Social, Economic and Ecological Drivers of Tuberculosis Disparities in Bangladesh: Implications for Health Equity and Sustainable Development Policy
Abstract
1. Introduction
Objectives
- To identify the social, economic, and ecological determinants contributing to the disproportionate burden of tuberculosis among low-SES populations in Bangladesh.
- To examine proximal mechanisms through which these determinants influence the TB burden.
- To generate sustainable policy recommendations aligned with the Sustainable Development Goals, WHO End TB Strategy, and Quadruple Aims towards Planetary Health Systems.
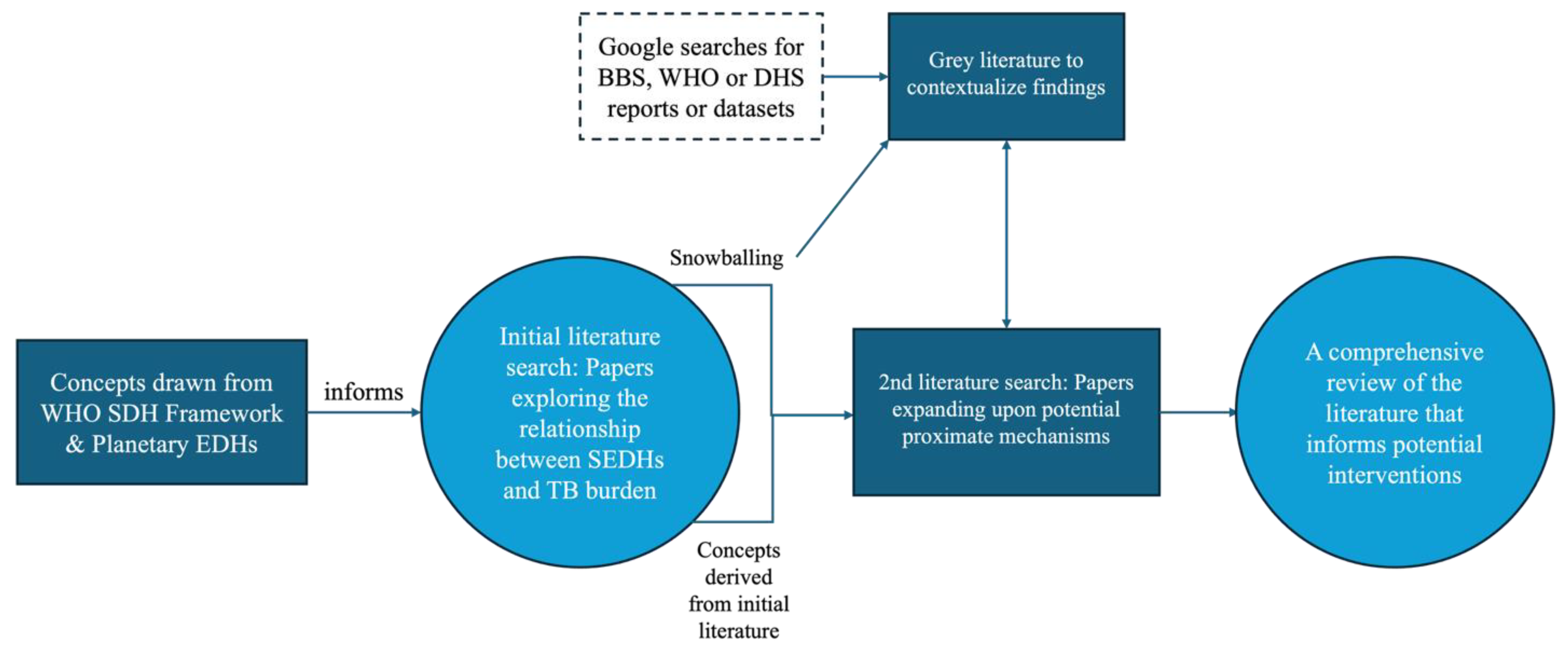
2. Methods
3. Results
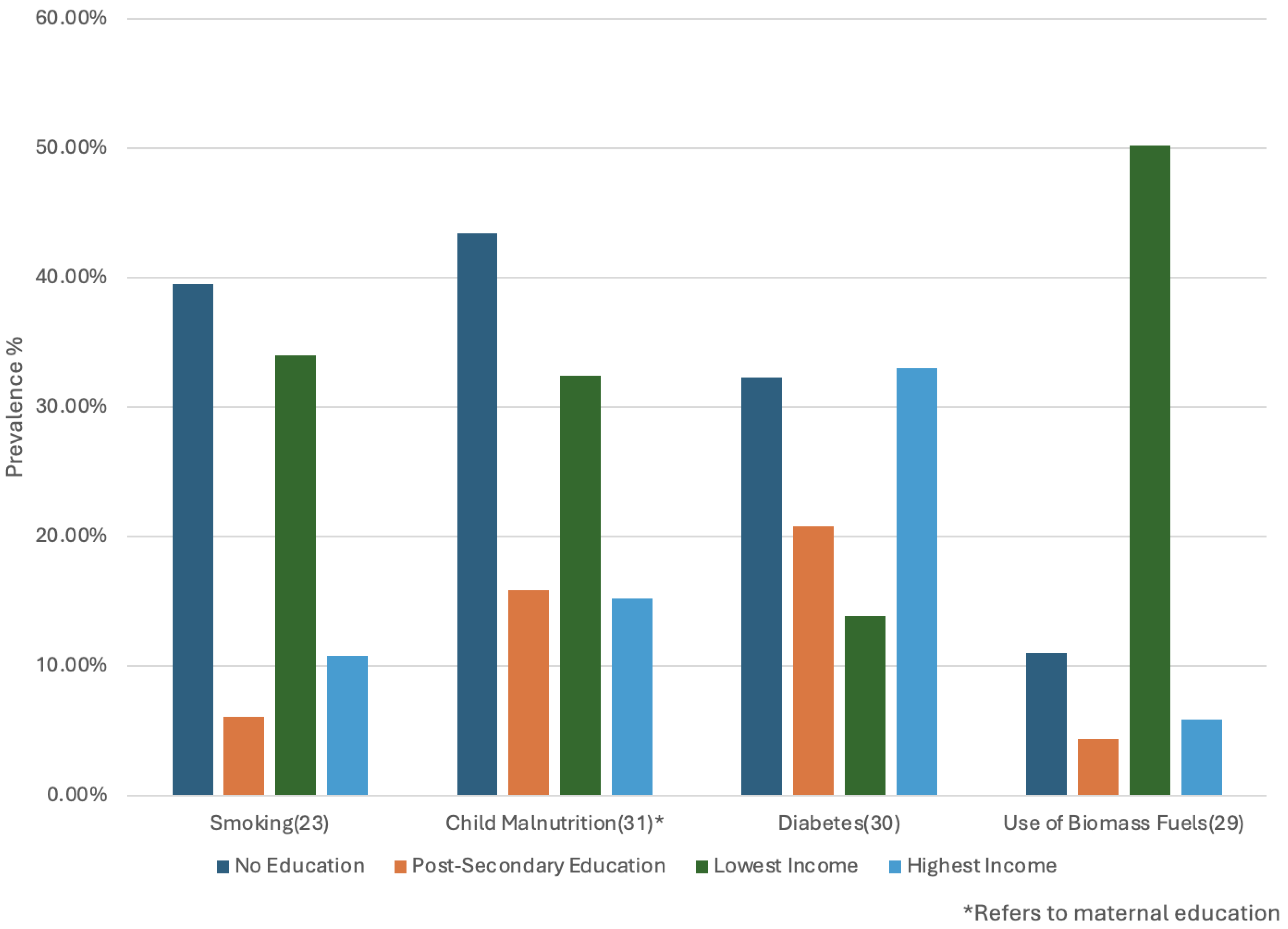
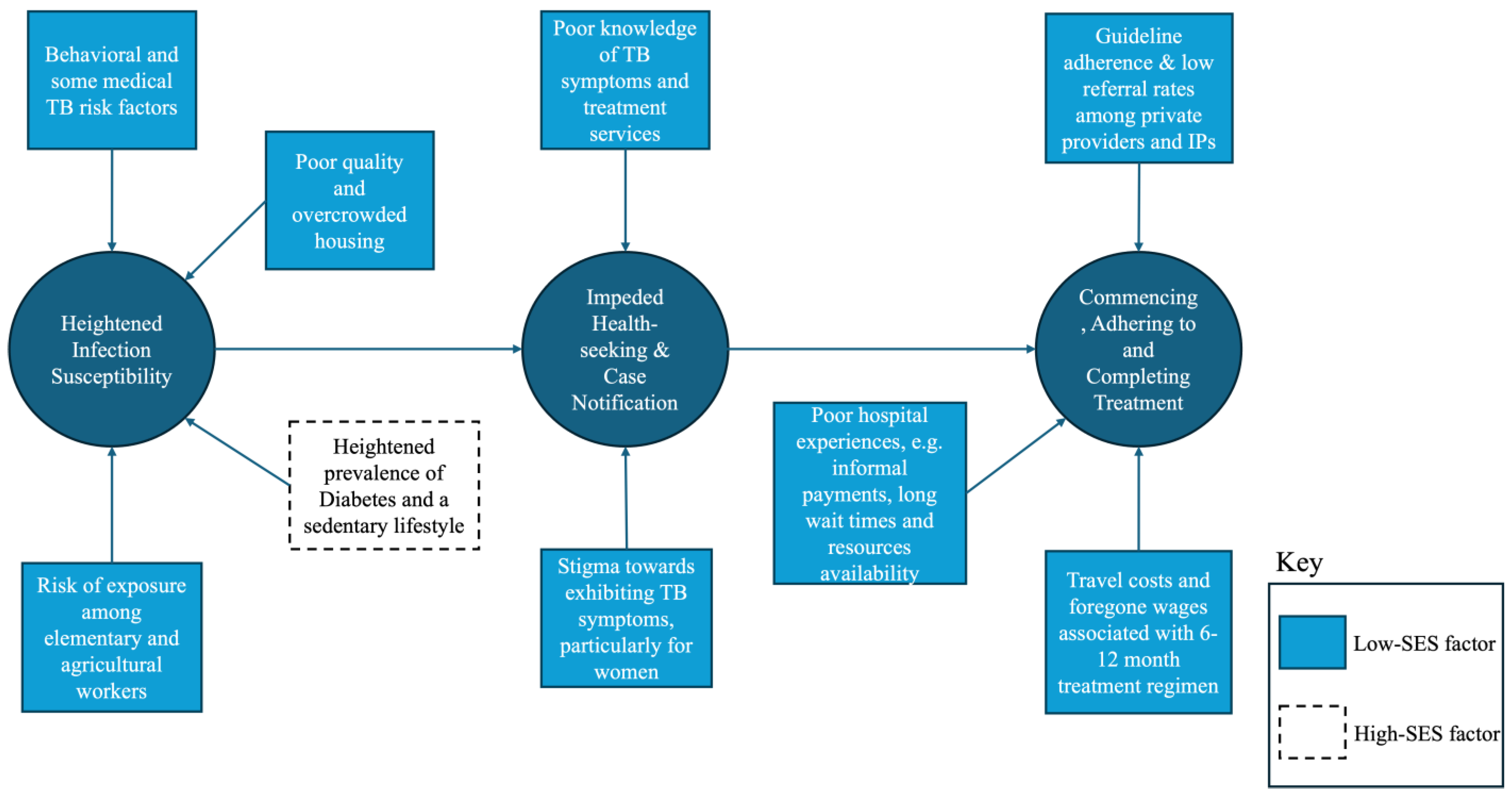
3.1. Distribution of TB Risk Factors by SES
3.2. Educational Attainment, Stigma and Barriers to Case Notification
3.3. Direct and Indirect Financial Barriers to TB Treatment
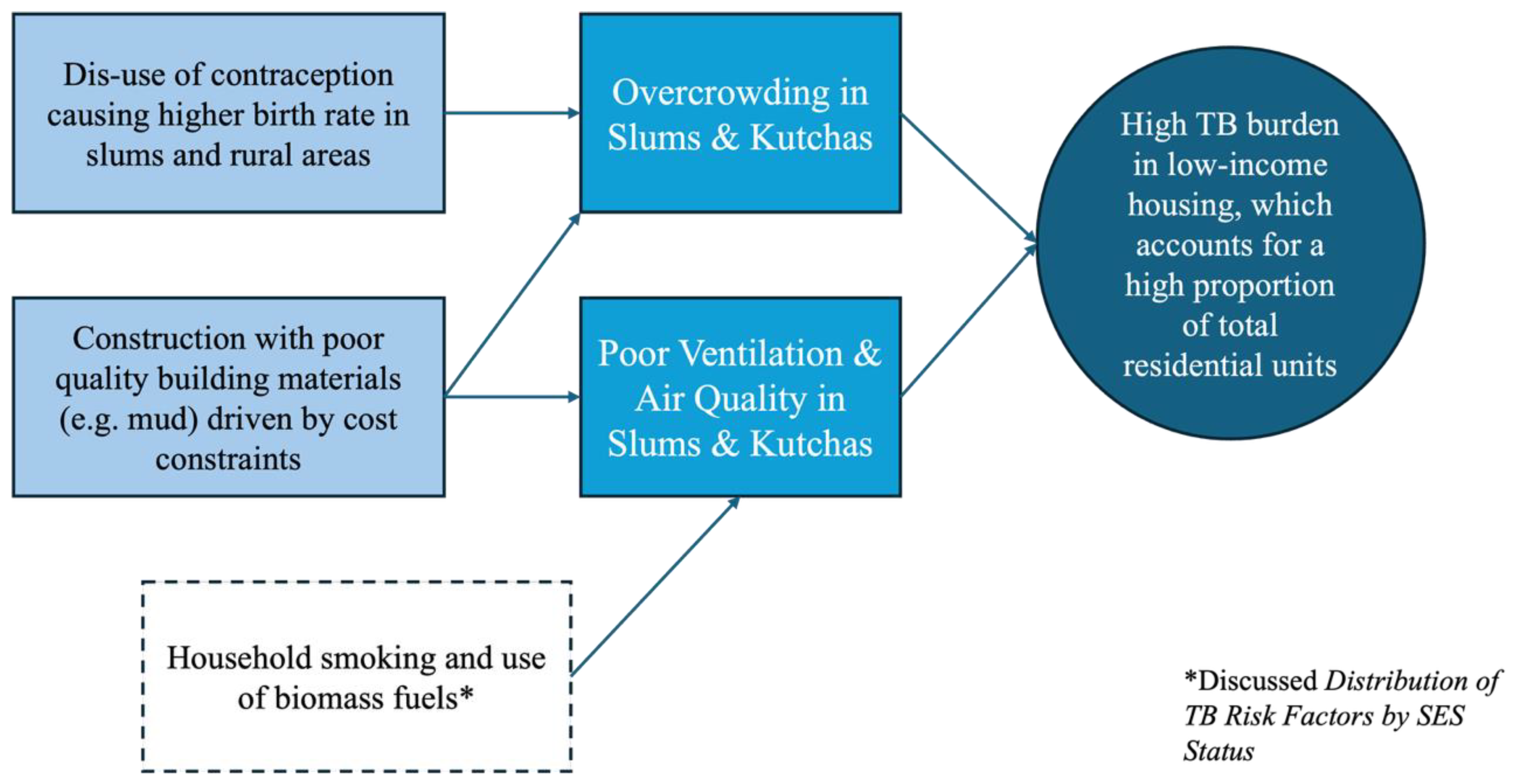
3.4. TB-Prone Characteristics of Low-SES Housing
3.5. Occupational Exposure Among Elementary and Agricultural Workers
4. Discussion
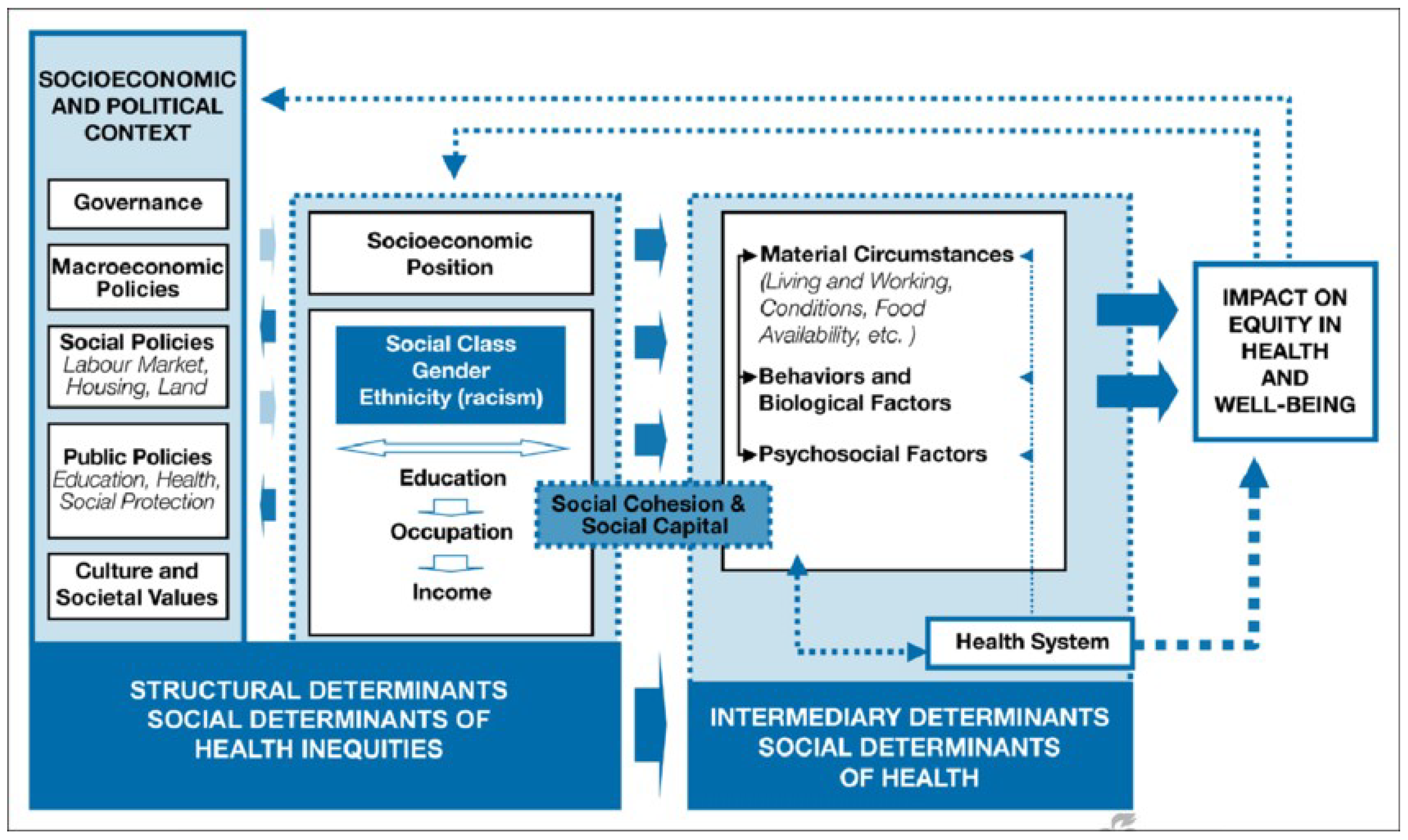
4.1. Contextualising Results Within the WHO SDH Framework
4.2. Recommendations
4.2.1. Recommendation 1: Streamline Diagnostic and Treatment Availability
4.2.2. Recommendation 2: Reduce Household and Workplace Overcrowding
4.2.3. Recommendation 3: Promote Gender Equality in Educational Attainment
4.2.4. Recommendation 4: Facilitate Integration with Private Providers and IPs
4.3. Research Gaps
4.4. Limitations
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Global Health Estimates 2021: Deaths by Cause, Age, Sex, by Country and by Region; World Health Organisation: Geneva, Switzerland, 2022. [Google Scholar]
- World Health Organization. WHO Global Lists of High Burden Countries for Tuberculosis (TB), TB/HIV and Multidrug/Rifampicin-Resistant TB; World Health Organisation Global Tuberculosis Programme: Geneva, Switzerland, 2021. [Google Scholar]
- Welfare/WHO MoHF. National Guideline and Operational Manual for Tuberculosis; Ministry of Health & Family Welfare/WHO: Dhaka, Bangladesh, 2021. [Google Scholar]
- Maher, D.; Mikulencak, M. A Guide to Understanding the WHO-recommended TB Control Strategy Known as DOTS; World Health Organisation: Geneva, Switzerland, 1999. [Google Scholar]
- Lonnroth, K.; Jaramillo, E.; Williams, B.G.; Dye, C.; Raviglione, M. Drivers of tuberculosis epidemics: The role of risk factors and social determinants. Soc. Sci. Med. 2009, 68, 2240–2246. [Google Scholar] [CrossRef] [PubMed]
- Whitmee, S.; Haines, A.; Beyrer, C.; Boltz, F.; Capon, A.G.; de Souza Dias, B.F.; Ezeh, A.; Frumkin, H.; Gong, P.P.; Head, P.; et al. Safeguarding human health in the Anthropocene epoch: Report of The Rockefeller Foundation-Lancet Commission on planetary health. Lancet 2015, 386, 1973–2028. [Google Scholar] [CrossRef]
- Solar, O.; Irwin, A. A Conceptual Framework For Action on the Social Determinants of Health; World Health Organisation: Geneva, Switzerland, 2010; Available online: https://www.who.int/publications/i/item/9789241500852 (accessed on 27 January 2024).
- Pham, L.T.; Kumar, P.; Dahana, W.D.; Nguyen, D.H. Promoting global health transdisciplinary research for planetary health: Towards achieving the 2030 Agenda for Sustainable Development. J. Glob. Health 2023, 13, 03007. [Google Scholar] [CrossRef]
- Sayed, Z. Transforming our world: The 2030 agenda for sustainable development. Ethics Crit. Think. J. 2015, 2015, 3. [Google Scholar]
- World Health Organization. The End TB Strategy; World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- Perilli, A.; Adduci, A.; Ricciardi, W.; de Belvis, A.G.; Cadeddu, C. Towards planetary health systems: A manifesto for a revised quadruple aim for healthcare improvement. Glob. Sustain. 2024, 7, e70. [Google Scholar] [CrossRef]
- Hossain, S.; Quaiyum, M.A.; Zaman, K.; Banu, S.; Husain, M.A.; Islam, M.A.; Cooreman, E.; Borgdorff, M.; Lönnroth, K.; Salim, A.H.; et al. Socio economic position in TB prevalence and access to services: Results from a population prevalence survey and a facility-based survey in Bangladesh. PLoS ONE 2012, 7, e44980. [Google Scholar] [CrossRef]
- Irfan, S.D.; Faruque, M.O.; Islam, M.U.; Sanjoy, S.S.; Afrin, D.; Hossain, A. Socio-Demographic Determinants of Adult Tuberculosis: A Matched Case-Control Study in Bangladesh. Am. J. Infect. Dis. 2017, 13, 32–37. [Google Scholar] [CrossRef][Green Version]
- Banu, S.; Rahman, M.T.; Uddin, M.K.; Khatun, R.; Ahmed, T.; Rahman, M.M.; Husain, M.A.; van Leth, F. Epidemiology of tuberculosis in an urban slum of Dhaka City, Bangladesh. PLoS ONE 2013, 8, e77721. [Google Scholar] [CrossRef]
- Mondal, M.N.I.; Chowdhury, M.R.K.; Sayem, M.A. Associated Factors of Pulmonary Tuberculosis in Rajshahi City of Bangladesh. J. Human. Ecol. 2017, 45, 61–68. [Google Scholar] [CrossRef]
- Shariful, M.; Uddin, R.; Das, S. The burden of diseases and risk factors in Bangladesh, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet Glob. Health 2023, 11, e1931–e1942. [Google Scholar]
- Kundu, S.; Marzan, M.; Gan, S.H.; Islam, M.A. Prevalence of Antibiotic-Resistant Pulmonary Tuberculosis in Bangladesh: A Systematic Review and Meta-Analysis. Antibiotics 2020, 9, 710. [Google Scholar] [CrossRef] [PubMed]
- Islam, M.S.; Gurley, E.S.; Banu, S.; Hossain, K.; Heffelfinger, J.D.; Amin Chowdhury, K.I.; Ahmed, S.; Afreen, S.; Islam, M.T.; Rahman, S.M.M.; et al. Prevalence and incidence of tuberculosis infection among healthcare workers in chest diseases hospitals, Bangladesh: Putting infection control into context. PLoS ONE 2023, 18, e0291484. [Google Scholar] [CrossRef]
- Berg, R.D.; Levitte, S.; O’Sullivan, M.P.; O’Leary, S.M.; Cambier, C.J.; Cameron, J.; Moens, C.B.; Tobin, D.M.; Keane, J.; Ramakrishnan, L. Lysosomal Disorders Drive Susceptibility to Tuberculosis by Compromising Macrophage Migration. Cell 2016, 165, 139–152. [Google Scholar] [CrossRef]
- Karim, M.R.; Alam, M.A.; Mamun, S.A.A.; Rahman, M.A. Sociocultural and host factors related to extra-pulmonary tuberculosis in rural Bangladesh: A case control study. Bangladesh Med. Res. Counc. Bull. 2015, 41, 59–66. [Google Scholar] [CrossRef]
- Silva, D.R.; Munoz-Torrico, M.; Duarte, R.; Galvao, T.; Bonini, E.H.; Arbex, F.F.; Arbex, M.A.; Augusto, V.M.; Rabahi, M.F.; Mello, F.C.Q. Risk factors for tuberculosis: Diabetes, smoking, alcohol use, and the use of other drugs. J. Bras. Pneumol. 2018, 44, 145–152. [Google Scholar] [CrossRef]
- Balinda, I.G.; Sugrue, D.D.; Ivers, L.C. More Than Malnutrition: A Review of the Relationship Between Food Insecurity and Tuberculosis. Open Forum. Infect. Dis. 2019, 6, ofz102. [Google Scholar] [CrossRef]
- Zhao, L.; Mbulo, L.; Twentyman, E.; Palipudi, K.; King, B.A. Disparities in smokeless tobacco use in Bangladesh, India, and Pakistan: Findings from the Global Adult Tobacco Survey, 2014–2017. PLoS ONE 2021, 16, e0250144. [Google Scholar] [CrossRef]
- Huque, R.; Abdullah, S.M.; Hossain, M.N.; Nargis, N. Price elasticity of cigarette smoking in Bangladesh: Evidence from the Global Adult Tobacco Surveys (GATS). Tob. Control. 2024, 33, s51–s58. [Google Scholar] [CrossRef] [PubMed]
- Khandker, N.N.; Biswas, T.; Khan, A.N.S.; Hasib, E.; Rawal, L.B. Socio-demographic characteristics and tobacco use among the adults in urban slums of Dhaka, Bangladesh. Tob. Induc. Dis. 2017, 15, 26. [Google Scholar] [CrossRef] [PubMed]
- Leung, C.C.; Lam, T.H.; Ho, K.S.; Yew, W.W.; Tam, C.M.; Chan, W.M.; Law, W.S.; Chan, C.K.; Chang, K.C.; Au, K.F. Passive smoking and tuberculosis. Arch. Intern. Med. 2010, 170, 287–292. [Google Scholar] [CrossRef]
- Haque, M.A.; Barman, N.; Islam, M.T.; Mannan, M.; Khan, M.H.; Karim, M.R.; Rob, M.A.; Hossain, M.A. Biomass Fuel Smoke and Tuberculosis: A Case-Control Study. Mymensingh Med. J. 2016, 25, 31–38. [Google Scholar] [PubMed]
- Hassan, M.K.; Halder, P.; Pelkonen, P.; Pappinen, A. Rural households’ preferences and attitudes towards biomass fuels—Results from a comprehensive field survey in Bangladesh. Energy Sustain. Soc. 2013, 3, 24. [Google Scholar] [CrossRef]
- Rasel, S.M.; Siddique, A.B.; Nayon, M.F.S.; Suzon, M.S.M.; Amin, S.; Mim, S.S.; Hossain, M.S. Assessment of the association between health problems and cooking fuel type, and barriers towards clean cooking among rural household people in Bangladesh. BMC Public Health 2024, 24, 512. [Google Scholar] [CrossRef] [PubMed]
- Sarker, M.; Barua, M.; Guerra, F.; Saha, A.; Aftab, A.; Latif, A.H.; Islam, S.; Islam, A. Double Trouble: Prevalence and Factors Associated with Tuberculosis and Diabetes Comorbidity in Bangladesh. PLoS ONE 2016, 11, e0165396. [Google Scholar] [CrossRef]
- National Institute of Population Research and Training (NIPORT); ICF. Bangladesh Demographic and Health Survey (BDHS) 2022 Preliminary Findings; NIPORT: Dhaka, Bangladesh; ICF: Rockville, MD, USA, 2023.
- Sarker, A.R.; Hossain, Z.; Morton, A. Drivers and distribution of the household-level double burden of malnutrition in Bangladesh: Analysis of mother-child dyads from a national household survey. Public Health Nutr. 2022, 25, 3158–3171. [Google Scholar] [CrossRef]
- Hasan, M.M.; Uddin, J.; Pulok, M.H.; Zaman, N.; Hajizadeh, M. Socioeconomic Inequalities in Child Malnutrition in Bangladesh: Do They Differ by Region? Int. J. Environ. Res. Public Health 2020, 17, 1079. [Google Scholar] [CrossRef]
- Ter Beek, L.; Bolhuis, M.S.; Jager-Wittenaar, H.; Brijan, R.X.D.; Sturkenboom, M.G.G.; Kerstjens, H.A.M.; de Lange, W.C.M.; Tiberi, S.; van der Werf, T.S.; Alffenaar, J.C.; et al. Malnutrition assessment methods in adult patients with tuberculosis: A systematic review. BMJ Open 2021, 11, e049777. [Google Scholar] [CrossRef]
- Gupta, R.D.; Chakraborty, P.A.; Hossain, M.B. Association of household wealth and education level with hypertension and diabetes among adults in Bangladesh: A propensity score-based analysis. Trop. Med. Int. Health 2021, 26, 1047–1056. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization, Global Tuberculosis Programme. Global Tuberculosis Control: WHO Report; World Health Organisation, Global Tuberculosis Programme: Geneva, Switzerland, 2024; Report No.: 2223-2583. [Google Scholar]
- Chowdhury, M.R.; Rahman, M.S.; Mondal, M.N.; Sayem, A.; Billah, B. Social Impact of Stigma Regarding Tuberculosis Hindering Adherence to Treatment: A Cross Sectional Study Involving Tuberculosis Patients in Rajshahi City, Bangladesh. Jpn. J. Infect. Dis. 2015, 68, 461–466. [Google Scholar] [CrossRef]
- Bam, K.; Bhatt, L.P.; Thapa, R.; Dossajee, H.K.; Angdembe, M.R. Illness perception of tuberculosis (TB) and health seeking practice among urban slum residents of Bangladesh: A qualitative study. BMC Res. Notes 2014, 7, 572. [Google Scholar] [CrossRef]
- (BBS) BBoS. Slum Statistics of Bangladesh; Bangladesh Bureau of Statistics (BBS): Dhaka, Bangladesh, 2022.
- Barua, M.; Van Driel, F.; Jansen, W. Tuberculosis and the sexual and reproductive lives of women in Bangladesh. PLoS ONE 2018, 13, e0201134. [Google Scholar] [CrossRef]
- Mondal, M.N.; Nazrul, H.M.; Chowdhury, M.R.; Howard, J. Socio-demographic factors affecting knowledge level of Tuberculosis patients in Rajshahi City, Bangladesh. Afr. Health Sci. 2014, 14, 855–865. [Google Scholar] [CrossRef] [PubMed]
- Ehsanul Huq, K.; Moriyama, M.; Zaman, K.; Chisti, M.J.; Long, J.; Islam, A.; Hossain, S.; Shirin, H.; Raihan, M.J.; Chowdhury, S.; et al. Health seeking behaviour and delayed management of tuberculosis patients in rural Bangladesh. BMC Infect. Dis. 2018, 18, 515. [Google Scholar] [CrossRef]
- Hossain, M.R.; Islam, M.S.; Akter, S.; Anisuzzaman, A.H.M.; Maruf, M.A.-A.; Mohammed, N. Impact of Education on Non-Compliance and MDR TB Risk: Specialized Hospital Study. Saudi J. Med. 2023, 8, 59–63. [Google Scholar] [CrossRef]
- Sarker, A.R.; Akram, R.; Ali, N.; Sultana, M. Coverage and factors associated with full immunisation among children aged 12–59 months in Bangladesh: Insights from the nationwide cross-sectional demographic and health survey. BMJ Open 2019, 9, e028020. [Google Scholar] [CrossRef]
- Karim, F.; Johansson, E.; Diwan, V.K.; Kulane, A. Community perceptions of tuberculosis: A qualitative exploration from a gender perspective. Public Health 2011, 125, 84–89. [Google Scholar] [CrossRef] [PubMed]
- Sarker, M.; Homayra, F.; Rawal, L.B.; Kabir, R.; Aftab, A.; Bari, R.; Dzokoto, A.; Shargie, E.B.; Islam, S.; Islam, A.; et al. Urban-rural and sex differentials in tuberculosis mortality in Bangladesh: Results from a population-based survey. Trop. Med. Int. Health 2019, 24, 109–115. [Google Scholar] [CrossRef] [PubMed]
- Begum, V.; de Colombani, P.; Das Gupta, S.; Salim Md, A.H.; Hussain, H.; Pietroni, M.; Rahman, S.; Pahan, D.; Borgdorff, M.W. Tuberculosis and patient gender in Bangladesh: Sex differences in diagnosis and treatment outcome. Int. J. Tuberc. Lung Dis. 2001, 5, 604–610. [Google Scholar]
- Karim, F.; Ahmed, F.; Begum, I.; Johansson, E.; Diwan, V.K. Female-male differences at various clinical steps of tuberculosis management in rural Bangladesh. Int. J. Tuberc. Lung Dis. 2008, 12, 1336–1339. [Google Scholar]
- Ferdos, M.A.; Islam, M.T. Tuberculosis Burden in Bangladesh: Progressions and Challenges of Continuing Control Intervention. Saudi J. Med. 2023, 8, 446–456. [Google Scholar] [CrossRef]
- Daru, P.; Zannat, F.; Jassim Al Mossawi, J.; Haumba, S.; Olkannen, A.; Chakraborty, K.; Kak, N. Delays in Diagnosis and Treatment of Tuberculosis in Bangladesh: A Cross-Sectional Study and Program Implications. ED Pulmonol. Respir. Med. 2019, 8, 32–45. [Google Scholar]
- Zafar Ullah, A.N.; Huque, R.; Husain, A.; Akter, S.; Islam, A.; Newell, J.N. Effectiveness of involving the private medical sector in the National TB Control Programme in Bangladesh: Evidence from mixed methods. BMJ Open 2012, 2, e001534. [Google Scholar] [CrossRef]
- Ahmed, S.M. Exploring Health-Seeking Behaviour of Disadvantaged Populations in Rural Bangladesh; Karolinska Institute: Stockholm, Sweden, 2005. [Google Scholar]
- Rifat, M.; Rusen, I.D.; Islam, M.A.; Enarson, D.A.; Ahmed, F.; Ahmed, S.M.; Karim, F. Why are tuberculosis patients not treated earlier? A study of informal health practitioners in Bangladesh. Int. J. Tuberc. Lung Dis. 2011, 15, 647–651. [Google Scholar] [CrossRef]
- Hossain, S.; Zaman, K.; Quaiyum, A.; Banu, S.; Husain, A.; Islam, A.; Borgdorff, M.; van Leth, F. Care seeking in tuberculosis: Results from a countrywide cluster randomised survey in Bangladesh. BMJ Open 2014, 4, e004766. [Google Scholar] [CrossRef]
- Chowdhury, A.S.; Ahmed, M.S.; Ahmed, S.; Khanam, F.; Farjana, F.; Reza, S.; Islam, S.; Islam, A.; Khan, J.A.M.; Rahman, M. Estimating Catastrophic Costs due to Pulmonary Tuberculosis in Bangladesh. J. Epidemiol. Glob. Health 2021, 11, 83–91. [Google Scholar] [CrossRef]
- Pavel, M.S.; Chakrabarty, S.; Gow, J. Cost of illness for outpatients attending public and private hospitals in Bangladesh. Int. J. Equity Health 2016, 15, 167. [Google Scholar] [CrossRef] [PubMed]
- (BBS) BBoS. Labour Force Survey 2022; Bangladesh Bureau of Statistics (BBS): Dhaka, Bangladesh, 2023.
- Naher, N.; Hassan, M.S.; Hoque, R.; Alamgir, N.; Ahmed, S.M. Irregularities, Informal Practices, and the Motivation of Frontline Healthcare Providers in Bangladesh: Current Scenario and Future Perspectives Towards Achieving Universal Health Coverage by 2030; ACE SOAS Consortium Working Paper; University of London: London, UK, 2018. [Google Scholar]
- Khanam, S.; Farjana, S.; Zaman, F.; Islam, M.Z. Accessibility to Health Care Services of Upazila Health Complex: Experience of Rural People. J. Prev. Social. Med. 2020, 38, 30–37. [Google Scholar]
- Islam, S.; Hirayama, T.; Islam, A.; Ishikawa, N.; Afsana, K. Treatment referral system for tuberculosis patients in Dhaka, Bangladesh. Public Health Action 2015, 5, 236–240. [Google Scholar] [CrossRef][Green Version]
- Lee, J.Y.; Kwon, N.; Goo, G.Y.; Cho, S.I. Inadequate housing and pulmonary tuberculosis: A systematic review. BMC Public Health 2022, 22, 622. [Google Scholar] [CrossRef] [PubMed]
- Karim, M.R.; Rahman, M.A.; Mamun, S.A.; Alam, M.A.; Akhter, S. Risk factors of childhood tuberculosis: A case control study from rural Bangladesh. WHO South-East Asia J. Public Health 2012, 1, 76–84. [Google Scholar] [CrossRef]
- Rahman, T.; Bhuiyan, M.; Saba, S.; Irfan, S.D.; Akter, A.; Hossain, A. Effects of Poor Protein Intake and In-House Overcrowding On Childhood Tuberculosis in a Low-Income Bangladeshi Rural Community: A Case-Control Study. J. Infect. Dis. 2018, 2. [Google Scholar]
- Islam, M.; Sultana, Z.Z.; Iqbal, A.; Ali, M.; Hossain, A. Effect of in-house crowding on childhood hospital admissions for acute respiratory infection: A matched case-control study in Bangladesh. Int. J. Infect. Dis. 2021, 105, 639–645. [Google Scholar] [CrossRef]
- Noykhovich, E.; Mookherji, S.; Roess, A. The Risk of Tuberculosis among Populations Living in Slum Settings: A Systematic Review and Meta-analysis. J. Urban Health 2019, 96, 262–275. [Google Scholar] [CrossRef]
- Rashid, S.F. Strategies to reduce exclusion among populations living in urban slum settlements in Bangladesh. J. Health Popul. Nutr. 2009, 27, 574–586. [Google Scholar] [CrossRef]
- Alam, M.Z.; Mamun, A.A. Dynamics of internal migration in Bangladesh: Trends, patterns, determinants, and causes. PLoS ONE 2022, 17, e0263878. [Google Scholar] [CrossRef]
- Khare, H.S. Barriers Constraining the Low and Middle Income Housing Finance Market in Bangladesh; World Bank: Washington, DC, USA, 2016. [Google Scholar]
- Shams, S.; Mahruf, M.; Shohel, C.; Ahsan, A. Housing Problems for Middle and Low Income People in Bangladesh: Challenges of Dhaka Megacity. Environ. Urban. Asia 2014, 5, 175–184. [Google Scholar] [CrossRef]
- Rahman, M.S.; Sarkar, S. An Analysis of the Construction of Kutcha Houses (Dwellings and Non-Dwellings) in Bangladesh. In Proceedings of the International Conference on Engineering Research, Shajalal University of Science & Technology, Sylhet, Bangladesh, 1–2 December 2022. [Google Scholar]
- Obore, N.; Kawuki, J.; Guan, J.; Papabathini, S.S.; Wang, L. Association between indoor air pollution, tobacco smoke and tuberculosis: An updated systematic review and meta-analysis. Public Health 2020, 187, 24–35. [Google Scholar] [CrossRef]
- Neelakanta, R.R.; Jagadeesan, A.R.; Goudhaman, L.; Athisayaraj, M.S. Factors Influencing Particulate Matter 2.5 Levels in Indoor Areas of Rural Houses: A Cross-sectional Study. J. Clin. Diagn. Res. 2022, 16. [Google Scholar] [CrossRef]
- Gurley, E.S.; Salje, H.; Homaira, N.; Ram, P.K.; Haque, R.; Petri, W.A., Jr.; Bresee, J.; Moss, W.J.; Luby, S.P.; Breysse, P.; et al. Seasonal concentrations and determinants of indoor particulate matter in a low-income community in Dhaka, Bangladesh. Environ. Res. 2013, 121, 11–16. [Google Scholar] [CrossRef]
- Hodgson, R.; Carter, M. Some Factors Governing Choices of Building Materials in Rural Bangladesh; Bangladesh University of Engineering and Technology: Dhaka, Bangladesh, 1999. [Google Scholar]
- (BBS) BBoS. Survey on Occupied Residential Houses and Real Estate Services; (BBS) BBoS, Ed.; Bangladesh Bureau of Statistics (BBS): Dhaka, Bangladesh, 2019.
- (BBS) BBoS. Population & Housing Census 2022; Bangladesh Bureau of Statistics (BBS): Dhaka, Bangladesh, 2022.
- (WOAH) WOfAH. Terrestrial Manual; World Organisation for Animal Health (WOAH): Paris, France, 2023. [Google Scholar]
- Islam, S.S.; Rumi, T.B.; Kabir, S.M.L.; Rahman, A.; Faisal, M.M.H.; Islam, R.; van der Zanden, A.G.M.; Ward, M.P.; Ross, A.G.; Rahim, Z. Zoonotic tuberculosis knowledge and practices among cattle handlers in selected districts of Bangladesh. PLoS Negl. Trop. Dis. 2021, 15, e0009394. [Google Scholar] [CrossRef] [PubMed]
- Islam, S.K.S.; Rumi, T.B.; Kabir, S.M.L.; van der Zanden, A.G.M.; Kapur, V.; Rahman, A.; Ward, M.P.; Bakker, D.; Ross, A.G.; Rahim, Z. Bovine tuberculosis prevalence and risk factors in selected districts of Bangladesh. PLoS ONE 2020, 15, e0241717. [Google Scholar] [CrossRef]
- Hossain, S.; Husain, A.; Imam, M.; Ali Ghosh, T.K.; Mahmood, N.; Kabir, H.; Sultana, N.; Kabir, I.; Munsi, R. Communities, Rights and Gender TB Tools Assessment in Bangladesh; BRAC/StopTB Partnership/UNOPS: Dhaka, Bangladesh, 2018. [Google Scholar]
- Saan, N. Assessment, Monitoring, and Awareness of Garment Workers Regarding the Prevalence of Tuberculosis in Savar, Dhaka. Eur. J. Med. Health Sci. 2019, 1, 30–40. [Google Scholar]
- Khandker, S.; Ahmad, S.A.; Khan, M.K.; Faruquee, M.H. Perceived Workplace Hazards and Health Problems Among the Workers of Garment Factory in Dhaka. J. Prev. Soc. Med. 2016, 35, 1–9. [Google Scholar]
- Islam, M.S.; Banu, S.; Tarannum, S.; Chowdhury, K.I.A.; Nazneen, A.; Islam, M.T.; Shafique, S.M.Z.; Islam, S.M.H.; Chughtai, A.A.; Seale, H. Examining pulmonary TB patient management and healthcare workers exposures in two public tertiary care hospitals, Bangladesh. PLoS Glob. Public Health 2022, 2, e0000064. [Google Scholar] [CrossRef]
- Nazneen, A.; Tarannum, S.; Chowdhury, K.I.A.; Islam, M.T.; Islam, S.M.H.; Ahmed, S.; Banu, S.; Islam, M.S. Implementation status of national tuberculosis infection control guidelines in Bangladeshi hospitals. PLoS ONE 2021, 16, e0246923. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, A.; Hossain, L.; Banik, G.; Sayeed, A.; Sajib, M.R.U.; Hasan, M.M.; Hoque, D.E.; Hasan, A.S.M.; Raghuyamshi, V.; Zaman, S.; et al. Measuring the effectiveness of an integrated intervention package to improve the level of infection prevention and control: A multi-centre study in Bangladesh. J. Hosp. Infect. 2024, 145, 22–33. [Google Scholar] [CrossRef] [PubMed]
- Hossain, S.; Hossen, A. Poverty Maps of Bangladesh; Bangladesh Bureau of Statistics (BBS): Dhaka, Bangladesh, 2016.
- Karim, F.; Islam, Q.S.; Islam, M.A.; Ahmed, J. Occupational Pulmonary Tuberculosis Among BRAC Community Health Workers of Trishal; BRAC University: Dhaka, Bangladesh, 2011. [Google Scholar]
- Ahmed, S. Taking Healthcare Where the Community is: The Story of the Shasthya Sebikas of BRAC in Bangladesh. BRAC Univ. J. 2008, 5, 39–45. [Google Scholar]
- Gbratto-Dobe, S.A.W.; Segnon, H.B. Is mother’s education essential to improving the nutritional status of children under five in Côte d′Ivoire? SSM-Health Syst. 2025, 4, 100056. [Google Scholar] [CrossRef]
- Attah, C.J.; Oguche, S.; Egah, D.; Ishaya, T.N.; Banwat, M.; Adgidzi, A.G. Risk factors associated with paediatric tuberculosis in an endemic setting. Alex. J. Med. 2019, 54, 403–409. [Google Scholar] [CrossRef]
- Vayr, F.; Martin-Blondel, G.; Savall, F.; Soulat, J.M.; Deffontaines, G.; Herin, F. Occupational exposure to human Mycobacterium bovis infection: A systematic review. PLoS Negl. Trop. Dis. 2018, 12, e0006208. [Google Scholar] [CrossRef]
- Paleckyte, A.; Dissanayake, O.; Mpagama, S.; Lipman, M.C.; McHugh, T.D. Reducing the risk of tuberculosis transmission for HCWs in high incidence settings. Antimicrob. Resist. Infect. Control 2021, 10, 106. [Google Scholar] [CrossRef]
- Chakrabartty, A.; Basu, P.; Ali, K.M.; Ghosh, D. Tuberculosis related stigma attached to the adherence of Directly Observed Treatment Short Course (DOTS) in West Bengal, India. Indian J. Tuberc. 2019, 66, 259–265. [Google Scholar] [CrossRef]
- Sudhinaraset, M.; Ingram, M.; Lofthouse, H.K.; Montagu, D. What is the role of informal healthcare providers in developing countries? A systematic review. PLoS ONE 2013, 8, e54978. [Google Scholar] [CrossRef]
- (GTB) GPoTaLH. Engaging Private Health Care Providers in TB Care and Prevention: A Landscape Analysis, 2nd ed.; World Health Organization: Geneva, Switzerland, 2021; Available online: https://www.who.int/publications/i/item/9789240027039 (accessed on 3 March 2024).
- Nguyen, H.B.; Vo, L.N.Q.; Forse, R.J.; Wiemers, A.M.C.; Huynh, H.B.; Dong, T.T.T.; Phan, Y.T.H.; Creswell, J.; Dang, T.M.H.; Nguyen, L.H.; et al. Is convenience really king? Comparative evaluation of catastrophic costs due to tuberculosis in the public and private healthcare sectors of Viet Nam: A longitudinal patient cost study. Infect. Dis. Poverty 2024, 13, 27. [Google Scholar] [CrossRef] [PubMed]
- Omran, A.R. The Epidemiologic Transition: A Theory of the Epidemiology of Population Change. Milbank Meml. Fund Q. 1971, 49, 509–538. [Google Scholar] [CrossRef]
- Biswas, R.K.; Kabir, E.; Khan, H.T.A. Causes of Urban Migration in Bangladesh: Evidence from the Urban Health Survey. Popul. Res. Policy Rev. 2019, 38, 593–614. [Google Scholar] [CrossRef]
- Akter, S.; Akram, A.B. Trend of National Housing Policy: Bangladesh Perspective (Can meet the challenge of housing for all?). Int. J. Res. Innov. Soc. Sci. (IJRISS) 2020, 4, 285. [Google Scholar]
- Authority, N.H. National Housing Policy. National Housing Authority: Dhaka, Bangladesh, 2016. [Google Scholar]
- International Trade Union Confederation (ITUC). Bangladesh Labour Legal Profile. International Trade Union Confederation; International Trade Union Confederation (ITUC): Singapore, 2023. [Google Scholar]
- Islam, M.M. Effective tobacco control measures in Bangladesh require a whole-of-government approach. Policy Des. Pract. 2023, 7, 105–113. [Google Scholar] [CrossRef]
- Westerbotn, M.; Monfors, F.; Reusser, J.; Tyrrell, M. Promoting health and preventing malnutrition among children in rural Bangladesh: A qualitative study. Nurs. Open 2023, 10, 5693–5700. [Google Scholar] [CrossRef]
- Sarker, M.M.; Niaz Uddin, A.G.M.; Alam, M.B. Overcoming Poor Governance: A Study on Public Health System in Bangladesh. Soc. Change 2010, 4. [Google Scholar]
- Dutta, G.K.; Rahman, M.M.; Bhattacharyya, D.S.; Rahman, M.M.; Dey, P.K.; Nur, M.E.; Alom, K.R. There is no cure for Tuberculosis: An Anthropological investigation on social perception, prejudice, and stigma in Bangladesh. Res. Sq. 2022, preprint. [Google Scholar] [CrossRef]
- Xu, S.; Shonchoy, A.S.; Fujii, T. Illusion of Gender Parity in Education: Intrahousehold Resource Allocation in Bangladesh; Asian Development Bank Institute: Tokyo, Japan, 2019. [Google Scholar]
- (BBS) BBoS. Education Scenario in Bangladesh: Gender Perspective; Bangladesh Bureau of Statistics (BBS): Dhaka, Bangladesh, 2017.
- Rifat, M.; Rusen, I.D.; Mahmud, M.H.; Nayer, I.; Islam, A.; Ahmed, F. From mosques to classrooms: Mobilizing the community to enhance case detection of tuberculosis. Am. J. Public Health 2008, 98, 1550–1552. [Google Scholar] [CrossRef] [PubMed]
- Shete, P.B.; Nalugwa, T.; Farr, K.; Ojok, C.; Nantale, M.; Howlett, P.; Haguma, P.; Ochom, E.; Mugabe, F.; Joloba, M.; et al. Feasibility of a streamlined tuberculosis diagnosis and treatment initiation strategy. Int. J. Tuberc. Lung Dis. 2017, 21, 746–752. [Google Scholar] [CrossRef] [PubMed]
- Kaso, A.; Hailu, A. Costs and cost-effectiveness of Gene Xpert compared to smear microscopy for the diagnosis of pulmonary tuberculosis using real-world data from Arsi zone, Ethiopia. PLoS ONE 2021, 16, e0259056. [Google Scholar] [CrossRef]
- Hasan, M.Z.; Ahmed, S.; Islam, Z.; Dorin, F.; Rabbani, M.G.; Mehdi, G.G.; Ahmed, M.W.; Tahsina, T.; Mahmood, S.S.; Islam, Z. Costs of services and funding gap of the Bangladesh National Tuberculosis Control Programme 2016–2022: An ingredient based approach. PLoS ONE 2023, 18, e0286560. [Google Scholar] [CrossRef]
- van Bree, E.M.; Snijder, L.E.; Ossebaard, H.C.; Brakema, E.A. Environmental Impact of Physical Visits and Telemedicine in Nursing Care at Home: Comparative Life Cycle Assessment. J. Med. Internet Res. 2025, 27, e67538. [Google Scholar] [CrossRef]
- MacNeill, A.J.; McGain, F.; Sherman, J.D. Planetary health care: A framework for sustainable health systems. Lancet Planet. Health 2021, 5, e66–e68. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, T.; Takahashi, K.; Otsuka, K. Gains from female education in rural Bangladesh: A multidimensional approach. Int. J. Educ. Dev. 2021, 81, 102344. [Google Scholar] [CrossRef]
- Khandker, S.; Hussain, A.; Samad, N.; Fuwa, R. The Female Secondary Stipend and Assistance Program in Bangladesh: What Did It Accomplish? Asian Development Bank: Manila, Philippines, 2021. [Google Scholar]
- Sarkar, R.K. Socio cultural barriers of girls’ educational attainment: Experiences from rural Bangladesh. Zenodo (CERN Eur. Organ. Nucl. Res.) 2022, 10, 348–358. [Google Scholar]
- Sinanovic, E.; Kumaranayake, L. Financing and cost-effectiveness analysis of public-private partnerships: Provision of tuberculosis treatment in South Africa. Cost. Eff. Resour. Alloc. 2006, 4, 11. [Google Scholar] [CrossRef][Green Version]
- Rashid, A.; Sheokand, S.; Fatima, R.; Habib, H.; Tahir, A.; Saleem, A.; Thapa, P.; Heitkamp, P. Maximizing tuberculosis services through private provider engagement—A case study from Pakistan. J. Clin. Tuberc. Other Mycobact. Dis. 2025, 39, 100506. [Google Scholar] [CrossRef]
- Bello, G.; Faragher, B.; Sanudi, L.; Namakhoma, I.; Banda, H.; Malmborg, R.; Thomson, R.; Squire, S.B. The effect of engaging unpaid informal providers on case detection and treatment initiation rates for TB and HIV in rural Malawi (Triage Plus): A cluster randomised health system intervention trial. PLoS ONE 2017, 12, e0183312. [Google Scholar] [CrossRef] [PubMed]
- Barua, M.; Thapa, P.; Narasimhan, P.; Jayasuriya, R.; Hall, J.J.; Mukherjee, P.S.; Das, D.K.; Beek, K. Barriers and facilitators to informal healthcare provider engagement in the national tuberculosis elimination program of India: An exploratory study from West Bengal. PLoS Glob. Public Health 2023, 3, e0001390. [Google Scholar]
- Sukhera, J. Narrative Reviews in Medical Education: Key Steps for Researchers. J. Grad. Med. Educ. 2022, 14, 418–419. [Google Scholar] [CrossRef] [PubMed]


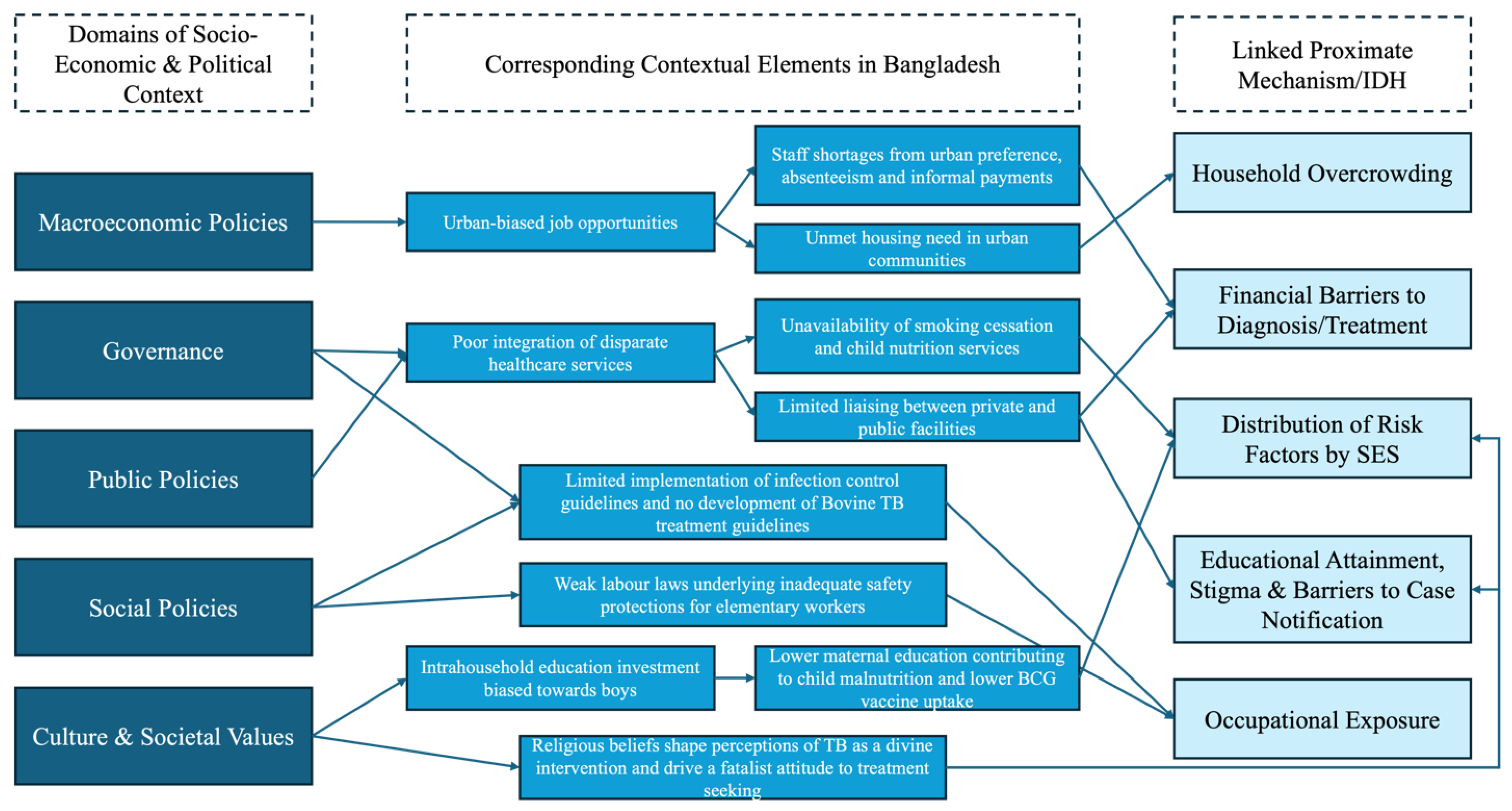
| Conceptual Framework Derived From | SEDH | Keywords |
|---|---|---|
| SDH Framework [7] | Wealth | Wealth OR salary OR pay OR wages OR earnings OR income |
| SDH Framework | Educational Attainment | Education OR schooling OR literacy OR graduate |
| Planetary Health EDHs [6]; SDH Framework | Housing, Land Use | Homelessness OR home ownership OR slum OR Kutcha OR Pucca OR poor-quality housing OR mud hut OR overcrowding OR urbanisation |
| SDH Framework | Occupation | Employment OR workplace hazard OR occupational hazard OR overcrowding |
| Planetary Health EDHs | Air quality | Pollution OR smoking OR dampness OR ventilation |
| IDH | Description |
|---|---|
| Section 3.1 Distribution of TB Risk Factors by SES | Low-SES populations have higher prevalence of smoking, child malnutrition, biomass fuel use while high-SES populations exhibit a higher Diabetes prevalence. |
| Section 3.2 Educational Attainment, Stigma, and Barriers to Case Notification | Low educational attainment contributes to stigma and poor disease knowledge, leading to delayed diagnosis and concealment. |
| Section 3.3 Financial Barriers to Treatment | Direct and indirect costs create obstacles from diagnosis to completion of treatment, creating a perpetual cycle of management delay. |
| Section 3.4 Housing Characteristics | Overcrowded, poorly ventilated, low-quality housing increases transmission risk compounded by risk factors in Section 3.1. |
| Section 3.5 Occupational Exposure | Predominantly low-income agricultural, elementary, and healthcare workers have increased TB risk. |
| Recommendation | Description | Stakeholders | Alignment with Quadruple Aims, SDGs, End TB Pillars | Monitoring Strategy |
|---|---|---|---|---|
| Streamline Diagnostic and Treatment Availability | Implement SIMPLE TB strategy to improve case detection and treatment initiation | Ministry of Health and Family Welfare; international aid organisations; NGOs | Quadruple Aims 3; End TB Strategy Pillar 1 | Case notification and diagnostic referrals |
| Reduce Household and Workplace Overcrowding | Increase public funding for homebuilding and promote campaigns to strengthen workers’ rights. | National Housing Authority; international development banks | Quadruple Aims 1; SDG 11.1; End TB Strategy Pillar 2 | Proportion of houses designated as kutchas or slums in the annual housing survey |
| Promote Gender Equality in Educational Attainment | Expand upon existing stipends and school-level interventions to improve gender equality in schools | Ministry of Education; Donor agencies (e.g., BRAC) | Quadruple Aims 1 and 2; SDGs 4 and 5; End TB Strategy Pillar 1 | Gender parity in secondary education completion and tertiary education enrolment |
| Facilitate Integration with Private Providers and IPs | Integrate private facilities as well as IPs into DOTS to improve case notification and treatment referral | NTP; Professional medical associations | Quadruple Aims 1; SDG 3; End TB Strategy Pillar 1 and Pillar 2 | TB diagnoses confirmed within an acceptable, 45.6 day, timeframe. |
| Domain | Discipline | Methodology | Research Need |
|---|---|---|---|
| Initial presentation to TB services | Behavioural Science, Public Health | Interviews and Longitudinal Patient Journey Mapping | Drivers of initial presentation to private hospitals for TB treatment, which are potentially disruptive to DOTS. |
| Relative influence of TB risk factors | Public Health | Case-based studies | Strength of risk factors present among low-SES TB patients versus those among high-SES. |
| Kutcha house construction method | Engineering Construction | Surveys on construction methods and associated drivers | Drivers of choice of materials used in kutcha house construction, which account for a majority of residential units and facilitate TB transmission |
| Incorporate planetary health into existing WHO SDH Framework | N/A | N/A | Incorporate ecological risk factors for disease into the existing WHO Framework to inform more holistic, sustainable epidemiological research and interventions |
| Efficacy of coordinated community action at improving TB awareness and case notification locally | Public health Behavioural Science | Pilot interventions | Determine whether engaging local community leaders is effective at tackling current misconceptions about TB that may impede case notification |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rahman, I.; Willott, C. Social, Economic and Ecological Drivers of Tuberculosis Disparities in Bangladesh: Implications for Health Equity and Sustainable Development Policy. Challenges 2025, 16, 37. https://doi.org/10.3390/challe16030037
Rahman I, Willott C. Social, Economic and Ecological Drivers of Tuberculosis Disparities in Bangladesh: Implications for Health Equity and Sustainable Development Policy. Challenges. 2025; 16(3):37. https://doi.org/10.3390/challe16030037
Chicago/Turabian StyleRahman, Ishaan, and Chris Willott. 2025. "Social, Economic and Ecological Drivers of Tuberculosis Disparities in Bangladesh: Implications for Health Equity and Sustainable Development Policy" Challenges 16, no. 3: 37. https://doi.org/10.3390/challe16030037
APA StyleRahman, I., & Willott, C. (2025). Social, Economic and Ecological Drivers of Tuberculosis Disparities in Bangladesh: Implications for Health Equity and Sustainable Development Policy. Challenges, 16(3), 37. https://doi.org/10.3390/challe16030037