No-Reflow after PPCI—A Predictor of Short-Term Outcomes in STEMI Patients
Abstract
1. Introduction
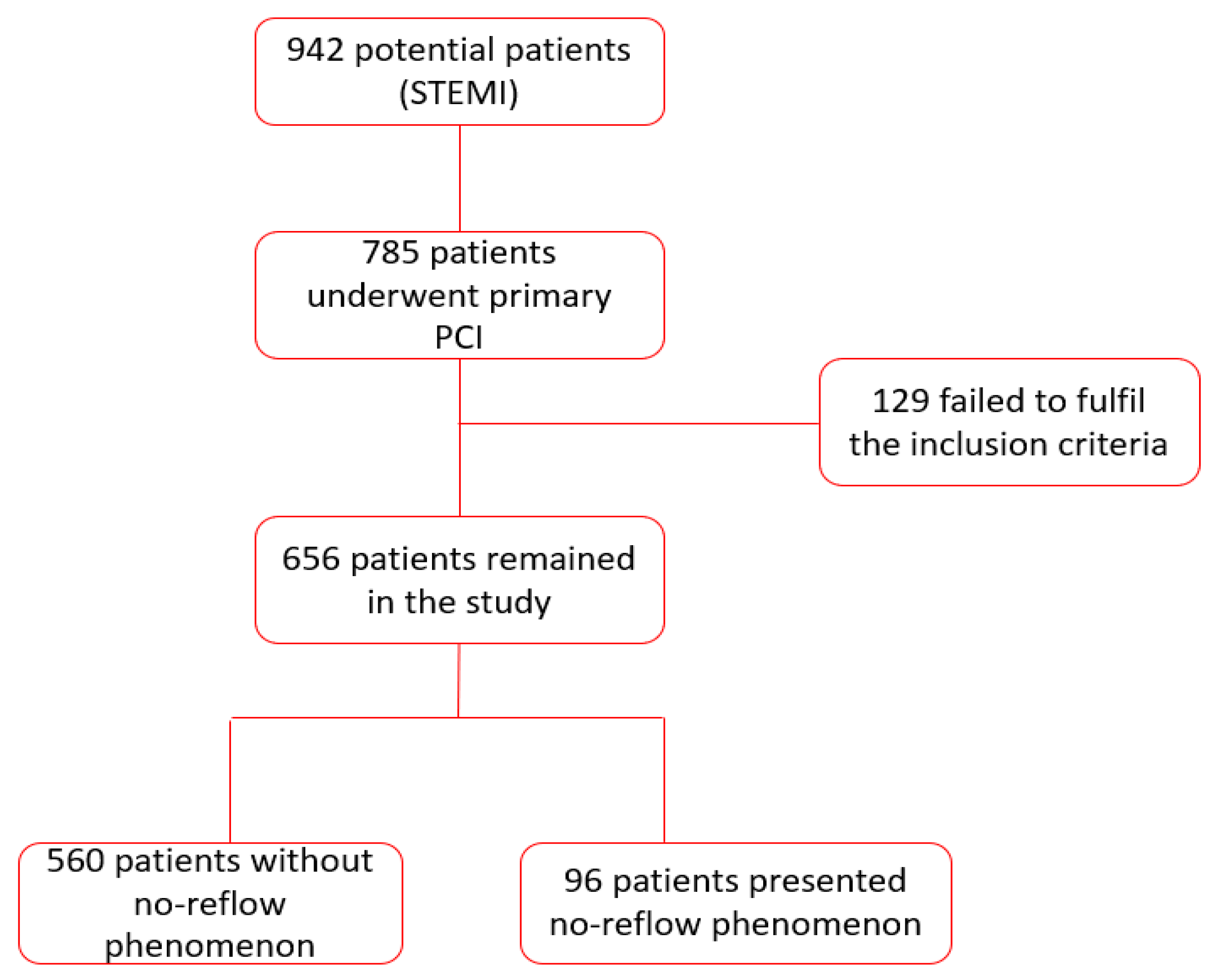
2. Materials and Methods
2.1. Study Design
2.2. Ethical Statement
2.3. Clinical Investigations
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Guarini, G.; Huqi, A.; Morrone, D.; Capozza, P.; Todiere, G.; Marzilli, M. Pharmacological Approaches to Coronary Microvascular Dysfunction. Pharmacol. Ther. 2014, 144, 283–302. [Google Scholar] [CrossRef] [PubMed]
- Goff, S.L.; Mazor, K.M.; Ting, H.H.; Kleppel, R.; Rothberg, M.B. How Cardiologists Present the Benefits of Percutaneous Coronary Interventions to Patients with Stable Angina: A Qualitative Analysis. JAMA Intern. Med. 2014, 174, 1614–1621. [Google Scholar] [CrossRef] [PubMed]
- Jaffe, R.; Charron, T.; Puley, G.; Dick, A.; Strauss, B.H. Microvascular Obstruction and the No-Reflow Phenomenon after Percutaneous Coronary Intervention. Circulation 2008, 117, 3152–3156. [Google Scholar] [CrossRef] [PubMed]
- Mazhar, J.; Mashicharan, M.; Farshid, A. Predictors and Outcome of No-Reflow Post Primary Percutaneous Coronary Intervention for ST Elevation Myocardial Infarction. IJC Heart Vasc. 2015, 10, 8–12. [Google Scholar] [CrossRef]
- Harrison, R.W.; Aggarwal, A.; Ou, F.S.; Klein, L.W.; Rumsfeld, J.S.; Roe, M.T.; Wang, T.Y. American College of Cardiology National Cardiovascular Data Registry. Incidence and Outcomes of No-Reflow Phenomenon during Percutaneous Coronary Intervention among Patients with Acute Myocardial Infarction. Am. J. Cardiol. 2013, 111, 178–184. [Google Scholar] [CrossRef]
- Fajar, J.K.; Heriansyah, T.; Rohman, M.S. The Predictors of No Reflow Phenomenon after Percutaneous Coronary Intervention in Patients with ST Elevation Myocardial Infarction: A Meta-Analysis. Indian Heart J. 2018, 70, S406–S418. [Google Scholar] [CrossRef]
- Sakakura, K.; Funayama, H.; Taniguchi, Y.; Tsurumaki, Y.; Yamamoto, K.; Matsumoto, M.; Wada, H.; Momomura, S.I.; Fujita, H. The Incidence of Slow Flow after Rotational Atherectomy of Calcified Coronary Arteries: A Randomized Study of Low Speed Versus High Speed. Catheter. Cardiovasc. Interv. 2017, 89, 832–840. [Google Scholar] [CrossRef]
- Assali, A.R.; Sdringola, S.; Ghani, M.; Denkats, A.E.; Yepes, A.; Hanna, G.P.; Schroth, G.; Fujise, K.; Anderson, H.V.; Smalling, R.W.; et al. Intracoronary Adenosine Administered during Percutaneous Intervention in Acute Myocardial Infarction and Reduction in the Incidence of “No Reflow” Phenomenon. Catheter. Cardiovasc. Interv. 2000, 51, 27–31. [Google Scholar] [CrossRef]
- Kim, M.C.; Cho, J.Y.; Jeong, H.C.; Lee, K.H.; Park, K.H.; Sim, D.S.; Yoon, N.S.; Youn, H.J.; Kim, K.H.; Hong, Y.J.; et al. Long-Term Clinical Outcomes of Transient and Persistent No Reflow Phenomena Following Percutaneous Coronary Intervention in Patients with Acute Myocardial Infarction. Korean Circ. J. 2016, 46, 490–498. [Google Scholar] [CrossRef]
- Tasar, O.; Karabay, A.K.; Oduncu, V.; Kirma, C. Predictors and Outcomes of No-Reflow Phenomenon in Patients with Acute ST-segment Elevation Myocardial Infarction Undergoing Primary Percutaneous Coronary Intervention. Coron. Artery Dis. 2019, 30, 270–276. [Google Scholar] [CrossRef]
- Resnic, F.S.; Wainstein, M.; Lee, M.K.; Behrendt, D.; Wainstein, R.V.; Ohno-Machado, L.; Kirshenbaum, J.M.; Rogers, C.D.; Popma, J.J.; Piana, R. No-reflow Is an Independent Predictor of Death and Myocardial Infarction After Percutaneous Coronary Intervention. Am. Heart J. 2003, 145, 42–46. [Google Scholar] [CrossRef] [PubMed]
- Berg, R.; Buhari, C. Treating and Preventing No Reflow in the Cardiac Catheterization Laboratory. Curr. Cardiol. Rev. 2012, 8, 209–214. [Google Scholar] [CrossRef] [PubMed]
- Morishima, I.; Sone, T.; Okumura, K.; Tsuboi, H.; Kondo, J.; Mukawa, H.; Matsui, H.; Toki, Y.; Ito, T.; Hayakawa, T. Angiographic No-Reflow Phenomenon as a Predictor of Adverse Long-Term Outcome in Patients Treated with Percutaneous Transluminal Coronary Angioplasty for First Acute Myocardial Infarction. J. Am. Coll. Cardiol. 2000, 36, 1202–1209. [Google Scholar] [CrossRef]
- Ito, H.; Maruyama, A.; Iwakura, K.; Takiuchi, S.; Masuyama, T.; Hori, M.; Higashino, Y.; Fujii, K.; Minamino, T. Clinical Implications of the ‘No Reflow’ Phenomenon. A Predictor of Complications and Left Ventricular Remodeling in Reperfused Anterior Wall Myocardial Infarction. Circulation 1996, 93, 223–228. [Google Scholar] [CrossRef] [PubMed]
- Ooi, E.; Tavella, R.; Arstall, M.; Chew, D.; Worthley, M.; Beltrame, J.; Zeitz, C. Incidence and outcomes of the no-reflow phenomenon during percutaneous coronary intervention: Insights from the CADOSA registry. Heart Lung Circ. 2015, 24, S279. [Google Scholar] [CrossRef]
- Gupta, S.; Gupta, M.M. No Reflow Phenomenon in Percutaneous Coronary Interventions in ST-segment Elevation Myocardial Infarction. Indian Heart J. 2016, 68, 539–551. [Google Scholar] [CrossRef]
- Papapostolou, S.; Andrianopoulos, N.; Duffy, S.J.; Brennan, A.L.; Ajani, A.E.; Clark, D.J.; Reid, C.M.; Freeman, M.; Sebastian, M.; Selkrig, L.; et al. Long-term Clinical Outcomes of Transient and Persistent No-Reflow Following Percutaneous Coronary Intervention (PCI): A Multicentre Australian Registry. EuroIntervention 2018, 14, 185–193. [Google Scholar] [CrossRef]
- World Medical Association declaration of Helsinki. Recommendations guiding physicians in biomedical research involving human subjects. JAMA 1997, 277, 925–926. [Google Scholar] [CrossRef]
- Thygesen, K.; Alpert, J.S.; Jaffe, A.S.; Chaitman, B.R.; Bax, J.J.; Morrow, D.A.; White, H.D.; ESC Scientific Document Group. Fourth universal definition of myocardial infarction (2018). Eur. Heart J. 2019, 40, 237–269. [Google Scholar] [CrossRef]
- Lee, A.S.; William, S.G.; John, J. TIMI Grade Flow. 2020. Available online: https://www.ncbi.nlm.nih.gov/books/NBK482412/ (accessed on 8 June 2020).
- Eitel, I.; Wöhrle, J.; Suenkel, H.; Meissner, J.; Kerber, S.; Lauer, B.; Pauschinger, M.; Birkemeyer, R.; Axthelm, C.; Zimmermann, R.; et al. Intracoronary Compared with Intravenous Bolus Abciximab Application During Primary Percutaneous Coronary Intervention in ST-Segment Elevation Myocardial Infarction: Cardiac Magnetic Resonance Substudy of the AIDA STEMI Trial. J. Am. Coll. Cardiol. 2013, 61, 1447–1454. [Google Scholar] [CrossRef]
- Hof, A.W.J.v.t.; Liem, A.; Suryapranata, H.; Hoorntje, J.C.A.; Boer, M.-J.d.; Zijlstra, F. Angiographic Assessment of Myocardial Reperfusion in Patients Treated with Primary Angioplasty for Acute Myocardial Infarction. Circulation 1998, 97, 2302–2306. [Google Scholar]
- Neumann, F.J.; Sousa-Uva, M.; Ahlsson, A.; Alfonso, F.; Banning, A.P.; Benedetto, U.; Byrne, R.A.; Collet, J.P.; Falk, V.; Head, S.J.; et al. 2018 ESC/EACTS Guidelines on Myocardial Revascularization. Eur. Heart J. 2019, 40, 87–165. [Google Scholar] [CrossRef] [PubMed]
- Priori, S.G.; Blomström-Lundqvist, C.; Mazzanti, A.; Blom, N.; Borggrefe, M.; Camm, J.; Elliott, P.M.; Fitzsimons, D.; Hatala, R.; Hindricks, G.; et al. 2015 ESC Guidelines for the Management of Patients with Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death: The Task Force for the Management of Patients with Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death of the European Society of Cardiology (ESC). Endorsed By: Association for European Paediatric and Congenital Cardiology (AEPC). Eur. Heart J. 2015, 36, 2793–2867. [Google Scholar] [PubMed]
- Werdan, K.; Russ, M.; Buerke, M.; Prondzinsky, R.; Dietz, S. Evidence-based Management of Cardiogenic Shock after Acute Myocardial Infarction. Interv. Cardiol. 2013, 8, 73–80. [Google Scholar] [CrossRef] [PubMed]
- Nair Rajesh, G.; Jayaprasad, N.; Madhavan, S.; Sudha Kumary, V.; Jayaprakash, K.; Raihanathul Misiriya, K.J.; Jayaprakash, V.L.; George, R. Predictors and Prognosis of No-Reflow during Primary Percutaneous Coronary Intervention. Bayl. Univ. Med. Cent. Proc. 2018, 32, 30–33. [Google Scholar] [CrossRef]
- Ndrepepa, G.; Tiroch, K.; Fusaro, M.; Keta, D.; Seyfarth, M.; Byrne, R.A.; Pache, J.; Alger, P.; Mehilli, J.; Schömig, A.; et al. 5-year Prognostic Value of No-Reflow Phenomenon After Percutaneous Coronary Intervention in Patients with Acute Myocardial Infarction. J. Am. Coll. Cardiol. 2010, 55, 2383–2389. [Google Scholar] [CrossRef]
- Rivera-Linares, B.M.; Bedolla-Barajas, M.; Morales-Romero, J.; Jiménez-Gómez, J.E. Predictors of No-Reflow Phenomenon after Primary Percutaneous Coronary Intervention. Rev. Med. Inst. Mex. Seguro Soc. 2014, 52, 522–529. [Google Scholar]
- Iwakura, K.; Ito, H.; Kawano, S.; Shintani, Y.; Yamamoto, K.; Kato, A.; Ikushima, M.; Tanaka, K.; Kitakaze, M.; Hori, M.; et al. Predictive Factors for Development of the No-Reflow Phenomenon in Patients with Reperfused Anterior Wall Acute Myocardial Infarction. J. Am. Coll. Cardiol. 2001, 38, 472–477. [Google Scholar] [CrossRef]
- Ndrepepa, G.; Tiroch, K.; Keta, D.; Fusaro, M.; Seyfarth, M.; Pache, J.; Mehilli, J.; Schömig, A.; Kastrati, A. Predictive Factors and Impact of No Reflow after Primary Percutaneous Coronary Intervention in Patients With Acute Myocardial Infarction. Circ. Cardiovasc. Interv. 2010, 3, 27–33. [Google Scholar] [CrossRef]
- Cenko, E.; Ricci, B.; Kedev, S.; Kalpak, O.; Câlmâc, L.; Vasiljevic, Z.; Knežević, B.; Dilic, M.; Miličić, D.; Manfrini, O.; et al. The No-Reflow Phenomenon in the Young and in the Elderly. Int. J. Cardiol. 2016, 222, 1122–1128. [Google Scholar] [CrossRef]
- Michael, M.; Breall, J.A. No-Reflow Phenomenon during PCI. Available online: https://www.dicardiology.com/article/no-reflow-phenomenon-during-pci (accessed on 3 September 2020).
- Ito, H. Etiology and Clinical Implications of Microvascular Dysfunction in Patients with Acute Myocardial Infarction. Int. Heart J. 2014, 55, 185–189. [Google Scholar] [CrossRef] [PubMed]
- Choo, E.H.; Kim, P.J.; Chang, K.; Ahn, Y.; Jeon, D.S.; Lee, J.M.; Kim, D.B.; Her, S.H.; Park, C.S.; Kim, H.Y.; et al. The Impact of No-Reflow Phenomena after Primary Percutaneous Coronary Intervention: A Time-Dependent Analysis of Mortality. Coron. Artery Dis. 2014, 25, 392–398. [Google Scholar] [CrossRef] [PubMed]
- Gagliardi, J.; Szarfer, J.; Travetto, C.; Escudero, A.G.; Gigena, G.; Rodriguez, A.; Alonso, A.; Blanco, R.; Blanco, F.S.; Sarmiento, R.A.; et al. Clinical Predictors of No-Reflow in Percutaneous Coronary Intervention for Acute Myocardial Infarction. Rev. Argent. Cardiol. 2013, 81, 240–245. [Google Scholar] [CrossRef]
- Zijlstra, F. Acute Myocardial Infarction: Primary Angioplasty. Heart 2001, 85, 705–709. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ito, H. No Reflow Phenomenon in Coronary Heart Disease. J. Cardiol. 2001, 37, 39–42. [Google Scholar] [PubMed]
- Vesa, C.M.; Popa, L.; Popa, A.R.; Rus, M.; Zaha, A.A.; Bungau, S.; Tit, D.M.; Corb Aron, R.A.; Zaha, D.C. Current Data Regarding the Relationship between Type 2 Diabetes Mellitus and Cardiovascular Risk Factors. Diagnostics 2020, 10, 314. [Google Scholar] [CrossRef]
- Stoicescu, M.; Csepento, C.; Muţiu, G.; Bungău, S. The Role of Increased Plasmatic Renin Level in the Pathogenesis of Arterial Hypertension in Young Adults. Rom. J. Morphol. Embryol. 2011, 52, 419–423. [Google Scholar]
- Moisi, M.; Vesa, C.M.; Bungau, S.; Tit, D.M.; Corb Aron, R.A.; Bratu, O.; Diaconu, C.C.; Rus, M.; Popescu, M.I. Acute kidney injury incidence and models for mortality prediction in acute coronary syndromes. Rom. J. Mil. Med. 2020, 113, 133–140. [Google Scholar]
- Moisi, M.I.; Rus, M.; Bungau, S.; Zaha, D.C.; Uivarosan, D.; Fratila, O.; Tit, D.M.; Endres, L.; Nistor-Cseppento, D.C.; Popescu, M.I. Acute Coronary Syndromes in Chronic Kidney Disease: Clinical and Therapeutic Characteristics. Medicina 2020, 56, 118. [Google Scholar] [CrossRef]
- Scarpone, M.; Cenko, E.; Manfrini, O. Coronary No-Reflow Phenomenon in Clinical Practice. Curr. Pharm. Des. 2018, 24, 2927–2933. [Google Scholar] [CrossRef]
- Kelbaek, H.; Terkelsen, C.J.; Helqvist, S.; Lassen, J.F.; Clemmensen, P.; Kløvgaard, L.; Kaltoft, A.; Engstrøm, T.; Bøtker, H.E.; Saunamäki, K.; et al. Randomized Comparison of Distal Protection Versus Conventional Treatment in Primary Percutaneous Coronary Intervention: The Drug Elution and Distal Protection in ST-elevation Myocardial Infarction (DEDICATION) Trial. J. Am. Coll. Cardiol. 2008, 51, 899–905. [Google Scholar] [CrossRef] [PubMed]
- Ramjane, K.; Han, L.; Jin, C. The Diagnosis and Treatment of the No-Reflow Phenomenon in Patients with Myocardial Infarction Undergoing Percutaneous Coronary Intervention. Exp. Clin. Cardiol. 2008, 13, 121–128. [Google Scholar] [PubMed]
- Jensen, L.O.; Maeng, M.; Thayssen, P.; Kaltoft, A.; Tilsted, H.H.; Bøttcher, M.; Lassen, J.F.; Hansen, K.N.; Krusell, L.R.; Rasmussen, K.; et al. Clinical Outcome after Primary Percutaneous Coronary Intervention with Drug-Eluting and Bare Metal Stents in Patients with ST-segment Elevation Myocardial Infarction. Circ. Cardiovasc. Interv. 2008, 1, 176–184. [Google Scholar] [CrossRef][Green Version]
- Levi, Y.; Sultan, A.; Alemayehu, M.; Wall, S.; Lavi, S. Association of Endothelial Dysfunction and No-Reflow during Primary Percutaneous Coronary Intervention for ST-elevation Myocardial Infarction. Cardiovasc. Revasc. Med. 2016, 17, 552–555. [Google Scholar] [CrossRef]
- Rezkalla, S.H.; Stankowski, R.V.; Hanna, J.; Kloner, R.A. Management of No-Reflow Phenomenon in the Catheterization Laboratory. JACC 2017, 10, 215–223. [Google Scholar] [CrossRef]
- Hamza, M.A.; Galal, A.; Suweilam, S.; Ismail, M. Local Intracoronary Eptifibatide versus Mechanical Aspiration in Patients with Acute ST-Elevation Myocardial Infarction. Int. J. Vasc. Med. 2014, 2014, 294065. [Google Scholar] [CrossRef] [PubMed]
- Piana, R.N.; Paik, G.Y.; Moscucci, M.; Cohen, D.J.; Gibson, C.M.; Kugelmass, A.D.; Carrozza, J.P., Jr.; Kuntz, R.E.; Baim, D.S. Incidence and treatment of ‘no-reflow’ after percutaneous coronary intervention. Circulation 1994, 89, 2514–2518. [Google Scholar] [CrossRef]
- Allencherril, J.; Jneid, H.; Atar, D.; Alam, M.; Levine, G.; Kloner, R.A.; Birnbaum, Y. Pathophysiology, Diagnosis, and Management of the No-Reflow Phenomenon. Cardiovasc. Drugs Ther. 2019, 33, 589–597. [Google Scholar] [CrossRef]
- Ndrepepa, G.; Alger, P.; Kufner, S.; Mehilli, J.; Schömig, A.; Kastrati, A. ST-segment Resolution After Primary Percutaneous Coronary Intervention in Patients with Acute ST-segment Elevation Myocardial Infarction. Cardiol. J. 2012, 19, 61–69. [Google Scholar] [CrossRef]
- Pineda, V.; Merino, X.; Gispert, S.; Mahía, P.; Garcia, B.; Domínguez-Oronoz, R. No-reflow Phenomenon in Cardiac MRI: Diagnosis and Clinical Implications. Am. J. Roentgenol. 2008, 191, 73–79. [Google Scholar] [CrossRef]
- Luo, A.K.; Wu, K.C. Imaging Microvascular Obstruction and Its Clinical Significance Following Acute Myocardial Infarction. Heart Fail. Rev. 2006, 11, 305–312. [Google Scholar] [CrossRef] [PubMed]
- van Kranenburg, M.; Magro, M.; Thiele, H.; de Waha, S.; Eitel, I.; Cochet, A.; Cottin, Y.; Atar, D.; Buser, P.; Wu, E.; et al. Prognostic Value of Microvascular Obstruction and Infarct Size, as Measured by CMR in STEMI Patients. JACC Cardiovasc. Imaging 2014, 7, 930–939. [Google Scholar] [CrossRef] [PubMed]


| Clinical and Angiographic Features | All Patients | NRP+ Group | NRP− Group | p Value | |||
|---|---|---|---|---|---|---|---|
| n = 656 | n = 96 | n = 560 | |||||
| No. | % | No. | % | No. | % | ||
| Clinical Features | |||||||
| Age (years) | |||||||
| <50 | 199 | 30.33 | 18 | 18.75 | 181 | 32.32 | * 0.008 |
| 51–70 | 278 | 42.38 | 43 | 44.79 | 235 | 41.96 | 0.603 |
| >70 | 179 | 27.29 | 35 | 36.45 | 144 | 25.71 | * 0.029 |
| Male | 432 | 65.85 | 64 | 66.6 | 368 | 65.71 | 0.857 |
| HBP | 448 | 68.29 | 70 | 72.91 | 378 | 67.5 | 0.294 |
| Diabetes | 187 | 28.5 | 42 | 43.75 | 145 | 25.89 | * <0.001 |
| Hyperlipidemia | 418 | 63.71 | 82 | 85 | 336 | 60 | * <0.001 |
| Smoking (current) | 289 | 44.05 | 56 | 58.33 | 233 | 41.6 | * 0.002 |
| Prior MI | 27 | 4.11 | 3 | 3.12 | 24 | 4.28 | 0.596 |
| Echocardiographic Features | |||||||
| LVEF at discharge (%) | |||||||
| lower EF ≤ 44 | 375 | 57.16 | 55 | 57.29 | 240 | 42.85 | * 0.009 |
| higher EF > 45 | 261 | 39.78 | 41 | 42.7 | 320 | 57.14 | * 0.009 |
| ECG Features | |||||||
| ST resolution (%) at 1 h after PCI | |||||||
| <50 | 560 | 85.36 | 0 | 0 | 560 | 85.36 | * <0.001 |
| >50–70 | 96 | 14.63 | 96 | 14.63 | 0 | 0 | * <0.001 |
| ST resolution (%) at discharge | |||||||
| <50 | 69 | 10.51 | 69 | 71.87 | 0 | 0 | * <0.0001 |
| >50–70 | 587 | 89.48 | 27 | 28.12 | 560 | 100 | * <0.0001 |
| Angiographic Features | |||||||
| Culprit artery | |||||||
| LAD | 351 | 53.5 | 64 | 66.6 | 287 | 51.25 | * 0.005 |
| RCA | 229 | 34.9 | 27 | 28.1 | 202 | 36.07 | 0.131 |
| LCX | 76 | 11.58 | 5 | 5.2 | 71 | 12.67 | 0.035 |
| Number of Affected Vessels | |||||||
| One vessel | 252 | 38.41 | 67 | 70 | 185 | 33 | * <0.0001 |
| Two vessels | 286 | 43.59 | 24 | 25 | 262 | 46.78 | * <0.0001 |
| Three vessels | 118 | 17.98 | 5 | 5 | 113 | 20.17 | * <0.0001 |
| Number of Stented Vessels | |||||||
| One | 543 | 82.77 | 87 | 90.62 | 456 | 81.42 | * 0.028 |
| Two | 113 | 17.22 | 9 | 9.37 | 104 | 18.57 | * 0.028 |
| Three | 0 | 0 | 0 | 0 | 0 | 0 | - |
| Number of Stents | |||||||
| One | 195 | 29.72 | 52 | 54.16 | 143 | 25.53 | * <0.0001 |
| Two | 363 | 55.33 | 35 | 36.45 | 328 | 58.57 | * <0.0001 |
| Three | 98 | 14.93 | 9 | 9.37 | 89 | 15.89 | 0.097 |
| Post PCI TIMI Flow | |||||||
| 0/1 | 37 | 5.64 | 37 | 38.54 | 0 | 0 | * <0.0001 |
| 2 | 29 | 4.42 | 29 | 30.2 | 0 | 0 | * <0.0001 |
| 3 | 590 | 89.93 | 30 | 3.12 | 560 | 100 | * <0.0001 |
| Post PCI MBG Flow | |||||||
| 0/1 | 30 | 4.57 | 30 | 31.25 | 0 | 0 | * <0.0001 |
| 2 | 15 | 2.28 | 15 | 15.62 | 0 | 0 | * <0.0001 |
| 3 | 611 | 93.14 | 51 | 53.12 | 560 | 100 | * <0.0001 |
| GPIIb/IIIa inhibitors | 66 | 10.06 | 66 | 68.75 | 0 | 0 | * <0.0001 |
| Time intervals | |||||||
| Symptom-to-device (min) | |||||||
| ≤720 | 561 | 85.51 | 71 | 73.95 | 490 | 87.5 | * <0.0001 |
| 60–120 | 214 | 32.62 | 24 | 25 | 190 | 33.92 | 0.418 |
| 180–240 | 181 | 27.59 | 21 | 21.87 | 160 | 28.57 | 0.603 |
| 300–480 | 107 | 16.31 | 17 | 17.7 | 90 | 16.07 | 0.263 |
| 540–720 | 59 | 8.99 | 9 | 9.37 | 50 | 8.92 | 0.529 |
| >720 | 95 | 14.48 | 25 | 26.04 | 70 | 12.5 | * <0.0001 |
| 780–1440 | 64 | 9.75 | 11 | 11.45 | 53 | 9.46 | * 0.004 |
| >1440 | 31 | 4.72 | 14 | 14.58 | 17 | 3.03 | * 0.004 |
| STC | 199 | 30.33 | 32 | 33.33 | 87 | 15.53 | * <0.0001 |
| Culprit Artery of the Patients Who Developed STC | |||||||
| Culprit artery | 119 | 18.14 | 32 | 4.87 | 87 | 15.53 | |
| LAD | 58 | 48.74 | 17 | 53.12 | 41 | 47.13 | 0.562 |
| RCA | 50 | 42.02 | 13 | 40.63 | 37 | 42.53 | 0.849 |
| LCX | 11 | 9.24 | 2 | 6.25 | 9 | 10.34 | 0.497 |
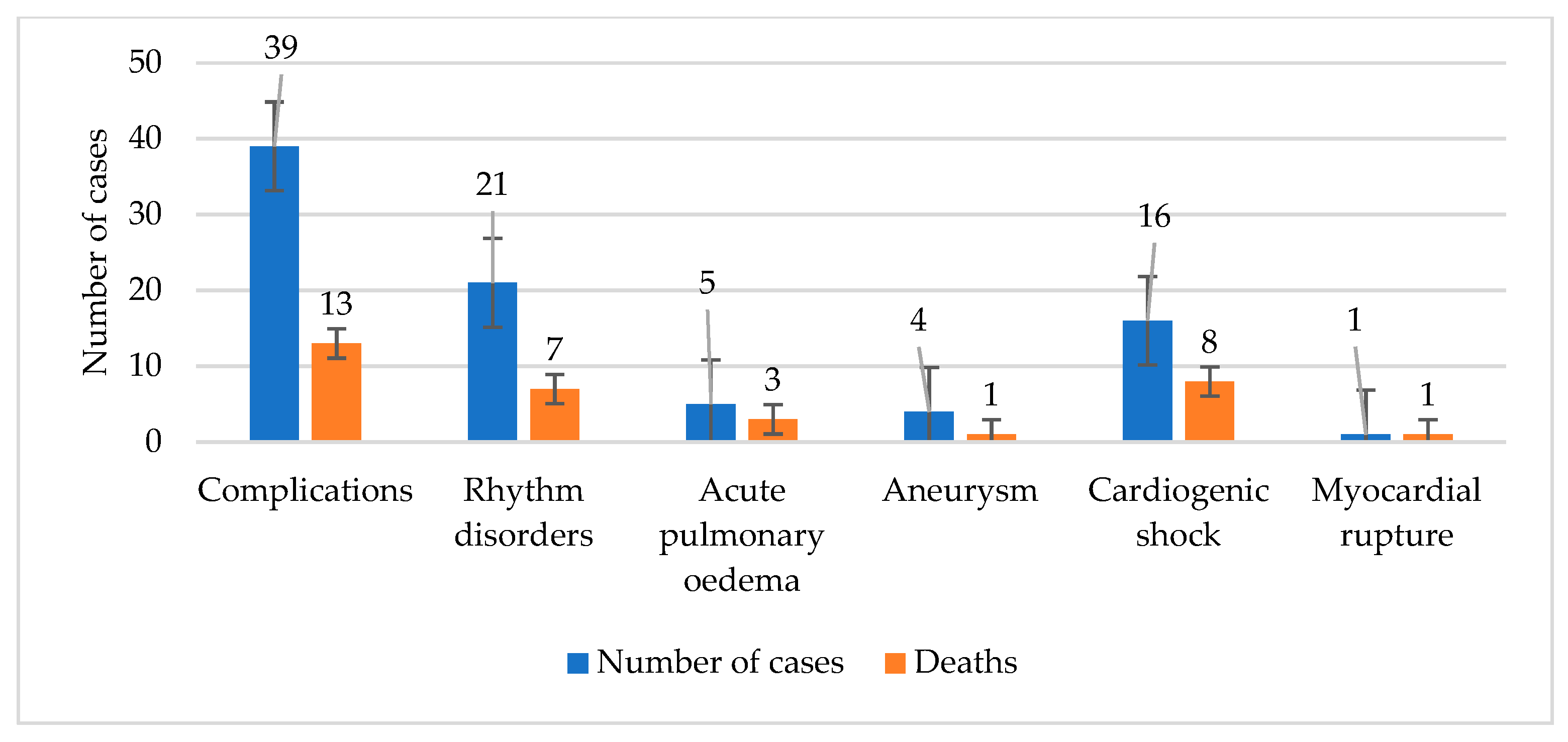
| Short-Term Complications | Group NRP+ n = 96 | Group NRP− n = 560 | p Value | ||
|---|---|---|---|---|---|
| No. | % | No. | % | ||
| Death | 14 | 14.58 | 25 | 4.46 | * <0.001 |
| All short-term complications | 32 | 33 | 87 | 15.53 | * <0.001 |
| Arrhythmias/conduction disorders | 14 | 43.75 | 38 | 43.68 | 0.992 |
| <12 h | 7 | 50 | 21 | 55.26 | 0.728 |
| 13–24 h | 2 | 14.29 | 4 | 10.53 | 0.704 |
| >24 h | 5 | 35.71 | 13 | 34.21 | 0.921 |
| Acute pulmonary edema | 5 | 15.63 | 17 | 19.54 | 0.624 |
| Aneurysm | 4 | 12.5 | 11 | 12.64 | 0.984 |
| Cardiogenic shock | 4 | 12.5 | 14 | 16.09 | 0.631 |
| Resuscitated cardiorespiratory arrest | 4 | 12.5 | 2 | 2.3 | * 0.024 |
| Myocardial rupture | 1 | 3.12 | 0 | 0 | 0.969 |
| Early stent thrombosis | 0 | 0 | 3 | 3.45 | 0.289 |
| Upper gastrointestinal bleeding | 0 | 0 | 2 | 2.30 | 0.389 |
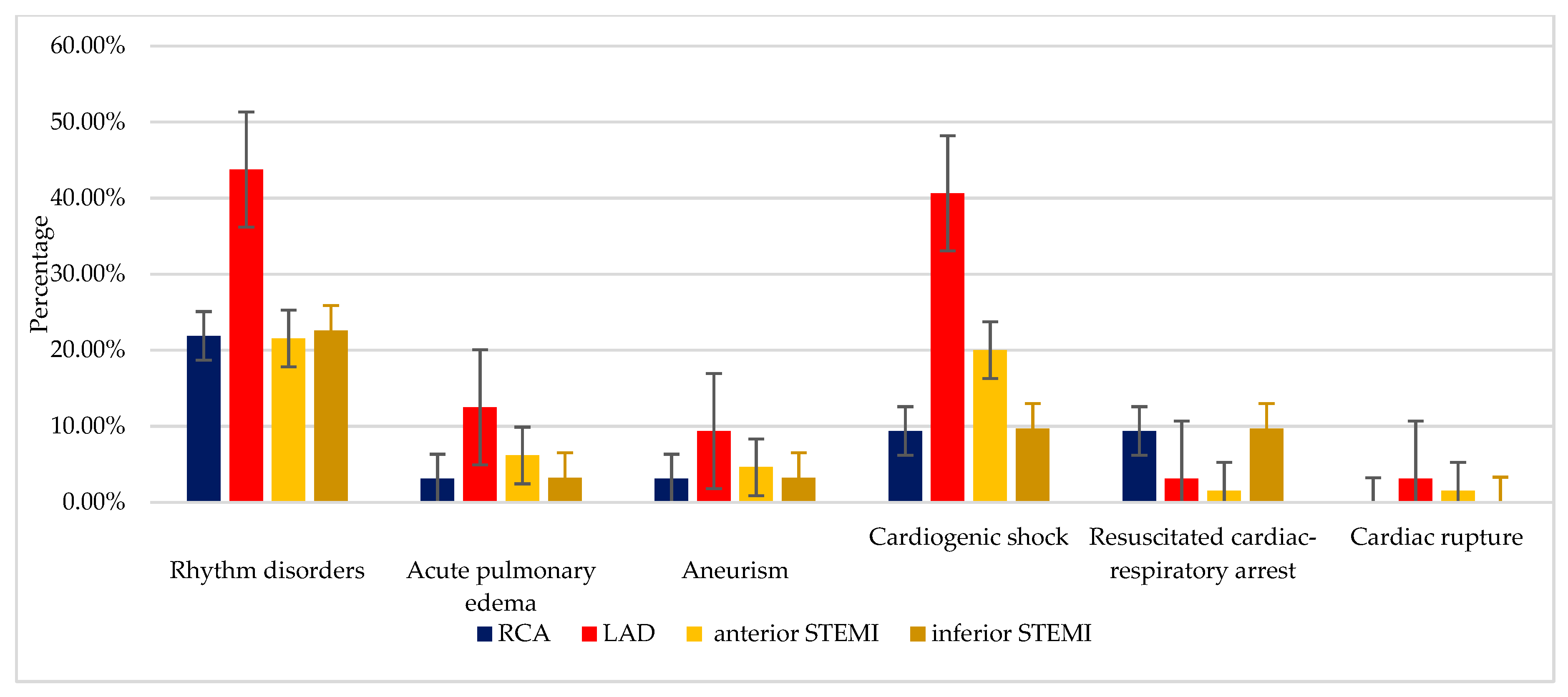
| Prevalence of Complications Depending on the Length of Time Elapsed Since the Onset of STEMI | ≤12 h (n = 71) | >12 h (n = 25) | 1 Stent (n = 52) | ≥2 Stents (n = 44) | ||||
|---|---|---|---|---|---|---|---|---|
| No. | % | No. | % | No. | % | No. | % | |
| Heart rhythm disorders | 14 | 19.72 | 7 | 28.00 | 7 | 13.46 | 14 | 31.82 |
| Acute pulmonary edema | 2 | 2.82 | 3 | 12.00 | 0 | 0.00 | 5 | 11.36 |
| Aneurysm | 2 | 2.82 | 2 | 8.00 | 3 | 5.77 | 1 | 2.27 |
| Cardiogenic shock | 9 | 12.68 | 7 | 28.00 | 7 | 13.46 | 9 | 20.45 |
| Resuscitated cardiac-respiratory arrest | 0 | 0 | 4 | 16.00 | 2 | 3.85 | 2 | 4.55 |
| Cardiac rupture | 0 | 0 | 1 | 4.00 | 1 | 1.92 | 0 | 0.00 |
| Prevalence of Complications Depending on the Artery Involved in STEMI | Risk Factor (The Risk Exposure) | |||
|---|---|---|---|---|
| Time (>12 h) | The Number of Stents (>1 Stent) | |||
| OR, 95% | p Value | OR, 95% | p Value | |
| Heart rhythm disorders | 0.4 | * 0.04 | ||
| Acute pulmonary edema | 0.1 | * 0.02 | ||
| Aneurism | 0.27 | 0.62 | ||
| Cardiogenic shock | 0.12 | 0.42 | ||
| Resuscitated cardiac-respiratory arrest | . | * 0.02 | 0.99 | |
| Cardiac rupture | . | 0.46 | 0.99 | |
| ANOVA Test | Sum of Squares | df | Mean Square | F Statistic | p Value |
|---|---|---|---|---|---|
| Regression | 10.143 | 1 | 10.143 | 35.773 | * <0.001 |
| Residual | 1.985 | 7 | 0.284 | ||
| Total | 12.128 | 8 | |||
| The independent variable is “Deaths”. | |||||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pantea-Roșan, L.R.; Pantea, V.A.; Bungau, S.; Tit, D.M.; Behl, T.; Vesa, C.M.; Bustea, C.; Moleriu, R.D.; Rus, M.; Popescu, M.I.; et al. No-Reflow after PPCI—A Predictor of Short-Term Outcomes in STEMI Patients. J. Clin. Med. 2020, 9, 2956. https://doi.org/10.3390/jcm9092956
Pantea-Roșan LR, Pantea VA, Bungau S, Tit DM, Behl T, Vesa CM, Bustea C, Moleriu RD, Rus M, Popescu MI, et al. No-Reflow after PPCI—A Predictor of Short-Term Outcomes in STEMI Patients. Journal of Clinical Medicine. 2020; 9(9):2956. https://doi.org/10.3390/jcm9092956
Chicago/Turabian StylePantea-Roșan, Larisa Renata, Vlad Alin Pantea, Simona Bungau, Delia Mirela Tit, Tapan Behl, Cosmin Mihai Vesa, Cristiana Bustea, Radu Dumitru Moleriu, Marius Rus, Mircea Ioachim Popescu, and et al. 2020. "No-Reflow after PPCI—A Predictor of Short-Term Outcomes in STEMI Patients" Journal of Clinical Medicine 9, no. 9: 2956. https://doi.org/10.3390/jcm9092956
APA StylePantea-Roșan, L. R., Pantea, V. A., Bungau, S., Tit, D. M., Behl, T., Vesa, C. M., Bustea, C., Moleriu, R. D., Rus, M., Popescu, M. I., Turi, V., & Diaconu, C. C. (2020). No-Reflow after PPCI—A Predictor of Short-Term Outcomes in STEMI Patients. Journal of Clinical Medicine, 9(9), 2956. https://doi.org/10.3390/jcm9092956













