Reliance on God’s Help Scale as a Measure of Religious Trust—A Summary of Findings
Abstract
:1. Background
2. The Reliance on God’s Help Scale: Description of Items
- Unconditional trust (“Whatever happens, I will trust in a higher power that carries me through”)
- Hopeful belief (“I have strong belief that God will help me”)
- Faith as a resource (“My faith is a stronghold, even in hard times”)
- Connection and effect/function (“I pray to become healthy again”)
- Behavioral correspondence (“I try to live in accordance with my religious convictions”)
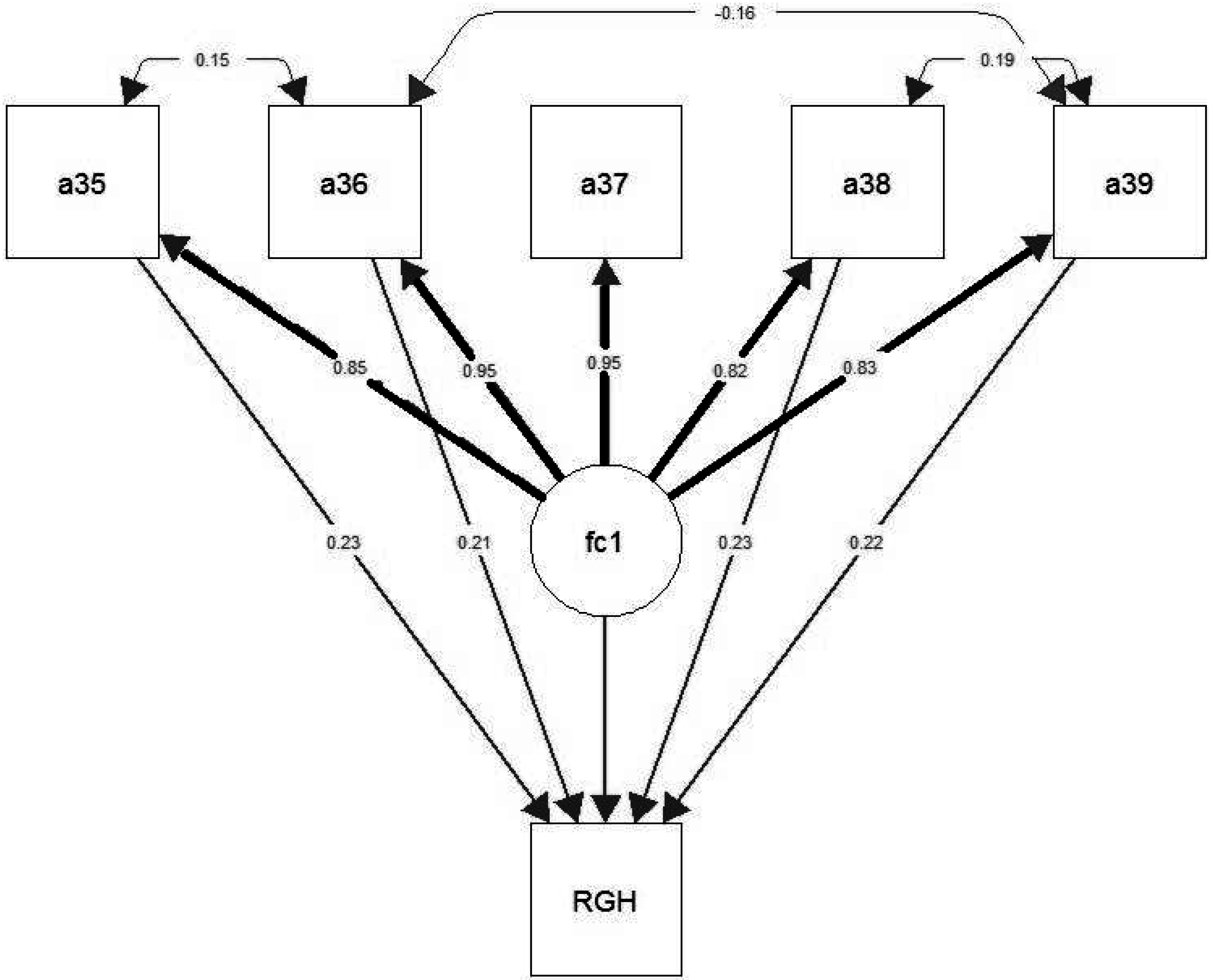
3. Reliance on God’s Help Scale: Internal Reliability Data and the Structural Equation Model
| Healthy persons [11] * | Chronic pain diseases [9] | Female cancer [8] | Depressive/addictive diseases [16] | Pastoral workers [17] * | |
|---|---|---|---|---|---|
| Sample size (n) | 3.593 | 448 | 390 | 110 | 5.460 |
| Mean age (years) | 63.9 ± 11.3 | 54.0 ± 14.9 | 59.7 ± 7.3 | 47.5 ± 10.1 | - |
| Cronbach’s alpha | 0.90 | 0.94 | 0.96 | 0.94 | 0.78 |
| Corrected Item—Scale Correlation | 0.77 to 0.87 | 0.79 to 0.92 | 0.82 to 0.93 | 0.77 to 0.91 | 0.46 to 0.66 |
| RGH Score (M ± SD) | 54.7 ± 34.8 | 55.3 ± 33.1 | 56.5 ± 35.0 | 45.8 ± 34.0 | 83.8 ± 14.0 |
| Agreement to Specific Statements | Scores (%): no—undecided—yes | ||||
| a35 “Whatever happens, I will trust in a higher power that carries me through” | 34 | 30 | 27 | 36 | 2 |
| 16 | 23 | 16 | 26 | 4 | |
| 50 | 47 | 57 | 39 | 94 | |
| a36 “I have strong belief that God will help me” | 32 | 29 | 30 | 40 | 2 |
| 18 | 23 | 17 | 21 | 8 | |
| 50 | 49 | 53 | 39 | 90 | |
| a37 “My faith is a stronghold, even in hard times” | 31 | 29 | 30 | 40 | 2 |
| 18 | 22 | 15 | 20 | 8 | |
| 51 | 49 | 55 | 40 | 90 | |
| a38 “I pray to become healthy again” ** | 40 | 35 | 34 | 54 | 2 |
| 16 | 16 | 13 | 12 | 6 | |
| 45 | 49 | 54 | 34 | 93 | |
| a 39 “I try to live in accordance with my religious convictions” | 37 | 35 | 36 | 49 | 8 |
| 17 | 19 | 20 | 20 | 9 | |
| 46 | 46 | 44 | 32 | 83 | |
4. Distribution of RGH Scores in Different Samples
5. Correlation between RGH Scores and Measures of Religiosity
| RHG scale | SpREUK’s Trust scale [13] |
|---|---|
| Whatever happens, I will trust in a higher power which carries me through. | Whatever happens, I will trust in a higher power which carries me through |
| I have strong belief that God will help me. | In my mind, I am connected with a “higher source”. |
| My faith is a stronghold, even in hard times. | I have faith in spiritual guidance in my life. |
| I pray to become healthy again. | I am convinced that death is not an end. |
| I try to live in accordance with my religious convictions. | In my mind, I am a religious individual. |
6. Methodological Issues: RGH is not Associated with Health-Related Measures
- faith (i.e., find comfort in faith; find strength in faith; difficult times have strengthened faith; know that whatever happens with illness, things will be okay),
- meaning (i.e., have a reason for living; life has been productive; feel a sense of purpose in life; life lacks meaning and purpose), and
- peace (feel peaceful; have trouble feeling peace of mind; able to reach down deep inside myself in order to feel comfort; feel a sense of harmony)
7. Conclusions
Acknowledgments
Conflicts of Interest
References
- Klaus Baumann. “The birth of human sciences, especially psychology.” In L’uomo moderno e la chiesa-atti del congresso (analecta gregoriana, 317). Edited by Paul Gilbert. Rome: Gregorian & Biblical Press, 2012, pp. 391–408. [Google Scholar]
- Harold G. Koenig, Dana King, and Verna Benner Carson. Handbook of Religion and Health, 2nd ed. Oxford: Oxford University Press, 2010. [Google Scholar]
- Richard S Lazarus, and Susan Folkman. Stress, Appraisal, and Coping. New York: Springer, 1984. [Google Scholar]
- Julian B. Rotter. “Generalized expectancies for internal versus external control of reinforcement.” Psychological Monographs: General & Applied 80 (1966): 1–28. [Google Scholar] [CrossRef]
- Hannah Levenson. “Multidimensional locus of control in psychiatric patients.” Journal of Consulting and Clinical Psychology 41 (1973): 397–404. [Google Scholar] [CrossRef] [PubMed]
- Arndt Büssing. “Health-related quality of life and reliance on god’s help.” In Encyclopedia of Quality of Life and Well-Being Research. Edited by Alex C. Michalos. Dordrecht: Springer, 2014, pp. 2801–7. [Google Scholar]
- Karin Jors, Arndt Büssing, Nield Christian Hvidt, and Klaus Baumann. “Personal prayer in patients dealing with chronic illness: A review of the research literature.” Evidence-based Complementary and Alternative Medicine 2015 Article 927973. (2015). [Google Scholar] [CrossRef] [PubMed]
- Arndt Büssing, Julia Fischer, Thomas Ostermann, and Peter F. Matthiessen. “Reliance on god’s help, depression and fatigue in female cancer patients.” The International Journal of Psychiatry in Medicine 38 (2008): 357–72. [Google Scholar] [CrossRef] [PubMed]
- Arndt Büssing, Nadja Keller, Andreas Michalsen, Susanne Moebus, Gustav Dobos, Thomas Osterman, and Peter F. Matthiessen. “Spirituality and adaptive coping styles in german patients with chronic diseases in a cam health care setting.” Journal of Complementary and Integrative Medicine 3 (2006): 1553–3840. [Google Scholar] [CrossRef]
- Arndt Büssing, Thomas Ostermann, and Peter F. Matthiessen. “Wer kontrolliert die Gesundheit?—Adaptive Krankheitsverarbeitungsstile bei Patienten mit chronischen Erkrankungen.” Deutsche Zeitschrift für Onkologie 40 (2008): 140–56. [Google Scholar]
- Arndt Büssing, Thomas Ostermann, and Peter F. Matthiessen. “Adaptive coping and spirituality as a resource in cancer patients.” Breast Care 2 (2007): 195–202. [Google Scholar]
- Arndt Büssing, Thomas Ostermann, and Peter F. Matthiessen. “Role of religion and spirituality in medical patients: Confirmatory results with the SpREUK questionnaire.” Health and Quality of Life Outcomes 3 (2005): 10. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Arndt Büssing. “Spirituality as a resource to rely on in chronic illness: The SpREUK questionnaire.” Religions 1 (2010): 9–17. [Google Scholar] [CrossRef]
- Kenneth I. Pargament. The Psychology of Religion and Coping: Theory, Research, Practice. New York: Guilford Press, 1997. [Google Scholar]
- Russel E. Phillips III, Quinten K. Lynn, Craig D. Crossley, and Kenneth I. Pargament. “Self-directing religious coping: A deistic god, abandoning god, or no god at all? ” Journal For The Scientific Study Of Religion 43 (2004): 409–18. [Google Scholar]
- Arndt Büssing, and Götz Mundle. “Reliance on god’s help in patients with depressive and addictive disorders is not associated with their depressive symptoms.” Religions 3 (2012): 455–66. [Google Scholar] [CrossRef]
- Eckhard Frick, Arndt Büssing, Klaus Baumann, Wolfgang Weig, and Christoph Jacobs. “Do self-efficacy expectation and spirituality provide a buffer against stress-associated impairment of health? A comprehensive analysis of the german pastoral ministry study.” Journal of Religion and Health. Published electronically 27 March 2015. Available online: http://link.springer.com/article/10.1007/s10943-015-0040-7. [CrossRef]
- Lynn G. Underwood, and Jeanne A. Teresi. “The daily spiritual experience scale: Development, theoretical description, reliability, exploratory factor analysis, and preliminary construct validity using health-related data.” Annals of Behavioral Medicine: A Publication of the Society of Behavioral Medicine 24 (2002): 22–33. [Google Scholar] [CrossRef]
- Lynn Underwood. “The daily spiritual experience scale: Overview and results.” Religions 2 (2011): 29–50. [Google Scholar] [CrossRef]
- Amy H. Peterman, George Fitchett, Marianne J. Brady, Lesbia Hernandez, and David Cella. “Measuring spiritual well-being in people with cancer: The functional assessment of chronic illness therapy—Spiritual well-being scale (FACIT-Sp).” Annals of Behavioral Medicine 24 (2002): 49–58. [Google Scholar] [CrossRef] [PubMed]
- Jason M. Bredle, John M. Salsman, Scott M. Debb, Benjamin J. Arnold, and David Cella. “Spiritual well-being as a component of health-related quality of life: The functional assessment of chronic illness therapy—Spiritual well-being scale (FACIT-Sp).” Religions 2 (2011): 77–94. [Google Scholar] [CrossRef]
- Andrea L. Canada, Patricia E. Murphy, George Fitchett, Amy H. Peterman, and Leslie R. Schover. “A 3-factor model for the FACITt-Sp.” Psycho-oncology 17 (2008): 908–16. [Google Scholar] [CrossRef] [PubMed]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Büssing, A.; Recchia, D.R.; Baumann, K. Reliance on God’s Help Scale as a Measure of Religious Trust—A Summary of Findings. Religions 2015, 6, 1358-1367. https://doi.org/10.3390/rel6041358
Büssing A, Recchia DR, Baumann K. Reliance on God’s Help Scale as a Measure of Religious Trust—A Summary of Findings. Religions. 2015; 6(4):1358-1367. https://doi.org/10.3390/rel6041358
Chicago/Turabian StyleBüssing, Arndt, Daniela Rodrigues Recchia, and Klaus Baumann. 2015. "Reliance on God’s Help Scale as a Measure of Religious Trust—A Summary of Findings" Religions 6, no. 4: 1358-1367. https://doi.org/10.3390/rel6041358
APA StyleBüssing, A., Recchia, D. R., & Baumann, K. (2015). Reliance on God’s Help Scale as a Measure of Religious Trust—A Summary of Findings. Religions, 6(4), 1358-1367. https://doi.org/10.3390/rel6041358








