Systemic Inflammatory Response and Outcomes in Community-Acquired Pneumonia Patients Categorized According to the Smoking Habit or Presence of Chronic Obstructive Pulmonary Disease
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design, Patients Enrolled and Definitions
2.2. Measurements at Admission
2.3. Outcomes
2.4. Statistical Analysis
3. Results
3.1. General, Clinical, and Microbiological Characteristics
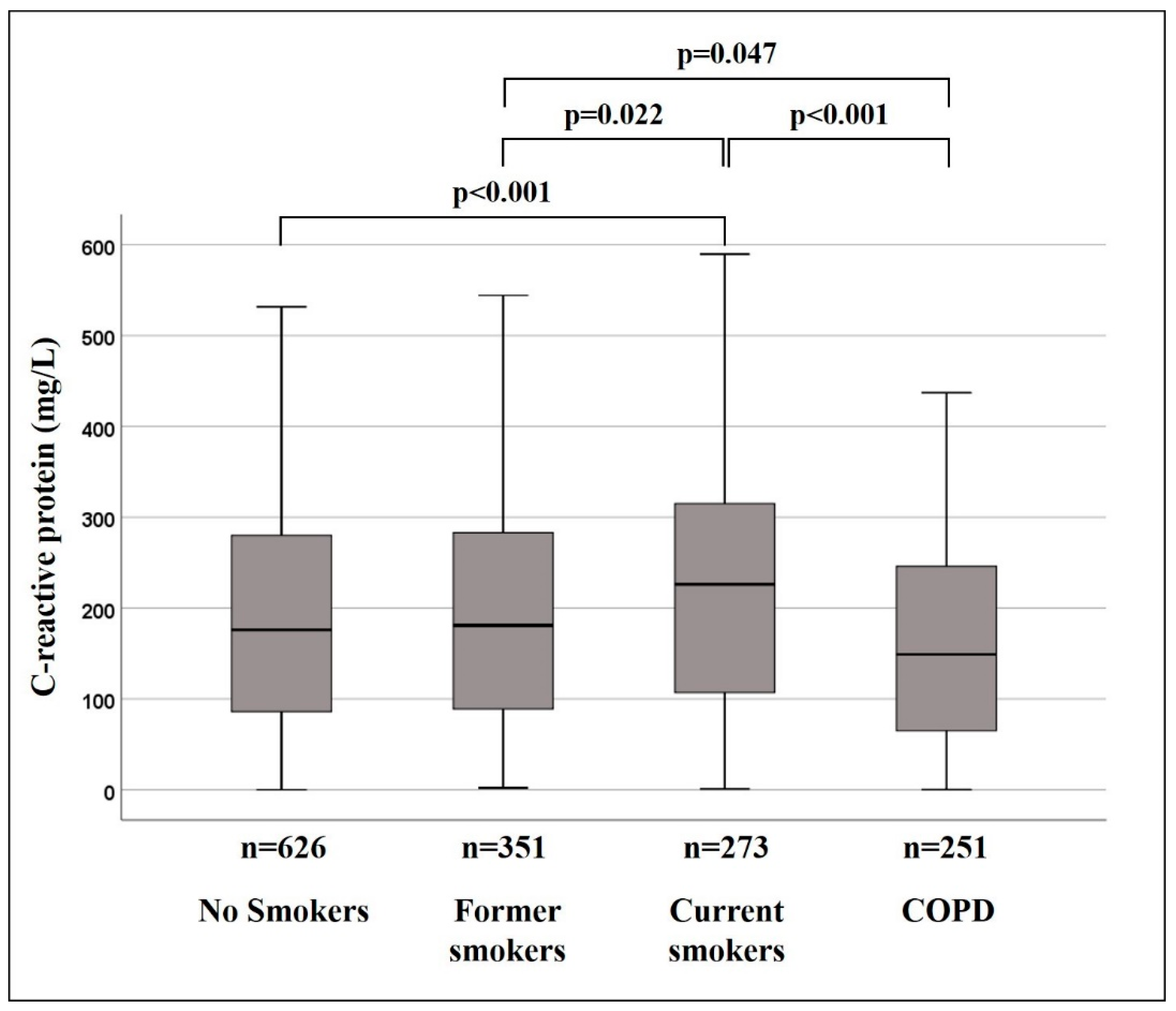
3.2. Systemic Inflammatory Response
3.3. Pleural Complications
3.4. Other Outcomes
4. Discussion
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Prina, E.; Ranzani, O.T.; Torres, A. Community-acquired pneumonia. Lancet 2015, 386, 1097–1108. [Google Scholar] [CrossRef]
- Zobel, K.; Martus, P.; Pletz, M.W.; Ewig, S.; Prediger, M.; Welte, T.; Bühling, F. CAPNETZ study group. Interleukin 6, lipopolysaccharide-binding protein and interleukin 10 in the prediction of risk and etiologic patterns in patients with community-acquired pneumonia: Results from the German competence network CAPNETZ. BMC Pulm. Med. 2012, 12, 6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Menéndez, R.; Martinez, R.; Reyes, S.; Mensa, J.; Polverino, E.; Filella, X.; Esquinas, C.; Martinez, A.; Ramirez, P.; Torres, A. Stability in community-acquired pneumonia: One step forward with markers? Thorax 2009, 64, 987–992. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Menéndez, R.; Cavalcanti, M.; Reyes, S. Markers of treatment failure in hospitalised community acquired pneumonia. Thorax 2008, 63, 447–452. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Menéndez, R.; Martínez, R.; Reyes, S.; Mensa, J.; Filella, X.; Marcos, M.A.; Martínez, A.; Esquinas, C.; Ramirez, P.; Torres, A. Biomarkers improve mortality prediction by prognostic scales in community-acquired pneumonia. Thorax 2009, 64, 587–591. [Google Scholar] [CrossRef] [Green Version]
- Pepys, M.B.; Hirschfield, G.M. C-reactive protein: A critical update. J. Clin. Investig. 2003, 111, 1805–1812. [Google Scholar] [CrossRef]
- Crisafulli, E.; Menéndez, R.; Huerta, A. Systemic inflammatory pattern of patients with community-acquired pneumonia with without, C.O.P.D. Chest 2013, 143, 1009–1017. [Google Scholar] [CrossRef]
- Huerta, A.; Crisafulli, E.; Menéndez, R. Pneumonic and nonpneumonic exacerbations of COPD: Inflammatory response and clinical characteristics. Chest 2013, 144, 1134–1142. [Google Scholar] [CrossRef] [Green Version]
- Gutierrez, P.; Closa, D.; Piñer, R.; Bulbena, O.; Menéndez, R.; Torres, A. Macrophage activation in exacerbated COPD with and without community-acquired pneumonia. Eur. Respir. J. 2010, 36, 285–291. [Google Scholar] [CrossRef] [Green Version]
- Taylor, A.E.; Finney-Hayward, T.K.; Quint, J.K. Defective macrophage phagocytosis of bacteria in, C.O.P.D. Eur. Respir. J. 2010, 35, 1039–1047. [Google Scholar] [CrossRef] [Green Version]
- Lim, W.S.; van der Eerden, M.M.; Laing, R. Defining community acquired pneumonia severity on presentation to hospital: An international derivation and validation study. Thorax 2003, 58, 377–382. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Torres, A.; Blasi, F.; Dartois, N.; Akova, M. Which individuals are at increased risk of pneumococcal disease and why? Impact of COPD, asthma, smoking, diabetes, and/or chronic heart disease on community-acquired pneumonia and invasive pneumococcal disease. Thorax 2015, 70, 984–989. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liapikou, A.; Polverino, E.; Ewig, S.; Cillóniz, C.; Marcos, M.A.; Mensa, J.; Bello, S.; Martin-Loeches, I.; Menéndez, R.; Torres, A. Severity and outcomes of hospitalised community-acquired pneumonia in COPD patients. Eur. Respir J. 2012, 39, 855–861. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bonnesen, B.; Baunbæk Egelund, G.; Vestergaard Jensen, A. Is chronic obstructive pulmonary disease a risk factor for death in patients with community acquired pneumonia? Infect. Dis. 2019, 51, 340–347. [Google Scholar] [CrossRef] [PubMed]
- Molinos, L.; Clemente, M.G.; Miranda, B.; ASTURPAR Group. Community-acquired pneumonia in patients with and without chronic obstructive pulmonary disease. J. Infect. 2009, 58, 417–424. [Google Scholar] [CrossRef] [PubMed]
- Jiang, H.L.; Chen, H.X.; Liu, W.; Fan, T.; Liu, G.J.; Mao, B. Is COPD associated with increased mortality and morbidity in hospitalized pneumonia? A systematic review and meta-analysis. Respirology 2015, 20, 1046–1054. [Google Scholar] [CrossRef] [PubMed]
- Naucler, P.; Darenberg, J.; Morfeldt, E.; Ortqvist, A.; Henriques Normark, B. Contribution of host, bacterial factors and antibiotic treatment to mortality in adult patients with bacteraemic pneumococcal pneumonia. Thorax 2013, 68, 571–579. [Google Scholar] [CrossRef] [Green Version]
- Garau, J.; Baquero, F.; Pérez-Trallero, E. NACER Group. Factors impacting on length of stay and mortality of community-acquired pneumonia. Clin. Microbiol. Infect. 2008, 14, 322–329. [Google Scholar] [CrossRef] [Green Version]
- Katanoda, K.; Marugame, T.; Saika, K. Population attributable fraction of mortality associated with tobacco smoking in Japan: A pooled analysis of three large-scale cohort studies. J. Epidemiol. 2008, 18, 251–264. [Google Scholar] [CrossRef] [Green Version]
- Cillóniz, C.; Polverino, E.; Ewig, S. Impact of age and comorbidity on cause and outcome in community-acquired pneumonia. Chest 2013, 144, 999–1007. [Google Scholar] [CrossRef]
- Bello, S.; Menéndez, R.; Torres, A.; Reyes, S.; Zalacain, R.; Capelastegui, A.; Aspa, J.; Borderías, L.; Martin-Villasclaras, J.J.; Alfageme, I.; et al. Tobacco smoking increases the risk for death from pneumococcal pneumonia. Chest 2014, 146, 1029–1037. [Google Scholar] [CrossRef] [PubMed]
- Baskaran, V.; Murray, R.L.; Hunter, A.; Lim, W.S.; McKeever, T.M. Effect of tobacco smoking on the risk of developing community acquired pneumonia: A systematic review and meta-analysis. PLoS ONE 2019, 14, e0220204. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Feldman, C.; Anderson, R. Cigarette smoking and mechanisms of susceptibility to infections of the respiratory tract and other organ systems. J. Infect. 2013, 67, 169–184. [Google Scholar] [CrossRef]
- Gaydos, J.; McNally, A.; Guo, R.; Vandivier, R.W.; Simonian, P.L.; Burnham, E.L. Alcohol abuse and smoking alter inflammatory mediator production by pulmonary and systemic immune cells. Am. J. Physiol. Lung. Cell. Mol. Physiol. 2016, 310, L507–L518. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, W.; Li, X.; Xu, J. Exposure to cigarette smoke downregulates β2-adrenergic receptor expression and upregulates inflammation in alveolar macrophages. Inhal. Toxicol. 2015, 27, 488–494. [Google Scholar] [CrossRef]
- Ringh, M.V.; Hagemann-Jensen, M.; Needhamsen, M.; Kular, L.; Breeze, C.E.; Sjöholm, L.K.; Slavec, L.; Kullberg, S.; Wahlström, J.; Grunewald, J.; et al. Tobacco smoking induces changes in true DNA methylation, hydroxymethylation and gene expression in bronchoalveolar lavage cells. EBioMedicine 2019, 46, 290–304. [Google Scholar] [CrossRef] [Green Version]
- Arnson, Y.; Shoenfeld, Y.; Amital, H. Effects of tobacco smoke on immunity, inflammation and autoimmunity. J. Autoimmun. 2010, 34, J258–J265. [Google Scholar] [CrossRef]
- Global Strategy for the Diagnosis, Management and Prevention of COPD, Global Initiative for Chronic Obstructive Lung Disease (GOLD) 2019. Available online: http://goldcopd.org (accessed on 16 December 2019).
- de Roux, A.; Cavalcanti, M.; Marcos, M.A. Impact of alcohol abuse in the etiology and severity of community-acquired pneumonia. Chest 2006, 129, 1219–1225. [Google Scholar] [CrossRef]
- Fine, M.J.; Auble, T.E.; Yealy, D.M. A prediction rule to identify low-risk patients with community-acquired pneumonia. N. Engl. J. Med. 1997, 336, 243–250. [Google Scholar] [CrossRef]
- Freeman, G.H.; Halton, J.H. Note on exact treatment of contingency, goodness of fit and other problems of significance. Biometrika 1951, 38, 141–149. [Google Scholar] [CrossRef]
- Torres, A.; Sibila, O.; Ferrer, M.; Polverino, E.; Menéndez, R.; Mensa Pueyo, J.; Gabarrús, A.; Sellarés, J.; Restrepo, M.; Anzueto, A.; et al. Effect of corticosteroids on treatment failure among hospitalized patients with severe community-acquired pneumonia and high inflammatory response: A randomized clinical trial. JAMA 2015, 313, 677–686. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sellares, J.; López-Giraldo, A.; Lucena, C.; Cilloniz, C.; Amaro, R.; Polverino, E.; Ferrer, M.; Menéndez, R.; Mensa, J.; Torres, A. Influence of previous use of inhaled corticoids on the development of pleural effusion in community-acquired pneumonia. Am. J. Respir. Crit. Care Med. 2013, 187, 1241–1248. [Google Scholar] [CrossRef] [PubMed]
- Huttunen, R.; Heikkinen, T.; Syrjänen, J. Smoking and the outcome of infection. J. Intern. Med. 2011, 269, 258–269. [Google Scholar] [CrossRef] [PubMed]
- Holter, J.C.; Ueland, T.; Jenum, P. Risk Factors for Long-Term Mortality after Hospitalization for Community-Acquired Pneumonia: A 5-Year Prospective Follow-Up Study. PLoS ONE 2016, 11, e0148741. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stefan, M.S.; Shieh, M.S.; Pekow, P.S.; Hill, N.; Rothberg, M.B.; Lindenauer, P.K. Trends in mechanical ventilation among patients hospitalized with acute exacerbations of COPD in the United States, 2001 to 2011. Chest 2015, 147, 959–968. [Google Scholar] [CrossRef] [Green Version]
- Straus, W.L.; Plouffe, J.F.; File, T.M., Jr. Risk factors for domestic acquisition of legionnaires disease. Ohio legionnaires Disease Group. Arch. Intern. Med. 1996, 156, 1685–1692. [Google Scholar] [CrossRef]
- Almirall, J.; Blanquer, J.; Bello, S. Community-acquired pneumonia among smokers. Arch. Bronconeumol. 2014, 50, 250–254. [Google Scholar] [CrossRef]
- Restrepo, M.I.; Babu, B.L.; Reyes, L.F.; Chalmers, J.D.; Soni, N.J.; Sibila, O.; Faverio, P.; Cilloniz, P.; Rodriguez-Cintron, W.; Alibertiet, S.; et al. Burden and risk factors for Pseudomonas aeruginosa community-acquired pneumonia: A multinational point prevalence study of hospitalised patients. Eur. Respir. J. 2018, 52, 1701190. [Google Scholar] [CrossRef] [Green Version]
- Asai, N.; Watanabe, H.; Shiota, A.; Kato, H.; Sakanashi, D.; Hagihara, M.; Koizumi, Y.; Yamagishi, Y.; Suematsu, H.; Mikamo, H. Efficacy and accuracy of qSOFA and SOFA scores as prognostic tools for community-acquired and healthcare-associated pneumonia. Int. J. Infect. Dis. 2019, 84, 89–96. [Google Scholar] [CrossRef]
| Variables | Non-Smokers | Former Smokers | Current Smokers | COPD | p Value |
| Number of patients | 626 | 351 | 273 | 251 | |
| Age, years | 77 [21] | 75 [16] | 53 [24] **,§§ | 75 [11] ## | <0.001 |
| Male, % | 30 | 87 ** | 72 **,§§ | 92 **,## | <0.001 |
| PSI, classes IV+V, % | 63 | 70 * | 42 **,§§ | 71 *,## | <0.001 |
| History of alcohol, % | 4 | 26 ** | 38 **,§ | 28 **,# | <0.001 |
| FEV1, % predicted | 48 [22] | ||||
| Chronic heart failure, % | 24 | 30 * | 8 **,§§ | 25 ## | <0.001 |
| Chronic liver disease, % | 3 | 3 | 6 | 5 | 0.086 |
| Chronic renal failure, % | 5 | 11 * | 4 § | 7 | 0.002 |
| Neurological disease, % | 33 | 23 * | 16 ** | 23 * | <0.001 |
| Diabetes mellitus, % | 20 | 25 | 13 *,§§ | 23 # | 0.003 |
| Malignancy, % | 4 | 9 * | 3 § | 13 **,## | <0.001 |
| Pneumonia during previous year, % | 17 | 22 | 13 § | 42 **,§§,## | <0.001 |
| Previous antibiotic in the last month, % | 30 | 31 | 25 | 37 | 0.090 |
| Previous ICS therapy, % | 12 | 20 * | 4 *,§§ | 65 **,§§,## | <0.001 |
| Previous OCS therapy, % | 4 | 6 | 3 | 12 **,§,## | <0.001 |
| Previous use of H2 antagonists, % | 16 | 16 | 8 *,§ | 15 # | 0.011 |
| Antipneumococcal vaccination | <0.001 | ||||
| No | 81 | 75 | 93 *,§§ | 70 **,§,## | |
| <5 years, % | 3 | 5 | 0.5 | 0.6 | |
| ≥5 years, % | 16 | 20 | 6.5 | 29.4 | |
| Influenza vaccination | <0.001 | ||||
| No | 40 | 37 | 71 **,§§ | 26 *,## | |
| <6 months, % | 39 | 44 | 16 | 49 | |
| ≥6 months, % | 21 | 19 | 13 | 25 |
| Variables | Non-Smokers | Former Smokers | Current Smokers | COPD | p Value |
| Temperature ≥ 39 °C, % | 13 | 10 | 17 | 12 | 0.093 |
| Chills, % | 54 | 60 | 59 | 58 | 0.225 |
| Cough, % | 79 | 81 | 83 | 84 | 0.364 |
| Pleuritic pain, % | 40 | 40 | 55 **,§§ | 43 # | <0.001 |
| Confusion, % | 28 | 23 | 21 | 20 | 0.067 |
| Respiratory rate ≥ 30 bpm, % | 28 | 28 | 30 | 38 *,§ | 0.044 |
| SBP ≤ 90 mmHg, % | 6 | 5 | 6 | 4 | 0.778 |
| Heart rate ≥ 120 bpm, % | 13 | 14 | 24 **,§ | 17 # | <0.001 |
| Multilobar involvement (≥2 lobes), % | 27 | 30 | 36 * | 19 *,§,## | <0.001 |
| Pulmonary atelectasis, % | 2 | 2 | 6 *,§ | 3 | 0.006 |
| Parapneumonic pleural effusion, % | 17 | 15 | 20 | 10 * # | 0.015 |
| Pulmonary empyema, % | 5 | 3 | 11 **,§ | 1 # | <0.001 |
| pH | 7.46 [0.07] | 7.46 [0.06] | 7.46 [0.08] | 7.44 [0.07] **,§§,# | <0.001 |
| PaCO2, mmHg | 35.3 [8.4] | 33.8 [6.7] | 32.9 [7.2] | 37.8 [11.5] **,§§,## | <0.001 |
| PaO2/FiO2 | 280.9 [76.2] | 276.2 [81.1] | 280.9 [90.5] | 265.8 [79.9] * | 0.023 |
| Leucocytes, 103/L | 12.7 [8.6] | 12.35 [7.9] | 13.5 [8] | 13.4 [7.7] | 0.142 |
| Neutrophils, % | 83 [11] | 83 [11] | 82 [10] | 83 [9.5] | 0.932 |
| Hematocrit, % | 39 [6] | 40 [6] * | 41 [7] * | 42 [7] **,§,# | <0.001 |
| Platelets, 103/L | 237 [112] | 221 [117] | 241 [119] | 239 [128] | 0.056 |
| Glucose, mg/dL | 127 [56] | 125 [54] | 120 [52] | 123 [60] | 0.682 |
| Creatinine, mg/dL | 1 [0.5] | 1.2 [0.7] * | 1 [0.5] | 1 [0.4] | 0.028 |
| Sodium, mEq/L | 135 [6] | 135 [6] | 134 [7.4] *,§ | 136 [5] # | 0.001 |
| Potassium, mEq/L | 4 [0.9] | 4.1 [0.7] | 3.9 [0.6] § | 4.1 [0.7] *,## | <0.001 |
| Variables | Non-Smokers | Former Smokers | Current Smokers | COPD | p Value |
|---|---|---|---|---|---|
| Patients with etiological diagnosis, n (%) | 255 (41) | 141 (40) | 153 (56) **,§§ | 111 (44) # | <0.001 |
| Streptococcus pneumoniae, n (%) | 116 (45.4) | 70 (50) | 72 (47.1) | 55 (49.5) | 0.832 |
| Streptococcus viridans, n (%) | 6 (2.3) | 3 (2.1) | 3 (2) | 4 (3.6) | 0.837 |
| Staphylococcus aureusa, n (%) | 19 (7.4) | 8 (5.7) | 7 (4.6) | 3 (2.7) | 0.293 |
| Staphylococcus spp., n (%) | 5 (2) | 5 (3.5) | 3 (2) | 3 (2.7) | 0.763 |
| Haemophilus influenzae, n (%) | 9 (3.5) | 2 (1.4) | 3 (2) | 3 (2.7) | 0.590 |
| Haemophilus parainfluenzae, n (%) | 1 (0.4) | 1 (0.7) | 1 (0.6) | 0 (0) | 0.943 |
| Moraxella catarrhalis, n (%) | 0 (0) | 1 (0.7) | 1 (0.6) | 2 (1.8) | 0.554 |
| Legionella pneumophila, n (%) | 14 (5.5) | 17 (12.1) * | 23 (15) * | 4 (3.6) §,# | <0.001 |
| Other atypical pathogens b, n (%) | 5 (2) | 2 (1.4) | 1 (0.6) | 1 (0.9) | 0.698 |
| Pseudomonas aeruginosa, n (%) | 12 (4.7) | 3 (2.1) | 3 (2) | 13 (11.7) *,§,# | <0.001 |
| Klebsiella pneumoniae, n (%) | 4 (1.6) | 1 (0.7) | 0 (0) | 0 (0) | 0.786 |
| Moraxella catarrhalis, n (%) | 0 (0) | 1 (0.7) | 1 (0.6) | 2 (1.8) | 0.554 |
| Escherichia coli, n (%) | 5 (2) | 2 (1.4) | 2 (1.31) | 2 (1.8) | 0.956 |
| Respiratory virus c, n (%) | 25 (9.8) | 15 (10.6) | 16 (10.5) | 7 (6.3) | 0.634 |
| Polymicrobial pneumonia, n (%) | 20 (7.8) | 18 (12.8) | 20 (13.1) | 15 (13.5) | 0.220 |
| Variables | Categories | Non-Smokers | Former Smokers | Current Smokers | COPD | p Value |
|---|---|---|---|---|---|---|
| Age | <65 years | n = 169 | n = 78 | n = 199 | n = 43 | 0.131 |
| CRP value, mg/L | 183.9 [205.5] | 187.4 [246.2] | 230 [216] | 192.7 [246] | ||
| ≥65 years | n = 457 | n = 273 | n = 74 | n = 208 | 0.001 | |
| CRP value, mg/L | 173 [193.1] | 179 [181.5] | 208.4 [190] | 135.2 [170.3] ## | ||
| Chronic heart failure | No | n = 476 | n = 244 | n = 250 | n = 189 | <0.001 |
| CRP value, mg/L | 187.1 [194.5] | 185.4 [194.1] | 224.2 [199.3] * | 172 [178] §,## | ||
| Yes | n = 148 | n = 107 | n = 21 | n = 62 | 0.278 | |
| CRP value, mg/L | 131.3 [193.4] | 153 [190.8] | 237.9 [251.1] | 112.2 [193.6] | ||
| Previous ICS therapy | No | n = 547 | n = 279 | n = 255 | n = 86 | 0.001 |
| CRP value, mg/L | 179 [192.7] | 181 [195] | 226.2 [198.1] * | 156.4 [176.7] # | ||
| Yes | n = 73 | n = 69 | n = 12 | n = 162 | 0.607 | |
| CRP value, mg/L | 130 [210.3] | 174 [183.6] | 189.2 [183.8] | 140.7 [190.5] | ||
| Previous oral corticosteroid therapy | No | n = 491 | n = 267 | n = 205 | n = 217 | <0.001 |
| CRP value, mg/L | 184.2 [196.2] | 187.5 [200] | 239 [173.8] **,§ | 152 [183] §,## | ||
| Yes | n = 20 | n = 18 | n = 6 | n = 29 | 0.101 | |
| CRP value, mg/L | 104.6 [180] | 100 [103.9] | 201.7 [170.3] | 172.7 [206.3] |
| Variables | Non-Smokers | Former Smokers | Current Smokers | COPD | p Value |
|---|---|---|---|---|---|
| Pleural complications, % | 13 | 13 | 21 *,§ | 8 * §,## | <0.001 |
| Length of hospital stay, days | 8 [5] | 8 [6] | 8 [8] | 8 [6] | 0.099 |
| NIMV, % | 3 | 7 * | 4 | 8 * | 0.033 |
| IMV, % | 4 | 5 | 10 *,§ | 4 # | 0.007 |
| ICU admission, % | 7 | 10 | 15 ** | 8 # | 0.004 |
| In-hospital mortality, % | 6 | 4 | 3 | 3 | 0.107 |
| 30-days mortality, % | 7 | 6 | 3 | 4 | 0.056 |
| Variables | Univariate | Multivariate | Multivariate Adjusted * | ||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p Value | OR | 95% CI | p Value | OR | 95% CI | p Value | |
| Non-smokers | 1 | 1 | 1 | ||||||
| Former smokers | 1.009 | 0.68 to 1.49 | 0.966 | 1.42 | 0.71 to 2.85 | 0.324 | 1.44 | 0.68 to 3.05 | 0.344 |
| Current smokers | 1.75 | 1.20 to 2.55 | 0.004 | 2.51 | 1.36 to 4.64 | 0.003 | 2.52 | 1.29 to 4.95 | 0.007 |
| COPD | 0.54 | 0.32 to 0.93 | 0.026 | 0.55 | 0.18 to 1.75 | 0.315 | 0.52 | 0.15 to 1.78 | 0.299 |
| Age, ≥65 y | 0.53 | 0.39 to 0.72 | <0.001 | ||||||
| Neurological disease, yes | 0.67 | 0.43 to 1.03 | 0.071 | ||||||
| Pneumonia during previous year, yes | 0.69 | 0.46 to 1.03 | 0.069 | ||||||
| Previous ICS therapy, yes | 0.38 | 0.24 to 0.62 | <0.001 | ||||||
| Influenza vaccination, No | 1 | ||||||||
| <6 months | 0.44 | 0.28 to 0.68 | <0.001 | ||||||
| ≥6 months | 0.67 | 0.41 to 1.10 | 0.106 | ||||||
| CRP, ≥150 mg/L | 1.50 | 1.10 to 2.06 | 0.012 | 2.46 | 1.25 to 4.81 | 0.009 | 2.58 | 1.30 to 5.10 | 0.007 |
| Temperature, ≥39 °C | 0.47 | 0.26 to 0.82 | 0.008 | ||||||
| Heart rate, ≥120 bpm | 1.61 | 1.11 to 2.35 | 0.013 | ||||||
| Pleuritic pain, yes | 3.71 | 2.67 to 5.15 | <0.001 | 4.88 | 2.72 to 8.75 | <0.001 | 5.13 | 2.78 to 9.46 | <0.001 |
| Positivity for S. pneumoniae | 1.50 | 1.09 to 2.05 | 0.012 | ||||||
| Platelets, +1 103/L | 1.002 | 1.000 to 1.003 | 0.026 | 1.003 | 1.001 to 1.006 | 0.006 | 1.003 | 1.001 to 1.006 | 0.004 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Crisafulli, E.; Cillóniz, C.; Liapikou, A.; Ferrari, M.; Busti, F.; Girelli, D.; Torres, A. Systemic Inflammatory Response and Outcomes in Community-Acquired Pneumonia Patients Categorized According to the Smoking Habit or Presence of Chronic Obstructive Pulmonary Disease. J. Clin. Med. 2020, 9, 2884. https://doi.org/10.3390/jcm9092884
Crisafulli E, Cillóniz C, Liapikou A, Ferrari M, Busti F, Girelli D, Torres A. Systemic Inflammatory Response and Outcomes in Community-Acquired Pneumonia Patients Categorized According to the Smoking Habit or Presence of Chronic Obstructive Pulmonary Disease. Journal of Clinical Medicine. 2020; 9(9):2884. https://doi.org/10.3390/jcm9092884
Chicago/Turabian StyleCrisafulli, Ernesto, Catia Cillóniz, Adamantia Liapikou, Marcello Ferrari, Fabiana Busti, Domenico Girelli, and Antoni Torres. 2020. "Systemic Inflammatory Response and Outcomes in Community-Acquired Pneumonia Patients Categorized According to the Smoking Habit or Presence of Chronic Obstructive Pulmonary Disease" Journal of Clinical Medicine 9, no. 9: 2884. https://doi.org/10.3390/jcm9092884
APA StyleCrisafulli, E., Cillóniz, C., Liapikou, A., Ferrari, M., Busti, F., Girelli, D., & Torres, A. (2020). Systemic Inflammatory Response and Outcomes in Community-Acquired Pneumonia Patients Categorized According to the Smoking Habit or Presence of Chronic Obstructive Pulmonary Disease. Journal of Clinical Medicine, 9(9), 2884. https://doi.org/10.3390/jcm9092884








