What Is the Ideal Blood Pressure Threshold for the Prevention of Atrial Fibrillation in Elderly General Population?
Abstract
1. Introduction
2. Experimental Section
2.1. BP Measurement
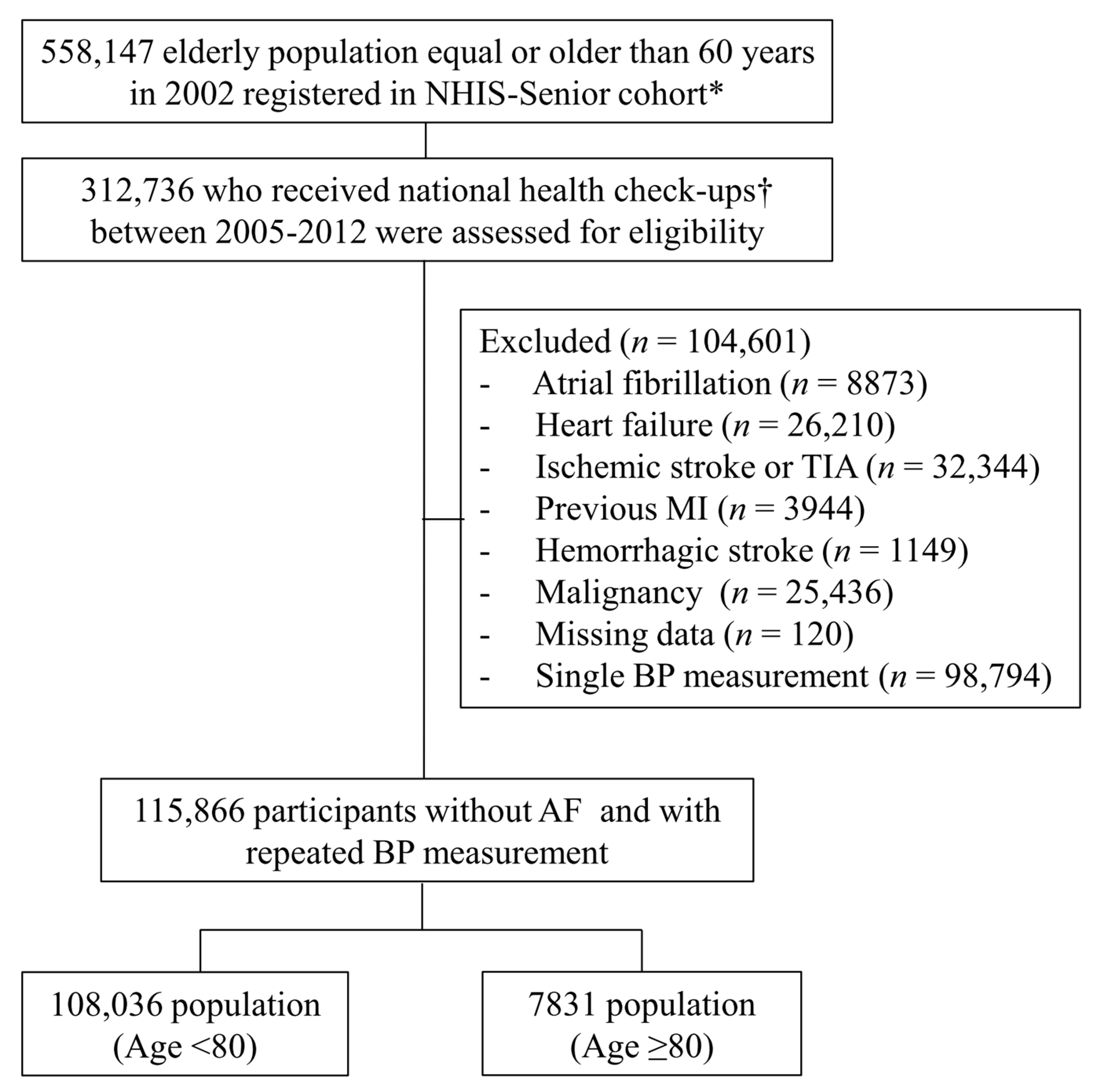
2.2. Study Population
2.3. Covariates
2.4. Hypertension and Atrial Fibrillation
2.5. Statistical Analysis
3. Results
3.1. Baseline Characteristics
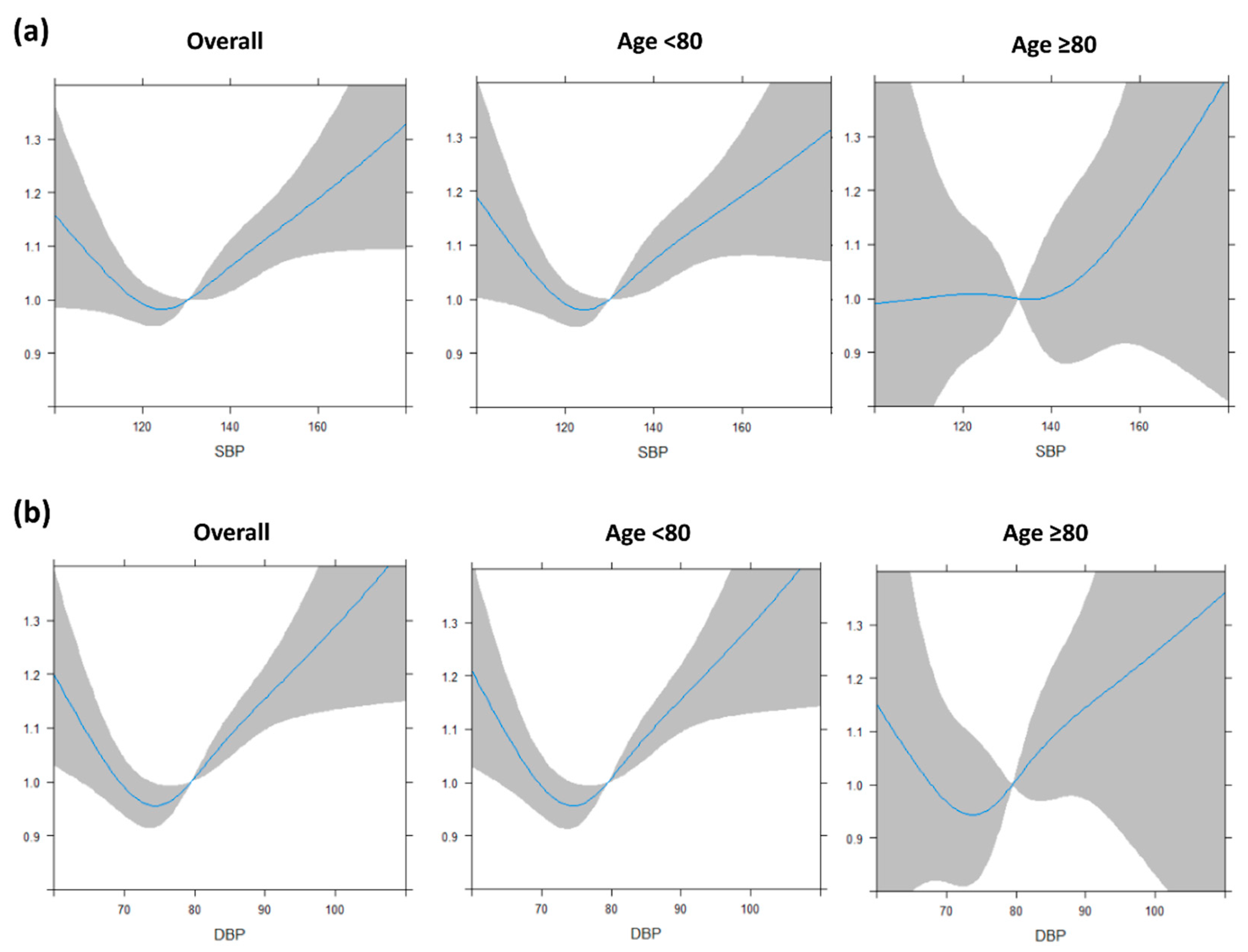
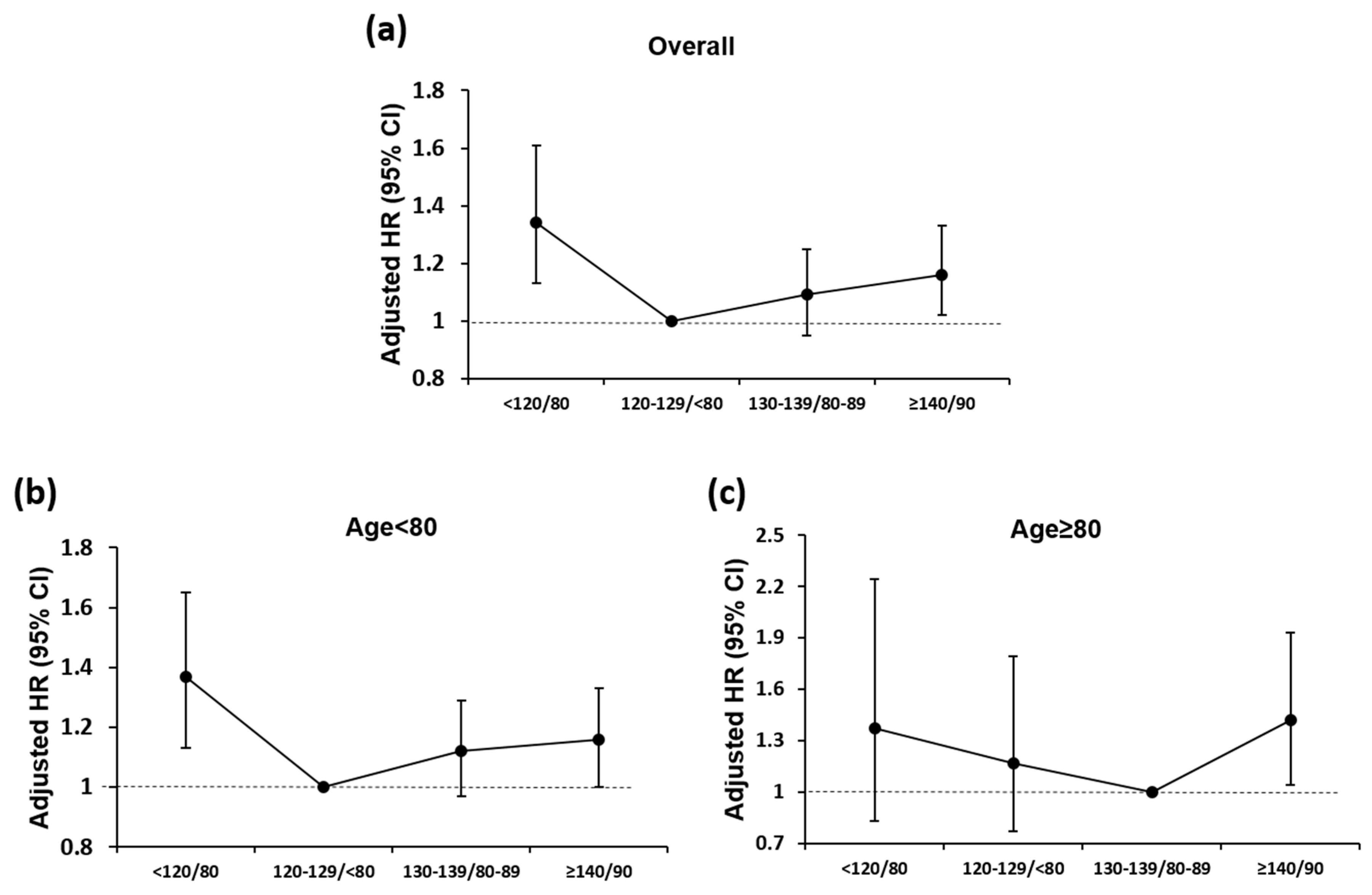
3.2. BP and Incident AF in Different Age Groups
3.3. BP and Incident AF in Patients with Treated Hypertension
3.4. Serious Adverse Events according to BP Status in Different Age Groups
4. Discussion
4.1. Optimal BP Levels and Incident AF in Octogenarians
4.2. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Kearney, P.M.; Whelton, M.; Reynolds, K.; Muntner, P.; Whelton, P.K.; He, J. Global burden of hypertension: Analysis of worldwide data. Lancet 2005, 365, 217–223. [Google Scholar] [CrossRef]
- Huxley, R.R.; Lopez, F.L.; Folsom, A.R.; Agarwal, S.K.; Loehr, L.R.; Soliman, E.Z.; Maclehose, R.; Konety, S.; Alonso, A. Absolute and attributable risks of atrial fibrillation in relation to optimal and borderline risk factors: The Atherosclerosis Risk in Communities (ARIC) study. Circulation 2011, 123, 1501–1508. [Google Scholar] [CrossRef] [PubMed]
- Emdin, C.A.; Anderson, S.G.; Salimi-Khorshidi, G.; Woodward, M.; MacMahon, S.; Dwyer, T.; Rahimi, K. Usual blood pressure, atrial fibrillation and vascular risk: Evidence from 4.3 million adults. Int. J. Epidemiol. 2017, 46, 162–172. [Google Scholar] [CrossRef]
- Dzeshka, M.S.; Shantsila, A.; Shantsila, E.; Lip, G.Y.H. Atrial Fibrillation and Hypertension. Hypertension 2017, 70, 854–861. [Google Scholar] [CrossRef] [PubMed]
- Gumprecht, J.; Domek, M.; Lip, G.Y.H.; Shantsila, A. Invited review: Hypertension and atrial fibrillation: Epidemiology, pathophysiology, and implications for management. J. Hum. Hypertens. 2019, 33, 824–836. [Google Scholar] [CrossRef] [PubMed]
- Lip, G.Y.H.; Coca, A.; Kahan, T.; Boriani, G.; Manolis, A.S.; Olsen, M.H.; Oto, A.; Potpara, T.S.; Steffel, J.; Marin, F.; et al. Hypertension and cardiac arrhythmias: A consensus document from the European Heart Rhythm Association (EHRA) and ESC Council on Hypertension, endorsed by the Heart Rhythm Society (HRS), Asia-Pacific Heart Rhythm Society (APHRS) and Sociedad Latinoamericana de Estimulacion Cardiaca y Electrofisiologia (SOLEACE). Europace 2017, 19, 891–911. [Google Scholar] [CrossRef] [PubMed]
- O’Neal, W.T.; Soliman, E.Z.; Qureshi, W.; Alonso, A.; Heckbert, S.R.; Herrington, D. Sustained pre-hypertensive blood pressure and incident atrial fibrillation: The Multi-Ethnic Study of Atherosclerosis. J. Am. Soc Hypertens. 2015, 9, 191–196. [Google Scholar] [CrossRef]
- Conen, D.; Tedrow, U.B.; Koplan, B.A.; Glynn, R.J.; Buring, J.E.; Albert, C.M. Influence of systolic and diastolic blood pressure on the risk of incident atrial fibrillation in women. Circulation 2009, 119, 2146–2152. [Google Scholar] [CrossRef]
- Grundvold, I.; Skretteberg, P.T.; Liestol, K.; Erikssen, G.; Kjeldsen, S.E.; Arnesen, H.; Erikssen, J.; Bodegard, J. Upper normal blood pressures predict incident atrial fibrillation in healthy middle-aged men: A 35-year follow-up study. Hypertension 2012, 59, 198–204. [Google Scholar] [CrossRef]
- Thomas, M.C.; Dublin, S.; Kaplan, R.C.; Glazer, N.L.; Lumley, T.; Longstreth, W.T., Jr.; Smith, N.L.; Psaty, B.M.; Siscovick, D.S.; Heckbert, S.R. Blood pressure control and risk of incident atrial fibrillation. Am. J. Hypertens. 2008, 21, 1111–1116. [Google Scholar] [CrossRef]
- Verdecchia, P.; Staessen, J.A.; Angeli, F.; de Simone, G.; Achilli, A.; Ganau, A.; Mureddu, G.; Pede, S.; Maggioni, A.P.; Lucci, D.; et al. Usual versus tight control of systolic blood pressure in non-diabetic patients with hypertension (Cardio-Sis): An open-label randomised trial. Lancet 2009, 374, 525–533. [Google Scholar] [CrossRef]
- Chen, L.Y.; Bigger, J.T.; Hickey, K.T.; Chen, H.; Lopez-Jimenez, C.; Banerji, M.A.; Evans, G.; Fleg, J.L.; Papademetriou, V.; Thomas, A.; et al. Effect of Intensive Blood Pressure Lowering on Incident Atrial Fibrillation and P-Wave Indices in the ACCORD Blood Pressure Trial. Am. J. Hypertens. 2016, 29, 1276–1282. [Google Scholar] [CrossRef] [PubMed]
- Soliman, E.Z.; Rahman, A.F.; Zhang, Z.M.; Rodriguez, C.J.; Chang, T.I.; Bates, J.T.; Ghazi, L.; Blackshear, J.L.; Chonchol, M.; Fine, L.J.; et al. Effect of Intensive Blood Pressure Lowering on the Risk of Atrial Fibrillation. Hypertension 2020, 75, 1491–1496. [Google Scholar] [CrossRef] [PubMed]
- Group, S.R.; Wright, J.T., Jr.; Williamson, J.D.; Whelton, P.K.; Snyder, J.K.; Sink, K.M.; Rocco, M.V.; Reboussin, D.M.; Rahman, M.; Oparil, S.; et al. A Randomized Trial of Intensive versus Standard Blood-Pressure Control. N. Engl. J. Med. 2015, 373, 2103–2116. [Google Scholar] [CrossRef]
- Williams, B.; Mancia, G.; Spiering, W.; Agabiti Rosei, E.; Azizi, M.; Burnier, M.; Clement, D.L.; Coca, A.; de Simone, G.; Dominiczak, A.; et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur. Heart J. 2018, 39, 3021–3104. [Google Scholar] [CrossRef]
- Kjeldsen, S.E.; Stenehjem, A.; Os, I.; Van de Borne, P.; Burnier, M.; Narkiewicz, K.; Redon, J.; Agabiti Rosei, E.; Mancia, G. Treatment of high blood pressure in elderly and octogenarians: European Society of Hypertension statement on blood pressure targets. Blood Press. 2016, 25, 333–336. [Google Scholar] [CrossRef]
- Phillips, R.A.; Xu, J.; Peterson, L.E.; Arnold, R.M.; Diamond, J.A.; Schussheim, A.E. Impact of Cardiovascular Risk on the Relative Benefit and Harm of Intensive Treatment of Hypertension. J. Am. Coll. Cardiol. 2018, 71, 1601–1610. [Google Scholar] [CrossRef]
- Lee, J.H.; Choi, J.K.; Jeong, S.N.; Choi, S.H. Charlson comorbidity index as a predictor of periodontal disease in elderly participants. J. Periodontal Implant. Sci. 2018, 48, 92–102. [Google Scholar] [CrossRef]
- Lee, S.S.; Ae Kong, K.; Kim, D.; Lim, Y.M.; Yang, P.S.; Yi, J.E.; Kim, M.; Kwon, K.; Bum Pyun, W.; Joung, B.; et al. Clinical implication of an impaired fasting glucose and prehypertension related to new onset atrial fibrillation in a healthy Asian population without underlying disease: A nationwide cohort study in Korea. Eur. Heart J. 2017, 38, 2599–2607. [Google Scholar] [CrossRef]
- Kim, D.; Yang, P.S.; Jang, E.; Yu, H.T.; Kim, T.H.; Uhm, J.S.; Kim, J.Y.; Pak, H.N.; Lee, M.H.; Joung, B.; et al. Increasing trends in hospital care burden of atrial fibrillation in Korea, 2006 through 2015. Heart 2018, 104, 2010–2017. [Google Scholar] [CrossRef]
- Lee, H.Y.; Yang, P.S.; Kim, T.H.; Uhm, J.S.; Pak, H.N.; Lee, M.H.; Joung, B. Atrial fibrillation and the risk of myocardial infarction: A nation-wide propensity-matched study. Sci. Rep. 2017, 7, 12716. [Google Scholar] [CrossRef] [PubMed]
- Verdecchia, P.; Angeli, F.; Reboldi, G. Hypertension and Atrial Fibrillation: Doubts and Certainties From Basic and Clinical Studies. Circ. Res. 2018, 122, 352–368. [Google Scholar] [CrossRef] [PubMed]
- Dzeshka, M.S.; Shahid, F.; Shantsila, A.; Lip, G.Y.H. Hypertension and Atrial Fibrillation: An Intimate Association of Epidemiology, Pathophysiology, and Outcomes. Am. J. Hypertens. 2017, 30, 733–755. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.; Yang, P.S.; Yu, H.T.; Kim, T.H.; Jang, E.; Sung, J.H.; Pak, H.N.; Lee, M.Y.; Lee, M.H.; Lip, G.Y.H.; et al. Risk of dementia in stroke-free patients diagnosed with atrial fibrillation: Data from a population-based cohort. Eur. Heart. J. 2019, 40, 2313–2323. [Google Scholar] [CrossRef]
- Kim, T.H.; Yang, P.S.; Uhm, J.S.; Kim, J.Y.; Pak, H.N.; Lee, M.H.; Joung, B.; Lip, G.Y.H. CHA2DS2-VASc Score (Congestive Heart Failure, Hypertension, Age >/=75 [Doubled], Diabetes Mellitus, Prior Stroke or Transient Ischemic Attack [Doubled], Vascular Disease, Age 65-74, Female) for Stroke in Asian Patients With Atrial Fibrillation: A Korean Nationwide Sample Cohort Study. Stroke 2017, 48, 1524–1530. [Google Scholar] [CrossRef]
- Lee, H.; Kim, T.H.; Baek, Y.S.; Uhm, J.S.; Pak, H.N.; Lee, M.H.; Joung, B. The Trends of Atrial Fibrillation-Related Hospital Visit and Cost, Treatment Pattern and Mortality in Korea: 10-Year Nationwide Sample Cohort Data. Korean Circ. J. 2017, 47, 56–64. [Google Scholar] [CrossRef]
- Baek, Y.S.; Yang, P.S.; Kim, T.H.; Uhm, J.S.; Park, J.; Pak, H.N.; Lee, M.H.; Joung, B. Associations of Abdominal Obesity and New-Onset Atrial Fibrillation in the General Population. J. Am. Heart Assoc. 2017, 6, e004705. [Google Scholar] [CrossRef]
- Song, S.; Yang, P.S.; Kim, T.H.; Uhm, J.S.; Pak, H.N.; Lee, M.H.; Joung, B. Relation of Chronic Obstructive Pulmonary Disease to Cardiovascular Disease in the General Population. Am. J. Cardiol. 2017, 120, 1399–1404. [Google Scholar] [CrossRef]


| All Population (N = 115,866) | Age | |||
|---|---|---|---|---|
| Age < 80 (n = 108,035) | Age ≥ 80 (n = 7831) | p-Value | ||
| Age, years | 71.7 (69.5–74.6) | 71.2 (69.3–74.0) | 82.2 (81.0–84.5) | <0.001 |
| Male | 53,609 (46.3) | 50,391 (46.6) | 3218 (41.1) | <0.001 |
| Systolic BP | 130.5 (122.5–140.0) | 130.0 (122.5–140.0) | 132.5 (124.5–142.5) | <0.001 |
| Diastolic BP * | 79.5 (74.0–85.0) | 79.5 (74.0–85.0) | 79.5 (73.5–85.0) | 0.017 |
| Economic state * | 7.0 (4.0–9.0) | 7.0 (4.0–9.0) | 7.0 (3.0–9.0) | 0.001 |
| Alcohol | <0.001 | |||
| No drinking | 64,681 (80.9) | 60,075 (80.6) | 4606 (85.8) | |
| Moderate drinking | 5982 (7.5) | 5673 (7.6) | 309 (5.8) | |
| Heavy drinking † | 9243 (11.6) | 8789 (11.8) | 454 (8.5) | |
| Smoking | <0.001 | |||
| Non-smoker or quit ≥12 months | 63,389 (79.3) | 58,993 (79.1) | 4396 (81.9) | |
| Quit <12 months | 5732 (7.2) | 5351 (7.2) | 381 (7.1) | |
| Current smoker | 10,785 (13.5) | 10,193 (13.7) | 592 (11.0) | |
| Comorbidities | ||||
| Hypertension | 46,519 (40.1) | 42,883 (39.7) | 3636 (46.4) | <0.001 |
| Diabetes | 14,767 (12.7) | 13,881 (12.8) | 886 (11.3) | <0.001 |
| Dyslipidemia | 34,200 (29.5) | 32,369 (30.0) | 1831 (23.4) | <0.001 |
| Chronic kidney disease | 997 (0.9) | 913 (0.8) | 84 (1.1) | 0.041 |
| Anemia | 17,715 (15.3) | 15,715 (14.6) | 2000 (25.6) | <0.001 |
| Hyperthyroidism | 2462 (2.1) | 2341 (2.2) | 121 (1.5) | <0.001 |
| Hypothyroidism | 2725 (2.4) | 2583 (2.4) | 142 (1.8) | 0.001 |
| COPD | 6960 (6.0) | 6262 (5.8) | 698 (8.9) | <0.001 |
| Liver disease | 23,559 (20.3) | 22,335 (20.7) | 1224 (15.6) | <0.001 |
| HCMP | 156 (0.1) | 149 (0.1) | 7 (0.1) | 0.331 |
| Osteoporosis | 33,139 (28.6) | 30,569 (28.3) | 2570 (32.8) | <0.001 |
| Medications | ||||
| Aspirin | 19,315 (16.7) | 17,957 (16.6) | 1358 (17.3) | 0.102 |
| P2Y12 inhibitor | 872 (0.8) | 816 (0.8) | 56 (0.7) | 0.742 |
| ACE-inhibitor/ARB | 18,425 (15.9) | 17,110 (15.8) | 1315 (16.8) | 0.027 |
| Beta blocker | 18,115 (15.6) | 16,815 (15.6) | 1300 (16.6) | 0.015 |
| Calcium channel blocker | 30,370 (26.2) | 27,945 (25.9) | 2425 (31.0) | <0.001 |
| Statin | 11,918 (10.3) | 11,333 (10.5) | 585 (7.5) | <0.001 |
| Diuretics | 23,665 (20.4) | 21,728 (20.1) | 1937 (24.7) | <0.001 |
| MRA | 1677 (1.4) | 1533 (1.4) | 144 (1.8) | 0.003 |
| All Population | Age < 80 Years | Age ≥ 80 Years | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Group | No. /Total No. 4393 /115,866 | Incidence Rate per 1000 Person-Years (95 CI) | Hazard Ratio (95 CI) | No. /Total No. 3946 /108,035 | Incidence Rate Per 1000 Person-Years (95 CI) | Hazard Ratio (95 CI) | No. /Total No. 447 /7831 | Incidence Rate Per 1000 Person-Years (95 CI) | Hazard Ratio (95 CI) |
| <120 /<80 | 713 /19,712 | 5.47 (5.07–5.88) | 1.15 (1.03–1.27) | 649 /18,556 | 5.24 (4.84–5.66) | 1.15 (1.03–1.28) | 64 /1156 | 9.78 (7.53–12.49) | 1.22 (0.90–1.64) |
| 120–129 /<80 | 721 /21,463 | 5.13 (4.76–5.52) | 1 (reference) | 647 /20,104 | 4.88 (4.51–5.27) | 1 (reference) | 74 /1359 | 9.37 (7.35–11.76) | 1.13 (0.85–1.50) |
| 130–139 /80–89 | 1526 /40,667 | 5.67 (5.39–5.96) | 1.08 (0.99–1.18) | 1386 /37,949 | 5.47 (5.19–5.77) | 1.10 (1.00–1.21) | 140 /2718 | 8.65 (7.28–10.21) | 1 (reference) |
| ≥140 /≥90 | 1433 /34,024 | 6.28 (5.96–6.62) | 1.15 (1.05–1.26) | 1264 /31,426 | 5.95 (5.63–6.29) | 1.14 (1.04–1.26) | 169 /2598 | 10.76 (9.20–12.52) | 1.26 (1.01–1.58) |
| All Population | Age <80 Years | Age ≥ 80 Years | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Group | No./ Total No. 2069 /46,519 | Incidence Rate per 1000 Person-Years (95 CI) | Hazard Ratio (95 CI) | No./ Total No. 1846 /42,883 | Incidence Rate per 1000 Person-Years (95 CI) | Hazard Ratio (95 CI) | No./ Total No. 223 /3636 | Incidence Rate Per 1000 Person-Years (95 CI) | Hazard Ratio (95 CI) |
| Intensive control (<120/80) | 210 /4159 | 8.22 (7.14–9.41) | 1.34 (1.13–1.61) | 189 /3814 | 7.96 (6.87–9.18) | 1.37 (1.13–1.65) | 21 /345 | 11.56 (7.16–17.67) | 1.37 (0.83–2.24) |
| Optimal control (120–129 /<80) | 290 /7466 | 6.22 (5.52–6.97) | 1 (reference) | 257 /6893 | 5.91 (5.21–6.68) | 1 (reference) | 33 /573 | 10.36 (7.13–14.55) | 1.17 (0.77–1.79) |
| Suboptimal control (130–139 /80–89) | 735 /17,268 | 6.66 (6.19–7.16) | 1.09 (0.95–1.25) | 667 /15,934 | 6.49 (6.01–7.01) | 1.12 (0.97–1.29) | 68 /1334 | 8.90 (6.91–11.29) | 1 (reference) |
| Poor control (≥140/90) | 834 /17,626 | 7.22 (6.74–7.73) | 1.16 (1.02–1.33) | 733 /16,242 | 6.83 (6.34–7.34) | 1.16 (1.00–1.33) | 101 /1384 | 12.46 (10.15–15.14) | 1.42 (1.04–1.93) |
| Blood Pressure Status | |||||
|---|---|---|---|---|---|
| <120/80 mmHg | 120–129/<80 mmHg | 130–139/80–89 mmHg | ≥140/90 mmHg | ||
| Overall | No. of total | 4159 | 7466 | 17,268 | 17,626 |
| Composite event | No. of events, HR (95 CI) | 341 1.08 (0.94–1.23) | 580 1 (reference) | 1269 0.95 (0.86–1.04) | 1437 1.01 (0.92–1.11) |
| Hypotension requiring hospitalization | No. of events, HR (95 CI) | 95, 1.15 (0.89–1.48) | 151, 1 (reference) | 348, 0.99 (0.82–1.20) | 366, 0.98 (0.81–1.19) |
| Syncope | No. of events HR (95 CI) | 33, 1.08 (0.70–1.67) | 55, 1 (reference) | 155, 1.23 (0.90–1.67) | 157, 1.18 (0.86–1.60) |
| Bradycardia | No. of events HR (95 CI) | 22 0.99 (0.59–1.67) | 41 1 (reference) | 96 1.01 (0.70–1.45) | 97 0.96 (0.67–1.39) |
| Electrolyte abnormality | No. of events HR (95 CI) | 142 0.99 (0.80–1.21) | 263 1 (reference) | 523 0.86 (0.75–1.00) | 646 1.01 (0.88–1.17) |
| Injurious falls | No. of events HR (95 CI) | 11 1.11 (0.52–2.37) | 17 1 (reference) | 46 1.18 (0.67–2.06) | 41 0.97 (0.55–1.71) |
| Acute kidney injury | No. of events HR (95 CI) | 106 1.18 (0.93–1.50) | 172 1 (reference) | 364 0.90 (0.75–1.08) | 433 0.96 (0.80–1.14) |
| Age < 80 Years | No. of total | 3814 | 6893 | 15,934 | 16,242 |
| Composite event | No. of events HR (95 CI) | 298 1.08 (0.94–1.25) | 506 1 (reference) | 1124 0.96 (0.87–1.07) | 1279 1.03 (0.93–1.15) |
| Hypotension requiring hospitalization | No. of events HR (95 CI) | 80 1.13 (0.85–1.49) | 129 1 (reference) | 313 1.05 (0.85–1.28) | 327 1.03 (0.84–1.27) |
| Syncope | No. of events HR (95 CI) | 31 1.28 (0.81–2.02) | 44 1 (reference) | 141 1.39 (0.99–1.96) | 143 1.33 (0.95–1.87) |
| Bradycardia | No. of events HR (95 CI) | 18 0.88 (0.50–1.55) | 38 1 (reference) | 91 1.03 (0.71–1.51) | 87 0.9. (0.63–1.36) |
| Electrolyte abnormality | No. of events HR (95 CI) | 122 0.98 (0.79–1.22) | 228 1 (reference) | 453 0.87 (0.74–1.02) | 573 1.04 (0.8–1.22) |
| Injurious falls | No. of events HR (95 CI) | 10 1.02 (0.45–2.24) | 17 1 (reference) | 40 1.04 (0.59–1.84) | 38 0.91 (0.51–1.61) |
| Acute kidney injury | No. of events HR (95 CI) | 96 1.25 (0.96–1.61) | 148 1 (reference) | 317 0.91 (0.75–1.11) | 378 0.98 (0.81–1.18) |
| Age ≥ 80 Years | No of total | 345 | 573 | 1334 | 1384 |
| Composite event | No. of events HR (95 CI) | 43 1.32 (0.94–1.86) | 74 1.25 (0.94–1.66) | 145 1 (reference) | 158 1.03 (0.82–1.29) |
| Hypotension requiring hospitalization | No. of events HR (95 CI) | 15 2.06 (1.12–3.81) | 22 1.64 (0.96–2.81) | 35 1 (reference) | 39 1.08 (0.68–1.72) |
| Syncope | No. of events HR (95 CI) | 2 0.57 (0.13–2.51) | 11 1.69 (0.74–3.85) | 14 1 (reference) | 14 1.69 (0.74–3.85) |
| Bradycardia | No. of events HR (95 CI) | 4 3.73 (0.97–14.32) | 3 0.98 (0.19–5.14) | 5 1 (reference) | 10 2.02 (0.68–6.01) |
| Electrolyte abnormality | No. of events HR (95 CI) | 20 1.21 (0.73–1.99) | 35 1.18 (0.78–1.79) | 70 1 (reference) | 73 0.98 (0.70–1.36) |
| Injurious falls | No. of events HR (95 CI) | 1 0.75 (0.09–5.90) | 0 | 6 1 (reference) | 3 0.44 (0.11–1.72) |
| Acute kidney Injury | No. of events HR (95 CI) | 10 1.06 (0.53–2.11) | 24 1.27 (0.77–2.11) | 47 1 (reference) | 55 1.02 (0.69–1.52) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, Y.J.; Yang, P.-S.; Yu, H.T.; Kim, T.-H.; Jang, E.; Uhm, J.-S.; Pak, H.-N.; Lee, M.-H.; Lip, G.Y.H.; Joung, B. What Is the Ideal Blood Pressure Threshold for the Prevention of Atrial Fibrillation in Elderly General Population? J. Clin. Med. 2020, 9, 2988. https://doi.org/10.3390/jcm9092988
Park YJ, Yang P-S, Yu HT, Kim T-H, Jang E, Uhm J-S, Pak H-N, Lee M-H, Lip GYH, Joung B. What Is the Ideal Blood Pressure Threshold for the Prevention of Atrial Fibrillation in Elderly General Population? Journal of Clinical Medicine. 2020; 9(9):2988. https://doi.org/10.3390/jcm9092988
Chicago/Turabian StylePark, Yoon Jung, Pil-Sung Yang, Hee Tae Yu, Tae-Hoon Kim, Eunsun Jang, Jae-Sun Uhm, Hui-Nam Pak, Moon-Hyoung Lee, Gregory Y.H. Lip, and Boyoung Joung. 2020. "What Is the Ideal Blood Pressure Threshold for the Prevention of Atrial Fibrillation in Elderly General Population?" Journal of Clinical Medicine 9, no. 9: 2988. https://doi.org/10.3390/jcm9092988
APA StylePark, Y. J., Yang, P.-S., Yu, H. T., Kim, T.-H., Jang, E., Uhm, J.-S., Pak, H.-N., Lee, M.-H., Lip, G. Y. H., & Joung, B. (2020). What Is the Ideal Blood Pressure Threshold for the Prevention of Atrial Fibrillation in Elderly General Population? Journal of Clinical Medicine, 9(9), 2988. https://doi.org/10.3390/jcm9092988






