Abstract
The positive effects of religion and/or spirituality through faith-based interventions on health and promoting health programs have been well documented over the last two decades. Research indicates that faith-related programs can motivate increased physical activity, among other behaviors. This review summarizes the literature on how religion and spirituality beliefs and practices support physical, mental, and psychosocial health, focusing primarily on physical activity. A literature search was conducted using databases (Medline/PubMed, Science Direct) and Google Scholar, with search terms like “religion”, “spirituality”, “physical activity”, “physical exercise”, and “health” to identify relevant studies from 2017 to 2023. Thirteen studies were selected, including seven cross-sectional designs, four randomized controlled trials, and two cohort studies. Eleven of these studies reported positive effects of religious faith, religiosity, and spirituality interventions on increasing physical activity or reducing sedentary behavior. These findings confirm that greater religious commitment is positively associated with better health outcomes, including increased physical activity. This research suggests that further studies are needed to identify specific religiosity/spirituality variables in the context of physical activity association and to clarify the underlying mechanisms. Such insights may inform the development of intervention programs aimed at promoting physical activity and strengthening health associations.
1. Introduction
Numerous studies have examined the effects of religiosity (R) and spirituality (S), (R/S), on health-related components (Seeman et al. 2003; Schlundt et al. 2008; Basu-Zharku 2011; Koenig 2012; VanderWeele 2017; Kang et al. 2020; Kvesić et al. 2020; Svensson et al. 2020; de Diego-Cordero et al. 2022; Aggarwal et al. 2023). The terms R and S are multidimensional constructs having different definitions, although they are related to each other (Paul Victor and Treschuk 2020; Gschwandtner 2021; Koenig et al. 2023). These constructs have been widely discussed in the literature and applied in a variety of contexts (Koenig 2012; Koenig et al. 2023). Evidence has shown much controversy and disagreement concerning definitions of these terms. According to Koenig (2012) “religion involves beliefs, practices, and rituals related to the transcendent”; R is an organized system that operates symbols, facilitating closeness to the sacred or transcendent (Koenig et al. 2023). In turn “Spirituality is intimately connected to supernatural, the mystical, and to organized religion”, although it also extends beyond R and begins before it, whereas faith is often correlated with R and S and is more personal (Koenig 2012). The literature data have maintained that R/S may positively change the health behaviors of both healthy people and patients with chronic diseases and cancer survivors, providing community support and self-acceptance regardless of religious affiliation (Powell et al. 2003; Seeman et al. 2003; Rassouli et al. 2015; Lumpkins et al. 2019; Hamdan et al. 2020). Research findings have shown a strong correlation of R/S with some determinants of physical health for pain, fatigue, physical well-being, mental health (depression, anxiety, emotional well-being), and psychosocial health (social distress, social well-being, social relationships and activity, support, or distress) (Salsman et al. 2015; Sherman et al. 2015; Shattuck and Muehlenbein 2020).
Recent evidence maintains that R/S faith creates optimism and quality of life (Salsman et al. 2015). A recently published review investigating the relation of R and S to lifestyle practices in religious communities (McManus 2024) reported that religious practices and communal living positively affect successful aging and well-being in older individuals. Improving quality of life and social interactions was reported to be positively correlated with S/R. Evidence has shown that social theories are well established to describe PA behaviors (Bauman et al. 2012; Stehr et al. 2021). According to these theories, individuals’ PA behaviors are determined by several factors, like interpersonal, physical, cultural, social, environmental (Alves and Oliveira 2018). A recent qualitative study by Stehr et al. (2021) presented two cognitive theories: the Theory of Planned Behavior and the Self-Determination Theory. Based on these theories, the authors suggest that the interplay between individuals’ beliefs and motivation is essential regarding PA among older people and can explain the complexity of their behavior. In a previous article, we explored faith-based health promotion interventions on Latino and African American populations (Blankinship et al. 2021). We demonstrated that faith-based health programs might affect positive healthy lifestyle, including long-term physical activity/physical exercise (PE), (PA)/(PE), cultural appropriateness, social community support, and self-efficacy. Moreover, evidence has shown that R and S play important roles in enhancing sports performance and contributing to athletes’ well-being (Noh et al. 2023). In addition, PA and sports have been closely linked regarding their effect on health-related components. Findings on the positive effect of R/S on the increase in PA is essential because physical inactivity, obesity/overweight, poor diet, and psychological stress, as well as other unhealthy behavioral risk factors, are initiators of oxidative stress (OS) and inflammation of the factors accompanying numerous chronic diseases, including cancer incidence and progression (Irwin 2009; Kruk et al. 2019a, 2019b). In addition, a sedentary lifestyle and obesity are prevalent among cancer survivors (Irwin 2009). Regular PA has been regarded as an integral part of promoting physical and mental health and well-being and as a tool to prevent and manage several chronic diseases (Saxena et al. 2005; Warburton et al. 2006; Koenig 2012; Neufer et al. 2015; VanderWeele 2017). However, supportive evidence shows that the global prevalence of physical inactivity remains high. According to the World Health Organization data, “Globally, 1 in 4 adults do not meet the global recommended levels of physical activity”, i.e., engaging in regular aerobic PA at least 150–300 min/week of moderate-intensity (3–<6 METs) or at least 75–150 min/week of vigorous-intensity activity (≥6 METs) or the equivalent combination of both intensities of activity (Bull et al. 2020). Physical inactivity has been regarded as the principal factor increasing overweight and obesity, which, together with unhealthy diets, leads to obesity-related disease burden and mortality worldwide. Consequently, there is a need to develop appropriate, cost-effective PA interventions to reduce sedentary lifestyles. One approach proposed is to use the R- and S-based programs (Blankinship et al. 2021). Given these facts, it is essential to recognize how R and S may stimulate individuals to undertake PA. This is important, especially since R/S plays an essential role in many people’s daily lives and PA is an integral part of people’s lives (Almaraz et al. 2022). The literature to date mostly emphasizes the R/S contribution to mental rather than physical health benefits (Vitorino et al. 2018; Lucchetti et al. 2021). Moreover, the scientific literature relating specifically to the impact of R and S on levels of PA is limited, reports scarce findings, and is based most often on cross-sectional studies (Almaraz et al. 2022; de Diego-Cordero et al. 2022; Aggarwal et al. 2023). The high percentage of adults who do not reach the current public health recommendations for PA for increased life expectancy and the essential impact of physical inactivity on chronic and age-dependent diseases support the need to update findings focusing on the association between R/S and PA as a potential factor in healthcare. Referencing the meta-analysis by Jim et al. (2015) that reported the beneficial effects of R and S on cancer patients’ health and a similar role of PA (Saxena et al. 2005; Warburton et al. 2006; Neufer et al. 2015), understanding the biological mechanisms operating between these factors is necessary. Therefore, this paper aims to review the impact of religious faith and spiritual practice on health components, mainly PA/PE. The objective of this paper was to (1) highlight briefly the beneficial role of R and S in health-related components: physical health, psychosocial health, mental health, and psychological well-being; (2) identify the post-2017 scientific literature evidence on the effect of R and S on engaging in PA/PE; and (3) discuss the biological plausibility of these putative associations. We also highlight areas for future studies.
2. Materials and Methods
2.1. Study Design
This systematic review briefly demonstrates actual knowledge about the effect of R and S on human health and analyzes the effect of these terms on involvement in PA.
2.2. Search Strategy
We followed the PRISMA quality standards methodology for reporting in this review. The review design involved a literature search in July 2022, which was updated in December 2023. The articles were searched and selected using the databases Medline/PubMed and Science Direct, along with Google Scholar (first 100 hits). In addition, we manually searched the reference lists of relevant articles, reviews, and meta-analysis papers. The terms “religion”, “spirituality”, “physical activity”, “physical exercise”, and “health” were applied as search terms, linked to each other through the Boolean operators “OR” and “AND”: (“spirituality” OR “spiritualities” OR “Religion” OR “Religions” OR “Religious”) AND “Physical Activity” OR “Physical Exercises” OR “Exercises” OR “Sports”).
2.3. Selection Criteria
The following inclusion criteria were defined: (1) observational studies and experimental studies published between January 2017 and December 2023, (2) reviews and meta-analyses, (3) studies of individuals aged ≥18 years, (4) studies published only in peer-reviewed journals in English, (5) studies with PA/PE and R/S measurement tools, (6) studies providing quantitative information on the associations between R/S and PA. The interaction of R and S on health-related components was examined separately by reviewing the literature on this topic. We excluded individuals under 18 years of age and studies based on small sample sizes of participants.
2.4. Data Extraction
Both authors reviewed the titles and abstracts of the retrieved articles independently for inclusion against the eligibility criteria. Any disagreements were resolved through discussion. The extracted data include name of first author, year of publication, country, study design, aim of a study, participants’ characteristics, study sample, instruments used to measure R and S, evaluation of PA/PE (self-reported or objectively measured), main results (odds ratios (ORs) with corresponding 95% confidence intervals (CIs), logistic regression coefficient, changes in PA dimension).
3. Results
3.1. Selected Articles
Figure 1 shows the flow diagram of the included and excluded articles.
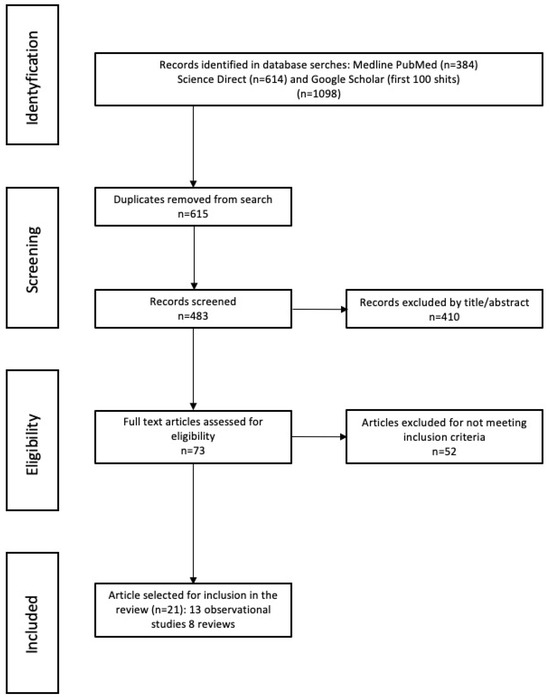
Figure 1.
Flow diagram of the literature review process.
A total of 1098 potential articles were originally retrieved. After removing duplicates (n = 615) and excluding records by titles and abstracts, we evaluated the full texts of 73 articles. Finally, 21 were included in this review, reporting the association of R and S with PA/PE. Of the included studies, 13 were observational studies, and 8 were reviews and meta-analysis research; the remaining studies (n = 52) did not meet inclusion criteria. We also identified additional articles through other sources (reference lists of selected articles, Google Scholar to present briefly the role of R and S in physical and mental health).
3.2. Role of Religion and Spirituality in Mental and Physical Health
Much effort has been devoted to addressing the association of R and S with health-related determinants among either healthy people or people suffering from chronic diseases (Salsman et al. 2015; Sherman et al. 2015; Ferreira et al. 2020; Kopeyko et al. 2020; Moreira et al. 2020; Shattuck and Muehlenbein 2020; Borges et al. 2021; Reisi et al. 2021; Almaraz et al. 2022). Research has generated interactions of R and S with several components of physical health, social well-being and community support, mental health, and psychological well-being, among others (Figure 2).
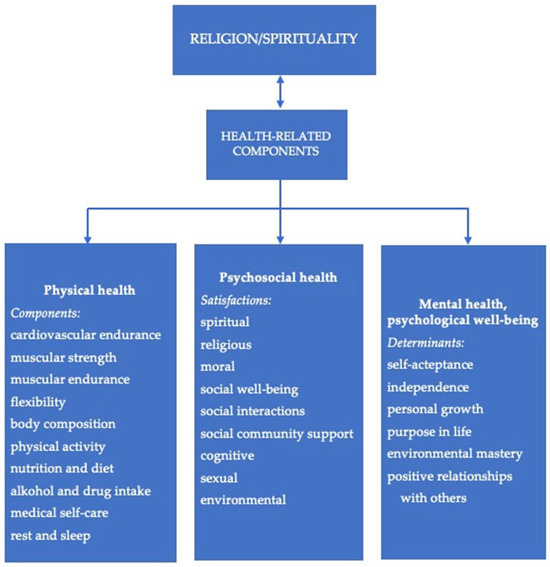
Figure 2.
Schematic presentation of the interaction between religion and/or spirituality and health-related components (after Shojaee and French 2014; Gonçalves et al. 2017; Rathod 2021; Almaraz et al. 2022; Hussain and Cunningham 2023; Koenig et al. 2023).
In this regard, the recent review by Doyle and Link (2024) demonstrated the tripartite model of health incorporating social, physical, and mental health localized in the human body, including the mind. The authors defined social health as “adequate quantity and quality of relationships in a particular context to meet an individual’s need for meaningful human connection.” Through a longitudinal study of three cohorts of different ages, Chen et al. (2021) found that religious beliefs and religious service attendance are essential forms of social integration potentially correlated with greater longevity, better mental health, healthier lifestyles, and greater psychosocial well-being. A large part of these studies focused on the relationship between R and S and mental health among patients diagnosed with cancer (Salsman et al. 2015; Sherman et al. 2015; Reisi et al. 2021). Because of space limitations, we will limit their presentation to representative reviews and observational studies. A systematic review of ten selected studies among healthy people by Borges et al. (2021) found that higher R or S levels among individuals were significantly associated with higher health-related quality-of-life domains such as physiological and social relationships and being prepared for environmental problems, e.g., pollution and global warming. The R and S aspects significantly impacted feelings of optimism, inner strength, hope, and happiness. Most studies deal with health problems in cancer patients as they are exposed to chronic stress that negatively affects many mental health outcomes. Cancer also negatively alters cancer survivors, as well as their family members, generating a disturbance in physical health and various mental health issues, such as feelings of fear, pain, anxiety, depression, sleep disturbance, and often hopelessness (Sun et al. 2019; Hashemi et al. 2020). Evidence has shown that R and S may be an effective approach to maintaining mental health and help in coping with cancer-related symptoms, thus improving physical and mental well-being (Rassouli et al. 2015; Salsman et al. 2015; Gonçalves et al. 2017; Ferreira et al. 2020; Yan et al. 2020; Almaraz et al. 2022; Goerge et al. 2023). Although research examining spiritual care relevant to cancer-related health outcomes is limited, current findings suggest moderate effects of spirituality in reducing anxiety and depression and improving well-being. Salsman et al. (2015) reviewed 148 studies with over 39,000 cancer cases, finding that greater R or S scores were corrected modestly with mental health. The effect depended on the R and S dimensions (affective and behavioral) and mental health domains (emotional well-being, general/cancer-specific distress, anxiety, depression). Another review of observational studies (n = 8) conducted in Iran from 2006 to 2020 by Reisi et al. (2021) on the effect of R/S on anxiety and depression in cancer patients confirmed a significant positive role of greater religious commitment toward coping with anxiety and depression. Jim et al. (2015) reviewed 101 articles that included 32,000 adult cancer patients, noticing a positive association between R/S with affective domains (feelings, emotions, attitudes), cognitive domains (knowledge, development of intellectual skills), and physical health outcomes. The authors found a statistically significant association between increased overall R/S and better overall physical health and functional well-being among cancer cases. Psychosocial health has also been the subject of several studies concerning R/S. For example, a meta-analysis by Sherman et al. (2015) of 78 studies with 14,277 individuals diagnosed with cancer dealing with the association of social health with overall R and S and their dimension with behavioral R/S reported that social health outcomes were modestly associated with the overall terms. Another review of 37 studies carried out between January 2009 and January 2019 by Ferreira et al. (2020) showed that R/S positively influence the biopsychosocial health of cancer patients, observing improved acceptance of cancer treatment, positive effects of the therapy, and greater hope of recovery. The suggestion that these terms consist of an essential coping strategy in psychological stress linked with cancer disease was also reported by Borges et al. (2021). Likewise, the observational studies (Al Eid et al. 2020; Hamdan et al. 2020; Kvesić et al. 2020; Kowalczyk et al. 2022), focusing on the role of R/S in the adaptation of cancer patients to the disease and the treatment, have confirmed that patients sought help in faith and spirituality. Also, the findings of an observational study that tested 294 cancer patients of both sexes from Saudi Arabia confirmed that the R and S support programs are an essential source for the patients’ social enhancement and healthcare delivery (Koenig et al. 2023). In turn, a cross-sectional study of 100 oncology patients and 80 internal medicine patients, carried out by Kvesić et al. (2020), observed that a lower level of religiousness is correlated with higher severity of psychological symptoms. Further, an observational study by Al Eid et al. (2020) examined 329 women with breast cancer in Saudi Arabia, reporting a statistically significant positive moderate correlation between the level of religiosity and psychological resilience independent of the stage of cancer and the duration of cancer treatment. They concluded that increased religiosity and psychological resilience are essential for cancer patients’ mental health outcomes. It is interesting to note that R and S can also help oncologists cope with negative emotions when working with their patients (Kowalczyk et al. 2022). The authors analyzed data from 60 medical clinicians specializing in oncological radiotherapy. The finding is that the R or S terms can help clinicians manage the challenging negative emotions connected with their work with cancer patients. Similarly, the current reviews show that practicing R or S is associated with better health and well-being. For example, Aggarwal et al. (2023) reported that religiosity and spirituality are positively correlated with mental well-being and health outcomes in adolescents, based on 45 longitudinal and 29 interventional studies. Also, a systematic review and meta-analysis of 18 clinical trials by de Diego-Cordero et al. (2022) reported that spiritual interventions decreased mental health symptoms, increased well-being, and elevated spirituality levels. Moreover, Almaraz et al. (2022) reviewed articles published between 2015 and March 2022 (26 articles selected), generally reporting a positive correlation of R/S with physical health in cancer patients. However, they also noticed a negative correlation. Also, earlier systematic reviews of RCTs by Gonçalves et al. (2017) (30 studies) demonstrated small benefits from R/S regarding physical health outcomes or quality of life in chronic patients, healthy individuals, and healthcare professionals. The reported findings have shown that recent research concentrated mainly on the effect of R/S on mental health and well-being. To summarize the above findings, the observed inconsistency in influence magnitudes may be due to methodological differences among studies, such as study design and the methods used to measure R/S variables, type of faith-based intervention, and health outcomes. Well-designed RCTs could provide valuable information on how these variables can influence health outcomes and identify more precise operating mechanisms between these variables.
3.3. Religion, Spirituality and, Physical Activity
3.3.1. Findings from Reviews
From a total of 1098 citations, we identified seven systematic reviews (five published between 2017 and 2023 and two dated from 2012) which summarized the previous evidence in this area.
To our knowledge, epidemiological research explicitly focused on the impact of R or S on PA was the subject of a limited number of reviews (Bopp et al. 2012; VanderWeele 2017; Parra et al. 2018; Moreira et al. 2020; Noh and Shahdan 2020; Maroney et al. 2023). Bopp et al. (2012) analyzed 19 faith-based interventions, focusing on spiritual or Biblical components and 8 faith-based interventions examining the effect of engaging PA within the African American community. They found increased PA in 12 of the 19 faith-based studies and four faith-based interventions among church members. However, the findings in most of these studies were based on self-reported PA. Koenig (2012) reviewed 37 studies on the relationship between R/S and exercise and PA published through 2010. The authors noticed that most studies reported a positive effect of R/S on health: 22 of the 37 reported significant positive associations between R/S and increased PA or engaging in exercise, and 6 reported inverse associations. Furthermore, of the 21 studies evaluated by the author as having the highest quality, 16 found positive relationships between these variables. Parra et al. (2018) reviewed 18 randomized and nonrandomized controlled trials on the PA interventions for adults associated in faith-based church organizations, mainly in the US, published through January 2016. They found increased PA and positive effects on their members’ health outcomes and physical fitness. The authors concluded that faith-based organizations provide support for the promotion of PA, and they mention the need for high-quality RCTs to improve the strengths of the evidence. In turn, a review by VanderWeele (2017) on the association between religion and PE and the power of faith-based intervention on diet quality and exercise suggested the positive effect of religion on promoting greater PE, with the effect dependent on the type of religious group. A systematic review of eight cohort and case-control studies, published between 2011 and 2017 by Moreira et al. (2020) on the effect of R and S on PA promotion, reported that spiritual practices such as prayer, awareness of God, spiritual meaning, and forgiveness can have a positive effect on participation in PA. In turn, a review by Noh and Shahdan (2020) on the role of R/S in sports performance (reviewed 56 articles) also reported a positive effect of these variables for athletes, e.g., through coping strategies, anxiety reduction, healing, and well-being. Another systematic review by Maroney et al. (2023) analyzed the effectiveness of church-based interventions for cardiovascular disease risk factors, including low PA. The authors analyzed 16 RCTs, three nonrandomized trials, and six pre–post comparisons. They found significant increases in PA in 12 studies and no significant effects of religious intervention in the remaining studies.
3.3.2. Findings from Experimental Studies
Characteristics of the included experimental studies are shown in Table 1.

Table 1.
The effects of religion and/or spirituality on engaging in physical activity/physical exercise.
From a total of 1098 citations, we identified 13 original studies which were eligible and met inclusion criteria, with the year 2023 showing 4 (30.8%) articles. Regarding the country of origin, eight were studies from the USA, two studies were developed in Europe, with one study consisting of international research involving several European countries, and the remaining studies were developed in Australia, Malaysia, and South Korea (one study each).
Considering the study methodology, seven studies (Silfee et al. 2017; Waters et al. 2018; Svensson et al. 2020; Buro et al. 2023; Goerge et al. 2023; Hussain and Cunningham 2023; Noh et al. 2023) used a cross-sectional design, four were RCTs (Ansari et al. 2017; Arredondo et al. 2017; Whitt-Glover et al. 2017; Wilcox et al. 2018), and two were cohort studies (Ahrenfeldt et al. 2018; Kang et al. 2020). Eleven studies used validated questionnaires and self-reports to obtain information on engagement in PA practice and two studies (Whitt-Glover et al. 2017; Wilcox et al. 2018) used electronic devices for PA assessment. The sample size ranged from 177 to 23,864; in four studies (Ansari et al. 2017; Whitt-Glover et al. 2017; Goerge et al. 2023; Hussain and Cunningham 2023), only women participated, and in one study (Buro et al. 2023) only men participated. The remaining eight studies included individuals of both genders. Two studies (Ansari et al. 2017; Waters et al. 2018) estimated the effect of R and S in cancer survivors.
Regarding the R and S variables used, six studies (Ahrenfeldt et al. 2018; Kang et al. 2020; Svensson et al. 2020; Buro et al. 2023; Hussain and Cunningham 2023; Noh et al. 2023) reported the effect of the R variable on PA, two studies (Silfee et al. 2017; Goerge et al. 2023) reported the impact of the S variable, two studies (Ansari et al. 2017; Waters et al. 2018) used R and S variables, and three studies (Arredondo et al. 2017; Whitt-Glover et al. 2017; Wilcox et al. 2018) developed faith-based interventions. Nine of thirteen studies reported a relationship between R/S variables and PA; the remainder considered PA as one of the health-related behavior components nnn ,m (Ansari et al. 2017; Ahrenfeldt et al. 2018; Kang et al. 2020; Svensson et al. 2020). A detailed description of the objectives, the type of design, the main characteristics of participants, a description of R/S and PA measures, and the results is shown in the table.
Eleven of thirteen studies reported quantitative data, providing odds ratios (ORs) (Silfee et al. 2017; Ahrenfeldt et al. 2018; Waters et al. 2018; Kang et al. 2020; Svensson et al. 2020; Buro et al. 2023; Goerge et al. 2023; ), the regression coefficient β (Hussain and Cunningham 2023), or correlation coefficient (Silfee et al. 2017; Buro et al. 2023; Noh et al. 2023) for daily walking steps (Whitt-Glover et al. 2017), energy expenditure (Ansari et al. 2017), or increased duration of activity (Arredondo et al. 2017). It must be underlined that the methods used in these studies were quite heterogeneous, thus ruling out the possibility of carrying out an overall quantitative estimate of the R/S effect on PA. Two of the thirteen studies (Ansari et al. 2017; Noh et al. 2023) found no association between R or S faith and PA. The remainder of the studies reported positive correlations between R/S and PA. The effect of spirituality was examined in healthy students (Waters et al. 2018) and among breast cancer survivors (Goerge et al. 2023). Both studies reported increased activity for a higher spirituality score. Waters et al. (2018) noticed that frequency, duration, and increased activity levels were age-dependent. A study by Goerge et al. (2023) demonstrated that the magnitude of the association ranged from a 78% increase in PA meeting the activity guidelines to a 90% increase for engaging in activity at least 681 min/wk. A statistically significant effect of spirituality on decreased sedentary behavior was also found in Latino and Hispanic men (Noh et al. 2023). Regarding the association between religious practice and faith-integrated interventions, reduced sedentary behavior was reported in the seven studies (Arredondo et al. 2017; Whitt-Glover et al. 2017; Ahrenfeldt et al. 2018; Wilcox et al. 2018; Kang et al. 2020; Buro et al. 2023; Hussain and Cunningham 2023). The results were distributed between a decrease in physical inactivity in participants who prayed or participated in a religious organization (by 12% and 46%, respectively) (Ahrenfeldt et al. 2018), the increased opportunity to engage in PA practice more frequently (Wilcox et al. 2018), the positive correlation between religion and PA intention in Muslim women (Hussain and Cunningham 2023), a two-fold increase in practicing vigorous activity (OR = 2.20) in Catholics (Kang et al. 2020), an increased weekly duration of PA (Arredondo et al. 2017; Buro et al. 2023), and increased daily walking over baseline (Whitt-Glover et al. 2017).
4. Discussion
First, this review summarizes the results of the research on the relationship between R/S and PA practice. We also summarize the research on the role of R/S in human health. Overall, previous reviews and the current review indicate a great potential for R/S to influence health-related components. We found that the literature presented in this article documented the epidemiological evidence and provided strong support for a positive correlation between R/S variables and some determinants of health outcomes regarding an influence on mental health and physical health outcomes or at least the correlation between these variables. This topic has been considered in relation to healthy people and patients with chronic diseases, particularly cancer patients. We believe the retrieved representative reviews and meta-analyses demonstrate previous and recent interest in the topic. The extracted studies have shown mixed results depending on the study design in which the R/S variables were measured. We observed that although this research topic is of great interest, a relatively small number of studies are focused on the effect of R/S on the physical health component—PA practice; the most recent research in this area mainly focuses on mental health and psychological well-being. Regarding the effect of R/S on PA, the majority of analyzed observational studies were carried out in developed countries, mainly in the USA, causing the findings to be difficult to generalize for populations in less developed countries, which have other demographic, social, and cultural characteristics that influence the health and disease process (Noh and Shahdan 2020). This highlights the need for future epidemiological observational studies to fill the gap in this field of research. Considering the objective of examining the effect of the R/S variables on PA practice, we found that the authors of the included studies in this review most often used validated questionnaires as instruments, such as the Daily Spirituality Experience Scale (Sun et al. 2019), the Lukwago Religiosity Scale (Chen et al. 2021), the Fetzer Short-Form Questionnaire for Measurements of Religiousness and (Goerge et al. 2023), and the Santa Clara Strength of Religious Faith Questionnaire (Hashemi et al. 2020). They gathered information on religious affiliation, frequency of praying, meditation practice, religious organization, etc. The other methods included a Faith and Secular Curriculum questionnaire to measure participation in biblical scripture and faith tenets (Kowalczyk et al. 2022) or questions regarding the frequency of attendance in a religious organization and frequency of praying (Parra et al. 2018). Thus, spiritual practice and religious expressions are different between the studies.
Regarding measures of PA, only two studies (Arredondo et al. 2017; Wilcox et al. 2018) applied objective measurements of PA levels using accelerometers and pedometers. The other studies carried out a subjective estimation of activity based on valid questionnaires or answers to questions about the type, frequency, intensity, and duration of PA practice (Lee et al. 2011; Ahrenfeldt et al. 2018). Electronic movement monitors provide objective activity measures but are non-practical in large-scale cohort studies. In turn, evidence indicates that the reliability of findings using a questionnaire is often insufficient in contrast to its validity, and very few developed questionnaires show both features well (validity and reliability) (Helmerhorst et al. 2012). For example, the International Physical Activity Questionnaire (IPAQ) appears to have good validity but worse reliability (Lee et al. 2011). Although there are concerns about repeatability and agreement for activity classification, both forms of the IPAQ (short and long) are commonly used to assess PA. Another questionnaire, the Global Physical Activity Questionnaire (GPAQ), was also used in the reviewed articles as a tool that minimizes difference in PA assessment between different countries. Its features increase usage compared to the IPAQ short and long forms (Stelmach 2018). Both questionnaires, IPAQ and GPAQ, allow us to estimate all domains of activity and their components and time in a sitting position.
It is known that self-reported PA/PE practices are often overestimated. This observation is seen in Arredondo et al.’s study (2017) (Table 1), where the authors reported significant increases in PA duration measured using an accelerometer and those reported by participants (22 min/wk and 40 min/wk, respectively).
Among the studies analyzed in this review, 11 reported consistent findings of the positive effects of religious faith or R/S intervention on the increased practice of PA or reduction in sedentary behavior, showing moderate to significant effects. Four studies (RCTs) (Ansari et al. 2017; Arredondo et al. 2017; Whitt-Glover et al. 2017; Wilcox et al. 2018) had an intervention design with intervention time ranging from 4 to 12 months, and two of them assessed PA using electronic devices (Al Eid et al. 2020; Kowalczyk et al. 2022). The R/S intervention programs also varied greatly in their mode and demographic factors. Regarding the reviewed studies in this article, the small number of studies, variations in the applied faith-based interventions, and large heterogeneity among the chosen research regarding the categorization of PA made meta-analysis impossible. However, the present study indicates a statistically significant positive effect of R/S on practicing PA/PE observed in approximately 85% of the retrieved studies. This finding agrees with the findings of the above-reported previous reviews on this topic (Bopp et al. 2012; Koenig 2012; VanderWeele 2017; Moreira et al. 2020; Noh and Shahdan 2020). It is worthwhile to add that the above-reported findings in the above reviews, as well as our findings, have shown mixed results, i.e., some studies did not confirm a direct correlation between R/S and PA. It may depend on how the R/S variables were operationalized and how PA was assessed (among other factors).
Due to a similar health benefit exerted by regular moderate to vigorous PA regarding mental and physical health, social interactions, and psychological well-being, physically active people may be more likely to engage in religious and spiritual practices. Research undertaken in the exercise and sports sciences has shown the correlation between happiness and sports participation (Balish et al. 2016) and between happiness and religious practice (Balish et al. 2016; Rizvi and Hossain 2017). In turn, the recent study by Tejero-Gonzales (Tejero-González 2020) on a large sample size (2378 individuals) reported the highest level of happiness in people who both participate in sports and practice a religion. However, a small correlation size was found. Benefits of co-exercise between sports participation and the use of sport in religion, including strengthening national unity, church membership, self-discipline, and coping with uncertainty, were reported (Wankel and Berger 1990; Jona and Okou 2013; Malm et al. 2019).
Although the biological processes responsible for the R/S effect on health-related components are not fully understood, several biologic pathways have been hypothesized: R/S are associated with lowered blood pressure, decreased levels of diabetes, and lowered cardiovascular risk markers and inflammatory markers (T cells, CRP, neutrophils/monocytes) (Seeman et al. 2003; Duru et al. 2010; Shattuck and Muehlenbein 2020). The researchers have maintained that the beneficial effect of the R/S variables could originate from the reduction in psychological stress levels and depression, followed by a reduction in inflammation. These interesting findings are the natural extension of earlier studies by Seeman et al. (2003). The authors reported that greater religious commitment is linked with lower blood pressure and reduced prevalence of hypertension, lower cholesterol and stress hormone levels, better lipid profiles, and improved immune functions. They also observed lower OS and better health outcomes. Regular moderate to vigorous PA with appropriate resting periods is a well-established component of a healthy lifestyle, as are medicine for treating inflammatory diseases (Cerqueira et al. 2020) and reducing fatigue and depression in cancer patients (Odynets et al. 2019). The health benefits of PA/PE are achieved by reduction in visceral adipose tissue and obesity, an increase in insulin sensitivity, improvement of lipid and carbohydrate metabolism, activation of redox-sensitive signaling, reduction in inflammation and oxidative stress, enhancement of immune system response by increasing the circulation of immune cells, enhancement of the expression of genes responsible for the generation of antioxidant enzymes, reduction in pro-inflammatory cytokines, increase in anti-inflammatory cytokines (IL-10, interleukin-1 receptor IL-1Ra), and reduction in psychological stress, among others (You et al. 2013; Silverman and Deuster 2014; Kruk et al. 2019b; Cerqueira et al. 2020). It is plausible that an increase in PA among participants exposed to the various R/S variables may partially explain the mechanism of their positive effects on physical and mental health indicators.
The present review has several limitations. Likewise, as with most reviews, this review was based mainly on cross-sectional surveys; only four RCTs were included in the study. The RCTs also have some limitations due to the absence of double blinding. Perhaps including a sample that is not religious as a control group could exhibit a more significant association between religion and PA. Also, a longitudinal study could better recognize whether religiosity exerts an increase in PA. In addition, we selected and analyzed only studies in English that met our inclusion criteria and excluded other studies. We also observed the limited number of research studies in the literature focused closely on this topic and often a lack of demography, which is one of the factors considered by authors as potential confounders in the R/S and PA relation. Another limitation was the difficulty in conducting a meta-analysis to calculate the total magnitude of the R/S effect on PA components due to different study designs and methodologies of R/S measures, overlapping between their terms, and different methods of PA measurement. However, both systematic reviews and meta-analyses are affected by selective publishing of articles and reported studies bias, which can lead to the overestimation of the correlation between the considered variables.
Among the advantages of this review is an analysis of the current studies based on relatively large sample sizes and the provision of information on measuring R/S and PA/PE assessment using validated tools in most of the studies. Another strength of our article is the restriction of the effect of R/S on changes in PA practice and the presentation of the studies that focused on correlation between these terms and PA, as well as those reporting results of religious intervention programs developed to increase engagement in PA/PE. Regardless of the diversity in aims and objectives of the analyzed published studies and methodological diversity, we were able to present the beneficial impact of R and S on PA practice and to identify research gaps in this area.
5. Conclusions
This review summarizes and demonstrates the current research results on the correlation between the R and S variables and PA/PE practice. The review reports briefly the literature findings on the role of R and S beliefs and practices in physical, mental, social health, and psychosocial well-being. Evidence continues to support earlier findings that individuals who are more involved in R or S practice can experience benefits in physical and mental health and better coping, e.g., with cancer-specific distress, anxiety, and depression. The findings suggest that more outstanding religious commitment may be positively associated with increased PA. We found that religious practice, spirituality, or faith interventions generally significantly reduced sedentary behavior among church/mosque members and were positively correlated with PA components (increased frequency of exercise practice, longer timing of exercise, higher levels of activity, regardless of gender). However, we also observed no association between religious faith and PA or faith-based interventions’ possibility to increase moderate activity in participants meeting the PA guidelines. It should be underlined that the literature data in this field are yet scarce, as are the religious intervention programs. The current review discovers difficulties in quantitatively measuring the impact of the individual components of R and S in research on physical health. Therefore, the available evidence does not yet deliver recommendations for these variables’ use regarding PA practice. The methodological limitations, such as multicomponent R/S intervention, PA assessment, and a limited number of studies specifically focused on this association, are partially responsible for such a statement. Despite the limitations, our review demonstrates that R/S and faith-based interventions may be promising actions for motivation to undertake increased PA and positive behavioral change. Biological mechanisms operating between the R/S variables and PA practice require future studies to enhance the understanding of correlations. Considering the commonly known benefits of regular moderate to vigorous PA and the reported increases in activity in individuals more involved in R/S practice, we can suggest that an increase in PA/PE and sports practice may partially explain the role of R and S in the biological benefits. Because many questions linked to these possible associations exist, more research in this field is needed. New studies should have high quality and be well-designed, double-blinded RCTs and longitudinal observational studies with a larger sample size design. They should include members of different religious types, consider R/S variables and confounding factors increasing/decreasing the R/S and PA correlation effect size, and be based on proper validated measures of these variables.
Author Contributions
Conceptualization, J.K.; Methodology, J.K. and B.H.A.-E.; Formal analysis, J.K.; Investigation, J.K.; Writing—original draft, J.K.; Writing—review and editing, J.K. and B.H.A.-E. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data sharing is not applicable. Since this paper is a systematic review, no new data were generated. Thus, data sharing is not applicable to this article. Moreover, the data presented in this review were derived from the articles cited herein. Hence, the data are available in the respective journals indicated in the list of references.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Aggarwal, Shilpa, Judith Wright, Amy Morgan, George Patton, and Nicola Reavley. 2023. Religiosity and spirituality in the prevention and management of depression and anxiety in young people: A systematic review and meta-analysis. BMC Psychiatry 23: 729. [Google Scholar] [CrossRef]
- Ahrenfeldt, Linda J., Sören Möller, Niels C. Hvidt, and Rune Lindahl-Jacobsen. 2018. Religiousness and lifestyle among Europeans in SHARE. Public Health 165: 74–81. [Google Scholar] [CrossRef]
- Al Eid, Nawal A., Mohammed Mj Alqahtani, Khaldoun Marwa, Boshra A Arnout, Hajar S Alswailem, and Al Anoud Al Toaimi. 2020. Religiosity, psychological resilience, and mental health among breast cancer patients in Kingdom of Saudi Arabia. Breast Cancer: Basic and Clinical Research 14: 1178223420903054. [Google Scholar] [CrossRef]
- Almaraz, David, Jesús Saiz, Florentino Moreno Martín, Iván Sánchez-Iglesias, Antonio J. Molina, and Tamara L. Goldsby. 2022. What aspects of religion and spirituality affect the physical health of cancer patients? A systematic review. Healthcare 10: 1447. [Google Scholar] [CrossRef]
- Alves, Sabrina Alaíde Amorim, and Maryldes Lucena Bezerra de Oliveira. 2018. Sociocultural aspects of health and disease and their pragmatic impact. Journal of Human Growth and Development 28: 183–88. [Google Scholar] [CrossRef]
- Ansari, Serene, Erica G. Soltero, Elizabeth Lorenzo, and Rebecca E. Lee. 2017. The impact of religiosity on dietary habits and physical activity in minority women participating in the Health is Power (HIP) study. Preventive Medicine Reports 5: 210–13. [Google Scholar] [CrossRef]
- Arredondo, Elva M., John P. Elder, Jessica Haughton, Donald J. Slymen, James F. Sallis, Lilian G. Perez, Natalicio Serrano, Maíra T. Parra, Rodrigo Valdivia, and Guadalupe X. Ayala. 2017. Fe en Acción: Promoting physical activity among churchgoing Latinas. American Journal of Public Health 107: 1109–15. [Google Scholar] [CrossRef]
- Balish, Shea M., Dan Conacher, and Lori Dithurbide. 2016. Sport and Recreation Are Associated With Happiness Across Countries. Research Quarterly for Exercise and Sport 87: 382–88. [Google Scholar] [CrossRef]
- Basu-Zharku, Iulia O. 2011. The influence of religion on health. Inquiries Journal 3: 1–3. [Google Scholar]
- Bauman, Adrian E., Rodrigo S. Reis, James F. Sallis, Jonathan C. Wells, Ruth Jf Loos, and Brian W. Martin. 2012. Correlates of physical activity: Why are some people physically active and others not? The Lancet 380: 258–71. [Google Scholar] [CrossRef]
- Blankinship, Lisa A., William A. Rouse, Joshua Bernstein, Joanna Kruk, and Basil H. Aboul-Enein. 2021. A narrative review of ethnic minority studies for faith-based health promotion interventions with special reference to the contemporary Christian Nurse. Journal of Religion and Health 60: 1375–87. [Google Scholar] [CrossRef] [PubMed]
- Bopp, Melissa, Jane A. Peterson, and Benjamin L. Webb. 2012. A comprehensive review of faith-based physical activity interventions. American Journal of Lifestyle Medicine 6: 460–78. [Google Scholar] [CrossRef]
- Borges, Cezimar Correia, dos Patrícia Roberta Santos, Polissandro Mortoza Alves, Renata Custódio Maciel Borges, Giancarlo Lucchetti, Maria Alves Barbosa, Celmo Celeno Porto, and Marcos Rassi Fernandes. 2021. Association between spirituality/religiousness and quality of life among healthy adults: A systematic review. Health and Quality of Life Outcomes 19: 246. [Google Scholar] [CrossRef] [PubMed]
- Bull, Fiona C., Salih S. Al-Ansari, Stuart Biddle, Katja Borodulin, Matthew P Buman, Greet Cardon, Catherine Carty, Jean-Philippe Chaput, Sebastien Chastin, Roger Chou, and et al. 2020. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. British Journal of Sports Medicine 54: 1451–62. [Google Scholar] [CrossRef] [PubMed]
- Buro, Acadia W., Tiffany L. Carson, Brent J. Small, Wenyi Fan, Laura B. Oswald, Heather S. L. Jim, Endrina Salas, Kellie Zambrano, Crystal Bryant, Kosj Yamoah, and et al. 2023. Sociocultural factors associated with physical activity in Black prostate cancer survivors. Supportive Care in Cancer 31: 482. [Google Scholar] [CrossRef] [PubMed]
- Cerqueira, Érica, Daniel A. Marinho, Henrique P. Neiva, and Olga Lourenço. 2020. Inflammatory effects of high and moderate intensity exercise—A systematic review. Frontiers in Physiology 10: 1550. [Google Scholar] [CrossRef]
- Chen, Ying, Eric S. Kim, and Tyler J. VanderWeele. 2021. Religious-service attendance and subsequent health and well-being throughout adulthood: Evidence from three prospective cohorts. International Journal of Epidemiology 49: 2030–40. [Google Scholar] [CrossRef]
- de Diego-Cordero, Rocío, Paola Suárez-Reina, Bárbara Badanta, Giancarlo Lucchetti, and Juan Vega-Escaño. 2022. The efficacy of religious and spiritual interventions in nursing care to promote mental, physical and spiritual health: A systematic review and meta-analysis. Applied Nursing Research 67: 151618. [Google Scholar] [CrossRef] [PubMed]
- Doyle, David Matthew, and Bruce G. Link. 2024. On social health: History, conceptualization, and population patterning. Health Psychology Review 13: 1–30. [Google Scholar] [CrossRef]
- Duru, O. Kenrik, Catherine A. Sarkisian, Mei Leng, and Carol M. Mangione. 2010. Sisters in motion: A randomized controlled trial of a faith-based physical activity intervention. Journal of the American Geriatrics Society 58: 1863–69. [Google Scholar] [CrossRef]
- Ferreira, Laura Fernandes, Alyssa De Pinho Freire, Ana Luiza Cunha Silveira, Anthony Pereira Martins Silva, de Hermon Corrêa Sá, Igor Soares Souza, Lohane Stefany Araújo Garcia, Rafael Silva Peralta, and Laís Moreira Borges Araujo. 2020. The influence of spirituality and religiosity in acceptance of the disease and treatment of oncologic patients: An integrative literature review. Revista Brasileira de Cancerologia 66: e-07422. [Google Scholar] [CrossRef]
- Goerge, Ally, Maureen Sanderson, Cristen Flewellen, Katherine Busen, and Sarah Nechuta. 2023. The role of spirituality on physical activity and sleep among African American long-term breast cancer survivors. Journal of Racial and Ethnic Health Disparities, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Gonçalves, Juliane Piasseschi de Bernardin, Giancarlo Lucchetti, Paulo Rossi Menezes, and Homero Vallada. 2017. Complementary religious and spiritual interventions in physical health and quality of life: A systematic review of randomized controlled clinical trials. PLoS ONE 12: e0186539. [Google Scholar] [CrossRef] [PubMed]
- Gschwandtner, Christina M. 2021. Faith, religion, and spirituality: A phenomenological and hermeneutic contribution to parsing the distinctions. Religions 12: 476. [Google Scholar] [CrossRef]
- Hamdan, Abdullah Bany, Fawzi Al-Odeh, Sherwynn Javison, Abdullah AlSuheil, Sami Alshammary, and Musa AlHarbi. 2020. Religious belief and social support among cancer patients in Saudi Arabia. Cureus 12: e7012. [Google Scholar] [CrossRef] [PubMed]
- Hashemi, Seyed-Mehdi, Mohammadreza Hormozi, Abolghasem Allahyari, Ali Arash Anoushirvani, Zahra Ameri, and Samaneh Ghasemipour. 2020. The prevalence of depression, anxiety, and stress in patients with breast cancer in Southeast Iran in 2019: A cross-sectional study. Oncology in Clinical Practice 16: 104–8. [Google Scholar] [CrossRef]
- Helmerhorst, Hendrik Hendrik JF, Søren Brage, Janet Warren, Herve Besson, and Ulf Ekelund. 2012. A systematic review of reliability and objective criterion-related validity of physical activity questionnaires. International Journal of Behavioral Nutrition and Physical Activity 9: 103–3. [Google Scholar] [CrossRef] [PubMed]
- Hussain, Umer, and George B. Cunningham. 2023. Physical activity among Muslim women: The roles of religious identity, health consciousness, and Muslim population density. Cogent Social Sciences 9: 2244839. [Google Scholar] [CrossRef]
- Irwin, Melinda L. 2009. Physical activity interventions for cancer survivors. British Journal of Sports Medicine 43: 32–38. [Google Scholar] [CrossRef]
- Jim, Heather S. L., James E. Pustejovsky, Crystal L. Park, Suzanne C. Danhauer, Allen C. Sherman, George Fitchett, Thomas V. Merluzzi, Alexis R. Munoz, Login George, Mallory A. Snyder, and et al. 2015. Religion, spirituality, and physical health in cancer patients: A meta-analysis. Cancer 121: 3760–68. [Google Scholar] [CrossRef]
- Jona, I. N., and F. T. Okou. 2013. Sports and religion. Asian Journal of Management Sciences & Education 2: 46–54. [Google Scholar]
- Kang, Mina, La Young Park, Seo Young Kang, Jisun Lim, and Young Sik Kim. 2020. Religion and health behaviors in primary care patients. Korean Journal of Family Medicine 41: 105–10. [Google Scholar] [CrossRef]
- Koenig, Harold G. 2012. Religion, spirituality, and health: The research and clinical implications. ISRN Psychiatry 2012: 278730. [Google Scholar] [CrossRef]
- Koenig, Harold G., Tyler VanderWeele, and John R. Peteet. 2023. Handbook of Religion and Health, 3rd ed. New York: Oxford Academic. [Google Scholar] [CrossRef]
- Kopeyko, Grigory, Olga Alexandrovna Borisova, E. V. Gedevani, and Vasilii Glebovich Kaleda. 2020. Vliianie faktora religioznosti na depressivnye sostoianiia i suitsidal’noe povedenie [The influence of religiosity on depressive disorders and suicidal behavior]. S.S. Korsakov Journal of Neurology and Psychiatry 120: 103–10. [Google Scholar] [CrossRef]
- Kowalczyk, Oliwia, Krzysztof Roszkowski, Wojciech Pawliszak, Agnieszka Rypel, Szymon Roszkowski, Jolanta Kowalska, Bartosz Tylkowski, and Anna Bajek. 2022. Religion and spirituality in oncology: An exploratory study of the communication experiences of clinicians in Poland. Journal of Religion and Health 61: 1366–75. [Google Scholar] [CrossRef]
- Kruk, Joanna, Basil Hassan Aboul-Enein, Joshua Bernstein, and Magdalena Gronostaj. 2019a. Psychological stress and cellular aging in cancer: A meta-analysis. Oxidative Medicine and Cellular Longevity 2019: 1270397. [Google Scholar] [CrossRef]
- Kruk, Joanna, Hassan Y. Aboul-Enein, Aleksandra Kładna, E. Jacquelyn, and Jacquelyn E. Bowser. 2019b. Oxidative stress in biological systems and its relation with pathophysiological functions: The effect of physical activity on cellular redox homeostasis. Free Radical Research 53: 497–521. [Google Scholar] [CrossRef]
- Kvesić, Antonija, Dragan Babic, Darjan Franjic, Inga Marijanovic, Romana Babic, and Marko Martinac. 2020. Correlation of religiousness with the quality of life and psychological symptoms in oncology patients. Psychiatria Danubina 32 Suppl. S2: 254–61. [Google Scholar]
- Lee, Paul H., Duncan J. Macfarlane, TH Lam, and Sunita M. Stewart. 2011. Validity of the international physical activity questionnaire short form (IPAQ-SF): A systematic review. International Journal of Behavioral Nutrition and Physical Activity 8: 115–15. [Google Scholar] [CrossRef]
- Lucchetti, Giancarlo, Harold G. Koenig, and Alessandra Lamas Granero Lucchetti. 2021. Spirituality, religiousness, and mental health: A review of the current scientific evidence. World Journal of Clinical Cases 9: 7620–31. [Google Scholar] [CrossRef]
- Lumpkins, Crystal Y., K Allen Greiner, Christine Daley, Jannette Berkley-Patton, Jinxiang Hu, and Shana Palla. 2019. An exploratory analysis of the role of religion in colorectal cancer screening among safety-net clinic patients. Journal of Geriatric Medicine and Gerontology 5: 058. [Google Scholar] [CrossRef]
- Malm, Christer, Johan Jakobsson, and Andreas Isaksson. 2019. Physical Activity and Sports—Real Health Benefits: A Review with Insight into the Public Health of Sweden. Sports 7: 127. [Google Scholar] [CrossRef]
- Maroney, Kieran, Jodie Laurent, Flor Alvarado, Alexandra Gabor, Caryn Bell, Keith Ferdinand, Jiang He, and Katherine T. Mills. 2023. Systematic review and meta-analysis of church-based interventions to improve cardiovascular disease risk factors. The American Journal of the Medical Sciences 366: 199–208. [Google Scholar] [CrossRef]
- McManus, Deborah Tessitore. 2024. The intersection of spirituality, religiosity, and lifestyle practices in religious communities to successful aging: A review article. Religions 15: 478. [Google Scholar] [CrossRef]
- Moreira, Wanderson Carneiro, Maria Do Perpétuo Socorro de Sousa Nóbrega, Fernanda Púpio Silva Lima, Eliana Campêlo Lago, and Mário Oliveira Lima. 2020. Effects of the association between spirituality, religiosity and physical activity on health/mental health: A systematic review. Revista da Escola de Enfermagem da USP 54: e03631. [Google Scholar] [CrossRef] [PubMed]
- Neufer, P. Darrell, Marcas M. Bamman, Deborah M. Muoio, Claude Bouchard, Dan M. Cooper, Bret H. Goodpaster, Frank W. Booth, Wendy M. Kohrt, Robert E. Gerszten, Mark P. Mattson, and et al. 2015. Understanding the cellular and molecular mechanisms of physical activity-induced health benefits. Cell Metabolism 22: 4–11. [Google Scholar] [CrossRef] [PubMed]
- Noh, Young-Eun, and Syazana Shahdan. 2020. A systematic review of religion/spirituality and sport: A psychological perspective. Psychology of Sport and Exercise 46: 101603. [Google Scholar] [CrossRef]
- Noh, Young-Eun, Boon Hooi Lim, and Mahmoud Danaee. 2023. Motives for physical activity participation: Does religious faith play a mediating role? International Journal of Sport and Exercise Psychology 21: 787–806. [Google Scholar] [CrossRef]
- Odynets, Tetiana, Yuriy Briskin, Valentina Todorova, and Olha Bondarenko. 2019. Impact of different exercise interventions on anxiety and depression in breast cancer patients. Physiotherapy Quarterly 27: 31–36. [Google Scholar] [CrossRef]
- Parra, Maíra Tristão, Gustavo J. M. Porfírio, Elva M. Arredondo, and Álvaro N. Atallah. 2018. Physical activity interventions in faith-based organizations: A systematic review. American Journal of Health Promotion 32: 677–90. [Google Scholar] [CrossRef]
- Paul Victor, Chitra G., and Judith V. Treschuk. 2020. Critical Literature Review on the Definition Clarity of the Concept of Faith, Religion, and Spirituality. Journal of Holistic Nursing 38: 107–13. [Google Scholar] [CrossRef]
- Powell, Lynda H., Leila Shahabi, and Carl E. Thoresen. 2003. Religion and spirituality: Linkages to physical health. American Psychologist 58: 36–52. [Google Scholar] [CrossRef] [PubMed]
- Rassouli, Maryam, Vahid Zamanzadeh, Akram Ghahramanian, Abbas Abbaszadeh, Hamid Alavi-Majd, and Alireza Nikanfar. 2015. Experiences of patients with cancer and their nurses on the conditions of spiritual care and spiritual interventions in oncology units. Iranian Journal of Nursing and Midwifery Research 20: 25–33. [Google Scholar] [PubMed]
- Rathod, Kalwyna. 2021. What Are the Health-Skill Related Components of Physical Fitness. Available online: https://www.femina.in/wellness/fitness/components-of-physical-fitness-183555.html (accessed on 30 March 2024).
- Reisi, Sajjad, Seyed Mojtaba Ahmadi, and Kheirollah Sadeghi. 2021. The effect of religion and spirituality on anxiety and depression in cancer patients: A review article. Journal of Quran and Medicine 6: 75–86. [Google Scholar]
- Rizvi, Mohd Ahsan Kabir, and Mohammad Zakir Hossain. 2017. Relationship between religious belief and happiness: A systematic literature review. Journal of Religion and Health 56: 1561–82. [Google Scholar] [CrossRef]
- Salsman, John M., James E. Pustejovsky, Heather S. L. Jim, Alexis R. Munoz, Thomas V. Merluzzi, Login George, Crystal L. Park, Suzanne C. Danhauer, Allen C. Sherman, Mallory A. Snyder, and et al. 2015. A meta-analytic approach to examining the correlation between religion/spirituality and mental health in cancer. Cancer 121: 3769–78. [Google Scholar] [CrossRef]
- Saxena, S., M. Van Ommeren, K. C. Tang, and T. P. Armstrong. 2005. Mental health benefits of physical activity. Journal of Mental Health 14: 445–51. [Google Scholar] [CrossRef]
- Schlundt, David G., Monica D. Franklin, Kushal Patel, Linda McClellan, Celia Larson, Sarah Niebler, and Margaret Hargreaves. 2008. Religious affiliation, health behaviors and outcomes: Nashville REACH 2010. American Journal of Health Behavior 32: 714–24. [Google Scholar] [CrossRef] [PubMed]
- Seeman, Teresa E., Linda Fagan Dubin, and Melvin Seeman. 2003. Religiosity/spirituality and health: A critical review of the evidence for biological pathways. American Psychologist 58: 53–63. [Google Scholar] [CrossRef]
- Shattuck, Eric C., and Michael P. Muehlenbein. 2020. Religiosity/spirituality and physiological markers of health. Journal of Religion and Health 59: 1035–54. [Google Scholar] [CrossRef]
- Sherman, Allen C., Thomas V. Merluzzi, James E. Pustejovsky, Crystal L. Park, Login George, George Fitchett, Heather S. L. Jim, Alexis R. Munoz, Suzanne C. Danhauer, Mallory A. Snyder, and et al. 2015. A meta-analytic review of religious or spiritual involvement and social health among cancer patients. Cancer 121: 3779–88. [Google Scholar] [CrossRef]
- Shojaee, Mahnaz, and Carmel French. 2014. The relationship between mental health components and locus of control in youth. Psychology 5: 966–78. [Google Scholar] [CrossRef]
- Silfee, Valerie J., Christina F. Haughton, Stephenie C. Lemon, Vilma Lora, and Milagros C. Rosal. 2017. Spirituality and physical activity and sedentary behavior among Latino men and women in Massachusetts. Ethnicity & Disease 27: 3–10. [Google Scholar] [CrossRef]
- Silverman, Marni N., and Patricia A. Deuster. 2014. Biological mechanisms underlying the role of physical fitness in health and resilience. Interface Focus 4: 20140040. [Google Scholar] [CrossRef] [PubMed]
- Stehr, Paula, Hanna Luetke Lanfer, and Constanze Rossmann. 2021. Beliefs and motivation regarding physical activity among older adults in Germany: Results of a qualitative study. International Journal of Qualitative Studies on Health and Well-Being 16: 1932025. [Google Scholar] [CrossRef] [PubMed]
- Stelmach, Marian. 2018. Physical activity assessment tools in monitoring physical activity: The Global Physical Activity Questionnaire (GPAQ), the International Physical Activity Questionnaire (IPAQ) or accelerometers—Choosing the best tools. Health Problems of Civilization 12: 57–63. [Google Scholar] [CrossRef]
- Sun, Hengwen, Yuan Yang, Jingying Zhang, Ting Liu, Hongmei Wang, Samradhvi Garg, and Bin Zhang. 2019. Fear of cancer recurrence, anxiety and depressive symptoms in adolescent and young adult cancer patients. Neuropsychiatric Disease and Treatment 15: 857–65. [Google Scholar] [CrossRef] [PubMed]
- Svensson, Nanna Herning, Niels Christian Hvidt, Susanne Pagh Nissen, Maria Munch Storsveen, Elisabeth Assing Hvidt, Jens Søndergaard, and Trine Thilsing. 2020. Religiosity and health-related risk behaviours in a secular culture—Is there a correlation? Journal of Religion and Health 59: 2381–96. [Google Scholar] [CrossRef] [PubMed]
- Tejero-González, Carlos M. 2020. Participating in sports and practicing a religion are related to levels of happiness. Physical Culture and Sport. Studies and Research 88: 11–17. [Google Scholar] [CrossRef]
- VanderWeele, Tyler J. 2017. Physical activity and physical and mental well-being in church settings. American Journal of Public Health 107: 1023–24. [Google Scholar] [CrossRef] [PubMed]
- Vitorino, Luciano Magalhães, Giancarlo Lucchetti, Frederico Camelo Leão, Homero Vallada, and Mario Fernando Prieto Peres. 2018. The association between spirituality and religiousness and mental health. Scientific Reports 8: 17233. [Google Scholar] [CrossRef]
- Wankel, Leonard M., and Bonnie G. Berger. 1990. The psychological and social benefits of sport and physical activity. Journal of Leisure Research 22: 167–82. [Google Scholar] [CrossRef]
- Warburton, Darren E.R., Crystal Whitney Nicol, and Shannon S.D. Bredin. 2006. Health benefits of physical activity: The evidence. CMAJ: Canadian Medical Association Journal 174: 801–9. [Google Scholar] [CrossRef] [PubMed]
- Waters, Edward K., Zelda Doyle, and Ellen Finlay. 2018. Spirituality/Religiosity (SpR), leisure-time physical activity, and sedentary behaviour in students at a Catholic University. Journal of Religion and Health 57: 869–82. [Google Scholar] [CrossRef] [PubMed]
- Whitt-Glover, Melicia C., Moses V. Goldmon, Ziya Gizlice, Marie Sillice, Lyndsey Hornbuckle, and Daniel P. Heil. 2017. Increasing physical activity in black women: Results from a randomized trial conducted in faith-based settings. Ethnicity & Disease 27: 411–20. [Google Scholar] [CrossRef]
- Wilcox, Sara, Ruth P. Saunders, Andrew T. Kaczynski, Melinda Forthofer, Patricia A. Sharpe, Cheryl Goodwin, Margaret Condrasky, Vernon L. Kennedy, Danielle E. Jake-Schoffman, Deborah Kinnard, and et al. 2018. Faith, activity, and nutrition randomized dissemination and implementation study: Countywide adoption, reach, and effectiveness. American Journal of Preventive Medicine 54: 776–85. [Google Scholar] [CrossRef] [PubMed]
- Yan, Bo, Xinyi Xu, Denise Shuk Ting Cheung, and Chia-Chin Lin. 2020. Spiritual and religious interventions for adults with cancer and their carers: An overview of systematic reviews. Cochrane Database of Systematic Reviews 2020: CD013675. [Google Scholar] [CrossRef]
- You, Tongjian, Nicole C. Arsenis, Beth L. Disanzo, and Michael J. LaMonte. 2013. Effects of exercise training on chronic inflammation in obesity. Sports Medicine 43: 243–56. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).