Retinal Response of Low Myopes during Orthokeratology Treatment
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Subjects
2.2. Contact Lenses
2.3. Electrophysiology
2.4. Statistical Analysis
3. Results
3.1. Subjects and Study Design
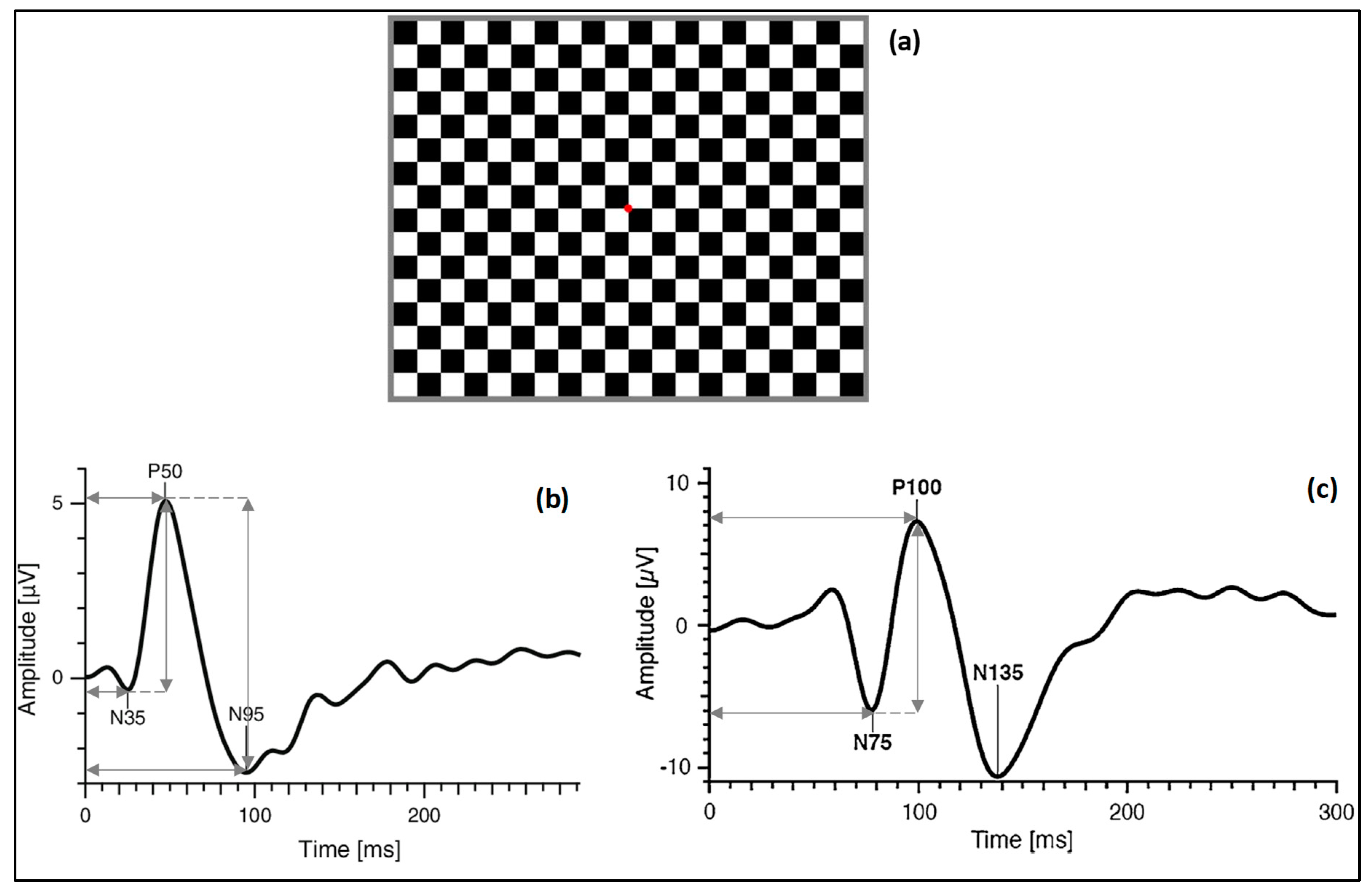
3.2. Pattern Electroretinography (PERG)
3.3. Visual Evoked Potential (VEP)
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Si, J.K.; Tang, K.; Bi, H.S.; Guo, D.D.; Guo, J.G.; Wang, X.R. Orthokeratology for myopia control: A meta-analysis. Optom. Vis. Sci. 2015, 92, 252–257. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.M.; Xie, P. The safety of orthokeratology—A systematic review. Eye Contact Lens 2016, 42, 35–42. [Google Scholar] [CrossRef] [PubMed]
- Alharbi, A.; Swarbrick, H.A. The effects of overnight orthokeratology lens wear on corneal thickness. Investig. Ophthalmol. Vis. Sci. 2003, 44, 2518–2523. [Google Scholar] [CrossRef] [PubMed]
- Queirós, A.; González-Méijome, J.M.; Villa-Collar, C.; Gutiérrez, A.R.; Jorge, J. Local steepening in peripheral corneal curvature after corneal refractive therapy and LASIK. Optom. Vis. Sci. 2010, 87, 432–439. [Google Scholar] [CrossRef]
- Kakita, T.; Hiraoka, T.; Oshika, T. Influence of overnight orthokeratology on axial elongation in childhood myopia. Investig. Ophthalmol. Vis. Sci. 2011, 52, 2170–2174. [Google Scholar] [CrossRef]
- Queirós, A.; Villa-Collar, C.; Gutiérrez, Á.R.; Jorge, J.; Ribeiro-Queirós, M.S.; Peixoto-de-Matos, S.C.; González-Méijome, J.M. Anterior and posterior corneal elevation after orthokeratology and standard and customized LASIK surgery. Eye Contact Lens 2011, 37, 354–358. [Google Scholar] [CrossRef]
- Queirós, A.; Amorim-de-Sousa, A.; Lopes-Ferreira, D.; Villa-Collar, C.; Gutiérrez, Á.R.; González-Méijome, J.M. Relative peripheral refraction across 4 meridians after orthokeratology and LASIK surgery. Eye Vis. 2018, 5, 12. [Google Scholar] [CrossRef]
- González-Méijome, J.M.; Faria-Ribeiro, M.A.; Lopes-Ferreira, D.P.; Fernandes, P.; Carracedo, G.; Queiros, A. Changes in Peripheral Refractive Profile after Orthokeratology for Different Degrees of Myopia. Curr. Eye Res. 2016, 41, 199–207. [Google Scholar] [CrossRef]
- Queirós, A.; Lopes-Ferreira, D.; González-Méijome, J.M. Astigmatic Peripheral Defocus with Different Contact Lenses: Review and Meta-Analysis. Curr. Eye Res. 2016, 41, 1005–1015. [Google Scholar] [CrossRef]
- Faria-Ribeiro, M.; Belsue, R.N.; López-Gil, N.; González-Méijome, J.M. Morphology, topography, and optics of the orthokeratology cornea. J. Biomed. Opt. 2016, 21, 075011. [Google Scholar] [CrossRef]
- Queirós, A.; Manuel González-Méijome, J.; Jorge, J.; Villa-Collar, C.; Gutiérrez, A.R. Peripheral Refraction in Myopic Patients After Orthokeratology. Optom. Vis. Sci. 2010, 87, 323–329. [Google Scholar] [CrossRef] [PubMed]
- Benavente-Pérez, A.; Nour, A.; Troilo, D. Axial eye growth and refractive error development can be modified by exposing the peripheral retina to relative myopic or hyperopic defocus. Investig. Ophthalmol. Vis. Sci. 2014, 55, 6765–6773. [Google Scholar] [CrossRef] [PubMed]
- Smith, E.L., III; Kee, C.S.; Ramamirtham, R.; Qiao-Grider, Y.; Hung, L.F. Peripheral vision can influence eye growth and refractive development in infant monkeys. Investig. Ophthalmol. Vis. Sci. 2005, 46, 3965–3972. [Google Scholar] [CrossRef] [PubMed]
- Smith, E.L., III; Ramamirtham, R.; Qiao-Grider, Y.; Hung, L.F.; Huang, J.; Kee, C.S.; Coats, D.; Paysse, E. Effects of foveal ablation on emmetropization and form-deprivation myopia. Investig. Ophthalmol. Vis. Sci. 2007, 48, 3914–3922. [Google Scholar] [CrossRef]
- Holder, G.E.; Brigell, M.G.; Hawlina, M.; Meigen, T.; Vaegan Bach, M. ISCEV standard for clinical pattern electroretinography—2007 update. Doc. Ophthalmol. 2007, 114, 111–116. [Google Scholar] [CrossRef]
- Odom, J.V.; Bach, M.; Brigell, M.; Holder, G.E.; McCulloch, D.L.; Mizota, A.; Tormene, A.P. ISCEV standard for clinical visual evoked potentials: (2016 update). Doc. Ophthalmol. 2016, 133, 1–9. [Google Scholar] [CrossRef]
- Kawabata, H.; Murayama, K.; Adachi-Usami, E. Multifocal electroretinogram in myopia. Investig. Ophthalmol. Vis. Sci. 1996, 37, 2844–2851. [Google Scholar]
- Chen, J.C.; Brown, B.; Schmid, K.L. Delayed mfERG responses in myopia. Vis. Res. 2006, 46, 1221–1229. [Google Scholar] [CrossRef]
- Koh, V.; Tan, C.; Nah, G.; Zhao, P.; Yang, A.; Lin, S.T.; Wong, T.Y.; Saw, S.M.; Chia, A. Correlation of structural and electrophysiological changes in the retina of young high myopes. Ophthalmic Physiol. Opt. 2014, 34, 658–666. [Google Scholar] [CrossRef]
- Luu, C.D.; Foulds, W.S.; Tan, D.T. Features of the multifocal electroretinogram may predict the rate of myopia progression in children. Ophthalmology 2007, 114, 1433–1438. [Google Scholar] [CrossRef]
- Chen, J.F.; Elsner, A.E.; Burns, S.A.; Hansen, R.M.; Lou, P.L.; Kwong, K.K.; Fulton, A.B. The effect of eye shape on retinal responses. Clin. Vis. Sci. 1992, 7, 521–530. [Google Scholar]
- Chan, H.L.; Mohidin, N. Variation of multifocal electroretinogram with axial length. Ophthalmic Physiol. Opt. 2003, 23, 133–140. [Google Scholar] [CrossRef] [PubMed]
- Flitcroft, D.I. The complex interactions of retinal, optical and environmental factors in myopia aetiology. Prog. Retin. Eye Res. 2012, 31, 622–660. [Google Scholar] [CrossRef] [PubMed]
- Queirós, A.; González-Méijome, J.M.; Fernandes, P.; Jorge, J.; Almeida, J.B.; Parafita, M.A. Non-contact tonometry synchronized with cardiac rhythm and its relationship with blood pressure. Ophthalmic Physiol. Opt. 2006, 26, 384–391. [Google Scholar] [CrossRef] [PubMed]
- Lu, F.; Simpson, T.; Sorbara, L.; Fonn, D. The relationship between the treatment zone diameter and visual, optical and subjective performance in Corneal Refractive Therapy lens wearers. Ophthalmic Physiol. Opt. 2007, 27, 568–578. [Google Scholar] [CrossRef] [PubMed]
- Amorim-de-Sousa, A.; Moreira, L.; Macedo-de-Araújo, R.; Amorim, A.; Jorge, J.; Fernandes, P.R.; Queirós, A.; González-Méijome, J.M. Impact of contact lens materials on the mfERG response of the human retina. Doc. Ophthalmol. 2020, 140, 103–113. [Google Scholar] [CrossRef] [PubMed]
- Atchison, D.A. Optical models for human myopic eyes. Vis. Res. 2006, 46, 2236–2250. [Google Scholar] [CrossRef]
- Anders, L.M.; Heinrich, S.P.; Lagrèze, W.A.; Joachimsen, L. Little effect of 0.01% atropine eye drops as used in myopia prevention on the pattern electroretinogram. Doc. Ophthalmol. 2019, 138, 85–95. [Google Scholar] [CrossRef]
- Berman, M.S.; Seki, S. Blur-induced changes in the visual evoked potential. Optom. Vis. Sci. 1982, 59, 556–560. [Google Scholar] [CrossRef]
- Bobak, P.; Bodis-Wollner, I.; Guillory, S. The effect of blur and contrast of VEP latency: Comparison between check and sinusoidal grating patterns. Electroencephalogr. Clin. Neurophysiol. Evoked Potentials 1987, 68, 247–255. [Google Scholar] [CrossRef]
- Bartel, P.R.; Vos, A. Induced refractive errors and pattern electroretinograms and pattern visual evoked potentials: Implications for clinical assessments. Electroencephalogr. Clin. Neurophysiol. Evoked Potentials 1994, 92, 78–81. [Google Scholar] [CrossRef]
- Bach, M.; Mathieu, M. Different effect of dioptric defocus vs. light scatter on the Pattern Electroretinogram (PERG). Doc. Ophthalmol. 2004, 108, 99–106. [Google Scholar] [CrossRef] [PubMed]
- Anand, A.; De Moraes, C.G.V.; Teng, C.C.; Liebmann, J.M.; Ritch, R.; Tello, C. Short-duration transient visual evoked potential for objective measurement of refractive errors. Doc. Ophthalmol. 2011, 123, 141–147. [Google Scholar] [CrossRef] [PubMed]
- Hidajat, R.; Mclay, J.; Burley, C.; Elder, M.; Morton, J.; Goode, D. Influence of axial length of normal eyes on PERG. Doc. Ophthalmol. 2003, 107, 195–200. [Google Scholar] [CrossRef]
- Thompson, D.; Drasdo, N. The effect of stimulus contrast on the latency and amplitude of the pattern electroretinogram. Vis. Res. 1989, 29, 309–313. [Google Scholar] [CrossRef]
- Tobimatsu, S.; Celesia, G.G.; Cone, S.B. Effects of pupil diameter and luminance changes on pattern electroretinograms and visual evoked potentials. Clin. Vis. Sci. 1988, 2, 293–302. [Google Scholar]
- Yang, Y.R.; Zhao, J.L.; Xiao, F.; Zhao, H.X.; Dai, Y. Effect of high-order aberrations on pattern-reversal visual evoked potentials. Vis. Res. 2019, 161, 52–59. [Google Scholar] [CrossRef]

| M (D) | J0 (D) | J45 (D) | HCDVA 1 | LCDVA 2 | |
|---|---|---|---|---|---|
| Pre-treatment | −1.60 ± 0.35 | 0.05 ± 0.22 | −0.02 ± 0.21 | −0.09 ± 0.08 | 0.08 ± 0.08 |
| Post-treatment | −0.05 ± 0.36 | −0.03 ± 0.15 | 0.01 ± 0.24 | −0.11 ± 0.11 | 0.15 ± 0.13 |
| p | <0.001 * | >0.050 + | >0.050 + | <0.050 + | >0.050 + |
| Baseline | 1 Night | 15 Nights | 30 Nights | 60 Nights | p | ||
|---|---|---|---|---|---|---|---|
| Implicit time (ms) | N35 | 29.83 ± 3.72 | 29.18 ± 3.84 | 30.26 ± 2.07 | 30.03 ± 3.49 | 29.96 ± 2.56 | 0.649 + |
| P50 | 53.09 ± 3.45 | 51.13 ± 4.30 | 53.57 ± 2.78 | 52.69 ± 4.11 | 52.05 ± 2.86 | 0.032 + | |
| N95 | 93.04 ± 6.53 | 97.05 ± 9.26 | 93.52 ± 6.97 | 96.88 ± 6.17 | 98.14 ± 5.30 | (a) 0.008 + | |
| Amplitude (μV) | P50 | 3.68 ± 1.13 | 3.68 ± 1.11 | 4.09 ± 1.20 | 3.56 ± 0.90 | 3.70 ± 1.27 | 0.469 + |
| N95 | 5.09 ± 1.53 | 5.82 ± 1.93 | 6.26 ± 1.63 | 5.96 ± 1.64 | 6.04 ± 1.89 | 0.430 + |
| Baseline | 1 Night | 15 Nights | 30 Nights | 60 Nights | p (a) | ||
|---|---|---|---|---|---|---|---|
| Implicit time (ms) | N75 | 68.41 ± 5.26 | 70.36 ± 4.21 | 70.57 ± 3.85 | 71.22 ± 5.44 | 70.61 ± 3.70 | 0.681 + |
| P100 | 101.60 ± 4.96 | 102.41 ± 5.04 | 102.60 ± 4.51 | 104.35 ± 4.40 | 102.66 ± 5.04 | 0.118 * | |
| Amplitude (μV) | P100 | 15.45 ± 5.79 | 16.76 ± 6.46 | 15.68 ± 6.64 | 14.97 ± 6.11 | 16.90 ± 4.95 | 0.093 + |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Queirós, A.; Pereira-da-Mota, A.F.; Costa, J.; Amorim-de-Sousa, A.; Fernandes, P.R.B.; González-Méijome, J.M. Retinal Response of Low Myopes during Orthokeratology Treatment. J. Clin. Med. 2020, 9, 2649. https://doi.org/10.3390/jcm9082649
Queirós A, Pereira-da-Mota AF, Costa J, Amorim-de-Sousa A, Fernandes PRB, González-Méijome JM. Retinal Response of Low Myopes during Orthokeratology Treatment. Journal of Clinical Medicine. 2020; 9(8):2649. https://doi.org/10.3390/jcm9082649
Chicago/Turabian StyleQueirós, António, Ana F. Pereira-da-Mota, Jéssica Costa, Ana Amorim-de-Sousa, Paulo R. B. Fernandes, and José M. González-Méijome. 2020. "Retinal Response of Low Myopes during Orthokeratology Treatment" Journal of Clinical Medicine 9, no. 8: 2649. https://doi.org/10.3390/jcm9082649
APA StyleQueirós, A., Pereira-da-Mota, A. F., Costa, J., Amorim-de-Sousa, A., Fernandes, P. R. B., & González-Méijome, J. M. (2020). Retinal Response of Low Myopes during Orthokeratology Treatment. Journal of Clinical Medicine, 9(8), 2649. https://doi.org/10.3390/jcm9082649








