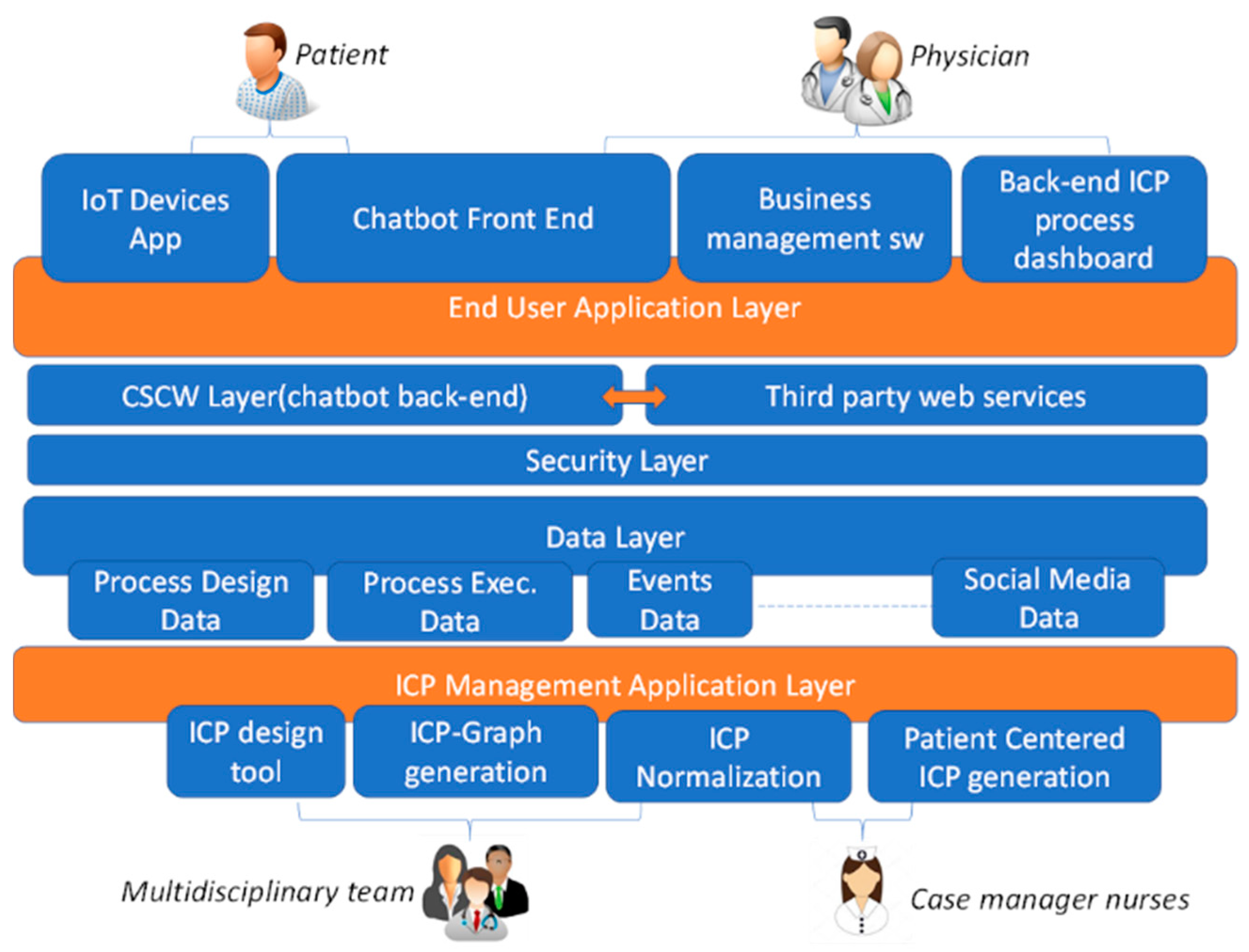
4.3. A Proposal of an Integrated Framework for ICP Execution
4.3.1. Data Layer
4.3.2. ICP Management Application Layer
4.3.3. Security Layer
4.3.4. CSCW Layer (Chatbot Back End) and Chatbot Front End
4.3.5. Back-End ICP Process Dashboard
4.3.6. Business Management Software
4.3.7. IoT Devices APP
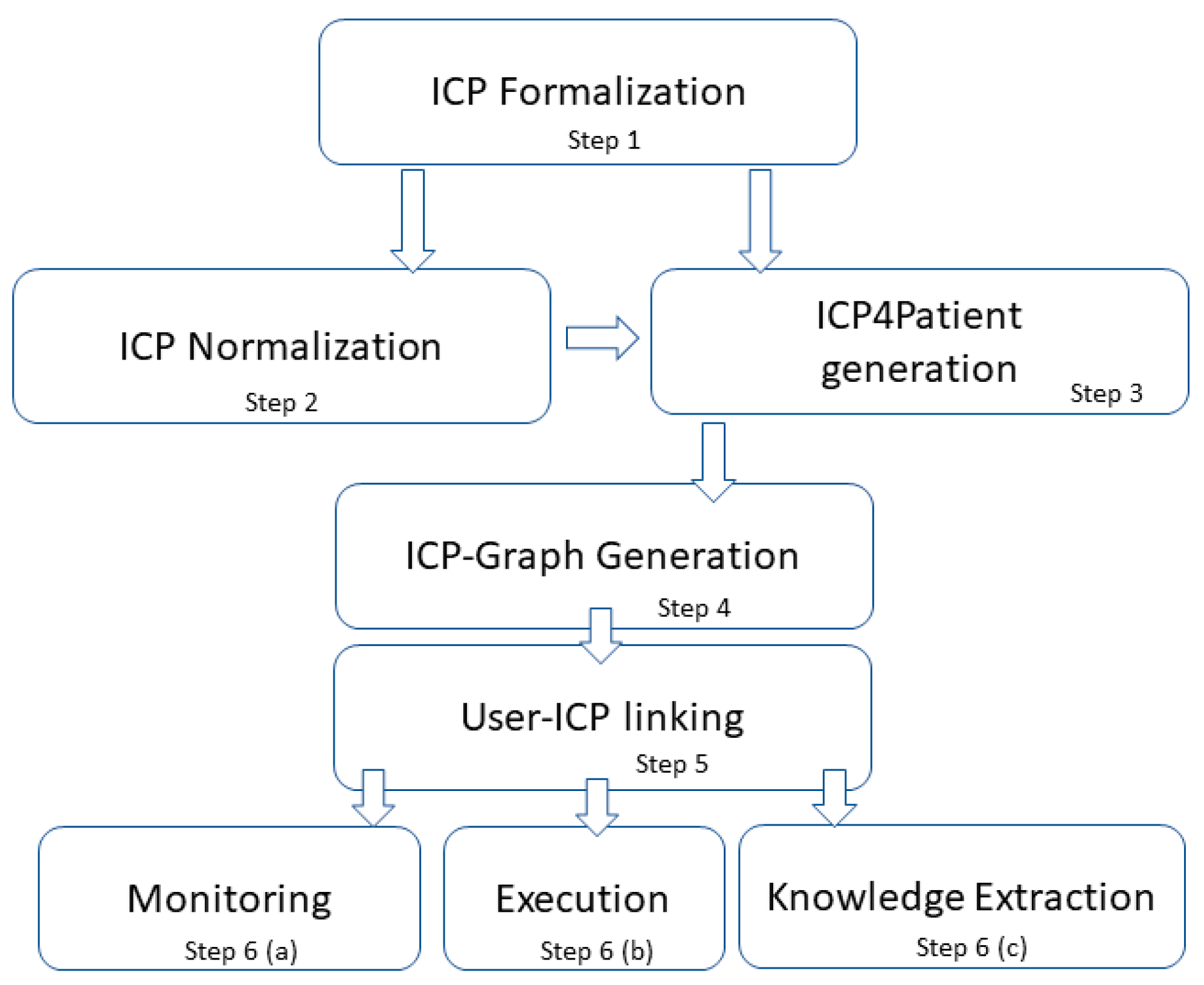
4.4. Methodology for Executable Clinical Pathway Generation
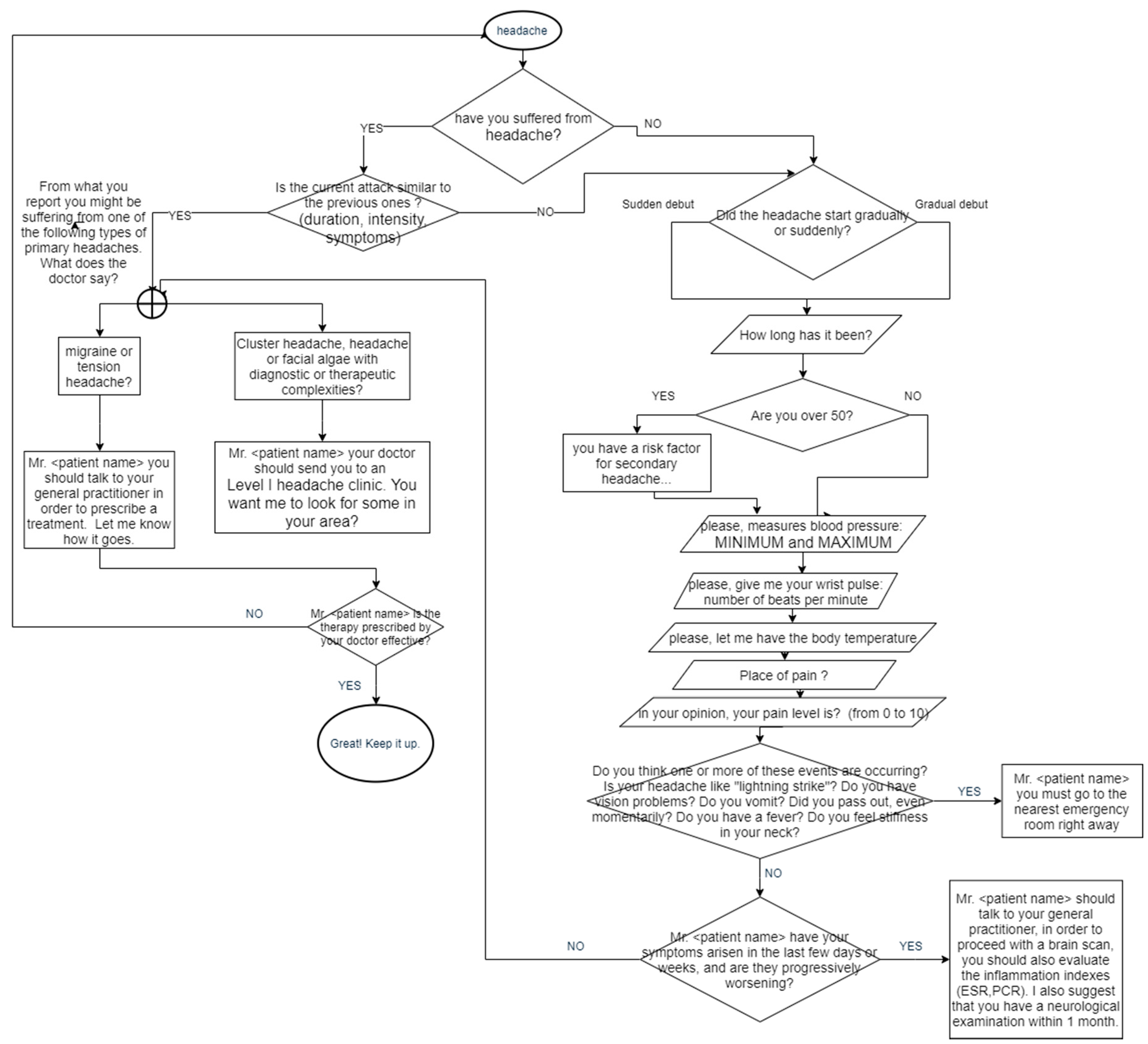
5. Results
6. Discussion
7. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Panella, M.; Zelm, R.; Sermeus, W.; Vanhaecht, K. Care pathways for the organization of patients’ care. Bull. Econ. Organ. Inform. Healthc. 2012, 28, 111–122. [Google Scholar] [CrossRef][Green Version]
- Dimauro, G.; Caivano, D.; Bevilacqua, V.; Girardi, F.; Napoletano, V. VoxTester, software for digital evaluation of speech changes in Parkinson disease. In Proceedings of the 2016 IEEE International Symposium on Medical Measurements and Applications (MeMeA), Benevento, Italy, 15–18 May 2016. [Google Scholar]
- Dimauro, G.; Girardi, F.; Gelardi, M.; Bevilacqua, V.; Caivano, D. Rhino-Cyt: A System for Supporting the Rhinologist in the Analysis of Nasal Cytology. In Intelligent Computing Theories and Application; Springer: Cham, Switzerland, 2018. [Google Scholar]
- Dimauro, G.; Ciprandi, G.; Deperte, F.; Girardi, F.; Ladisa, E.; Latrofa, S.; Gelardi, M. Nasal cytology with deep learning techniques. Int. J. Med Inform. 2019, 122, 13–19. [Google Scholar] [CrossRef] [PubMed]
- Dimauro, G.; Guarini, A.; Caivano, D.; Girardi, F.; Pasciolla, C.; Iacobazzi, A. Detecting clinical signs of anaemia from digital images of the palpebral conjunctiva. IEEE Access 2019, 7, 113488–113498. [Google Scholar] [CrossRef]
- Dimauro, G.; de Ruvo, S.; di Terlizzi, F.; Ruggieri, A.; Volpe, V.; Colizzi, L.; Girardi, F. Estimate of Anemia with New Non-Invasive Systems—A Moment of Reflection. Electronics 2020, 9, 780. [Google Scholar] [CrossRef]
- Dimauro, G.; Caivano, D.; Girardi, F.; Ciccone, M.M. The Patient Centered Electronic Multimedia Health Fascicle-EMHF. In Proceedings of the 2014 IEEE Workshop on Biometric Measurements and Systems for Security and Medical Applications (BIOMS) Proceedings, Rome, Italy, 17 October 2014. [Google Scholar]
- Dimauro, G.; Girardi, F.; Caivano, D.; Colizzi, L.N. Personal Health E-Record—Toward an enabling Ambient Assisted Living Technology for communication and information sharing between patients and care providers. In Italian Forum of Ambient Assisted Living; Springer: Cham, Switzerland, 2018. [Google Scholar]
- Allen, D.; Gillen, E.; Rixson, L. Systematic review of the effectiveness of integrated care pathways: What works, for whom, in which circumstances? Int. J. Evid. Based Healthc. 2009, 7, 61–74. [Google Scholar] [CrossRef] [PubMed]
- Aspland, E.; Gartner, D.; Harper, P. Clinical pathway modelling: A literature review. Health Syst. 2019, 1–23. [Google Scholar] [CrossRef]
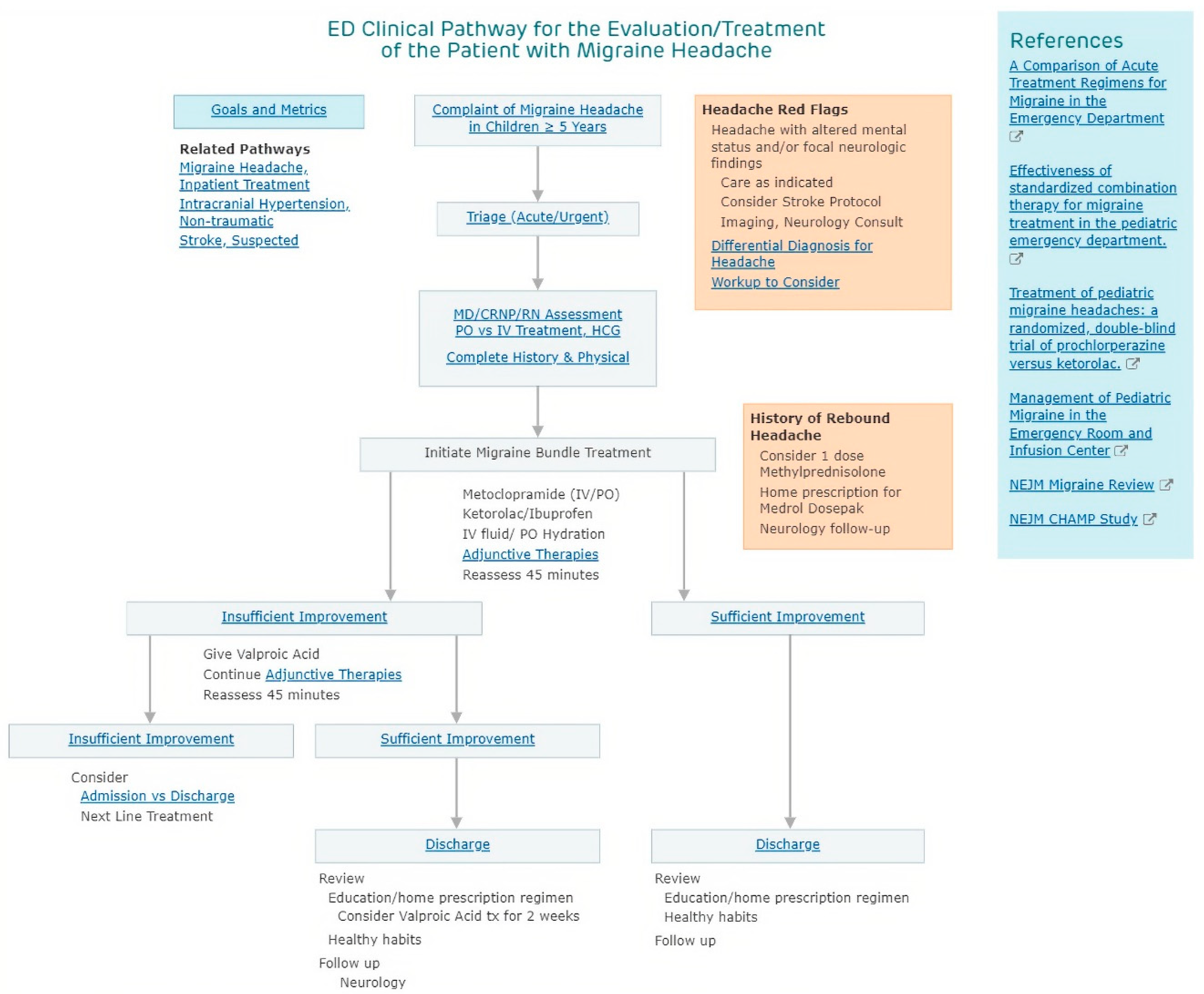
- Philadelphia, C.H.O. ED Clinical Pathway for the Evaluation/Treatment of the Patient with Migraine Headache. Available online: https://www.chop.edu/clinical-pathway/migraine-headache-emergent-care-clinical-pathway (accessed on 1 May 2020).
- Burwitz, M.; Schlieter, H.; Esswein, W. Modeling Clinical Pathways-Design and Application of a Domain-Specific Modeling Language. In Proceedings of the 11th International Conference on Wirtschaftsinformatik (WI2013), Leipzig, Germany, 27 February–1 March 2013. [Google Scholar]
- Stroppi, L.J.R.; Chiotti, O.; Villarreal, P.D. Extending BPMN 2.0: Method and tool support. In Business Process Model and Notation; Springer: Berlin/Heidelberg, Germany, 2011. [Google Scholar]
- Pawlewski, P.; Hoffa, P. Languages of process modeling. Res. Logist. Prod. 2014, 4, 221–229. [Google Scholar]
- Wang, W.; Ding, H.; Dong, J.; Ren, C. A Comparison of Business Process Modeling Methods. In Proceedings of the 2006 IEEE International Conference on Service Operations and Logistics, and Informatics, Shanghai, China, 21–23 June 2006. [Google Scholar]
- Amjad, A.; Azam, F.; Anwar, M.; Butt, W.; Rashid, M. Event-Driven Process Chain for Modeling and Verification of Business Requirements–A Systematic Literature Review. IEEE Access 2018, 6, 9027–9048. [Google Scholar] [CrossRef]
- Müller, R.; Rogge-Solti, A. BPMN for healthcare processes. In Proceedings of the 3rd Central-European Workshop on Services and their Composition, Karlsruhe, Germany, 21–22 February 2011. [Google Scholar]
- The Object Management Group. Business Process Model and Notation (BPMN) Version 2.0; OMG Specification; Object Management Group: Needham, MA, USA, 2011; pp. 22–31. [Google Scholar]
- The Object Management Group. Business Process Model and Notation. 2011. Available online: https://www.omg.org/spec/BPMN/2.0/ (accessed on 14 June 2019).
- Arevalo, C.; Escalona, M.; Ramos, I.; Domínguez-Muñoz, M. A metamodel to integrate business processes time perspective in BPMN 2.0. Inf. Softw. Technol. 2016, 77, 17–33. [Google Scholar] [CrossRef]
- Braun, R.; Schlieter, H.; Burwitz, M.; Esswein, W. BPMN4CP: Design and implementation of a BPMN extension for clinical pathways. In Proceedings of the IEEE International Conference on Bioinformatics and Biomedicine (BIBM ‘14), Belfast, UK, 2–5 November 2014. [Google Scholar]
- Braun, R.; Schlieter, H.; Burwitz, M.; Esswein, W. Extending a Business Process Modeling Language for Domain-Specific Adaptation in Healthcare. In Proceedings of the 12th International Conference on Wirtschaftsinformatik, Osnabrück, Germany, 4–6 March 2015. [Google Scholar]
- Braun, R.; Schlieter, H.; Burwitz, M.; Esswein, W. BPMN4CP Revised—Extending BPMN for Multi-perspective Modeling of Clinical Pathways. In Proceedings of the 2016 49th Hawaii International Conference on System Sciences (HICSS), Koloa, HI, USA, 10 March 2016. [Google Scholar]
- IEEE Std-Standard for Functional Modeling Language-1320.1; IEEE: Piscataway, NJ, USA, 1998.
- Kravchenko, O. Development of medical diagnostic decision support systems and their economic efficiency. Echnology Audit Prod. Reserves 2018, 2, 4–10. [Google Scholar] [CrossRef][Green Version]
- Weske, M. Business Process Modelling Foundation. In Business Process Management; Springer: Berlin/Heidelberg, Germany, 2019; pp. 71–122. [Google Scholar]
- Jeston, J. Business Process Management; Routledge: New York, NY, USA, 2014. [Google Scholar]
- Reis, L.; Maier, C.; Mattke, J.; Weitzel, T. Chatbots in Healthcare: Status Quo, Application Scenarios for Physicians and Patients and Future Directions. In Proceedings of the 28th European Conference on Information Systems (ECIS), Online AIS Conference, Marrakech, Morocco, 15–17 June 2020. [Google Scholar]
- Bhirud, N.; Tataale, S.; Randive, S.; Nahar, S. A Literature Review On Chatbots In Healthcare Domain. Int. J. Sci. Technol. Res. 2019, 8, 225–231. [Google Scholar]
- Zamanirad, S.; Benatallah, B.; Rodriguez, C.; Yaghoubzadehfard, M.; Bouguelia, S.; Brabra, H. State Machine Based Human-Bot Conversation Model and Services. In International Conference on Advanced Information Systems Engineering; Springer: Cham, Switzerland, 2020. [Google Scholar]
- Rooein, D.; Bianchini, D.; Leotta, F.; Mecella, M.; Paolini, P.; Pernici, B. Chatting About Processes in Digital Factories: A Model-Based Approach. In Enterprise, Business-Process and Information Systems Modeling; Springer: Cham, Switzerland, 2020; pp. 70–84. [Google Scholar]
- López, A.; Sànchez-Ferreres, J.; Carmona, J.; Padró, L. From process models to chatbots. In International Conference on Advanced Information Systems Engineering; Springer: Cham, Switzerland, 2019. [Google Scholar]
- Ayanouz, S.; Abdelhakim, B.A.; Benhmed, M. A Smart Chatbot Architecture based NLP and Machine Learning for Health Care Assistance. In Proceedings of the 3rd International Conference on Networking, Information Systems & Security, Modena, Italy, 19–21 February 2020. [Google Scholar]
- Pereira, J.; Díaz, O. A quality analysis of Facebook Messenger’s most popular. In Proceedings of the Symposium on Applied Computing, Pau, France, 9–13 April 2018. [Google Scholar]
- 2020. Available online: https://www.safeinbreastfeeding.com/safedrugbot-chatbot-medical-assistant/ (accessed on 1 June 2020).
- Caley, M.S.K. Estimating the future healthcare costs of an aging population in the UK: Expansion of morbidity and the need for preventative care. J. Public Health 2011, 33, 117–122. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, M.N.; Toor, A.S.; O’Neil, K.; Friedland, D. Cognitive computing and the future of health care cognitive computing and the future of healthcare: The cognitive power of IBM Watson has the potential to transform global personalized medicine. Ieee Pulse 2017, 8, 4–9. [Google Scholar] [CrossRef] [PubMed]
- 2020. Available online: http://www.superizzy.ai/ (accessed on 1 June 2020).
- 2020. Available online: https://getforksy.com/ (accessed on 1 June 2020).
- 2020. Available online: https://www.babylonhealth.com/ (accessed on 1 June 2020).
- Iacobucci, G. Babylon Health holds talks with “significant” number of NHS trusts. BMJ 2020, 368, m266. [Google Scholar] [CrossRef] [PubMed]
- Chittamuru, D.; Ramondt, S.; Kravitz, R.; Ramirez, S. Who uses an online intelligent medical information system and what do they do with that information? Results from a pilot study of users of Buoy Health. In APHA’s 2019 Annual Meeting and Expo; American Public Health Association: Washington, DC, USA, 2019. [Google Scholar]
- 2020. Available online: https://www.buoyhealth.com/ (accessed on 1 June 2020).
- 2020. Available online: https://www.facebook.com/CancerChatbot/ (accessed on 1 June 2020).
- Available online: http://www.sensely.com/ (accessed on 1 June 2020).
- Available online: https://gyant.com/ (accessed on 1 June 2020).
- Available online: https://woebot.io (accessed on 1 June 2020).
- Fitzpatrick, K.K.; Darcy, A.; Vierhile, M. Delivering cognitive behavior therapy to young adults with symptoms of depression and anxiety using a fully automated conversational agent (Woebot): A randomized controlled trial. Jmir Ment. Health 2017, 4, e19. [Google Scholar] [CrossRef] [PubMed]
- Merry, S.N.; Stasiak, K.; Shepherd, M.; Frampton, C.; Fleming, T.; Lucassen, M.F. The effectiveness of SPARX, a computerised self help intervention for adolescents seeking help for depression: Randomised controlled non-inferiority trial. BMJ 2012, 344, e2598. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://www.healthtap.com (accessed on 1 June 2020).
- Your.MD. Available online: https://www.your.md (accessed on 1 June 2020).
- Ada. Available online: https://ada.com (accessed on 1 June 2020).
- Zagorecki, A.; Orzechowski, P.; Hołownia, K. Online diagnostic system based on Bayesian networks. In Conference on Artificial Intelligence in Medicine in Europe; Springer: Berlin/Heidelberg, Germany, 2013; pp. 145–149. [Google Scholar]
- bots4health. Available online: https://cristinasantamarina.com/work/bots4health/ (accessed on 1 June 2020).
- Tschanz, M.; Dorner, T.L.; Denecke, K. eMedication Meets eHealth with the Electronic Medication Management Assistant (eMMA). Stud. Health Technol. Inform. 2017, 236, 196–203. [Google Scholar]
- Thalheim, B. The enhanced entity-relationship model. In Handbook of Conceptual Modeling; Springer: Berlin/Heidelberg, Germany, 2011; pp. 165–206. [Google Scholar]
- Active Knowledge Modeling: Simplifying BPMN 2.0. 2010. Available online: https://activeknowledgemodeling.com/2010/03/23/simplifying-bpmn-2-0/ (accessed on 14 May 2020).
- Mills, K. Computer-Supported Cooperative Work; Marcel Dekker: New York, NY, USA, 2003; pp. 666–677. [Google Scholar]
- Laranjo, L.; Dunn, A.; Tong, H.; Kocaballi, A.; Chen, J.; Bashir, R.; Surian, D.; Gallego, B.; Magrabi, F.; Lau, A.; et al. Conversational agents in healthcare: A systematic review. J. Am. Med. Inform. Assoc. 2018, 25, 1248–1258. [Google Scholar] [CrossRef] [PubMed]
- Linn, L.; Koo, M. Blockchain for health data and its potential use in health it and health care related research. In ONC/NIST Use of Blockchain for Healthcare and Research Workshop; ONC/NIST: Gaithersburg, MD, USA, 2016. [Google Scholar]
- Girardi, F.; de Gennaro, G.; Colizzi, L.; Convertini, N. Improving the Healthcare Effectiveness: The Possible Role of EHR, IoMT and Blockchain. Electronics 2020, 9, 884. [Google Scholar] [CrossRef]
- Fielding, R.T.; Taylor, R.N.; Erenkrantz, J.R.; Gorlick, M.M.; Whitehead, J.; Khare, R.; Oreizy, P. Reflections on the REST architectural style and” principled design of the modern web architecture. In Proceedings of the 2017 11th Joint Meeting on Foundations of Software Engineering, Paderborn, Germany, 4–8 September 2017; pp. 4–14. [Google Scholar]
- Emilia-Romagna, R. Organizzazione Dell’assistenza Integrata al Paziente con Cefalea: Percorso Cefalea-Approvazione Linee Guida per le Aziende Sanitarie Della Regione Emilia-Romagna. 2013. Available online: https://bur.regione.emilia-romagna.it/bur/area-bollettini/bollettini-pubblicati/2013/n.-372-del-12.12.2013.2013-12-11.0512037846/organizzazione-dellassistenza-integrata-al-paziente-con-cefalea-percorso-cefalea-approvazione-linee-guida-per-le-aziende-sanit (accessed on 15 June 2019).
- Ferragina, P.; Scaiella, U. Tagme: On-the-fly annotation of short text fragments (by wikipedia entities). In Proceedings of the 19th ACM international conference on Information and knowledge management, Toronto, ON, Canada, 26–30 October 2010. [Google Scholar]
- TAGme API. Available online: https://sobigdata.d4science.org/web/tagme/tagme-help (accessed on 1 September 2019).
- ISO. IEC25010: 2011 systems and software engineering—Systems and software quality requirements and evaluation (square)–system and software quality models. Int. Organ. Stand. 2011, 34, 2910. [Google Scholar]





| BPMN2.0 Use Modality | Class in the Meta-Model |
|---|---|
| Simple | start, end, task, sequence flow, AND, OR, subprocess |
| Descriptive | add task types, event types, swim lanes, message flows, data objects |
| Analytic | full enterprise architecture modelling |
| Executable | complete set for executable models |
| Chatbot Name | Main Functions | Underlying Methodology and/or Technology | References |
|---|---|---|---|
| SafedrugBot | Helps doctor access right information about drug dosage; breastfeeding pathway assistant | It retrieves information from open data dataset | [35] |
| Florence chatbot | Reminds patients to take pills; tracks body weight, tracks moods; finds a doctor or pharmacy nearby | AI and machine learning | [36] |
| IBM Watson | Symptom checker, analyzes high volumes of data, understands complex questions posed in natural language, and proposes EBM answers | AI, natural conversation, deep learning techniques to derive question’s intent | [37] |
| Izzy | Helps women track periods; provides information on the user’s sexual issues and menstrual health | Conversational agent | [38] |
| Forksy | Tracks calories; promotes healthy eating habits | Automated feedback powered by AI technology | [39] |
| Babylon Health | Remote consultation with healthcare professionals and doctors; patient’s medical database; symptom checker | Consultation driven by AI Probabilistic Graph Model with nodes annotated by medical ontologies (Snomed, NCI) | [40,41] |
| Buoy Health | Assists patients in diagnosis | AI for diagnoses. Algorithm was trained on clinical data from over 18,000 clinical papers | [42,43] |
| CancerChatbot | Offers detailed information on cancer and related topics | NLP, flow dedicated to training supporters in how to talk to a cancer patient and how to be helpful | [44] |
| Sensely | Tracks health symptoms using both text and speech communication; diagnosis formulation | AI to recommend diagnoses based on patient symptoms | [45] |
| GYANT | Symptom checker | Artificial intelligence-enabled platform, machine-learning intelligence, physician oversight | [46] |
| Woebot | Studies patient mood and personality and suggests remedies as a therapist for the depression | Artificially intelligent chatbot designed from simulating human cognitive-behavioral therapy (CBT) | [47,48,49] |
| HealthTap | Vast repository of knowledge available to patients | AI; question prompts to submit symptoms | [50] |
| Your.Md | Symptom checker | AI and machine learning. It constructs a Bayesian network with massive medical knowledge to compute the most likely cause of an indisposition | [51] |
| Ada Health | Symptom checker; analyzes patient-related data, past medical history, symptoms and risk factors | AI-based database, machine learning | [52] |
| Infermedica | Symptom checker through natural language processing, using chat (text) and images | AI and machine learning, automated generation of Bayesian network models | [53] |
| Bots4Health | Sexual and reproductive health; chats about a wide range of health issues | Conversational interfaces, Chatfuel and Dialogflow NLP API | [54] |
| eMMA | Electronic medication assistant, clinical data repository | ConversationAl user interface (CUI), query mode answer retrieval by key words | [55] |
| Process Design Standard | Entity in the Data Model |
|---|---|
| IDEF0 | PROCESS_NODE, TASK, INPUT, OUTPUT |
| FLOW CHART | PROCESS_NODE, TASK, CONDITION, INPUT, OUTPUT |
| UML ACTIVITY DIAGRAM | PROCESS_NODE, TASK, SUBJECT, CONDITION, INPUT, OUTPUT |
| EPC | PROCESS_NODE, TASK, CONDITION, EVENT, INPUT, OUTPUT |
| BPMN 2.0 | PROCESS_NODE, EVENT, TASK, SUBJECT, CONDITION, INPUT, OUTPUT |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ardito, C.; Caivano, D.; Colizzi, L.; Dimauro, G.; Verardi, L. Design and Execution of Integrated Clinical Pathway: A Simplified Meta-Model and Associated Methodology. Information 2020, 11, 362. https://doi.org/10.3390/info11070362
Ardito C, Caivano D, Colizzi L, Dimauro G, Verardi L. Design and Execution of Integrated Clinical Pathway: A Simplified Meta-Model and Associated Methodology. Information. 2020; 11(7):362. https://doi.org/10.3390/info11070362
Chicago/Turabian StyleArdito, Carmelo, Danilo Caivano, Lucio Colizzi, Giovanni Dimauro, and Loredana Verardi. 2020. "Design and Execution of Integrated Clinical Pathway: A Simplified Meta-Model and Associated Methodology" Information 11, no. 7: 362. https://doi.org/10.3390/info11070362
APA StyleArdito, C., Caivano, D., Colizzi, L., Dimauro, G., & Verardi, L. (2020). Design and Execution of Integrated Clinical Pathway: A Simplified Meta-Model and Associated Methodology. Information, 11(7), 362. https://doi.org/10.3390/info11070362






