Aorto-Iliac Artery Calcification Prior to Kidney Transplantation
Abstract
1. Introduction
2. Methods
2.1. Subjects and Study Design
2.2. Outcome Measures and Clinical Variables
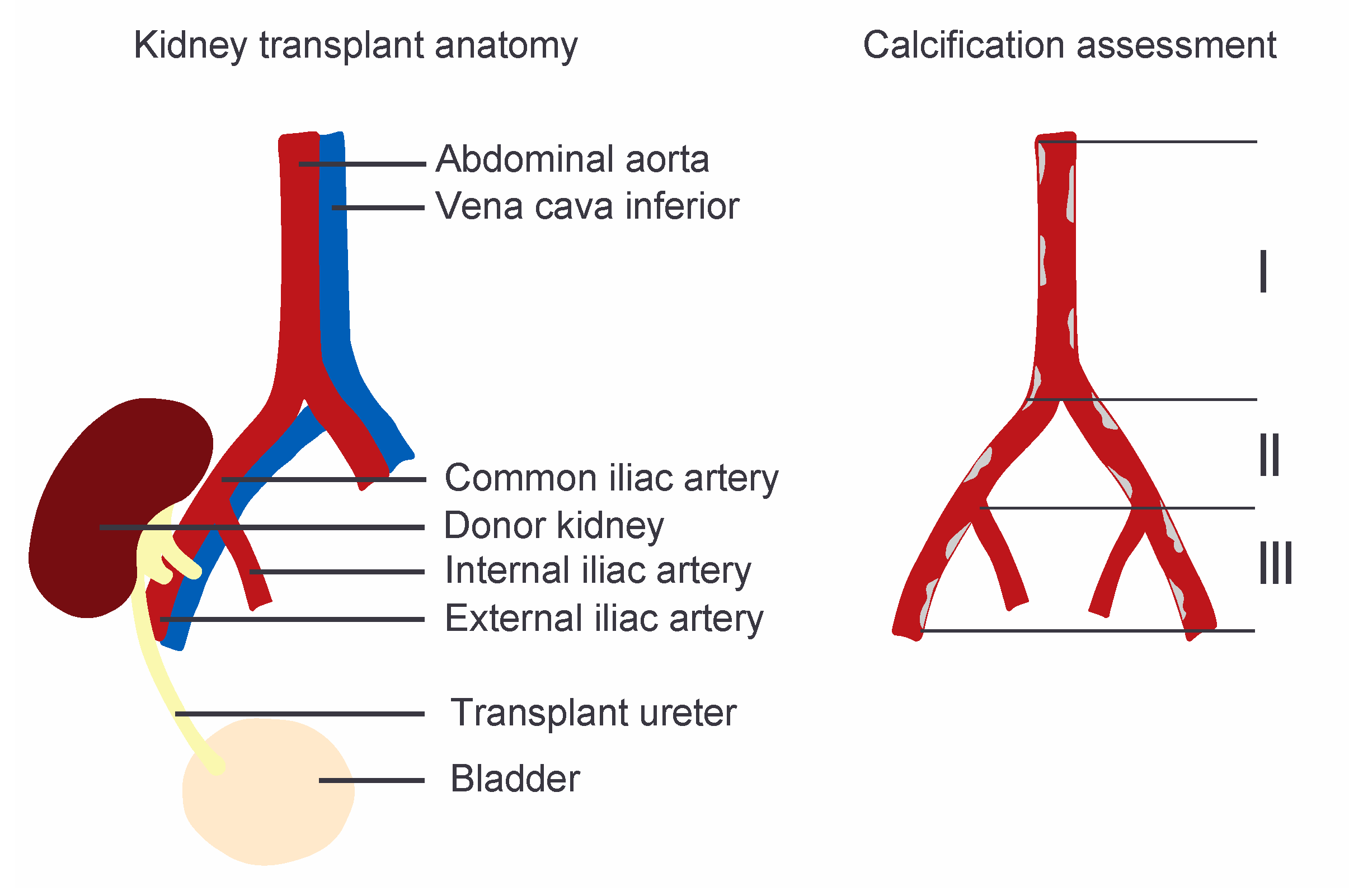
2.3. Quantification of Aorto-iliac Calcification
2.4. Statistical Analysis
3. Results
3.1. Study Population
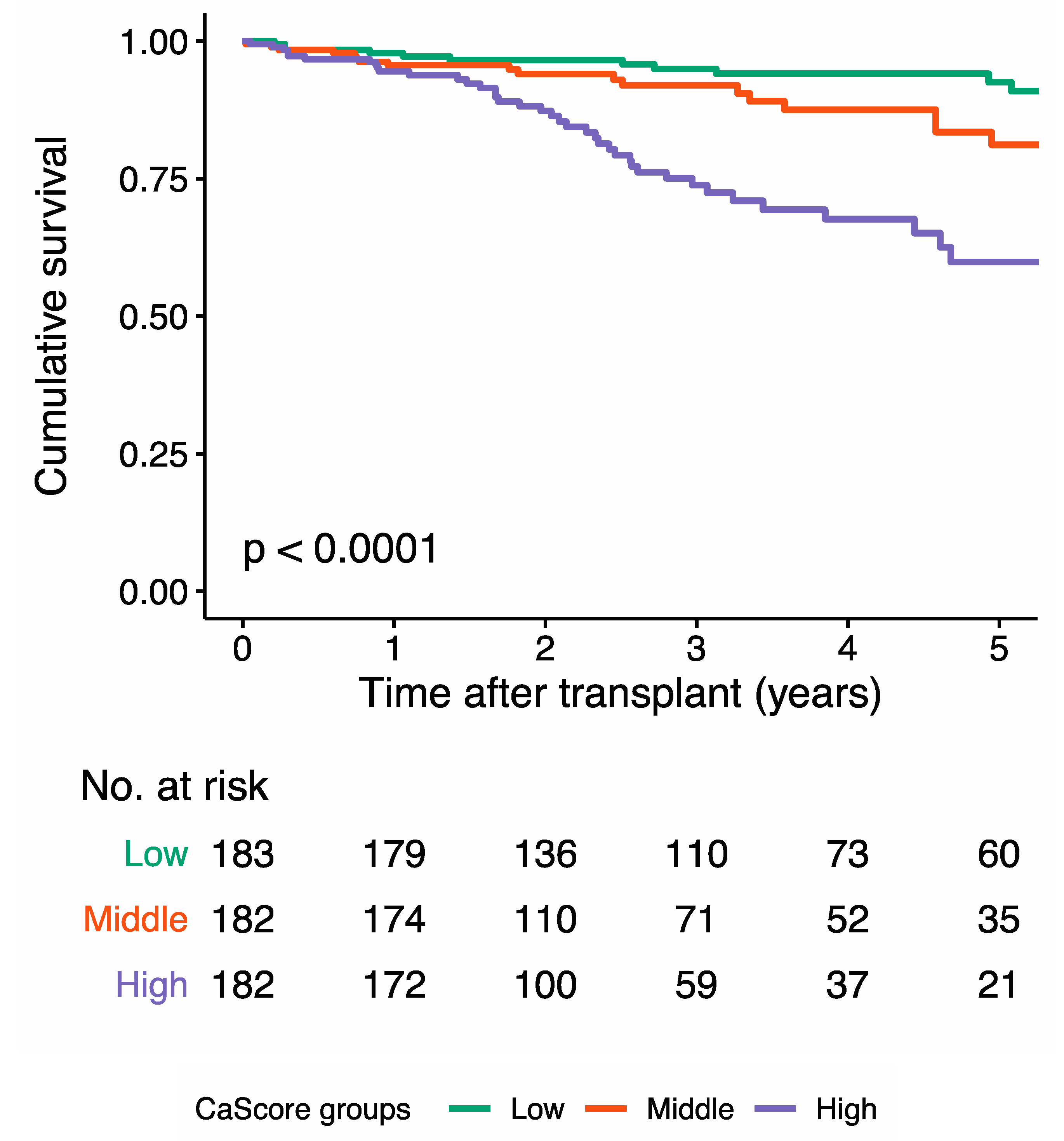
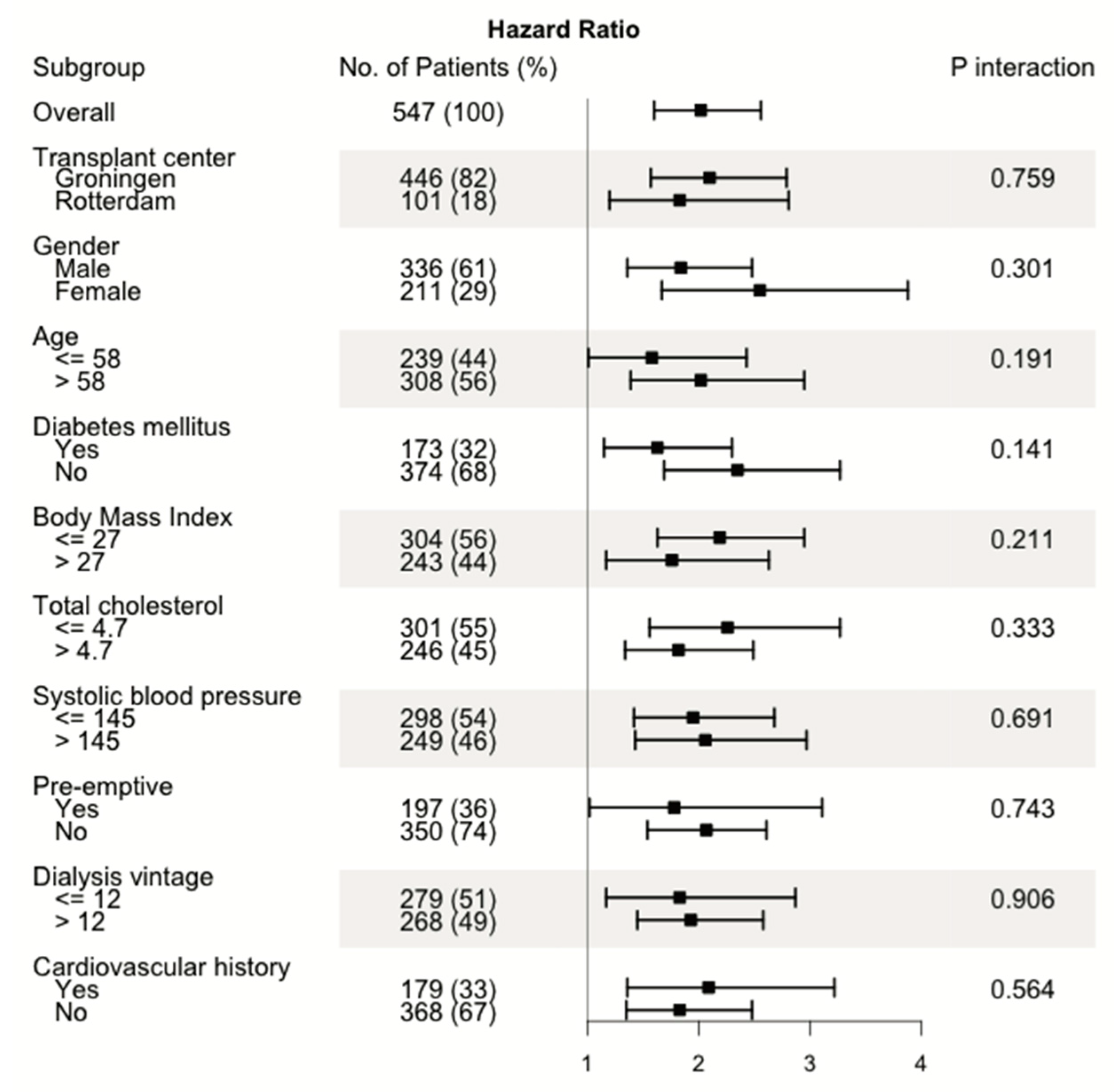
3.2. Aorto-Iliac CaScore and All-Cause Mortality
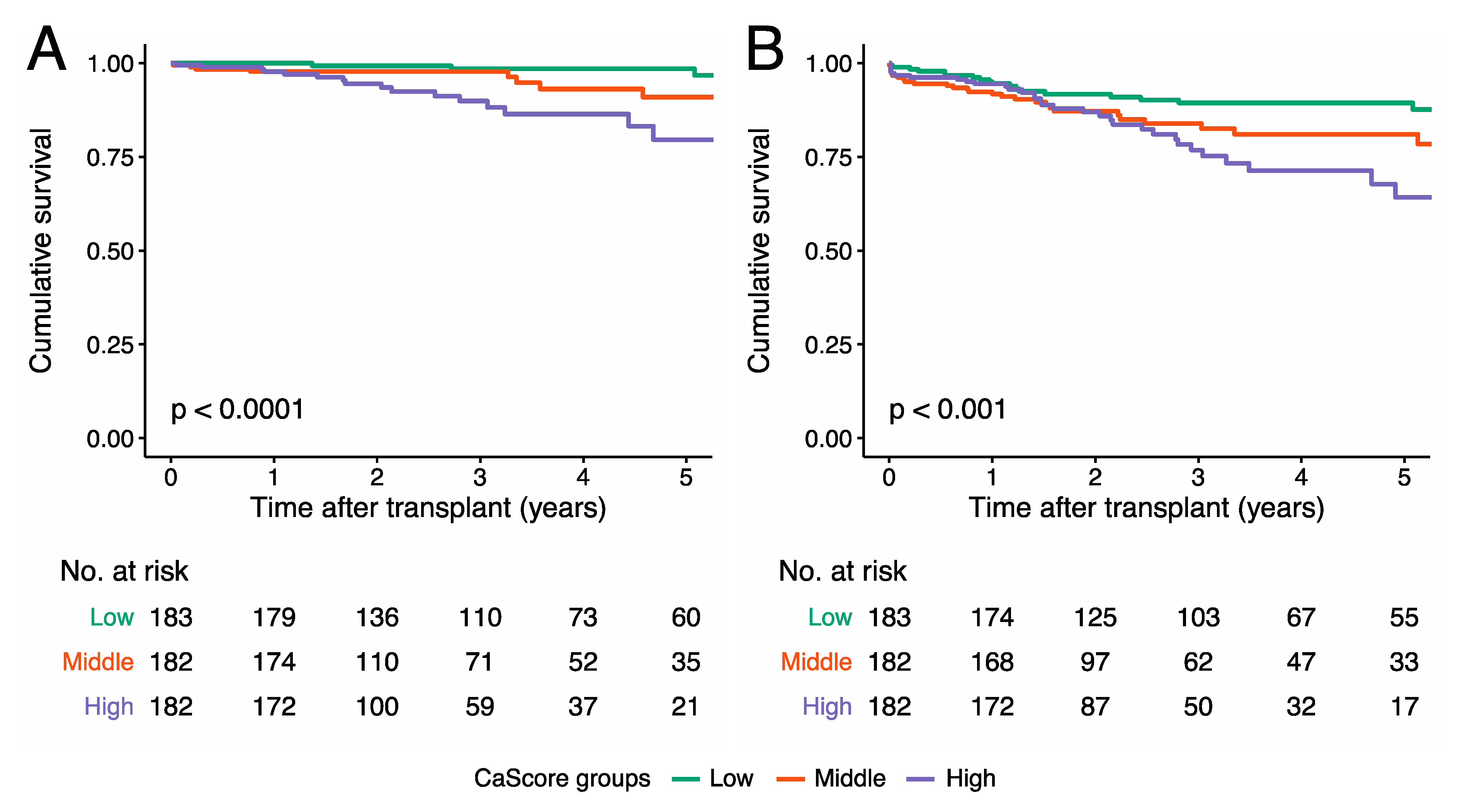
3.3. Aorto-iliac CaScore and Cardiovascular Mortality
3.4. Aorto-Iliac CaScore and Cardiovascular Events
3.5. Discriminative Capacity of the Aorto-iliac CaScore
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Tonelli, M.; Wiebe, N.; Knoll, G.; Bello, A.; Browne, S.; Jadhav, D.; Klarenbach, S.; Gill, J. Systematic review: Kidney transplantation compared with dialysis in clinically relevant outcomes. Arab. Archaeol. Epigr. 2011, 11, 2093–2109. [Google Scholar] [CrossRef] [PubMed]
- Rangaswami, J.; Mathew, R.O.; Parasuraman, R.; Tantisattamo, E.; Lubetzky, M.; Rao, S.; Yaqub, M.S.; Birdwell, K.A.; Bennett, W.; Dalal, P.; et al. Cardiovascular disease in the kidney transplant recipient: Epidemiology, diagnosis and management strategies. Nephrol. Dial. Transplant. 2019, 34, 760–773. [Google Scholar] [CrossRef] [PubMed]
- Harhay, M.N.; Rao, M.K.; Woodside, K.J.; Johansen, K.L.; Lentine, K.L.; Tullius, S.G.; Parsons, R.F.; Alhamad, T.; Berger, J.; Cheng, X.S.; et al. An overview of frailty in kidney transplantation: Measurement, management and future considerations. Nephrol. Dial. Transplant. 2020, 35, 1099–1112. [Google Scholar] [CrossRef] [PubMed]
- National Institute of Health; National Institute of Diabetes and Digestive and Kidney Diseases. United States Renal Data System 2017 USRDS Annual Data Report: Epidemiology of Kidney Disease in the United States; National Institute of Health: Bethesda, MD, USA, 2017. [Google Scholar]
- Hart, A.; Weir, M.R.; Kasiske, B.L. Cardiovascular risk assessment in kidney transplantation. Kidney Int. 2015, 87, 527–534. [Google Scholar] [CrossRef]
- Kulu, Y.; Fathi, P.; Golriz, M.; Khajeh, E.; Sabagh, M.; Ghamarnejad, O.; Mieth, M.; Ulrich, A.; Hackert, T.; Müller-Stich, B.P.; et al. Impact of surgeon’s experience on vascular and haemorrhagic complications after kidney transplantation. Eur. J. Vasc. Endovasc. Surg. 2019, 57, 139–149. [Google Scholar] [CrossRef]
- Matia, I.; Adamec, M.; Varga, M.; Janousek, L.; Lipar, K.; Viklický, O. Aortoiliac reconstruction with allograft and kidney transplantation as a one-stage procedure: Long term results. Eur. J. Vasc. Endovasc. Surg. 2008, 35, 353–357. [Google Scholar] [CrossRef]
- Silver, S.A.; Huang, M.; Nash, M.M.; Prasad, G.V.R. Framingham risk score and novel cardiovascular risk factors underpredict major adverse cardiac events in kidney transplant recipients. Transplantation 2011, 92, 183–189. [Google Scholar] [CrossRef]
- Sotomayor, C.G.; Benjamens, S.; Gomes-Neto, A.W.; Pol, R.A.; Groothof, D.; Velde-Keyzer, C.A.T.; Chong, G.; Glaudemans, A.W.J.M.; Berger, S.P.; Bakker, S.J.L.; et al. Bone mineral density and aortic calcification. Transplantation 2020, 1. [Google Scholar] [CrossRef]
- Manoushagian, S.; Meshkov, A. Evaluation of solid organ transplant candidates for coronary artery disease. Arab. Archaeol. Epigr. 2014, 14, 2228–2234. [Google Scholar] [CrossRef]
- Keyzer, C.A.; De Borst, M.H.; Berg, E.V.D.; Jahnen-Dechent, W.; Arampatzis, S.; Farese, S.; Bergmann, I.P.; Floege, J.; Navis, G.; Bakker, S.J.; et al. Calcification propensity and survival among renal transplant recipients. J. Am. Soc. Nephrol. 2015, 27, 239–248. [Google Scholar] [CrossRef]
- Benjamens, S.; Pol, R.A.; Glaudemans, A.W.J.M.; Wieringa, I.; Berger, S.P.; Bakker, S.; Slart, R.H.J.A. A high abdominal aortic calcification score by dual X-ray absorptiometry is associated with cardiovascular events after kidney transplantation. Nephrol. Dial. Transplant. 2018, 33, 2253–2259. [Google Scholar] [CrossRef] [PubMed]
- Rijkse, E.; Van Dam, J.L.; Roodnat, J.I.; Kimenai, H.J.A.N.; Ijzermans, J.N.M.; Minnee, R.C. The prognosis of kidney transplant recipients with aorto-iliac calcification: A systematic review and meta-analysis. Transpl. Int. 2020, 33, 483–496. [Google Scholar] [CrossRef] [PubMed]
- Maréchal, C.; Coche, E.; Goffin, E.; Dragean, A.; Schlieper, G.; Nguyen, P.; Floege, J.; Kanaan, N.; Devuyst, O.; Jadoul, M. Progression of coronary artery calcification and thoracic aorta calcification in kidney transplant recipients. Am. J. Kidney Dis. 2012, 59, 258–269. [Google Scholar] [CrossRef] [PubMed]
- Schankel, K.; Robinson, J.; Bloom, R.D.; Guerra, C.; Rader, D.; Joffe, M.; Rosas, S.E. Determinants of coronary artery calcification progression in renal transplant recipients. Arab. Archaeol. Epigr. 2007, 7, 2158–2164. [Google Scholar] [CrossRef] [PubMed]
- Deloach, S.S.; Joffe, M.M.; Mai, X.; Goral, S.; Rosas, S.E. Aortic calcification predicts cardiovascular events and all-cause mortality in renal transplantation. Nephrol. Dial. Transplant. 2008, 24, 1314–1319. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, P.T.; Henrard, S.; Coche, E.; Goffin, E.; Devuyst, O.; Jadoul, M. Coronary artery calcification: A strong predictor of cardiovascular events in renal transplant recipients. Nephrol. Dial. Transplant. 2010, 25, 3773–3778. [Google Scholar] [CrossRef] [PubMed]
- Roe, P.; Wolfe, M.; Joffe, M.; Rosas, S.E. Inflammation, coronary artery calcification and cardiovascular events in incident renal transplant recipients. Atherosclerosis 2010, 212, 589–594. [Google Scholar] [CrossRef]
- Aalten, J.; Dekker, H.M.; van der Vliet, J.A.; Hoitsma, A.J. Does a plain X-ray of the pelvis predict arterial complications in renal transplantation? A prospective study. Nephrol. Dial. Transplant. 2010, 26, 2007–2012. [Google Scholar] [CrossRef]
- Lewis, J.R.; Wong, G.; Taverniti, A.; Vucak-Dzumhur, M.; Elder, G.J. Association between aortic calcification, cardiovascular events, and mortality in kidney and pancreas-kidney transplant recipients. Am. J. Nephrol. 2019, 50, 177–186. [Google Scholar] [CrossRef]
- Claes, K.; Heye, S.; Bammens, B.; Kuypers, D.R.; Meijers, B.; Naesens, M.; Vanrenterghem, Y.; Evenepoel, P. Aortic calcifications and arterial stiffness as predictors of cardiovascular events in incident renal transplant recipients. Transpl. Int. 2013, 26, 973–981. [Google Scholar] [CrossRef]
- Rijkse, E.; Kimenai, H.J.; Roodnat, J.I.; Raa, S.T.; BijdeVaate, D.C.; van Dam, J.L.; Muller, K.; Ijzermans, J.N.; van der Zijden, M.A.; Minnee, R.C.; et al. Impact of aortoiliac stenosis on graft and patient survival in kidney transplant recipients using the tasc II classification. Transplantation 2019, 103, 2164–2172. [Google Scholar] [CrossRef] [PubMed]
- Davis, B.; Marin, D.; Hurwitz, L.M.; Ronald, J.; Ellis, M.J.; Ravindra, K.V.; Collins, B.H.; Kim, C.Y. Application of a novel ct-based iliac artery calcification scoring system for predicting renal transplant outcomes. Am. J. Roentgenol. 2016, 206, 436–441. [Google Scholar] [CrossRef] [PubMed]
- Chavent, B.; Maillard, N.; Boutet, C.; Albertini, J.-N.; Duprey, A.; Favre, J.-P. Prognostic value of aortoiliac calcification score in kidney transplantation recipients. Ann. Vasc. Surg. 2017, 44, 245–252. [Google Scholar] [CrossRef] [PubMed]
- Chadban, S.; Ahn, C.; Axelrod, D.A.; Foster, B.J.; Kasiske, B.L.; Kher, V.; Kumar, D.; Oberbauer, R.; Pascual, J.; Pilmore, H.L.; et al. Summary of the kidney disease. Transplantation 2020, 104, 708–714. [Google Scholar] [CrossRef]
- Benjamens, S.; Glaudemans, A.W.J.M.; Berger, S.P.; Slart, R.H.J.A.; Pol, R.A. Have we forgotten imaging prior to and after kidney transplantation? Eur. Radiol. 2018, 28, 3263–3267. [Google Scholar] [CrossRef]
- Saboo, S.S.; Abbara, S.; Rybicki, F.J.; Chatzizisis, Y.S. Quantification of aortic calcification—How and why should we do it? Atherosclerosis 2015, 240, 469–471. [Google Scholar] [CrossRef][Green Version]
- O’Connor, S.D.; Graffy, P.; Zea, R.; Pickhardt, P.J. Does nonenhanced ct-based quantification of abdominal aortic calcification outperform the framingham risk score in predicting cardiovascular events in asymptomatic adults? Radiology 2019, 290, 108–115. [Google Scholar] [CrossRef]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef]
- Ramos, L.F.; Shintani, A.; Ikizler, T.A.; Himmelfarb, J. Oxidative stress and inflammation are associated with adiposity in moderate to severe CKD. J. Am. Soc. Nephrol. 2008, 19, 593–599. [Google Scholar] [CrossRef]
- Hayashi, K.; Eguchi, S. The power-integrated discriminant improvement: An accurate measure of the incremental predictive value of additional biomarkers. Stat. Med. 2019, 38, 2589–2604. [Google Scholar] [CrossRef]
- van Dijk, M.; van Roon, A.M.; Said, M.Y.; Bemelman, F.J.; Homan van der Heide, J.J.; de Fijter, H.W.; de Vries, A.P.J.; Bakker, S.J.L.; Sanders, J.S.F. Long-term cardiovascular outcome of renal transplant recipients after early conversion to everolimus compared to calcineurin inhibition: Results from the randomized controlled MECANO trial. Transpl. Int. 2018, 31, 1380–1390. [Google Scholar] [CrossRef]
- Ghadri, J.R.; Goetti, R.; Fiechter, M.; Pazhenkottil, A.P.; Küest, S.M.; Nkoulou, R.N.; Windler, C.; Buechel, R.R.; Herzog, B.A.; Gaemperli, O.; et al. Inter-scan variability of coronary artery calcium scoring assessed on 64-multidetector computed tomography vs. dual-source computed tomography: A head-to-head comparison. Eur. Hear. J. 2011, 32, 1865–1874. [Google Scholar] [CrossRef] [PubMed]
- Mori, S.; Takaya, T.; Kinugasa, M.; Ito, T.; Takamine, S.; Fujiwara, S.; Nishii, T.; Kono, A.; Inoue, T.; Satomi-Kobayashi, S.; et al. Three-dimensional quantification and visualization of aortic calcification by multidetector-row computed tomography: A simple approach using a volume-rendering method. Atherosclerosis 2015, 239, 622–628. [Google Scholar] [CrossRef] [PubMed]
- Vittinghoff, E.; McCulloch, C.E. Relaxing the rule of ten events per variable in logistic and cox regression. Am. J. Epidemiology 2007, 165, 710–718. [Google Scholar] [CrossRef] [PubMed]
- Laging, M.; Gestel, J.A.K.-V.; van de Wetering, J.; Ijzermans, J.N.M.; Betjes, M.G.H.; Weimar, W.; Roodnat, J.I. A high comorbidity score should not be a contraindication for kidney transplantation. Transplantation 2016, 100, 400–406. [Google Scholar] [CrossRef]
| Variables | Total (n = 547) | Low (n = 183) | Medium (n = 182) | High (n = 182) | p-Value |
|---|---|---|---|---|---|
| Male gender a | 336 (61.4) | 98 (53.6) | 108 (57.8) | 131 (72.0) | 0.001d |
| Age, years c | 60 (51, 68) | 48 (39, 56) | 62 (55, 68) | 66 (60, 71) | <0.001e |
| Diabetes mellitus a | 173 (31.6) | 56 (30.6) | 61 (33.5) | 56 (30.8) | 0.798 d |
| Body Mass Index, kg/m2 b | 26.8 (4.7) | 26.0 (5.1) | 27.7 (4.6) | 26.7 (4.1) | 0.002e |
| Smoker a | <0.001d | ||||
| Non | 154 (28.2) | 74 (40.4) | 45 (24.7) | 35 (19.2) | |
| Former | 332 (60.7) | 89 (48.6) | 117 (64.3) | 126 (69.2) | |
| Current | 61 (11.2) | 20 (10.9) | 20 (11.0) | 21 (11.5) | |
| Total cholesterol, mmol/L b | 4.7 (1.3) | 4.7 (1.2) | 4.8 (1.5) | 4.5 (1.2) | 0.066 e |
| Hypercholesterolemia a | 153 (28.0) | 37 (20.2) | 59 (32.4) | 57 (31.3) | 0.016d |
| Systolic blood pressure, mmHg b | 145 (22) | 141 (20) | 145 (22) | 148 (24) | 0.014e |
| Diastolic blood pressure, mmHg b | 80 (14) | 82 (13) | 80 (13) | 78 (14) | 0.018e |
| Use of antihypertensive medication a | 439 (80.3) | 132 (72.1) | 150 (82.4) | 157 (86.3) | 0.002d |
| Type of donation a | 0.200 d | ||||
| Living-donation | 301 (55.0) | 110 (60.1) | 105 (57.7) | 86 (47.3) | |
| Donation after circulatory death | 128 (23.4) | 39 (21.3) | 36 (19.8) | 53 (29.1) | |
| Donation after brain death | 118 (21.6) | 34 (18.6) | 41 (22.5) | 43 (23.6) | |
| Previous transplants a | 0.161 d | ||||
| Non | 514 (94.0) | 167 (93.3) | 176 (96.7) | 171 (94.0) | |
| One | 22 (4.0) | 10 (5.5) | 4 (2.2) | 8 (4.4) | |
| Two | 11 (2.0) | 6 (3.3) | 2 (1.1) | 3 (1.6) | |
| Type of dialysis a | 0.196 d | ||||
| Pre-emptive | 197 (36.0) | 71 (38.8) | 71 (39.0) | 55 (30.2) | |
| Hemodialysis | 250 (45.7) | 77 (42.1) | 85 (46.7) | 88 (48.4) | |
| Peritoneal dialysis | 100 (18.3) | 36 (19.1) | 26 (14.3) | 39 (21.4) | |
| Dialysis vintage pre-transplantation, months c | 12 (0, 28) | 10 (0, 23) | 12 (0, 29) | 16 (0, 33) | 0.017f |
| History of MI a | 82 (15.0) | 9 (4.9) | 30 (16.5) | 43 (23.6) | <0.001d |
| History of CVA a | 40 (7.3) | 7 (3.8) | 11 (6.0) | 22 (12.1) | 0.007d |
| History of TIA a | 23 (4.2) | 4 (2.2) | 11 (6.0) | 8 (4.4) | 0.183 d |
| History of PAD a | 78 (14.3) | 18 (9.8) | 24 (13.2) | 36 (19.8) | 0.022d |
| Charlson Comorbidity Index b | 6.4 (2.5) | 5.1 (2.0) | 6.3 (1.9) | 7.7 (2.7) | <0.001e |
| Framingham score, % c | 9.6 (3.4, 18.8) | 3.5 (0.6, 9.5) | 10.2 (4.1, 20.2) | 16.6 (9.4, 23.8) | <0.001f |
| Variables | Total (n = 547) | Low (n = 183) | Medium (n = 182) | High (n = 182) | p-Value |
|---|---|---|---|---|---|
| Laboratory values a | |||||
| eGFR b | 51.3 (20.6) | 55.9 (22.2) | 50.2 (18.1) | 47.68 (20.82) | 0.001e |
| Calcium, mmol/L b | 2.43 (0.14) | 2.40 (0.14) | 2.45 (0.13) | 2.45 (0.14) | 0.001e |
| Phosphate, mmol/L b | 0.93 (0.21) | 0.94 (0.23) | 0.95 (0.19) | 0.89 (0.19) | 0.014e |
| Albumin, g/L b | 43.3 (3.1) | 43.2 (3.4) | 43.6 (2.9) | 43.0 (3.0) | 0.237 e |
| PTH, pmol/L c | 10.4 (7.4, 15.6) | 9.4 (6.5, 12.8) | 10.6 (7.8, 16.3) | 11.6 (8.0, 16.4) | 0.020f |
| CNI d | 535 (97.8) | 178 (97.3) | 179 (98.4) | 178 (97.8) | 0.779 g |
| Ciclosporin d | 42 (7.7) | 16 (8.7) | 13 (7.1) | 13 (7.1) | 0.803 g |
| Tacrolimus d | 494 (90.3) | 163 (89.1) | 166 (91.2) | 165 (90.7) | 0.773 g |
| Total (n = 547) | Low (n = 183) | Medium (n = 182) | High (n = 182) | p-Value | |
|---|---|---|---|---|---|
| Median follow-up, years | 3.1 (1.4, 5.2) | 3.6 (2.0, 6.0) | 2.6 (1.3, 4.9) | 2.7 (1.2, 4.2) | - |
| Mortality | |||||
| All-cause | 80 (14.7) | 14 (7.7) | 22 (12.1) | 44 (24.3) | <0.001 |
| Cardiovascular | 32 (5.9) | 4 (2.2) | 10 (5.5) | 18 (9.9) | 0.007 |
| Cardiovascular events | |||||
| MI | 46 (8.4) | 7 (3.8) | 17 (9.3) | 22 (12.1) | 0.015 |
| CVA | 16 (2.9) | 6 (3.3) | 7 (3.8) | 3 (1.6) | 0.434 |
| TIA | 2 (0.4) | 0 (0.0) | 0 (0.0) | 2 (1.1) | 0.134 |
| PAD | 30 (5.7) | 7 (3.8) | 9 (4.9) | 15 (8.2) | 0.166 |
| Combined | 84 (15.5) | 18 (9.8) | 30 (16.5) | 36 (19.8) | 0.027 |
| Low | Medium | High | Continuous | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Hazard Ratio | Hazard Ratio | 95% CI | Hazard Ratio | 95% CI | P (Trend) Value | Hazard Ratio | 95% CI | p-Value | |
| All-cause mortality | |||||||||
| Univariate | 1.0 (Ref) | 2.12 | 1.08–4.15 | 5.22 | 2.84–9.58 | <0.0001 | 2.02 | 1.59–2.56 | <0.0001 |
| Model 1 | 1.0 (Ref) | 2.20 | 1.12–4.32 | 5.45 | 2.94–10.07 | <0.0001 | 2.02 | 1.60–2.56 | <0.0001 |
| Model 2 | 1.0 (Ref) | 1.61 | 0.80–3.25 | 3.40 | 1.69–6.85 | <0.001 | 1.72 | 1.31–2.28 | <0.001 |
| Model 3 | 1.0 (Ref) | 1.39 | 0.67–2.88 | 3.31 | 1.60–6.87 | <0.001 | 1.75 | 1.31–2.33 | <0.001 |
| Model 4 | 1.0 (Ref) | 1.28 | 0.61–2.70 | 2.84 | 1.34–6.00 | 0.002 | 1.59 | 1.19–2.14 | 0.002 |
| Model 5 | 1.0 (Ref) | 1.27 | 0.60–2.66 | 2.59 | 1.22–5.51 | 0.006 | 1.53 | 1.14–2.06 | 0.005 |
| Model 6 | 1.0 (Ref) | 1.50 | 0.64–3.51 | 3.12 | 1.34–7.26 | 0.006 | 1.72 | 1.22–2.43 | 0.002 |
| Cardiovascular mortality | |||||||||
| Univariate | 1.0 (Ref) | 3.42 | 1.07–10.91 | 7.86 | 2.63–23.47 | <0.0001 | 2.27 | 1.55–3.34 | <0.0001 |
| Model 1 | 1.0 (Ref) | 3.45 | 1.08–11.05 | 7.69 | 2.55–23.14 | <0.0001 | 2.24 | 1.53–3.29 | <0.0001 |
| Model 2 | 1.0 (Ref) | 2.40 | 0.72–8.00 | 4.66 | 1.38–15.74 | 0.009 | 1.94 | 1.24–3.04 | 0.004 |
| Model 3 | 1.0 (Ref) | 1.91 | 0.56–6.59 | 4.32 | 1.22–15.38 | 0.014 | 1.92 | 1.19–3.09 | 0.007 |
| Model 4 | 1.0 (Ref) | 1.65 | 0.47–5.74 | 4.40 | 1.19–16.24 | 0.013 | 2.03 | 1.20–3.42 | 0.008 |
| Model 5 | 1.0 (Ref) | 1.64 | 0.46–5.76 | 4.46 | 1.19–16.71 | 0.014 | 2.04 | 1.20–3.45 | 0.008 |
| Model 6 | 1.0 (Ref) | 2.30 | 0.64–8.32 | 55.67 | 1.68–8.32 | 0.004 | 2.13 | 1.32–3.43 | 0.002 |
| Cardiovascular events | |||||||||
| Univariate | 1.0 (Ref) | 2.13 | 1.19–3.84 | 2.86 | 1.62–5.08 | <0.001 | 1.56 | 1.25–1.95 | <0.0001 |
| Model 1 | 1.0 (Ref) | 2.20 | 1.22–3.98 | 2.61 | 1.46–4.64 | <0.001 | 1.60 | 1.28–1.99 | <0.0001 |
| Model 2 | 1.0 (Ref) | 1.88 | 1.00–3.53 | 2.45 | 1.25–4.81 | 0.010 | 1.48 | 1.13–1.93 | 0.004 |
| Model 3 | 1.0 (Ref) | 1.69 | 0.89–3.20 | 2.58 | 1.20–4.77 | 0.013 | 1.48 | 1.12–1.94 | 0.005 |
| Model 4 | 1.0 (Ref) | 1.48 | 0.76–2.88 | 2.13 | 1.05–4.35 | 0.034 | 1.39 | 1.04–1.85 | 0.025 |
| Model 5 | 1.0 (Ref) | 1.47 | 0.76–2.85 | 1.98 | 0.97–4.07 | 0.060 | 1.35 | 1.01–1.80 | 0.042 |
| Model 6 | 1.0 (Ref) | 1.47 | 0.76–2.87 | 2.17 | 1.08–4.37 | 0.028 | 1.45 | 1.09–1.92 | 0.010 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Benjamens, S.; Rijkse, E.; te Velde-Keyzer, C.A.; Berger, S.P.; Moers, C.; de Borst, M.H.; Yakar, D.; Slart, R.H.J.A.; Dor, F.J.M.F.; Minnee, R.C.; et al. Aorto-Iliac Artery Calcification Prior to Kidney Transplantation. J. Clin. Med. 2020, 9, 2893. https://doi.org/10.3390/jcm9092893
Benjamens S, Rijkse E, te Velde-Keyzer CA, Berger SP, Moers C, de Borst MH, Yakar D, Slart RHJA, Dor FJMF, Minnee RC, et al. Aorto-Iliac Artery Calcification Prior to Kidney Transplantation. Journal of Clinical Medicine. 2020; 9(9):2893. https://doi.org/10.3390/jcm9092893
Chicago/Turabian StyleBenjamens, Stan, Elsaline Rijkse, Charlotte A. te Velde-Keyzer, Stefan P. Berger, Cyril Moers, Martin H. de Borst, Derya Yakar, Riemer H. J. A. Slart, Frank J. M. F. Dor, Robert C. Minnee, and et al. 2020. "Aorto-Iliac Artery Calcification Prior to Kidney Transplantation" Journal of Clinical Medicine 9, no. 9: 2893. https://doi.org/10.3390/jcm9092893
APA StyleBenjamens, S., Rijkse, E., te Velde-Keyzer, C. A., Berger, S. P., Moers, C., de Borst, M. H., Yakar, D., Slart, R. H. J. A., Dor, F. J. M. F., Minnee, R. C., & Pol, R. A. (2020). Aorto-Iliac Artery Calcification Prior to Kidney Transplantation. Journal of Clinical Medicine, 9(9), 2893. https://doi.org/10.3390/jcm9092893











