Effectiveness of Global Postural Reeducation in Ankylosing Spondylitis: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
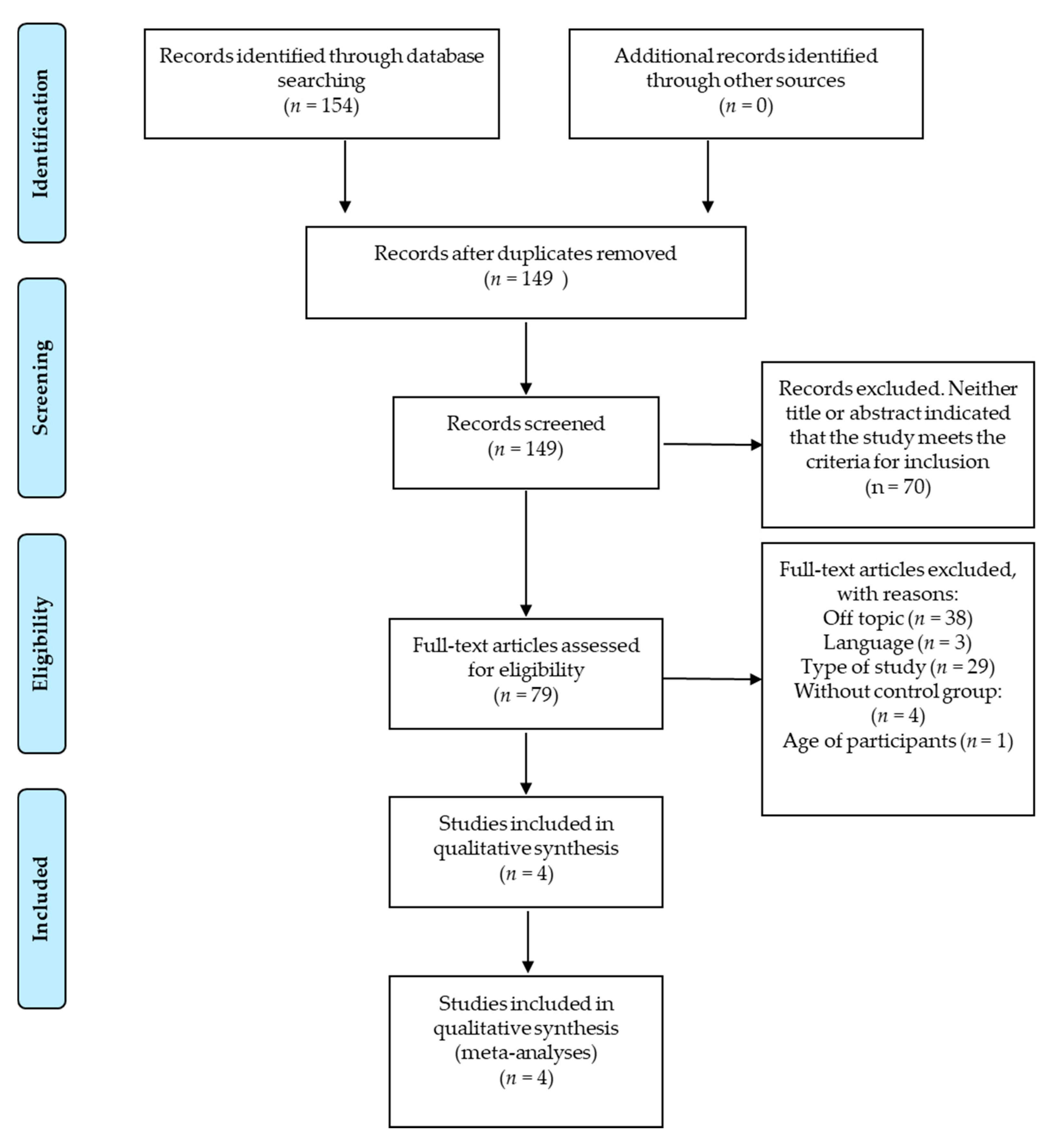
2. Material and Methods
2.1. Study Design
2.2. Search Strategy
2.3. Criteria for Considering Studies for This Review
2.4. Data Extraction
2.5. Data Analysis and Outcomes
2.6. Evaluation of Clinical Relevance
3. Results
3.1. Data Extraction
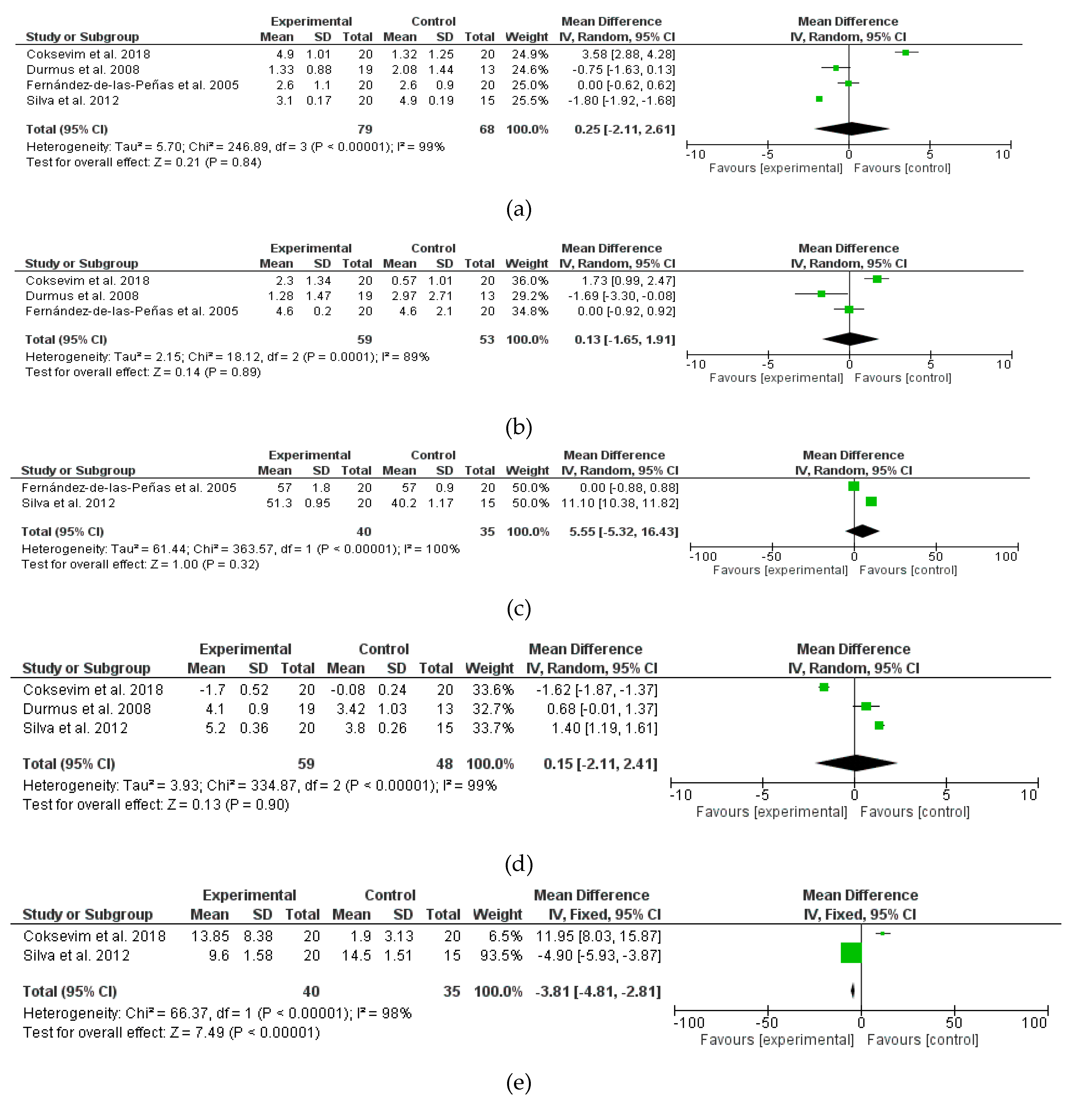
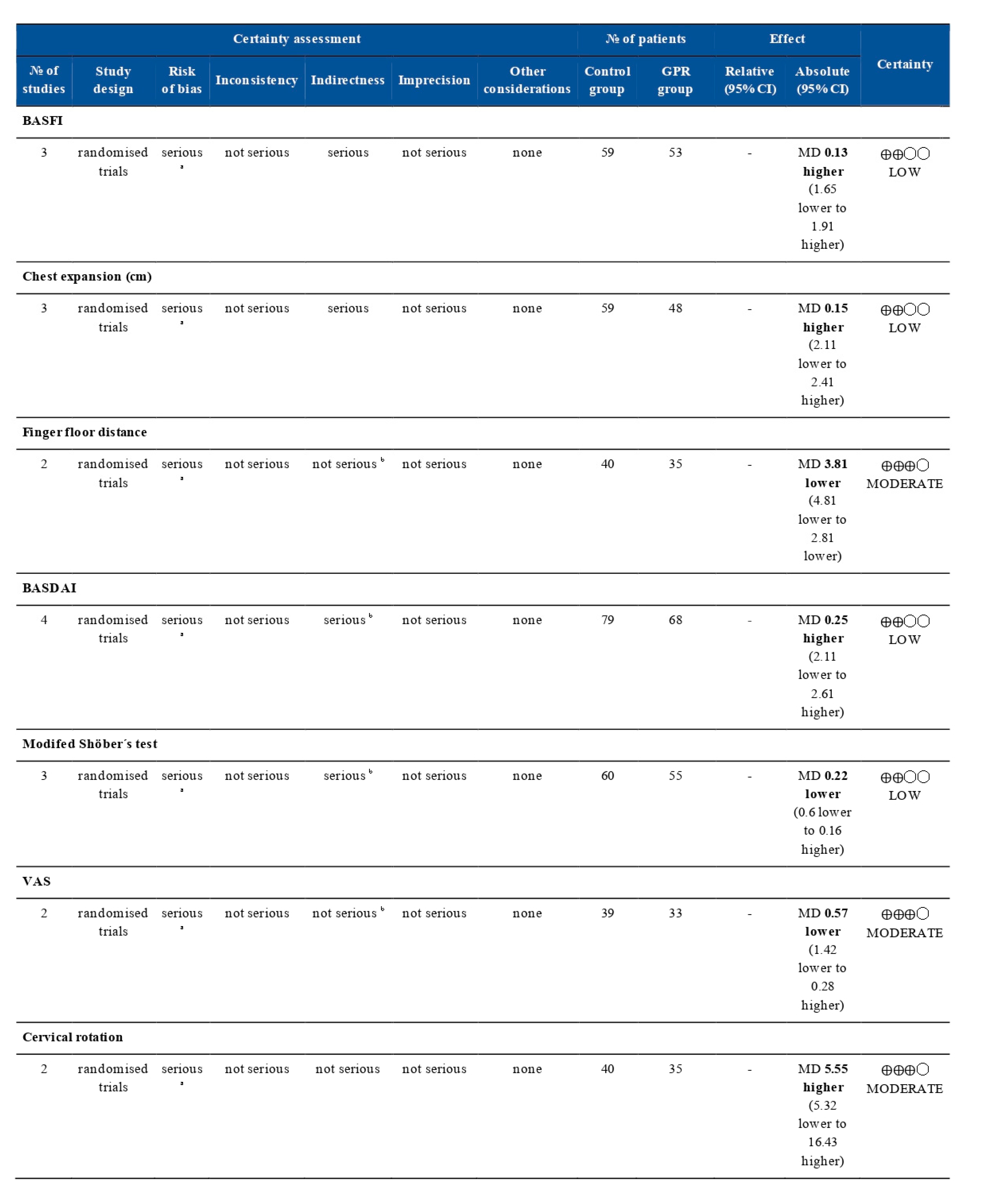
3.2. Data Analysis and Meta-Analyses
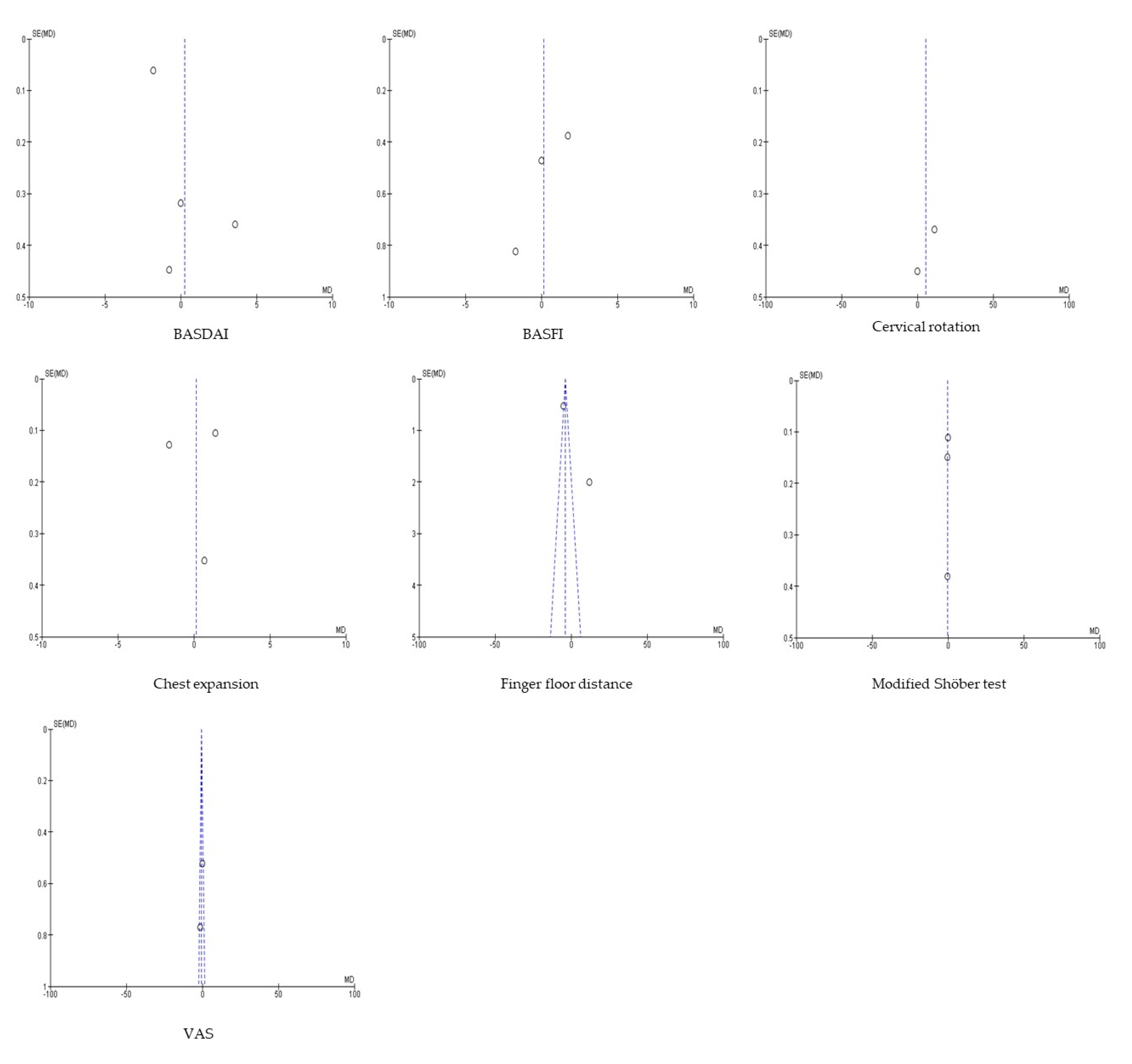
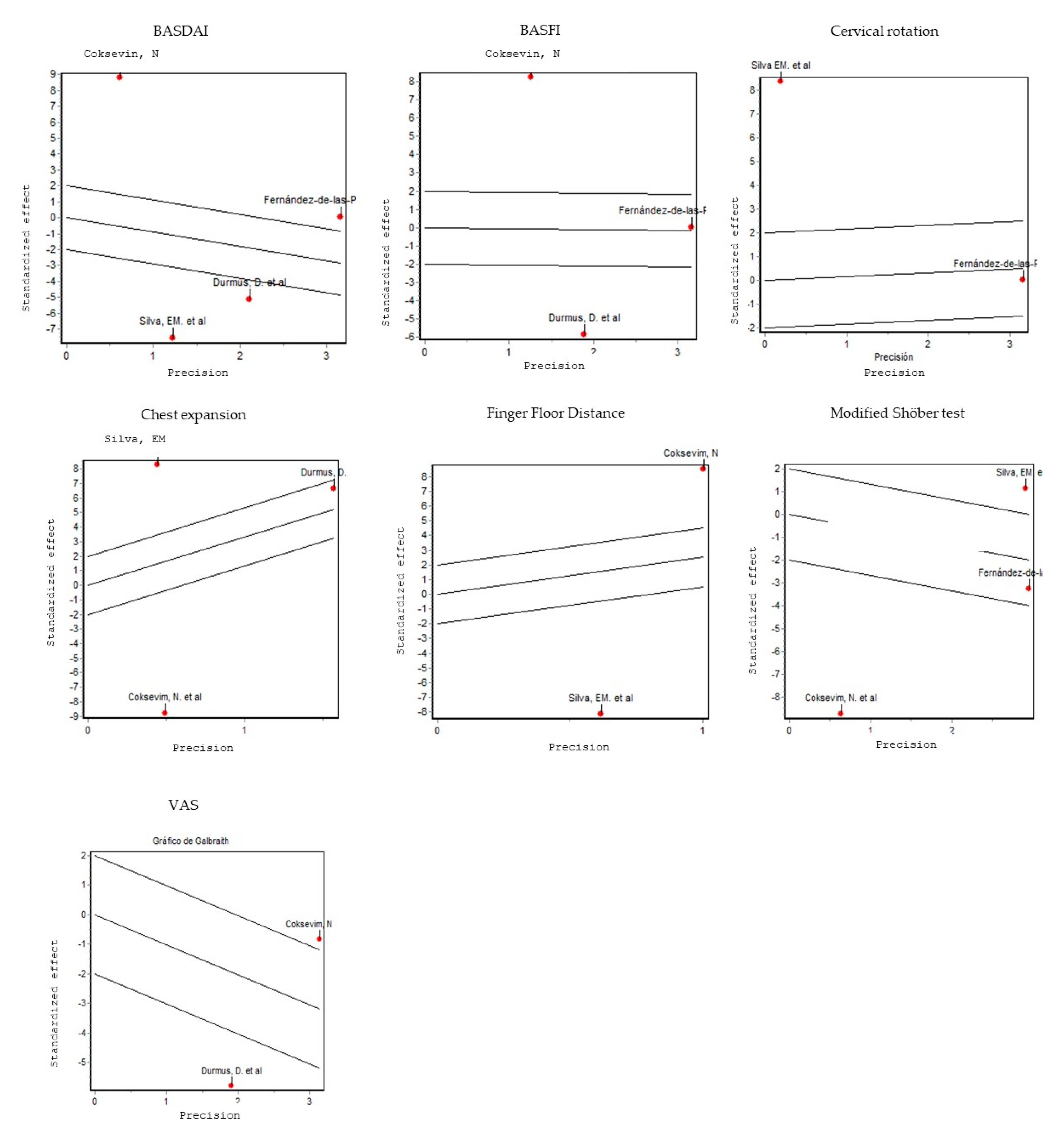
3.3. Risk of Bias, Sensitivity and Heterogeneity
3.4. Evaluation of Clinical Relevance
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Simone, D.; Al Mossawi, M.H.; Bowness, P. Progress in our understanding of the pathogenesis of ankylosing spondylitis. Rheumatology 2018, 57, vi4–vi9. [Google Scholar] [CrossRef] [PubMed]
- Smith, J.A. Update on ankylosing spondylitis: Current concepts in pathogenesis. Curr. Allergy Asthma Rep. 2014, 15. [Google Scholar] [CrossRef]
- Sandal, R.; Mishra, K.; Jandial, A.; Khadwal, A.; Malhotra, P. Ankylosing spondylitis and bamboo spine. Qjm Int. J. Med. 2018, 111, 913–914. [Google Scholar] [CrossRef]
- Silva, E.M.; Andrade, S.C.; Vilar, M.J. Evaluation of the effects of global postural reeducation in patients with ankylosing spondylitis. Rheumatol. Int. 2011, 32, 2155–2163. [Google Scholar] [CrossRef]
- Saracoglu, I.; Kurt, G.; Okur, E.O.; Afsar, E.; Seyyar, G.K.; Calik, B.B.; Taspinar, F. The effectiveness of specific exercise types on cardiopulmonary functions in patients with ankylosing spondylitis: A systematic review. Rheumatol. Int. 2016, 37, 409–421. [Google Scholar] [CrossRef]
- Bohn, R.; Cooney, M.; Deodhar, A.; Curtis, J.R.; Golembesky, A. Incidence and prevalence of axial spondyloarthritis: Methodologic challenges and gaps in the literature. Clin. Exp. Rheumatol. 2017, 36, 263–274. [Google Scholar]
- Van Der Heijde, D.; Sieper, J.; Maksymowych, W.P.; Lambert, R.G.W.; Chen, S.; Hojnik, M.; Anderson, J.K.; Pangan, A. Clinical and MRI remission in patients with nonradiographic axial spondyloarthritis who received long-term open-label adalimumab treatment: 3-year results of the ABILITY-1 trial. Arthritis Res. Ther. 2018, 20, 61. [Google Scholar] [CrossRef]
- Van Der Heijde, D.; Breban, M.; Halter, D.; DiVittorio, G.; Bratt, J.; Cantini, F.; Kary, S.; Pangan, A.L.; Kupper, H.; Rathmann, S.S.; et al. Maintenance of improvement in spinal mobility, physical function and quality of life in patients with ankylosing spondylitis after 5 years in a clinical trial of adalimumab. Rheumatology 2014, 54, 1210–1219. [Google Scholar] [CrossRef] [PubMed]
- Cuenca-Martínez, F.; Cortés-Amador, S.; Espí-López, G.V. Effectiveness of classic physical therapy proposals for chronic non-specific low back pain: A literature review. Phys. Ther. Res. 2018, 21, 16–22. [Google Scholar] [CrossRef] [PubMed]
- de Freitas, N.C.G.; Freire, C. Reeducação Postural global souchard e stretching global ativo no esporte. Man Ther. Posturol. Rehabil. J. 2013, 11, 597–604. [Google Scholar]
- Souchard, P.E. Rpg. Principios de la Reeducación Postural Global; Paidotribo: Barcelona, Spain, 2005; pp. 10–84. [Google Scholar]
- Ribeiro, F. A reeducação postural global é uma ferramenta útil no tratamento da incontinência urinária de esforço feminina? Rev Assoc Med Bras. 2008, 54, 3. [Google Scholar] [CrossRef] [PubMed]
- Soares, P.; Cabral, V.; Mendes, M.; Vieira, R.; Avolio, G.; Vale, R.G.D.S. Efeitos do programa escola de postura e reeducação postural global sobre a amplitude de movimento e níveis de dor em pacientes com lombalgia crônica. Rev. Andal. Med. Deport. 2016, 9, 23–28. [Google Scholar] [CrossRef]
- Dönmez, U.; Ozturk, C.; Kocanaogullari, H.; Gucenmez, S.; Hepguler, S. Do physical therapy modalities have additional benefit over exercise therapy in the management of ankylosing spondylitis? A randomized controlled trial. Ann Rheum Dis. 2014, 73 (Suppl. 2), 726–727. [Google Scholar] [CrossRef]
- Agosti, V.; Vitale, C.; Avella, D.; Rucco, R.; Santangelo, G.; Sorrentino, P.; Varriale, P.; Sorrentino, P. Erratum to: Effects of Global Postural Reeducation on gait kinematics in parkinsonian patients: A pilot randomized three-dimensional motion analysis study. Neurol. Sci. 2016, 37, 523–524. [Google Scholar] [CrossRef]
- Henriquez, L.; Palomer, L.; Leppe, J.; Tuttle, N. Changes in symptoms and resting position of jaw, atlas and axis in patients with TMJ dysfunction following Global Postural Reeducation. Man. Ther. 2016, 25, e103–e104. [Google Scholar] [CrossRef]
- Lawand, P.; Júnior, I.L.; Jones, A.; Sardim, C.; Ribeiro, L.H.; Natour, J. Effect of a muscle stretching program using the global postural reeducation method for patients with chronic low back pain: A randomized controlled trial. Jt. Bone Spine 2015, 82, 272–277. [Google Scholar] [CrossRef]
- Castagnoli, C.; Cecchi, F.; Del Canto, A.; Paperini, A.; Boni, R.; Pasquini, G.; Vannetti, F.; Macchi, C. Effects in short and long term of global postural reeducation (gpr) on chronic low back pain: A controlled study with one-year follow-up. Sci. World J. 2015, 2015, 1–8. [Google Scholar] [CrossRef]
- de Melo, V.G.A.; Castro, L.D.; Moura, C.V.E.; Da Conceição, T.S.C.R. A influência do método de reeducação postural global sobre a flexibilidade dos músculos da cadeia posterior. Fisioter Bras. 2016, 15. [Google Scholar] [CrossRef]
- Lawand, P.A.; Jones, A.; Sardim, C.C.; Ribeiro, L.H.; Lombardi, I.; Natour, J. AB0664 Global postural reeducation to treat chronic low back pain: Randomized, controlled trial. Ann. Rheum. Dis. 2013, 72. [Google Scholar] [CrossRef]
- Lozano-Quijada, C.; Poveda-Pagán, E.J.; Segura, J.V.; Hernández-Sánchez, S.; Prieto-Castelló, M.J. Changes in postural sway after a single global postural reeducation session in university students: A randomized controlled trial. J. Manip. Physiol. Ther. 2017, 40, 467–476. [Google Scholar] [CrossRef]
- Todri, J.; Lena, O.; Martínez, G.J.L. An experimental pilot study of Global Postural Reeducation concerning the cognitive approach of patients with Alzheimer’s disease. Am. J. Alzheimer’s Dis. Other Dementiasr 2019, 35. [Google Scholar] [CrossRef] [PubMed]
- de Oliveira, S.R.L.; Natsumi, H.M.L.; Lobato, S.L.; Dias, M.L.; De Souza, S.M.C.; Barbosa, R.R.S. Influence of global postural reeducation method on respiratory muscle strength and parkinsonian quality of life. Man. Ther. Posturol. Rehabil. J. 2018, 15. [Google Scholar] [CrossRef][Green Version]
- Coksevim, N.H.; Durmus, D.; Kuru, O. Effects of global postural reeducation exercise and anti-TNF treatments on disease activity, function, fatigue, mobility, sleep quality and depression in patients with active Ankylosing spondylitis: A prospective follow-up study. J. Back Musculoskelet. Rehabilit. 2018, 31, 1005–1012. [Google Scholar] [CrossRef] [PubMed]
- De Amorim, C.S.M.; Gracitelli, M.E.C.; Marques, A.P.; Alves, C. Effectiveness of global postural reeducation compared to segmental exercises on function, pain, and quality of life of patients with scapular dyskinesis associated with neck pain: A preliminary clinical trial. J. Manip. Physiol. Ther. 2014, 37, 441–447. [Google Scholar] [CrossRef]
- Todri, J.; Lena, O.; Gil, J.M. A single blind randomized controlled trial of global postural re-education: Cognitive effects on Alzheimer disease patients. Eur. J. Psychiatry 2019, 33, 83–90. [Google Scholar] [CrossRef]
- Bonetti, F.; Curti, S.; Mattioli, S.; Mugnai, R.; Vanti, C.; Violante, F.S.; Pillastrini, P. Effectiveness of a ’global postural reeducation’ program for persistent low back pain: A non-randomized controlled trial. BMC Musculoskelet. Disord. 2010, 11, 285. [Google Scholar] [CrossRef]
- Fernández-de-las-Peñas, C.; Alonso-Blanco, C.; Morales-Cabezas, M.; Miangolarra-Page, J.C. Two exercise interventions for the management of patients with ankylosing spondylitis: A randomized controlled trial. Am. J. Phys. Med. Rehabilit. 2005, 84, 407–419. [Google Scholar] [CrossRef]
- Mota, Y.L.; Barreto, S.L.; Bin, P.R.; Simões, H.G.; Campbell, C.S.G. Cardiovascular responses in the seated posture of the Global Postural Reeducation (GPR) method. Braz. J. Phys. Ther. 2008, 12. [Google Scholar] [CrossRef]
- Chang, W.D.; Tsou, Y.A.; Lee, C.L. Comparison between specific exercises and physical therapy for managing patients with ankylosing spondylitis: A meta-analysis of randomized controlled trials. Int. J. Clin. Exp. Med. 2016, 9, 17028–17039. [Google Scholar] [CrossRef]
- Ferreira, G.E.; Barreto, R.G.P.; Robinson, C.C.; Plentz, R.D.M.; Silva, M.F. Global postural reeducation for patients with musculoskeletal conditions: A systematic review of randomized controlled trials. Braz. J. Phys. Ther. 2016, 20, 194–205. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. PLoS Med. 2009, 6, e1000100. [Google Scholar] [CrossRef] [PubMed]
- Haywood, K.L.; Garratt, A.M.; Dziedzic, K.; Dawes, P.T. Generic measures of health-related quality of life in ankylosing spondylitis: Reliability, validity and responsiveness. Rheumatology 2002, 41, 1380–1387. [Google Scholar] [CrossRef] [PubMed]
- Navarro, S.F.; Ariza, A.R.; Hernández, C.B. La versión española del BASDAI es fiable y se correlaciona con la actividad de la enfermedad en pacientes con espondilitis anquilosante. Rev. Española Reumatol. Órgano Soc. Española Reumatol. 2004, 31, 372. [Google Scholar]
- Vera, M.R.; Gutiérrez-González, L.A.; Maldonado, I.; Al Snih, S. The reliability and validity of a venezuelan version of the bath ankylosing spondylitis functional index (BASFI) and bath ankylosing spondylitis disease activity index (BASDAI). Reumatología Clínica 2019, 15, 223–228. [Google Scholar] [CrossRef]
- Gopalakrishna, G.; Mustafa, R.A.; Davenport, C.; Scholten, R.J.; Hyde, C.; Brozek, J.; Schünemann, H.J.; Bossuyt, P.M.; Leeflang, M.M.; Langendam, M.W. Applying grading of recommendations assessment, development and evaluation (GRADE) to diagnostic tests was challenging but doable. J. Clin. Epidemiol. 2014, 67, 760–768. [Google Scholar] [CrossRef]
- Durmus, D.; Alayli, G.; Uzun, O.; Tander, B.; Cantürk, F.; Bek, Y.; Erkan, L.; Alaylı, G. Effects of two exercise interventions on pulmonary functions in the patients with ankylosing spondylitis. Jt. Bone Spine 2009, 76, 150–155. [Google Scholar] [CrossRef]
- A Martins, N.; Furtado, G.E.; Campos, M.J.; Leitão, J.C.; Filaire, E.; Ferreira, J.P. Exercise and ankylosing spondylitis with New York modified criteria: A systematic review of controlled trials with meta-analysis. Acta Reum. Port. 2014, 39, 298–308. [Google Scholar]

| Databases and Total Found Articles | Search |
|---|---|
PubMed: 43 *PEDro: 14 *SciELO: 18 *WoS: 74 | 1. (“Pain”(Mesh) OR “Acute Pain”(Mesh) OR “Pelvic Girdle Pain”(Mesh) OR “Musculoskeletal Pain”(Mesh) OR “Chronic Pain”(Mesh) OR “Visceral Pain”(Mesh) OR “Nociceptive Pain”(Mesh) OR “Pain Perception”(Mesh) OR “Pain, Referred”(Mesh) OR “Shoulder Pain”(Mesh) OR “Neck Pain”(Mesh) OR “Pelvic Pain”(Mesh)) AND “Global Postural Reeducation” 2. (“Range of Motion, Articular”(Mesh)) AND “Global Postural Reeducation” 3. (“Quality of Life/psychology”(Major)) AND “Global Postural Reeducation” 4. (“Ventilation”(Mesh) OR “Respiration”(Mesh) OR “Ventilation-Perfusion Ratio”(Mesh) OR “Pulmonary Ventilation”(Mesh) OR “Maximal Voluntary Ventilation”(Mesh) OR “Respiration, Artificial”(Mesh)) AND “Global Postural Reeducation” 5. (“Spondylitis”(Mesh) OR “Spondylitis, Ankylosing”(Mesh) OR “Spondylarthropathies”(Mesh) spondyloarthritis ankylopoietica OR ankylosing spondylarthritis OR ankylosing spondylarthritides OR spondylarthritides, ankylosing OR spondylarthritis, ankylosing OR ankylosing spondylitis OR spondylarthritis ankylopoietica OR bechterew disease OR bechterew’s disease OR bechterew s disease OR marie-struempell disease OR marie struempell disease OR rheumatoid spondylitis OR spondylitis, rheumatoid OR spondylitis ankylopoietica OR ankylosing spondyloarthritis OR ankylosing spondylarthritides OR spondylarthritides, ankylosing OR spondyloarthritis, ankylosing) AND “Global Postural Reeducation” 6. “Global Postural Reeducation” |
| Author (Year) | Intervention(s) | Control | Primary Outcome Measure | Secondary Outcome Measure | Follow-Up | Results |
|---|---|---|---|---|---|---|
| Coksevim, N et al., (2018) [24] | Anti-TNF therapy plus GPR program and conventional exercise therapy | Conventional exercises | BASDAI 1, BASFI 2, chest expansion, finger-floor distance, Modified Shöber test and VAS 3 | 6MWD 4, MAF 5, PSQI 6 and BDI7 | 3 months | The improvements in all parameters were better in the anti-TNF groups than in the control group regarding the change scores between BT 15-AT 16. The anti-TNF plus GPR exercise therapy resulted in greater improvements than the anti-TNF plus conventional exercise therapy in pain, walking performance, mobility parameters. |
| Durmus, D et al., (2008) [37] | Conventional exercise regimen and GPR | Conventional exercises | BASDAI 1, BASFI 2, Chest expansion and VAS 3 | 6MW 4, FVC 8, FEV1 9, PEF 10, VC 11 and MVV 12 | 3 months | The intergroup comparison (pre-post scores) in both exercise groups showed that the GPR group obtained more improvement than the conventional exercise group in FVC, FEV1, and PEF parameters. |
| Fernández-de-las-Peñas, C et al., (2005) [28] | GRP | Conventional protocol of physical therapy in AS | BASDAI 1, BASFI 2, cervical rotation and modified Schöber test | Tragus to wall distance, lumbar side flexion, and intermalleolar distance | 4 months | The intergroup comparison between the improvement (pre-post scores) in both groups showed that the GPR group obtained a greater improvement than the control group in all the clinical measures of cervical rotation and modified Schöber test lumbar side flexion, and intermalleolar distance, as well as in the BASFI index. |
| Silva, EM. et al., (2012) [4] | GPR | Conventional exercise | BASDAI 1, chest expansion and VAS 3 | Morning stiffness, spine mobility, HAQ- S 13 and SF-36 14. | 4 months | In the inter-group comparison, there was significantly more improvement in the GPR group in all measures, except for the finger-floor distance (p = 0.12). |
| Evaluation Criteria (Items) 1 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | Total Score |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Author-Year | ||||||||||||
| Coksevim, N. et al.-2018 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 4 |
| Silva, E. et al.-2012 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 4 |
| Durmus, D. et al.-2008 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 4 |
| Fernández-de-las-Peñas, C. et al.-2005 | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 6 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gonzalez-Medina, G.; Perez-Cabezas, V.; Marin-Paz, A.-J.; Galán-Mercant, A.; Ruiz-Molinero, C.; Jimenez-Rejano, J.J. Effectiveness of Global Postural Reeducation in Ankylosing Spondylitis: A Systematic Review and Meta-Analysis. J. Clin. Med. 2020, 9, 2696. https://doi.org/10.3390/jcm9092696
Gonzalez-Medina G, Perez-Cabezas V, Marin-Paz A-J, Galán-Mercant A, Ruiz-Molinero C, Jimenez-Rejano JJ. Effectiveness of Global Postural Reeducation in Ankylosing Spondylitis: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2020; 9(9):2696. https://doi.org/10.3390/jcm9092696
Chicago/Turabian StyleGonzalez-Medina, Gloria, Veronica Perez-Cabezas, Antonio-Jesus Marin-Paz, Alejandro Galán-Mercant, Carmen Ruiz-Molinero, and Jose Jesus Jimenez-Rejano. 2020. "Effectiveness of Global Postural Reeducation in Ankylosing Spondylitis: A Systematic Review and Meta-Analysis" Journal of Clinical Medicine 9, no. 9: 2696. https://doi.org/10.3390/jcm9092696
APA StyleGonzalez-Medina, G., Perez-Cabezas, V., Marin-Paz, A.-J., Galán-Mercant, A., Ruiz-Molinero, C., & Jimenez-Rejano, J. J. (2020). Effectiveness of Global Postural Reeducation in Ankylosing Spondylitis: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine, 9(9), 2696. https://doi.org/10.3390/jcm9092696







