The Prevalence and Impact of Polycystic Ovary Syndrome in Recurrent Miscarriage: A Retrospective Cohort Study and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Population and Study Design of the Retrospective Cohort
2.2. Parameters Analyzed
2.3. Meta-Analysis
2.4. Statistical Analysis
3. Results
3.1. Retrospective Cohort Study: Results of Complete Evaluation for Recurrent Miscarriage
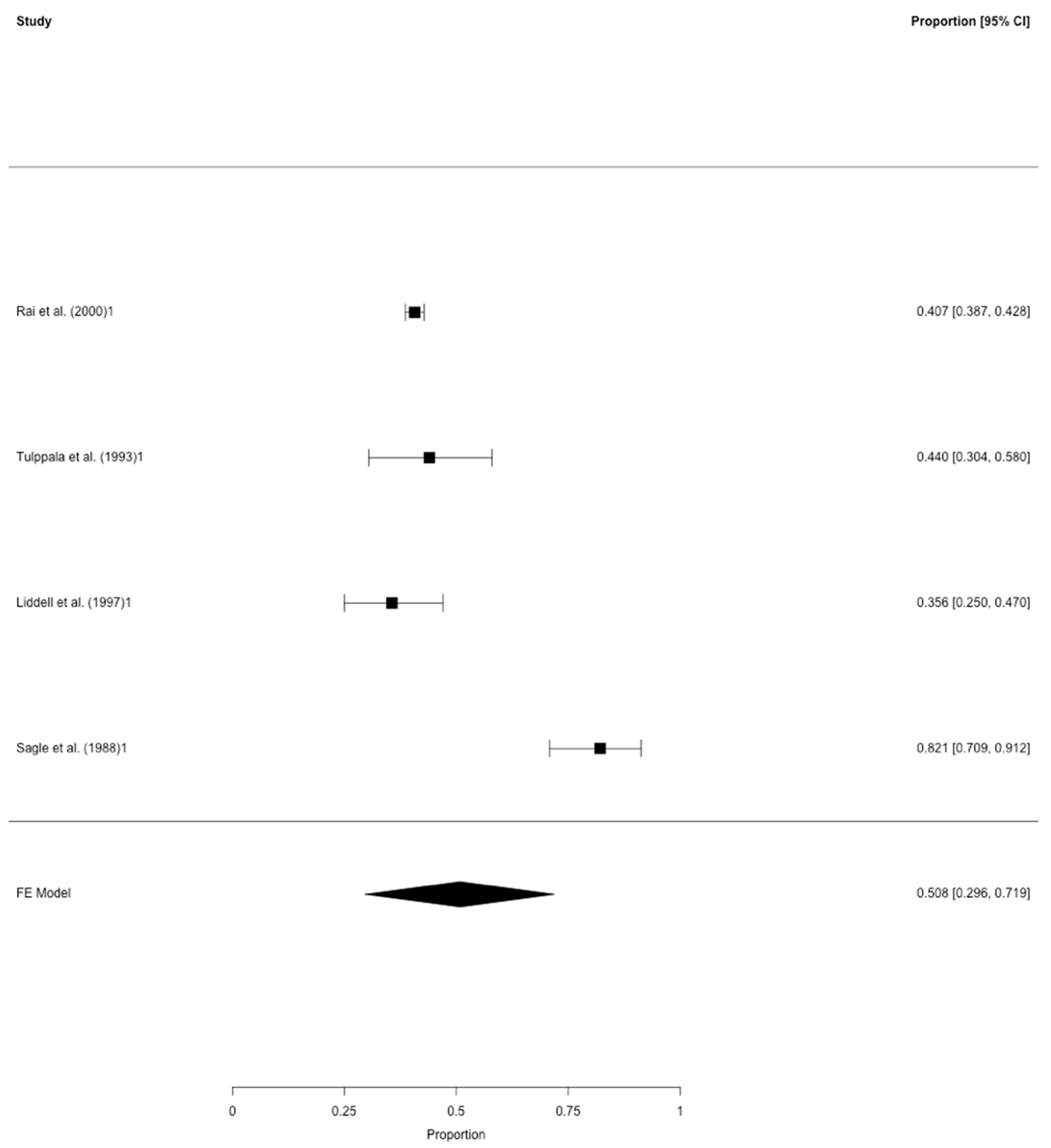
3.2. Meta-Analysis on the Prevalence of Polycystic Ovarian Morphology and PCOS in RM
3.3. Outcome of Women with PCOS and RM in the Retrospective Cohort Study
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
Availability of Data and Materials
References
- Norman, R.J.; Dewailly, D.; Legro, R.S.; Hickey, T.E. Polycystic ovary syndrome. Lancet 2007, 370, 685–697. [Google Scholar] [CrossRef]
- Sirmans, S.M.; Pate, K.A. Epidemiology, diagnosis and management of polycystic ovary syndrome. Clin. Epidemiol. 2013, 6, 1–13. [Google Scholar] [PubMed]
- The Rotterdam ESHRE/ASRM-sponsored PCOS consensus workshop group. Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome (PCOS). Hum. Reprod. 2004, 19, 41–47. [Google Scholar] [CrossRef] [PubMed]
- Rai, R.; Regan, L. Recurrent miscarriage. Lancet 2006, 368, 601–611. [Google Scholar] [CrossRef]
- Pils, S.; Promberger, R.; Springer, S.; Joura, E.; Ott, J. Decreased Ovarian Reserve Predicts Inexplicability of Recurrent Miscarriage? A Retrospective Analysis. PLoS ONE 2016, 11, e0161606. [Google Scholar] [CrossRef] [PubMed]
- Pils, S.; Stepien, N.; Kurz, C.; Nouri, K.; Promberger, R.; Ott, J. Anti-Mullerian hormone is linked to the type of early pregnancy loss in idiopathic recurrent miscarriage: A retrospective cohort study. Reprod. Boil. Endocrinol. 2017, 15, 60. [Google Scholar] [CrossRef]
- Garrido-Gimenez, C.; Reig, J.A. Recurrent miscarriage: Causes, evaluation and management. Postgrad. Med. J. 2015, 91, 151–162. [Google Scholar] [CrossRef]
- Shahine, L.; Lathi, R. Recurrent pregnancy loss: Evaluation and treatment. Obstet. Gynecol. Clin. N. Am. 2015, 42, 117–134. [Google Scholar] [CrossRef]
- Li, T.C.; Makris, M.; Tomsu, M.; Tuckerman, E.; Laird, S.M. Recurrent miscarriage: Aetiology, management and prognosis. Hum. Reprod. Update 2002, 8, 463–481. [Google Scholar] [CrossRef]
- Ke, R.W. Endocrine basis for recurrent pregnancy loss. Obstet. Gynecol. Clin. N. Am. 2014, 41, 103–112. [Google Scholar] [CrossRef]
- Cocksedge, K.A.; Saravelos, S.H.; Metwally, M.; Li, T.C. How common is polycystic ovary syndrome in recurrent miscarriage? Reprod. Biomed. Online 2009, 19, 572–576. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Sugiura-Ogasawara, M.; Sato, T.; Suzumori, N.; Kitaori, T.; Kumagai, K.; Ozaki, Y. The polycystic ovary syndrome does not predict further miscarriage in Japanese couples experiencing recurrent miscarriages. Am. J. Reprod. Immunol. 2009, 61, 62–67. [Google Scholar] [CrossRef] [PubMed]
- Sagle, M.; Bishop, K.; Ridley, N.; Alexander, F.M.; Michel, M.; Bonney, R.C.; Beard, R.W.; Franks, S. Recurrent early miscarriage and polycystic ovaries. BMJ 1988, 297, 1027–1028. [Google Scholar] [CrossRef] [PubMed]
- Rai, R.; Backos, M.; Rushworth, F.; Regan, L. Polycystic ovaries and recurrent miscarriage—A reappraisal. Hum. Reprod. 2000, 15, 612–615. [Google Scholar] [CrossRef] [PubMed]
- Tulppala, M.; Stenman, U.-H.; Cacciatore, B.; Ylikorkala, O. Polycystic ovaries and levels of gonadotrophins and androgens in recurrent miscarriage: Prospective study in 50 women. Br. J. Obstet. Gynaecol. 1993, 100, 348–352. [Google Scholar] [CrossRef] [PubMed]
- Liddell, H.S.; Sowden, K.; Farquhar, C.M. Recurrent miscarriage: Screening for polycystic ovaries and subsequent pregnancy outcome. Aust. N. Z. J. Obstet. Gynaecol. 1997, 37, 402–406. [Google Scholar] [CrossRef]
- Cocksedge, K.A.; Li, T.-C.; Saravelos, S.H.; Metwally, M. A reappraisal of the role of polycystic ovary syndrome in recurrent miscarriage. Reprod. Biomed. Online 2008, 17, 151–160. [Google Scholar] [CrossRef]
- Toth, B.; Wurfel, W.; Bohlmann, M.; Zschocke, J.; Rudnik-Schoneborn, S.; Nawroth, F.; Schleuner, E.; Rogenhofer, N.; Wishmann, T.; von Wolff, M.; et al. Recurrent Miscarriage: Diagnostic and Therapeutic Procedures. Guideline of the DGGG, OEGGG and SGGG (S2k-Level, AWMF Registry Number 015/050). Geburtshilfe Frauenheilkd. 2018, 78, 364–381. [Google Scholar] [CrossRef]
- Pils, S.; Stepien, N.; Kurz, C.; Nouri, K.; Springer, S.; Hager, M.; Promberger, R.; Ott, J. Does anti-Mullerian hormone predict the outcome of further pregnancies in idiopathic recurrent miscarriage? A retrospective cohort study. Arch. Gynecol. Obstet. 2018, 299, 259–265. [Google Scholar] [CrossRef]
- Carp, H. A systematic review of dydrogesterone for the treatment of recurrent miscarriage. Gynecol. Endocrinol. 2015, 31, 422–430. [Google Scholar] [CrossRef]
- Hyldgaard, J.; Bor, P.; Ingerslev, H.J.; Tørring, N. Comparison of two different methods for measuring anti-mullerian hormone in a clinical series. Reprod. Boil. Endocrinol. 2015, 13, 107. [Google Scholar] [CrossRef] [PubMed]
- Wells, A. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses. Available online: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed on 14 March 2020).
- Hager, M.; Wenzl, R.; Riesenhuber, S.; Marschalek, J.; Kuessel, L.; Mayrhofer, D.; Ristl, R.; Kurz, C.; Ott, J. The Prevalence of Incidental Endometriosis in Women Undergoing Laparoscopic Ovarian Drilling for Clomiphene-Resistant Polycystic Ovary Syndrome: A Retrospective Cohort Study and Meta-Analysis. J. Clin. Med. 2019, 8, 1210. [Google Scholar] [CrossRef] [PubMed]
- Matjila, M.J.; Hoffman, A.; van der Spuy, Z.M. Medical conditions associated with recurrent miscarriage-Is BMI the tip of the iceberg? Eur. J. Obstet. Gynecol. Reprod. Boil. 2017, 214, 91–96. [Google Scholar] [CrossRef] [PubMed]
- Diejomaoh, M.; Jirous, J.; Al-Azemi, M.; Baig, S.; Gupta, M.; Tallat, A. The relationship of recurrent spontaneous miscarriage with reproductive failure. Med. Princ. Pract. 2003, 12, 107–111. [Google Scholar] [CrossRef] [PubMed]
- Kousta, E.; White, D.; Cela, E.; McCarthy, M.M.; Franks, S. The prevalence of polycystic ovaries in women with infertility. Hum. Reprod. 1999, 14, 2720–2723. [Google Scholar] [CrossRef][Green Version]
- Okon, M.A. Serum androgen levels in women who have recurrent miscarriages and their correlation with markers of endometrial function. Fertil. Steril. 1998, 69, 682–690. [Google Scholar] [CrossRef]
- Clifford, K.; Rai, R.; Watson, H.; Regan, L. An informative protocol for the investigation of recurrent miscarriage: Preliminary experience of 500 consecutive cases. Hum. Reprod. 1994, 9, 1328–1332. [Google Scholar] [CrossRef]
- Bozdag, G.; Mumusoglu, S.; Zengin, D.; Karabulut, E.; Yildiz, B.O. The prevalence and phenotypic features of polycystic ovary syndrome: A systematic review and meta-analysis. Hum. Reprod. 2016, 31, 2841–2855. [Google Scholar] [CrossRef]
- Hahn, K.A.; Hatch, E.E.; Rothman, K.J.; Mikkelsen, E.M.; Brogly, S.B.; Sørensen, H.T.; Riis, A.H.; Wise, L.A. Body size and risk of spontaneous abortion among danish pregnancy planners. Paediatr. Perinat. Epidemiol. 2014, 28, 412–423. [Google Scholar] [CrossRef]
- Boots, C.; Stephenson, M.D. Does obesity increase the risk of miscarriage in spontaneous conception: A systematic review. Semin. Reprod. Med. 2011, 29, 507–513. [Google Scholar] [CrossRef]
- Cavalcante, M.B.; Sarno, M.; Peixoto, A.B.; Júnior, E.A.; Barini, R. Obesity and recurrent miscarriage: A systematic review and meta-analysis. J. Obstet. Gynaecol. Res. 2019, 45, 30–38. [Google Scholar] [CrossRef] [PubMed]
- Broughton, D.E.; Moley, K.H. Obesity and female infertility: Potential mediators of obesity’s impact. Fertil. Steril. 2017, 107, 840–847. [Google Scholar] [CrossRef] [PubMed]
- Grodnitskaya, E.; Kurtser, M.A. Homocysteine metabolism in polycystic ovary syndrome. Gynecol. Endocrinol. 2012, 28, 186–189. [Google Scholar] [CrossRef] [PubMed]
- Pugeat, M.; Ducluzeau, P.H. Insuin resistance, polycystic ovary syndrome and metformin. Drugs 1999, 58 (Suppl. 1), 41–46, discussion 75–82. [Google Scholar] [CrossRef] [PubMed]
- Glueck, C.J.; Streicher, P.; Wang, P. Treatment of polycystic ovary syndrome with insulin-lowering agents. Expert Opin. Pharmacother. 2002, 3, 1177–1189. [Google Scholar] [PubMed]
- Nestler, J.E.; Jakubowicz, D.J.; Evans, W.S.; Pasquali, R. Effects of metformin on spontaneous and clomiphene-induced ovulation in the polycystic ovary syndrome. N. Engl. J. Med. 1998, 338, 1876–1880. [Google Scholar] [CrossRef]
- Craig, L.B.; Ke, R.W.; Kutteh, W.H. Increased prevalence of insulin resistance in women with a history of recurrent pregnancy loss. Fertil. Steril. 2002, 78, 487–490. [Google Scholar] [CrossRef]
- Kazerooni, T.; Ghaffarpasand, F.; Asadi, N.; Dehkhoda, Z.; Dehghankhalili, M.; Kazerooni, Y. Correlation between thrombophilia and recurrent pregnancy loss in patients with polycystic ovary syndrome: A comparative study. J. Chin. Med. Assoc. 2013, 76, 282–288. [Google Scholar] [CrossRef]
- Tian, L.; Shen, H.; Lu, Q.; Norman, R.J.; Wang, J. Insulin resistance increases the risk of spontaneous abortion after assited reproduction technology treatment. J. Clin. Endocrinol. Metab. 2007, 92, 1430–1433. [Google Scholar] [CrossRef]
- Barbieri, R.L.; Makris, A.; Randall, R.W.; Daniels, G.; Kistner, R.W.; Ryan, K.J. Insulin stimulates androgen accumulation in incubations of ovarian stroma obtained from women with hyperandrogenism. J. Clin. Endocrinol. Metab. 1986, 62, 904–910. [Google Scholar] [CrossRef]
- Glueck, C.J.; Wang, P.; Goldenberg, N.; Sieve-Smith, L. Pregnancy outcomes among women with polycystic ovary syndrome treated with metformin. Hum. Reprod. 2002, 17, 2858–2864. [Google Scholar] [CrossRef] [PubMed]
- Santos, T.D.S.; Ieque, A.L.; De Carvalho, H.C.; Sell, A.M.; Lonardoni, M.V.C.; Demarchi, I.G.; Neto, Q.A.D.L.; Teixeira, J.J.V. Antiphospholipid syndrome and recurrent miscarriage: A systematic review and meta-analysis. J. Reprod. Immunol. 2017, 123, 78–87. [Google Scholar] [CrossRef] [PubMed]
- Cavalcante, M.B.; Sarno, M.; Cavalcante, C.T.D.M.B.; Júnior, E.A.; Barini, R. Coagulation Biomarkers in Women with Recurrent Miscarriage and Polycystic Ovarian Syndrome: Systematic Review and Meta-Analysis. Geburtshilfe Frauenheilkd. 2019, 79, 697–704. [Google Scholar] [CrossRef] [PubMed]
- Pritchard, A.M.; Hendrix, P.W.; Paidas, M.J. Hereditary Thrombophilia and Recurrent Pregnancy Loss. Clin. Obstet. Gynecol. 2016, 59, 487–497. [Google Scholar] [CrossRef] [PubMed]
- Puente, E.; Alonso, L.; Laganà, A.S.; Ghezzi, F.; Casarin, J.; Carugno, J. Chronic Endometritis: Old Problem, Novel Insights and Future Challenges. Int. J. Fertil. Steril. 2020, 13, 250–256. [Google Scholar]

| Age (years) * | 33.8 ± 6.1 | |
| BMI (kg/m2) * | 24.9 ± 5.0 | |
| Number of previous miscarriages # | 3 | 322 (71.2) |
| 4 | 78 (17.3) | |
| ≥5 | 52 (11.5) | |
| Type of recurrent miscarriage # | Primary | 318 (70.4) |
| Secondary | 134 (29.6) | |
| PCOS # | 43 (9.5) | |
| Underlying causes for RM+: | ||
| Recurrent miscarriage negative for selected risk factors # | 181 (40.0) | |
| Recurrent miscarriage negative for selected risk factors (includes women with PCOS only) | 209 (46.2) | |
| BMI >25 kg/m2 | 156 (34.5) | |
| Hypothyroidism # | 16 (13.5) | |
| Hyperthyroidism # | 11 (2.4) | |
| Antiphospholipid syndrome # | 17 (3.8) | |
| Antithrombin deficiency # | 7 (1.5) | |
| Factor V Leiden-mutation # | 16 (3.5) | |
| Prothrombin deficiency # | 5 (1.1) | |
| Protein C deficiency # | 7 (1.5) | |
| Protein S deficiency # | 9 (2.0) | |
| Bacterial vaginosis (including infection with ureaplasm and mycoplasma hominis) | 23 (5.1) | |
| Uterine malformation (septate or bicornuate uterus) # | 25 (5.5) | |
| Uterine abnormalities (endometrial polyp, myoma, intrauterine synechia) | 43 (9.5) | |
| Parental chromosomal abnormalities | 1 (0.2) | |
| First Author | Year | Study Design | PCO Morphology Definition | Total Number of Women with RM | Number of Women with PCOM */PCOS | Rate of Women with PCOM */PCOS # |
|---|---|---|---|---|---|---|
| Studies on polycystic ovarian morphology (PCOM) | ||||||
| Sagle et al. [13] | 1988 | retrospective | ≥10 cysts of 2–8 mm | 56 | 46 | 82.1 |
| Tulppala et al. [15] | 1993 | prospective | ≥10 cysts of ≥2 mm | 50 | 22 | 44.0 |
| Liddell et al. [16] | 1997 | prospective | ≥10 cysts of ≥2 mm | 73 | 26 | 35.6 |
| Rai et al. [14] | 2000 | retrospective | ovarian volume >9 mL, ≥10 cysts of 2–8 mm | 2199 | 895 | 40.7 |
| Studies on polycystic ovarian syndrome (PCOS) | ||||||
| Cocksedge et al. [11] | 2009 | retrospective | - | 300 | 30 | 10.0 |
| Matjila et al. [24] | 2017 | retrospective | - | 592 | 148 | 25.0 |
| Mayrhofer et al. | 2020 | retrospective | - | 452 | 43 | 9.5 |
| RM Negative for Selected Risk Factors with PCOS (n = 28) | RM Negative for Selected Risk Factors without PCOS (n = 28) | p | ||
|---|---|---|---|---|
| Age (years) * | 29.9 ± 4.8 | 29.9 ± 4.5 | 0.989 | |
| BMI (kg/m2) * | 25.6 ± 5.1 | 25.1 ± 4.6 | 0.669 | |
| Number of previous miscarriages # | 3 | 20 (71.4) | 20 (71.4) | 1.000 |
| 4 | 5 (17.9) | 6 (21.4) | ||
| ≥5 | 3 (10.7) | 2 (7.1) | ||
| Type of recurrent miscarriage # | Primary | 20 (71.4) | 17 (60.7) | 0.573 |
| Secondary | 8 (28.6) | 11 (39.3) | ||
| FSH (mIU/mL) * | 5.3 ± 2.1 | 5.6 ± 2.8 | 0.656 | |
| LH (mIU/mL) * | 8.8. ± 4.1 | 5.9 ± 3.8 | 0.009 + | |
| LH:FSH ratio | 1.9 ± 1.1 | 1.3 ± 1.3 | 0.125 | |
| Total testosterone (ng/mL) * | 0.61 ± 0.12 | 0.28 ± 0.10 | <0.001 + | |
| AMH (ng/mL) * | 5.59 ± 2.62 | 2.12 ± 1.89 | <0.001 + | |
| Follow-up period (months) * | 18.6 ± 4.5 | 18.3 ± 4.9 | 0.799 | |
| One or more further miscarriages # | 20 (71.4) | 15 (53.6) | 0.031 + | |
| One or more live births # | 12 (42.9) | 17 (60.7) | 0.285 | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mayrhofer, D.; Hager, M.; Walch, K.; Ghobrial, S.; Rogenhofer, N.; Marculescu, R.; Seemann, R.; Ott, J. The Prevalence and Impact of Polycystic Ovary Syndrome in Recurrent Miscarriage: A Retrospective Cohort Study and Meta-Analysis. J. Clin. Med. 2020, 9, 2700. https://doi.org/10.3390/jcm9092700
Mayrhofer D, Hager M, Walch K, Ghobrial S, Rogenhofer N, Marculescu R, Seemann R, Ott J. The Prevalence and Impact of Polycystic Ovary Syndrome in Recurrent Miscarriage: A Retrospective Cohort Study and Meta-Analysis. Journal of Clinical Medicine. 2020; 9(9):2700. https://doi.org/10.3390/jcm9092700
Chicago/Turabian StyleMayrhofer, Daniel, Marlene Hager, Katharina Walch, Stefan Ghobrial, Nina Rogenhofer, Rodrig Marculescu, Rudolf Seemann, and Johannes Ott. 2020. "The Prevalence and Impact of Polycystic Ovary Syndrome in Recurrent Miscarriage: A Retrospective Cohort Study and Meta-Analysis" Journal of Clinical Medicine 9, no. 9: 2700. https://doi.org/10.3390/jcm9092700
APA StyleMayrhofer, D., Hager, M., Walch, K., Ghobrial, S., Rogenhofer, N., Marculescu, R., Seemann, R., & Ott, J. (2020). The Prevalence and Impact of Polycystic Ovary Syndrome in Recurrent Miscarriage: A Retrospective Cohort Study and Meta-Analysis. Journal of Clinical Medicine, 9(9), 2700. https://doi.org/10.3390/jcm9092700






