Prevalence of Antibodies to SARS-CoV-2 in Italian Adults and Associated Risk Factors
Abstract
1. Introduction
2. Experimental Methods
2.1. Participants
2.2. Endpoint
2.3. Detection of Infection
2.4. Statistical Analysis
2.5. Ethical Consideration
3. Results
3.1. Participant Demographics and Exposures
3.2. Prevalence of Sars-CoV-2 Antibodies
3.3. Factors Associated with Anti-Sars-CoV-2 Antibodies Positivity
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Onder, G.; Rezza, G.; Brusaferro, S. Case-Fatality Rate and Characteristics of Patients Dying in Relation to COVID-19 in Italy. JAMA 2020, 323, 1775–1776. [Google Scholar] [CrossRef]
- Available online: http://www.salute.gov.it/portale/nuovocoronavirus/ (accessed on 30 April 2020).
- Bassetti, M.; Vena, A.; Giacobbe, D.R. The novel Chinese coronavirus (2019-nCoV) infections: Challenges for fighting the storm. Eur. J. Clin. Investig. 2020, 50, e13209. [Google Scholar] [CrossRef]
- Kim, G.U.; Kim, M.J.; Ra, S.H.; Lee, J.; Bae, S.; Jung, J.; Kim, S.-H. Clinical characteristics of asymptomatic and symptomatic patients with mild COVID-19. Clin. Microbiol. Infect. 2020, 26, 948.e1–948.e3. [Google Scholar] [CrossRef] [PubMed]
- Mizumoto, K.; Kagaya, K.; Zarebski, A.; Chowell, G. Estimating the asymptomatic proportion of coronavirus disease 2019 (COVID-19) cases on board the Diamond Princess cruise ship, Yokohama, Japan, 2020. Eurosurveillance 2020, 25, 2000180. [Google Scholar] [CrossRef] [PubMed]
- Thursky, K.; Cordova, S.P.; Smith, D.; Kelly, H. Working towards a simple case definition for influenza surveillance. J. Clin. Virol. 2003, 27, 170–179. [Google Scholar] [CrossRef]
- Lippi, G.; Salvagno, G.L.; Pegoraro, M.; Militello, V.; Caloi, C.; Peretti, A.; Gaino, S.; Bassi, A.; Bovo, C.; Cascio, G.L. Assessment of immune response to SARS-CoV-2 with fully automated MAGLUMI 2019-nCoV IgG and IgM chemiluminescence immunoassays. Clin. Chem. Lab. Med. 2020, 58. [Google Scholar] [CrossRef]
- Padoan, A.; Cosma, C.; Sciacovelli, L.; Faggian, D.; Plebani, M. Analytical performances of a chemiluminescence immunoassay for SARS-CoV-2 IgM/IgG and antibody kinetics. Clin. Chem. Lab. Med. 2020, 58. [Google Scholar] [CrossRef]
- Li, Z.; Yi, Y.; Luo, X.; Xiong, N.; Liu, Y.; Li, S.; Sun, R.; Wang, Y.; Hu, B.; Chen, W.; et al. Development and clinical application of a rapid IgM-IgG combined antibody test for SARS-CoV-2 infection diagnosis. J. Med. Virol. 2020, 92. [Google Scholar] [CrossRef]
- Stringhini, S.; Wisniak, A.; Piumatti, G.; Azman, A.S.; Lauer, S.A.; Baysson, H.; De Ridder, D.; Petrovic, D.; Schrempft, S.; Marcus, K.; et al. Seroprevalence of anti-SARS-CoV-2 IgG antibodies in Geneva, Switzerland (SEROCoV-POP): A population-based study. Lancet 2020, 396, 313–319. [Google Scholar] [CrossRef]
- Pollan, M.; Perez-Gomez, B.; Pastor-Barriuso, R.; Oteo, J.; Hernan, M.A.; Perez-Olmeda, M.; Sanmartín, J.L.; Fernández-García, A.; Cruz, I.; De Larrea, N.F.; et al. Prevalence of SARS-CoV-2 in Spain (ENE-COVID): A nationwide, population-based seroepidemiological study. Lancet 2020. [Google Scholar] [CrossRef]
- Soriano, V.; Meirino, R.; Corral, O.; Guallar, M.P. SARS-CoV-2 antibodies in adults in Madrid, Spain. Clin. Infect. Dis. 2020. [Google Scholar] [CrossRef]
- Petersen, M.S.; Strom, M.; Christiansen, D.H.; Fjallsbak, J.P.; Eliasen, E.H.; Johansen, M.; Veyhe, A.S.; Kristiansen, M.F.; Gaini, S.; Møller, L.F.; et al. Seroprevalence of SARS-CoV-2-Specific Antibodies, Faroe Islands. Emerg. Infect. Dis. 2020, 26. [Google Scholar] [CrossRef]
- Biggs, H.M.; Harris, J.B.; Breakwell, L.; Dahlgren, F.S.; Abedi, G.R.; Szablewski, C.M.; Drobeniuc, J.; Bustamante, N.D.; Almendares, O.; Schnall, A.H.; et al. Estimated Community Seroprevalence of SARS-CoV-2 Antibodies—Two Georgia Counties, 28 April–3 May 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 965–970. [Google Scholar] [CrossRef] [PubMed]
- Menachemi, N.; Yiannoutsos, C.T.; Dixon, B.E.; Duszynski, T.J.; Fadel, W.F.; Wools-Kaloustian, K.K.; Needleman, N.U.; Box, K.; Caine, V.; Norwood, C.; et al. Population Point Prevalence of SARS-CoV-2 Infection Based on a Statewide Random Sample—Indiana, 25–29 April 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 960–964. [Google Scholar] [CrossRef] [PubMed]
- Fischer, B.; Knabbe, C.; Vollmer, T. SARS-CoV-2 IgG seroprevalence in blood donors located in three different federal states, Germany, March to June 2020. Eurosurveillance 2020, 25, 2001285. [Google Scholar] [CrossRef] [PubMed]
- Havers, F.P.; Reed, C.; Lim, T.; Montgomery, J.M.; Klena, J.D.; Hall, A.J.; Fry, A.M.; Cannon, D.L.; Chiang, C.-F.; Gibbons, A.; et al. Seroprevalence of Antibodies to SARS-CoV-2 in 10 Sites in the United States, 23 March–12 May 2020. JAMA Intern. Med. 2020. [Google Scholar] [CrossRef]
- Amorim Filho, L.; Szwarcwald, C.L.; Mateos, S.O.G.; Leon, A.; Medronho, R.A.; Veloso, V.G.; Lopes, J.I.F.; De Moraes Sobrino Porto, L.C.; Chieppe, A.; Werneck, G.L. Seroprevalence of anti-SARS-CoV-2 among blood donors in Rio de Janeiro, Brazil. Rev. Saude Publica 2020, 54, 69. [Google Scholar]
- Percivalle, E.; Cambie, G.; Cassaniti, I.; Nepita, E.V.; Maserati, R.; Ferrari, A.; Di Martino, R.; Isernia, P.; Mojoli, F.; Bruno, R.; et al. Prevalence of SARS-CoV-2 specific neutralising antibodies in blood donors from the Lodi Red Zone in Lombardy, Italy, as at 06 April 2020. Eurosurveillance 2020, 25, 2001031. [Google Scholar] [CrossRef]
- Sood, N.; Simon, P.; Ebner, P.; Eichner, D.; Reynolds, J.; Bendavid, E.; Bhattacharya, J. Seroprevalence of SARS-CoV-2-Specific Antibodies Among Adults in Los Angeles County, California, on 10–11 April 2020. JAMA 2020, 323, 2425–2427. [Google Scholar] [CrossRef]
- Tan, L.F.; Seetharaman, S. Preventing the Spread of COVID-19 to Nursing Homes: Experience from a Singapore Geriatric Centre. J. Am. Geriatr. Soc. 2020, 68, 942. [Google Scholar] [CrossRef]
- Abrams, H.R.; Loomer, L.; Gandhi, A. Grabowski DCCharacteristics of, U.S. Nursing Homes with COVID-19 Cases. J. Am. Geriatr. Soc. 2020, 68. [Google Scholar] [CrossRef] [PubMed]
- McMichael, T.M.; Currie, D.W.; Clark, S.; Pogosjans, S.; Kay, M.; Schwartz, N.G.; Lewis, J.; Baer, A.; Kawakami, V.; Lukoff, M.D.; et al. Epidemiology of Covid-19 in a Long-Term Care Facility in King County, Washington. N. Engl. J. Med. 2020, 382, 2005–2011. [Google Scholar] [CrossRef]
- Stone, P.W.; Herzig, C.T.; Pogorzelska-Maziarz, M.; Carter, E.; Bjarnadottir, R.I.; Semeraro, P.K.; Cohen, C.C.; Travers, J.; Schweon, S. Understanding infection prevention and control in nursing homes: A qualitative study. Geriatr. Nurs. 2015, 36, 267–272. [Google Scholar] [CrossRef] [PubMed]
- Herzig, C.T.; Stone, P.W.; Castle, N.; Pogorzelska-Maziarz, M.; Larson, E.L.; Dick, A.W. Infection Prevention and Control Programs in US Nursing Homes: Results of a National Survey. J. Am. Med. Dir. Assoc. 2016, 17, 85–88. [Google Scholar] [CrossRef]
- Pena, S.A.; Davis, S.S.; Lu, X.; Sakthivel, S.K.K.; Peret, T.C.T.; Rose, E.B.; Smelser, C.; Schneider, E.; Stone, N.D.; Watson, J. Severe Respiratory Illness Associated with Human Metapneumovirus in Nursing Home, New Mexico, USA. Emerg. Infect. Dis. 2019, 25, 383–384. [Google Scholar] [CrossRef]
- Ursic, T.; Miksic, N.G.; Lusa, L.; Strle, F.; Petrovec, M. Viral respiratory infections in a nursing home: A six-month prospective study. BMC Infect. Dis. 2016, 16, 637. [Google Scholar] [CrossRef]
- Seynaeve, D.; Augusseau-Riviere, B.; Couturier, P.; Morel-Baccard, C.; Landelle, C.; Bosson, J.L.; Gavazzi, G.; Mallaret, M.-R. Outbreak of Human Metapneumovirus in a Nursing Home: A Clinical Perspective. J. Am. Med. Dir. Assoc. 2020, 21, 104–109.e1. [Google Scholar] [CrossRef] [PubMed]
- Montoya, A.; Cassone, M.; Mody, L. Infections in Nursing Homes: Epidemiology and Prevention Programs. Clin. Geriatr. Med. 2016, 32, 585–607. [Google Scholar] [CrossRef]
- De Maria, A.; Varese, P.; Dentone, C.; Barisione, E.; Bassetti, M. High prevalence of olfactory and taste disorder during SARS-CoV-2 infection in outpatients. J. Med. Virol. 2020. [Google Scholar] [CrossRef]
- Butowt, R.; Bilinska, K. SARS-CoV-2: Olfaction, Brain Infection, and the Urgent Need for Clinical Samples Allowing Earlier Virus Detection. ACS Chem. Neurosci. 2020, 11, 1200–1203. [Google Scholar] [CrossRef]
- Al-Tawfiq, J.A. Asymptomatic coronavirus infection: MERS-CoV and SARS-CoV-2 (COVID-19). Travel Med. Infect. Dis. 2020, 35, 101608. [Google Scholar] [CrossRef] [PubMed]
- Iacobucci, G. Sixty seconds on the contact tracing app. BMJ 2020, 369, m1818. [Google Scholar] [CrossRef] [PubMed]
- Wu, F.; Wang, A.; Liu, M.; Wang, Q.; Chen, J.; Xia, S.; Ling, Y.; Zhang, Y.; Xun, J.; Lu, L.; et al. Neutralizing antibody responses to SARS-CoV-2 in a COVID-19 recovered patient cohort and their implications. medRxiv 2020. [CrossRef]
- Fang, B.; Meng, Q.H. The laboratory’s role in combating COVID-19. Crit. Rev. Clin. Lab. Sci. 2020, 57, 400–414. [Google Scholar] [CrossRef] [PubMed]
- Ghaffari, A.; Meurant, R.; Ardakani, A. COVID-19 Serological Tests: How Well Do They Actually Perform? Diagnostics 2020, 10, 453. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | N = 3609 (%) |
|---|---|
| Sex | |
| Female | 2007 (55.6) |
| Male | 1602 (44.4) |
| Age groups (Years) | |
| 18–35 | 556 (15.4) |
| 36–45 | 631 (17.4) |
| 46–55 | 929 (25.7) |
| >55 | 1493 (41.4) |
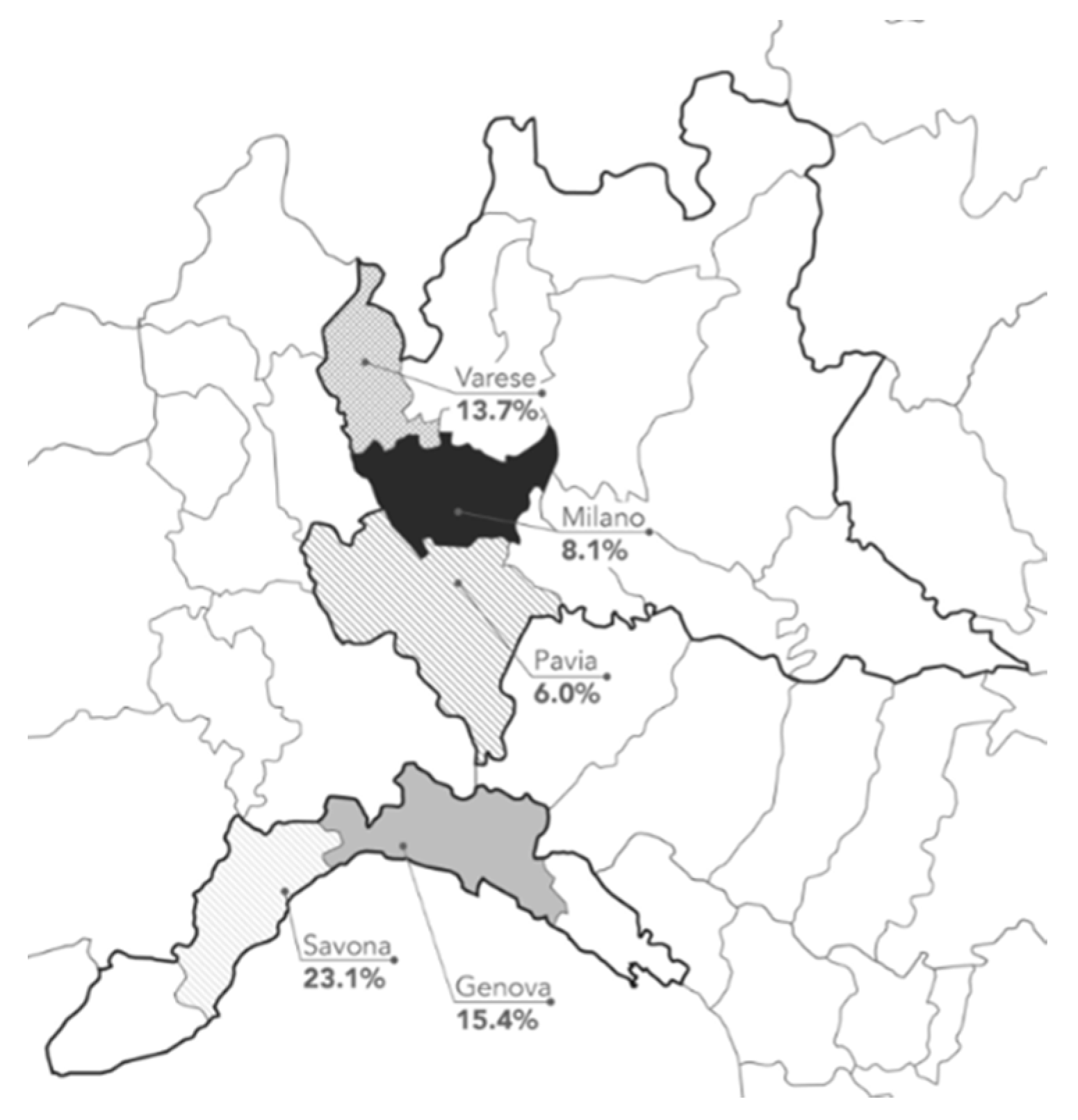
| Region | |
| Lombardia | 3065 (84.9) |
| Liguria | 544 (15.1) |
| Administrative department | |
| Varese | 1430 (39.6) |
| Pavia | 871 (24.1) |
| Milano | 764 (21.2) |
| Genova | 492 (13.6) |
| Savona | 52 (1.4) |
| Resident in a long-term care facility | 207 (5.7) |
| n (%) | Sars-CoV-2 IgG+ or IgM (95% Confidence Interval) | |
|---|---|---|
| Medical Center | 1885 (52.2) | 11.5% (10.1%–13.0%) |
| Istituto Diagnostico Varelli | 1180 (32.7) | 8.0% (6.5%–9.7%) |
| Casa della salute di Genova | 544 (15.1) | 16.2% (13.2%–19.5%) |
| Characteristics | Tested | SARS-CoV-2 IgG+ or IgM+ | Univariate Analysis | ||
|---|---|---|---|---|---|
| N | n (%) | OR | 95% CI | p-Value | |
| Sex | |||||
| Female | 2007 | 251 (12.5) | 1.36 | 1.12–1.65 | 0.002 |
| Male | 1602 | 147 (9.2) | Ref | Ref | Ref |
| Age group (Years) | |||||
| 18–35 | 556 | 66 (11.9) | 1.10 | 0.83–1.46 | 0.50 |
| 36–45 | 631 | 45 (7.1) | 0.57 | 0.41–0.79 | 0.001 |
| 46–55 | 929 | 90 (9.7) | 0.82 | 0.64–1.05 | 0.24 |
| >55 | 1493 | 197 (13.2) | 1.44 | 1.17–1.78 | 0.001 |
| Living in a long-term care facility | |||||
| No | 3402 | 312 (9.2) | Ref | Ref | Ref |
| Yes | 207 | 86 (41.5) | 7.56 | 5.58–10.23 | 0.001 |
| Occupational exposure | |||||
| No | 3430 | 363 (10.6) | Ref | Ref | Ref |
| Yes | 178 | 35 (19.7) | 2.60 | 1.76–3.88 | 0.001 |
| Private Exposure | |||||
| No | 3469 | 376 (10.8) | Ref | Ref | Ref |
| Yes | 140 | 21 (15.0) | 1.45 | 0.90–2.36 | 0.12 |
| Occurrence of Symptoms in the previous month | |||||
| No symptoms | 3147 | 226 (7.2) | Ref | Ref | Ref |
| Influenza-like illness | 427 | 427 (34.2) | 6.71 | 5.27–8.54 | 0.001 |
| Loss of sense or taste | 35 | 26 (74.3) | 37.33 | 17.28–80.64 | 0.001 |
| Characteristics | OR | 95% CI | p-Value |
|---|---|---|---|
| Male sex | 0.79 | 0.63–1.01 | 0.06 |
| Age 36–45 | 1.40 | 0.99–1.93 | 0.06 |
| Age > 55 | 1.17 | 0.88–1.55 | 0.27 |
| Living in a long-term care facility | 4.53 | 3.19–6.45 | 0.001 |
| Occupational exposure | 2.36 | 1.59–3.50 | 0.001 |
| Prior history of influenza-like illness | 4.86 | 3.75–6.30 | 0.001 |
| Prior history of loss of sense or taste | 41.00 | 18.94–88.71 | 0.001 |
| Author | Country; Area | Number of Participants | Prevalence of Anti-SARS-CoV-2 Antibodies |
|---|---|---|---|
| Petersen M.S. [13] | Faroe Islands; Nationwide study | 1075 | 0.6% |
| Biggs H. [14] | U.S.; two metropolitan Atlanta counties | 696 | 2.5% |
| Menachemi N. [15] | U.S; Indiana | 3658 | 2.79% |
| Fischer B. [16] | Germany; three federal states | 3186 | 0.91% |
| Pollan M. [11] | Spain; Nationwide study | 61,075 | 5.0% |
| Havers F. [17] | U.S; 10 sites | 16,025 | From 1.0% (San Francisco) to 6.9% (New York City) |
| Amorim Filho L. [18] | Brazil; Rio de Janeiro | 2857 | 4.0% |
| Percivalle E. [19] | Italy; Lodi area | 390 | 23.0% |
| Soriano V. [12] | Spain, Madrid | 674 | 13.8% |
| Stringhini S. [10] | Switzerland, Geneve | 2766 | 9.7% |
| Sood N. [20] | U.S., Los Angeles | 1702 | 4.3% |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vena, A.; Berruti, M.; Adessi, A.; Blumetti, P.; Brignole, M.; Colognato, R.; Gaggioli, G.; Giacobbe, D.R.; Bracci-Laudiero, L.; Magnasco, L.; et al. Prevalence of Antibodies to SARS-CoV-2 in Italian Adults and Associated Risk Factors. J. Clin. Med. 2020, 9, 2780. https://doi.org/10.3390/jcm9092780
Vena A, Berruti M, Adessi A, Blumetti P, Brignole M, Colognato R, Gaggioli G, Giacobbe DR, Bracci-Laudiero L, Magnasco L, et al. Prevalence of Antibodies to SARS-CoV-2 in Italian Adults and Associated Risk Factors. Journal of Clinical Medicine. 2020; 9(9):2780. https://doi.org/10.3390/jcm9092780
Chicago/Turabian StyleVena, Antonio, Marco Berruti, Andrea Adessi, Pietro Blumetti, Michele Brignole, Renato Colognato, Germano Gaggioli, Daniele Roberto Giacobbe, Luisa Bracci-Laudiero, Laura Magnasco, and et al. 2020. "Prevalence of Antibodies to SARS-CoV-2 in Italian Adults and Associated Risk Factors" Journal of Clinical Medicine 9, no. 9: 2780. https://doi.org/10.3390/jcm9092780
APA StyleVena, A., Berruti, M., Adessi, A., Blumetti, P., Brignole, M., Colognato, R., Gaggioli, G., Giacobbe, D. R., Bracci-Laudiero, L., Magnasco, L., Signori, A., Taramasso, L., Varelli, M., Vendola, N., Ball, L., Robba, C., Battaglini, D., Brunetti, I., Pelosi, P., & Bassetti, M. (2020). Prevalence of Antibodies to SARS-CoV-2 in Italian Adults and Associated Risk Factors. Journal of Clinical Medicine, 9(9), 2780. https://doi.org/10.3390/jcm9092780









