Short-Term Effects of a Myofunctional Appliance on Atypical Swallowing and Lip Strength: A Prospective Study
Abstract
1. Introduction
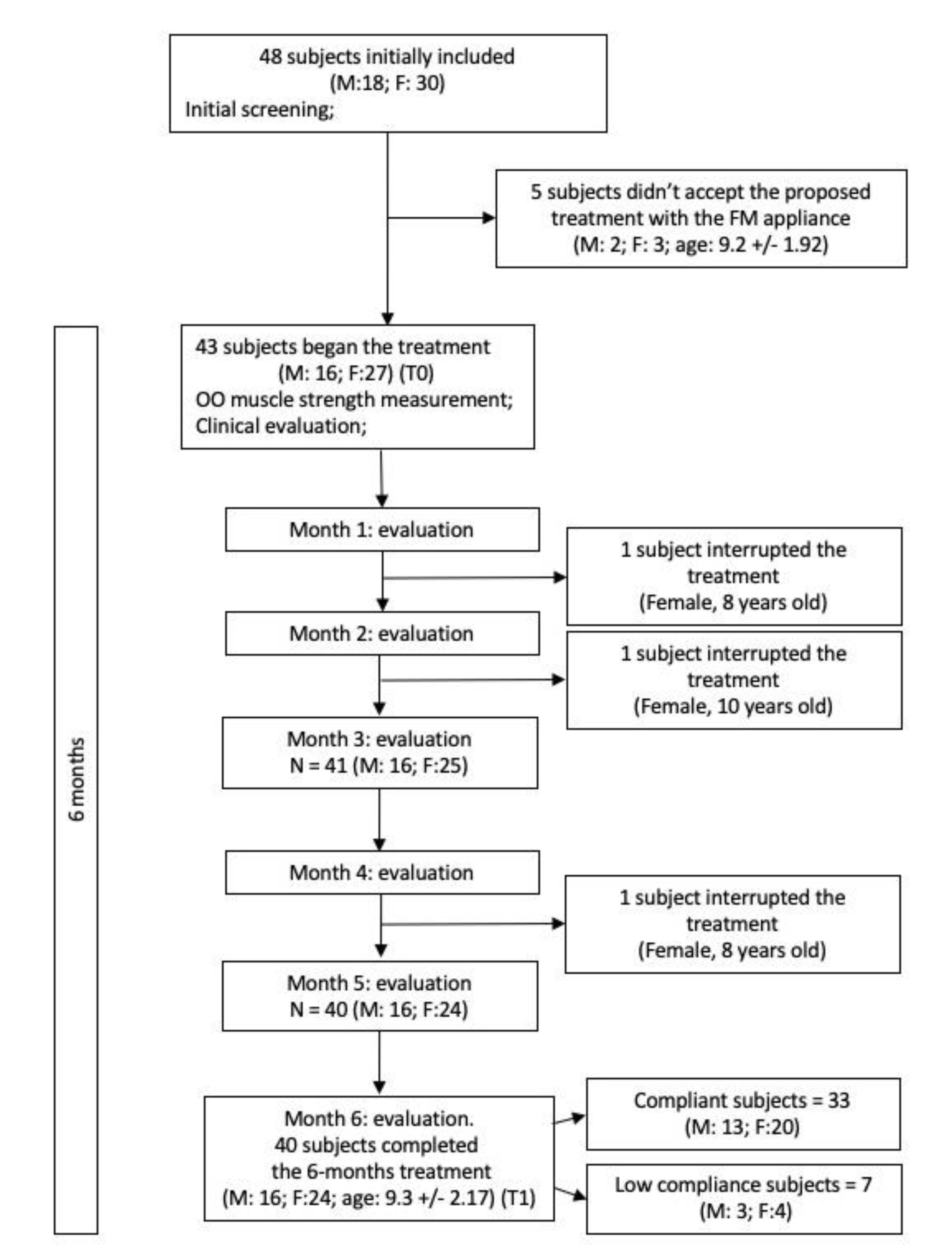
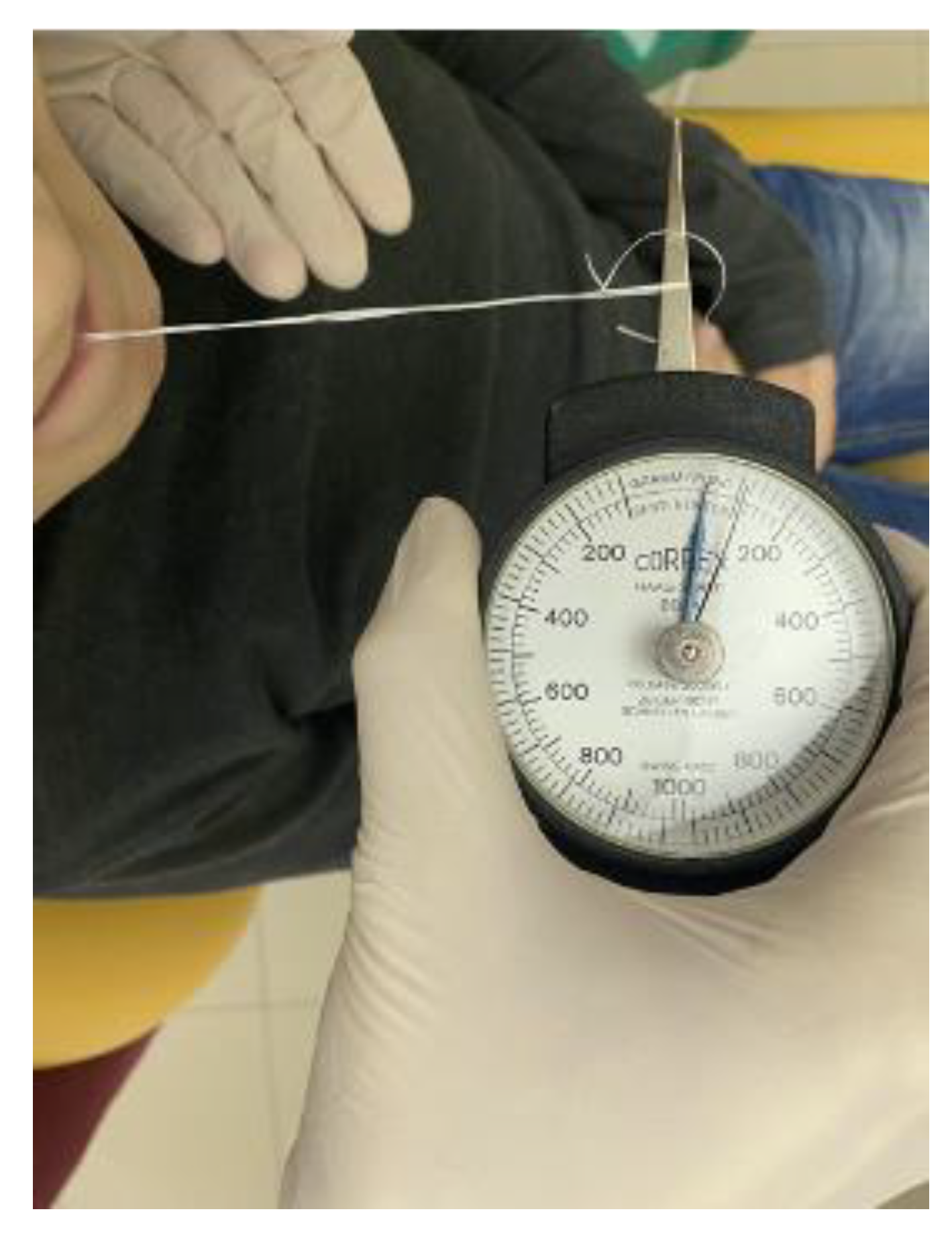
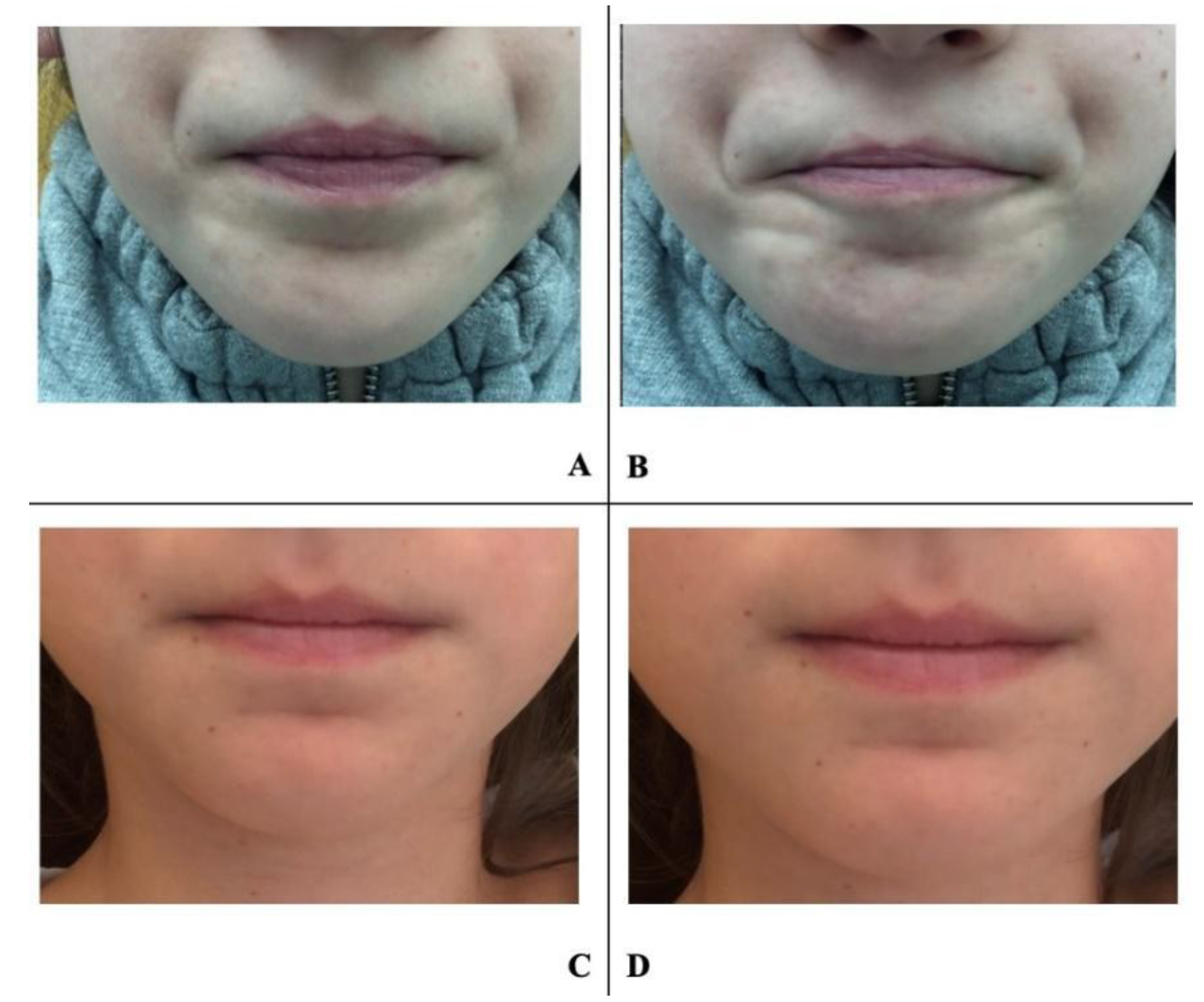
2. Experimental Section
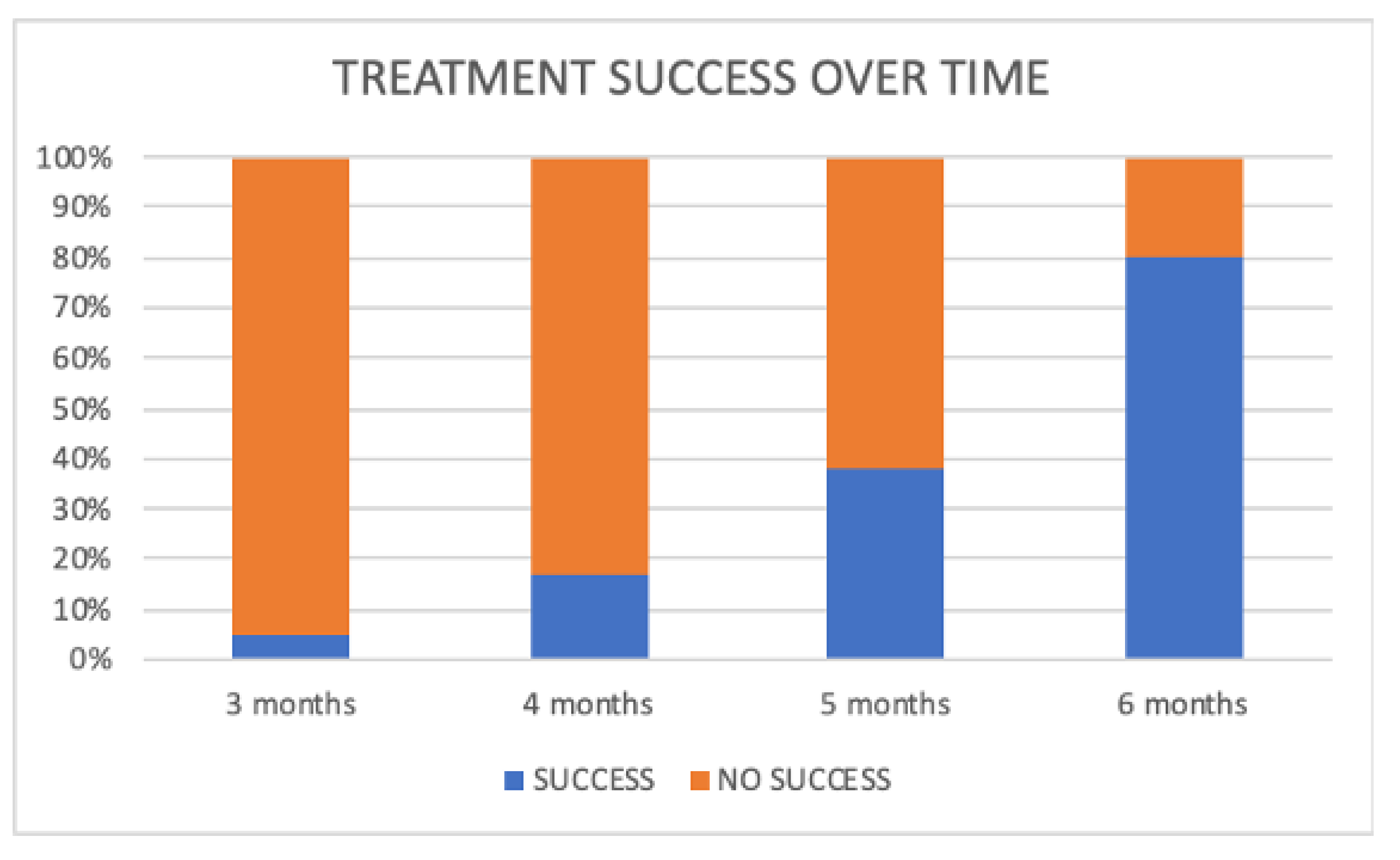
3. Results
4. Discussion
Limitations of the Study
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Fellus, P. Dynamic and postural changes in the tongue: Influence on facial growth. Mondo Ortod. 1989, 14, 791–798. [Google Scholar]
- Fellus, P. From digit-sucking-cum-deglutition to deglutition in dentate subjects. Orthod. Fr. 2016, 87, 89–90. [Google Scholar] [CrossRef]
- Fellus, P. Tongue disfunction and abnormal development. Orthod. Fr. 2006, 77, 105–112. [Google Scholar] [CrossRef]
- Begnoni, G.; Cadenas de Llano-Pérula, M.; Dellavia, C.; Willems, G. Cephalometric traits in children and adolescents with and without atypical swallowing: A retrospective study. Eur. J. Paediatr. Dent. 2020, 21, 46–52. [Google Scholar]
- Condò, R.; Costacurta, M.; Perugia, C.; Docimo, R. Atypical deglutition: Diagnosis and interceptive treatment. A clinical study. Eur. J. Paediatr. Dent. 2012, 13, 209–214. [Google Scholar]
- Maspero, C.; Prevedello, C.; Giannini, L.; Galbiati, G.; Farronato, G. Atypical swallowing: A review. Minerva Stomatol. 2014, 63, 217–227. [Google Scholar] [PubMed]
- Schmid, K.M.; Kugler, R.; Nalabothu, P.; Bosch, C.; Verna, C. The effect of pacifier sucking on orofacial structures: A systematic literature review. Prog. Orthod. 2018, 19, 8. [Google Scholar] [CrossRef] [PubMed]
- Caruso, S.; Nota, A.; Darvizeh, A.; Severino, M.; Gatto, R.; Tecco, S. Poor oral habits and malocclusions after usage of orthodontic pacifiers: An observational study on 3-5 years old children. BMC Pediatr. 2019, 19, 294. [Google Scholar] [CrossRef] [PubMed]
- Begnoni, G.; Dellavia, C.; Pellegrini, G.; Scarponi, L.; Schindler, A.; Pizzorni, N. The efficacy of myofunctional therapy in patients with atypical swallowing. Eur. Arch. Otorhinolaryngol. 2020, 277, 2501–2511. [Google Scholar] [CrossRef] [PubMed]
- Tecco, S.; Baldini, A.; Mummolo, S.; Marchetti, E.; Giuca, M.R.; Marzo, G.; Gherlone, E.F. Frenulectomy of the tongue and the influence of rehabilitation exercises on the sEMG activity of masticatory muscles. J. Electromyogr. Kinesiol. 2015, 25, 619–628. [Google Scholar] [CrossRef] [PubMed]
- Machado, A.J.; Crespo, A.N. Cephalometric evaluation of the airway space and hyoid bone in children with normal and atypical deglutition: Correlation study. Sao Paulo Med. J. 2012, 130, 236–241. [Google Scholar] [CrossRef] [PubMed]
- Nota, A.; Tecco, S.; Ehsani, S.; Padulo, J.; Baldini, A. Postural stability in subjects with temporomandibular disorders and healthy controls: A comparative assessment. J. Electromyogr. Kinesiol. 2017, 37, 21–24. [Google Scholar] [CrossRef] [PubMed]
- Baldini, A.; Nota, A.; Cravino, G.; Cioffi, C.; Rinaldi, A.; Cozza, P. Influence of vision and dental occlusion on body posture in pilots. Aviat. Space. Environ. Med. 2013, 84, 823–827. [Google Scholar] [CrossRef] [PubMed]
- Saccucci, M.; Tettamanti, L.; Mummolo, S.; Polimeni, A.; Festa, F.; Tecco, S. Scoliosis and dental occlusion: A review of the literature. Scoliosis 2011, 6, 15. [Google Scholar] [CrossRef]
- Tecco, S.; Mummolo, S.; Marchetti, E.; Tetè, S.; Campanella, V.; Gatto, R.; Gallusi, G.; Tagliabue, A.; Marzo, G. SEMG activity of masticatory, neck, and trunk muscles during the treatment of scoliosis with functional braces. A longitudinal controlled study. J. Electromyogr. Kinesiol. 2011, 21, 885–892. [Google Scholar] [CrossRef]
- Tecco, S.; Caputi, S.; Festa, F. Evaluation of cervical posture following palatal expansion: A 12-month follow-up controlled study. Eur. J. Orthod. 2007, 29, 45–51. [Google Scholar] [CrossRef]
- Saccucci, M.; Tecco, S.; Ierardoa, G.; Luzzi, V.; Festa, F.; Polimeni, A. Effects of interceptive orthodontics on orbicular muscle activity: A surface electromyographic study in children. J. Electromyogr. Kinesiol. 2011, 21, 665–671. [Google Scholar] [CrossRef]
- Takada, J.; Miyamoto, J.J.; Sato, C.; Dei, A.; Moriyama, K. Comparison of EMG activity and blood flow during graded exertion in the orbicularis oris muscle of adult subjects with and without lip incompetence: A cross-sectional survey. Eur. J. Orthod. 2018, 40, 304–311. [Google Scholar] [CrossRef]
- Hur, M.-S. Anatomical connections between the buccinator and the tendons of the temporalis. Ann. Anat. Anat. Anzeiger 2017, 214, 63–66. [Google Scholar] [CrossRef]
- Jungbauer, R.; Koretsi, V.; Proff, P.; Rudzki, I.; Kirschneck, C. Twenty-year follow-up of functional treatment with a bionator appliance: A retrospective dental cast analysis. Angle Orthod. 2020, 90, 209–215. [Google Scholar] [CrossRef]
- Tecco, S.; Farronato, G.; Salini, V.; Di Meo, S.; Filippi, M.R.; Festa, F.; D’Attilio, M. Evaluation of cervical spine posture after functional therapy with FR-2: A longitudinal study. Cranio 2005, 23, 53–66. [Google Scholar] [CrossRef] [PubMed]
- Leite, J.S.; Matiussi, L.B.; Salem, A.C.; Provenzano, M.G.A.; Ramos, A.L. Effects of palatal crib and bonded spurs in early treatment of anterior open bite: A prospective randomized clinical study. Angle Orthod. 2016, 86, 734–739. [Google Scholar] [CrossRef] [PubMed]
- Giuca, M.R.; Pasini, M.; Pagano, A.; Mummolo, S.; Vanni, A. Longitudinal study on a rehabilitative model for correction of atypical swallowing. Eur. J. Paediatr. Dent. 2008, 9, 170–174. [Google Scholar] [PubMed]
- Bigenzahn, W.; Fischman, L.; Mayrhofer-Krammel, U. Myofunctional Therapy in Patients with Orofacial Dysfunctions Affecting Speech. Folia Phoniatr. Logop. 1992, 44, 238–244. [Google Scholar] [CrossRef]
- Di Vecchio, S.; Manzini, P.; Candida, E.; Gargari, M. Froggy mouth: A new myofunctional approach to atypical swallowing. Eur. J. Paediatr. Dent. 2019, 20, 33–37. [Google Scholar]
- Begnoni, G.; Cadenas de Llano-Pérula, M.; Willems, G.; Pellegrini, G.; Musto, F.; Dellavia, C. Electromyographic analysis of the oral phase of swallowing in subjects with and without atypical swallowing: A case-control study. J. Oral Rehabil. 2019, 46, 927–935. [Google Scholar] [CrossRef]
- da Silva, G.R.; Rech, R.S.; Vidor, D.C.G.M.; Santos, K.W. Dos Influence of Masticatory Behavior on Muscle Compensations During the Oral Phase of Swallowing of Smokers. Int. Arch. Otorhinolaryngol. 2019, 23, e317–e321. [Google Scholar]
- Berggren, K.N.; Hung, M.; Dixon, M.M.; Bounsanga, J.; Crockett, B.; Foye, M.D.; Gu, Y.; Campbell, C.; Butterfield, R.J.; Johnson, N.E. Orofacial strength, dysarthria, and dysphagia in congenital myotonic dystrophy. Muscle Nerve 2018, 58, 413–417. [Google Scholar] [CrossRef]
- Cheng, H.-C.; Hu, H.-T.; Chang, Y.-C. Effectiveness of Enzyme Dentifrices on Oral Health in Orthodontic Patients: A Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2019, 16, 2243. [Google Scholar] [CrossRef]
- Mummolo, S.; Marchetti, E.; Giuca, M.R.; Gallusi, G.; Tecco, S.; Gatto, R.; Marzo, G. In-office bacteria test for a microbial monitoring during the conventional and self-ligating orthodontic treatment. Head Face Med. 2013, 9, 7. [Google Scholar] [CrossRef]
- Sfondrini, M.F.; Debiaggi, M.; Zara, F.; Brerra, R.; Comelli, M.; Bianchi, M.; Pollone, S.R.; Scribante, A. Influence of lingual bracket position on microbial and periodontal parameters in vivo. J. Appl. Oral Sci. 2012, 20, 357–361. [Google Scholar] [CrossRef] [PubMed]
- Mummolo, S.; Tieri, M.; Nota, A.; Caruso, S.; Darvizeh, A.; Albani, F.; Gatto, R.; Marzo, G.; Marchetti, E.; Quinzi, V.; et al. Salivary concentrations of Streptococcus mutans and Lactobacilli during an orthodontic treatment. An observational study comparing fixed and removable orthodontic appliances. Clin. Exp. Dent. Res. 2020, 6, 181–187. [Google Scholar] [CrossRef] [PubMed]
- Mummolo, S.; Nota, A.; Albani, F.; Marchetti, E.; Gatto, R.; Marzo, G.; Quinzi, V.; Tecco, S. Salivary levels of Streptococcus mutans and Lactobacilli and other salivary indices in patients wearing clear aligners versus fixed orthodontic appliances: An observational study. PLoS ONE 2020, 15, e0228798. [Google Scholar] [CrossRef] [PubMed]

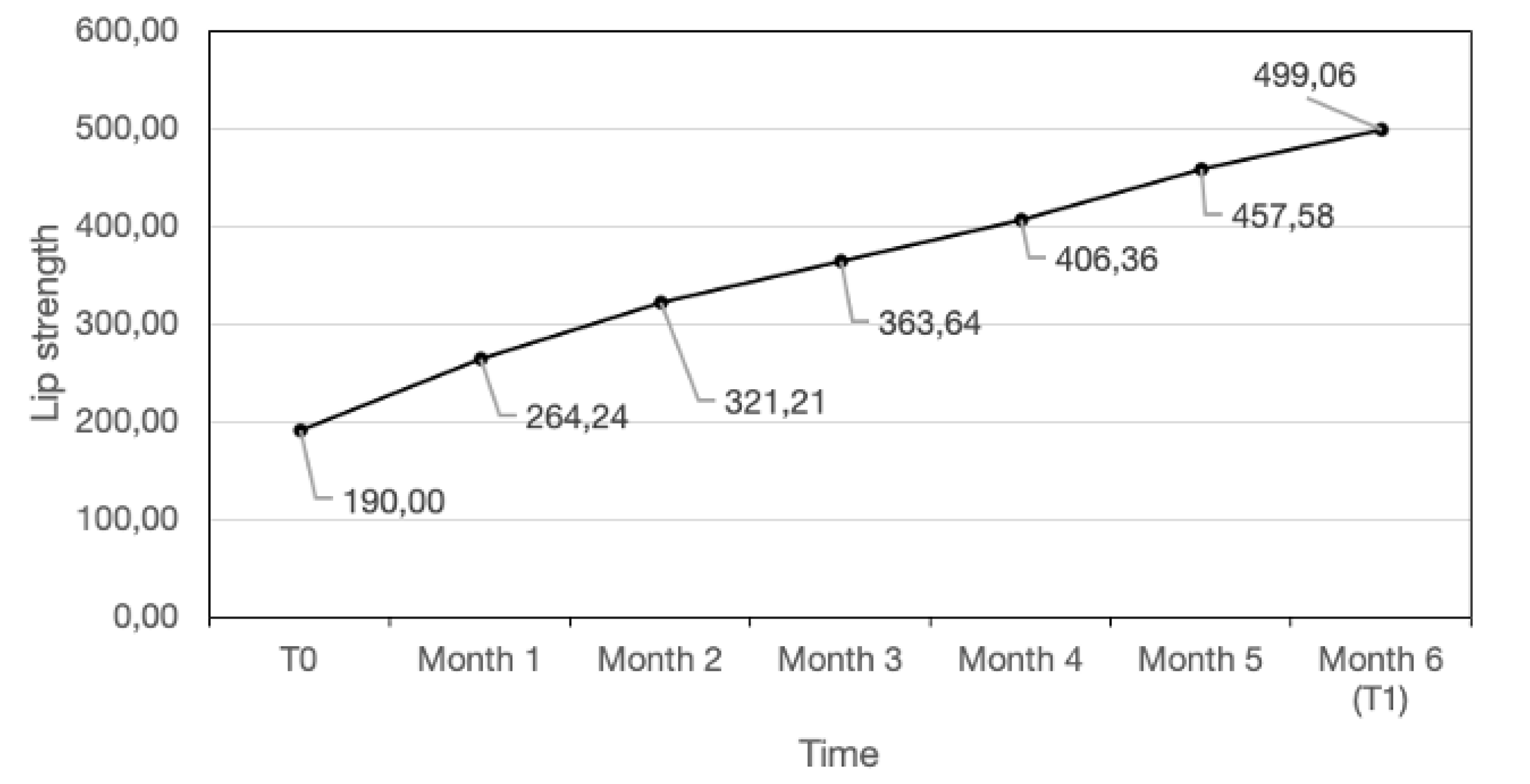
| Lip Strength | Lip Strength | t0–t1 | Paired Sample’ t Test (p) | |
|---|---|---|---|---|
| at t0 | at t1 | Difference | ||
| (centiNewton) | (centiNewton) | Mean ± SD | ||
| Mean ± SD | Mean ± SD | |||
| Compliant Children (n = 33) | 190.30 ± 86.04 | 489.39 ± 123.36 | −299.09 ± 128.63 | −12.23 (p < 0.001) |
| Low compliant Children (n = 7) | 231.43 ± 144.62 | 408.57 ± 91.55 | 177.14 ± 140.20 | 2.73 (p = 0.015) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Quinzi, V.; Nota, A.; Caggiati, E.; Saccomanno, S.; Marzo, G.; Tecco, S. Short-Term Effects of a Myofunctional Appliance on Atypical Swallowing and Lip Strength: A Prospective Study. J. Clin. Med. 2020, 9, 2652. https://doi.org/10.3390/jcm9082652
Quinzi V, Nota A, Caggiati E, Saccomanno S, Marzo G, Tecco S. Short-Term Effects of a Myofunctional Appliance on Atypical Swallowing and Lip Strength: A Prospective Study. Journal of Clinical Medicine. 2020; 9(8):2652. https://doi.org/10.3390/jcm9082652
Chicago/Turabian StyleQuinzi, Vincenzo, Alessandro Nota, Eleonora Caggiati, Sabina Saccomanno, Giuseppe Marzo, and Simona Tecco. 2020. "Short-Term Effects of a Myofunctional Appliance on Atypical Swallowing and Lip Strength: A Prospective Study" Journal of Clinical Medicine 9, no. 8: 2652. https://doi.org/10.3390/jcm9082652
APA StyleQuinzi, V., Nota, A., Caggiati, E., Saccomanno, S., Marzo, G., & Tecco, S. (2020). Short-Term Effects of a Myofunctional Appliance on Atypical Swallowing and Lip Strength: A Prospective Study. Journal of Clinical Medicine, 9(8), 2652. https://doi.org/10.3390/jcm9082652









