Healthcare Service Quality from the Point of Healthcare Providers’ Perception at the Time of COVID-19
Abstract
:1. Introduction
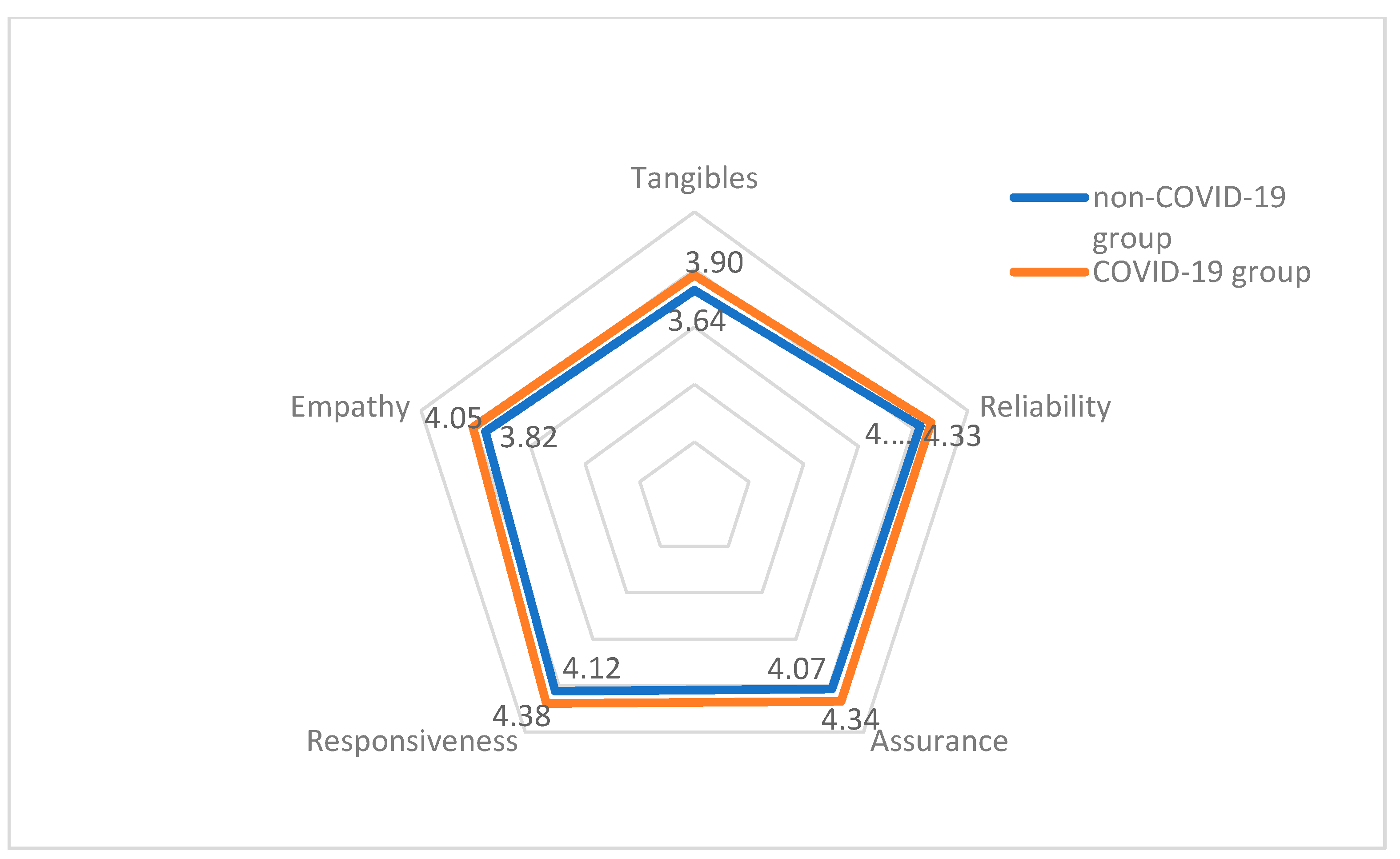
- Tangibles
- Reliability
- Responsiveness
- Assurance
- Empathy
2. Materials and Methods
Data Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Title 1 | Title 2 | Title 3 |
|---|---|---|
| D1.1 | Gender (circle) | Male Female |
| D1.2 | Age (circle) | Under 30 years of age From 31 to 40 years of age From 41 to 50 years of age From 51 to 60 years of age Over 60 years of age |
| D1.3 | Level of education (circle) | Elementary school High school lasting 3 years High school lasting 4 years College (vocational studies) University (Bachelor’s degree) University (Master’s degree) University (PhD) |
| D1.4 | City of residence (write) | |
| D1.5 | Job (circle) | Nurse MD general practitioner MD specialist |
| D1.6 | Monthly salary—net (circle) | Under 20,000 RSD From 20,000 to 30,000 RSD From 30,000 to 40,000 RSD From 40,000 to 50,000 RSD From 50,000 to 60,000 RSD From 60,000 to 70,000 RSD From 70,000 to 80,000 RSD From 80,000 to 100,000 RSD Over 100,000 RSD |
| D1.7 | Marital status (circle) | Not married Married Divorced Widow/widower |
| D1.8 | Institution/hospital of workplace (write) | |
| D1.9 | Ward (write) |
| No | Description | Absolutely Disagree | Partially Agree | Absolutely Agree | ||
|---|---|---|---|---|---|---|
| D2.1 | 1. In the health institution I work in, the staff take care of the hygiene in the areas where patients are treated. | 1 | 2 | 3 | 4 | 5 |
| D2.2 | 2. The surroundings in the health institution I work in are comfortable enough for the patients to rest. | 1 | 2 | 3 | 4 | 5 |
| D2.3 | 3. The health institution I work in has good and modern equipment for treating patients. | 1 | 2 | 3 | 4 | 5 |
| D2.5 | 4. The health staff in the health institution I work in are tidy and professional. | 1 | 2 | 3 | 4 | 5 |
| D2.6 | 5. In the health institution I work in, patients receive adequate material and information about the health care they receive (i.e., brochures). | 1 | 2 | 3 | 4 | 5 |
| D2.7 | 6. The medical staff in the health institution I work in give the patients precise service with the knowledge of all needed skills. | 1 | 2 | 3 | 4 | 5 |
| D2.8 | 7. Patients receive all necessary information about treatment and are asked for certain permissions when they are needed. | 1 | 2 | 3 | 4 | 5 |
| D2.10 | 8. The medical staff in the health institution I work in are dependable. | 1 | 2 | 3 | 4 | 5 |
| D2.11 | 9. The health service is given to the patients within the time told to them. | 1 | 2 | 3 | 4 | 5 |
| D2.12 | 10. The health institution I work in provides excellent effects in treating its patients. | 1 | 2 | 3 | 4 | 5 |
| D2.14 | 11. When the patient needs help, the medical staff in the health institution I work in always willingly help. | 1 | 2 | 3 | 4 | 5 |
| D2.16 | 12. The patients receive the services in time, as well as necessary medications. | 1 | 2 | 3 | 4 | 5 |
| D2.17 | 13. The health institution I work in has a simple system for making an appointment. | 1 | 2 | 3 | 4 | 5 |
| D2.18 | 14. The medical staff in the health institution I work in willingly answer to the questions of the patients. | 1 | 2 | 3 | 4 | 5 |
| D2.19 | 15. The medical staff in the health institution I work in have the knowledge to give needed services. | 1 | 2 | 3 | 4 | 5 |
| D2.20 | 16. Patients are given all necessary information about the hospitalization (when it is needed) in the health institution I work in. | 1 | 2 | 3 | 4 | 5 |
| D2.22 | 17. The medical staff in the health institution I work in give the patients services with a sense of duty. | 1 | 2 | 3 | 4 | 5 |
| D2.23 | 18. Patients feel safe when interacting with the medical staff in the health institution I work in. | 1 | 2 | 3 | 4 | 5 |
| D2.24 | 19. The buildings of the health institution I work in are safe. | 1 | 2 | 3 | 4 | 5 |
| D2.26 | 20. The medical staff in the health institution I work in respect the individual personalities of the patients. | 1 | 2 | 3 | 4 | 5 |
| D2.27 | 21. The patients’ complaints are heard and listened to in the health institution I work in. | 1 | 2 | 3 | 4 | 5 |
| D2.29 | 22. The privacy of the patients is respected in the health institution I work in. | 1 | 2 | 3 | 4 | 5 |
| D2.30 | 23. Care is taken with the families of the patients and those coming to visit them in the health institution I work in (in case the patient is held in for therapy). | 1 | 2 | 3 | 4 | 5 |
| D2.31 | 24. In the health institution I work in, the biggest system of motivation to give the patients better services is the salary. | 1 | 2 | 3 | 4 | 5 |
| D2.32 | 25. In the health institution I work in, the biggest system of motivation to give the patients better services is the modern equipment. | 1 | 2 | 3 | 4 | 5 |
| D2.33 | 26. In the health institution I work in, the biggest system of motivation to give the patients better services is the possibility of further education of the staff through seminars and symposiums. | 1 | 2 | 3 | 4 | 5 |
References
- Alami, H.; Lehoux, P.; Fleet, R.; Fortin, J.P.; Liu, J.; Attieh, R.; Ag Ahmed, M.A. How can health systems better prepare for the next pandemic? Lessons learned from the management of COVID-19 in Quebec (Canada). Front. Public Health 2021, 9, 696. [Google Scholar] [CrossRef] [PubMed]
- Leoni, G.; Lai, A.; Stacchezzini, R.; Steccolini, I.; Brammer, S.; Linnenluecke, M.; Demirag, I. Accounting, management and accountability in times of crisis: Lessons from the COVID-19 pandemic. Account. Audit. Account. J. 2021, 34, 1305–1319. [Google Scholar] [CrossRef]
- Ćulafić, S.; Janovac, T.; Jovanović, S.V.; Tadić, J.; Jaganjac, J.; Milošević, A.; Bibić, A. State Incentives and Sustainable Motivation System in the Health Sector. Sustainability 2021, 13, 13592. [Google Scholar] [CrossRef]
- Global Health Security Index 2021. Available online: https://www.ghsindex.org/country/serbia/ (accessed on 22 March 2022).
- Sagan, A.; Webb, E.; McKee, M.; Greer, S.L.; Karanikolos, M.; Williams, G.A.; Cylus, J.; Richardson, E.; Waitzberg, R.; Lessof, S.; et al. Health Systems Resilience during COVID-19: Lessons for Building Back Better. © World Health Organization 2021, ISBN 978 92 890 5187 3. Available online: https://apps.who.int/iris/rest/bitstreams/1390564/retrieve (accessed on 15 March 2022).
- Razu, S.R.; Yasmin, T.; Arif, T.B.; Islam, S.; Islam, S.M.S.; Gesesew, H.A.; Ward, P. Challenges Faced by Healthcare Professionals During the COVID-19 Pandemic: A Qualitative Inquiry From Bangladesh. Front. Public Health 2021, 9, 2296–2565. Available online: https://www.frontiersin.org/article/10.3389/fpubh.2021.647315 (accessed on 1 April 2022). [CrossRef] [PubMed]
- Kazemi, N.; Ehsani, P.; Abdi, F.; Bighami, M. Measuring hospital service quality and its influence on patient satisfaction: An empirical study using structural equation modeling. Manag. Sci. Lett. 2013, 3, 2125–2136. [Google Scholar] [CrossRef]
- Pouragha, B.; Zarei, E. The effect of outpatient service quality on patient satisfaction in teaching hospitals in Iran. Mater. Socio-Med. 2016, 28, 21. [Google Scholar] [CrossRef] [Green Version]
- Marzban, S.; Najafi, M.; Etedal, M.G.; Moradi, S.; Rajaee, R. The evaluation of outpatient quality services in physiotherapy in the teaching health centers of ShahidBeheshti University based on SERVQUAL tools. Eur. J. Biol. Med. Sci. Res. 2015, 3, 46–53. [Google Scholar]
- Zarei, A.; Arab, M.; Froushani, A.R.; Rashidian, A.; Tabatabaei, S.M.G. Service quality of private hospitals: The Iranian Patients’ perspective. BMC Health Serv. Res. 2012, 12, 31. [Google Scholar] [CrossRef] [Green Version]
- Irfan, S.M.; Ijaz, A.; Farooq, M.M. Patient satisfaction and service quality of public hospitals in Pakistan: An empirical assessment. Middle-East J. Sci. Res. 2012, 12, 870–877. [Google Scholar]
- Rakhmawati, T.; Sumaedi, S.; Bakti, I.G.M.Y.; Astrini, N.J.; Widianti, M.Y.T.; Sekar, D.C.; Vebriyanti, D.I. Developing a service quality measurement model of public health center in Indonesia. Manag. Sci. Eng. 2013, 7, 1–5. [Google Scholar]
- Fatima, I.; Humayun, A.; Iqbal, U.; Shafiq, M. Dimensions of service quality in healthcare: A systematic review of literature. Int. J. Qual. Health Care 2019, 31, 11–29. [Google Scholar] [CrossRef]
- Parasuraman, A.; Zeithaml, V.A.; Berry, L.L. SERVQUAL: A multi-item scale formeasuring consumer perceptions of service quality. J. Retail. 1988, 64, 21–40. [Google Scholar]
- Cronin, J.J.; Taylor, S. SERPERF versus SERQUAL: Reconciling Performance-Based and Perception-Minus-Expectations Measurement of Service Quality. J. Mark. 1994, 58, 125–131. [Google Scholar] [CrossRef]
- World Health Organization. Regional Office for the Western Pacific. 2016. Available online: https://apps.who.int/iris/handle/10665/208286 (accessed on 3 April 2022).
- Waitzberg, R.; Gerkens, S.; Dimova, A.; Bryndová, L.; Vrangbæk, K.; Jervelund, S.S.; Birk, H.O.; Rajan, S.; Habicht, T.; Tynkkynen, L.-K.; et al. Balancing financial incentives during COVID-19:Acomparison of provider payment adjustment across 20 countries. Health Polica 2021, 14, 33. [Google Scholar] [CrossRef]
- Tripathi, S.N.; Siddiqui, M.H. Assesing the quality of healthcare services: Assessing the quality of healthcare services:A SERVQUAL approach. Int. J. Healthc. Manag. 2018, 13, 133–144. [Google Scholar] [CrossRef]
- Cronin, J.J.; Taylor, S.A. Measuring service quality: A reexamination and extension. J. Mark. 1992, 56, 55–68. [Google Scholar] [CrossRef]
- Canman, J.M. Consumer perception of service quality: An assessment of the SERVQUAL dimensions. J. Retail. 1990, 66, 33–55. [Google Scholar]
- Narayanan, A.; Greco, M.; Powell, H.; Bealing, T. Measuring the quality of hospital doctors through colleague and patient feedback. J. Manag. Mark. Healthc. 2011, 14, 180–195. [Google Scholar] [CrossRef]
- Westbrook, K.W.; Grant, C.C.; Rafalski, E.; Babakus, E. Patient-family centred care. J. Health Manag. 2015, 17, 304–315. [Google Scholar] [CrossRef]
- Rumintjap, A.F.; Wandebori, H. Developing healthcare service quality model using SERPERF scale: An application to the inpatient department at a private hospital in Bogor. J. Bus. Manag. 2017, 6, 56–65. [Google Scholar]
- Paul, P.D. What is the best approach for measuring service quality of periodontists? Clin. Res. Regul. Aff. 2003, 20, 457–468. [Google Scholar] [CrossRef]
- Endeshaw, B. Healthcare service quality-measurement models: A review. J. Health Res. 2021, 35, 106–117. [Google Scholar] [CrossRef]
- Ovretveit, J. Total quality management in European Healthcare. Int. J. Health Care Qual. Assur. 2000, 13, 74–79. [Google Scholar] [CrossRef]
- Kilbourne, W.E.; Duffy, J.A.; Duffy, M.; Giarchi, G. The applicability of SERVQUAL in cross-national measurement of health-care quality. J. Serv. Mark. 2004, 18, 524–533. [Google Scholar] [CrossRef]
- Brouwers, J.; Cox, B.; Van Wilder, A.; Claessens, F.; Bruyneel, L.; De Ridder, D.; Eeckloo, K.; Vanhaecht, K. The future of hospital quality of care policy: A multi-stakeholder discrete choice experiment in Flanders, Belgium. Health Policy 2021, 125, 1565–1573. [Google Scholar] [CrossRef]
- Li, H.; Yuan, B.; Wang, D.; Meng, Q. Motivating factors on performance of primary care workers in China: A systematic review and meta-analysis. BMJ Open 2019, 9, e8619. [Google Scholar] [CrossRef] [Green Version]
- Van Eerde, W. Motivation and Reward Systems; Wiley Encyclopedia of Management: Hoboken, NJ, USA, 2015; pp. 1–4. [Google Scholar]
- Anku, J.S.; Amewugah, B.K.; Glover, M.K. Concept of reward management, reward system and corporate efficiency. Int. J. Econ. Commer. Manag. 2018, 6, 621–637. [Google Scholar]
- Pakurár, M.; Haddad, H.; Nagy, J.; Popp, J.; Oláh, J. The Service Quality Dimensions that Affect Customer Satisfaction in the Jordanian Banking Sector. Sustainability 2019, 11, 1113. [Google Scholar] [CrossRef] [Green Version]
- Ramsaran-Fowdar, R.R. The relative importance of service dimensions in a healthcare setting. Int. J. Health Care Qual. Assur. 2008, 21, 104–124. [Google Scholar] [CrossRef]

| Non-COVID-19 Group | COVID-19 Group | ||
|---|---|---|---|
| Age (year) | min | 22 | 20 |
| max | 63 | 65 | |
| mean | 43.6 | 44.1 | |
| SD | 11.6 | 11.1 | |
| p | 0.468 a | ||
| amount of income (€) | min | 230 | 190 |
| max | 1410 | 1650 | |
| mean | 568.20 | 866.22 | |
| SD | 265.0 | 371.9 | |
| p | >0.001 a | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ivanov, O.; Gojković, Z.; Simeunović, N.; Gračanin, D.; Milovančev, A.; Ivanov, D.; Bojović, M.; Bugarčić, M.; Stojić, N. Healthcare Service Quality from the Point of Healthcare Providers’ Perception at the Time of COVID-19. Challenges 2022, 13, 26. https://doi.org/10.3390/challe13010026
Ivanov O, Gojković Z, Simeunović N, Gračanin D, Milovančev A, Ivanov D, Bojović M, Bugarčić M, Stojić N. Healthcare Service Quality from the Point of Healthcare Providers’ Perception at the Time of COVID-19. Challenges. 2022; 13(1):26. https://doi.org/10.3390/challe13010026
Chicago/Turabian StyleIvanov, Olivera, Zoran Gojković, Nenad Simeunović, Danijela Gračanin, Aleksandra Milovančev, Dejan Ivanov, Marko Bojović, Miloš Bugarčić, and Nikola Stojić. 2022. "Healthcare Service Quality from the Point of Healthcare Providers’ Perception at the Time of COVID-19" Challenges 13, no. 1: 26. https://doi.org/10.3390/challe13010026
APA StyleIvanov, O., Gojković, Z., Simeunović, N., Gračanin, D., Milovančev, A., Ivanov, D., Bojović, M., Bugarčić, M., & Stojić, N. (2022). Healthcare Service Quality from the Point of Healthcare Providers’ Perception at the Time of COVID-19. Challenges, 13(1), 26. https://doi.org/10.3390/challe13010026






