A Systematic Review of COVID-19 Infection in Kidney Transplant Recipients: A Universal Effort to Preserve Patients’ Lives and Allografts
Abstract
:1. Introduction
2. Materials and Methods
2.1. Search Strategy
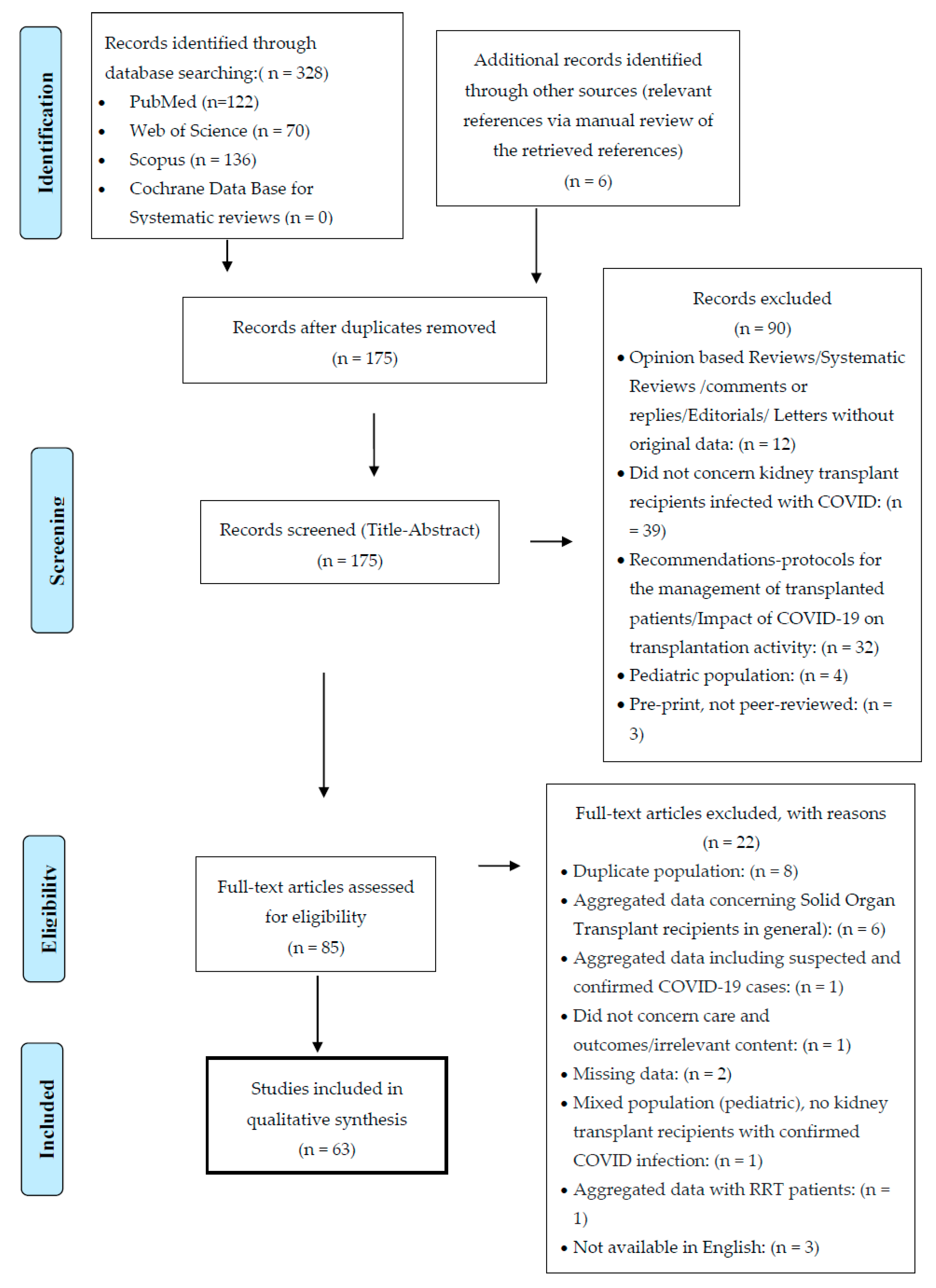
2.2. Study Selection
2.3. Data Extraction
2.4. Statistical Analysis
3. Results
3.1. Overview of Studies
3.2. Demographic and Baseline Characteristics, Clinical Outcomes, and Treatment of Kidney Transplant Recipients with COVID-19 Infection
3.2.1. Patients’ Demographics and Baseline Characteristics
3.2.2. Major Clinical Outcomes after COVID-19 Infection
3.2.3. Baseline Immunosuppression and Modifications during COVID-19 Infection
3.2.4. COVID-19-Targeted Therapies
3.3. Subgroup Analysis
4. Discussion
4.1. Infection Rates
4.2. Clinical Presentation
4.3. Disease Course
4.4. Disease Severity
4.5. Baseline Status of Kidney Transplant Recipients
4.6. Comorbidities
4.7. Major Outcomes
4.8. Modifications in Immunosuppression
4.9. COVID-Targeted Therapies
4.10. Subgroup Analysis
4.11. Limitations and Need for Future Research
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Sun, P.; Lu, X.; Xu, C.; Sun, W.; Pan, B. Understanding of COVID-19 based on current evidence. J. Med. Virol. 2020, 92, 548–551. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. People with Underlying Medical Conditions, Immunocompromised State (Weakened Immune System) from Solid Organ Transplant. 2020. Available online: https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html#immunocompromised-state (accessed on 30 July 2020).
- Akalin, E.; Azzi, Y.; Bartash, R.; Seethamraju, H.; Parides, M.; Hemmige, V.; Ross, M.; Forest, S.; Goldstein, Y.D.; Ajaimy, M.; et al. Covid-19 and Kidney Transplantation. N. Engl. J. Med. 2020, 382, 2475–2477. [Google Scholar] [CrossRef] [PubMed]
- Pereira, M.R.; Mohan, S.; Cohen, D.J.; Husain, S.A.; Dube, G.K.; Ratner, L.E.; Arcasoy, S.; Aversa, M.M.; Benvenuto, L.J.; Dadhania, D.M.; et al. COVID-19 in solid organ transplant recipients: Initial report from the US epicenter. Am. J. Transpl. 2020, 20, 1800–1808. [Google Scholar] [CrossRef] [PubMed]
- Fishman, J.A. Infection in solid-organ transplant recipients. N. Engl. J. Med. 2007, 357, 2601–2614. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nair, V.; Jandovitz, N.; Hirsch, J.S.; Nair, G.; Abate, M.; Bhaskaran, M.; Grodstein, E.; Berlinrut, I.; Hirschwerk, D.; Cohen, S.L.; et al. COVID-19 in kidney transplant recipients. Am. J. Transpl. 2020, 20, 1819–1825. [Google Scholar] [CrossRef]
- Alberici, F.; Delbarba, E.; Manenti, C.; Econimo, L.; Valerio, F.; Pola, A.; Maffei, C.; Possenti, S.; Zambetti, N.; Moscato, M.; et al. A single center observational study of the clinical characteristics and short-term outcome of 20 kidney transplant patients admitted for SARS-CoV2 pneumonia. Kidney Int. 2020, 97, 1083–1088. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [Green Version]
- Akdur, A.; Karakaya, E.; Ayvazoglu Soy, E.H.; Alshalabi, O.; Kirnap, M.; Arslan, H.; Ulubay, G.; Hekimoglu, K.; Moray, G.; Haberal, M. Coronavirus Disease (COVID-19) in Kidney and Liver Transplant Patients: A Single-Center Experience. Exp. Clin. Transpl. 2020, 18, 270–274. [Google Scholar] [CrossRef]
- Allam, S.R.; Dao, A.; Madhrira, M.M.; Antiporta, P.B.; Nair, R.R.; Guiteau, J.J.; Reyad, A.I. Interleukin-6 receptor antagonist therapy to treat SARS-CoV-2 driven inflammatory syndrome in a kidney transplant recipient. Transpl. Infect. Dis. 2020, 22, e13326. [Google Scholar] [CrossRef]
- Bartiromo, M.; Borchi, B.; Botta, A.; Bagalà, A.; Lugli, G.; Tilli, M.; Cavallo, A.; Xhaferi, B.; Cutruzzulà, R.; Vaglio, A.; et al. Threatening drug-drug interaction in a kidney transplant patient with coronavirus disease 2019 (COVID-19). Transpl. Infect. Dis. 2020, 22, e13286. [Google Scholar] [CrossRef] [Green Version]
- Billah, M.; Santeusanio, A.; Delaney, V.; Cravedi, P.; Farouk, S.S. A catabolic state in a kidney transplant recipient with COVID-19. Transpl. Int. 2020. [Google Scholar] [CrossRef]
- Bussalino, E.; De Maria, A.; Russo, R.; Paoletti, E. Immunosuppressive therapy maintenance in a kidney transplant recipient with SARS-CoV-2 pneumonia: A case report. Am. J. Transpl. 2020, 20, 1922–1924. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, S.; Yin, Q.; Shi, H.; Du, D.; Chang, S.; Ni, L.; Qiu, H.; Chen, Z.; Zhang, J.; Zhang, W. A familial cluster, including a kidney transplant recipient, of Coronavirus Disease 2019 (COVID-19) in Wuhan, China. Am. J. Transpl. 2020, 20, 1869–1874. [Google Scholar] [CrossRef] [PubMed]
- Cheng, D.R.; Wen, J.Q.; Liu, Z.Z.; Lv, T.F.; Chen, J.S. Coronavirus disease 2019 in renal transplant recipients: Report of two cases. Transpl. Infect. Dis. 2020, e13329. [Google Scholar] [CrossRef] [PubMed]
- Chenna, A.; Konala, V.M.; Gayam, V.; Naramala, S.; Adapa, S. Coronavirus Disease 2019 (COVID-19) in a Renal Transplant Patient. Cureus 2020, 12, e8038. [Google Scholar] [CrossRef]
- Dirim, A.B.; Demir, E.; Ucar, A.R.; Garayeva, N.; Safak, S.; Oto, O.A.; Yazici, H.; Alibeyoglu, A.M.; Orhun, G.; Cagatay, A.A.; et al. Fatal SARS-CoV-2 infection in a renal transplant recipient. CEN Case Rep. 2020, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Fontana, F.; Alfano, G.; Mori, G.; Amurri, A.; Tei, L.; Ballestri, M.; Leonelli, M.; Facchini, F.; Damiano, F.; Magistroni, R.; et al. COVID-19 pneumonia in a kidney transplant recipient successfully treated with tocilizumab and hydroxychloroquine. Am. J. Transpl. 2020, 20, 1902–1906. [Google Scholar] [CrossRef] [Green Version]
- Gandolfini, I.; Delsante, M.; Fiaccadori, E.; Zaza, G.; Manenti, L.; Degli Antoni, A.; Peruzzi, L.; Riella, L.V.; Cravedi, P.; Maggiore, U. COVID-19 in kidney transplant recipients. Am. J. Transpl. 2020, 20, 1941–1943. [Google Scholar] [CrossRef]
- Guillen, E.; Pineiro, G.J.; Revuelta, I.; Rodriguez, D.; Bodro, M.; Moreno, A.; Campistol, J.M.; Diekmann, F.; Ventura-Aguiar, P. Case report of COVID-19 in a kidney transplant recipient: Does immunosuppression alter the clinical presentation? Am. J. Transpl. 2020, 20, 1875–1878. [Google Scholar] [CrossRef] [Green Version]
- Hasan Ahmad, S.; Smith, R.; Camilleri, B. Belatacept, kidney transplantation and COVID-19: Successful management of the first reported case within the United Kingdom. Clin. Transpl. 2020, e14026. [Google Scholar] [CrossRef]
- Hsu, J.J.; Gaynor, P.; Kamath, M.; Fan, A.; Al-Saffar, F.; Cruz, D.; Nsair, A. COVID-19 in a high-risk dual heart and kidney transplant recipient. Am. J. Transpl. 2020, 20, 1911–1915. [Google Scholar] [CrossRef]
- Huang, J.; Lin, H.; Wu, Y.; Fang, Y.; Kumar, R.; Chen, G.; Lin, S. COVID-19 in posttransplant patients-report of 2 cases. Am. J. Transpl. 2020, 20, 1879–1881. [Google Scholar] [CrossRef] [PubMed]
- Jiang, J.; Miao, Y.; Zhao, Y.; Lu, X.; Zhou, P.; Zhou, X.; Chen, Z.; Du, D. Convalescent Plasma Therapy: Helpful Treatment of COVID-19 in a Kidney Transplant Recipient presenting with serve clinical manifestation and complex complications. Clin. Transpl. 2020, e14025. [Google Scholar] [CrossRef]
- Kates, O.S.; Fisher, C.E.; Stankiewicz-Karita, H.C.; Shepherd, A.K.; Church, E.C.; Kapnadak, S.G.; Lease, E.D.; Riedo, F.X.; Rakita, R.M.; Limaye, A.P. Earliest cases of coronavirus disease 2019 (COVID-19) identified in solid organ transplant recipients in the United States. Am. J. Transpl. 2020, 20, 1885–1890. [Google Scholar] [CrossRef] [PubMed]
- Kemmner, S.; Guba, M.O.; Schönermarck, U.; Stangl, M.; Fischereder, M. Cyclosporine as a preferred calcineurin inhibitor in renal allograft recipients with COVID-19 infection. Kidney Int. 2020, 98, 507–508. [Google Scholar] [CrossRef]
- Kim, Y.; Kwon, O.; Paek, J.H.; Park, W.Y.; Jin, K.; Hyun, M.; Lee, J.Y.; Kim, H.A.; Han, S. Two distinct cases with COVID-19 in kidney transplant recipients. Am. J. Transpl. 2020. [Google Scholar] [CrossRef]
- Kocak, B.; Arpali, E.; Akyollu, B.; Yelken, B.; Tekin, S.; Kanbay, M.; Turkmen, A.; Kalayoglu, M. A Case Report of Oligosymptomatic Kidney Transplant Patients with COVID-19: Do They Pose a Risk to Other Recipients? Transpl. Proc. 2020. [Google Scholar] [CrossRef] [PubMed]
- Kolonko, A.; Dudzicz, S.; Wiecek, A.; Król, R. COVID-19 infection in solid organ transplant recipients: A single-center experience with patients immediately after transplantation. Transpl. Infect. Dis. 2020, e13381. [Google Scholar] [CrossRef]
- Kumar, R.N.; Tanna, S.D.; Shetty, A.A.; Stosor, V. COVID-19 in an HIV-positive Kidney Transplant Recipient. Transpl. Infect. Dis. 2020, e13338. [Google Scholar] [CrossRef]
- Lauterio, A.; Valsecchi, M.; Santambrogio, S.; De Carlis, R.; Merli, M.; Calini, A.; Centonze, L.; Buscemi, V.; Bottiroli, M.; Puoti, M.; et al. Successful recovery from severe COVID-19 pneumonia after kidney transplantation: The interplay between immunosuppression and novel therapy including tocilizumab. Transpl. Infect. Dis. 2020, e13334. [Google Scholar] [CrossRef]
- Machado, D.J.B.; Ianhez, L.E. COVID-19 pneumonia in kidney transplant recipients-Where we are? Transpl. Infect. Dis. 2020, e13306. [Google Scholar] [CrossRef]
- Man, Z.; Jing, Z.; Huibo, S.; Bin, L.; Fanjun, Z. Viral shedding prolongation in a kidney transplant patient with COVID-19 pneumonia. Am. J. Transpl. 2020. [Google Scholar] [CrossRef] [PubMed]
- Marx, D.; Moulin, B.; Fafi-Kremer, S.; Benotmane, I.; Gautier, G.; Perrin, P.; Caillard, S. First case of COVID-19 in a kidney transplant recipient treated with belatacept. Am. J. Transpl. 2020, 20, 1944–1946. [Google Scholar] [CrossRef]
- Meziyerh, S.; Zwart, T.C.; van Etten, R.W.; Janson, J.A.; van Gelder, T.; Alwayn, I.P.J.; de Fijter, J.W.; Reinders, M.E.J.; Moes, D.; de Vries, A.P.J. Severe COVID-19 in a renal transplant recipient: A focus on pharmacokinetics. Am. J. Transpl. 2020, 20, 1896–1901. [Google Scholar] [CrossRef] [PubMed]
- Namazee, N.; Mahmoudi, H.; Afzal, P.; Ghaffari, S. Novel Corona Virus 2019 pneumonia in a kidney transplant recipient. Am. J. Transpl. 2020. [Google Scholar] [CrossRef] [PubMed]
- Ning, L.; Liu, L.; Li, W.; Liu, H.; Wang, J.; Yao, Z.; Zhang, S.; Zhao, D.; Nashan, B.; Shen, A.; et al. Novel coronavirus (SARS-CoV-2) infection in a renal transplant recipient: Case report. Am. J. Transpl. 2020, 20, 1864–1868. [Google Scholar] [CrossRef] [Green Version]
- Seminari, E.; Colaneri, M.; Sambo, M.; Gallazzi, I.; Di Matteo, A.; Roda, S.; Bruno, R. SARS Cov-2 infection in a renal-transplanted patient: A case report. Am. J. Transpl. 2020, 20, 1882–1884. [Google Scholar] [CrossRef]
- Serrano, O.K.; Kutzler, H.L.; Rochon, C.; Radojevic, J.A.; Lawlor, M.T.; Hammond, J.A.; Gluck, J.; Feingold, A.D.; Jaiswal, A. Incidental COVID-19 in a heart-kidney transplant recipient with malnutrition and recurrent infections: Implications for the SARS-CoV-2 immune response. Transpl. Infect. Dis. 2020, e13367. [Google Scholar] [CrossRef]
- Shingare, A.; Bahadur, M.M.; Raina, S. COVID-19 in recent kidney transplant recipients. Am. J. Transpl. 2020. [Google Scholar] [CrossRef]
- Antony, S.J.; Singh, J.; de Jesus, M.; Lance, J. Early Use of Tocilizumab in Respiratory Failure Associated with Acute COVID-19 Pneumonia in Recipients with Solid Organ Transplantation. IDCases 2020, e00888. [Google Scholar] [CrossRef]
- Suwanwongse, K.; Shabarek, N. Fatal Outcome in a Kidney-Pancreas Transplant Recipient With COVID-19. Cureus 2020, 12. [Google Scholar] [CrossRef] [PubMed]
- Tantisattamo, E.; Reddy, U.G.; Duong, D.K.; Ferrey, A.J.; Ichii, H.; Dafoe, D.C.; Kalantar-Zadeh, K. Hyponatremia: A Possible Immuno-Neuroendocrine Interface with COVID-19 in a Kidney Transplant Recipient. Transpl. Infect. Dis. 2020, e13355. [Google Scholar] [CrossRef]
- Thammathiwat, T.; Tungsanga, S.; Tiankanon, K.; Torvorapanit, P.; Chumpangern, W.; Udomkarnjananun, S.; Avihingsanon, Y.; Sriprasart, T.; Srisawat, N.; Jutivorakool, K.; et al. A Case of Successful Treatment of Severe COVID-19 Pneumonia with Favipiravir and Tocilizumab in Post-kidney Transplant Recipient. Transpl. Infect. Dis. 2020, e13388. [Google Scholar] [CrossRef]
- Velioglu, A.; Tuglular, S. Care of Asymptomatic SARS-CoV-2 positive Kidney Transplant Recipients. Transpl. Int. 2020. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Li, X.; Cao, G.; Wu, X.; Wang, Z.; Yan, T. COVID-19 in a Kidney Transplant Patient. Eur. Urol. 2020, 77, 769–770. [Google Scholar] [CrossRef]
- Xia, T.; Wang, Y. Coronavirus disease 2019 and transplantation: The combination of lopinavir/ritonavir and hydroxychloroquine is responsible for excessive tacrolimus trough level and unfavorable outcome. Am. J. Transpl. 2020. [Google Scholar] [CrossRef]
- Xu, J.J.; Samaha, D.; Mondhe, S.; Massicotte-Azarniouch, D.; Knoll, G.; Ruzicka, M. Renal infarct in a COVID-19-positive kidney-pancreas transplant recipient. Am. J. Transpl. 2020. [Google Scholar] [CrossRef]
- Zhong, Z.; Zhang, Q.; Xia, H.; Wang, A.; Liang, W.; Zhou, W.; Zhou, L.; Liu, X.; Rao, L.; Li, Z.; et al. Clinical characteristics and immunosuppressant management of coronavirus disease 2019 in solid organ transplant recipients. Am. J. Transpl. 2020, 20, 1916–1921. [Google Scholar] [CrossRef] [Green Version]
- Abrishami, A.; Samavat, S.; Behnam, B.; Arab-Ahmadi, M.; Nafar, M.; Sanei Taheri, M. Clinical Course, Imaging Features, and Outcomes of COVID-19 in Kidney Transplant Recipients. Eur. Urol. 2020, 78, 281–286. [Google Scholar] [CrossRef]
- Banerjee, D.; Popoola, J.; Shah, S.; Ster, I.C.; Quan, V.; Phanish, M. COVID-19 infection in kidney transplant recipients. Kidney Int. 2020, 97, 1076–1082. [Google Scholar] [CrossRef]
- Bösch, F.; Börner, N.; Kemmner, S.; Lampert, C.; Jacob, S.; Koliogiannis, D.; Stangl, M.; Michel, S.; Kneidinger, N.; Schneider, C.; et al. Attenuated early inflammatory response in solid organ recipients with COVID-19. Clin. Transpl. 2020, e14027. [Google Scholar] [CrossRef]
- Bossini, N.; Alberici, F.; Delbarba, E.; Valerio, F.; Manenti, C.; Possenti, S.; Econimo, L.; Maffei, C.; Pola, A.; Terlizzi, V.; et al. Kidney transplant patients with SARS-CoV-2 infection: The brescia renal COVID task force experience. Am. J. Transpl. 2020. [Google Scholar] [CrossRef] [PubMed]
- Chen, T.Y.; Farghaly, S.; Cham, S.; Tatem, L.L.; Sin, J.H.; Rauda, R.; Ribisi, M.; Sumrani, N. COVID-19 pneumonia in kidney transplant recipients: Focus on immunosuppression management. Transpl. Infect. Dis. 2020, e13378. [Google Scholar] [CrossRef]
- University, C. Early Description of Coronavirus 2019 Disease in Kidney Transplant Recipients in New York. J. Am. Soc. Nephrol. 2020, 31, 1150–1156. [Google Scholar] [CrossRef]
- Crespo, M.; Pérez-Sáez, M.J.; Redondo-Pachón, D.; Llinàs-Mallol, L.; Montero, M.M.; Villar-García, J.; Arias-Cabrales, C.; Buxeda, A.; Burballa, C.; Vázquez, S.; et al. COVID-19 in elderly kidney transplant recipients. Am. J. Transpl. 2020. [Google Scholar] [CrossRef] [PubMed]
- Devresse, A.; Belkhir, L.; Vo, B.; Ghaye, B.; Scohy, A.; Kabamba, B.; Goffin, E.; De Greef, J.; Mourad, M.; De Meyer, M.; et al. COVID-19 Infection in Kidney Transplant Recipients: A Single-Center Case Series of 22 Cases From Belgium. Kidney Med. 2020. [Google Scholar] [CrossRef]
- Fernández-Ruiz, M.; Andrés, A.; Loinaz, C.; Delgado, J.F.; López-Medrano, F.; San Juan, R.; González, E.; Polanco, N.; Folgueira, M.D.; Lalueza, A.; et al. COVID-19 in solid organ transplant recipients: A single-center case series from Spain. Am. J. Transpl. 2020, 20, 1849–1858. [Google Scholar] [CrossRef] [PubMed]
- Fung, M.; Chiu, C.Y.; DeVoe, C.; Doernberg, S.B.; Schwartz, B.S.; Langelier, C.; Henrich, T.J.; Yokoe, D.; Davis, J.; Hays, S.R.; et al. Clinical outcomes and serologic response in solid organ transplant recipients with COVID-19: A case series from the United States. Am. J. Transpl. 2020. [Google Scholar] [CrossRef]
- Maritati, F.; Cerutti, E.; Zuccatosta, L.; Fiorentini, A.; Finale, C.; Ficosecco, M.; Cristiano, F.; Capestro, A.; Balestra, E.; Taruscia, D.; et al. SARS-CoV-2 infection in kidney transplant recipients: Experience of the italian marche region. Transpl. Infect. Dis. 2020, e13377. [Google Scholar] [CrossRef]
- Mehta, S.A.; Leonard, J.; Labella, P.; Cartiera, K.; Soomro, I.; Neumann, H.; Montgomery, R.A.; Ali, N.M. Outpatient management of kidney transplant recipients with suspected COVID-19-Single-center experience during the New York City surge. Transpl. Infect. Dis. 2020, e13383. [Google Scholar] [CrossRef]
- Mella, A.; Mingozzi, S.; Gallo, E.; Lavacca, A.; Rossetti, M.; Clari, R.; Randone, O.; Maffei, S.; Salomone, M.; Imperiale, D.; et al. Case series of six kidney transplanted patients with COVID-19 pneumonia treated with tocilizumab. Transpl. Infect. Dis. 2020, e13348. [Google Scholar] [CrossRef]
- Montagud-Marrahi, E.; Cofan, F.; Torregrosa, J.V.; Cucchiari, D.; Ventura-Aguiar, P.; Revuelta, I.; Bodro, M.; Piñeiro, G.J.; Esforzado, N.; Ugalde, J.; et al. Preliminary data on outcomes of SARS-CoV-2 infection in a Spanish single center cohort of kidney recipients. Am. J. Transpl. 2020. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Cubillo, B.; Moreno de la Higuera, M.A.; Lucena, R.; Valdes Franci, E.; Hurtado, M.; Calvo Romero, N.; Rodriguez Moreno, A.; Valencia, D.; Velo, M.; Sagastagoitia Fornie, I.; et al. Should cyclosporine be useful in renal transplant recipients affected by SARS-CoV-2? Am. J. Transpl. 2020. [Google Scholar] [CrossRef] [PubMed]
- Silva, F.; Cipriano, A.; Cruz, H.; Tavares, J.; Fragoso, J.; Malheiro, J.; Almeida, M.; Martins, S.; Abreu, M.; Pedroso, S.; et al. SARS-CoV-2 infection in kidney transplant recipients: Early report of five cases. Transpl. Infect. Dis. 2020, e13394. [Google Scholar] [CrossRef]
- Trujillo, H.; Caravaca-Fontán, F.; Sevillano, Á.; Gutiérrez, E.; Caro, J.; Yuste, C.; Andrés, A.; Praga, M. SARS-CoV-2 Infection in Hospitalized Patients with Kidney Disease. Kidney Int. Rep. 2020, 5, 905–909. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Dai, H.; Xie, X. Solid Organ Transplantation During the COVID-19 Pandemic. Front. Immunol. 2020, 11, 1392. [Google Scholar] [CrossRef] [PubMed]
- Zhu, L.; Gong, N.; Liu, B.; Lu, X.; Chen, D.; Chen, S.; Shu, H.; Ma, K.; Xu, X.; Guo, Z.; et al. Coronavirus Disease 2019 Pneumonia in Immunosuppressed Renal Transplant Recipients: A Summary of 10 Confirmed Cases in Wuhan, China. Eur. Urol. 2020, 77, 748–754. [Google Scholar] [CrossRef]
- Imam, A.; Abukhalaf, S.A.; Imam, R.; Abu-Gazala, S.; Merhav, H.; Khalaileh, A. Kidney Transplantation in the Times of COVID-19—A Literature Review. Ann. Transpl. 2020, 25, e925755. [Google Scholar] [CrossRef]
- Esagian, S.M.; Ziogas, I.A.; Giannis, D.; Hayat, M.H.; Elias, N.; Tsoulfas, G. Challenges in Abdominal Organ Transplantation During the COVID-19 Pandemic. Front. Med. 2020, 7, 287. [Google Scholar] [CrossRef]
- Husain, S.A.; Dube, G.; Morris, H.; Fernandez, H.; Chang, J.H.; Paget, K.; Sritharan, S.; Patel, S.; Pawliczak, O.; Boehler, M.; et al. Early Outcomes of Outpatient Management of Kidney Transplant Recipients with Coronavirus Disease 2019. Clin. J. Am. Soc. Nephrol. 2020. [Google Scholar] [CrossRef]
- D’Antiga, L. Coronaviruses and Immunosuppressed Patients: The Facts During the Third Epidemic. Liver Transplant. 2020, 26, 832–834. [Google Scholar] [CrossRef] [PubMed]
- Zhou, F.; Yu, T.; Du, R.; Fan, G.; Liu, Y.; Liu, Z.; Xiang, J.; Wang, Y.; Song, B.; Gu, X.; et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 2020, 395, 1054–1062. [Google Scholar] [CrossRef]
- Garg, S.; Kim, L.; Whitaker, M.; O’Halloran, A.; Cummings, C.; Holstein, R.; Prill, M.; Chai, S.J.; Kirley, P.D.; Alden, N.B.; et al. Hospitalization Rates and Characteristics of Patients Hospitalized with Laboratory-Confirmed Coronavirus Disease 2019—COVID-NET, 14 States, 1–30 March 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 458–464. [Google Scholar] [CrossRef]
- Lighter, J.; Phillips, M.; Hochman, S.; Sterling, S.; Johnson, D.; Francois, F.; Stachel, A. Obesity in Patients Younger Than 60 Years Is a Risk Factor for COVID-19 Hospital Admission. Clin. Infect. Dis. 2020, 71, 896–897. [Google Scholar] [CrossRef] [Green Version]
- Johns Hopkins Coronavirus Resource Center. Available online: https://coronavirus.jhu.edu/map.html (accessed on 6 September 2020).
- Yang, X.; Yu, Y.; Xu, J.; Shu, H.; Xia, J.; Liu, H.; Wu, Y.; Zhang, L.; Yu, Z.; Fang, M.; et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: A single-centered, retrospective, observational study. Lancet Respir. Med. 2020, 8, 475–481. [Google Scholar] [CrossRef] [Green Version]
- Chu, K.H.; Tsang, W.K.; Tang, C.S.; Lam, M.F.; Lai, F.M.; To, K.F.; Fung, K.S.; Tang, H.L.; Yan, W.W.; Chan, H.W.; et al. Acute renal impairment in coronavirus-associated severe acute respiratory syndrome. Kidney Int. 2005, 67, 698–705. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tisoncik, J.R.; Korth, M.J.; Simmons, C.P.; Farrar, R.J.; Martin, T.; Katze, M.G. Into the Eye of the Cytokine Storm. Microbiol. Mol. Biol. Rev. 2012, 76, 16–32. [Google Scholar] [CrossRef] [Green Version]
- Mombelli, M.; Kampouri, E.; Manuel, O. Influenza in solid organ transplant recipients: Epidemiology, management, and outcomes. Expert Rev. Anti-Infect. Ther. 2020, 18, 103–112. [Google Scholar] [CrossRef]
- Ritter, M.L.; Pirofski, L. Mycophenolate mofetil: Effects on cellular immune subsets, infectious complications, and antimicrobial activity. Transpl. Infect. Dis. 2009, 11, 290–297. [Google Scholar] [CrossRef] [Green Version]
- Berger, S.P.; Sommerer, C.; Witzke, O.; Tedesco, H.; Chadban, S.; Mulgaonkar, S.; Qazi, Y.; de Fijter, J.W.; Oppenheimer, F.; Cruzado, J.M.; et al. Two-year outcomes in de novo renal transplant recipients receiving everolimus-facilitated calcineurin inhibitor reduction regimen from the TRANSFORM study. Am. J. Transpl. 2019, 19, 3018–3034. [Google Scholar] [CrossRef]
- Zaza, G.; Granata, S.; Tomei, P.; Masola, V.; Gambaro, G.; Lupo, A. mTOR inhibitors and renal allograft: Yin and Yang. J. Nephrol. 2014, 27, 495–506. [Google Scholar] [CrossRef] [PubMed]
- Marfo, K.; Greenstein, S. Antiretroviral and immunosuppressive drug-drug interactions in human immunodeficiency virus-infected liver and kidney transplant recipients. Transpl. Proc. 2009, 41, 3796–3799. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.Y.; Wang, F.L.; Lin, C.C. Chronic hydroxychloroquine use associated with QT prolongation and refractory ventricular arrhythmia. Clin. Toxicol. 2006, 44, 173–175. [Google Scholar] [CrossRef] [PubMed]
- Warren, T.K.; Jordan, R.; Lo, M.K.; Ray, A.S.; Mackman, R.L.; Soloveva, V.; Siegel, D.; Perron, M.; Bannister, R.; Hui, H.C.; et al. Therapeutic efficacy of the small molecule GS-5734 against Ebola virus in rhesus monkeys. Nature 2016, 531, 381–385. [Google Scholar] [CrossRef] [PubMed]
- Beigel, J.H.; Tomashek, K.M.; Dodd, L.E.; Mehta, A.K.; Zingman, B.S.; Kalil, A.C.; Hohmann, E.; Chu, H.Y.; Luetkemeyer, A.; Kline, S.; et al. Remdesivir for the Treatment of Covid-19-Preliminary Report. N. Engl. J. Med. 2020. [Google Scholar] [CrossRef] [PubMed]
- Gautret, P.; Lagier, J.C.; Parola, P.; Hoang, V.T.; Meddeb, L.; Mailhe, M.; Doudier, B.; Courjon, J.; Giordanengo, V.; Vieira, V.E.; et al. Hydroxychloroquine and azithromycin as a treatment of COVID-19: Results of an open-label non-randomized clinical trial. Int. J. Antimicrob. Agents 2020, 56, 105949. [Google Scholar] [CrossRef]
- WHO. Discontinues Hydroxychloroquine and Lopinavir/Ritonavir Treatment Arms for COVID-19. Published online 4 July 2020; WHO Website. 2020. Available online: https://www.who.int/news-room/detail/04-07-2020-who-discontinues-hydroxychloroquine-and-lopinavir-/ritonavir-treatment-arms-for-covid-19 (accessed on 30 July 2020).
- Shang, L.; Zhao, J.; Hu, Y.; Du, R.; Cao, B. On the use of corticosteroids for 2019-nCoV pneumonia. Lancet 2020, 395, 683–684. [Google Scholar] [CrossRef] [Green Version]
- Horby, P.; Lim, W.S.; Emberson, J.R.; Mafham, M.; Bell, J.L.; Linsell, L.; Staplin, N.; Brightling, C.; Ustianowski, A.; Elmahi, E.; et al. Dexamethasone in Hospitalized Patients with Covid-19—Preliminary Report. N. Engl. J. Med. 2020. [Google Scholar] [CrossRef]
- Frey, N.; Porter, D. Cytokine Release Syndrome with Chimeric Antigen Receptor T Cell Therapy. Biol. Blood Marrow Transpl. 2019, 25, e123–e127. [Google Scholar] [CrossRef] [Green Version]
| Case Reports | ||||
|---|---|---|---|---|
| Authors | Region/Country | Patients (No.) | Type of Study | Hospitalized |
| [9] Akdur et al. | Ankara, Turkey | 1 | Case Report | 0 |
| [10] Allam et al. | Fort Worth, TX, USA | 1 | Correspondence | 1 |
| [11] Bartiromo et al. | Florence, Italy | 1 | Correspondence | 1 |
| [12] Billah et al. | New York, NY, USA | 1 | Correspondence | 1 |
| [13] Bussalino et al. | Genoa, Italy | 1 | Case Report | 1 |
| [14] Chen et al. | Wuhan, China | 1 | Case Report | 1 |
| [15] Cheng et al. | Nanjing, China | 2 | Case Report | 2 |
| [16] Chenna et al. | Albany, NY, USA | 1 | Case Report | 1 |
| [17] Dirim et al. | Istanbul, Turkey | 1 | Case Report | 1 |
| [18] Fontana et al. | Modena, Italy | 1 | Case Report | 1 |
| [19] Gandolfini et al. | Parma, Italy | 2 | Correspondence | 2 |
| [20] Guillen et al. | Barcelona, Spain | 1 | Case Report | 1 |
| [21] Hasan Ahmad et al. | Ipswich, UK. | 1 | Correspondence | 1 |
| [22] Hsu et al. | Los Angeles, CA, USA | 1 | Case Report | 1 |
| [23] Huang et al. | Fuzhou, China | 1 | Case Report | 1 |
| [24] Jiang et al. | Wuhan, China | 1 | Correspondence | 1 |
| [25] Kates et al. | Seattle, WA, USA | 1 | Case Report | 1 |
| [26] Kemmner et al. | Munich, Germany | 1 | Correspondence | 1 |
| [27] Kim et al. | Daegu, Korea | 2 | Case Report | 2 |
| [28] Kocak et al. | Istanbul, Turkey | 2 | Case Report | 2 |
| [29] Kolonko et al. | Katowice, Poland | 3 | Case Report | 3 |
| [30] Kumar et al. | Chicago, IL, USA | 1 | Case Report | 0 |
| [31] Lauterio et al. | Milan, Italy | 1 | Correspondence | 1 |
| [32] Machado et al. | Sao Paulo, Brazil | 1 | Case Report | 1 |
| [33] Man et al. | Wuhan, China | 1 | Correspondence | 1 |
| [34] Marx et al. | Strasbourg, France | 1 | Correspondence | 1 |
| [35] Meziyerh et al. | Leiden, Netherlands | 1 | Case Report | 1 |
| [36] Namazee et al. | Semnan, Iran | 1 | Case Report | 1 |
| [37] Ning et al. | Hefei, China | 1 | Case Report | 1 |
| [38] Seminari et al. | Pavia, Italy | 1 | Case Report | 1 |
| [39] Serrano et al. | Hartford, CT, USA | 1 | Case Report | 1 |
| [40] Shingare et al. | Mumbai, India | 2 | Case Report | 2 |
| [41] SJ Antony et al. | El Paso, TX, USA | 1 | Case Report | 1 |
| [42] Suwanwongse et al. | New York, NY, USA | 1 | Case Report | 1 |
| [43] Tantisattamo et al. | Orange, CA, USA | 1 | Case Report | 1 |
| [44] Thammathiwat et al. | Bangkok, Thailand | 1 | Case Report | 1 |
| [45] Velioglu et al. | Istanbul, Turkey | 1 | Correspondence | 0 |
| [46] Wang et al. | Zhengzhou, China | 1 | Correspondence | 1 |
| [47] Xia et al. | Wuhan, China | 1 | Correspondence | 1 |
| [48] Xu et al. | Ottawa, Canada | 1 | Case Report | 1 |
| [49] Zhong et al. | Wuhan, China | 1 | Case Report | 1 |
| Case Series | ||||||
|---|---|---|---|---|---|---|
| Authors | Region/Country | Patients (No) | Type of Study | Hospitalized | Infection Rate (%) | CFR (%) |
| [50] Abrishami et al. | Tehran, Iran | 12 | Case Series | 12 | - | 66.7 |
| [3] Akalin et al. | Bronx, NY, USA | 36 | Correspondence | 28 | - | 27.8 |
| [7] Alberici et al. | Brescia, Italy | 20 | Case Series | 20 | 1.67 | 25 |
| [51] Banerjee et al. | London, UK. | 7 | Case Series | 5 | - | - |
| [52] Bosch et al. | Munich, Germany | 3 | Case Series | 3 | - | - |
| [53] Bossini et al. | Brescia, Italy | 53 | Case Series | 45 | - | 28.3 |
| [54] Chen et al. | Brooklyn, NY, USA | 30 | Case Series | 30 | - | 20 |
| [55] Columbia University | New York, NY, USA | 15 | Case Series | 15 | - | 13.3 |
| [56] Crespo et al. | Barcelona, Spain | 16 | Correspondence | 15 | 4.93 | 50 |
| [57] Devresse et al. | Brussels, Belgium | 22 | Case Series | 18 | 1.83 | 9.1 |
| [58] Fernandez-Ruiz et al. | Madrid, Spain | 8 | Correspondence | 8 | - | - |
| [59] Fung et al. | San Francisco, CA, USA | 7 | Case Series | 5 | - | - |
| [60] Maritati et al. | Ancona, Italy | 5 | Case Series | 5 | - | 25 |
| [61] Mehta et al. | New York, NY, USA | 34 | Correspondence | 34 | - | 17.1 |
| [62] Mella et al. | Turin, Italy | 6 | Case Series | 6 | - | - |
| [63] Montagud-Marrahi et al. | Barcelona, Spain | 33 | Correspondence | 26 | - | 6 |
| [6] Nair et al. | Hempstead, NY, USA | 10 | Case Series | 9 | - | 33.3 |
| [64] Rodriguez-Cubillo et al. | Madrid, Spain | 29 | Correspondence | 29 | - | 20.7 |
| [65] Silva et al. | Porto, Portugal | 5 | Case Series | 4 | - | - |
| [66] Trujillo et al. | Madrid, Spain | 26 | Case Series | 26 | 1.04 | 23.1 |
| [67] Zhang et al. | Wuhan, China | 5 | Case Series | 5 | - | - |
| [68] Zhu et al. | Wuhan, China | 10 | Case–control Study | 10 | 0.33 | 10 |
| Demographics | |
|---|---|
| Age (years, median) (n = 169) | 55 (21–80) |
| Gender (male) | 276/415 (67%) |
| Type of donor (deceased donor) | 195/264 (74%) |
| Multiple organ transplant recipients | 7/420 (2%) |
| Repeat KTx | 7/420 (2%) |
| Time from KTx (years, median) | 6.5 (0–33) |
| Time from KTx ≤ 1 year | 48/209 (23%) |
| Comorbidities (n = 326) | |
| HTN | 81% |
| DM | 36% |
| CVD | 21% |
| Obesity | 15% |
| COPD | 5% |
| Malignancy | 4% |
| Chronic viral infection | 2% |
| Renal function | |
| Baseline sCr (mg/dL, median) (n = 91) | 1.47 (0.62–5.09) |
| Peak sCr during hospitalization (mg/dL, median) (n = 74) | 2.17 (0.62–10.94) |
| sCr at discharge (median) (n = 58) | 1.45 (0.29–6.45) |
| Baseline Immunosuppressive regimen | |
| MPA/AZA + CNI ± CS | 136/186 (73%) |
| Hospital admission (n = 420) | 93% |
| Duration of hospitalization (days, median) (n = 104) | 16 (1–100) |
| Admission to ICU | 118/391 (30%) |
| Duration of ICU stay (days, median) (n = 32) | 8.5 (1–34) |
| Type of Ventilation | |
| NIV | 27/379 (7%) |
| IMV | 88/379 (23%) |
| ARDS | 175/391 (45%) |
| AKI | 150/345 (44%) |
| RRT | 34/150 (23%) |
| Immunosuppression management | |
| IS discontinuation | 66/212 (31%) |
| IS reduction | 97/357 (27%) |
| Switch TAC or mTORi to CsA | 24/358 (7%) |
| CNI tapering | 65/204 (32%) |
| CNI withdrawal | 118/204 (58%) |
| Antimetabolite withdrawal | 227/250 (91%) |
| COVID-19 treatment | |
| Antivirals | 123/414 (30%) |
| Lopinavir/Ritonavir | 94/123 (76%) |
| HCQ | 320/409 (78%) |
| Antibiotics | 290/399 (73%) |
| Azithromycin | 155/290 (53%) |
| CS (IV bolus or Dexamethasone) | 83/331 (25%) |
| Anti-IL agents | 59/213 (28%) |
| IV immunoglobulins | 35/415 (8%) |
| Major outcomes | |
| Death | 93/420 (22%) |
| Discharge | 232/391 (59%) |
| Characteristics of Patients with KTx for ≤1 year | |
|---|---|
| Age (years, mean ± SD) (n = 29) | 53.9 ± 13.9 |
| Gender (male) | 18/34 (53%) |
| Baseline sCr (mg/dL, median) (n = 21) | 1.24 (0.75–2.7) |
| Induction immunosuppression (n = 17) | |
| Antithymocyte globulin (ATG) | 8/17 (47%) |
| Basiliximab | 1/17 (6%) |
| Baseline Immunosuppression (n = 34) | |
| MPA + CNI ± CS | 31/34 (91.2%) |
| IS discontinuation | 9/34 (27%) |
| IS reduction | 18/34 (53%) |
| Antimetabolite withdrawal | 26/34 (77%) |
| COVID-19 Treatment | |
| Antivirals | 7/34 (21%) |
| HCQ | 18/32 (56%) |
| Azithromycin | 3/32 (9%) |
| Corticosteroids (IV) | 3/32 (9%) |
| Tocilizumab | 3/32 (9%) |
| Hospital admission | 32/34 (94%) |
| Admission to ICU | 9/32 (28%) |
| ARDS | 10/32 (31%) |
| AKI | 12/32 (38%) |
| Death | 5/34 (15%) |
| Characteristics of patients ≥ 65 years | |
| Age (years, mean ± SD) (n = 54) | 71.6 ± 4.7 |
| Gender (male) | 45/70 (64%) |
| Baseline sCr (mg/dL, median) (n = 23) | 1.8 (0.62–3.39) |
| Baseline Immunosuppression (n = 52) | |
| MPA/AZA + CNI ± CS | 34/52 (65%) |
| mTORi-based regimen | 9/52 (17%) |
| IS discontinuation | 28/54 (52%) |
| IS reduction | 17/54 (32%) |
| COVID-19 Treatment | |
| Antivirals | 19/69 (28%) |
| HCQ | 53/70 (76%) |
| Azithromycin | 19/63 (30%) |
| Corticosteroids (IV) | 18/70 (26%) |
| Tocilizumab | 11/70 (16%) |
| Hospital admission | 69/70 (99%) |
| Admission to ICU | 13/69 (19%) |
| ARDS | 32/69 (46%) |
| AKI | 24/68 (35%) |
| Death | 22/69 (32%) |
| Characteristics of patients who died | |
| Age (years, mean ± SD) (n = 37) | 64.2 ± 9.1 |
| Gender (male) | 37/61 (61%) |
| Baseline sCr (mg/dL, mean ± SD) (n = 20) | 2.14 ± 0.9 |
| IS discontinuation | 36/65 (55%) |
| IS reduction | 18/51 (35%) |
| COVID-19 Treatment | |
| Antivirals | 26/79 (33%) |
| HCQ | 51/64 (80%) |
| Azithromycin | 19/54 (35%) |
| Corticosteroids (IV) | 32/74 (43%) |
| Tocilizumab | 15/74 (20%) |
| Admission to ICU | 47/81 (58%) |
| ARDS | 62/77 (81%) |
| AKI | 26/45 (58%) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marinaki, S.; Tsiakas, S.; Korogiannou, M.; Grigorakos, K.; Papalois, V.; Boletis, I. A Systematic Review of COVID-19 Infection in Kidney Transplant Recipients: A Universal Effort to Preserve Patients’ Lives and Allografts. J. Clin. Med. 2020, 9, 2986. https://doi.org/10.3390/jcm9092986
Marinaki S, Tsiakas S, Korogiannou M, Grigorakos K, Papalois V, Boletis I. A Systematic Review of COVID-19 Infection in Kidney Transplant Recipients: A Universal Effort to Preserve Patients’ Lives and Allografts. Journal of Clinical Medicine. 2020; 9(9):2986. https://doi.org/10.3390/jcm9092986
Chicago/Turabian StyleMarinaki, Smaragdi, Stathis Tsiakas, Maria Korogiannou, Konstantinos Grigorakos, Vassilios Papalois, and Ioannis Boletis. 2020. "A Systematic Review of COVID-19 Infection in Kidney Transplant Recipients: A Universal Effort to Preserve Patients’ Lives and Allografts" Journal of Clinical Medicine 9, no. 9: 2986. https://doi.org/10.3390/jcm9092986
APA StyleMarinaki, S., Tsiakas, S., Korogiannou, M., Grigorakos, K., Papalois, V., & Boletis, I. (2020). A Systematic Review of COVID-19 Infection in Kidney Transplant Recipients: A Universal Effort to Preserve Patients’ Lives and Allografts. Journal of Clinical Medicine, 9(9), 2986. https://doi.org/10.3390/jcm9092986







